Abstract
Discoid lateral meniscus (DLM) is a rare meniscal variant characterized by an increased amount of meniscal tissue that resembles the shape of a disc as opposed to the typical crescent shape of the lateral meniscus. Surgical intervention is recommended for symptomatic DLM with persistent pain, mechanical symptoms, or motion impairment. The technique described is a reliable and reproducible method to identify and treat intrasubstance degeneration (ID) in the setting of DLM. A small arthroscope is used that allows more room for a meniscal repair device, as well as improved visualization and access of the lateral compartment. An accessory medial portal is used that allows perpendicular access to the anterior half of the body, as well as the posterior aspect of the anterior horn for repair. Successful surgery with this technique preserves meniscus and produces a strong reliable all-meniscal based repair of ID that allows early weight bearing and range of motion postoperatively.
Technique Video
Demonstration of our technique for saucerization of a symptomatic discoid lateral meniscus and repair of intrasubstance degeneration. The video highlights the use of a small arthroscope to better visualize the lateral compartment during all-inside meniscus-based repair. We also demonstrate the use of an accessory medial portal that allows perpendicular access to the tear with our repair device.
Introduction
The discoid lateral meniscus (DLM) is a rare meniscal variant characterized by an increased amount of meniscal tissue that more resembles the shape of a disc, as opposed to the typical crescentic shape of the lateral meniscus.1 This disc-shaped meniscus often occupies the majority or entirety of the lateral tibiofemoral compartment. The DLM can also have absent meniscotibial ligaments that cause meniscus hypermobility.2 Further, there is often an altered and erratic collagen arrangement within the discoid meniscus that can lead to atraumatic degeneration.3, 4, 5 These “three S’s” of the discoid meniscus are size, stability, and micro-structure, and these are responsible for the typical presenting symptoms, which include pain, mechanical symptoms (typically, a clunk during range of motion), and flexion contracture. Magnetic resonance imaging (MRI) may also show an area of increased T2 signal enhancement within the meniscus. When a DLM becomes symptomatic, surgical treatment is typically necessary.6,7 Standard treatment includes arthroscopic saucerization and repair/stabilization, as needed.2,8, 9, 10 When intrasubstance degeneration (ID) is present, it is often not seen until near completion of saucerization because of its presence on the outer portion of the meniscus. The meniscus will typically split into a superior and inferior leaflet, and the decision has to be made to repair them or resect one or both based on intraoperative assessment of thickness and tissue quality. This technique article describes a method for saucerization and repair using a small arthroscope and an accessory medial portal. This technique represents a modification to a similar technique published previously.11
Indications
Briefly, surgical indications are made from history, physical exam, and imaging findings. Patients often have lateral knee pain with or without mechanical symptoms, and MRI invariably shows an enlarged meniscus with high T2 signal (Fig 1). The meniscus may also show displacement in any direction, and there may be additional tearing present. If there is persistent pain, mechanical symptoms or a block to full motion of the knee, surgical intervention is recommended. The technique below describes treatment of isolated ID. If there is peripheral instability and/or tearing present, it can be treated accordingly, and the treatment of the ID can be incorporated.
Fig 1.
Representative MRI image from a T2 coronal series of a left knee demonstrating an enlarged lateral meniscus with intrasubstance high signal intensity (arrow).
Surgical Technique
The patient is positioned supine on the operating table with standard arthroscopic set up per surgeon preference. Our preference is to perform the surgery under tourniquet control on a flat table with the leg in a figure four position to increase access to the lateral compartment. Diagnostic arthroscopy is carried out using a standard anterolateral viewing portal using a small 1.9 mm 0° arthroscope (NanoScope, Arthrex, Naples, FL). This smaller arthroscope has an easier time getting between the femoral condyle and the superior surface of the meniscus to improve visualization throughout the compartment (Fig 2). A standard anteromedial working portal is used for probing and instrumentation. The discoid meniscus is assessed for any peripheral instability or tearing. If there is any ID, it will not typically be encountered at this time, as it is usually located peripherally, and the superior surface of the meniscus will often look normal. Using a standard arthroscopic punch or a small arthroscopic punch (NanoBiter, Arthrex, Naples, FL), the saucerization is carried out in standard fashion. As a general rule, the saucerization is complete once 8-10 mm of peripheral meniscal tissue is present for adolescent or adult patients and 6-7 mm for pediatric patients. Sometimes the anterior horn tissue will be difficult to resect with a biter and an 11-blade scalpel can be introduced through the anteromedial portal to assist in resection (Fig 3).
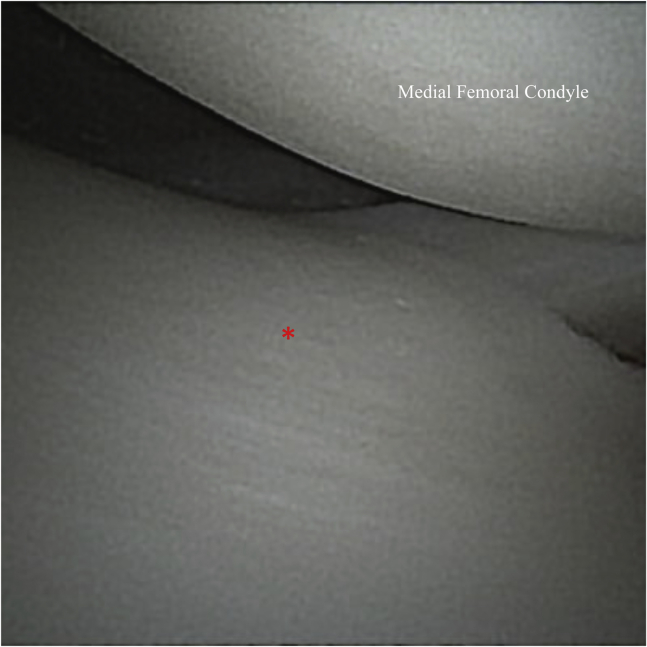
Fig 2.
View of the medial compartment of a left knee, with intact medial meniscus (asterisk), from the standard anterolateral viewing portal using a small, 1.9-mm, 0-degree arthroscope. The smaller scope can provide improved access and visualization, while minimizing risk of iatrogenic injury.
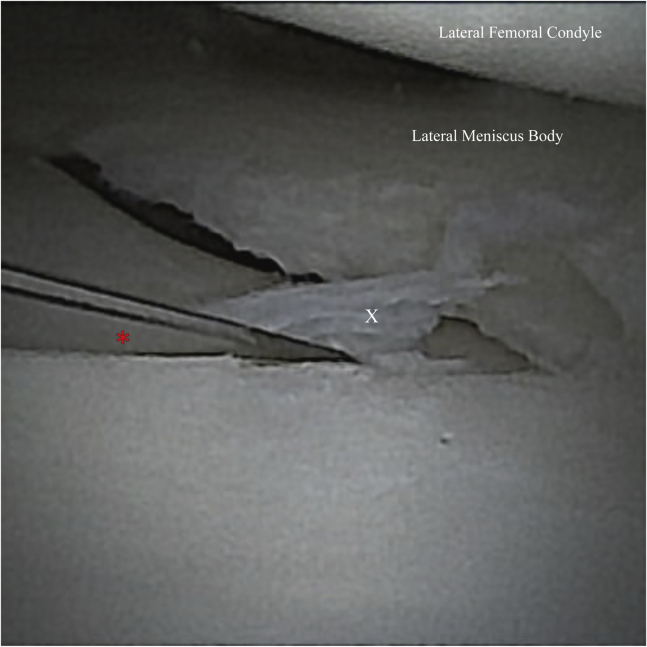
Fig 3.
Arthroscopic image viewing from the anterolateral portal during saucerization of the lateral meniscus. While performing the saucerization, resection of the lateral meniscus anterior horn tissue (X) with an arthroscopic biter can be difficult. Careful use of a #11 blade (asterisk), introduced through the anteromedial portal, is useful during this step.
After completion of saucerization, the arthroscope is placed through the anteromedial portal and a probe is placed through the anterolateral portal. The free edge of the meniscus is probed for ID (Fig 4). Often, the degeneration will already have presented itself during saucerization, and the meniscus will have a superior and inferior leaflet (Fig 5). Other times, the degeneration will be less obvious, and a probe will be needed to determine its presence. The location of the ID is typically in the body with variable extension into the anterior and posterior horns. The probe is used to determine the extent of the ID. There is typically loose and irregular tissue within the leaflets that is resected at this time with an arthroscopic shaver, typically through the anteromedial portal. At this point, the leaflets are assessed for feasibility of repair, as well as thickness. If one leaflet is patently unhealthy or damaged, it may need to be resected. Likewise, if the DLM is very thick, which is common when a flexion contracture is present, one of the leaflets may need to be resected to debulk the compartment. If both leaflets are deemed healthy, arthroscopic repair is commenced.
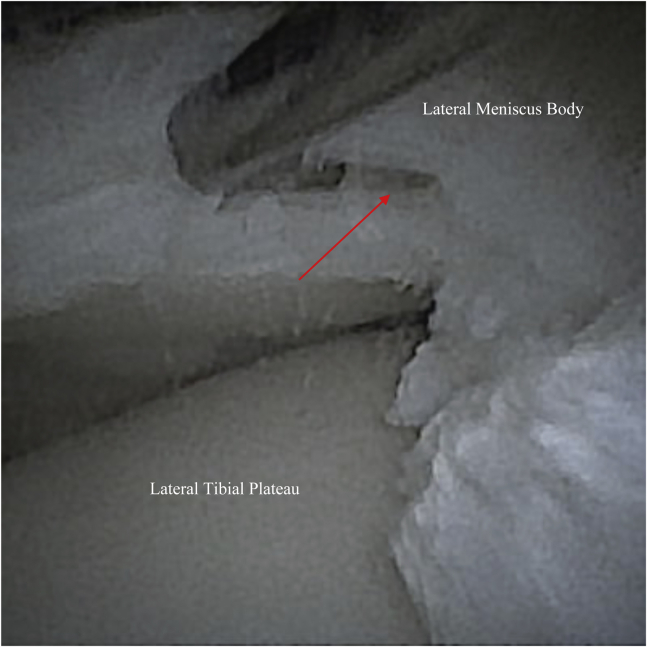
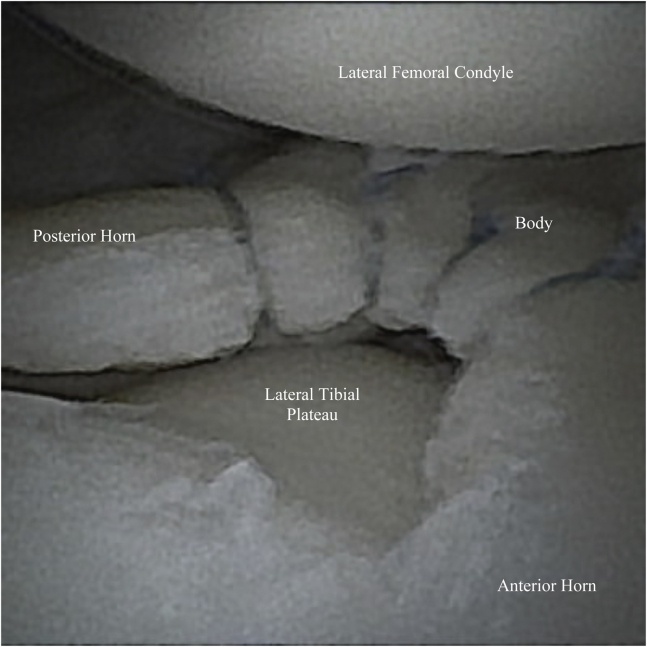
Fig 4.
After saucerization is complete, the scope is switched to the anteromedial portal and a probe is introduced through the anterolateral portal. The free edge of the meniscus is probed to identify intrasubstance degeneration (arrow).
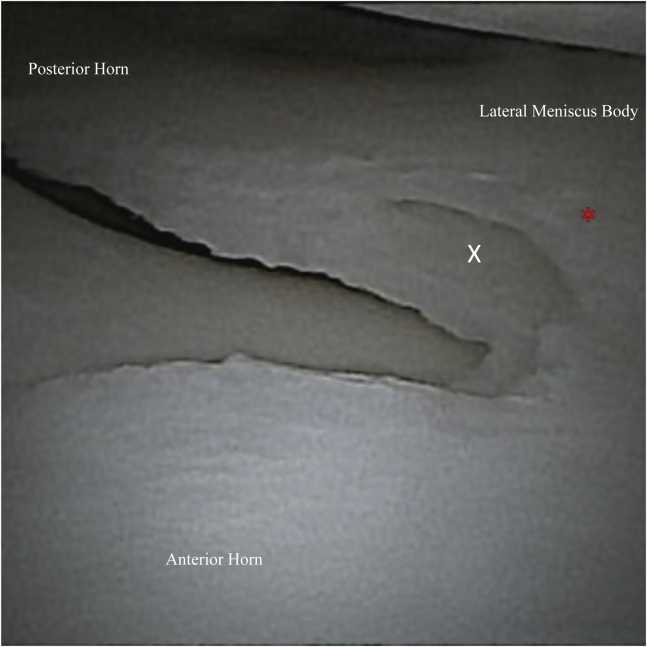
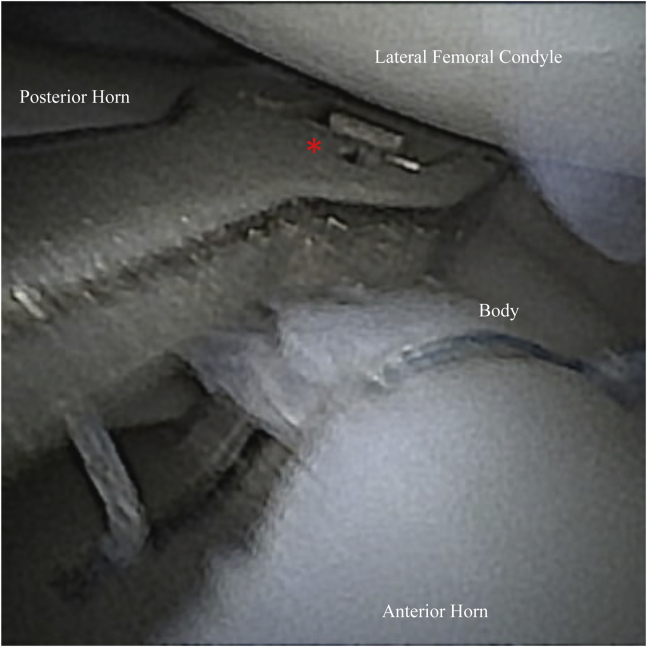
Fig 5.
Left knee arthroscopy view from the anterolateral portal of the lateral discoid meniscus showing intrasubstance degeneration and superior (asterisk) and inferior (X) leaflets revealed during saucerization.
Using a spinal needle for localization, an accessory far medial portal is established just anterior to the medial femoral condyle. This allows perpendicular access to the more anterior aspect of the meniscus and ID (Fig 6, Fig 7, Fig 8, Fig 9). Using an all-inside meniscus-based repair device (Knee Scorpion, Arthrex, Naples, FL) approximation and compression of the two leaflets is commenced through this accessory portal. A nonabsorbable suture in the size range of 0 to 2-0 is ideal for all inside meniscus-based repair. Our preference is to use a small 0.9-mm suture tape (Mini SutureTape, Arthrex, Naples, FL) for more broad compression. At this point, the arthroscope is viewing from the anteromedial portal. This allows improved visualization of the more anterior aspect of the meniscus. The small arthroscope is advantageous here, as it causes significantly less crowding of the meniscus repair device compared to a standard 4.0-mm arthroscope. A single pass of suture is placed through the more peripheral aspect of the ID to ensure complete closure, and the suture is tied in a 360° compression, or haybale, fashion (Fig 10, Fig 11). Sutures are typically placed 4-5 mm apart from each other. A helpful way to determine this is to place the jaws of the repair device adjacent to the last stitch placed (Fig 12). This will typically yield an optimal spacing of suture (Fig 13). As the repair proceeds posteriorly, the repair device can be switched from the accessory medial portal to the standard anteromedial portal, and the arthroscope will correspondingly be placed in the anterolateral portal. After completion of the repair, marrow venting is routinely performed as a biologic augment. We prefer to introduce a 0.62 Kirschner wire percutaneously into the nonchondral portion of the medial femoral condyle (Fig 14). This approach allows for a superior number of vents to be placed compared to the intercondylar notch. We routinely create 10-15 venting sites. At the completion of the case, wounds are closed in standard fashion. Video 1 details the surgical procedure as well.
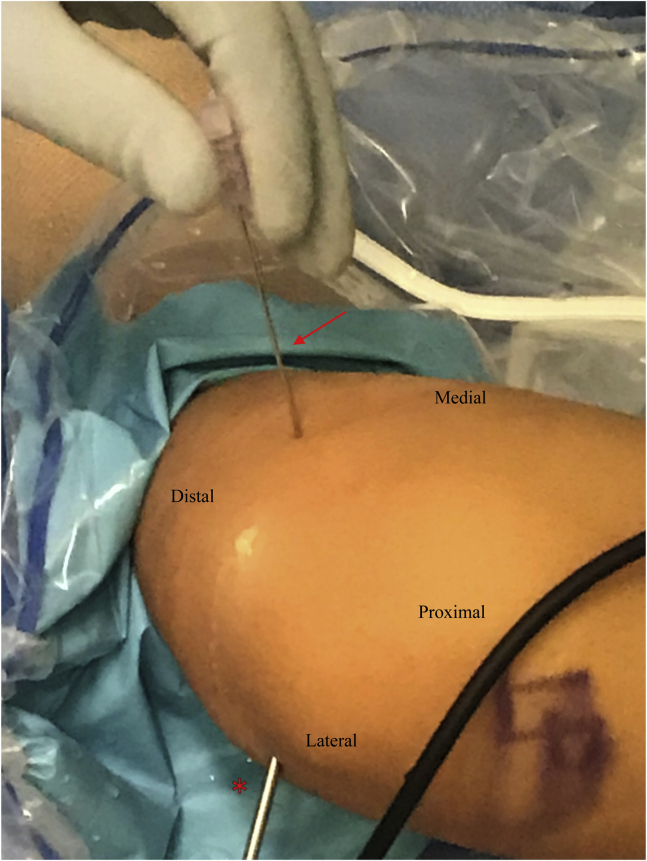
Fig 6.
A spinal needle (arrow) is used for localization of the far medial portal just anterior to the media femoral condyle (Fig 7). The scope is kept in the anterolateral portal for direct visualization (asterisk).
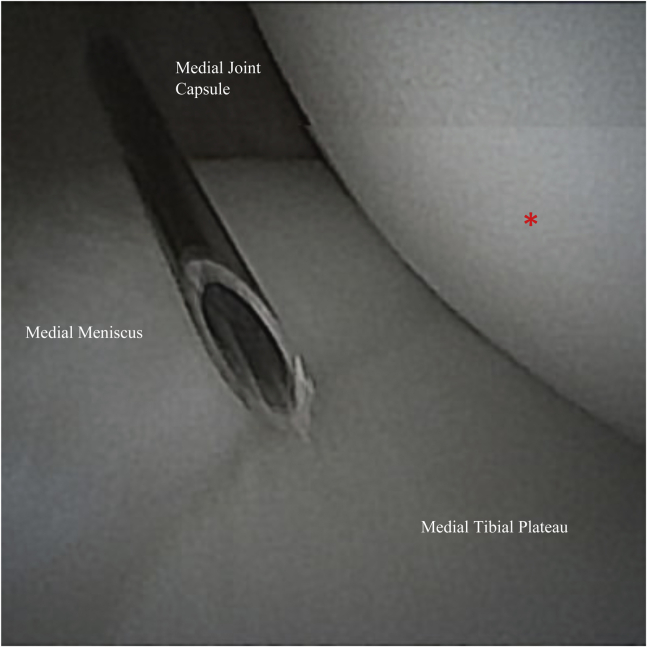
Fig 7.
Intraarticular view from the anterolateral portal during localization of the accessory far medial portal. The spinal needle is used to confirm safe access across the joint into the lateral compartment. Clearance of the medial femoral condyle (asterisk) is key to avoiding injury to the articular cartilage and allowing desired access to the body of the lateral meniscus.
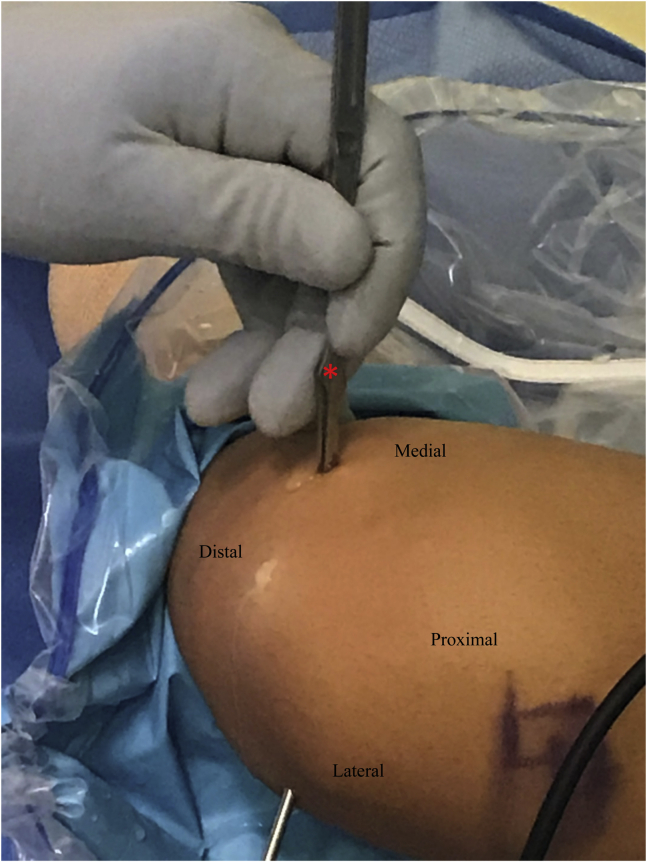
Fig 8.
After spinal need localization (Figs 6 and 7), the far medial portal is made using a #11 blade (asterisk).
Fig 9.
The repair device loaded with high tensile strength nonabsorbable suture (asterisk) is introduced through the far medial portal and carefully brought across the joint into the lateral compartment.
Fig 10.
Viewing with the small arthroscope from the anteromedial portal, the repair device (asterisk) is brought through the accessory medial portal, and a single suture pass is made in the peripheral aspect of the intrasubstance degeneration of the lateral meniscus to ensure complete closure of the separate leaflets.
Fig 11.
Arthroscopic image viewing from the standard anteromedial portal. Following passing of the repair stitch using the repair device (Fig 10), the suture is tied in a 360° compression, or haybale, fashion. The suture tails are then cut prior to placement of the next stitch.
Fig 12.
Sutures are placed approximately 4-5 mm apart from each other. Positioning the jaws of the repair device (asterisk) adjacent to the last stitch placed is helpful in achieving proper spacing of the sutures.
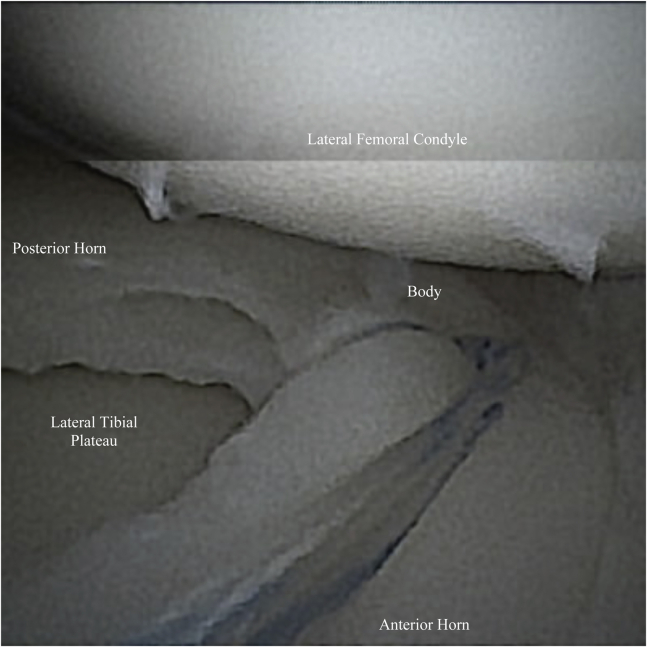
Fig 13.
View from the anteromedial portal of the final repair construct showing proper spacing of the sutures, approximately 4-5 mm apart. The intrasubstance degeneration has been sealed with the use of multiple 360 degree compression sutures.
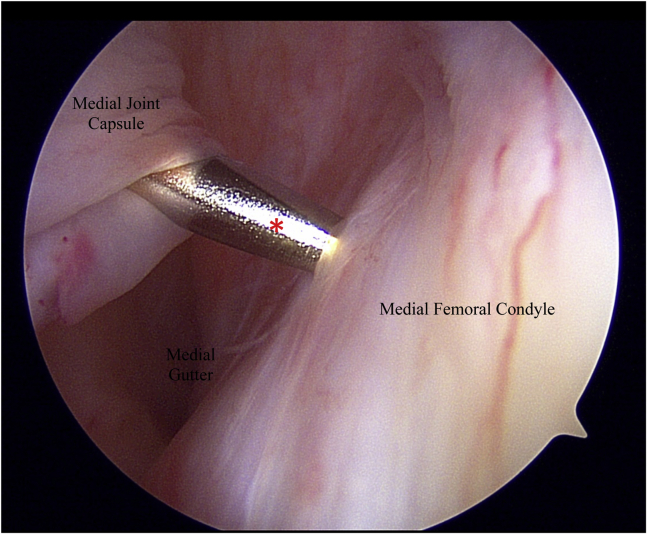
Fig 14.
Marrow venting is performed as a biologic augment to the repair. A 0.62 Kirshner wire (asterisk) is inserted percutaneously into the nonchondral portion of the medial femoral condyle. Typically, 10-15 venting sites are established.
Postoperatively, the patient is allowed to weight bear as tolerated with full knee motion. Because all of the fixation is contained within the meniscus and is not anchored on the capsule, normal meniscal translation during knee range of motion does not stress the repair. If there are other tears present that require repair, any restrictions are based on that aspect of the surgery. If rehab progresses smoothly, impact activities are typically resumed between 3 and 6 months after surgery. Table 1 describes pearls and pitfalls associated with this technique.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Switching the viewing and working portals often will improve visualization and diagnosis of pathology. In particular, viewing from a medial portal will improve visualization of the anterior horn. | The extent of intrasubstance degeneration may not be fully appreciated, especially in the anterior horn. The arthroscope will need to view from the anteromedial or the far medial accessory portal while probing through the anterolateral portal to effectively determine this. |
| Make sure to probe the periphery of the meniscus before and after saucerization to confirm the presence or absence of any peripheral instability. | Failure to resect enough meniscus tissue may leave a patient with persistent mechanical symptoms and may fail to expose any intrasubstance degeneration. A general guideline is to leave 8-10 mm. |
| Once saucerization is complete, probe the free edge of the meniscus, particularly in the body, to see whether there is any subtle intrasubstance degeneration. It may not always be immediately apparent. | If too few sutures are placed, the area of intrasubstance degeneration may not be adequately closed down, which will allow synovial fluid to get into the space and prevent healing. Space the sutures no more than 5 mm apart to adequately close down the space. |
Discussion
DLM is a rare meniscal variant that can cause significant morbidity and is often encountered in younger patients. Because of the broad and persistent symptoms, the DLM can cause, surgical intervention is often necessary. Intrasubstance degeneration is a common finding in a complete DLM and can create a dilemma for the treating surgeon who has to determine whether to repair or resect. As a general rule, preservation of as much meniscal tissue as possible is preferred for long-term joint health, thus repair should be considered as a first option.2,6,8,9,12,13
The technique described here is a straightforward, reproducible, and advantageous method to identify and treat ID in the setting of a DLM. First, the use of a small arthroscope allows for better access and visualization of the lateral compartment. Given that a DLM often becomes symptomatic in a patient who may be a child or young adolescent, access to the lateral compartment may already be tight, even before the extra tissue present in a DLM is considered. Further, the small arthroscope creates more room for meniscal repair devices and can get much closer to the site of repair. This improves visualization and allows for more precise placement of meniscus repair constructs. The small arthroscope also has an obvious advantage in this situation to cause less iatrogenic chondral damage.
The accessory medial portal has become a workhorse portal in our hands to treat the DLM, as well as several different tear types in the body of a nondiscoid lateral meniscus. It allows perpendicular access to the anterior half of the body, as well as the posterior aspect of the anterior horn of the meniscus. In addition to its use as a working portal, viewing through this portal is also helpful, as it provides superior visualization of the anterior horn of the lateral meniscus.
Preservation of meniscus tissue in the setting of a DLM is inconsistent with regard to outcome. There is a considerably high reoperation rate after index surgery for a DLM. However, the literature is unclear as to the nature and technical aspects of treatment.9,10,12,14 Regardless, a thoughtful and careful attempt at preservation of meniscal tissue should be attempted in these situations, and the literature has yet to offer a valid alternative. Although the frequency in which ID is encountered is unclear, having a reliable protocol for treatment is key to retaining a maximum amount of meniscus tissue. Using an all-inside meniscus-based repair technique provides superior biomechanical compression and is technically very straightforward to perform. It is worth noting that the knot stacks from this repair technique do not cause chondral damage on the femoral condyles. Although the exact process is unclear, it seems as though the weightbearing function of the knee causes the knots to become incorporated into the adjacent meniscus tissue and the knots are often not visible on second-look arthroscopy. Thus, the technique detailed here represents a reliable way to treat intrasubstance degeneration in the setting of a discoid lateral meniscus.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.P. reports grants and personal fees from Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Demonstration of our technique for saucerization of a symptomatic discoid lateral meniscus and repair of intrasubstance degeneration. The video highlights the use of a small arthroscope to better visualize the lateral compartment during all-inside meniscus-based repair. We also demonstrate the use of an accessory medial portal that allows perpendicular access to the tear with our repair device.
References
- 1.Kramer D.E., Micheli L.J. Meniscal tears and discoid meniscus in children: Diagnosis and treatment. J Am Acad Orthop Sur. 2009;17:698–707. doi: 10.5435/00124635-200911000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Good C.R., Green D.W., Griffith M.H., Valen A.W., Widmann R.F., Rodeo S.A. Arthroscopic treatment of symptomatic discoid meniscus in children: Classification, technique, and results. Arthroscopy. 2007;23:157–163. doi: 10.1016/j.arthro.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Atay O.A., Pekmezci M., Doral M.N., Sargon M.F., Ayvaz M., Johnson D.L. Discoid meniscus: An ultrastructural study with transmission electron microscopy. Am J Sports Med. 2007;35:475–478. doi: 10.1177/0363546506294678. [DOI] [PubMed] [Google Scholar]
- 4.Choi Y.-H., Seo Y.-J., Ha J.M., Jung K.H., Kim J., Song S.Y. Collagenous ultrastructure of the discoid meniscus: A transmission electron microscopy study. Am J Sports Med. 2017;45:598–603. doi: 10.1177/0363546516674181. [DOI] [PubMed] [Google Scholar]
- 5.Papadopoulos A., Kirkos J.M., Kapetanos G.A. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25:262–268. doi: 10.1016/j.arthro.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Grimm N.L., Pace J.L., Levy B.J., et al. Demographics and epidemiology of discoid menisci of the knee: Analysis of a large regional insurance database. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120950669. 23259671209506692020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sabbag O.D., Hevesi M., Sanders T.L., et al. Incidence and treatment trends of symptomatic discoid lateral menisci: An 18-year population-based study. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118797886. 2325967118797886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho W.-J., Kim J.-M., Lee B.-S., Kim H.-J., Bin S.-I. Discoid lateral meniscus: A simple horizontal tear was associated with less articular cartilage degeneration compared to other types of tear. Knee Surg Sports Traumatol Arthrosc. 2019;27:3390–3395. doi: 10.1007/s00167-019-05363-z. [DOI] [PubMed] [Google Scholar]
- 9.Ng Y.H., Tan S.H.S., Lim A.K.S., Hui J.H. Meniscoplasty leads to good mid-term to long-term outcomes for children and adolescents with discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2021;2:352–357. doi: 10.1007/s00167-020-05929-2. [DOI] [PubMed] [Google Scholar]
- 10.Smuin D.M., Swenson R.D., Dhawan A. Saucerization versus complete resection of a symptomatic discoid lateral meniscus at short- and long-term follow-up: A systematic review. Arthroscopy. 2017;33:1733–1742. doi: 10.1016/j.arthro.2017.03.028. [DOI] [PubMed] [Google Scholar]
- 11.Zuke W.A., Cvetanovich G.L., Go B., Forsythe B. Arthroscopic saucerization and all-inside repair of a delaminated discoid lateral meniscus. Arthrosc Techniques. 2017;6:e1387–e1391. doi: 10.1016/j.eats.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabbag O.D., Hevesi M., Sanders T.L., et al. High rate of recurrent meniscal tear and lateral compartment osteoarthritis in patients treated for symptomatic lateral discoid meniscus: A population-based study. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119856284. 2325967119856284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishino K., Hashimoto Y., Nishida Y., Yamasaki S., Nakamura H. Magnetic resonance imaging T2 relaxation times of articular cartilage before and after arthroscopic surgery for discoid lateral meniscus. Arthroscopy. 2021;37:647–654. doi: 10.1016/j.arthro.2020.09.036. [DOI] [PubMed] [Google Scholar]
- 14.Willimon S.C., Busch M., Perkins C. Outcomes of discoid meniscus repairs in children and adolescents. Arthroscopy. 2021;37(Suppl 1):e68. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demonstration of our technique for saucerization of a symptomatic discoid lateral meniscus and repair of intrasubstance degeneration. The video highlights the use of a small arthroscope to better visualize the lateral compartment during all-inside meniscus-based repair. We also demonstrate the use of an accessory medial portal that allows perpendicular access to the tear with our repair device.
Demonstration of our technique for saucerization of a symptomatic discoid lateral meniscus and repair of intrasubstance degeneration. The video highlights the use of a small arthroscope to better visualize the lateral compartment during all-inside meniscus-based repair. We also demonstrate the use of an accessory medial portal that allows perpendicular access to the tear with our repair device.