Abstract
College students have experienced significant disruptions related to COVID-19, and limited international data suggest they may be at elevated risk for mental health symptom increases related to COVID. Given their potentially elevated risk, our aim was to evaluate differences from pre-college closures to post-closure in mental health symptoms, alcohol, and cannabis use. Participants (N = 4749) were from seven U.S. public universities/colleges. They were 70.1 % female and 48.5 % white, non-Hispanic/Latino, with 48.1 % in their first college/university year. 30-day retrospective assessments of alcohol and cannabis use, and past 2-week retrospective assessments of anxiety, depression, anger, and insomnia were captured at the time of the survey. We examined differences between those providing data pre- and post-university closure via linear and negative binomial regressions. Alcohol and cannabis use days were 13 % and 24 % higher, respectively, from pre-to post-university closure; also, prevalence of any 30-day alcohol use and alcohol use consequences were both higher in the post-closure sample (odds ratios = 1.34 and 1.31, respectively). In contrast, days of binge alcohol use were 4 % lower in the post-closing sample. Depressive symptoms and anger were both modestly higher in post-closing participants (d < 0.1), with no differences in anxiety symptoms or insomnia. The modest differences in substance use and mental health from pre-closure through two months post-college closure suggest unexpected resilience in a large and diverse sample of students. College health providers will need to identify those students experiencing the greatest increases in mental health symptoms and substance use, using innovative outreach and treatment.
Keywords: COVID-19, College student, Depressive symptoms, Anxiety, Substance use
1. Introduction
The novel coronavirus, SARS-Cov-2 or COVID-19, is responsible for a pandemic on a scale not experienced since the 1918-20 H1N1 influenza pandemic. The highly infectious nature of the COVID-19 virus, its rapid spread throughout the world, and the significant mortality associated with it have greatly changed many peoples’ lives (Galea et al., 2020). Often, individuals are encouraged to limit transmission by restricting time out of the home to necessary activities, such as obtaining food or medical care, working, and exercise, depending on the locality (Weible et al., 2020). This policy of limiting contact with others is often termed “social distancing” (U.S. Centers for Disease Control and Prevention, 2020), though some prefer “physical distancing” to encourage ongoing social interaction (Galea et al., 2020).
Evidence from across the population in China, which was first impacted by COVID-19, suggests that levels of anxiety, depressive, and post-traumatic stress symptoms were higher than expected after the outbreak of COVID-19, with poorer sleep quality as well (Ahmed et al., 2020; Liang et al., 2020). Also, this evidence suggests that young adults, 21–30 years, may be most affected (Ahmed et al., 2020; Liang et al., 2020). Xiong et al. (2020) reviewed the literature on mental health symptoms from eight countries after the COVID-19 outbreak and found high rates of anxiety, depressive, and post-traumatic stress symptoms, with elevations in stress and psychological distress as well; those 40 years and younger and who were students were more affected than older age groups and non-students (Xiong et al., 2020). Evidence also suggests that substance use has increased, with the best evidence for increased alcohol use (Lechner et al., 2020; Neill et al., 2020; Pollard et al., 2020), though increases are not always found (e.g., Lopez-Bueno et al., 2020) and vary around the strictness and timing of COVID-related lockdowns (Grigoletto et al., 2020). These inconsistencies may also result from the population studied and levels of preexisting use, with greater increases in alcohol use among adults with higher pre-existing levels of alcohol use (Neill et al., 2020). Cannabis use changes related to COVID-19 are virtually unstudied, with only one study finding decreased use prevalence but increased use frequency among Canadian adolescents (Dumas et al., 2020).
The effects of COVID-19 are largely unstudied in college students, but they are already a group at elevated risk for substance use and mental health symptoms (Meredith et al., 2019), Young adults, 18–25 years of age, have the highest cannabis, illicit drug, and prescription drug misuse rates of any cohort, with alcohol use prevalence rates that only slightly trail those of adults aged 26–39 years (Substance Abuse and Mental Health Services Administration, 2019). Among young adults, college students have higher rates of problematic alcohol use than non-college students (Carter et al., 2010), with increasing rates of cannabis use and alcohol-cannabis co-use (McCabe et al., 2021). The typical college years coincide with the peak age period for incidence of many mental health conditions (de Girolamo et al., 2012), with high rates of depressive disorders, anxiety disorders (Meredith et al., 2019), and poor sleep (Taylor et al., 2011). Significant substance use and mental health symptoms are each linked to poorer academic performance, college dropout, and other poor outcomes (Arria et al., 2013; Auerbach et al., 2016), yet the vast majority of affected students do not receive treatment, likely due to inadequate campus resources (Auerbach et al., 2016, 2018).
College students have experienced many significant COVID-related stressors, including the transition to distance learning, unstable housing situations and/or unexpected moves back to the parental home, cancelled or delayed graduation ceremonies, and disrupted access to campus-based mental health treatment (Sahu, 2020). Self-report of changes in mental health symptoms suggest increases in stress and mood disorder symptoms (Charles et al., 2021; Son et al., 2020), but these are limited by smaller samples. Studies of alcohol use in United States (U.S.) college students have produced conflicting results with reference to changes related to COVID. On the one hand, two studies suggested increases in alcohol use (Charles et al., 2021; Lechner et al., 2020), while three studies found decreases in alcohol use following university closures (Jaffe et al., 2021; Ryerson et al., 2021; White et al., 2020). A sixth found a complex pattern of changes, with increases in frequency of use that were counteracted by declines in quantity of use and binge drinking, all of which was moderated by pre-COVID use patterns (Jackson et al., 2021).
While college students are an important population in which to examine changes in mental health and substance use related to COVID-19, the findings are limited by conflicting data on alcohol use changes. Also, studies to date have not assessed cannabis use in U.S. college students. Given this limited evidence on college student mental health and substance use related to university closures, outstanding questions remain about cannabis use changes and the degree of change and direction of mental health and alcohol use changes.
To address these outstanding questions, we used data from the U.S. college-based Stimulant Norms and Prevalence (SNAP) study. This cross-sectional study collected data from college students on mental health symptoms, alcohol, and cannabis use from September 2019 to May 2020, allowing for examination of differences in psychopathology symptoms from before to after outbreaks of COVID-19 in the students’ communities. Our primary aim was to examine differences related to university COVID-19 closure announcements (CCAs) in mental health and substance use in U.S. college students.
2. Materials and Methods
College students (N = 4749) completed an hour-long online survey at seven universities across six U.S. states (Colorado, New Mexico, New York, Texas, Virginia, and Wyoming), with COVID-19 closure announcements (CCAs) occurring between March 11th and 19th. After providing informed consent that followed a complete written explanation of the procedures, participants completed sociodemographic, mental health, and substance use measures. This study used a single-site IRB model, with procedures approved by the University of Wyoming IRB. All procedures were carried out in accordance with the latest version of the Declaration of Helsinki.
2.1. Measures
Demographics included age (ordinal), sex at birth (male/female), race/ethnicity (race: American Indian/Alaska Native, Asian, Black/African-American, Native Hawaiian/Pacific Islander, White, and Other; ethnicity: Hispanic/Latino; participants chose as many as applied), socioeconomic status (SES) while growing up (poor, working class, middle class, upper middle class, wealthy), classification in school (first-year, sophomore, junior, senior), and current grade point average.
Alcohol measures included lifetime alcohol use, and any past 30-day alcohol use among those with lifetime use. Quantity and days of 30-day alcohol use was assessed using a modified version of the Daily Drinking Questionnaire (DDQ; Collins et al., 1985). The modified DDQ and similar measures have been used in past research among college students (Bravo et al., 2020), with visual guidelines defining a standard drink to increase reliability and validity. 30-day binge alcohol use was also captured, defined as four or five alcoholic drinks in a period of 2 h or less for males and females, respectively. As with alcohol use, those who reported lifetime cannabis use also reported frequency of 30-day cannabis use via the Marijuana Use Grid (MUG), patterned on the DDQ (Collins et al., 1985).
For both 30-day alcohol and 30-day cannabis use, alcohol use consequences and cannabis use consequences were captured. Alcohol use consequences were captured via the Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ), a questionnaire assessing 24 dichotomous (yes/no) consequences; it is a valid, reliable measure in young adults (Kahler et al., 2005). Cannabis use consequences were captured via the Brief Marijuana Consequences Questionnaire (B-MACQ), a valid measure of cannabis use consequences in young adults (Bravo et al., 2019, Simons et al., 2012). The B-MACQ measures 21 cannabis use consequences dichotomously, similar to the B-YAACQ.
DSM-5 Psychiatric Symptoms were assessed via the DSM-5 Level 1 Cross-Cutting Symptom Measure (American Psychiatric Association, 2013), a 23-item screener for the past 14 days. Answers are on a five-point Likert-type scale, from zero (None/“none at all”) to four (Severe/“nearly every day”). Assessed domains include depressive symptoms (two items: anhedonia and down mood), anxiety symptoms (three items: nervousness/worry/anxiety, panic, and avoidance of anxiety-inducing situations), sleep quality (single-item), and anger (single-item). Prior research suggests that the DSM-5 Cross-Cutting Symptom Measure is a reliable and valid assessment of psychopathology in college students (Bravo et al., 2018).
2.2. Participants
The mean age of participants was 19.9 years (SD = 3.5), and 62.2 % provided responses before their university's COVID-19 closure announcements (CCAs), while 37.8 % provided responses after their university's CCA. Participants who completed their survey prior to the university's CCA were included in the pre-CCA sample, while those who completed it at any point after the CCA were in the post-CCA sample, resulting in two different, independent samples. We also performed sensitivity analyses that excluded all participants providing data within 30 days of their university's CCA, to examine potential confounding of data on days before and after the CCA. Characteristics of participants in the pre-CCA versus post-CCA samples are included in Table 1 . We evaluated differences in demographics pre- and post-CCA via X2 tests, with magnitude of differences evaluated by Cramer's V. Based on our data structure, Cramer's V values of 0.1, 0.3, and 0.5 correspond to small, medium, and large values, respectively (Cohen, 1988). While a number of demographic variables showed statistically significant differences pre- and post-CCA, the effect size of these differences was small in all cases. Among participants, 19.6 % of participants provided responses within 30 days of the CCA at their University. Participant characteristics of the total analytic sample by university are captured in Table 2 .
Table 1.
Sample characteristics by COVID cancellation announcement status.
| Characteristic | Pre-CCA | Post-CCA | Χ2 | Cramer's V |
|---|---|---|---|---|
| Female Sex | 72.6 % | 68.0 % | 11.1** | 0.05 |
| Race/Ethnicity | 34.5** | 0.09 | ||
| White | 50.5 % | 45.3 % | ||
| Black | 11.5 % | 16.4 % | ||
| Hispanic/Latinx | 6.5 % | 5.9 % | ||
| Asian | 6.8 % | 7.0 % | ||
| Native Hawaiian or Pacific Islander | 0.0 % | 0.2 % | ||
| American Indian or Alaska Native | 0.6 % | 0.3 % | ||
| Other | 1.0 % | 0.8 % | ||
| Multi-racial | 23.0 % | 24.1 % | ||
| Socioeconomic status | 5.1 | 0.03 | ||
| Poor | 4.8 % | 4.4 % | ||
| Working class | 19.7 % | 21.3 % | ||
| Middle Class | 45.8 % | 46.8 % | ||
| Upper middle class | 27.0 % | 24.5 % | ||
| Wealthy | 2.7 % | 3.0 % | ||
| Classification in School | 11.4** | 0.05 | ||
| First year (Freshman) | 48.1 % | 48.0 % | ||
| Second year (Sophomore) | 25.9 % | 23.8 % | ||
| Third year (Junior) | 14.9 % | 18.3 % | ||
| Fourth year and above (Senior) | 11.15 % | 10.0 % | ||
| Grade Point Average (GPA) | 70.9** | 0.12 | ||
| below 2.0 | 2.4 % | 3.9 % | ||
| 2.0–2.99 | 22.4 % | 32.1 % | ||
| 3.00–3.49 | 38.3 % | 34.4 % | ||
| 3.50 and greater | 36.9 % | 29.6 % | ||
| 30-day Substance Abstinence | ||||
| Alcohol | 34.0 % | 34.4 % | ||
| Cannabis | 70.4 % | 68.0 % |
CCA = COVID-19 closure announcement (for the participant's university).
Note: *p < .05, **p < .01.
Table 2.
Sample characteristics.
| Characteristic | % or Mean (SD) |
|---|---|
| Female Sex | 70.1 % |
| Race/Ethnicity | |
| White | 48.5 % |
| Black | 13.4 % |
| Hispanic/Latinx | 6.3 % |
| Asian | 6.9 % |
| Native Hawaiian or Pacific Islander | 0.1 % |
| American Indian or Alaska Native | 0.5 % |
| Other | 0.9 % |
| Multi-racial | 23.4 % |
| Socioeconomic status | |
| Poor | 4.7 % |
| Working class | 20.3 % |
| Middle Class | 46.2 % |
| Upper middle class | 26.0 % |
| Wealthy | 2.8 % |
| Classification in School | |
| First year (Freshman) | 48.1 % |
| Second year (Sophomore) | 25.1 % |
| Third year (Junior) | 16.2 % |
| Fourth year and above (Senior) | 10.7 % |
| Grade Point Average (GPA) | |
| below 2.0 | 3.0 % |
| 2.0–2.99 | 26.0 % |
| 3.00–3.49 | 36.8 % |
| 3.50 and greater | 34.2 % |
| University/College (Site) | |
| Texas State University | 19.2 % |
| Old Dominion University | 18.2 % |
| College of William & Mary | 13.8 % |
| University of Wyoming | 13.3 % |
| State University of New York at Albany | 12.7 % |
| Colorado State University | 12.1 % |
| University of New Mexico | 10.6 % |
| Substance Use | |
| Days of Alcohol Use (past 30) | 3.74 (5.18) |
| Days of Binge Alcohol Use (past 30) | 1.92 (3.45) |
| Alcohol Use Consequences | 3.57 (5.00) |
| Days of Cannabis Use (past 30) | 3.55 (8.01) |
| Cannabis Use Consequences | 1.30 (3.20) |
| Psychopathology | |
| Depression | 2.62 (2.32) |
| Anxiety | 3.81 (3.41) |
| Sleep Interference | 1.12 (1.27) |
| Anger | 1.26 (1.19) |
2.3. Analytic plan
To evaluate differences in average symptom levels before and after COVID-19 closure announcements (CCAs), zero-inflated negative binomial (ZINB) regression was used for count outcomes (pertaining to substance use). Thus, the main independent variable in all analyses was pre- or post-CCA survey completion status. Substance use outcomes are likely to be characterized by long-term abstinence in some participants, while other participants are not abstinent. The ZINB models account for both kinds of substance patterns simultaneously via a 2-part model, with a binary part of the model seeking to identify complete abstinence (or zero values for use), and a second count part of the model accounting for substance use rates via negative binomial regression. This approach to modeling accounts for dual processes that can occur during substance use, where some participants might have zero use during a period of time but still potentially engage in use at other times (which is modeled by the count model part of ZINB models), while some participants might never engage in any substance use (which reflects a different underlying process and is addressed by the binomial part of ZINB models). Of note, the binary part of the model addressing binge drinking prevented model convergence, likely as a consequence of limited variance explained. Linear regression (LR) was used for continuous outcomes (pertaining to psychopathology).
In addition to hypothesis tests, we evaluated effect sizes in terms of incidence risk ratios (IRRs) for the count process part of ZINB models testing for days of use, odds ratios (ORs) for the binomial process part of ZINB models testing for any 30-day use, and raw unit differences in LR (reflected by unstandardized beta values). To further support model choice, we ran overdispersion tests following approaches suggested by Venables and Ripley (2013) and we tested for zero-inflation and improvements in model fit compared to simpler models using Vuong non-nested model tests (Vuong, 1989). Both overdispersion and zero-inflation were consistently detected across models.
We also evaluated moderation by SES, sex at birth, and race/ethnicity through statistical interactions with the COVID cancellation announcement (CCA). Moderators were dummy coded with reference groups of “poor” for SES, “male” for sex, and “White, non-Hispanic/Latino” for race/ethnicity. Per Benjamini and Hochberg (1995), all moderator hypothesis tests were adjusted using false discovery rate procedures (FDR), such that each single predictor/outcome was considered as a separate family of hypotheses for evaluation (e.g., the use of SES as a moderator of class membership resulted in 52 hypothesis tests across all dependent variables, so the FDR procedure corrected for false discoveries based on 52 hypothesis tests for SES).
To account for site-based clustering of participants, university/site served as a fixed effects covariate (McNeish and Kelley, 2019). Missing data were very limited (<1 %) except for binge drinking (22.6 %). To address missing data, multiple imputation was employed using predictive mean matching and the fully conditional specification (Liu and De, 2015). All analyzed variables (including site) were included in the imputation model, and 40 imputations were employed (following recommendations by Graham, 2009). The R statistical software language version 4.0.2 (R Core Team, 2020. https://www.R-project.org/) was used for all analyses, including the “mice” package for multiple imputation (Buuren and Groothuis-Oudshoorn, 2010) and the “pscl” package for ZINB regression (https://github.com/atahk/pscl/; Jackman, 2020).
3. Results
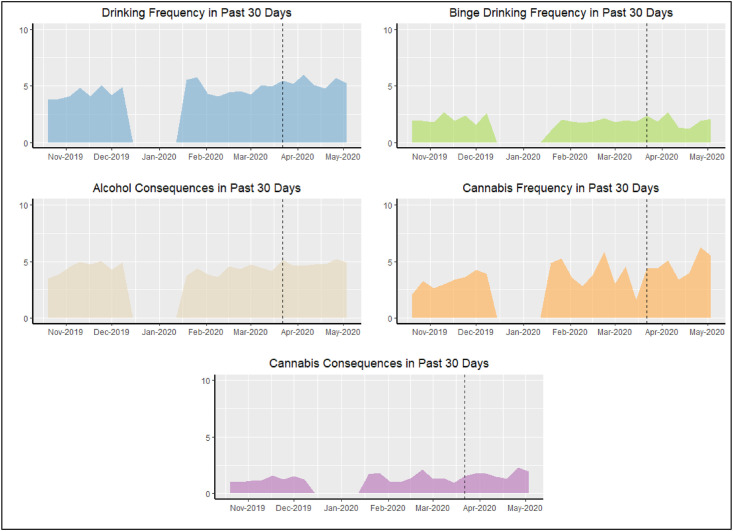
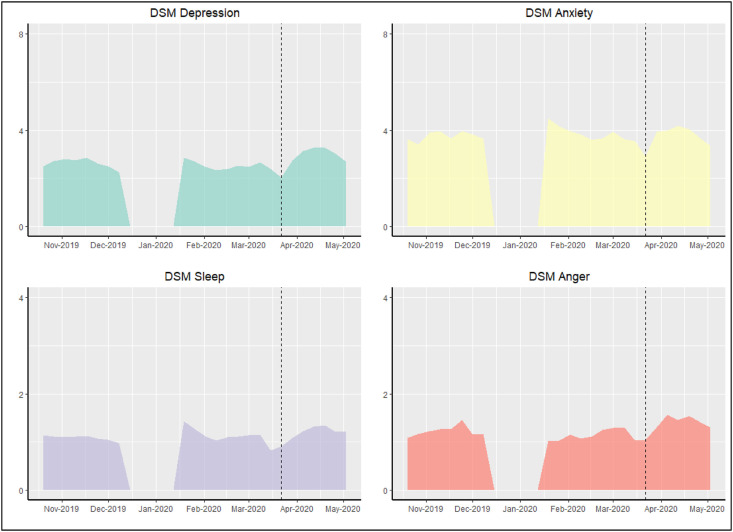
Observed substance use and psychopathology patterns appear in Fig. 1, Fig. 2 , respectively, with Table 3 capturing beta values, odds ratios (ORs), or incidence rate ratios (IRRs) that compared post- COVID closure announcement (CCAs; from March 11th to 19th, depending on university) participants to the reference group of pre-CCA participants. For substance use, survey completion after CCAs was associated with significant differences in days of alcohol use (b = 0.15, p < .001, IRR = 1.17), any 30-day alcohol use (vs. abstinence; b = 0.29, p = .03, OR = 1.34), days of cannabis use (b = 0.18, p = .02, IRR = 1.20), number of alcohol-related consequences (b = 0.09, p = .02, IRR = 1.09), and experiencing any alcohol consequences (b = 0.27, p < .001, OR = 1.31). For all of these outcomes, the post-CCA level of use was larger than the pre-CCA level of use.
Fig. 1.
Substance use reports by date. The dashed line denotes the date of the latest university COVID closure announcement (CCA): March 19th.
Fig. 2.
Psychopathology reports by date. The dashed line denotes the date of the latest university COVID closure announcement (CCA): March 19th.
Table 3.
Post-COVID closure announcement (CCA) participant regression main effects, versus Pre-CCA participants, with sensitivity analysis.
| Complete Sample | Sample After Removing All Participants Within 30 Days of CCA | |||
|---|---|---|---|---|
| ZINB - Binomial (modeling abstinence) | Betaa | Odds Ratio | Betaa | Odds Ratio |
| Drinking Frequency | 0.29* | 1.34 | 0.52** | 1.67 |
| Binge Drinkinga | ||||
| Alcohol Consequences | 0.27** | 1.31 | 0.45** | 1.58 |
| Cannabis Frequency | 0.03 | 1.03 | 0.08 | 1.09 |
| Cannabis Consequences | −0.06 | 0.94 | −0.05 | 0.96 |
| ZINB - Negative Binomial (modeling rate of use) | Betaa | Incidence Risk Ratio | Betaa | Incidence Risk Ratio |
| Drinking Frequency | 0.15** | 1.17 | 0.14* | 1.15 |
| Binge Drinking | −0.15* | 0.86 | −0.38** | 0.68 |
| Alcohol Consequences | 0.09* | 1.09 | 0.13* | 1.14 |
| Cannabis Frequency | 0.18* | 1.20 | 0.24* | 1.28 |
| Cannabis Consequences | 0.08 | 1.08 | 0.10 | 1.11 |
| Linear Regression (modeling mental health outcomes) | Betaa,b | Betaa,b | ||
| DSM Depression | 0.18* | 0.35** | ||
| DSM Anxiety | −0.20 | −0.16 | ||
| DSM Sleep | 0.02 | 0.14** | ||
| DSM Anger | 0.13** | 0.22** |
Note: *p < .05, **p < .01; ZINB = Zero-inflated negative binomial.
Model convergence was not achieved for the binomial part of ZINB models for binge drinking.
Beta values compare substance use outcomes in post-COVID closure announcement (CCA) participants to the reference group of pre-CCA participants.
Unstandardized betas in linear regression reflect effect sizes via raw unit differences between groups assessed pre- and post-CCA, with the pre-CCA group as the reference.
Number of days of alcohol use was 13 % larger, from 3.57 (pre-CCA) to 4.02 (post-CCA), and the odds ratio for any alcohol use was 34 % larger post-CCA, versus pre-CCA. The difference in alcohol use odds corresponds to a small effect size (d = 0.16), however, per Chinn (2000). The count of alcohol use consequences was 9 % larger and the odds of any alcohol use consequences was 31 % larger from pre-to post-CCA. As with any alcohol use, the effect size for any alcohol use consequences was small (d = 0.15). Finally, days of cannabis use differed by 24 %, from 3.26 (pre-CCA) to 4.04 (post-CCA), but any (i.e., dichotomous) cannabis use and consequences were all unrelated to CCAs.
In contrast to most alcohol use results, binge drinking frequency was lower in those who responded after the CCA (b = −0.15, p = .02, IRR = 0.86) by 4 %: from 2.00 to 1.92 in the past 30 days. All other main effects for substance use were non-significant, including 30-day cannabis use (b = 0.03, p = .71, OR = 1.03), and cannabis-related consequences in count form (b = 0.08, p = .25, IRR = 1.08) or dichotomous form (b = −0.06, p = .45, OR = 0.94).
With regard to psychopathology, respondents completing the survey after their university's CCA had higher levels of depressive symptoms (b = 0.18, p = .01) and anger (b = 0.13, p < .001), with no differences in anxiety (b = −0.20, p = .06) or sleep interference (b = 0.02, p = .55) versus those who completed the survey prior to the CCA. For depressive symptoms and anger, the effect sizes were very small (ds < 0.1), with an increase of 0.19 on the five-point Likert scale for depressive symptoms (2.60 versus 2.79) and 0.11 for anger (1.22 versus 1.33). Anxiety symptoms evidenced a non-significant difference (3.89–3.68), and sleep interference values were nearly identical pre-to post-CCA (1.12–1.14).
After applying the FDR correction, no significant moderation was observed based on SES, birth sex, or race/ethnicity. Of note, model overparameterization precluded estimation of several analyses, including the binomial part of ZINB models predicting binge alcohol use (based on main effect prediction from CCAs and for moderation by SES and race/ethnicity) and cannabis consequences (for moderation by race/ethnicity). A hypothesis test for the moderator effect of Native Hawaiian/Pacific Islander related to MACQ was precluded by sparse data, though the parameter estimate was small (b < 0.001, IRR = 1.00).
Roughly 20 % of participants provided data within 30 days of their respective university's CCA, meaning that their data included both pre- and post-CCA days. In order to assess potential confounding of outcomes from participants with both pre- and post-CCA data, we excluded all of these participants in sensitivity analyses. As with data from the entire sample, missing data were then imputed (see Methods for more) only in those with data that did not include both pre- and post-CCA days. Per Table 3, only one outcome significantly changed: sleep interference from the DSM-5 Cross-Cutting measure. In the entire sample, this outcome was non-significant, but after removing participants with data that straddled a CCA, sleep problems were significantly greater in the post-CCA sample. This effect was very small (b = 0.14). For other outcomes, changes were only in magnitude of betas and ORs or IRRs, with small changes in magnitude. To illustrate, the largest effect size change (0.12) was for 30-day alcohol use odds, from an OR of 1.34 in the entire sample to 1.67 in the restricted sample. Together, these findings suggest limited changes when removing participants with both pre- and post-CCA data.
4. Discussion
These results provided evidence of generally greater levels of substance use and psychopathology in students completing the survey after their university's COVID closure announcement (CCA), though changes were generally modest and not seen for all outcomes. On the one hand, depressive symptoms and anger were greater in students who completed the survey after their CCA, though anxiety symptoms did not vary. In the model with all participants, sleep interference was non-significant, though in the model without participants whose data straddled their university's CCA, post-CCA participants had significantly greater sleep interference. This was a very small effect, though. Furthermore, most alcohol and cannabis use indicators were higher in those taking the survey post-CCA, yet binge drinking days were lower in those assessed after closings. None of the pre-to post-CCA differences in substance use or mental health symptoms were moderated by sex at birth, race/ethnicity, or SES.
Together, these findings suggest a picture of modestly higher levels of substance use, depressive symptoms, and anger among U.S. college students from pre-through a two-month period post-university closure. These results, however, do not correspond with research in other countries about COVID-related mental health among young adults and students. That research suggested much larger differences in mental health symptoms than found here (Xiong et al., 2020). One reason could be that our methodology compared two separate groups of college students, while the predominant measure in other studies has been for the participant to self-report change in symptoms after the spread of COVID-19 in their community, which is likely to suffer from retrospective bias. Alternatively, U.S. college students may perceive lesser threat from COVID-19 than non-U.S. samples. For alcohol use, our results add to the conflicting literature in U.S. college students by suggesting increases in frequency of use and level of consequences but decreases in binge use. Our findings are most similar to those of Jackson et al. (2021), as they found increases in frequency but decreases in indices of heavy use.
Clinically, these results suggest that universities and care providers for college students need to carefully screen for alcohol and cannabis use and for depressive symptoms and problematic anger in students. Sleep problems also may warrant examination. While the overall level of pre-to post-CCA difference in outcomes was modest, that does not mean that a specific individual's change related to university closings will necessarily be modest. Data from across Australian adults found the greatest increases in alcohol use among those with greater pre-COVID levels of use (Neill et al., 2020), and providers should be aware of the possibility for greater increases among those with pre-existing substance use and mental health problems. Furthermore, these data only examine the first two months post-CCA, and substance use and mental health symptoms are likely to continue changing in college students. Ensuring continuity of care to those already enrolled in treatment could be crucial in preventing significant problems in the most vulnerable students. In addition, universities may need to increase availability of substance use and mental health treatment services, but given that most college students who need treatment do not receive it while in college (Auerbach et al., 2016, 2018), college health professionals may need to consider innovative screening, outreach, and broad use of self-help materials and/or technology-aided treatment solutions to reach a broad and dispersed population of students (e.g., Kählke et al., 2019).
4.1. Limitations
First, participants are younger, four-year undergraduate students at public universities and are not a representative sample of all college students. These include older students, private school students, and those attending two-year schools. Second, these results cannot be generalized to non-college young adults, who differ in significant ways from young adults in college. Another limitation comes from the measures employed: while they have strong psychometrics, they also were brief screening measures, and post-traumatic stress symptoms were not assessed. Also, the measures captured retrospective ratings of 30-day substance use and 14-day mental health symptoms. As such, students who completed the survey within 30 or 14 days of their university's CCA were reporting on both pre- and post-CCA experiences for substance use and/or psychopathology symptoms, respectively. Those who were in the pre-CCA sample were reporting on only pre-CCA dates. This means that the post-CCA ratings should be interpreted in light of the inclusion of limited pre-CCA data. With that said, we performed sensitivity analyses (Table 3) that suggested only one change in significance when participants were excluded if they had data including both pre- and post-CCA days.
Furthermore, these data are cross-sectional, which prevents tests of within-participant change and reduces the strength causal inference in the relationships of COVID-19/CCAs and mental health or substance use changes. Finally, the data are subject to both self-report and self-selection bias, given the nature of the data and that some eligible students opted to participate in other research studies for course credit. These weaknesses, however, were balanced by the large and diverse sample from seven universities/colleges across the U.S. the valid and reliable measures of alcohol use, cannabis use, and psychopathology, and the robust analytic plan.
5. Conclusions
In a broad sample of U.S. college students, days of alcohol and cannabis use, prevalence of alcohol use and alcohol use consequences, depressive symptoms, and anger were all significantly higher in participants who provided data in the two months post-university closing, versus pre-closing. Only binge drinking days were significantly lower in the post-CCA sample, and the groups did not differ on anxiety symptoms, with evidence of greater sleep interference in the post-CCA sample when participants with data that straddled the CCA were excluded. All of these pre-to post-CCA differences were relatively modest with small to moderate effect sizes for the substance use outcomes and small effect sizes for psychopathology. Given the large size of the U.S. college population, though, these modest effects can have large overall impacts. Universities should continue to consider innovative ways to screen for substance use and mental health symptoms and to initiate treatment, and those with pre-existing problems might have the greatest treatment needs.
CRediT authorship contribution statement
Ty S. Schepis: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Project administration, Funding acquisition. Alessandro S. De Nadai: Conceptualization, Methodology, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. Adrian J. Bravo: Conceptualization, Investigation, Data curation, Writing – review & editing, Funding acquisition. Alison Looby: Conceptualization, Investigation, Writing – review & editing. Margo C. Villarosa-Hurlocker: Conceptualization, Investigation, Writing – review & editing. Mitch Earleywine: Conceptualization, Investigation, Writing – review & editing.
Declaration of competing interest
None.
Acknowledgement
This work was supported by R01DA043691 from the National Institute on Drug Abuse (NIDA) and a summer research grant from the Office of the Provost of William and Mary University.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.07.040.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. The DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure – Adult. Available at: http://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM5_Level-1-Measure-Adult.pdf.
- Arria A.M., Caldeira K.M., Vincent K.B., Winick E.R., Baron R.A., O'Grady K.E. Discontinuous college enrollment: associations with substance use and mental health. Psychiatr. Serv. 2013;64(2):165–172. doi: 10.1176/appi.ps.201200106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach R.P., Alonso J., Axinn W.G., Cuijpers P., Ebert D.D., Green J.G., Hwang I., Kessler R.C., Liu H., Mortier P., Nock M.K., Pinder-Amaker S., Sampson N.A., Aguilar-Gaxiola S., Al-Hamzawi A., Andrade L.H., Benjet C., Caldas-de-Almeida J.M., Demyttenaere K., Florescu S., de Girolamo G., Gureje O., Haro J.M., Karam E.G., Kiejna A., Kovess-Masfety V., Lee S., McGrath J.J., O'Neill S., Pennell B.E., Scott K., Ten Have M., Torres Y., Zaslavsky A.M., Zarkov Z., Bruffaerts R. Mental disorders among college students in the world health organization world mental health surveys. Psychol. Med. 2016;46(14):2955–2970. doi: 10.1017/S0033291716001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach R.P., Mortier P., Bruffaerts R., Alonso J., Benjet C., Cuijpers P., Demyttenaere K., Ebert D.D., Green J.G., Hasking P., Murray E., Nock M.K., Pinder-Amaker S., Sampson N.A., Stein D.J., Vilagut G., Zaslavsky A.M., Kessler R.C., Collaborators W.W.-I. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018;127(7):623–638. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y., Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. Roy. Stat. Soc. B. 1995;57(1):289–300. [Google Scholar]
- Bravo A.J., Pearson M.R., Baumgardner S.F. The relationship between negative affect and alcohol and marijuana use outcomes among dual users. Subst. Use Misuse. 2020;55(4):658–665. doi: 10.1080/10826084.2019.1696820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo A.J., Pearson M.R., Pilatti A., Mezquita L., Cross-Cultural Addictions Study T. Negative marijuana-related consequences among college students in five countries: measurement invariance of the Brief Marijuana Consequences Questionnaire. Addiction. 2019;114(10):1854–1865. doi: 10.1111/add.14646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo A.J., Villarosa-Hurlocker M.C., Pearson M.R. College student mental health: an evaluation of the DSM-5 self-rated Level 1 cross-cutting symptom measure. Psychol. Assess. 2018;30(10):1382–1389. doi: 10.1037/pas0000628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buuren S.v., Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J. Stat. Software. 2010:1–68. [Google Scholar]
- Carter A.C., Brandon K.O., Goldman M.S. The college and noncollege experience: a review of the factors that influence drinking behavior in young adulthood. J. Stud. Alcohol Drugs. 2010;71(5):742–750. doi: 10.15288/jsad.2010.71.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles N.E., Strong S.J., Burns L.C., Bullerjahn M.R., Serafine K.M. Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatr. Res. 2021;296:113706. doi: 10.1016/j.psychres.2021.113706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat. Med. 2000;19(22):3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::aid-sim784>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Cohen J. second ed. Erlbaum; Hillsdale, NJ: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Collins R.L., Parks G.A., Marlatt G.A. Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. J. Consult. Clin. Psychol. 1985;53(2):189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- de Girolamo G., Dagani J., Purcell R., Cocchi A., McGorry P.D. Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiol. Psychiatr. Sci. 2012;21(1):47–57. doi: 10.1017/s2045796011000746. [DOI] [PubMed] [Google Scholar]
- Dumas T.M., Ellis W., Litt D.M. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J. Adolesc. Health. 2020;67(3):354–361. doi: 10.1016/j.jadohealth.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Graham J.W. Missing data analysis: making it work in the real world. Annu. Rev. Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Grigoletto V., Cognigni M., Occhipinti A.A., Abbracciavento G., Carrozzi M., Barbi E., Cozzi G. Rebound of severe alcoholic intoxications in adolescents and young adults after COVID-19 lockdown. J. Adolesc. Health. 2020;67(5):727–729. doi: 10.1016/j.jadohealth.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackman S. United States Studies Centre, University of Sydney; Sydney, New South Wales, Australia: 2020. Pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory. [Google Scholar]
- Jackson K.M., Merrill J.E., Stevens A.K., Hayes K.L., White H.R. Changes in alcohol use and drinking context due to the COVID-19 pandemic: a multimethod study of college student drinkers. Alcohol Clin. Exp. Res. 2021;45(4):752–764. doi: 10.1111/acer.14574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe A.E., Kumar S.A., Ramirez J.J., DiLillo D. Is the COVID-19 pandemic a high-risk period for college student alcohol use? A comparison of three spring semesters. Alcohol Clin. Exp. Res. 2021;45(4):854–863. doi: 10.1111/acer.14572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler C.W., Strong D.R., Read J.P. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcohol Clin. Exp. Res. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Kählke F., Berger T., Schulz A., Baumeister H., Berking M., Auerbach R.P., Bruffaerts R., Cuijpers P., Kessler R.C., Ebert D.D. Efficacy of an unguided internet-based self-help intervention for social anxiety disorder in university students: a randomized controlled trial. Int. J. Methods Psychiatr. Res. 2019;28(2) doi: 10.1002/mpr.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lechner W.V., Laurene K.R., Patel S., Anderson M., Grega C., Kenne D.R. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict. Behav. 2020;110:106527. doi: 10.1016/j.addbeh.2020.106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., De A. Multiple imputation by fully conditional specification for dealing with missing data in a large epidemiologic study. Int. J. Stat. Med. Res. 2015;4(3):287–295. doi: 10.6000/1929-6029.2015.04.03.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Bueno R., Calatayud J., Casana J., Casajus J.A., Smith L., Tully M.A., Andersen L.L., Lopez-Sanchez G.F. COVID-19 confinement and health risk behaviors in Spain. Front. Psychol. 2020;11:1426. doi: 10.3389/fpsyg.2020.01426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S.E., Arterberry B.J., Dickinson K., Evans-Polce R.J., Ford J.A., Ryan J., Schepis T.S. Changes in alcohol and marijuana abstinence, Co-use, and use disorders among US young adults: 2002-2018. JAMA Pediatrics. 2021;175(1):64–72. doi: 10.1001/jamapediatrics.2020.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeish D., Kelley K. Fixed effects models versus mixed effects models for clustered data: reviewing the approaches, disentangling the differences, and making recommendations. Psychol. Methods. 2019;24(1):20–35. doi: 10.1037/met0000182. [DOI] [PubMed] [Google Scholar]
- Meredith G.R., Rakow D.A., Eldermire E.R.B., Madsen C.G., Shelley S.P., Sachs N.A. Minimum time dose in nature to positively impact the mental health of college-aged students, and how to measure it: a scoping review. Front. Psychol. 2019;10:2942. doi: 10.3389/fpsyg.2019.02942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill E., Meyer D., Toh W.L., van Rheenen T.E., Phillipou A., Tan E.J., Rossell S.L. Alcohol use in Australia during the early days of the COVID-19 pandemic: initial results from the COLLATE project. Psychiatr. Clin. Neurosci. 2020;74(10):542–549. doi: 10.1111/pcn.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D., Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing.https://www.R-project.org/ [Google Scholar]
- Ryerson N.C., Wilson O.W.A., Pena A., Duffy M., Bopp M. What happens when the party moves home? The effect of the COVID-19 pandemic on U.S. college student alcohol consumption as a function of legal drinking status using longitudinal data. Transl Behav Med. 2021;11(3):772–774. doi: 10.1093/tbm/ibab006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahu P. Closure of universities due to coronavirus Disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4) doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons J.S., Dvorak R.D., Merrill J.E., Read J.P. Dimensions and severity of marijuana consequences: Development and validation of the Marijuana Consequences Questionnaire (MACQ) Addict. Beh. 2012;37:613–621. doi: 10.1016/j.addbeh.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on college students mental health in the US: an interview-survey study. J. Med. Internet Res. 2020;22(9):e2179. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2019. Results from the 2018 National Survey on Drug Use and Health: Detailed Tables. [Google Scholar]
- Taylor D.J., Gardner C.E., Bramoweth A.D., Williams J.M., Roane B.M., Grieser E.A., Tatum J.I. Insomnia and mental health in college students. Behav. Sleep Med. 2011;9(2):107–116. doi: 10.1080/15402002.2011.557992. [DOI] [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention Social distancing, quarantine, and isolation: keep your distance to slow the spread. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
- Venables W.N., Ripley B.D. Springer Science & Business Media; 2013. Modern Applied Statistics with S-PLUS. [Google Scholar]
- Vuong Q.H. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica: Journal of the Econometric Society. 1989:307–333. [Google Scholar]
- Weible C.M., Nohrstedt D., Cairney P., Carter D.P., Crow D.A., Durnová A.P., Heikkila T., Ingold K., McConnell A., Stone D. COVID-19 and the policy sciences: initial reactions and perspectives. Pol. Sci. 2020:1–17. doi: 10.1007/s11077-020-09381-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White H.R., Stevens A.K., Hayes K., Jackson K.M. Changes in alcohol consumption among college students due to COVID-19: effects of campus closure and residential change. J. Stud. Alcohol Drugs. 2020;81(6):725–730. doi: 10.15288/jsad.2020.81.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.