Abstract
The neural mechanisms of acupuncture are not well-understood. Over the past decades, an increasing number of studies have used MRI to investigate the response of the brain to acupuncture. The current review aims to provide an update on acupuncture therapy in disease. The PubMed, Embase, Web of Science, and Cochrane Library databases were searched from inception to January 31, 2021. Article selection and data extraction were conducted by two review authors. A total of 107 publications about MRI in acupuncture were included, the collective findings of which were as follows: (1) stroke and GB34 (Yanglingquan) are the most studied disease and acupoint. Related studies suggested that the mechanism of acupuncture treatment for stroke may associate with structural and functional plasticity, left and right hemispheres balance, and activation of brain areas related to movement and cognition. GB34 is mainly used in stroke and Parkinson's disease, which mainly activates brain response in the premotor cortex, the supplementary motor area, and the supramarginal gyrus; (2) resting-state functional MRI (rs-fMRI) and functional connectivity (FC) analysis are the most frequently used approaches; (3) estimates of efficacy and brain response to acupuncture depend on the type of sham acupuncture (SA) used for comparison. Brain processing after acupuncture differs between patients and health controls (HC) and occurs mainly in disorder-related areas. Factors that influence the effect of acupuncture include depth of needling, number and locations of acupoints, and deqi and expectation effect, each contributing to the brain response. While studies using MRI have increased understanding of the mechanism underlying the effects of acupuncture, there is scope for development in this field. Due to the small sample sizes, heterogeneous study designs, and analytical methods, the results were inconsistent. Further studies with larger sample sizes, careful experimental design, multimodal neuroimaging techniques, and standardized methods should be conducted to better explain the efficacy and specificity of acupuncture, and to prepare for accurate efficacy prediction in the future.
Keywords: acupuncture, MRI, diseases, mechanism, review
Introduction
Acupuncture has been practiced in China for more than 3,000 years as a minimally invasive therapeutic modality of traditional Chinese medicine (TCM) (Zhuang et al., 2013). It has gained increasing popularity and acceptance due to its obvious efficacy (Liang and Wu, 2006). Several systematic reviews have indicated that acupuncture therapy may improve symptoms in various diseases, such as depression (Smith et al., 2018), ischemic stroke (Lu et al., 2016), migraine (Da, 2015), functional diarrhea (Guo et al., 2020), and Alzheimer's disease (Huang et al., 2019). However, the mechanisms underlying the efficacy of acupuncture therapy remain unclear, arousing widespread skepticism and attention.
Since the 1970s, many studies using animal models have shown that the effects of acupuncture are related to the integration of the central nervous system (Han, 2011; Xiao et al., 2018). MRI, as advanced visualization and non-invasive brain imaging technique, can provide comprehensive, multiparametric information on brain anatomy and function (Yousaf et al., 2018). It has been widely used to elucidate the functional and structural response to acupuncture (Usichenko et al., 2015; Li et al., 2020a). Thus, revealing the mechanism underlying the effect of acupuncture has become an area of research interest in recent years.
With an increasing amount of MRI-based research on acupuncture, a summary to date is useful as a basis for further exploration in the future. Although four reviews (He et al., 2015; Scheffold et al., 2015; Cai et al., 2018; Huang et al., 2019) have been conducted on functional MRI (fMRI) studies to explore the mechanism of acupuncture, several limitations are remaining. First, the literature included studies published from 1999 to 2016. However, numerous MRI studies on acupuncture have emerged in recent years and need to be updated. Second, many of the previous studies involved acupuncture in healthy people, but research has shown that acupuncture effects are more apparent in pathological conditions (Han et al., 2019). Moreover, the emergence of acupuncture as a treatment stems from its function in patients rather than healthy people. Third, it may be necessary to summarize the current literature from different perspectives, such as analytic methods and study designs.
Overall, reviews to date on MRI research in acupuncture provide limited understanding of treatment effects in disease. Therefore, the purpose of this study is to provide an updated review of MRI studies on the mechanism of acupuncture therapy in disease, focusing on disease types and acupoints, experimental design and analysis methods, and research topics.
Materials and Methods
Literature Search and Study Selection
A systematic search was conducted to find potentially eligible studies published in English from inception to January 2021 in PubMed, EMBASE, Web of Science, and Cochrane Library databases. Keywords were: (1) MRI, blood oxygen level dependent (BOLD), regional homogeneity (ReHo), the amplitude of low-frequency fluctuation (ALFF), fractional ALFF (fALFF), white matter, voxel-based analysis, voxel based morphometry (VBM), Freesurfer, surface-based morphometry, cortical thickness, surface area, cortical volume, gray matter volume, gray matter density, and (2) acupuncture therapy, acupuncture, acupuncture point, ear, body acupuncture, auricular acupuncture, electroacupuncture (EA), and moxibustion. Studies eligible for inclusion met the following criteria: (1) subjects including patients and not only healthy volunteers; (2) the study was an original article that was peer-reviewed and published in English; (3) studies using acupuncture, EA, or laser acupuncture; and (4) subjects underwent two MRI scans before and after acupuncture or one MRI scan during acupuncture. Exclusion criteria were: (1) protocol, case reports, or case series; (2) other interventions that do not belong to traditional acupuncture, such as transcutaneous electrical nerve stimulation, transcutaneous vagus nerve stimulation, and so on; (3) analytical methods using magnetic resonance spectroscopy (MRS); and (4) experimental animal study.
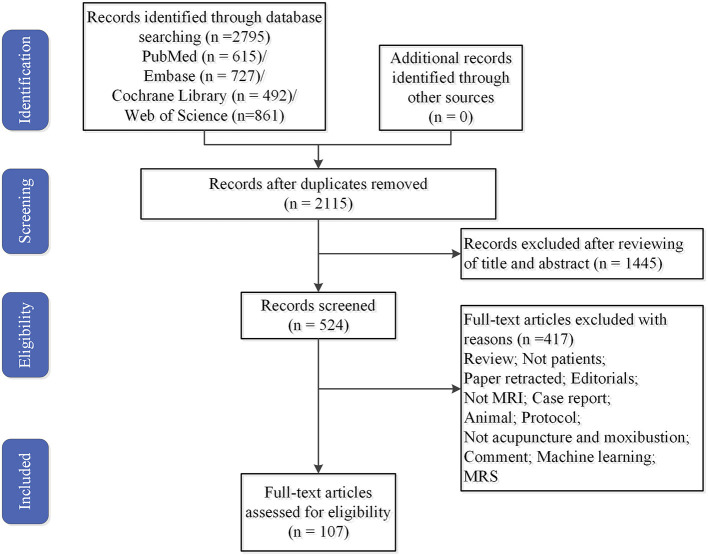
All identified studies were imported into endnote after careful reading of the titles and abstracts. Duplicate studies and those that did not meet the inclusion criteria were excluded. Finally, 107 studies were included (Figure 1).
Figure 1.
Flowchart of literature selection. MRI, magnetic resonance imaging; MRS, magnetic resonance spectroscopy.
Data Extraction
The following data were extracted by two authors: year of publication, author details, number of participants, diseases, intervention/control groups, needling details, types of acupuncture, sample size, acupuncture points, data analysis, experimental design, and study design. Any inconsistencies were discussed with a third author to reach an agreement.
In addition, although several study designs investigating the mechanism of MRI-based acupuncture are involved in this review, considering reliability and rigor of results, we focused in particular on the verum acupuncture (VA) vs. sham acupuncture (SA) in patients and health controls (HC).
Results
Study Characteristics
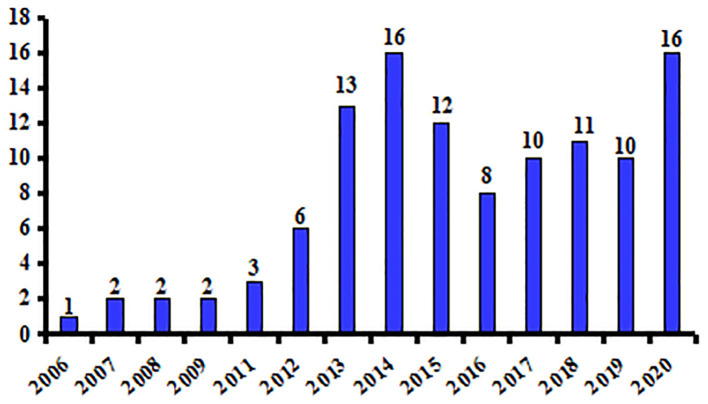
The search yielded 107 studies that were published between 2006 and 2021 (Supplementary Table 1). The mean sample size was 28 (range 6–102), and the total number of participants in all studies included 2,957 patients and 928 HC. Acupuncture manipulation modality in these studies included manual acupuncture (MA), EA, and laser acupuncture. Figure 2 shows the number of publications per year, with the highest number (n = 16) in 2014 and 2020. Seventeen of the studies used 1.5 and 2.0 T MRI systems, and the remaining (85%) used 3.0 T systems.
Figure 2.
Numbers of MRI studies of acupuncture in diseases.
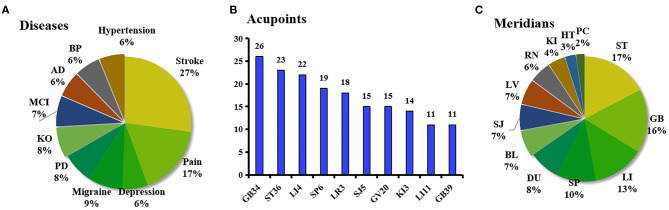
Diseases, Acupoints, and Meridians
The studies involved more than 30 types of diseases, mainly related to neurological and digestive systems. The top 10 diseases are shown in Figure 3A. Stroke (including stable somatosensory, chronic, aphasia, ischemic, stable recovery, and subcortical stroke) was the most frequently studied disease.
Figure 3.
(A) Proportion of the top ten most studied diseases in the reviewed studies. (B) Frequency of the top ten most used acupoints in the reviewed studies. (C) Percentage of meridians where acupoints are located in the reviewed studies. AD, Alzheimer's disease; BP, Bell's palsy; BL, the Bladder Meridian; DU, the Du Meridian; HT, the Heart Meridian; KO, Knee osteoarthritis; LI, the Liver Meridian; MCI, mild cognitive impairment; PD, Parkinson's disease; PC, the Pericardium Meridian; KI, the Kidney Meridian; RN, the Ren Meridian, RN; SJ, the Sanjiao Meridian; SP, the Spleen Meridian.
GB34 (Yanglingquan) was found to be the most frequently applied acupoint and singly applied in 11 studies on stroke (n = 8) and Parkinson's disease (n = 3). Other acupoints used frequently in the 107 studies are shown in Figure 3B. The meridians used in these studies are summarized in Figure 3C. The acupoints of the stomach meridian in ST36 (Zusanli) were used most commonly, mainly in combination with other acupoints.
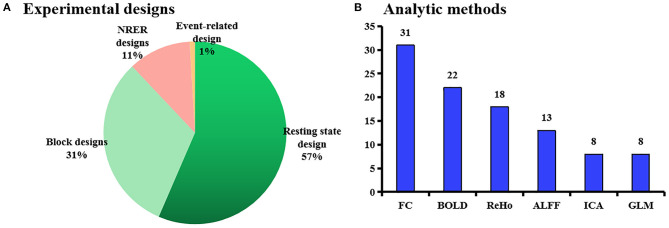
Experimental Designs and Analytic Methods
Four types of experimental design were applied (Figure 4A), and the resting-state fMRI (rs-fMRI) approach was used most frequently in 60 of the 107 studies. This method was used particularly in the latter 5 years of the publication date range, with 43 of the 60 (70%) being published between 2016 and 2020.
Figure 4.
(A) Proportion of experimental designs in the reviewed studies. (B) Analytical methods used in the reviewed studies. ALFF, the amplitude of low-frequency fluctuation; BOLD, blood oxygen level-dependent; FC, functional connectivity; ICA, independent component analysis; GLM, general linear model, NRER, non-repeated event-related.
The six most frequently applied analysis methods are summarized in Figure 4B. Functional connectivity (FC) was used most frequently (in 31 studies), whereas VBM and diffusion tensor imaging (DTI) were used less. The earliest application of the FC analysis in this sample was in 2007, but it did not appear for several years. Thirty-one of the studies analyzed FC changes using predefined seed points or regions of interest.
Research Topics
The research topics in the included studies could be approximately categorized as MRI investigations of (1) the mechanism by which acupuncture takes effect in disease and (2) factors influencing efficacy (Figure 5).
Figure 5.
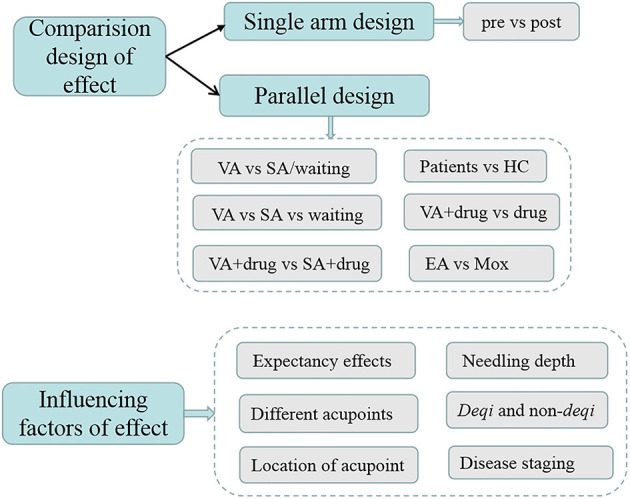
Topics of studies on acupuncture for diseases based on MRI.
Effect of Acupuncture
Single and parallel arm study designs were used to assess the effect of acupuncture. However, in this review, we focused in particular on the VA vs. SA in patients and HC.
(1) Verum acupuncture and SA
- Three types of SA were used in 26 of all studies, including (a) cutaneous stimulation at the acupuncture points or sham points or areas; (b) use of a blunt needle (Streitberger (Streitberger and Kleinhenz, 1998), plastic, or Park (Park et al., 2002) needle: with a blunt tip, to simulate an acupuncture procedure without penetrating the skin); (c) needling at non-acupuncture points close to acupuncture points (Table 1).
- (a) Cutaneous stimulation at the same acupuncture point
- (b) Blunt needles
- A total of eight studies using blunt needles as control showed heterogeneous results. Three studies (Schaechter et al., 2007; Chae et al., 2009; Chen et al., 2015) used the Streitberger needle, one study used the plastic tubes (Wang et al., 2016a), one study used the foam cubes (Chu et al., 2012), and two placebo control studies (Chae et al., 2009; Yeo et al., 2014) used the Park device. All showed significantly higher brain activation in VA than SA, which was related to the pathological mechanism of disease. In addition, two studies (Hashmi et al., 2014; Gollub et al., 2018) using the Streitberger needle investigated the expectation effect in patients with knee osteoarthritis between VA and SA, and found that expectation significantly and similarly modulates the pain experience in both VA and SA.
- (c) Needling at non-acupuncture points close to acupuncture points
- Fourteen (56%) studies (Huang et al., 2011; Liu et al., 2012; Kang et al., 2013; Maeda et al., 2013; Chen et al., 2014; Qi et al., 2014; Zhao et al., 2014; Egorova et al., 2015; von Deneen et al., 2015; Li et al., 2016, 2018; Zheng et al., 2016; Tan et al., 2017; Wang et al., 2020) adapted at non-acupuncture points close to acupuncture points as VA in patients.
Table 1.
Characteristics of studies about VA and SA.
| Numbers | References | Subjects | Intervention | Groups | Were HC intervened (Y/N) | Acupoints | Data analysis | Experimental design | Type of SA |
|---|---|---|---|---|---|---|---|---|---|
| Tactile stimulation | |||||||||
| 1 | Li et al., 2006 | 12 stroke/12 HC | EA | VA/SA | Y | LI4, LI11 | SPM | Block/R(45s)-S(45s), 3 times | / |
| Blunt needling | |||||||||
| 2 | Napadow et al., 2007 | 13 Carpal Tunnel Syndrome/12 HC | MA | VA/SA | Y | LI4, SJ5, PC7 | FC | RS, 3 times/week for 3 weeks and 2 times per week for the remaining 2 weeks. | Non-insertive cutaneous stimulation over the acupoint |
| 3 | Schaechter et al., 2007 | 7 stroke | MA | 4 VA/3 SA | / | N | GLM | RS, twice/week for 10 weeks. | Streitberger needle |
| 4 | Chae et al., 2009 | 10 Parkinson's Diseases/10 HC | MA | VA/covert placebo/overt placebo | N | Left GB34 | SPM | Block, R(2min)-S(1min), 3 times | Park needle |
| 5 | Chen et al., 2015 | 30 knee osteoarthritis | MA | 10 high dose VA/10 low dose VA/10 SA | / | ST35 and Xi yan (extra point), GB34, SP9, GB39 and SP6 | FC, left posterior medial prefrontal cortex (pMPFC), Cortical thickness analysis | RS, 6 acupuncture treatment sessions in 1 month (twice/week for the first 2 weeks, once/week for the last 2 weeks | Non-acupoints, Streitberger needle |
| 5 | Hashmi et al., 2014 | 40 knee osteoarthritis | EA | 20 VA/20 SA | / | LI3 and LI4 | Graph-theoretic metrics of network topology | RS (real or sham acupuncture), lasted 25 min. | Streitberger needle |
| 7 | Gollub et al., 2018 | 43 knee osteoarthritis | MA | 21 MA/22 SA | / | Right Liv3 and LI4 | ReHo | RS, five times/week, for 4 consecutive weeks. | Streiberger needle |
| 8 | Chu et al., 2012 | 30 irritable bowel syndrome | EA | 15 EA/15 SA | / | Bilateral ST36, ST37 and SP6 | SPM | Block, 30 min EA | Foam cubes |
| 9 | Yeo et al., 2012 | 12 Parkinson's Disease/12 HC | MA | VA/SA | Y | Right GB34 | SPM | R(4min)-sham(S(1min)-R(1min-S(1min)-R(1min))-R(4min)-T1(10min)-verm(S(1min)-R(1min)-S(1min)-R(1min)-R(4min) | The blunt type needle was not inserted into the skin |
| 10 | Yeo et al., 2014 | 12 Parkinson's disease/12 HC | MA | VA/SA | Y | GB34 | SPM | Block, SA: R(60s)-S(60s)-R(60s)-S(60s)-R(60s)-structural images(15min); then RA: R(60s)-S(60s)-R(60s)-S(60s)-R(60s) | Park needle |
| 11 | Wang et al., 2016b | 46 depression | MA | 22 MA and fluoxetine/24 SA and fluoxetine | / | RN12, RN10, RN6, RN4, KL 17, ST24, and Qipang. | FC, bilateral amygdala as the seed region | RS, once a day for the first 3 days and subsequently once every 3 days for the remainder of the 8-week trial. | Short plastic tubes |
| Needling at non-acupuncture points in close proximity to acupuncture points | |||||||||
| 12 | Huang et al., 2011 | 12 ischemic stroke | MA | 6 VA/6 SA | / | SJ5 | SPM | Block, S(30s)-R(30sn), 6 times | / |
| 13 | Liu et al., 2012 | 41 myopia | MA | 11 VA and TI/ 11 VA and NI/10 SA and TI/9 SA and NI | / | LR3 | GLM | RS, R(186s)-S(180s) | / |
| 14 | Maeda et al., 2013 | 59 carpal tunnel syndrome | EA | 22 local VA/18 distal VA/19 SA | / | Local VA: PC7, SJ5; distal VA: SP-6, LV-4; SA: SH1 and SH2. | GLM | RS, event-related/2-s stimulation events with randomized interstimulus interval (ISI), 6–12 s, and total scan time 5 min and 6 s | / |
| 15 | Kang et al., 2013 | 25 smoke | MA | 12 VA/13 SA | / | Left HT7 | SPM | Block, S(60s)-R(60s), 3 times | / |
| 16 | Qi et al., 2014 | 16 ischemic stroke | MA | 8 VA/8 SA | / | SJ5 | SPM | Block, R(30s)-S(30s), total 6min6s | / |
| 17 | Zhao et al., 2014 | 40 migraine | MA | 20 active point/20 inactive point | / | Active point: bilateral SJ5,GB20, GB34, and GB40 inactive point: bilateral SJ22, PC7, GB37, and SP3 | ReHo | RS, 4 times/week for 30 min each for 8 weeks | / |
| 18 | Chen et al., 2014 | 6 ischemic stroke | MA | VA/SA | / | SJ5 | SPM | Block, R(5 min)-SAstimulus(6 min30s)-R(6mmin2s)-VA(6 min30 s). | / |
| 19 | Zhu et al., 2014 | 28 irritable bowel syndromes | Mox | 15 VA/13 SA | / | ST25, RN6, and RN12 | ICA | RS, three times/week for 4 weeks | 2 cm in diameter, 1.14 g in weight |
| 20 | von Deneen et al., 2015 | 19 overweight | MA | 10 MA/9 SA | / | Bilateral ST 36 and SP 9 | SPM | Block, R(5 min)-S(21min)-S(1min)-R(7 min) anatomical scan -(9 min) postscan | / |
| 21 | Egorova et al., 2015 | 41 knee osteoarthritis | MA | 6 acupoints/2 acupoints/SA | / | 2 acupoint: ST35 and Xi yan (extra point) and 6 acupoints: additionally, at GB34, SP9, GB39 and SP6 | FC, periaqueductal gray (PAG) as the seed | RS, 6 times 25 min acupuncture sessions in 1 month | / |
| 22 | Li et al., 2016 | 62 migraine/46 HC | MA | 11 VA1/11 VA2/13 VA3/11 SA/16 WT | N | VA1: GB34, GB40 and SJ5; VA2: GB33, GB42 and SJ8; VA3: ST36, ST42 -and L16; SA: NAP1, NAP2 and NAP3 | FC, periaqueductal gray (PAG) as the seed region | RS, 30 min, 5 times/week, 4 weeks. | / |
| 23 | Zheng et al., 2016 | 28 hypertension | MA | 14 MA/14 SA | / | LR3 | FC, hypothalamus as the seed | RS, 30 min, three times/week for 2 week | / |
| 24 | Tan et al., 2017 | 32 mild cognitive impairment | MA | 16 MA/16 SA | / | EX-HN1, EX-HN3, PC6, KI3, ST40, and LR3 | FC, pregenual ACC, sub-ACC, MTL-hippocampus, IPL, and anterior insula as the seed region | RS, 5 times/week, for 4 consecutive weeks. | / |
| 25 | Li et al., 2018 | 35 Parkinson's disease | MA | 14 MA/11 SA/10 WT | / | DU20, bilateral GB20, and the Chorea-Tremor Controlled Zone | DC,ReHo,ALFF | RS, 30 min, 2 times/week, for 12 weeks | / |
| 26 | Wang et al., 2020 | 45 primary insomnia | MA | 15 S-Acu/15 M-Acu/15 N-Acu | / | S-Acu: bilateral HT7; M-Acu: combination of bilateral HT-7, bilateral SP6 and single DU20; N-Acu: sham point | fALFF | RS, 30 min, 5 times/week, for 5 weeks | / |
ACC, anterior cingulate cortex; DC, degree centrality; EA, Electroacupuncture; fALFF, fractional amplitude of low-frequency fluctuations; FC, functional connectivity analysis; GLM, general linear model; HC, health controls; ICA, independent component analysis; MA, manual acupuncture; M, multiple; /, irrelevant; NAP, non-acupoint; NI, non-treatment instruction; N, no; NRER, non-repeated event-related; RS, resting state; ReHo, regional homogeneity; SA: sham acupuncture; S, single; TI, treatment instruction; WT, waiting list; VA, verum acupuncture; Y, yes; Acupoints: BL23, Shenshu; BL25, Dachangshu; BL40, Weizhong; BL62, Shenmai; BL26, Guanyuanshu; BL36, Chengfu; BL54, Zhibian; BL60, Kunlun; BL58, Feiyang; BL27, Xiaochangshu; BL37, Yinmen; DU3, Yaoyangguan; DU20, Baihui; DU23, Shangxing; DU29, Yintang; EX-HN5,Taiyang; EX-HN1, Sishenchong; GB8, Shuaigu; GB30, Huantiao; GB31, Fengshi; GB33,Xiyangguan; GB39, Xuanzhong; GB40, Qiuxu; GB41, Zulinqi; HT3, Shaohai; HT5, Tongli; HT7, Shenmen; KI3, Taixi; LI3, Sanjian; LI4, Hegu; LI6, Pianli; LI7, Lieque; LR8, Ququan; LR14,Jimen; LR3, Taichong; PC6, Neiguan; PC7, Daling; PC8, Laogong; RN4, Guanyuan; RN6,Qihai; RN10, Xiawan; RN12, Zhongwan;RN14, Juque; SJ6, Zhigou; SJ5, Waiguan; SJ8, Sanyangluo; SJ22, Erheliao; SJ23, Sizhukong; SP6, Sanyinjiao; SP8, Diji; SP9, Yinlingquan; SP3, Taibai; SP14, Fujie; SP11, Jimen; SP13, Fushe; SP15, Daheng; ST6, Jiache; ST9, Renying; ST21,Liangmen; ST24, Huaroumen; ST25, Tianshu; ST26, Wailing; ST27, Daju; ST35, Dubi; ST36, Zusanli; ST37, Shangjuxu; ST38, Tiaokou; ST39, Xiajuxu; ST40, Fenglong; ST42, Chongyang; ST44, Neiting.
Overall, there was a great deal of heterogeneity between the studies. Some studies (Li et al., 2016; Wang et al., 2020) showed no statistical and clinical significance between the real acupoint group and the non-acupoint group. Other studies (Tan et al., 2017; Li et al., 2018) showed significant improvements in clinical symptoms, however, needling produced more significant activation at acupuncture points than at non-acupoints.
Interestingly, two studies (Huang et al., 2011; Chen et al., 2014) randomly assigned stroke patients to two groups: one group underwent sham needling (tactile stimulation) and true needling at the SJ5 (Waiguan) in healthy upper limb and the other group underwent sham and true needling at a sham point. Results showed that needling at SJ5 in healthy upper limbs of stroke patients resulted in reduced activation of brain functional areas, with no evident activation points, compared with tactile stimulation and needling at sham points. In addition, a significant difference in activation reduction was found between tactile stimulation and needling in sham point groups.
(2) Patients and HC
A total of 20 studies on neural response of patients and HC to acupuncture were included (Table 2).
Table 2.
Characteristics of studies about patients and HC.
| Numbers | References | Subjects | Intervention | Groups | Acupoints | Data analysis | Experimental design | Results |
|---|---|---|---|---|---|---|---|---|
| 1 | Li et al., 2006 | 12 stroke/12 HC | EA | / | LI4 and LI11 | SPM | Block/R(45s)-S(45s), 3 times | Compared to HC, patients showed greater activation in the somatosensory cortex with both the tactile task and the acupoint stimulation |
| 2 | Wu et al., 2008 | 11 spastic cerebral palsy/10 HC | MA | / | Left LI3 | SPM | Block/S(1min)-R(1min),3 times | Compared to HC, the children with cerebral showed significant decrease in the frontal lobe contralateral temporal lobe, and parahippocampal gyrus; and signal increase in bilateral occipitallobe and ipsilateral insula. |
| 3 | Li and Yang, 2011 | 7 aphasia stroke/14 HC | EA | / | SJ 8 | SPM | Block/R(45s)-S(45s), 3 times | Compared to HC, patients showed significant activation in the opercular, triangular, or insula. |
| 4 | Feng et al., 2012 | 12 mild cognitive impairment/12 HC | MA | DA/SA | KI3 | FC | NRER/R(1min)-S(DA/SA)(2min)-R(6min) | Compared to HC, mild cognitive impairment patients showed enhanced the correlations related with the temporal regions. |
| 5 | Yeo et al., 2012 | 12 Parkinson's Disease/12 HC | MA | VA/SA | Right GB34 | SPM | R(4min)-sham(S(1min)-R(1min-S(1min)-R(1min)-R(4min)-T1(10min)-verm(S(1min)-R(1min)-S(1min)-R(1min)-R(4min) | Compared to the HC, patients with Parkinson's disease showed a significantly higher signal increase in the thalamus |
| 6 | Chen J. et al., 2013 | 10 ischemic stroke/6 HC | MA | / | SJ5 | SPM | Block/R(30s)-S(30s), 6 times | Compared to the HC, stroke patients showed enhanced activation in the left Brodmann areas, hypothalamus, and the ventral posterolateral nucleus, and the right BA4, 6, 7, 18, 19, and 32. |
| 7 | Cho et al., 2013 | 11 stroke/10 HC | MA | / | LI11 and ST36 | SPM | Block/R(30s)-S(30s), 3 times | Compared to the HC, stroke group showed less brain activation. |
| 8 | Zhou et al., 2013 | 24 functional diarrhea/24 HC | MA | / | ST25 | ReHo and FC | RS/2 weeks, 5 sessions per week | Compared to HC, functional diarrhea was more effective in clinical outcome and had more extensive cerebral ReHo changes. |
| 9 | Quah-Smith et al., 2013 | 10 depression/10 HC | LA | / | LR14, LR8, RN14, and HT7 | ICA | Task/block(2s delay-R(2s)-s(20s))/8 times, 8 session | Compared to HC, depressed participants had wider posterior default mode network modulation at the parieto–temporal–limbic cortices. |
| 10 | Zhang et al., 2014 | 8 ischemic stroke/10 HC | MA | DA/SA | GB34 | SPM | NRER/R(1min)-S(1min)-R(8min) | Compared to HC, stroke patients showed the enhanced interregional interactions between the anterior cingulate cortex (ACC) and posterior cingulate cortex (PCC). |
| 11 | Xie et al., 2014 | 9 stable recovery stroke/8 HC | MA | / | GB34 | GLM and GCA | NRER/R(1min)-S(1min)-R(8min) | Compared to HC, stroke patients showed specific modulations of motor-related network in stroke patients. |
| 12 | He et al., 2014 | 28 Bell's palsy/20 HC | MA | 18 early group/21 late group/19 recovered group | LI4 on the contralateral side of paresis | FC, SI as the seed region | RS/10 min, three times a week | No significant changes in HC, Bell's pals patients showed significant connectivity changes in the SI region. |
| 13 | Wang et al., 2014 | 14 Alzheimer's Disease/14 HC | MA | / | Bilateral LR3 and LI4 | FC, bilateral hippocampus as the seed region | Block/R(3min)-S(3min)-R(10min) | No significant changes in HC, Alzheimer's Disease(AD) patients showed increased FC in right hippocampus and right STG. |
| 14 | Liang et al., 2014 | 9 Alzheimer's Disease/11 HC | MA | / | Right Liv3 and LI4 | ICA | Block/R(3min)-S(3min)-R(10min) | All the brain activation modulated by acupuncture were specifically for AD but not for HC. |
| 15 | Li et al., 2014d | 24 functional dyspepsia/24 HC | MA | / | Right ST36 | GLM | Block/R(1min)-S(1min)-R(1min)-S(1min)-R(1min)-S(1min)-R(1min) | Compared to HC, acupuncture evoked pronounced changes, especially in the homeostatic afferent processing network of FD patients. |
| 16 | Yeo et al., 2014 | 12 Parkinson's disease/12 HC | MA | VA/SA | GB34 | SPM | Block/SA:R(60s)-S(60s)-R(60s)-S(60s)-R(60s)-structural images(15min); then RA:R(60s)-S(60s)-R(60s)-S(60s)-R(60s) | Compared with HC, patients with PD showed significantly higher brain activity in the prefrontal cortex and precentral gyrus, especially visible in the left hemisphere. which are all known to be affected by PD |
| 17 | Gao et al., 2015 | 10 ischemic stroke/10 HC | MA | / | ST36 | SPM | Block/(30s)-S(30s), 6 times | Significant regions in the HC included the prefrontal cortex, cingulum, thalamus, and cerebellum; Significant regions in the stroke patients included the cuneus, supplementary motor area, and inferior parietal gyrus. |
| 18 | Wu et al., 2015 | 20 Bell's Palsy/20 HC | MA | / | LI4 | FC, ACC as the seed region | RS, block/R(10min)-S(10min, Rotate needles10 s every 2 min)-R(10min) | Significant decreased connectivity of the right ACC in the early group, no significant effect on FC of bilateral ACC in HC. |
| 19 | Han et al., 2019 | 22 poststroke motor impairment/22 HC | MA | / | GB34 | TBSS and FC | NRER/R(8 min10s)-S(1min)-R(8 min10s) | Compared with the HC, stroke patients showed enhanced FC between the (PM)/supplementary motor area (SMA) and supramarginal gyrus (SMG). |
| 20 | Han et al., 2020 | 26 ischemic stroke/21 HC | MA | / | GB34 | Graph Theoretical Network Analysis | RS/R(8min10s)-S(60s)-R(8min10s) | Compared with the HC, the stroke patients had a decreased normalized small-worldness (σ), global efficiency (Eg), and the mean local efficiency (Eloc) of the whole-brain network in the resting state. |
LA, laser acupuncture; SI, primary somatosensory area; TBSS, tract-based spatial statistics.
Except for three studies (He et al., 2014; Liang et al., 2014; Wang et al., 2014) that showed no significant brain activation in HC, most found that similar brain regions are activated by acupuncture in patients and HC. However, in patients, brain region activation and enhanced FC caused by acupuncture were disease-related brain areas.
Factors Influencing the Effect of Acupuncture
The factors influencing acupuncture efficacy have always been of strong research interest, which are helpful to increase understanding of the therapeutic mechanism and to provide guidance for clinical practice. However, it is not clear how these factors affect clinical efficacy.
Factors identified as potential influencing acupuncture efficacy are shown in Supplementary Table 2. Several studies investigated the influence of expectation, treatment instruction, augmented context, duration of acupuncture, disease stage, and selection of acupoints on the effect of acupuncture and the related brain response.
(a) Needling depth
Three studies (Feng et al., 2012; Bai et al., 2013; Chen S. et al., 2013) were performed to compare the effects and brain responses between deep and shallow needling, and results showed that deep needling is relatively more effective in mild cognitive impairment.
(b) Deqi and non-deqi
Two studies were performed to explore the differences in brain function between deqi and non-deqi, and results showed stronger brain activation in the deqi group.
(c) Expectation effects
Five studies (Liu et al., 2012; Hashmi et al., 2014; Gollub et al., 2018; Kong et al., 2018; Tu et al., 2019) were performed to explore the expectation effect, and results showed that expectation reduced symptoms and stimulated brain activity, which was influenced by the form of expectation.
(d) Selection of different acupoints
Three studies (Wang et al., 2016b, 2020; Zhang et al., 2020) were performed to compare the effects and brain mechanisms between single and multiple acupoints on diseases, mainly related to hypertension and primary insomnia. The results consistently showed that a combination of multiple acupoints was more effective by activating more brain regions than single acupoints.
In addition, several studies (Chen et al., 2015; Egorova et al., 2015; Li et al., 2016, 2017, 2020b) were performed to compare different acupoints or dosage levels, and results reported clinical but not brain activation differences, which might be due to small sample sizes. The consensus of these findings was that a combination of different acupoints has no significant difference in treatment effect.
- (e) Location of acupoint
- ① Ipsilateral and contralateral sides [opposing needling (ON)]
- Two fMRI studies (Zhang et al., 2018; Yan et al., 2020) on unilateral chronic shoulder pain compared brain activation in acupuncture on ipsilateral and contralateral sides (ON). They found that treatment on either side alleviates pain intensity and improves shoulder function, but the latter improvement was higher in the contralateral than the ipsilateral group. In addition, ReHo values and degree centrality (DC) differed between these groups.
- ② Local point and distal point
- One study (Maeda et al., 2013) was performed to compare the therapeutic effects of and brain response to acupuncture at local and distal points and found that visual analog scores for paresthesia showed significant reductions in the local but not distal group. In terms of brain response, consistent activation in two groups was found in the bilateral insula and secondary somatosensory cortex.
Discussions
Research on TCM has reached a point at which researchers should pause and reflect on its future directions. For thousands of years, its curative effect has not been widely accepted because it was based on unclear mechanisms. Therefore, a relatively objective theoretical system needs to be formed in the future for the sake of long-term development. The meridian effect was one of the essential building blocks of TCM theory and acupuncture. In recent years, the specificity of meridian acupoints has also become a research focus (Rong et al., 2013; Li et al., 2014a). Such a progression of research trends is in line with the development of modern technology such as fMRI, which was not available in the past.
To enhance understanding of the mechanism of acupuncture revealed by MRI, we conducted a comprehensive literature search with three key findings: (1) stroke and GB34 were the most studied disease and acupoint, respectively; (2) rs-fMRI and FC were the most often used experimental and analytic methods; (3) despite the heterogeneity among studies, the general trend was that effects are more specific in VA than SA, and that brain activation effects of needling inpatients were more specific than in HC. In addition, factors affecting the efficacy of acupuncture mainly included depth, acupoint, deqi, location, and expectancy effects.
Diseases and Acupoints
The most common disease types considered in the included studies were neuropsychiatric, perhaps due to the known treatment efficacy of acupuncture in these diseases. Among these, stroke was the most frequently studied. Stroke, defined as a neurological deficit attributed to an acute focal vascular injury of the central nervous system (Sacco et al., 2013), is a major cause of death and disability globally (Campbell and Khatri, 2020). It brings burdens to the family, seriously affecting the quality of life of the patient (Dowswell et al., 2000) which may be improved by rehabilitation of total motor dysfunction (Hamzat and Peters, 2009).
Acupuncture is recommended by the WHO as an alternative and complementary strategy for stroke treatment (Chavez et al., 2017). Clinical trial and meta-analysis findings have demonstrated the efficacy of acupuncture in improving balance function, reducing spasticity, and increasing muscle strength and general well-being post-stroke (Liu et al., 2009; Zhao et al., 2009; Chavez et al., 2017). Thus, uncovering the mechanism of the effect of acupuncture on movement in stroke has been of strong research interest in recent years.
Studies have found that acupuncture could not only induce brain activation in the motor and sensorimotor networks and increase motor-cognition connectivity but also enhance FC between the bilateral primary motor cortices and the default mode network (Ning et al., 2017). In addition, acupuncture could evoke pronounced structural reorganization (Wu et al., 2018). Importantly, research has shown that improvements in function and structure are interrelated, structural plasticity being associated with recovery of motor ability. However, due to small sample sizes and differences in affected brain regions, study designs and analytic methods, the precise link between acupoint, disease, and brain region remains unclear.
With the exception of GV20 (Baihui), the most frequently used acupoints in the included studies were in the four limbs, since these locations are accessible in the scanning state.
GB34 is located on the fibular aspect of the leg in the depression anterior and distal to the head of the fibula. According to TCM theory, GB34 was not only the “he” (meeting) point of the Gallbladder Meridian of Foot-Shao yang but also the influential point of tendons. Therefore, GB34 is often used to treat diseases of the motor system in clinical practice and trials, for example, recovering motor function for patients with stroke hemiplegia (Fang et al., 2016; Yang et al., 2016). In addition, different acupuncture techniques at GB34, such as MA, EA, fire acupuncture, and moxibustion, showed specific characteristics of therapeutic effects. Specifically, the main roles of moxibustion at GB34 are to warm the meridians, regulate Qi, and promote blood circulation, to relieve pain, EA at GB34 mainly focused on treating the motor system, and fire acupuncture at GB34 showed both above effects. One recent review (Xiaoling et al., 2020) investigated fMRI in acupuncture at GB34 and found activation of specific brain areas in the bilateral superior temporal gyrus, bilateral anterior central gyrus, bilateral orbital gyrus, and right inferior temporal gyrus. However, high heterogeneity and conflicting results were found among studies, indicating that further exploration is necessary based on large samples and careful experimental design to understand how to obtain reliable and stable brain responses to acupuncture at GB34.
Experimental Designs and Analytic Methods
Task state-fMRI during acupuncture administrations is often used to observe the immediate effect of acupuncture. Scanning methods are mostly blocked design and non-repeat event-related design, which can obtain real-time imaging data of the brain regions activated or inhibited by acupuncture, and signal to the noise level of BOLD responses may be increased by manipulating the acupuncture stimulation (Lee et al., 2016; Yin et al., 2019).
Although this method is simple and easy to perform, the experimental period is short. According to the theory of TCM, the effect of acupuncture may depend on the cumulative effect, which has been confirmed by several studies (Shi et al., 2012; Li et al., 2014b). Thus, it may be more suitable to explore the mechanism of immediate effect. The task state-fMRI design can be used to explore the specificity of different acupoints, acupuncture manipulation, and the response of different diseases to the same acupoints. In addition, this design is very suitable for diseases that respond quickly to acupuncture, such as pain diseases (Shi et al., 2015; Zhang et al., 2018). The rs-fMRI technique is a relatively novel approach in which participants are typically asked to rest quietly with their eyes open or closed for several minutes without performing any task (Mwansisya et al., 2017). Rs-fMRI investigates naturally occurring low-frequency (typically 0.01–0.08 Hz) fluctuations in BOLD signals, which has been considered to reflect physiologically meaningful changes of spontaneous neural activity in the resting-state networks (Mwansisya et al., 2017; Takamura and Hanakawa, 2017). Moreover, the network system in the resting state has a considerable degree of stability and presents a high degree of FC (Greicius et al., 2003). More importantly, it is well-known that acupuncture has a cumulative effect. This kind of experimental design is used to observe the changes in brain response after acupuncture treatment, which is helpful to explore the mechanism of long-term acupuncture effect such as investigating the effect of different courses of acupuncture and among different patients, and it is suitable for chronic diseases, such as insomnia (Wang et al., 2020) and depression (Wang et al., 2016b).
Various methods have been proposed for the processing and analysis of MRI data including structural MRI, Rs-fMRI, and DTI. In the present review, structural MRI, which plays an important role to help in understanding the anatomical changes related to acupuncture, mainly involved VBM and surfaced-based morphometry, whereas rs-fMRI mainly involved ReHo, ALFF, FC, seed-based correlation analysis, independent component analysis, and graph-theoretic metrics (Lee et al., 2013; Smitha et al., 2017), which have been widely used to gain a greater understanding of brain circuitry changes after acupuncture.
Different analytical methods are used to investigate the efficacy of acupuncture from different perspectives. FC, which is most commonly used, is defined as the temporal correlation between spatially remote neurophysiological events (Fu et al., 2017), expressed as deviation from statistical independence (temporal correlation) across these events in distributed neuronal groups and areas (Fingelkurts et al., 2005). This may suggest that neural plasticity may potentially be a bridge between acupuncture and the treatment of various diseases such as stroke.
Most studies used seed-based FC due to simplicity and ease of interpretation, with the advantage of focusing only on specific brain regions of interest and not the entire brain network. However, the resulting FC network is dependent on the selection of seed location, and the final FC network may vary significantly even if the seed location changes slightly (Cole et al., 2010; Sohn et al., 2015). Thus, the FC network is highly dependent on seed choice, leading to variation that may obscure results (Bell et al., 2019). Based on the above information, the selection of seed points and the combination of a variety of analytical methods are still important. As for the changes of FC caused by acupuncture, it is equally important to select the appropriate seed point to investigate the mechanism of acupuncture for different diseases.
Interestingly, few studies have focused on structural MRI analysis, perhaps due to the fact that structural change is relatively hard to observe, especially for immediate or short-term effects. While many previous studies reported no significant structural changes, the possibility that they occur could not be excluded, and more studies using modern methods are warranted for verification. Indeed, multimodal MRI may enhance understanding of the mechanism underpinning acupuncture effects due to the well-established links between structure and function of the brain.
Effect of Acupuncture
Verum Acupuncture and SA
Despite over 3,500 clinical studies on acupuncture, the debate about its effect continues (Colquhoun and Novella, 2013). Imaging technology provides an objective basis for the difference in curative effect between VA and SA. Consistent with several previous studies (Yoo et al., 2007; Deng et al., 2008; Dougherty et al., 2008), we found that VA significantly improves clinical symptoms and brain activation related to disease.
However, previous findings in HC are inconsistent. Some studies provided showed evidence that acupoints may have their functional specificity (He et al., 2015), whereas other findings (Fang et al., 2009; Hui et al., 2009) showed that no statistical difference was found between acupoints and sham acupoints. This may be explained by similar segmental innervations in HC. As shown by a recent systematic review (Ots et al., 2020), VA and SA have similar therapeutic effects due to their position in overlapping dermatomes, which partly explain several previous clinical studies (Assefi et al., 2005; Hinman et al., 2014) that showed no significant difference in the effect of VA compared with SA. Thus, to obtain reliable results, the location of the needles selected for SA should be at non-overlapping cutaneous segments based on the knowledge of segmental anatomy.
In addition, acupuncture at different acupoints could achieve different brain activation through dynamic reconstruction of neural networks and, thus, achieve therapeutic effects (Qin et al., 2011). However, Cho et al. (2006) found that acupoint and sham acupoint (away from the Meridians) showed a striking similarity in fMRI results, indicating that acupuncture is effective in pain relief regardless of the choice of point. Moreover, the authors proposed that the effect of acupuncture was one of stress analgesia alone. An activation likelihood estimation meta-analysis of fMRI studies (Chae et al., 2013) showed that a similar but weaker pattern of response was observed with control tactile stimulation than with acupuncture needling. Previous studies (Treede et al., 1999; Kong et al., 2010) also found that the brain areas in which activation was changed by acupuncture needle stimulation largely overlap with those that constitute the so-called pain matrix, suggesting that the brain response to acupuncture is triggered by the pain of needle penetration into the skin. Neuroimaging data demonstrate that placebo analgesia activates subcortical and cortical opioid sensitive brain regions, such as the periaqueductal gray, rostral anterior cingulate, and thalamus, many of which overlap with the area of acupuncture modulation (Dhond et al., 2007). It is important to note that the above studies all included patients with pain, and the placebo response is often strong in pain studies (Vase and Wartolowska, 2019).
In summary, brain activation may be observed in SA and responses may be similar to those of VA in both patients and HC. The type of disease and the acupoints used should be considered when deciding which type of SA to be used as control.
Patients and HC
In this review, we included 20 studies that investigated differences in acupuncture-related brain activation in patients and HC. Differences in brain activation between these groups indicated higher specificity in patients than HC in brain regions associated with the relevant disease. These findings imply functional specificity of acupuncture, indicating that acupuncture exerted obvious effects under a pathological condition (Han et al., 2019).
To date, research has shown that the therapeutic effects of acupuncture are achieved not by relieving the diseased area locally but by reestablishing the balance of the internal milieu (involving Ying/Yang, the Five Elements, and the Zang-Fus) (Leung, 2012). It is generally agreed that acupuncture plays a homeostatic role, and thus may have a greater effect on patients with a pathological imbalance compared to HC (Kaptchuk, 2002). Therefore, a lack of significant effect in fMRI studies on healthy subjects may reflect homeostasis existing prior to the intervention in those individuals.
Based on the TCM theory, acupuncture could regulate the body in a bidirectional manner, the regulatory effects differing under physiological and pathological conditions. Acupuncture is a normal part of physiological functions for healthy people and a reflection of the normal Qi and blood running conditions. However, for patients, therapeutic effects of acupuncture are observed in disease, under pathological conditions. Interestingly, one meta-analysis showed that experimental pain in HC and chronic clinical pain conditions in patients have overlapping brain activation patterns, but the mechanism differs (Apkarian et al., 2005).
Thus, more scientific evidence is needed to convincingly demonstrate the specificity of acupuncture in patients.
Factors Influencing Efficacy
Depth of Acupuncture
Acupuncture textbooks provide recommended ranges for the depth of insertion, mainly for safety purposes (Maoliang and Shanchen, 1985). In this review, the depth of insertion is considered as a factor in the efficacy of acupuncture. However, MacPherson et al. (2008) found no significant difference in the activation of brain regions between superficial and deep acupuncture in healthy subjects, perhaps related to the used acupoint (LI4, Hegu), where deqi and efficacy are easily achieved.
In this review, studies investigated the efficacy and mechanism of acupuncture for mild cognitive impairment at different depths using different analytic methods, and they found that deep acupuncture is necessary to achieve significant clinical results (Feng et al., 2012; Bai et al., 2013; Chen S. et al., 2013). Such findings are consistent with the Layer Analysis as described in the Yellow Emperor's Inner Classic (Goh et al., 2014). Moreover, the studies consistently showed that deep needling affected a larger number of abnormal brain regions than superficial needling, especially at the hippocampus. In addition, deep needling can induce much stronger and wider-ranging deqi (Bai et al., 2013).
Physiological mechanisms related to the effect of deep insertion can be explained based on the structures affected by the needle: the skin, muscle fascia, and muscle. At greater depths, needling may better interact with ascending nerve tracks than with cutaneous afferents (Goldman et al., 2010). Sandberg et al. (2003) indicated that the intensity of deqi resulted in a pronounced increase in both skin and muscle blood flows using photoplethysmography, demonstrating that the depth of acupuncture also is an important factor for deqi.
Deqi
For decades, it has been thought that the deqi of acupuncture is related to clinical efficacy. Several studies (Li et al., 2014c; Shi et al., 2014; Yin et al., 2017; Zhao et al., 2017) reported that deqi group can significantly reduce the severity of symptoms and showed better efficacy compared with acupuncture without deqi. Deqi in pain may be driven by slow conduction of pain fibers. Integrating these signals into the central nervous system leads to the modulation of other sensory inputs, which is at least part of the acupuncture effects (Zhou and Benharash, 2014).
Results from two studies (Li et al., 2015; Sun et al., 2020) on acupuncture for a pathological condition were inconsistent with previous research (Sun et al., 2013) on deqi, showing that the effect of deqi was related to the processing of somatosensory or pain signals. The discrepancy between results was explained by small sample sizes, different physiological states, diseases, and acupoints.
Although we are aware of the correlation between deqi and clinical efficacy, as described by Sun et al. (2013), standardization of the quantitative methods of deqi, deeper understanding of the link between deqi and sharp pain, and improvements of statistical methods are necessary to better investigate the mechanism of deqi.
Expectation
Studies suggested that non-specific factors such as the expectations of a participant could significantly modulate the effects of acupuncture treatment (Pariente et al., 2005; Kong et al., 2009) and play an important role in the placebo response (Kaptchuk et al., 2008; Howe et al., 2017). In the present review, several studies (Kong et al., 2009, 2018; Gollub et al., 2018) were consistent that expectation can significantly enhance the analgesic effect of VA.
Interestingly, the oldest canonical classic of Chinese medicine, the Yellow Emperor's Inner Classic (Huang Di Nei Jing), has long recorded this. Written in the first century BCE, the text states that “if a patient does not consent to therapy with positive engagement, the physician should not proceed as the therapy will not succeed” (SuWen Chapter 11).
However, two studies (Tu et al., 2019; Yu et al., 2020) included in this review did not detect the expected significant differences between high and low context groups. Perhaps the method of creating expectation affected brain response and clinical efficacy, since gaining the trust of patients is a complicated process. Warmth and empathy maybe just two of several factors that can influence the expectations and beliefs of patients (Kong et al., 2009).
To date, research on the expectation effect has mainly involved analgesia, which found that although the expectation and acupuncture could achieve similar analgesic effects, their brain activation responses were different (Kong et al., 2009). Moreover, brain networks involved in expectation modulation can vary with the methods used to create expectations. Therefore, it may be important to investigate the most effective method to generate expectations in patients based on the standard expectation scale and with large sample size.
Different Acupoints
The choice of acupoints is a key factor affecting the therapeutic effect of acupuncture (Armour and Smith, 2016). It is even more important to understand the specific brain activation of each acupoint, but this is not straightforward. One previous study (Cho et al., 1998) has shown that acupuncture at BL67 activated the visual cortex, but the results have not been replicated (Siedentopf et al., 2002; Li et al., 2003). In addition, GB37 (Gareus et al., 2002) and GB43 (Wesolowski et al., 2009) were used to explore visual and auditory cortical activation, respectively, but the evidence is of insufficient quality.
All the three studies included in this review showed that multiple acupoints activated more brain regions and showed better efficacy than a single acupoint. Although the difference in efficacy was not statistically significant, the results indicated that the combined acupoints created broader stimulation of brain areas (Zhang et al., 2019), rather than a simple sum of the effects at more than one acupoint. However, some researchers found no difference between two-point and single-point stimulation (Alizadeh et al., 2014; Xing, 2016; Qu et al., 2020).
While there is broad agreement on acupoint number as a factor in the efficacy of acupuncture, some inconsistencies remain. Further comparison of brain responses between different single and multiple acupoints is imperative to establish the link between acupoints and diseases.
Location of Acupoints
According to TCM theory, diseases are caused by an imbalance between Yin and Yang. Therefore, balancing Yin and Yang is a key to treating diseases (Shuang et al., 2020). ON, as a method of achieving this balance, is widely used in the treatment of various diseases, including using the left acupoint to treat the right, using the lower acupoint to treat the upper, and using the front acupoint to treat conditions of the back, which produced beneficial effects. In this review, two studies (Zhang et al., 2018; Yan et al., 2020) used fMRI to explore the mechanism and efficacy of acupuncture at non-painful side ST38 on the painful side of chronic shoulder pain and between local and distal points. However, there is no clear definition in the literature on the distance that should be considered local or distant (Wong et al., 2015). The differences in efficacy and mechanism found between the two do provide evidence that can be used in the clinic, but long-term efficacy and prognosis still need to be further verified.
In summary, it can be seen from the above discussion that further research is needed to explore the mechanisms by which a range of factors influence the acupuncture effect. This is because the factors are numerous, and they are not limited to needle depth, deqi, disease stage, treatment course, and some non-specific effects, such as expectation effect and understanding of patients about acupuncture. Additional factors such as acupuncture time, manipulation, and duration need to be further investigated in the future.
Limitations and Perspectives for Future Studies
Overall, acupuncture does have some effects on brain activation. The application of modern technology such as MRI, the diversification of analytical methods, and the development of algorithms make the study of brain responses more accurate. However, some limitations should be acknowledged. First, many non-acupuncture factors interfere with brain response to stimulation at acupoints. The form of the placebo, the psychological attitude of the participants toward acupuncture, and the illness of the patients were the three most interesting factors. Second, although this review has explored the effect of acupuncture and the factors influencing acupuncture efficacy from many perspectives, it cannot draw a reliable conclusion due to the small samples and large heterogeneity of the included studies. Third, while many studies have been conducted on the immediate effects of acupuncture, those evaluating brain responses to long periods of clinical acupuncture treatment are still lacking. Fourth, we did not include non-English studies; therefore, a language bias may be present.
In summary, there is much room for further research investigating the links among acupoint, brain activation, and disease type. First, the selection of appropriate SA is the basis of clinical effectiveness since SA type affects the assessment of the efficacy of acupuncture. Second, brain response differs between patients and HC. The response to acupuncture in pathological conditions is mainly concentrated at the pathology-related brain regions, so the same acupuncture in HC could not elicit a similar brain effect to stimulation at this acupoint. Third, standardization of MRI parameters and data collection may increase the homogeneity of results, and results such as coordinates should be made public to pave the way for verification studies and other future applications. Fourth, adherence to the Standards for Reporting Interventions in Clinical Trials of Acupuncture guidelines is necessary since the standardization of acupuncture methodology is very important to obtain reliable and precise results.
In brief, exploring the mechanism of acupuncture with imaging tools is a promising avenue for TCM. However, future developments, such as the accuracy of patient-specific predictions made by machine learning approaches, should be based on high-quality data, including the standardization of acupuncture and MRI parameters.
Conclusions
In conclusion, MRI, as an advanced visualization method, facilitates a better understanding of the neural mechanisms of acupuncture. We found that stroke and GB34 were the most studied disease and acupoint, and rs-fMRI and FC were the most applied experimental and analytic methods. We found that the type of SA affected the efficacy of acupuncture and the brain response. Processing in the brain after acupuncture differs between patients and healthy individuals. The brain response to acupuncture in patients occurs mainly in disorder-related areas. The factors influencing the efficacy of acupuncture, including depth of needling, number and location of acupoints, deqi, and expectation effect, could be objectively assessed through brain responses. However, due to small sample sizes, different study designs, and analytical methods, the results were heterogeneous. Further studies with larger sample sizes, careful experimental design, and multimodal neuroimaging techniques, and standardized acupuncture and MRI methods should be conducted to better explain the efficacy and specificity of acupuncture, and to prepare for accurate efficacy prediction in the future.
Author Contributions
JZ and JX designed the whole study, analyzed the data, and wrote the manuscript. ZhL and ZiL searched and selected the studies. JL participated in the interpretation of data. HY and QH offered good suggestions. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
Funding. This study was supported by the National Key R&D Program of China (2019YFC1712200), International standards research on clinical research and service of Acupuncture-Moxibustion (2019YFC1712205), Shenzhen Key Basic Research Program (JCYJ20200109114816594), and Shenzhen's Sanming Project (SZSM201612001).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnhum.2021.694919/full#supplementary-material
References
- Alizadeh R., Esmaeili S., Shoar S., Bagheri-Hariri S., Shoar N. (2014). Acupuncture in preventing postoperative nausea and vomiting: efficacy of two acupuncture points versus a single one. J. Acupunct. Meridian Stud. 7, 71–75. 10.1016/j.jams.2013.04.005 [DOI] [PubMed] [Google Scholar]
- Apkarian A. V., Bushnell M. C., Treede R. D., Zubieta J. K. (2005). Human brain mechanisms of pain perception and regulation in health and disease. Eur. J. Pain 9, 463–484. 10.1016/j.ejpain.2004.11.001 [DOI] [PubMed] [Google Scholar]
- Armour M., Smith C. A. (2016). Treating primary dysmenorrhoea with acupuncture: a narrative review of the relationship between acupuncture 'dose' and menstrual pain outcomes. Acupunct. Med. 34, 416–424. 10.1136/acupmed-2016-011110 [DOI] [PubMed] [Google Scholar]
- Assefi N. P., Sherman K. J., Jacobsen C., Goldberg J., Smith W. R., Buchwald D. (2005). A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann. Intern. Med. 143, 10–19. 10.7326/0003-4819-143-1-200507050-00005 [DOI] [PubMed] [Google Scholar]
- Bai L., Zhang M., Chen S., Ai L., Xu M., Wang D., et al. (2013). Characterizing Acupuncture De Qi in mild cognitive impairment: relations with small-world efficiency of functional brain networks. Evid. Based Compl. Alt. 2013, 1–8. 10.1155/2013/304804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell C. S., Mohd K. N., Ding Z., Wilkes D. M. (2019). Bayesian framework for robust seed-based correlation analysis. Med. Phys. 46, 3055–3066. 10.1002/mp.13522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai R., Shen G., Wang H., Guan Y. (2018). Brain functional connectivity network studies of acupuncture: a systematic review on resting-state fMRI. J. Integr. Med. 16, 26–33. 10.1016/j.joim.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Campbell B., Khatri P. (2020). Stroke. Lancet 396, 129–142. 10.1016/S0140-6736(20)31179-X [DOI] [PubMed] [Google Scholar]
- Chae Y., Chang D. S., Lee S. H., Jung W. M., Lee I. S., Jackson S., et al. (2013). Inserting needles into the body: a meta-analysis of brain activity associated with acupuncture needle stimulation. J. Pain 14, 215–222. 10.1016/j.jpain.2012.11.011 [DOI] [PubMed] [Google Scholar]
- Chae Y., Lee H., Kim H., Kim C., Chang D., Kim K., et al. (2009). Parsing brain activity associated with acupuncture treatment in Parkinson's diseases. Movement Disord. 24, 1794–1802. 10.1002/mds.22673 [DOI] [PubMed] [Google Scholar]
- Chavez L. M., Huang S. S., MacDonald I., Lin J. G., Lee Y. C., Chen Y. H. (2017). Mechanisms of acupuncture therapy in ischemic stroke rehabilitation: a literature review of basic studies. Int. J. Mol. Sci. 18:2270. 10.3390/ijms18112270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Huang Y., Lai X., Tang C., Yang J., Chen H., et al. (2013). Acupuncture at Waiguan (TE5) influences activation/deactivation of functional brain areas in ischemic stroke patients and healthy people: a functional MRI study. Neural Regen Res 8, 226–232. 10.3969/j.issn.1673-5374.2013.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Wang J., Huang Y., Lai X., Tang C., Yang J., et al. (2014). Modulatory effect of acupuncture at Waiguan (TE5) on the functional connectivity of the central nervous system of patients with ischemic stroke in the left basal ganglia. PLoS ONE 9:e96777. 10.1371/journal.pone.0096777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Bai L., Xu M., Wang F., Yin L., Peng X., et al. (2013). Multivariate Granger causality analysis of acupuncture effects in mild cognitive impairment patients: an fMRI study. Evid. Based Compl. Alt. 2013:127271. 10.1155/2013/127271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Spaeth R. B., Retzepi K., Ott D., Kong J. (2015). Acupuncture modulates cortical thickness and functional connectivity in knee osteoarthritis patients. Sci. Rep. UK 4:6482. 10.1038/srep06482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho S. Y., Kim M., Sun J. J., Jahng G. H., Kim H. J., Park S. U., et al. (2013). A comparison of brain activity between healthy subjects and stroke patients on fMRI by acupuncture stimulation. Chin. J. Integr. Med. 19, 269–276. 10.1007/s11655-013-1436-4 [DOI] [PubMed] [Google Scholar]
- Cho Z. H., Chung S. C., Jones J. P., Park J. B., Park H. J., Lee H. J., et al. (1998). New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc. Natl. Acad. Sci. U. S. A. 95, 2670–2673. 10.1073/pnas.95.5.2670 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Cho Z. H., Hwang S. C., Wong E. K., Son Y. D., Kang C. K., Park T. S., et al. (2006). Neural substrates, experimental evidences and functional hypothesis of acupuncture mechanisms. Acta Neurol. Scand. 113, 370–377. 10.1111/j.1600-0404.2006.00600.x [DOI] [PubMed] [Google Scholar]
- Chu W. C., Wu J. C., Yew D. T., Zhang L., Shi L., Yeung D. K., et al. (2012). Does acupuncture therapy alter activation of neural pathway for pain perception in irritable bowel syndrome?: a comparative study of true and sham acupuncture using functional magnetic resonance imaging. J. Neurogastroenterol. 18, 305–316. 10.5056/jnm.2012.18.3.305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole D. M., Smith S. M., Beckmann C. F. (2010). Advances and pitfalls in the analysis and interpretation of resting-state FMRI data. Front. Syst. Neurosci. 4:8. 10.3389/fnsys.2010.00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colquhoun D., Novella S. P. (2013). Acupuncture is theatrical placebo. Anesth. Analg. 116, 1360–1363. 10.1213/ANE.0b013e31828f2d5e [DOI] [PubMed] [Google Scholar]
- Da S. A. (2015). Acupuncture for migraine prevention. Headache 55, 470–473. 10.1111/head.12525 [DOI] [PubMed] [Google Scholar]
- Deng G., Hou B. L., Holodny A. I., Cassileth B. R. (2008). Functional magnetic resonance imaging (fMRI) changes and saliva production associated with acupuncture at LI-2 acupuncture point: a randomized controlled study. BMC Complement. Altern. Med. 8:37. 10.1186/1472-6882-8-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhond R. P., Kettner N., Napadow V. (2007). Do the neural correlates of acupuncture and placebo effects differ? Pain 128, 8–12. 10.1016/j.pain.2007.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty D. D., Kong J., Webb M., Bonab A. A., Fischman A. J., Gollub R. L. (2008). A combined [11C]diprenorphine PET study and fMRI study of acupuncture analgesia. Behav. Brain Res. 193, 63–68. 10.1016/j.bbr.2008.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowswell G., Lawler J., Dowswell T., Young J., Forster A., Hearn J. (2000). Investigating recovery from stroke: a qualitative study. J. Clin. Nurs. 9, 507–515. 10.1046/j.1365-2702.2000.00411.x [DOI] [PubMed] [Google Scholar]
- Egorova N., Gollub R. L., Kong J. (2015). Repeated verum but not placebo acupuncture normalizes connectivity in brain regions dysregulated in chronic pain. Neuroimage Clin. 9, 430–435. 10.1016/j.nicl.2015.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J., Chen L., Ma R., Keeler C. L., Shen L., Bao Y., et al. (2016). Comprehensive rehabilitation with integrative medicine for subacute stroke: a multicenter randomized controlled trial. Sci. Rep. 6:25850. 10.1038/srep25850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J., Jin Z., Wang Y., Li K., Kong J., Nixon E. E., et al. (2009). The salient characteristics of the central effects of acupuncture needling: limbic-paralimbic-neocortical network modulation. Hum. Brain Mapp. 30, 1196–1206. 10.1002/hbm.20583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Bai L., Ren Y., Chen S., Wang H., Zhang W., et al. (2012). FMRI connectivity analysis of acupuncture effects on the whole brain network in mild cognitive impairment patients. Magn. Reson. Imaging 30, 672–682. 10.1016/j.mri.2012.01.003 [DOI] [PubMed] [Google Scholar]
- Fingelkurts A. A., Fingelkurts A. A., Kahkonen S. (2005). Functional connectivity in the brain–is it an elusive concept? Neurosci. Biobehav. Rev. 28, 827–836. 10.1016/j.neubiorev.2004.10.009 [DOI] [PubMed] [Google Scholar]
- Fu C., Li K., Ning Y., Tan Z., Zhang Y., Liu H., et al. (2017). Altered effective connectivity of resting state networks by acupuncture stimulation in stroke patients with left hemiplegia. Medicine 96:e8897. 10.1097/MD.0000000000008897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y., Lin Z., Tao J., Yang S., Chen R., Jiang C., et al. (2015). Evidence of timing effects on acupuncture: a functional magnetic resonance imaging study. Exp. Ther. Med. 9, 59–64. 10.3892/etm.2014.2056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gareus I. K., Lacour M., Schulte A. C., Hennig J. (2002). Is there a BOLD response of the visual cortex on stimulation of the vision-related acupoint GB 37? J. Magn. Reson. Imaging 15, 227–232. 10.1002/jmri.10059 [DOI] [PubMed] [Google Scholar]
- Goh Y. L., Liu J., Zhao B. (2014). Use of the Layer Analysis Method of the Yellow Emperor's Inner Classic in modern society. J. Acupunct. Meridian Stud. 7, 331–336. 10.1016/j.jams.2014.02.004 [DOI] [PubMed] [Google Scholar]
- Goldman N., Chen M., Fujita T., Xu Q., Peng W., Liu W., et al. (2010). Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat. Neurosci. 13, 883–888. 10.1038/nn.2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollub R. L., Kirsch I., Maleki N., Wasan A. D., Edwards R. R., Tu Y., et al. (2018). A functional neuroimaging study of expectancy effects on pain response in patients with knee osteoarthritis. J. Pain 19, 515–527. 10.1016/j.jpain.2017.12.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greicius M. D., Krasnow B., Reiss A. L., Menon V. (2003). Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc. Natl. Acad. Sci. U. S. A. 100, 253–258. 10.1073/pnas.0135058100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Xing X., Wu J., Zhang H., Yun Y., Qin Z., et al. (2020). Acupuncture for adults with diarrhea-predominant irritable bowel syndrome or functional diarrhea: a systematic review and meta-analysis. Neural Plast. 2020:8892184. 10.1155/2020/8892184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamzat T. K., Peters G. O. (2009). Motor function recovery and quality of life among stroke survivors in Ibadan, Nigeria. A 6-month follow-up study. Eur. J. Phys. Rehabil. Med. 45, 179–183. 10.1177/0269215509102957 [DOI] [PubMed] [Google Scholar]
- Han J. S. (2011). Acupuncture analgesia: areas of consensus and controversy. Pain 152, S41–S48. 10.1016/j.pain.2010.10.012 [DOI] [PubMed] [Google Scholar]
- Han X., Bai L., Sun C., Niu X., Ning Y., Chen Z., et al. (2019). Acupuncture enhances communication between cortices with damaged white matters in poststroke motor impairment. Evid. Based Compl. Alt. 2019, 1–11. 10.1155/2019/4245753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X., Jin H., Li K., Ning Y., Jiang L., Chen P., et al. (2020). Acupuncture modulates disrupted whole-brain network after ischemic stroke: evidence based on graph theory analysis. Neural Plast. 2020, 1–10. 10.1155/2020/8838498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashmi J. A., Kong J., Spaeth R., Khan S., Kaptchuk T. J., Gollub R. L. (2014). Functional network architecture predicts psychologically mediated analgesia related to treatment in chronic knee pain patients. J. Neurosci. 34, 3924–3936. 10.1523/JNEUROSCI.3155-13.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He T., Zhu W., Du S. Q., Yang J. W., Li F., Yang B. F., et al. (2015). Neural mechanisms of acupuncture as revealed by fMRI studies. Auton. Neurosci. 190, 1–9. 10.1016/j.autneu.2015.03.006 [DOI] [PubMed] [Google Scholar]
- He X., Zhu Y., Li C., Park K., Mohamed A. Z., Wu H., et al. (2014). Acupuncture-induced changes in functional connectivity of the primary somatosensory cortex varied with pathological stages of Bell's palsy. Neuroreport 25, 1162–1168. 10.1097/WNR.0000000000000246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinman R. S., McCrory P., Pirotta M., Relf I., Forbes A., Crossley K. M., et al. (2014). Acupuncture for chronic knee pain: a randomized clinical trial. JAMA 312, 1313–1322. 10.1001/jama.2014.12660 [DOI] [PubMed] [Google Scholar]
- Howe L. C., Goyer J. P., Crum A. J. (2017). Harnessing the placebo effect: exploring the influence of physician characteristics on placebo response. Health Psychol. 36, 1074–1082. 10.1037/hea0000499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q., Luo D., Chen L., Liang F. X., Chen R. (2019). Effectiveness of acupuncture for Alzheimer's disease: an updated systematic review and meta-analysis. Curr Med Sci 39, 500–511. 10.1007/s11596-019-2065-8 [DOI] [PubMed] [Google Scholar]
- Huang Y., Xiao H., Chen J., Qu S., Zheng Y., Lu Y., et al. (2011). Needling at the Waiguan (SJ5) in healthy limbs deactivated functional brain areas in ischemic stroke patients A functional magnetic resonance imaging study. Neural Regen Res 6, 2829–2833. 10.3969/j.issn.1673-5374.2011.36.005 [DOI] [Google Scholar]
- Hui K. K., Marina O., Claunch J. D., Nixon E. E., Fang J., Liu J., et al. (2009). Acupuncture mobilizes the brain's default mode and its anti-correlated network in healthy subjects. Brain Res. 1287, 84–103. 10.1016/j.brainres.2009.06.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang O. S., Kim S. Y., Jahng G. H., Kim H., Kim J. W., Chung S. Y., et al. (2013). Neural substrates of acupuncture in the modulation of cravings induced by smoking-related visual cues: an fMRI study. Psychopharmacology 228, 119–127. 10.1007/s00213-013-3015-y [DOI] [PubMed] [Google Scholar]
- Kaptchuk T. J. (2002). Acupuncture: theory, efficacy, and practice. Ann. Intern. Med. 136, 374–383. 10.7326/0003-4819-136-5-200203050-00010 [DOI] [PubMed] [Google Scholar]
- Kaptchuk T. J., Kelley J. M., Conboy L. A., Davis R. B., Kerr C. E., Jacobson E. E., et al. (2008). Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 336, 999–1003. 10.1136/bmj.39524.439618.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J., Kaptchuk T. J., Polich G., Kirsch I., Vangel M., Zyloney C., et al. (2009). Expectancy and treatment interactions: a dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage 45, 940–949. 10.1016/j.neuroimage.2008.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J., Loggia M. L., Zyloney C., Tu P., LaViolette P., Gollub R. L. (2010). Exploring the brain in pain: activations, deactivations and their relation. Pain 148, 257–267. 10.1016/j.pain.2009.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong J., Wang Z., Leiser J., Minicucci D., Edwards R., Kirsch I., et al. (2018). Enhancing treatment of osteoarthritis knee pain by boosting expectancy: a functional neuroimaging study. Neuroimage Clin. 18, 325–334. 10.1016/j.nicl.2018.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Yang J., Li C., Yuan A., Wu H., Wang A., et al. (2016). Cortical reorganization in patients recovered from Bell's Palsy: an orofacial and finger movements task-state fMRI study. Neural Plast. 2016:8231726. 10.1155/2016/8231726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M. H., Smyser C. D., Shimony J. S. (2013). Resting-state fMRI: a review of methods and clinical applications. AJNR Am. J. Neuroradiol. 34, 1866–1872. 10.3174/ajnr.A3263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung L. (2012). Neurophysiological basis of acupuncture-induced analgesia–an updated review. J. Acupunct. Meridian Stud. 5, 261–270. 10.1016/j.jams.2012.07.017 [DOI] [PubMed] [Google Scholar]
- Li C., Yang J., Park K., Wu H., Hu S., Zhang W., et al. (2014b). Prolonged repeated acupuncture stimulation induces habituation effects in pain-related brain areas: an FMRI study. PLoS ONE 9:e97502. 10.1371/journal.pone.0097502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Yang M., Zhao L., Zheng H., Li Y., Chang X., et al. (2014a). Acupuncture for chronic, stable angina pectoris and an investigation of the characteristics of acupoint specificity: study protocol for a multicenter randomized controlled trial. Trials 15:50. 10.1186/1745-6215-15-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Cheung R. T., Ma Q. Y., Yang E. S. (2003). Visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. Neuroreport 14, 669–673. 10.1097/00001756-200304150-00002 [DOI] [PubMed] [Google Scholar]
- Li G., Jack C. R., Yang E. S. (2006). An fMRI study of somatosensory-implicated acupuncture points in stable somatosensory stroke patients. J. Magn. Reson. Imaging 24, 1018–1024. 10.1002/jmri.20702 [DOI] [PubMed] [Google Scholar]
- Li G., Yang E. S. (2011). An fMRI study of acupuncture-induced brain activation of aphasia stroke patients. Complement. Ther. Med. 19, S49–S59. 10.1016/j.ctim.2010.11.004 [DOI] [PubMed] [Google Scholar]
- Li H., Liu H., Liu C., Shi G., Zhou W., Zhao C., et al. (2014c). Effect of “Deqi” during the study of needling “Wang's Jiaji” acupoints treating spasticity after stroke. Evid. Based Complement. Alternat. Med. 2014, 715351. 10.1155/2014/715351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Wang Z., Yu H., Pang R., Ni H., Li C. R., et al. (2020a). The long-term effects of acupuncture on hippocampal functional connectivity in aMCI with hippocampal atrophy: a randomized longitudinal fMRI study. Neural Plast. 2020, 1–9. 10.1155/2020/8814239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Zhang J. H., Yi T., Tang W. J., Wang S. W., Dong J. C. (2014d). Acupuncture treatment of chronic low back pain reverses an abnormal brain default mode network in correlation with clinical pain relief. Acupunct. Med. 32, 102–108. 10.1136/acupmed-2013-010423 [DOI] [PubMed] [Google Scholar]
- Li M. K., Li Y. J., Zhang G. F., Chen J. Q., Zhang J. P., Qi J., et al. (2015). Acupuncture for ischemic stroke: cerebellar activation may be a central mechanism following Deqi. Neural Regen. Res. 10, 1997–2003. 10.4103/1673-5374.172318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Chen J., Cheng J., Huang S., Hu Y., Wu Y., et al. (2018). Acupuncture modulates the cerebello-thalamo-cortical circuit and cognitive brain regions in patients of Parkinson's disease with tremor. Front. Aging Neurosci. 10:206. 10.3389/fnagi.2018.00206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Liu M., Lan L., Zeng F., Makris N., Liang Y., et al. (2016). Altered periaqueductal gray resting state functional connectivity in migraine and the modulation effect of treatment. Sci. Rep. UK 6:20298. 10.1038/srep20298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Zeng F., Yin T., Lan L., Makris N., Jorgenson K., et al. (2017). Acupuncture modulates the abnormal brainstem activity in migraine without aura patients. Neuroimage Clin. 15, 367–375. 10.1016/j.nicl.2017.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Zhou J., Cheng S., Lan L., Sun R., Liu M., et al. (2020b). Cerebral fractional amplitude of low-frequency fluctuations may predict headache intensity improvement following acupuncture treatment in migraine patients. J. Tradit. Chin. Med. 40, 1041–1051. 10.19852/j.cnki.jtcm.2020.06.016 [DOI] [PubMed] [Google Scholar]
- Liang F. R., Wu X. (2006). The developmental status and prospect of the science of acupuncture and moxibustion abroad. Zhongguo Zhen Jiu 26, 79–82. [PubMed] [Google Scholar]
- Liang P., Wang Z., Qian T., Li K. (2014). Acupuncture stimulation of Taichong (Liv3) and Hegu (LI4) modulates the default mode network activity in Alzheimer's disease. Am. J. Alzheimers Dis. Other Dementiasr 29, 739–748. 10.1177/1533317514536600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Xu J., Shan B., Li Y., Li L., Xue J., et al. (2012). Determining the precise cerebral response to acupuncture: an improved FMRI study. PLoS ONE 7:e49154. 10.1371/journal.pone.0049154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S. Y., Hsieh C. L., Wei T. S., Liu P. T., Chang Y. J., Li T. C. (2009). Acupuncture stimulation improves balance function in stroke patients: a single-blinded controlled, randomized study. Am. J. Chin. Med. 37, 483–494. 10.1142/S0192415X09006990 [DOI] [PubMed] [Google Scholar]
- Lu L., Zhang X. G., Zhong L. L., Chen Z. X., Li Y., Zheng G. Q., et al. (2016). Acupuncture for neurogenesis in experimental ischemic stroke: a systematic review and meta-analysis. Sci. Rep. 6:19521. 10.1038/srep19521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson H., Green G., Nevado A., Lythgoe M. F., Lewith G., Devlin R., et al. (2008). Brain imaging of acupuncture: comparing superficial with deep needling. Neurosci. Lett. 434, 144–149. 10.1016/j.neulet.2008.01.058 [DOI] [PubMed] [Google Scholar]
- Maeda Y., Kettner N., Lee J., Kim J., Cina S., Malatesta C., et al. (2013). Acupuncture-evoked response in somatosensory and prefrontal cortices predicts immediate pain reduction in carpal tunnel syndrome. Evid. Based Compl. Alt. 2013, 1–13. 10.1155/2013/795906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maoliang Q., Shanchen Z. (1985). Study of Acupuncture and Moxibustion. Shanghai, China: Shanghai Science and Techonlogy Publishing House. [Google Scholar]
- Mwansisya T. E., Hu A., Li Y., Chen X., Wu G., Huang X., et al. (2017). Task and resting-state fMRI studies in first-episode schizophrenia: a systematic review. Schizophr. Res. 189, 9–18. 10.1016/j.schres.2017.02.026 [DOI] [PubMed] [Google Scholar]
- Napadow V., Kettner N., Liu J., Li M., Kwong K. K., Vangel M., et al. (2007). Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome. Pain 130, 254–266. 10.1016/j.pain.2006.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ning Y., Li K., Fu C., Ren Y., Zhang Y., Liu H., et al. (2017). Enhanced functional connectivity between the bilateral primary motor cortices after acupuncture at Yanglingquan (GB34) in right-hemispheric subcortical stroke patients: a resting-state fMRI study. Front. Hum. Neurosci. 11:178. 10.3389/fnhum.2017.00178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ots T., Kandirian A., Szilagyi I., DiGiacomo S. M., Sandner-Kiesling A. (2020). The selection of dermatomes for sham (placebo) acupuncture points is relevant for the outcome of acupuncture studies: a systematic review of sham (placebo)-controlled randomized acupuncture trials. Acupunct. Med. 38, 211–226. 10.1177/0964528419889636 [DOI] [PubMed] [Google Scholar]
- Pariente J., White P., Frackowiak R. S., Lewith G. (2005). Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage 25, 1161–1167. 10.1016/j.neuroimage.2005.01.016 [DOI] [PubMed] [Google Scholar]
- Park J., White A., Stevinson C., Ernst E., James M. (2002). Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. Acupunct. Med. 20, 168–174. 10.1136/aim.20.4.168 [DOI] [PubMed] [Google Scholar]
- Qi J., Chen J., Huang Y., Lai X., Tang C., Yang J., et al. (2014). Acupuncture at Waiguan (SJ5) and sham points influences activation of functional brain areas of ischemic stroke patients: a functional magnetic resonance imaging study. Neural Regen. Res. 9, 293–300. 10.4103/1673-5374.128227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin W., Bai L., Dai J., Liu P., Dong M., Liu J., et al. (2011). The temporal-spatial encoding of acupuncture effects in the brain. Mol. Pain 7:19. 10.1186/1744-8069-7-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu L. Z., Zhao H. C., Shen H. X., Yan Y., Ma S. J., Wang K. Q. (2020). Electroacupuncture of both single- and multi-acupoints promotes recovery of gastrointestinal function in laparoscopic cholecystectomy patients. Zhen Ci Yan Jiu 45, 136–140. 10.13702/j.1000-0607.1904016 [DOI] [PubMed] [Google Scholar]
- Quah-Smith I., Suo C., Williams M. A., Sachdev P. S. (2013). The antidepressant effect of laser acupuncture: a comparison of the resting brain's default mode network in healthy and depressed subjects during functional magnetic resonance imaging. Med. Acupunct. 25, 124–133. 10.1089/acu.2012.0901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rong P. J., Zhao J. J., Gao J. H., Li X., Li S. Y., Ben H., et al. (2013). Progress of research on specificity of meridian acupoint efficacy. Chin. J. Integr. Med. 19, 889–893. 10.1007/s11655-013-1651-z [DOI] [PubMed] [Google Scholar]
- Sacco R. L., Kasner S. E., Broderick J. P., Caplan L. R., Connors J. J., Culebras A., et al. (2013). An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44, 2064–2089. 10.1161/STR.0b013e318296aeca [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg M., Lundeberg T., Lindberg L. G., Gerdle B. (2003). Effects of acupuncture on skin and muscle blood flow in healthy subjects. Eur. J. Appl. Physiol. 90, 114–119. 10.1007/s00421-003-0825-3 [DOI] [PubMed] [Google Scholar]
- Schaechter J. D., Connell B. D., Stason W. B., Kaptchuk T. J., Krebs D. E., Macklin E. A., et al. (2007). Correlated change in upper limb function and motor cortex activation after verum and sham acupuncture in patients with chronic stroke. J. Alter. Compl. Med. 13, 527–532. 10.1089/acm.2007.6316 [DOI] [PubMed] [Google Scholar]
- Scheffold B. E., Hsieh C., Litscher G. (2015). Neuroimaging and Neuromonitoring effects of electro and manual acupuncture on the central nervous system: a literature review and analysis. Evid. Based Compl. Alt. 2015, 1–29. 10.1155/2015/641742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi G. X., Li Q. Q., Liu C. Z., Zhu J., Wang L. P., Wang J., et al. (2014). Effect of acupuncture on Deqi traits and pain intensity in primary dysmenorrhea: analysis of data from a larger randomized controlled trial. BMC Complement. Altern. Med. 14:69. 10.1186/1472-6882-14-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi G. X., Yang X. M., Liu C. Z., Wang L. P. (2012). Factors contributing to therapeutic effects evaluated in acupuncture clinical trials. Trials 13:42. 10.1186/1745-6215-13-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Liu Z., Zhang S., Li Q., Guo S., Yang J., et al. (2015). Brain network response to acupuncture stimuli in experimental acute low back pain: an fMRI study. Evid. Based Compl. Alt. 2015, 1–13. 10.1155/2015/210120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuang L., Ranwei L., Jun G. (2020). Examples of application of contra-part needing. World J. Acupunct. Moxibustion 30, 307–310. 10.1016/j.wjam.2020.11.007 [DOI] [Google Scholar]
- Siedentopf C. M., Golaszewski S. M., Mottaghy F. M., Ruff C. C., Felber S., Schlager A. (2002). Functional magnetic resonance imaging detects activation of the visual association cortex during laser acupuncture of the foot in humans. Neurosci. Lett. 327, 53–56. 10.1016/S0304-3940(02)00383-X [DOI] [PubMed] [Google Scholar]
- Smith C. A., Armour M., Lee M. S., Wang L. Q., Hay P. J. (2018). Acupuncture for depression. Cochrane Database Syst. Rev. 3:CD004046. 10.1002/14651858.CD004046.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smitha K. A., Akhil R. K., Arun K. M., Rajesh P. G., Thomas B., Kapilamoorthy T. R., et al. (2017). Resting state fMRI: a review on methods in resting state connectivity analysis and resting state networks. Neuroradiol. J. 30, 305–317. 10.1177/1971400917697342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn W. S., Yoo K., Lee Y. B., Seo S. W., Na D. L., Jeong Y. (2015). Influence of ROI selection on resting state functional connectivity: an individualized approach for resting state fMRI analysis. Front. Neurosci. 9:280. 10.3389/fnins.2015.00280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streitberger K., Kleinhenz J. (1998). Introducing a placebo needle into acupuncture research. Lancet 352, 364–365. 10.1016/S0140-6736(97)10471-8 [DOI] [PubMed] [Google Scholar]
- Sun J., Zhu Y., Yang Y., Jin L., von Deneen K. M., Qin W., et al. (2013). What Is the de-qi-Related Pattern of BOLD Responses? A review of acupuncture studies in fMRI. Evid. Based Compl. Alt. Med. 2013:297839. 10.1155/2013/297839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun R., He Z., Ma P., Yin S., Yin T., Liu X., et al. (2020). The participation of basolateral amygdala in the efficacy of acupuncture with deqi treating for functional dyspepsia. Brain Imaging Behav. 15, 216–230. 10.1007/s11682-019-00249-7 [DOI] [PubMed] [Google Scholar]
- Takamura T., Hanakawa T. (2017). Clinical utility of resting-state functional connectivity magnetic resonance imaging for mood and cognitive disorders. J. Neural Transm. 124, 821–839. 10.1007/s00702-017-1710-2 [DOI] [PubMed] [Google Scholar]
- Tan T. T., Wang D., Huang J. K., Zhou X. M., Yuan X., Liang J. P., et al. (2017). Modulatory effects of acupuncture on brain networks in mild cognitive impairment patients. Neural Regen. Res. 12, 250–258. 10.4103/1673-5374.200808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treede R. D., Kenshalo D. R., Gracely R. H., Jones A. K. (1999). The cortical representation of pain. Pain 79, 105–111. 10.1016/S0304-3959(98)00184-5 [DOI] [PubMed] [Google Scholar]
- Tu Y., Ortiz A., Gollub R. L., Cao J., Gerber J., Lang C., et al. (2019). Multivariate resting-state functional connectivity predicts responses to real and sham acupuncture treatment in chronic low back pain. Neuroimage Clin. 23:101885. 10.1016/j.nicl.2019.101885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usichenko T. I., Wesolowski T., Lotze M. (2015). Verum and sham acupuncture exert distinct cerebral activation in pain processing areas: a crossover fMRI investigation in healthy volunteers. Brain Imaging Behav. 9, 236–244. 10.1007/s11682-014-9301-4 [DOI] [PubMed] [Google Scholar]
- Vase L., Wartolowska K. (2019). Pain, placebo, and test of treatment efficacy: a narrative review. Br. J. Anaesth. 123, e254–e262. 10.1016/j.bja.2019.01.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Deneen K. M., Qin W., Liu P., Dong M., Chen P., Xie H., et al. (2015). Connectivity study of the neuromechanism of acute acupuncture needling during fMRI in “Overweight” subjects. Evid. Based Compl. Alt. 2015, 1–12. 10.1155/2015/384389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Wang Z., Liu J., Chen J., Liu X., Nie G., et al. (2016a). Repeated acupuncture treatments modulate amygdala resting state functional connectivity of depressive patients. Neuroimage Clin. 12, 746–752. 10.1016/j.nicl.2016.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Li T., Ha L., Lv Z., Wang F., Wang Z., et al. (2020). Effectiveness and cerebral responses of multi-points acupuncture for primary insomnia: a preliminary randomized clinical trial and fMRI study. BMC Compl. Med. Ther. 20:254. 10.1186/s12906-020-02969-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Zheng Y., Qu S., Zhang J., Zhong Z., Zhang J., et al. (2016b). Cerebral targeting of acupuncture at combined acupoints in treating essential hypertension: an Rs-fMRI study and curative effect evidence. Evid. Based Compl. Alt. 2016, 1–12. 10.1155/2016/5392954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Liang P., Zhao Z., Han Y., Song H., Xu J., et al. (2014). Acupuncture modulates resting state hippocampal functional connectivity in Alzheimer disease. PLoS ONE 9:e91160. 10.1371/journal.pone.0091160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesolowski T., Lotze M., Domin M., Langner S., Lehmann C., Wendt M., et al. (2009). Acupuncture reveals no specific effect on primary auditory cortex: a functional magnetic resonance imaging study. Neuroreport 20, 116–120. 10.1097/WNR.0b013e328321004d [DOI] [PubMed] [Google Scholar]
- Wong L. W. D., Wang Y., Xue C. C., Wang L. P., Liang F. R., Zheng Z. (2015). Local and distant acupuncture points stimulation for chronic musculoskeletal pain: a systematic review on the comparative effects. Eur. J. Pain 19, 1232–1247. 10.1002/ejp.671 [DOI] [PubMed] [Google Scholar]
- Wu H., Kan H., Li C., Park K., Zhu Y., Mohamed A. Z., et al. (2015). Effect of acupuncture on functional connectivity of anterior cingulate cortex for Bell's palsy patients with different clinical duration. Evid. Based Compl. Alt. 2015, 1–7. 10.1155/2015/646872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P., Zhou Y., Liao C., Tang Y., Li Y., Qiu L., et al. (2018). Structural changes induced by acupuncture in the recovering brain after ischemic stroke. Evid. Based Compl. Alt. 2018, 1–8. 10.1155/2018/2958717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jin Z., Li K., Lu Z., Wong V., Han T., et al. (2008). Effect of acupuncture on the brain in children with spastic cerebral palsy using functional neuroimaging (fMRI). J. Child Neurol. 23, 1267–1274. 10.1177/0883073808318049 [DOI] [PubMed] [Google Scholar]
- Xiao L. Y., Wang X. R., Yang Y., Yang J. W., Cao Y., Ma S. M., et al. (2018). Applications of acupuncture therapy in modulating plasticity of central nervous system. Neuromodulation 21, 762–776. 10.1111/ner.12724 [DOI] [PubMed] [Google Scholar]
- Xiaoling L., Haitao J., Feng W., Lina C., Xiaohui L., Danna C., et al. (2020). Research Progress on fMRI Image of Needling GB34. Inform. Trad. Chin. Med. 37, 126–129. 10.19656/j.cnki.1002-2406.200028 [DOI] [Google Scholar]
- Xie Z., Cui F., Zou Y., Bai L. (2014). Acupuncture enhances effective connectivity between cerebellum and primary sensorimotor cortex in patients with stable recovery stroke. Evid. Based Compl. Alt. 2014, 1–9. 10.1155/2014/603909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing Y. (2016). Comparison of Curative Effect of Single Point and Multi-Point Application on Primary Dysmenorrhea. Beijing: Beijing University of Chinese Medicine. [Google Scholar]
- Yan C., Huo J., Wang X., Zhou P., Zhang Y., Li J., et al. (2020). Different degree centrality changes in the brain after acupuncture on contralateral or ipsilateral acupoint in patients with chronic shoulder pain: a resting-state fMRI study. Neural Plast. 2020, 1–11. 10.1155/2020/5701042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang A., Wu H. M., Tang J. L., Xu L., Yang M., Liu G. J. (2016). Acupuncture for stroke rehabilitation. Cochrane Database Syst. Rev. 2016:CD004131. 10.1002/14651858.CD004131.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo S., Choe I. H., van den Noort M., Bosch P., Jahng G. H., Rosen B., et al. (2014). Acupuncture on GB34 activates the precentral gyrus and prefrontal cortex in Parkinson's disease. BMC Compl. Altern. Med. 14:336. 10.1186/1472-6882-14-336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo S., Lim S., Choe I. H., Choi Y. G., Chung K. C., Jahng G. H., et al. (2012). Acupuncture stimulation on GB34 activates neural responses associated with Parkinson's disease. CNS Neurosci. Ther. 18, 781–790. 10.1111/j.1755-5949.2012.00363.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin T., He Z., Ma P., Qiu K., Zeng F. (2019). A narrative review of task design in acupuncture-fMRI researches. Chin. Arch. Trad. Chin. Med. 37, 1657–1660. 10.13193/j.issn.1673-7717.2019.07.029 [DOI] [Google Scholar]
- Yin X., Gou M., Xu J., Dong B., Yin P., Masquelin F., et al. (2017). Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med. 37, 193–200. 10.1016/j.sleep.2017.02.012 [DOI] [PubMed] [Google Scholar]
- Yoo S. S., Kerr C. E., Park M., Im D. M., Blinder R. A., Park H., et al. (2007). Neural activities in human somatosensory cortical areas evoked by acupuncture stimulation. Complement. Ther. Med. 15, 247–254. 10.1016/j.ctim.2007.01.010 [DOI] [PubMed] [Google Scholar]
- Yousaf T., Dervenoulas G., Politis M. (2018). Advances in MRI methodology. Int. Rev. Neurobiol. 141, 31–76. 10.1016/bs.irn.2018.08.008 [DOI] [PubMed] [Google Scholar]
- Yu S., Ortiz A., Gollub R. L., Wilson G., Gerber J., Park J., et al. (2020). Acupuncture treatment modulates the connectivity of key regions of the descending pain modulation and reward systems in patients with chronic low back pain. J. Clin. Med. 9:1719. 10.3390/jcm9061719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Cai X., Wang Y., Zheng Y., Qu S., Zhang Z., et al. (2019). Different brain activation after acupuncture at combined acupoints and single acupoint in hypertension patients: an Rs-fMRI study based on ReHo analysis. Evid. Based Compl. Alt. 2019, 1–10. 10.1155/2019/5262896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Lyu T., Yang Y., Wang Y., Zheng Y., Qu S., et al. (2020). Acupuncture at LR3 and KI3 shows a control effect on essential hypertension and targeted action on cerebral regions related to blood pressure regulation: a resting state functional magnetic resonance imaging study. Acupunct. Med. 39, 53–63. 10.1177/0964528420920282 [DOI] [PubMed] [Google Scholar]
- Zhang S., Wang X., Yan C., Hu S., Huo J., Wang Z., et al. (2018). Different mechanisms of contralateral- or ipsilateral-acupuncture to modulate the brain activity in patients with unilateral chronic shoulder pain: a pilot fMRI study. J. Pain Res. 11, 505–514. 10.2147/JPR.S152550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Li K., Ren Y., Cui F., Xie Z., Shin J., et al. (2014). Acupuncture modulates the functional connectivity of the default mode network in stroke patients. Evid. Based Compl. Alt. 2014, 1–7. 10.1155/2014/546097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J. G., Cao C. H., Liu C. Z., Han B. J., Zhang J., Li Z. G., et al. (2009). Effect of acupuncture treatment on spastic states of stroke patients. J. Neurol. Sci. 276, 143–147. 10.1016/j.jns.2008.09.018 [DOI] [PubMed] [Google Scholar]
- Zhao L., Liu J., Zhang F., Dong X., Peng Y., Qin W., et al. (2014). Effects of long-term acupuncture treatment on resting-state brain activity in migraine patients: a randomized controlled trial on active acupoints and inactive acupoints. PLoS ONE 9:e99538. 10.1371/journal.pone.0099538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao M. Y., Zhang P., Li J., Wang L. P., Zhou W., Wang Y. X., et al. (2017). Influence of de qi on the immediate analgesic effect of SP6 acupuncture in patients with primary dysmenorrhoea and cold and dampness stagnation: a multicentre randomised controlled trial. Acupunct. Med. 35, 332–338. 10.1136/acupmed-2016-011228 [DOI] [PubMed] [Google Scholar]
- Zheng Y., Zhang J., Wang Y., Wang Y., Lan Y., Qu S., et al. (2016). Acupuncture decreases blood pressure related to hypothalamus functional connectivity with frontal lobe, cerebellum, and insula: a study of instantaneous and short-term acupuncture treatment in essential hypertension. Evid. Based Compl. Alt. 2016, 1–10. 10.1155/2016/6908710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S., Zeng F., Liu J., Zheng H., Huang W., Liu T., et al. (2013). Influence of acupuncture stimulation on cerebral network in functional diarrhea. Evid. Based Compl. Alt. 2013, 1–9. 10.1155/2013/975769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou W., Benharash P. (2014). Significance of “Deqi” response in acupuncture treatment: myth or reality. J. Acupunct. Meridian Stud. 7, 186–189. 10.1016/j.jams.2014.02.008 [DOI] [PubMed] [Google Scholar]
- Zhu Y., Wu Z., Ma X., Liu H., Bao C., Yang L., et al. (2014). Brain regions involved in moxibustion-induced analgesia in irritable bowel syndrome with diarrhea: a functional magnetic resonance imaging study. BMC Complement. Altern. Med. 14:500. 10.1186/1472-6882-14-500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang Y., Xing J. J., Li J., Zeng B. Y., Liang F. R. (2013). History of acupuncture research. Int. Rev. Neurobiol. 111, 1–23. 10.1016/B978-0-12-411545-3.00001-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.