Abstract
Varus deformity of the knee can lead to early degeneration of the medial tibiofemoral joint. Pediatric patients can be pathologically affected with this deformity known as Blount disease. The cause of this pathology is still uncertain, but some risk factors are well established, such as obesity and family history. The diagnosis is made through clinical history, physical examination, and the radiographic analysis after the age of 2.5 years. The analysis of the metaphyseal-diaphyseal angle, described by Levine and Drennan, is also commonly used for prognosis. When this angle is greater than 16°, it is considered to be grossly abnormal. Possible options for correcting the generated angular deformity are epiphysiodesis, osteotomy (acute or gradual correction), and gradual correction by distraction of the physis. In this surgical technique, we performed a double tibial osteotomy with controlled gradual opening using monolateral external fixator (Orthofix, Verona, Italy). Our technique proved to be an effective way to correct the adolescent tibia vara and is practical and reproducible. Moreover, the use of gradual opening osteotomy allowed a more accurate outcome.
Technique Video
Preoperative surgery planning is carried out. In this artificial bone model, we observe the gradual opening of the double osteotomy being performed. In this way, we can predict the outcome of the planned surgery. We present a patient with neglected severe bilateral Blount disease. Preoperative radiographs showed a metaphyseal diaphyseal angle of approximately 45° to the left and 35° to the right. Surgery was performed starting on the left side. We start with the predrilling visualizing in the lateral fluoroscopy, and then we insert the two proximal pins, parallel to medial physis in an almost vertical direction. Then, we placed two more distal pins in the tibia and performed the fibular ostectomy, resecting a structural bone graft of about 2 cm in length. We used the same surgical approach of the proximal pins 2 cm distal to them; we performed the first osteotomy initially with drill perforations and then with an osteotome. The direction of the osteotomy is from medial to proximal and lateral toward the lateral tibial spine. In this case, the deformity is very severe, and the external fixador does not have enough angulation to be placed on the pins. If this occurs, the first osteotomy can be opened with a spreader, thereby reducing the deformity and allowing the external fixator to be placed. Then the fibular bone graft is introduced. After this step, we place the accessory pin in the anterior plane, distal to the first osteotomy and 3 cm distal to it, we performed the second osteotomy from medial to lateral, keeping the lateral cortical integral. We then use the L-shaped key and then open the second osteotomy about 1.5 cm. We compress distractors as much as possible, and surgery is completed. We observed the patient in the immediate postoperative period performing partial load with the aid of crutches. After 10 days postoperatively, we start the opening of the fixator with 1/4 turn of the compresson-distraction unit every 6 hours. At this moment, the opening of the external fixator occurs without any accessory bars connected. When we observe that the epiphyseal deformity was corrected, we installed the accessory bar and connected it with the accessory pin and with the fixator’s proximal pins, locking the opening of the proximal osteotomy. If we observe the correction of the metaphyseal deformity first, we block the distal osteotomy, connecting the bar to the accessory pin and the distal pins of the fixator. When we observe clinically and radiologically that the lower limb is aligned, we stop the distraction and wait for bone consolidation as the drawing shows. Here, we can observe the sequential and gradual correction of severe deformity of neglected Blount disease. After observing the correction of the left knee, the patient underwent the same treatment on the contralateral side. We then observed the result obtained after the two sides were gradually corrected by the double osteotomy: preoperatively and postoperatively of this patient with both sides already operated not simultaneously.
Introduction
Varus deformity of the knee can lead to early degeneration of the medial tibiofemoral joint.1 This type of angular knee deformity is the most commonly observed in the population, being 10 times more prevalent than the valgus deformity of this joint.2, 3, 4
Pediatric patients can be pathologically affected with the deformity caused by Blount disease.5 This type of injury corresponds to a growth disorder of the physeal and epiphyseal surfaces of the proximal medial tibia that leads to a progressive varus deformity, internal rotation, and procurvatum of the affected lower limb.6
There are two clinical forms of Blount disease.7 The early-onset type, which affects children around 4 years of age—known as Infantile Blount Disease—and the Juvenile and Adolescent’s Blount disease, which affects patients older than 10 years of age but with the physis still open.8
The cause of this pathology is still uncertain, but some risk factors are well established.9, 10, 11 Obesity exerts a significant mechanical role as it can lead to the development of Blount disease. It is hypothesized that increased load through the joint may cause the structural deformity.12 Metabolic factors such as vitamin D deficiency are also associated with this pathological entity.13
The diagnosis depends on both the clinical examination and radiographic imaging after the age of 2.5 years.14,15 Commonly, affected patients start walking before 1 year of age and usually display a familial pattern. Asymmetric deformities are the most common, and buckling can be observed during gait in the affected limb.16
The Langeskiold classification is commonly used to stage de disease.14,17 We use the Langeskiold classification simplified by Laville, which divides the deformities into 3 stages: Stage 0, patient younger than 2.5 years, in which the diagnosis is still uncertain and an observation period is necessary; Stage 1, confirmed Blount disease, but with absence of medial metaphyseal bony bridge; and Stage 2, presence of medial bar formation across the deformed physis.18
The analysis of the metaphyseal-diaphyseal angle (MD), described by Levine and Drennan, is commonly used to differentiate Blount disease from physiological bowing. An angle that is greater than 16° tends to progress to varus deformity, demanding surgical intervention.14,19
Nonoperative treatment of Blount disease can be considered in patients younger than 3 years of age with unilateral and mild disease, through the use of orthoses.20 However, the effectiveness of brace treatment is controversial, with limited indication and difficult patient compliance. Therefore, surgical intervention is considered crucial to achieve permanent and lasting correction even in early stages. Possible options for correcting the generated angular deformity are epiphysiodesis, osteotomy (acute or gradual correction), and gradual correction by distraction of the physis.8,21
We will describe the steps of a surgical technique used to correct severe and relapsed Blount disease, posteromedial growth arrest, MDA > 16° and Laville Stage 2. In this surgical technique, we performed a double tibial osteotomy with controlled gradual opening using monolateral external fixator (Orthofix, Verona, Italy).
Surgical Technique
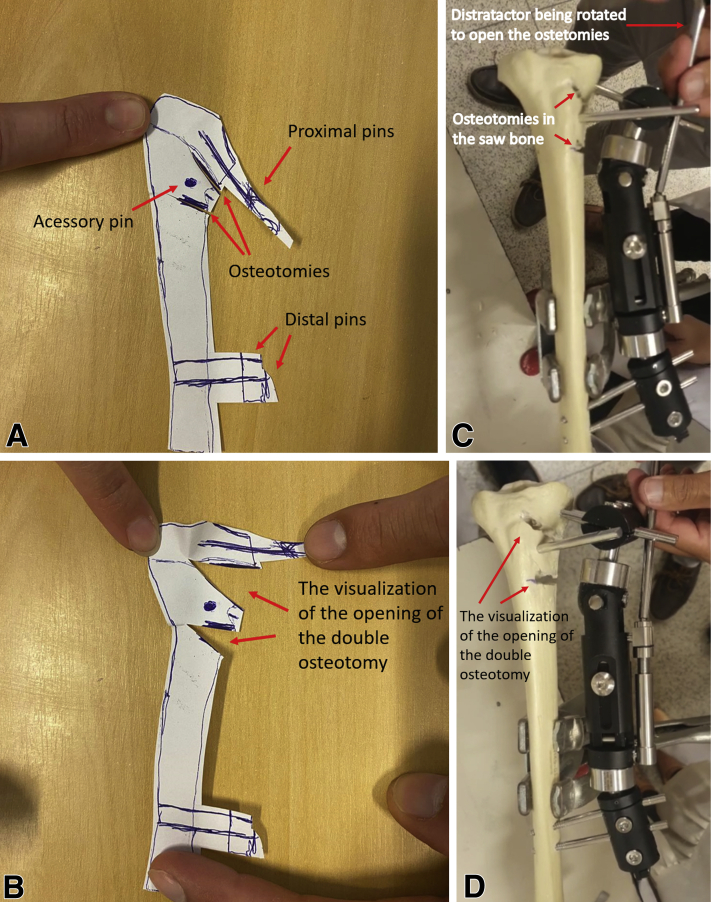
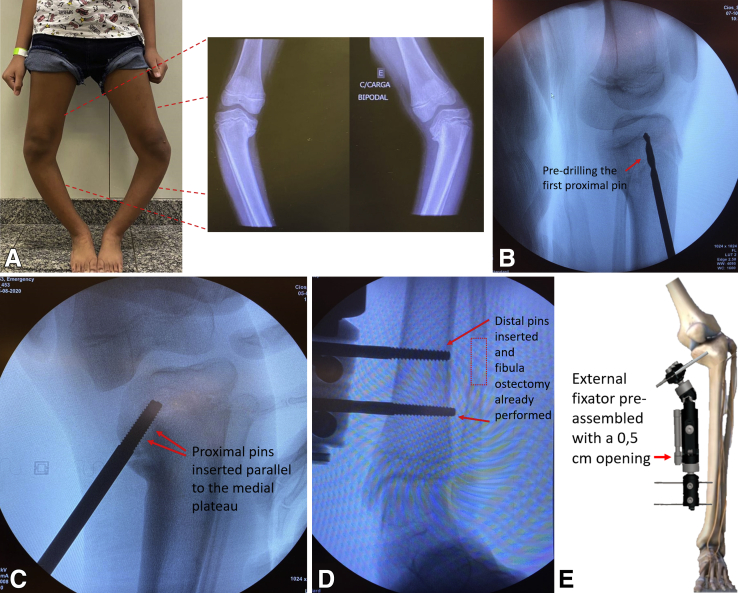
Careful preoperative planning is carried out, observing how the two osteotomies should be performed (Fig 1, A-D). Figure 2A shows a patient with severe Blount disease stage 2 of Laville, with an MDA 45° to the left knee and 35° to the right knee (Video 1).
Fig 1.
Preoperative planning. (A) Template for deformity in varus due to neglected Blount disease with proximal, distal, and accessory pins positioned and double osteotomy already performed. (B) Opening of a double osteotomy observing correction of the deformity. (C and D) Training of the surgical technique in the saw bone, observing the simultaneous opening of the double osteotomy with the opening of the distractor (Orthofix, Verona, Italy). Right Tibia in template and in saw bone model.
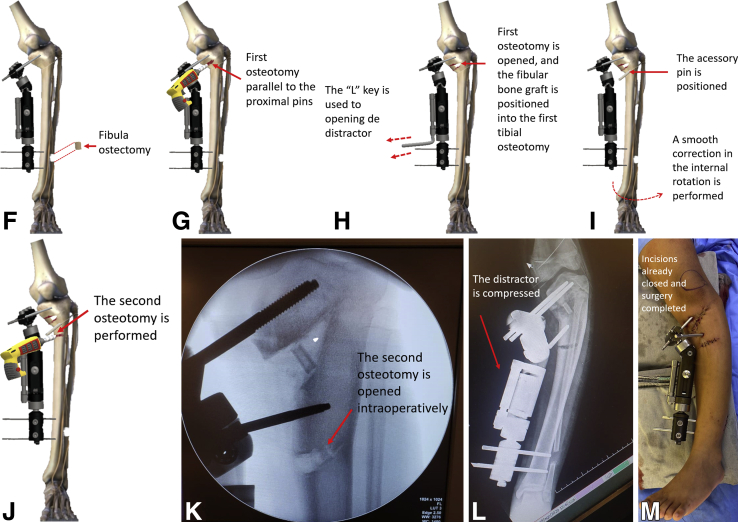
Fig 2.
Intraoperatively steps. (A) Patient with severe Blount disease stage 2 of Laville, with an MDA 45° to the left knee and 35° to the right knee. (B) Visualization by fluoroscopic image in lateral view of the right knee observing the predrilling of the first proximal pin. (C) Proximal pins inserted parallel to the medial plateau (right knee). (D) Distal pins inserted and fibula ostectomy already performed. (E) External fixator preassembled with a 0.5-cm opening. (F) Two-centimeter fibula ostectomy is performed. (G) First osteotomy, parallel to proximal pins, is performed initially with a drill. The partial osteotomy is terminated with the use of an osteotome, from medial to proximal and lateral. (H) First osteotomy is opened, and the fibular bone graft is positioned into the first tibial osteotomy. The “L” key is used to turn and opening the distractor. (I) The accessory pin is positioned. A smooth correction in the internal rotation is performed. (J) The second osteotomy is performed. (K) The second osteotomy is opened intraoperatively, on the left knee. (L) At the end of the surgery, the distractor is compressed to its maximum. (M) View of the left patient’s leg in the immediate postoperative period.
Identification of the Center of Rotation of Angulation (CORA) is the first step of surgical planning. The CORA is the intersection of the proximal and distal axis of a deformed bone and represents the point whereupon a deformity can be corrected with rotation only. Hence, the osteotomy should be carried out as close to the CORA as possible in order to allow correction with partial osteotomy without translation of the fragments.22
Blount disease consists of a multiapical deformity, which means that two CORAs were identified, with one CORA standing at the epiphyseal plate and one at metaphyseal level. Furthermore, as the disease affects the articular surface, it demands a whole limb frontal plane analysis, as described by Paley, with mechanical axis deviation, tibial–femoral angle, medial proximal tibial angle, and posterior proximal tibial angle measurements.
The major treatment goal is to restore the joint line, so, for the proximal deformity, we used the joint line convergence angle (JLCA) as a guide for the first osteotomy planning. JLCA consists of the angle formed between a line tangential to the distal femoral condyle and the tibial plateau and has a normal range between 0° and 2° . Varus of the knee results in a JLCA > 2°.
The location of the CORA is identified preoperatively, during surgical planning. As we mentioned earlier, a multiapical deformity was presented, with one CORA standing at the epiphyseal plate and one at metaphyseal level.
The patient is positioned supine on a radiolucent table, which allows radioscopy to be performed throughout the surgical procedure. The fluoroscopy is positioned and tested. The affected leg is prepped and draped into the surgical field. The distal femur, knee, the entire tibia, and foot must be exposed.
First, a small stab incision is made at the proximal medial tibia, at the desired pin sites, with posterior blunt dissection through the subcutaneous tissues to the level of tibial cortex. Then, predrilling is performed, 1 cm distal to the deformed tibial plateau, and two terminally threaded pins (6.0 mm) (Orthofix, Verona, Italy) are placed in the proximal tibia. Pin placement is performed under C-arm fluoroscopy guidance. They should be parallel to the medial tibial plateau and, in the sagittal, coronal, and axial plane, parallel to each other. The thread must be placed up to the depth of the medial intercondylar tibial tubercle (Fig 2, B and C).
The external fixator (Orthofix, Verona, Italy) frame is preassembled with an 0.5-cm opening. Following the same pin insertion technique, two more pins (Orthofix, Verona, Italy) are drilled into the medial aspect of the distal third of the tibia. The distal pins must be inserted perpendicular to the distal bone axis and parallel to each other in the coronal, sagittal, and axial planes, with minimum distance between them (Fig 2, D and E).
Next, a 2-cm fibular ostectomy is performed via lateral approach, 15 cm proximal to the lateral malleolus (Fig 2, D and F). Through a 4-cm medial approach, the proximal tibia is accessed, at the predetermined CORA. The osteotomy site lies within 1 cm distally to the proximal pins and must be parallel to them and inclined in a way that it points to the lateral growth plate.
We start with a multiple-drill hole osteotomy, on account of better bone healing. Thus, the proximal osteotomy is performed by drilling various adjacent holes with a 2.0 drill, in the previously determined direction. The osteotomy stops at the level of the anterior tibial tubercle line (Fig 2G).
The partial osteotomy is accomplished by connecting the multiple drill holes with a small chisel, from medial to proximal and lateral, guided toward the lateral plateau. This first osteotomy stands in an almost vertical position and ought to be closely guided by C-arm fluoroscopy in order to preserve the opposite tibial cortex. The lateral cortex works as a hinge for angular correction.
Afterward, the osteotomy is amplified with the opening of the compression-distraction unit. When the deformity is severe, the external fixator may not have enough angulation to be placed on the pins. If this occurs, the first osteotomy can be opened with a spreader, thereby, reducing the deformity and allowing the external fixator to be placed (Fig 2H). In such a way, the medial and lateral tibial plateaus are aligned. Once that balance is confirmed through fluoroscopy, the fibular fragment previously removed is placed in the proximal osteotomy gap, under compression, in order to maintain a stable and congruent articular surface.
Then, an accessory pin (Orthofix, Verona, Italy) is placed distally to the osteotomy, in line with the rotation point of the external fixator. A smooth correction in the internal rotation is performed (Fig 2I).
Afterward, a second partial osteotomy is performed, at the proximal tibial diaphysis, inferior to the accessory pin (Fig 2J). Again, the lateral tibial cortex is preserved.
Subsequently, the compression-distraction unit is triggered intraoperatively, and the extent of movement at the opening wedge is accessed; the goal is to reach 1.5 cm (Fig 2K).
Finally, the external fixator is locked at maximal compression (Fig 2, L and M). The final hemostasis is performed, and the skin is sutured. The patient remains hospitalized for around 24 h.
Rehabilitation and Gradual Opening Osteotomy Control
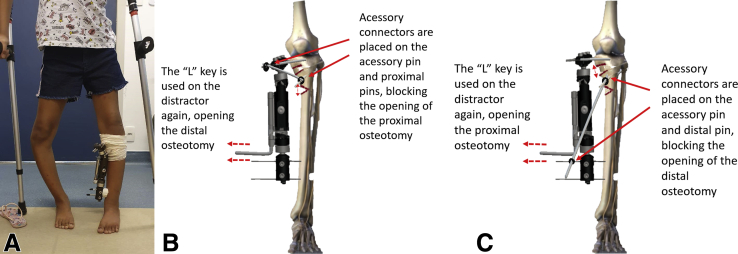
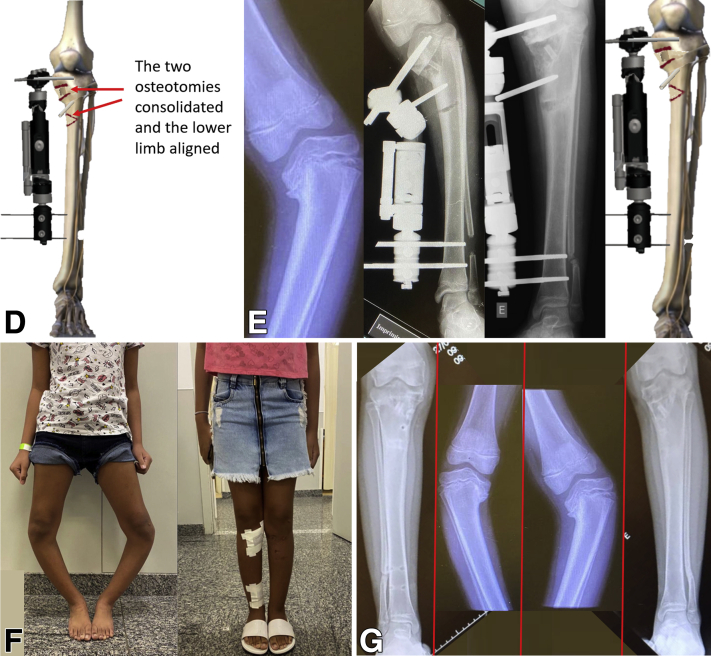
Postoperatively, the patient is instructed to bear partial weight with crutches (Fig 3A). Joint mobility of the knee and ankle is emphasized. After 10 days, the distraction process starts with 1/4 turn of the compression-distraction unit every 6 hours. At this moment, we start to open the external fixator without any accessory bars connected. Weekly medical consultations are fundamental for radiographic control and mechanical axis evaluation. When correction of the epiphyseal deformity is achieved, we install the accessory bar and connect it to the accessory pin and the fixator’s proximal pins, locking the opening of the proximal osteotomy. By connecting the bar to the accessory pin that lays distal to the osteotomy and the fixator pin, proximally, and locking each connector, the opening of the proximal osteotomy is blocked. If we observe the correction of the metaphyseal deformity first, we block the distal osteotomy, as described above, connecting the bar to the accessory pin and the distal pins of the fixator (Fig 3, B and C), observing the gradual correction of the deformity (Fig 3, D and E). At the final stage, in cases of bilateral deformity, the same procedure can be performed on the contralateral limb in a nonsimultaneous manner, even when using the fixator on the contralateral side.
Fig. 3.
Postoperative period. (A) Patient in the initial postoperative period performing partial load with the aid of crutches. (B) The period of gradual opening is started with 1/4 turn of the compression-distraction unit every 6 hours. Initially, the external fixator is opened without the connection between the accessory pin to the fixators pins. When we observe that the epiphyseal deformity was corrected, we installed the accessory bar and connected it with the accessory pin and with the fixator’s proximal pins, locking the opening of the proximal osteotomy. (C) After the distal osteotomy has been opened, correcting the metaphyseal deformity, or if we observe the correction of the metaphyseal deformity first, we block the distal osteotomy, connecting the bar to the accessory pin and the distal pins of the fixator. (D) The two osteotomies consolidated and the lower limb aligned. (E) Observation of sequential and gradual correction of severe deformity of neglected Blount disease. (F) Preoperative and postoperative picture of a patient with both sides already operated not simultaneously. (G) Right leg after the controlled double gradual opening osteotomy, right knee before the treatment. Left knee before the treatment, left leg after the controlled double gradual opening osteotomy.
Once satisfactory limb alignment is achieved, the device can be locked. The patient is then followed up at progressively longer intervals for imaging evaluation of callus formation. (AP weight-bearing radiographic view and lateral view of the knee). An early sign of bone regeneration is an increase in bone density at the osteotomy surfaces. The osteotomy gap is successively consolidated from lateral to medial, and the device can be removed after significant bone contact and structured callus are observed (Fig 3, F and G).
Discussion
Recent studies demonstrate the importance of correcting the mechanical axis in patients with varus deformities.23,24 In the case of patients with Blount’s disease, this correction is essential to prevent serious osteochondral lesions and can, thus, significantly improve the quality of life of these patients.25 In this study, we demonstrate a safe technique that combines gradual correction of tibial osteotomy and plateau elevation to treat this severe type of deformity.
The observation at our institution of the failure of conventional surgical treatment for the treatment of patients with Blount’s disease was one of the main motivators to create this new surgical treatment. In a recent study that evaluated the postoperative results of Blount disease treated with a tension band plate, a failure rate of the procedure of 41% was observed: a failure rate too high. The authors of this study concluded that this type of plate is an independent risk factor for failure of treatment.26
McCarthy et al.27 also demonstrated a double osteotomy with safety, but with multiplanar fixator and epiphysiodeses of the proximal fibula and proximal lateral tibia. Also, a lateral compartment fasciotomy was done.22 We recommend the lateral monoframe assembly, which we consider easier to use and found no need to proceed with epiphysiodeses.
Burton et al.28 described a technique in which a 6-hole, 4.5-mm plate is used for fixation of a closing wedge osteotomy. In his technique, a lateral compartment fasciotomy is also performed, in association with an anterior compartment fasciotomy. Once a plate is used for the osteotomy, there is no room for further corrections, considering that the fixation is final. In our case, the use of a monolateral fixator for gradual correction allowed late corrections during the postoperative follow up. Also, once a gradual correction technique is chosen, there is no need of fasciotomy in any compartment.
Edwards et al.29 performed a double osteotomy using a hexapod external fixator to simultaneously correct the alignment, rotation, and length. They also did a proximal fibular osteotomy. In their study, two patients had evidence of nerve injury.29 We recommend a distal fibular ostectomy, avoiding the possibility of nerve injury. We also consider that the use of the hexapod frame is harder for the patients to understand when compared with the monolateral frame. In the Edwards study, recurrence was noted in three patients.
The main risk of this surgical technique is the incorrect use of the L-shaped key to perform the gradual correction every 6 hours daily. The patient who will undergo this surgery should be trained to know how to perform the rotation of the distractor with the L-shaped key. The advantages, disadvantages, risks, and limitations of our technique can be seen in Table 1.
Table 1.
Advantages, Disadvantages, Risks and Limitations Associated with the Dual Gradual Opening Osteotomy Technique for the Treatment of Severe Varus of the Knee
| Advantages | Disadvantages | Risks | Limitations |
|---|---|---|---|
| Greater control of the amount of the angular correction | Fibula ostectomy is necessary. It should be performed in the middle third of the fibula, to avoid injury to the fibular nerve or instability of the ankle. | Fibula ostectomy must be performed in the middle third of the fibula, to avoid injury to the fibular nerve (if ostectomy was performed proximal) or instability of the ankle (if ostectomy was performed distal). | The patient must be a high level of understanding how to handle the L-shaped key in conjunction with a compression-distraction unit. |
| Fasciotomy is not necessary | The patient controls the opening wedge by turn off the compression-distraction unit every 6 hours | Incorrect wedge opening due to a possible error by the patient handling the compression-distraction unit | Can be performed only using articulated external monoplanar fixator (Orthofix, Verona, Italy) |
| Monolateral external fixator is more comfortable for the patient | Weekly monitoring of the patient with radiological control is necessary | Exposition to weekly radiation until the correction of the deformity | |
| Major deformities can be corrected, allowing the joint line to be raised. | After significant bone contact and structured callus are observed, the external fixator must be removed in the operating room. And the path of the pins must be curetted to avoid pin path infection. | Pin path infection | |
| Weight bearing on operated member is allowed |
Our technique is an effective way to correct the adolescent tibia vara and is practical and reproducible. The use of gradual open osteotomy allows for more accurate outcomes.
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Preoperative surgery planning is carried out. In this artificial bone model, we observe the gradual opening of the double osteotomy being performed. In this way, we can predict the outcome of the planned surgery. We present a patient with neglected severe bilateral Blount disease. Preoperative radiographs showed a metaphyseal diaphyseal angle of approximately 45° to the left and 35° to the right. Surgery was performed starting on the left side. We start with the predrilling visualizing in the lateral fluoroscopy, and then we insert the two proximal pins, parallel to medial physis in an almost vertical direction. Then, we placed two more distal pins in the tibia and performed the fibular ostectomy, resecting a structural bone graft of about 2 cm in length. We used the same surgical approach of the proximal pins 2 cm distal to them; we performed the first osteotomy initially with drill perforations and then with an osteotome. The direction of the osteotomy is from medial to proximal and lateral toward the lateral tibial spine. In this case, the deformity is very severe, and the external fixador does not have enough angulation to be placed on the pins. If this occurs, the first osteotomy can be opened with a spreader, thereby reducing the deformity and allowing the external fixator to be placed. Then the fibular bone graft is introduced. After this step, we place the accessory pin in the anterior plane, distal to the first osteotomy and 3 cm distal to it, we performed the second osteotomy from medial to lateral, keeping the lateral cortical integral. We then use the L-shaped key and then open the second osteotomy about 1.5 cm. We compress distractors as much as possible, and surgery is completed. We observed the patient in the immediate postoperative period performing partial load with the aid of crutches. After 10 days postoperatively, we start the opening of the fixator with 1/4 turn of the compresson-distraction unit every 6 hours. At this moment, the opening of the external fixator occurs without any accessory bars connected. When we observe that the epiphyseal deformity was corrected, we installed the accessory bar and connected it with the accessory pin and with the fixator’s proximal pins, locking the opening of the proximal osteotomy. If we observe the correction of the metaphyseal deformity first, we block the distal osteotomy, connecting the bar to the accessory pin and the distal pins of the fixator. When we observe clinically and radiologically that the lower limb is aligned, we stop the distraction and wait for bone consolidation as the drawing shows. Here, we can observe the sequential and gradual correction of severe deformity of neglected Blount disease. After observing the correction of the left knee, the patient underwent the same treatment on the contralateral side. We then observed the result obtained after the two sides were gradually corrected by the double osteotomy: preoperatively and postoperatively of this patient with both sides already operated not simultaneously.
References
- 1.Nha K.W., Lee Y.S., Hwang D.H., et al. Second-look arthroscopic findings after open-wedge high tibia osteotomy focusing on the posterior root tears of the medial meniscus. Arthroscopy. 2013;29:226–231. doi: 10.1016/j.arthro.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 2.Brouwer G.M., van Tol A.W., Bergink A.P., et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56:1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 3.Sharma L., Song J., Dunlop D., et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69:1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma L., Song J., Felson D.T., Cahue S., Shamiyeh E., Dunlop D.D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;11:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 5.Blount W.P. Tibia vara: Osteochondris deformans tibiae. J Bone Joint Surg. 1937;19:1–29. [Google Scholar]
- 6.Sabharwal S.J. Blount disease. J Bone Joint Surg Am. 2009;91:1758–1776. doi: 10.2106/JBJS.H.01348. [DOI] [PubMed] [Google Scholar]
- 7.Thompson G.H., Carter J.R. Late-onset tibia vara (Blount’s disease). Current concepts. Clin Orthop Relat Res. 1990;(255):24–35. [PubMed] [Google Scholar]
- 8.de Pablos J., Arbeloa-Gutierrez L., Arenas-Miquelez A. Update on treatment of adolescent Blount disease. Curr Opin Pediatr. 2018;30:71–77. doi: 10.1097/MOP.0000000000000569. [DOI] [PubMed] [Google Scholar]
- 9.De Pablos J., Alfaro J., Barrios C. Treatment of adolescent Blount disease by asymmetric physeal distraction. J Pediatr Orthop. 1997;17:54–58. [PubMed] [Google Scholar]
- 10.Li Y., Spencer S., Hedequist D. Proximal tibial osteotomy and Taylor Spatial Frame application for correction of tibia vara in morbidly obese adolescents. J Pediatr Orthop. 2013;33:276–281. doi: 10.1097/BPO.0b013e31828800fe. [DOI] [PubMed] [Google Scholar]
- 11.Sabharwal S., Zhao C., Sakamoto S.M., McClemens E. Do children with Blount disease have lower body mass index after lower limb realignment? J Pediatr Orthop. 2014;34:213–218. doi: 10.1097/BPO.0b013e3182a11d59. [DOI] [PubMed] [Google Scholar]
- 12.Sabharwal S. Blount disease: An update. Orthop Clin North Am. 2015;46:37–47. doi: 10.1016/j.ocl.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Montgomery C.O., Young K.L., Austen M., et al. Increased risk of Blount disease in obese children and adolescents with vitamin D deficiency. J Pediatr Orthop. 2010;30:879–882. doi: 10.1097/BPO.0b013e3181f5a0b3. [DOI] [PubMed] [Google Scholar]
- 14.Catonné Y. Cahiers d’enseignement de laSociété franç aise d’orthopédie et traumatologie. Expansion ScientifiqueFranç aise; Paris: 1997. La maladie de Blount; pp. 147–163. [Google Scholar]
- 15.Herring J.A. Tachdjian’s pediatric orthopedics. 3rd ed. Saunders; Philadelphia: 2002. Genu varum; pp. 839–855. [Google Scholar]
- 16.Janoyer M. Blount disease. Orthop Traumatol Surg Res. 2019;105:S111–S121. doi: 10.1016/j.otsr.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Sabharwal S, Lee Jr J, Zhao CJ. Multiplanar deformity analysis of untreated Blount disease. J Pediatr Orthop 2007;27:260–265 [Erratum in J Pediatr Orthop 2007;27:483]. [DOI] [PubMed]
- 18.Laville J.M., Chau E., Willemen L., Kohler R., Garin C. Blount's disease: Classification and treatment. J Pediatr Orthop B. 1999;8:19–25. [PubMed] [Google Scholar]
- 19.Levine A.M., Drennan J.C. Physiological bowing and tibia vara. J Bone Joint Surg Am. 1983;64:1158–1163. [PubMed] [Google Scholar]
- 20.Sabharwal S., Sabharwal S. Treatment of infantile Blount disease. J Pediatr Orthopaed. 2017;37:S26–S31. doi: 10.1097/BPO.0000000000001027. [DOI] [PubMed] [Google Scholar]
- 21.Stevens P.M. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 22.Cerqueira F.S., Cerqueira F.S., Motta G.A.T.A. Reconstrução e alongamento ósseo: Ed 1, Chapter 3, INTO: Comunicações, 2017:13–18. [Google Scholar]
- 23.Rocha de Faria J.L., Pavao D.M., Moreirão M.C., et al. Posterior root repair of medial meniscus combined with valgus opening wedge tibial osteotomy. Arthrosc Tech. 2021;10:e1373–e1382. doi: 10.1016/j.eats.2021.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ke X., Qiu J., Chen S., et al. Concurrent arthroscopic meniscal repair during open-wedge high tibial osteotomyis not clinically beneficial for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2021;29:955–965. doi: 10.1007/s00167-020-06055-9. [DOI] [PubMed] [Google Scholar]
- 25.Dakshina Murthy T.S., De Leucio A. StatPearls [Internet] StatPearls Publishing; Treasure Island, FL: 2021. Blount Disease. In: [Google Scholar]
- 26.Jain M.J., Inneh I.A., Zhu H., Phillips W.A. Tension band plate (TBP)-guided hemiepiphysiodesis in Blount disease: 10-Year single-center experience with a systematic review of literature. J Pediatr Orthop. 2020;40:e138–e143. doi: 10.1097/BPO.0000000000001393. [DOI] [PubMed] [Google Scholar]
- 27.McCarthy J.J., MacIntyre N.R., Hooks B., Davidson R.S. Double osteotomy for the treatment of severe Blount disease. J Pediatr Orthopaed. 2009;29:115–119. doi: 10.1097/BPO.0b013e3181982512. [DOI] [PubMed] [Google Scholar]
- 28.Burton A., Hennrikus W. Complete closing wedge osteotomy for the correction of tibia vara—A technique. Pediatrics. 2016;137 doi: 10.1542/peds.137.supplement_3.572a. :572A (Suppl 3). [DOI] [PubMed] [Google Scholar]
- 29.Edwards T.A., Hughes R., Monsell F. The challenges of a comprehensive surgical approach to Blount’s disease. J Child Orthop. 2017;11:479–487. doi: 10.1302/1863-2548.11.170082. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preoperative surgery planning is carried out. In this artificial bone model, we observe the gradual opening of the double osteotomy being performed. In this way, we can predict the outcome of the planned surgery. We present a patient with neglected severe bilateral Blount disease. Preoperative radiographs showed a metaphyseal diaphyseal angle of approximately 45° to the left and 35° to the right. Surgery was performed starting on the left side. We start with the predrilling visualizing in the lateral fluoroscopy, and then we insert the two proximal pins, parallel to medial physis in an almost vertical direction. Then, we placed two more distal pins in the tibia and performed the fibular ostectomy, resecting a structural bone graft of about 2 cm in length. We used the same surgical approach of the proximal pins 2 cm distal to them; we performed the first osteotomy initially with drill perforations and then with an osteotome. The direction of the osteotomy is from medial to proximal and lateral toward the lateral tibial spine. In this case, the deformity is very severe, and the external fixador does not have enough angulation to be placed on the pins. If this occurs, the first osteotomy can be opened with a spreader, thereby reducing the deformity and allowing the external fixator to be placed. Then the fibular bone graft is introduced. After this step, we place the accessory pin in the anterior plane, distal to the first osteotomy and 3 cm distal to it, we performed the second osteotomy from medial to lateral, keeping the lateral cortical integral. We then use the L-shaped key and then open the second osteotomy about 1.5 cm. We compress distractors as much as possible, and surgery is completed. We observed the patient in the immediate postoperative period performing partial load with the aid of crutches. After 10 days postoperatively, we start the opening of the fixator with 1/4 turn of the compresson-distraction unit every 6 hours. At this moment, the opening of the external fixator occurs without any accessory bars connected. When we observe that the epiphyseal deformity was corrected, we installed the accessory bar and connected it with the accessory pin and with the fixator’s proximal pins, locking the opening of the proximal osteotomy. If we observe the correction of the metaphyseal deformity first, we block the distal osteotomy, connecting the bar to the accessory pin and the distal pins of the fixator. When we observe clinically and radiologically that the lower limb is aligned, we stop the distraction and wait for bone consolidation as the drawing shows. Here, we can observe the sequential and gradual correction of severe deformity of neglected Blount disease. After observing the correction of the left knee, the patient underwent the same treatment on the contralateral side. We then observed the result obtained after the two sides were gradually corrected by the double osteotomy: preoperatively and postoperatively of this patient with both sides already operated not simultaneously.
Preoperative surgery planning is carried out. In this artificial bone model, we observe the gradual opening of the double osteotomy being performed. In this way, we can predict the outcome of the planned surgery. We present a patient with neglected severe bilateral Blount disease. Preoperative radiographs showed a metaphyseal diaphyseal angle of approximately 45° to the left and 35° to the right. Surgery was performed starting on the left side. We start with the predrilling visualizing in the lateral fluoroscopy, and then we insert the two proximal pins, parallel to medial physis in an almost vertical direction. Then, we placed two more distal pins in the tibia and performed the fibular ostectomy, resecting a structural bone graft of about 2 cm in length. We used the same surgical approach of the proximal pins 2 cm distal to them; we performed the first osteotomy initially with drill perforations and then with an osteotome. The direction of the osteotomy is from medial to proximal and lateral toward the lateral tibial spine. In this case, the deformity is very severe, and the external fixador does not have enough angulation to be placed on the pins. If this occurs, the first osteotomy can be opened with a spreader, thereby reducing the deformity and allowing the external fixator to be placed. Then the fibular bone graft is introduced. After this step, we place the accessory pin in the anterior plane, distal to the first osteotomy and 3 cm distal to it, we performed the second osteotomy from medial to lateral, keeping the lateral cortical integral. We then use the L-shaped key and then open the second osteotomy about 1.5 cm. We compress distractors as much as possible, and surgery is completed. We observed the patient in the immediate postoperative period performing partial load with the aid of crutches. After 10 days postoperatively, we start the opening of the fixator with 1/4 turn of the compresson-distraction unit every 6 hours. At this moment, the opening of the external fixator occurs without any accessory bars connected. When we observe that the epiphyseal deformity was corrected, we installed the accessory bar and connected it with the accessory pin and with the fixator’s proximal pins, locking the opening of the proximal osteotomy. If we observe the correction of the metaphyseal deformity first, we block the distal osteotomy, connecting the bar to the accessory pin and the distal pins of the fixator. When we observe clinically and radiologically that the lower limb is aligned, we stop the distraction and wait for bone consolidation as the drawing shows. Here, we can observe the sequential and gradual correction of severe deformity of neglected Blount disease. After observing the correction of the left knee, the patient underwent the same treatment on the contralateral side. We then observed the result obtained after the two sides were gradually corrected by the double osteotomy: preoperatively and postoperatively of this patient with both sides already operated not simultaneously.