Abstract
The question of how to implement medical triages has become highly salient during the COVID-19 pandemic and continues to be actively discussed. It is important to know how members of the general public think about this issue. For one, knowledge about the public's standpoint can help resolve important questions where ethical considerations are by themselves not sufficient, for instance whether the patient's age should matter. It can also help identify if more communication with the public about medical ethics is needed. We study how members of the Swiss public would allocate intensive medical care among COVID-19 patients using data from two original conjoint survey experiments conducted in Switzerland in the context of the first and second pandemic waves in 2020 (N = 1457 & N = 1450). We find that our participants would not base triage decisions on the patient's age. However, they do give much importance to the patient's behavior prior and during illness, discriminate against non-nationals, and assign only a relatively small and inconsistent role to medical considerations. Our findings suggest that there is a need for more communication with the public about the ethics of medical triage.
Keywords: COVID-19, Pandemic triage, Intensive care, Attitudes, Survey, Conjoint experiment, Switzerland
1. Introduction
The question of how to implement medical triages has become highly salient during the COVID-19 pandemic. Unsurprisingly, many recent contributions have been concerned with the ethics of medical triage (e.g. Emanuel et al., 2020; Farrell et al., 2020; White and Lo, 2020), and medical associations in several countries have adapted existing triage guidelines or developed new ones (Ehni et al., 2021; Jöbges et al., 2020).
In discussions about the design of triage guidelines, medical, ethical, and legal considerations are obviously central. However, many have pointed out that it is also important to learn about the general public's attitudes toward pandemic triage or the rationing of medical care more generally (Biddison et al., 2019; Fallucchi et al., 2021; Kuylen et al., 2021; Neuberger and Ubel, 2000). For one, the existing medical ethics literature has identified not one but several different ethically permissible approaches to conducting triages (Biddison et al., 2019, p. 849), which have in part directly contradictory implications. One notable contradiction revolves around the role of the patient's age as a triage criterion. Age can be considered a criterion for triage based on the principle of maximizing benefits, according to which resources should be allocated in a way that saves the most lives or life-years. In this case, older patients could be de-prioritized because, all else equal, they tend to have more comorbidities and fewer life-years to gain (Emanuel et al., 2020). However, disadvantaging older patients in this way is of course problematic according to the principle of equal treatment and non-discrimination (Farrell et al., 2020). Existing guidelines differ considerably in how they consider age as a criterion (e.g. Ehni et al., 2021), which underscores the lack of consensus about how this issue should be resolved. In cases like this, the public's views can provide additional guidance.
A second reason for why knowledge about the public's views on pandemic triage is important is that the public's preferences might deviate in important respects from some accepted paradigms (e.g. Fallucchi et al., 2021). For example, ethical considerations and triage guidelines rule out discrimination based on the patient's gender, nationality, or prior behavior (Ehni et al., 2021; Jöbges et al., 2020) – but much research has shown that the public would base allocation decisions in part on precisely such non-permissible criteria, including whether patients contributed to their falling ill (Ubel et al., 2001; see also Petersen, 2012) or their nationality (Larsen and Schaeffer, 2020; O'Dell et al., 2019). Gender is also among the list of attributes on which the public tends to discriminate in the allocation of medical resources – notably to the advantage of women (Furnham, 1996).
Large deviations between guidelines and public sentiment may produce resentment (Fallucchi et al., 2021) and may also make the issue of medical triage vulnerable to politicization. A concrete example is the case of a Swiss academic, who during the COVID-19 pandemic publicly suggested that persons who violate social distancing rules should be registered and denied ICU treatment if they later contract the disease (Tagesanzeiger, 2020). To defuse such situations, communication with the public is needed, and research on public attitudes is crucial for such communication strategies to work (see also Lupia, 2013).
We contribute to research on popular attitudes toward pandemic triage by studying how members of the Swiss public would allocate beds in an intensive care unit (ICU) among COVID-19 patients, using data from original conjoint survey experiments (Hainmueller et al., 2014) conducted in Switzerland in the spring and fall of 2020.
2. Method
2.1. Experiment
Conjoint experiments are a widely used tool to study preferences and choice behavior. In conjoint experiments, participants evaluate a set of fictional persons or objects based on brief profiles containing information about a set of attributes of those persons or objects. Crucially, the precise attribute values of each profile are varied randomly so that each participant evaluates a different set of profiles, all with random attribute combinations. By letting many participants evaluate several different profiles with random attributes, researchers can disentangle the unique effect of each profile attribute on participants' evaluations (Hainmueller et al., 2014) – for instance, how a patient's age or gender affect their perceived deservingness to medical care.
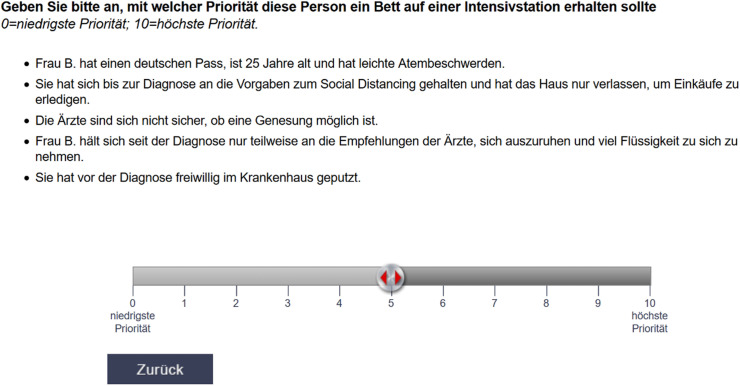
In our experiment, participants were presented with profiles of fictional COVID-19 patients and were asked to indicate on an integer 0–10 scale with which priority each patient should receive ICU treatment. Fig. 1 displays an example patient profile (in German) and the response scale as they would have been seen by the participants. Each participant rated two such profiles, one at a time.
Fig. 1.
Example rating task (German version).
The patient profiles varied in the attributes shown in Table 1 (we provide the exact formulations in our Supplement). These attributes and their respective values relate to several permissible and non-permissible criteria for pandemic triage. The two medical criteria (breathing difficulties, prognosis) are typically considered permissible triage criteria, whereas the patient's behavior, gender or nationality are all non-permissible (e.g. Ehni et al., 2021). Age is, as discussed above, particularly interesting since it can be considered permissible according to some ethical principles and guidelines but not according to others. Overall, this setup allows us to see on which criteria the public would base the allocation of critical medical care and how this differs from ethical guidelines.
Table 1.
Patient profile attributes.
| Attribute | Value |
|---|---|
| Gender | “Mr." |
| “Mrs." | |
| Age | 25 |
| 40 | |
| 55 | |
| 70 | |
| Nationality | Swiss |
| German/French (depending on participant's linguistic region) | |
| Turkish | |
| Nigerian | |
| Compliance with social distancing rules | Continued to meet family and friends in larger groups |
| Adhered fully and left house only to do groceries | |
| Compliance with treatment protocol | Complies fully with doctors' recommendations |
| Complies only partly | |
| Volunteering before illness | Did not volunteer |
| Cleaned in hospital | |
| Did groceries for elderly neighbors | |
| Breathing difficulties | Light |
| Moderate | |
| Severe | |
| Prognosis | Doctors see good chances of recovery |
| Doctors are not sure | |
| Doctors expect no recovery |
Each individual profile was a draw from the entire universe (or “full factorial”) of all possible combinations of patient attributes. The profiles were drawn based on a design plan generated with the SSI Web 8.4.8 software, using the “Complete Enumeration” algorithm. This algorithm randomizes profiles in a way that all attribute values are equally represented (e.g. about as many male as female patients) and that the attributes are uncorrelated with each other (Sawtooth Software, 2015).
Note that our design plan excluded two particular attribute combinations that we determined could be seen as implausible by our participants, namely being 70 years old and doing groceries for elderly neighbors, and having light breathing difficulties but no chance of recovery. Such seemingly implausible profiles can confuse participants or give them the impression that the experiment is broken, which can adversely affect the quality of the data. Therefore, implausible attribute combinations are usually excluded from conjoint designs (Hainmueller et al., 2014; Jasso, 2006).
2.2. Survey
We embedded this experiment within a larger survey on popular attitudes toward the COVID-19 pandemic in Switzerland (Gandenberger et al., 2020). Next to the experiment on attitudes toward pandemic triage we describe here, the survey included three additional conjoint experiments on attitudes toward travel restrictions, government aid to small companies, and health care policies (Fossati and Trein, 2021, Gandenberger et al., 2021). Also included were questions concerning the distribution of COVID vaccines (Knotz et al., 2021) and a range of other pandemic-related topics. Participants were also asked about their general political orientations and demographic attributes (see also https://idheapunitepolsoc.shinyapps.io/covid_dashboard).
Upon starting the survey, participants first received a brief general introduction to the survey and were advised about the confidentiality of their responses and their right to withdraw. Following this, they completed the four conjoint experiments in random order. Each conjoint experiment started with a brief introductory text explaining the task to be completed, followed by the experiment itself (see the Supplement for the instructions for the triage experiment). Immediately after the conjoint experiments, participants were asked how realistic they thought the last experiment they completed was, and how confident they felt when making their evaluations. Then they were asked further questions about the above-mentioned other topics.
We fielded this survey twice. The first round was fielded between April 22 and May 4, 2020, which was just after the peak of the first wave of the pandemic in Switzerland. The second round was fielded between November 19 and December 14, 2020, shortly after the peak of the second and more severe wave.
Our participants were recruited from an incentivized online panel operated by a European public opinion research and marketing firm (Bilendi). Participants received 2.40 and 2.30 CHF for participating in round one and two of our survey, respectively. Samples from incentivized online panels are increasingly widely used, including in studies very similar to ours (e.g. Fallucchi et al., 2021; O'Dell et al., 2019). Such samples are of course less representative than traditional probability samples (Yeager et al., 2011), but it has been shown that experiments produce very similar results regardless of whether they are run on samples from online panels or high-quality representative samples (e.g. Weinberg et al., 2014).
Participants were recruited from the online panel using quotas for age, gender (male, female), educational attainment, and linguistic region (German- or French-speaking). The quotas were based on official statistics. We obtained two diverse samples that resemble the Swiss population on key demographics: Participants were on average around 51 years old (round one: 51.6 years, st.dev. 18.1; round two: 51.3, st.dev. 17.3), and balanced by gender (50.1 percent female in round one; 49.3 percent female in round two). About three quarters of participants in both rounds were from the German-speaking region (round one: 74.1 percent; round two: 69.8 percent) with the remainder coming from the French-speaking region. About half of the participants completed advanced secondary education (Sekundarstufe II in the Swiss system; round one: 49.9 percent; round two: 52.1 percent) and a further around 40 percent had a tertiary degree (round one: 37.5 percent; round two: 40.1 percent). The remainder completed lower secondary education (Obligatorische Schule) or less. Most of our participants were Swiss (round one: 86.7 percent; round two: 85.7 percent), a combined around eight percent were German, French, Italian or Austrian citizens, and a further around five percent came from other countries; around 0.5 percent of participants did not state their nationality. We provide summary statistics of the key demographics of our samples and comparisons to official figures as well as an ethics statement in our Supplement.
1535 persons completed the first round of our survey. We excluded data from 78 participants who performed the triage experiment either very quickly (<5 s) or very slowly (>180 s). 1498 persons completed the second round of our survey, but we again we excluded 48 participants with very fast or very slow response times using the same criteria as before. This left us with samples of N = 1457 (round one) and N = 1450 (round two) for our analysis.
Note that our two samples overlap only partly (only around 60 percent of first-round participants also participated in the second round) and we therefore treat our data as separate cross-sections, not as panel data.
2.3. Statistical analysis
Our central quantity of interest are the average priority ratings for patient profiles with a particular attribute (e.g. a female patient), holding all other attributes constant. We computed these “marginal means” with 95 % confidence intervals using the estimator by Leeper et al. (2020).
We also performed several data quality checks. First, we inspected our data for carryover effects, which can arise when participants’ evaluations of the second profile they are shown are influenced by what they saw in the first profile (Hainmueller et al., 2014, p. 22). We did so by estimating a linear regression model that included covariates for all profile characteristics, each interacted with an indicator for the number of the rating task, and then testing the joint significance of all interaction terms using a Wald test. The test indicated that carryover effects are indeed present in our data from the first round (χ2 = 28.6, df = 15, p = 0.018). This problem did not appear in the data from the second round, however (χ2 = 19.3, df = 15, p = 0.2). We followed the recommendation by Hainmueller et al. (2014) to use only the data from the first rating task in our analysis. Note that we did this also in our analysis of the data from the second survey round to ensure the results are directly comparable across rounds. We show in our Supplement that the conclusions do not change if we use the data from both rating tasks from the second survey round.
We further used chi-squared tests and Cramer's V statistics to see if the randomization of profiles was successful and if the random assignment of profiles to participants was successful. In addition, we inspected the display frequencies of the different patient attributes to verify that all attributes were indeed represented in the profiles seen by the participants, and that no attributes were over- or underrepresented. We found no evidence of problems with the randomization of profile attributes or the random assignment of profiles to participants. These analyses and results are presented in detail in our Supplement.
Finally, we checked participants’ post-experimental evaluations of the realism of the patient profiles and their confidence in their own responses. Just over half of the participants in both rounds found the profiles realistic or very realistic, and a further around 30 percent found them at least somewhat realistic. 40 to 50 percent of the participants in both rounds were also sure or very sure about their responses, although a further ca. 40 percent of participants in both rounds were somewhat unsure. The latter is arguably to be expected given the difficult subject matter (see the Supplement for the detailed figures).
Replication data and code files for the R statistical software package are provided as supplementary materials.
3. Results
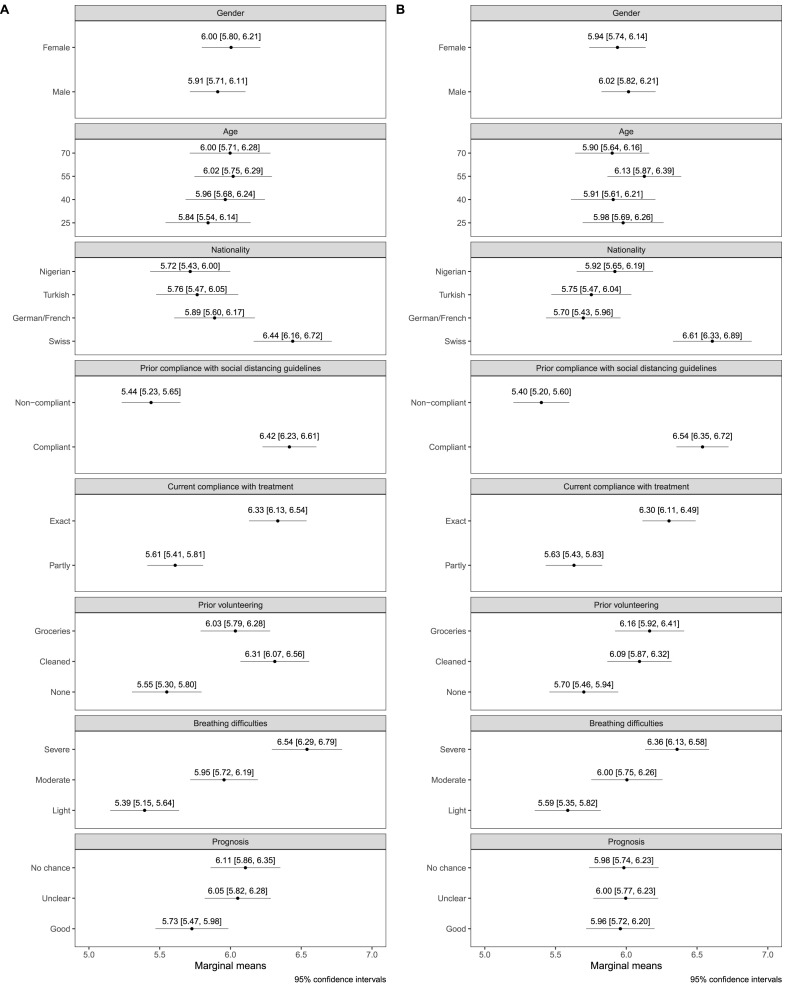
Fig. 2 presents the marginal mean estimates computed from the data from our two conjoint experiments. The results from the first round are presented in panel A, the results from the second round are presented in panel B.
Fig. 2.
Marginal average priority ratings.
A first notable finding is that participants did not discriminate based on gender, contrary to what could have been expected (Furnham, 1996). In both rounds, participants assigned, on average, very similar priority scores to both male and female patients. The fact that the confidence intervals enclose the respective other point estimate indicates that the difference is not significant.
We also find no evidence that participants prioritized either younger or older patients. In round one (panel A), the scores assigned to patients of different ages were all highly similar and enclosed in each other's confidence intervals. The same is true in the data from round two (panel B), even though 55-year-old patients received somewhat higher scores now. Overall, this indicates that participants did not use age as a criterion.
Matters are very different when looking at the role of the patient's nationality. Here, it is immediately apparent that participants had a very clear preference for patients with a Swiss nationality. In substantive terms, this means that participants were willing to discriminate against non-Swiss patients, all other patient attributes held equal.
The patient's behavior prior and during their illness also had strong effects on their perceived priority to receive ICU treatment. In both rounds, patients who did not fully comply with social distancing guidelines were given priority scores of about one point less compared to those who fully complied. The results are similar when it comes to patients' compliance with treatment protocols: patients who complied fully with their doctors’ recommendations were clearly given a higher priority compared to patients who did not. Furthermore, patients who engaged in volunteering before falling ill were given a higher priority than those who did not.
The two medical criteria, patients' breathing difficulties and their prognosis, mattered only partly. On the one hand, participants did pay attention to the patient's medical condition and clearly prioritized patients with severe breathing difficulties over those with moderate or light difficulties. However, at least in round one participants also ranked patients with a good prognosis as less deserving of treatment than patients whose prognosis is unclear or where there is no chance of a full recovery. This is not the case in round two, where there were no appreciable differences between patients with different prognoses. Overall, participants did base their triage decisions on medical need, but less on who had likely most to gain from receiving treatment.
4. Discussion & conclusion
Members of the Swiss public would conduct a medical triage of COVID-19 patients only partly in line with medical guidelines. Overall, participants gave considerable weight to non-medical criteria such as whether patients adhered to social distancing guidelines and volunteered before falling ill, or if they complied with their doctors' recommendations. There was also clear bias against foreign nationals. However, participants did not discriminate based on gender and, more importantly, did not use the patient's age as a criterion. Medical criteria did play a role, but not consistently. Notably, and contrary to existing guidelines (Jöbges et al., 2020, p. 8), participants would not prioritize patients based on their prognoses. The latter could indicate that participants were hesitant about allocating medical care based on the rather “cold and rational” principle of maximizing benefits. At a minimum, participants did not seem to rely on this principle intuitively. These patterns were generally stable across the two rounds of our survey.
Our findings have two main implications. One concerns the design of triage guidelines, where ethical considerations alone often do not produce clear-cut answers, for instance concerning the relevance of the patient's age (e.g. Emanuel et al., 2020; Farrell et al., 2020). Our finding that members of the Swiss public would not base triage decisions on the patient's age, in combination with similar results from other countries (Kuylen et al., 2021), lends support to voices that suggest caution in using age as a criterion (Farrell et al., 2020). Our findings also suggest that there might be a discrepancy between Swiss public sentiment and the existing Swiss guidelines (Scheidegger et al., 2020), according to which age is considered under some conditions.
The second main implication concerns communication with the public. Our participants clearly diverge from accepted ethical standards in that they would be willing to discriminate against foreigners and would allocate medical treatment based on patients’ behavior. Clearly, there is a need for communication about applicable ethical standards and their rationales to not leave these gaps between public sentiment and official practice vulnerable to politicization. In this respect, our conclusions echo those of Fallucchi et al. (2021).
Our study has of course also some limitations. For one, our study covered only a single European country, and it is not self-evident that our findings generalize to other contexts. However, several related studies from other countries have produced similar results. In the UK, Kuylen et al. (2021) found, as mentioned above, that the public is reluctant to use age as a criterion for pandemic triage. In addition, Larsen and Schaeffer (2020) found similar to us a pronounced tendency to discriminate against foreigners in the allocation of medical care in Denmark. More generally, our findings are similar to those from the above-mentioned research on public attitudes toward the allocation of scarce medical resources in the United States, which has found that the public prioritizes patients who did not cause their illness themselves and who are fellow nationals (O'Dell et al., 2019; Ubel et al., 2001). We therefore suggest that our findings are also of relevance outside of the Swiss context.
A further limitation of our study is that our experiment only simulated the situation where an initial decision about whom to treat is made – but not the arguably even more problematic case in which treatment must be withdrawn from one patient in favor of another. Others have already pointed out that this is an aspect where more guidance is needed (White and Lo, 2020), and we suggest that future public opinion research could provide one important type of input here. Finally, we did also not consider if there is variation between groups of participants in how they would prefer to administer pandemic triage. We think this could also be a fruitful avenue for future research. In particular the willingness to discriminate against foreigners might be more pronounced among those with ethnocentrist (Hainmueller et al., 2014) or authoritarian personality traits (Feldman, 2003).
Credit author statement
Carlo M. Knotz: Conceptualization, Investigation, Data curation, Writing – Original draft, Writing – Review & Editing, Visualization, Mia Gandenberger: Conceptualization, Investigation, Data curation, Writing – Original draft, Writing – Review & Editing, Visualization, Project administration, Flavia Fossati: Conceptualization, Investigation, Data curation, Writing – Original draft, Writing – Review & Editing, Resources, Supervision, Funding Acquisition, Giuliano Bonoli: Conceptualization, Investigation, Writing – Original draft, Writing – Review & Editing, Resources, Supervision, Funding Acquisition.
Acknowledgments
This research was supported by the National Centre of Competence in Research for Migration and Mobility studies (NCCR – on the move), which is funded by the Swiss National Science Foundation (SNSF Project No. 51NF40-182897).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.114238.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Biddison E.L.D., Faden R., Gwon H.S., Mareiniss D.P., Regenberg A.C., Schoch-Spana M., Schwartz J., Toner E.S. Too many patients…A framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155:848–854. doi: 10.1016/j.chest.2018.09.025. [DOI] [PubMed] [Google Scholar]
- Ehni H.-J., Wiesing U., Ranisch R. Saving the most lives—a comparison of European triage guidelines in the context of the COVID-19 pandemic. Bioethics. 2021;35:125–134. doi: 10.1111/bioe.12836. [DOI] [PubMed] [Google Scholar]
- Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A., Zhang C., Boyle C., Smith M., Phillips J.P. Fair allocation of scarce medical resources in the time of covid-19. N. Engl. J. Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Fallucchi F., Faravelli M., Quercia S. Fair allocation of scarce medical resources in the time of COVID-19: what do people think? J. Med. Ethics. 2021;47:3–6. doi: 10.1136/medethics-2020-106524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell T.W., Francis L., Brown T., Ferrante L.E., Widera E., Rhodes R., Rosen T., Hwang U., Witt L.J., Thothala N., Liu S.W., Vitale C.A., Braun U.K., Stephens C., Saliba D. Rationing limited healthcare resources in the COVID-19 era and beyond: ethical considerations regarding older adults. J. Am. Geriatr. Soc. 2020;68:1143–1149. doi: 10.1111/jgs.16539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman S. Enforcing social conformity: a theory of authoritarianism. Polit. Psychol. 2003;24:41–74. [Google Scholar]
- Fossati F., Trein P. University of Lausanne; 2021. Protection but no Control: The Micro-Foundations of Democratic Crisis Governance. Under Review. [Google Scholar]
- Furnham A. Factors relating to the allocation of medical resources. J. Soc. Behav. Pers. 1996;11:615–624. [PubMed] [Google Scholar]
- Gandenberger M., Knotz C., Fossati F., Bonoli G. University of Lausanne; 2021. Conditional Solidarity - Attitudes towards support for others during the 2020 COVID-19 pandemic. Under Review. [Google Scholar]
- Gandenberger M., Trein P., Knotz C., Fossati F., Bonoli G., Varone F. Lausanne & Neuchâtel : IDHEAP, Université de Lausanne & NCCR - on the move; 2020. The IDHEAP/NCCR-on the move survey “Solidarity in times of crisis”. [Google Scholar]
- Hainmueller J., Hopkins D.J., Yamamoto T. Causal inference in conjoint analysis: understanding multidimensional choices via stated preference experiments. Polit. Anal. 2014;22:1–30. [Google Scholar]
- Jasso G. Factorial survey methods for studying beliefs and judgments. Socio. Methods Res. 2006;34:334–423. [Google Scholar]
- Jöbges S., Vinay R., Luyckx V.A., Biller‐Andorno N. Recommendations on COVID-19 triage: international comparison and ethical analysis. Bioethics. 2020;34:948–959. doi: 10.1111/bioe.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knotz C., Gandenberger M., Fossati F., Bonoli G. Popular Attitudes Toward the Distribution of Vaccines Against COVID-19: The Swiss Case. Swiss Political Science Review. 2021;27(2):297–310. doi: 10.1111/spsr.12461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuylen M.N.I., Kim S.Y., Keene A.R., Owen G.S. Should age matter in COVID-19 triage? A deliberative study. J. Med. Ethics. 2021;47:291–295. doi: 10.1136/medethics-2020-107071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen M.H., Schaeffer M. Healthcare chauvinism during the COVID-19 pandemic. J. Ethnic Migrat. Stud. 2020:1–19. 0. [Google Scholar]
- Leeper T.J., Hobolt S.B., Tilley J. Measuring subgroup preferences in conjoint experiments. Polit. Anal. 2020;28:207–221. [Google Scholar]
- Lupia A. Communicating science in politicized environments. Proc. Natl. Acad. Sci. Unit. States Am. 2013;110:14048–14054. doi: 10.1073/pnas.1212726110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuberger J., Ubel P.A. Finding a place for public preferences in liver allocation decisions. Transplantation. 2000;70:1411–1413. doi: 10.1097/00007890-200011270-00001. [DOI] [PubMed] [Google Scholar]
- O'Dell H.W., McMichael B.J., Lee S., Karp J.L., VanHorn R.L., Karp S.J. Public attitudes toward contemporary issues in liver allocation. Am. J. Transplant. 2019;19:1212–1217. doi: 10.1111/ajt.15227. [DOI] [PubMed] [Google Scholar]
- Petersen M.B. Social welfare as small-scale help: evolutionary psychology and the deservingness heuristic. Am. J. Polit. Sci. 2012;56:1–16. doi: 10.1111/j.1540-5907.2011.00545.x. [DOI] [PubMed] [Google Scholar]
- Sawtooth Software . 2015. SSI Web 8.4.8. [Google Scholar]
- Scheidegger D., Fumeaux T., Samia H., Salathé M. COVID-19 pandemic: triage for intensive-care treatment under resource scarcity. Swiss Med. Wkly. 2020;150 doi: 10.4414/smw.2020.20229. [DOI] [PubMed] [Google Scholar]
- Tagesanzeiger . 2020. Corona-Skeptiker verwirken ihr Recht auf einen Intensivplatz bei Engpässen.https://www.tagesanzeiger.ch/corona-skeptiker-verwirken-ihr-recht-auf-einen-intensivplatz-bei-engpaessen-229138575079 [Google Scholar]
- Ubel P.A., Jepson C., Baron J., Mohr T., McMorrow S., Asch D.A. Allocation of transplantable organs: do people want to punish patients for causing their illness? Liver Transplant. 2001;7:600–607. doi: 10.1053/jlts.2001.25361. [DOI] [PubMed] [Google Scholar]
- Weinberg J., Freese J., McElhattan D. Comparing data characteristics and results of an online factorial survey between a population-based and a crowdsource-recruited sample. SocScience. 2014;1:292–310. [Google Scholar]
- White D.B., Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. J. Am. Med. Assoc. 2020;323:1773–1774. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]
- Yeager D.S., Krosnick J.A., Chang L., Javitz H.S., Levendusky M.S., Simpser A., Wang R. Comparing the accuracy of RDD telephone surveys and internet surveys conducted with probability and non-probability samples. Publ. Opin. Q. 2011;75:709–747. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.