Abstract
Background
The incidence of severe (S-HTG) and very severe hypertriglyceridemia (VS-HTG) among Canadians is unknown. This study aimed to determine the incidence, characteristics, predictors and care patterns for individuals with VS-HTG.
Methods
Using linked administrative healthcare databases, a population-based cohort study of Ontario adults was conducted to determine incidence of new onset S-HTG (serum triglycerides (TG) > 10–20 mmol/L) and VS-HTG (TG > 20 mmol/L) between 2010 and 2015. Socio-demographic and clinical characteristics of those with VS-HTG were compared to those who had no measured TG value > 3 mmol/L. Univariable and multivariable logistic regression were used to determine predictors for VS-HTG. Healthcare patterns were evaluated for 2 years following first incidence of TG > 20 mmol/L.
Results
Incidence of S-HTG and VS-HTG in Ontario was 0.16 and 0.027% among 10,766,770 adults ≥18 years and 0.25 and 0.041% among 7,040,865 adults with at least one measured TG, respectively. Predictors of VS-HTG included younger age [odds ratios (OR) 0.64/decade, 95% confidence intervals (CI) 0.62–0.66], male sex (OR 3.83; 95% CI 3.5–4.1), diabetes (OR 5.38; 95% CI 4.93–5.88), hypertension (OR 1.69; 95% CI 1.54–1.86), chronic liver disease (OR 1.71; 95% CI 1.48–1.97), alcohol abuse (OR 2.47; 95% CI 1.90–3.19), obesity (OR 1.49; 95% CI 1.13–1.98), and chronic kidney disease (OR 1.39; 95% CI 1.19–1.63).
Conclusion
The 5-year incidence of S-HTG and VS-HTG in Canadian adults was 1 in 400 and 1 in 2500, respectively. Males, those with diabetes, obese individuals and those with alcohol abuse are at highest risk for VS-HTG and may benefit from increased surveillance.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12944-021-01517-6.
Keywords: Triglycerides, Pancreatitis, Fibrates, Secondary hypertriglyceridemia
Background
Triglyceride (TG) values > 20 mmol/L can have significant consequences. One of the most detrimental outcomes is pancreatitis, which often requires hospitalization or admission to intensive care, and associated mortality. Pancreatitis is linked with the presence of chylomicrons in the serum, which occurs when TG levels exceed 10 mmol/L, with risk rising sharply as levels exceed 20 mmol/L [1–5]. In clinical practice, very severe hypertriglyceridemia (VS-HTG), defined in this study as triglyceride (TG) levels that exceed 20 mmol/L, is captured through routine lipid testing and commonly misattributed to an exclusive genetic etiology. A minority of cases of VS-HTG (~ 1 in 1 million) arise from a primary TG disorder, typically caused by bi-allelic mutations in genes including lipoprotein lipase (LPL), apolipoprotein C-II (APOC2), apolipoprotein A-V (APOA5), lipase maturation factor 1 (LMF1) and glycosylphosphatidylinositol-anchored high density lipoprotein binding protein 1 (GPIHBP1) [6]. Most cases result from secondary causes, often in conjunction with inherited partial impairment in TG metabolism [7–11]. These cases may only manifest under conditions that increase TG production or impair clearance. Previous studies conducted elsewhere have suggested that secondary causes of VS-HTG, include obesity and metabolic syndrome, poorly controlled diabetes, nephrotic syndrome, severe hypothyroidism, oral estrogen or tamoxifen, glucocorticoids, beta blockers, retinoids and HIV antiretroviral regimens [3, 12, 13]. Irrespective of the underlying cause, VS-HTG is of clinical concern due to the risk of HTG-associated pancreatitis. Thus, it remains important to understand and manage the secondary risk factors associated with this condition [5].
While studies conducted in other regions, such as Norway and the United States, have suggested the prevalence of S-HTG to be between 0.13–0.4% [14, 15] and VS-HTG to be 0.05–0.1% [16, 17], there is minimal documentation of the epidemiology of S-HTG or VS-HTG in Canada. This study examined the incidence of S-HTG and VS-HTG in Canada’s most populous province (Ontario), which is ethnically and socially distinct from populations studied previously [14, 16]. The demographic distribution, laboratory features and co-morbidities associated with VS-HTG in Canada were also examined. Further, as studies conducted in regions without universal health care coverage [16] suggest a significant care gap for patients with VS-HTG, the care patterns of Ontario residents with VS-HTG were examined to determine whether a similar care gaps exist.
Methods
Design and setting
This was a population-based retrospective cohort study of adults ≥18 years in Ontario, Canada between 2010 and 2015. Ontario’s approximately 13.5 million residents have universal healthcare through the Ontario Health Insurance Program (OHIP), with comprehensive medication coverage provided to those ≥65 years or using social assistance. Information on the use of these health services is maintained at ICES (formerly The Institute for Clinical Evaluative Sciences). ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, for health system evaluation and improvement.
Participants
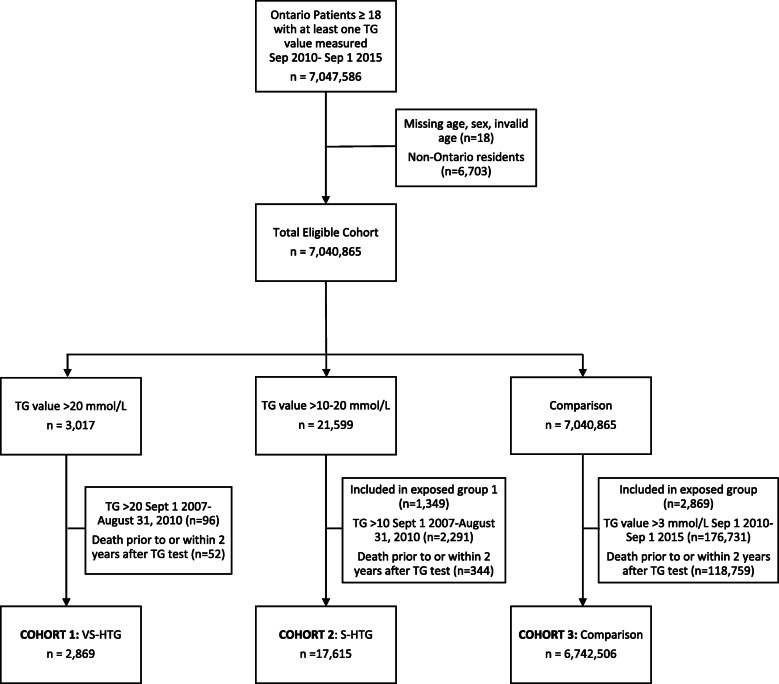
All individuals aged ≥18 years with at least one TG value in the Ontario Laboratories Information System (OLIS) between September 1, 2010 and September 1, 2015 were included. This study period was selected to allow for a 2-year follow up for care patterns and outcomes of interest following identification of an incident case (OLIS laboratory data available until the end of 2017). Standard data cleaning excluded those with invalid health card numbers, age ≥ 105 years, missing sex, and non-Ontario residents. Three patient cohorts were then created. Individuals who had TG levels > 20 mmol/L were included in the VS-HTG cohort (cohort 1) and individuals who had TG levels > 10–20 mmol/L were included in the S-HTG cohort (cohort 2). Those with prior evidence of TG > 20 or > 10 mmol/L between September 12, 2007–August 31, 2010 were excluded to define new evidence of VS-HTG or S-HTG respectively.
A third cohort (cohort 3) was used to contrast characteristics of those with VS-HTG and with no HTG and establish predictors for VS-HTG. This comparator group included all Ontario residents ages ≥18 years with at least one TG value in OLIS during the study period, no evidence of TG value > 3 mmol/L and who were not already in the S-HTG or VS-HTG cohort. In all cohorts, those who died within 2 years after a TG test were excluded to establish their follow up care patterns. If individuals had more than one TG test during the study period, the first TG test was selected (Fig. 1).
Fig. 1.
Flowchart of study participants. After removal of duplicate and invalid data, the final cohorts included 2869 individuals in VS-HTG cohort 1 (TG > 20 mmol/L), 17,615 in S-HTG cohort 2 (TG > 10-20 mmol/L) and 6,742,506 in the comparison cohort 3 (no TG > 3.0 mmol/L)
Sources of data
Data were drawn from a number of ICES databases (Supplemental Table 1). Datasets were linked using unique encoded identifiers and analyzed at ICES. Demographic data were obtained from the Registered Persons Database (RPDB), which includes all individuals who have been issued an Ontario health card. The Client Agency Program Enrolment (CAPE) database was used to determine patients who were rostered to a family physician. The Canadian Institutes for Health Information’s Discharge Abstract Database (CIHI-DAD) and the National Ambulatory Care Reporting System (NACRS) contain diagnostic and procedural information captured during hospitalizations and emergency department visits, respectively, using International Classification of Diseases 10th Revision (ICD-10) [18] and Canadian Classification of Health Interventions (CCI) [19] codes. Additional comorbidities and healthcare services use was captured through OHIP, which contains billing and diagnostic codes (Supplemental Table 1). Hypertension and diabetes status were determined from the hypertension database (HYPER) [20] and Ontario Diabetes Database (ODD) [21], respectively. For individuals ≥65 years, use of medications that can be associated with or used to treat HTG was captured using the Ontario Drug Benefit (ODB) and Drug Identification Number (DIN) database. Laboratory data were obtained through OLIS. The OLIS database holds laboratory data from both community and hospital laboratories with good catchment across Ontario [22]. As of 2016, 95% of community lab volume and over 80% of total provincial lab volume were recorded in OLIS [23]. Supplementary Table 1 includes full details on variable definitions.
Incidence of VS-HTG
The primary aim was to calculate the incidence of S-HTG and VS-HTG over the 5 year period. This was done using two denominators: the mean number of Ontarians ≥18 years between 2010 and 2015, and the number of adults ≥18 years who had a measured TG level over the study period.
Outcomes
The 2-year patterns of care of those with VS-HTG were examined, including contacts with family physicians, internists and endocrinologists, repeat TG testing, new prescriptions for fibrates, statins and niacin, and minimum and last follow-up TG values. The secondary exploratory outcomes of interest included hospital encounters for pancreatitis, acute myocardial infarction or ischemic stroke over the 2-year follow up period.
Statistical analysis
The incidence of S-HTG and VS-HTG was provided as a rate per 100,000. Descriptive statistics were used to capture baseline differences between the VS-HTG cohort and the comparator cohort 3. Continuous variables were reported as mean +/− standard deviation (SD) and median with interquartile range (IQR). Binary variables were reported as percentages. Differences between cohorts were evaluated using standardized differences (StDiff), with a value of > 0.1 considered significant [24]. One-way ANOVA or Chi Square tests were also used to compare the means and medians of continuous variables and the proportions of categorical variables, respectively. P-value s < 0.05 were considered statistically significant. Variables that were hypothesized to affect TG levels, co-exist with HTG or related complications from HTG were included in the analysis. To identify predictors of VS-HTG, both univariable and multivariable logistic regression were used (nominal P-value for significance < 0.05) and reported results as odds ratios (OR) and 95% confidence intervals (CI). Descriptive statistics were used to report crude rates of secondary outcomes of interest.
Ethics approval
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a Research Ethics Board. Guidelines for reporting of studies outlined by routine collected healthcare data (RECORD) were used (Supplemental Table 2) [25], as well as STROBE cohort reporting guidelines for observational studies [26].
Results
There were 22,745,387 TG tests performed in Ontario between 2010 and 2015 in those ≥18 years (7,047,586 unique individuals). A total of 17,615 and 2869 people had S-THG and VS-HTG respectively. The comparison cohort included 6,742,506 individuals (Fig. 1).
Baseline differences considered between the VS-HTG cohort 1 and the comparison cohort 3 are shown in Table 1. In general, those with VS-HTG were more often male (78.0% vs 45.6%; StDiff 0.71, P-value < 0.001), had diabetes (44.0% vs 13.9%; StDiff 0.7, P-value < 0.001), chronic liver disease (7.9% vs 3.4%; StDiff 0.19, P-value < 0.001), alcohol abuse (2.3% vs 0.4%; StDiff 0.17; P-value < 0.001), obesity (1.8% vs 0.6%; StDiff 0.12; P-value < 0.001) and HbA1c > 8.5% (13.8% vs 1.5%; StDiff 0.48; P-value < 0.001). Significantly more individuals in the VS-HTG cohort had a baseline history of pancreatitis (6.2% vs 0.3%; StDiff 0.34; P-value < 0.001) (Table 1). All measured components of metabolic syndrome appeared higher in the VS-HTG cohort: (HTN (43.4% vs 33.1%; StDiff 0.21; P-value < 0.001), low HDL cholesterol (C) (mean 0.97 vs 1.27 mmol/L; StDiff 0.79; P-value < 0.001), elevated HbA1c (mean 7.88% vs 6.63%; StDiff 0.67; P-value < 0.001) and obesity (1.8% vs 0.6%; StDiff 0.12; P-value < 0.001).
Table 1.
Baseline characteristics of VS-HTG and comparison cohorts
| VS-HTG Cohort N = 2869 |
Comparison Cohort N = 6,742,506 |
Standardized differences | P-value | |
|---|---|---|---|---|
| Age at index date, years | ||||
| Mean (SD) | 47.28 ± 10.87 | 51.74 ± 16.21 | 0.32 | < 0.001 |
| Median (IQR) | 47.0 (40.00–54.00) | 52.0 (40.00–63.00) | 0.35 | < 0.001 |
| 18–30 yrs | 174 (6.1%) | 744,062 (11.0%) | 0.18 | < 0.001 |
| 31–45 yrs | 1078 (37.6%) | 1,642,193 (24.4%) | 0.29 | |
| 46–65 yrs | 1481 (51.6%) | 2,963,456 (44.0%) | 0.15 | |
| 66+ yrs | 136 (4.7%) | 1,392,795 (20.7%) | 0.49 | |
| Sex, female | 630 (22.0%) | 3,667,595 (54.4%) | 0.71 | < 0.001 |
| Income quintilea | ||||
| 1 - lowest | 690 (24.1%) | 1,231,411 (18.3%) | 0.14 | < 0.001 |
| 2 | 649 (22.6%) | 1,323,360 (19.6%) | 0.07 | |
| 3 | 635 (22.1%) | 1,371,761 (20.3%) | 0.04 | |
| 4 | 493 (17.2%) | 1,432,535 (21.2%) | 0.1 | |
| 5 - highest | 402 (14.0%) | 1,383,439 (20.5%) | 0.17 | |
| Rostered to a GP | 2346 (81.8%) | 5,619,709 (83.3%) | 0.04 | 0.023 |
| Comorbidities | ||||
| Diabetes (Type 1 and Type 2) | 1262 (44.0%) | 940,151 (13.9%) | 0.70 | < 0.001 |
| Hypertension | 1244 (43.4%) | 2,232,885 (33.1%) | 0.21 | < 0.001 |
| Coronary artery disease (excluding angina) | 339 (11.8%) | 600,499 (8.9%) | 0.10 | < 0.001 |
| Cardiovascular disease | 87 (3.0%) | 218,670 (3.2%) | 0.01 | 0.524 |
| Peripheral vascular disease | 18 (0.6%) | 21,539 (0.3%) | 0.04 | 0.003 |
| Chronic liver disease | 226 (7.9%) | 230,046 (3.4%) | 0.19 | < 0.001 |
| Alcohol | 66 (2.3%) | 24,957 (0.4%) | 0.17 | < 0.001 |
| Obesity | 53 (1.8%) | 38,645 (0.6%) | 0.12 | < 0.001 |
| Hypothyroidism | 15 (0.5%) | 24,618 (0.4%) | 0.02 | 0.161 |
| Multiple myeloma | 0 | 1060 (0.0%) | 0.02 | 0.502 |
| Nephrotic syndrome | 29 (1.0%) | 14,392 (0.2%) | 0.10 | < 0.001 |
| Chronic kidney disease | 199 (6.9%) | 209,348 (3.1%) | 0.18 | < 0.001 |
| Acute Pancreatitis | 177 (6.2%) | 19,602 (0.3%) | 0.34 | < 0.001 |
| Gallstone disease | 212 (7.4%) | 114,035 (1.7%) | 0.28 | < 0.001 |
| Current pregnancy in women | 47 (1.6%) | 385,120 (5.7%) | 0.22 | < 0.001 |
| Charlson comorbidity index | ||||
| Mean (SD) | 0.92 ± 1.38 | 0.44 ± 1.05 | 0.39 | < 0.001 |
| Median (IQR) | 0.00 (0.00–1.00) | 0.00 (0.00–0.00) | 0.52 | < 0.001 |
| 0 | 2241 (78.1%) | 6,104,946 (90.5%) | 0.35 | < 0.001 |
| 1 | 331 (11.5%) | 302,652 (4.5%) | 0.26 | |
| 2 | 142 (4.9%) | 193,468 (2.9%) | 0.11 | |
| 3+ | 155 (5.4%) | 141,440 (2.1%) | 0.17 | |
| Health care utilization | ||||
| Primary care (FP/GP) visits | ||||
| Mean (SD) | 6.87 ± 8.85 | 5.24 ± 6.45 | 0.21 | < 0.001 |
| Median (IQR) | 5.00 (2.00–8.00) | 4.00 (2.00–7.00) | 0.21 | < 0.001 |
| Endocrinologist visits | ||||
| Mean (SD) | 0.23 ± 0.93 | 0.06 ± 0.48 | 0.22 | < 0.001 |
| Internal medicine visits | ||||
| Mean (SD) | 1.03 ± 2.90 | 0.62 ± 2.36 | 0.15 | < 0.001 |
| Laboratory measurements | ||||
| HbA1c | 1083 (37.7%) | 929,242 (13.8%) | 0.57 | < 0.001 |
| HbA1c > 8.5% | 397 (13.8%) | 100,258 (1.5%) | 0.48 | < 0.001 |
| Mean (SD) | 7.88 ± 2.29 | 6.63 ± 1.37 | 0.67 | < 0.001 |
| Median (IQR) | 7.30 (6.00–9.40) | 6.20 (5.80–7.10) | 0.53 | < 0.001 |
| LDL cholesterol | 485 (16.9%) | 955,143 (14.2%) | 0.08 | < 0.001 |
| Mean (SD) mmol/L | 2.52 ± 1.49 | 2.71 ± 1.02 | 0.15 | < 0.001 |
| Median (IQR) mmol/L | 2.31 (1.49–3.26) | 2.58 (1.93–3.38) | 0.25 | < 0.001 |
| HDL cholesterol | 1202 (41.9%) | 986,111 (14.6%) | 0.64 | < 0.001 |
| Mean (SD) mmol/L | 0.97 ± 0.38 | 1.27 ± 0.38 | 0.79 | < 0.001 |
| Median (IQR) mmol/L | 0.91 (0.76–1.11) | 1.21 (1.00–1.47) | 0.93 | < 0.001 |
| non-HDL cholesterol | 327 (11.4%) | 18,595 (0.3%) | 0.49 | < 0.001 |
| Mean (SD) mmol/L | 5.14 ± 2.27 | 4.58 ± 1.38 | 0.30 | < 0.001 |
| Median (IQR) mmol/L | 4.68 (3.75–5.98) | 4.52 (3.64–5.40) | 0.17 | 0.001 |
| Total cholesterol | 1206 (42.0%) | 994,409 (14.7%) | 0.63 | < 0.001 |
| Mean (SD) mmol/L | 6.41 ± 2.75 | 4.78 ± 1.25 | 0.76 | < 0.001 |
| Median (IQR) mmol/L | 5.79 (4.71–7.33) | 4.66 (3.85–5.57) | 0.74 | < 0.001 |
| ALT | 1282 (44.7%) | 1,384,012 (20.5%) | 0.53 | < 0.001 |
| Mean (SD) U/L | 40.99 ± 39.83 | 27.36 ± 29.50 | 0.39 | < 0.001 |
| Median (IQR) | 31.00 (21.00–46.00) | 22.00 (17.00–31.00) | 0.58 | < 0.001 |
| Corrected calcium | 210 (7.3%) | 166,005 (2.5%) | 0.23 | < 0.001 |
| Mean (SD) mmol/L | 2.30 ± 0.15 | 2.31 ± 0.11 | 0.12 | 0.045 |
| Median (IQR) mmol/L | 2.29 (2.23–2.37) | 2.31 (2.24–2.37) | 0.10 | 0.127 |
Standardized difference > 10% are considered statistically significant; < 1% of income quintiles were missing and were re-coded as ‘3’; Small cells (< 6) are suppressed as per ICES privacy policy; Comorbidities were obtained in the 5 years prior to the index date; Health care utilization measures were obtained in the 1 year prior to index date; Health care utilization measures were obtained in the 1 year prior to index date; Laboratory measurements were obtained in the 1 year prior to index prescription date; Evidence of pregnancy in women was obtained in the 1 year prior and within 9 month after to index date. Please refer to supplementary Table 1 for further information on coded data included for each variable. aMissing income (< 1%) was recoded as ‘3’. Missing Charlson (~ 50%) was due to patients having no hospitalizations for relevant comorbidities found during the 5 year lookback period; they were recoded as ‘0’; ^P-value for variable as a whole
Abbreviations: VS-HTG very severe hypertriglyceridemia (TG > 20 mmol/L), yrs. years, SD Standard deviation, IQR Interquartile range, GP General Practitioner, HTN hypertension, CAD coronary artery disease, PVD peripheral vascular disease, CVD cerebrovascular disease, CKD chronic kidney disease, FP family practitioner, HbA1c hemoglobin A1c, LDL low-density lipoprotein, HDL high density lipoprotein, ALT alanine aminotransferase
Incidence of S-HTG and VS-HTG in Ontario adults between 2010 and 2015 was 163.61 and 26.65 per 100,000 (~ 1 in 615 and 1 in 3750) adults overall, and 250.18 and 40.75 per 100,000 (~ 1 in 400 and 1 in 2500) adults who had at least one TG test (Table 2). Combined incidence rate of TG > 10 mmol/L was ~ 1 in 344 adults who had at least one TG value and ~ 1 in 526 adults overall (Fig. 2). The highest incidence of S-HTG and VS-HTG appeared between ages 31–45 (315.17 and 63.07/100,000 with a TG test; 197.12 and 39.45/100,000 population) and 46–65 (324.86 and 48.21/100,000 with a TG test; 266.40 and 39.54/100,000 population) (Table 2). Overall, incidence was higher in men (Supplemental Table 3).
Table 2.
Incidence of severe (S-HTG; TG > 10-20 mmol/L) and very severe (VS-HTG; TG > 20 mmol/L) hypertriglyceridemia in Ontario by age group
| Ages 18–30 | Ages 31–45 | Ages 46–65 | Ages 66+ | Total | |
|---|---|---|---|---|---|
| Number of individuals with at least one TG test | 761,224 | 1,709,237 | 3,071,797 | 1,498,607 | 7,040,865 |
| Mean Ontario population between 2010 and 2015 | 2,412,041 | 2,732,915 | 3,745,940 | 1,875,874 | 10,766,770 |
| S-HTG | |||||
| n | 835 | 5387 | 9979 | 1414 | 17,615 |
| Incidence in those with at least one TG test (per 100,000) | 109.69 | 315.17 | 324.86 | 94.35 | 250.18 |
| Incidence in Ontario population (per 100,000) | 34.62 | 197.12 | 266.40 | 75.38 | 163.61 |
| VS-HTG | |||||
| n | 174 | 1078 | 1481 | 136 | 2869 |
| Incidence in those with at least one TG test (per 100,000) | 22.86 | 63.07 | 48.21 | 9.08 | 40.75 |
| Incidence in Ontario population (per 100,000) | 7.21 | 39.45 | 39.54 | 7.25 | 26.65 |
Abbreviations: S-HTG severe hypertriglyceridemia (TG > 10–20 mmol/L), VS-HTG very severe hypertriglyceridemia (TG > 20 mmol/L), ON Ontario, pop population, n number of individuals
Fig. 2.
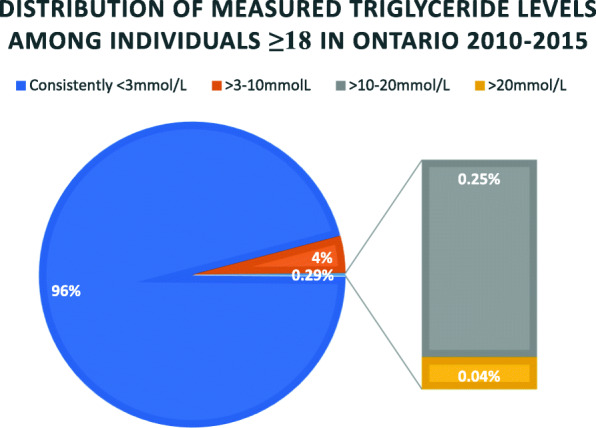
Summary of measured triglyceride (TG) values in Ontario from 2010 to 2015. Among 7,040,865 individuals ≥18 years with measured TG in Ontario between 2010 and 2015: 6,742,506 (96%) had no TG value measured above 3 mmol/L; 21,484 individuals in Ontario (0.29%) had at least one TG value > 10 mmol/L, with 0.25% (n = 17,615) having severe hypertriglyceridemia (TG > 10–20 mmol/L) and 0.04% (n = 2869) having very severe hypertriglyceridemia (TG > 10 mmol/L). 277,875 (4%) individuals were not included in the other three cohorts and were assumed to have at least one measured TG value within the range of > 3–10 mmol/L
Medication use was only available for individuals ≥65 years (N = 136 in the VS-HTG cohort) (Supplemental Table 4). At baseline, a higher proportion of VS-HTG patients used a fibrate (18.4% vs 1.6%; SD 0.58) and a lower proportion used statins (40.4% vs 45.7%; StDiff 0.11) compared to the comparison cohort (N = 1,392,795). A higher proportion of VS-HTG patients also appeared to use other lipid-lowering agents (11.8% vs 4.2%; StDiff 0.28), oral furosemide (16.2% vs 6.3%; StDiff 0.32) chlorthalidone (< 5% vs 0.6%; StDiff 0.14) and salicylates (5.9% vs 3.5%; StDiff 0.11) (supplemental Table 3).
Results of univariable and multivariable analysis are presented in Table 3. In multivariable analysis, significant predictors of VS-HTG were diabetes (OR 5.38, CI 4.93–5.88), male sex (OR 3.83, CI 3.50–4.18), alcohol abuse (OR 2.47, CI 1.90–3.19), chronic liver disease (OR 1.71, CI 1.48–1.97), hypertension (OR 1.69, CI 1.54–1.86), obesity (OR 1.49, CI 1.13–1.98), and chronic kidney disease (OR 1.39, CI 1.19–1.63). Older age was associated with reduced risk of VS-HTG (OR 0.64/decade, CI 0.62–0.66). Higher income quintiles (4 and 5) were associated with lower odds of having VS-HTG in both univariable and multivariable analysis (0.78, CI 0.70–0.88 for quintile 4 and 0.72, CI 0.63–0.81 for quintile 5). In univariable analysis, lowest income quintile was associated with VS-HTG (OR 1.21, CI 1.09–1.35) but this did not remain significant in the multivariate analysis. Likewise, higher Charlson comorbidity scores (moderate to high) were associated with VS-HTG in the univariate analysis. A Charlson index of 3+ was no longer significantly associated with VS-HTG in multivariable analysis (Table 3).
Table 3.
Predictors of VS-HTG, ranked by odds ratio
| Univariable analysis | Multivariable analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | LCL | UCL | P-value | Odds Ratio | LCL | UCL | P-value | |
| Diabetes | 4.85 | 4.50 | 5.22 | < 0.0001 | 5.38 | 4.93 | 5.88 | < 0.0001 |
| Sex | ||||||||
| Male | 4.24 | 3.88 | 4.63 | < 0.0001 | 3.83 | 3.50 | 4.18 | < 0.0001 |
| Female | REF | REF | REF | REF | REF | REF | ||
| Alcohol | 6.34 | 4.96 | 8.09 | < 0.0001 | 2.47 | 1.90 | 3.19 | < 0.0001 |
| Chronic liver disease | 2.42 | 2.11 | 2.77 | < 0.0001 | 1.71 | 1.48 | 1.97 | < 0.0001 |
| HTN | 1.55 | 1.44 | 1.67 | < 0.0001 | 1.69 | 1.54 | 1.86 | < 0.0001 |
| Obesity | 3.27 | 2.49 | 4.29 | < 0.0001 | 1.49 | 1.13 | 1.98 | 0.0049 |
| CKD | 2.33 | 2.01 | 2.69 | < 0.0001 | 1.39 | 1.19 | 1.63 | < 0.0001 |
| Income quintile | ||||||||
| 1 - lowest | 1.21 | 1.09 | 1.35 | 0.0005 | 1.09 | 0.98 | 1.22 | 0.1134 |
| 2 | 1.06 | 0.95 | 1.18 | 0.3011 | 1.02 | 0.92 | 1.14 | 0.6747 |
| 3 | REF | REF | REF | REF | REF | REF | ||
| 4 | 0.74 | 0.66 | 0.84 | < 0.0001 | 0.78 | 0.70 | 0.88 | < 0.0001 |
| 5 - highest | 0.63 | 0.55 | 0.71 | < 0.0001 | 0.72 | 0.63 | 0.81 | < 0.0001 |
| Age (per decade) | 0.84 | 0.82 | 0.86 | < 0.0001 | 0.64 | 0.62 | 0.66 | < 0.0001 |
| Charlson comorbidity indexa | ||||||||
| 0 | REF | REF | REF | REF | REF | REF | ||
| 1 | 2.98 | 2.66 | 3.34 | < 0.0001 | 1.61 | 1.42 | 1.82 | < 0.0001 |
| 2 | 2.00 | 1.69 | 2.37 | < 0.0001 | 1.26 | 1.05 | 1.50 | 0.0137 |
| 3+ | 2.99 | 2.54 | 3.51 | < 0.0001 | 1.15 | 0.95 | 1.38 | 0.1504 |
Sample size is the full cohort (N = 6,745,375); Exposed (n = 2869); Unexposed (n = 6,742,506) All predictors were associated with the odds of having hypertriglyceridemia. Diabetes includes both type 1 and type 2
Abbreviations: LCL lower confidence limit, UCL upper confidence limit, HTN hypertension, CKD chronic kidney disease, REF used as reference
a Missing income (< 1%) was recoded as ‘3’. Missing charlson (~ 50%) was due to patients having no hospitalizations for relevant comorbidities found during the 5 year lookback period; they were recoded as ‘0’
Outcomes
The majority of individuals with VS-HTG received follow-up healthcare within 2 years of their TG test (Table 4); 98.4% had at least one follow up visit to a family physician (FP), 32.8% had at least one visit to an endocrinologist and 56.7% had at least one visit to a general internist. The majority achieved TG reduction below the high-risk pancreatitis threshold of 10 mmol/L, with 89.3% having a repeat TG test. The last TG measured had a median TG value of 4.7 mmol/L (IQR 2.7–9.1) and lowest TG value had a median TG value of 3.3 mmol/L (IQR 2.0–5.9). For individuals > 65 years of age, new prescriptions for statins were provided in 32.4% and for fibrates, in 19.9% (Supplemental Table 3).
Table 4.
Healthcare Patterns and Events of Interest in patients with VS-HTG
| Within 1 year | Within 2 years | |
|---|---|---|
| Healthcare patterns (N = 2869) | ||
| General practitioner visit | 2786 (97.1%) | 2822 (98.4%) |
| Endocrinologist visit | 775 (27.0%) | 941 (32.8%) |
| Internist visita | 1279 (44.6%) | 1628 (56.7%) |
| TG test | 2218 (77.3%) | 2561 (89.3%) |
| Last TG value | ||
| Mean (SD) (mmol/L) | 7.66 ± 8.29 | 7.68 ± 8.35 |
| Median (IQR) (mmol/L) | 4.7 (2.7–9.1) | 4.7 (2.7–9.1) |
| Lowest TG value | ||
| Mean (SD) (mmol/L) | 6.09 ± 6.74 | 5.30 ± 6.05 |
| Median (IQR) (mmol/L) | 3.8 (2.2–7.1) | 3.3 (2.0–5.9) |
| New prescriptions (restricted to ages 66+,N = 136) | ||
| Statin | 35 (25.7%) | 44 (32.4%) |
| Fibrate | 25 (18.4%) | 27 (19.9%) |
| Niacin | 0 | 0 |
| Events | Within 1 year | Within 2 years |
| At least one hospital encounter for pancreatitis | 118 (4.1%) | 171 (6.0%) |
| At least one hospital encounter for acute myocardial infarction | 22 (0.8%) | 39 (1.4%) |
| At least one hospital encounter for Ischemic stroke | 12 (0.4%) | 24 (0.8%) |
a For the purposes of this data ‘internal medicine’ refers specifically to the subspecialty of general internal medicine and does not include other internal medicine subspecialties
Following detection of VS-HTG, pancreatitis occurred in 4.1 and 6.0% of individuals in the VS-HTG cohort within one and 2 years, respectively (Table 4). Within 2 years, 1.4 and 0.8% of individuals in the VS-HTG cohort had at least one hospital encounter for acute myocardial infarction and ischemic stroke, respectively (Table 4).
Discussion
The incidence of TG > 10–20 (S-HTG) and > 20 mmol/L (VS-HTG) between 2010 and 2015 was approximately 1 in 400 (0.25%) and 1 in 2500 (0.04%) among adults in Ontario with measured TG, and 1 in 613 (0.16%) and 1 in 3750 (0.27%) of the adult population, respectively. These numbers align with prevalence rates reported in other studies [14, 16, 17]. Peak age of incidence was 30–65 years, which may correspond to the age at which a screening lipid profile may first be conducted, or the age at which related chronic conditions start to manifest. While the Endocrine Society defines severe hypertriglyceridemia as a serum TG level > 1000 mg/dL (11.3 mmol/L) and very severe as > 3000 mg/dL (22.6 mmol/L) [1], the approximations of 10 and 20 mmol/L, respectively, are more practical for a Canadian population.
Significant predictors of VS-HTG in Ontario included male sex, as well as known risk factors for HTG, including diabetes, chronic liver disease, alcohol abuse, obesity and chronic kidney disease. Hypertension was likely a predictor given its association with metabolic syndrome. The two most significant controllable predictors were diabetes and alcohol abuse. The definition used for alcohol abuse in this study was broad to allow for increased sensitivity, but included any complication that stemmed from chronic or acute alcohol ingestion (see Supplemental Table 1). It is thus difficult to determine which specific alcohol-related behaviors or patterns of intake may be most contributory.
The VS-HTG cohort had more contacts with healthcare providers, which may relate to more associated chronic diseases. This may have predisposed individuals to having had a screening lipid test. Patients in the VS-HTG group were also more likely to have had HbA1c testing, and to have an HbA1c > 8.5%, likely relating to the higher prevalence of metabolic syndrome and diabetes in the VS-HTG cohort. Mean LDL-C was minimally but significantly higher in the VS-HTG. Mean HDL-C was significantly lower in the VS-HTG cohort, reflecting the inverse relationship between TG and HDL-C. Non-HDL and total cholesterol were higher in the VS-HTG cohort, likely driven by elevated TG-rich lipoproteins and remnant particles.
While other studies showed poor follow up care following identification of HTG, in this Ontario cohort, no significant gaps in appropriate care were identified. This may be due to universal healthcare access in Ontario, which was not a feature of other populations studied [16]. Within the 2 year follow-up period, 98.4% of individuals in the VS-HTG cohort were seen by a FP and 89.3% had a repeat TG test. One-third were seen by an endocrinologist and over half by an internist. Follow-up TG tests showed significant reductions in TG levels, with the median TG level falling below the threshold for pancreatitis risk (4.7 mmol/L; IQR 2.7–9.1). The median of the lowest recorded TG values remained elevated at 3.3 mmol/L (IQR 2.0–5.9) (normal < 1.7 mmol/L), likely reflecting the limitations of currently available pharmacological and lifestyle interventions to fully correct TG to a normal range, particularly in those with underlying inherited metabolic defects. Discussions of current management recommendations for HTG and options are beyond the scope of this work, but are discussed in detail elsewhere [5]. In the subset of the VS-HTG cohort that were over the age of 65, most were on, or were placed on, a statin (40.4% at baseline, 32.4% with new prescriptions following identification of VS-HTG) and a third were on a fibrate (18.4% at baseline, 19.9% with new prescriptions). The substantial reduction in TG levels, despite only a third of patients with medication information available being placed on a fibrate, suggests that control of contributory secondary factors, such as diabetes, obesity or lifestyle may have played a considerable role in the improvements in TG levels.
Pancreatitis rates in individuals with VS-HTG (4.1% within 1 year, 6% within 2 years) were within the range of expectation based on other reports [27]. There was no apparent excess risk of atherosclerotic cardiovascular disease within the VS-HTG cohort at baseline or within the 2-year follow up period. However, this study was not designed to examine these outcomes. A separate study focusing on the risk of ASCVD and ischemic stroke in the VS-HTG population that accounts for potential confounders may provide further support for the findings observed.
Future studies that evaluate TG as a continuous variable would help define the risk of acute pancreatitis associated with a given degree of HTG. Further investigations that focus on outcomes in VS-HTG patients is another avenue of investigation, including prevalence and predictors of pancreatitis and its complications. Genetic investigation into a subset of this cohort may also help define the spectrum of genetic variation that may underlie a presentation of VS-HTG.
Comparison with other provinces in Canada and European Union (EU) countries
All Canadian provinces have universal healthcare coverage, however there are differences across the Canadian provinces in terms of risk factors for VS-HTG (e.g. obesity and type 2 diabetes) For example, provinces such as Saskatchewan, New Brunswick, Nova Scotia and Newfoundland and Labrador have higher rates of obesity (35–38%) compared to Ontario (26%), which is just below the national average of 27% (range of all provinces 22–38%) [28]. Approximately 30% of Ontarians live with diabetes or prediabetes, which is slightly higher than the national average of 29% (range of all province 25–35%) [29]. There is also ethnic variation between the provinces, with Ontario and British Columbia having the highest rates of ethnic diversity (29.3 and 30.3% of adult population identifying as visible minorities, respectively, national average 22.3%, range for all provinces 2.3–30.3%) [30].
Most EU countries are similar to Ontario in that they have universal access to healthcare, but may differ in other ways that could affect prevalence and predictors of VS-HTG. Obesity rates are overall lower in the EU compared to Ontario (17%; range 10.7–30.6%) [31], as are rates of type 2 diabetes (~ 10%) [32]. There may also be differences in ethnic diversity.
Study strengths and limitations
Strengths of this study include access to province-wide laboratory data, the large study cohort with access to universal health services and the use of well-defined coding algorithms used to investigate patient characteristics. It is also, to our knowledge, the first study to systematically assess incidence and characteristics associated with HTG in a Canadian population.
While this study provides useful province-wide information on incidence of S- and VS-HTG, there are some limitations. Prevalence was not examined and information was only gathered over a 5-year time frame with the study collection period ending in 2015, limiting capture of more recent trends. Furthermore, not all laboratory data were available for all individuals (e.g. HbA1c), potentially creating bias. Additionally, not all laboratories submitted data to OLIS simultaneously and data may be less complete for earlier time points [22]. Inclusion in the VS-HTG or S-HTG cohort were also based upon a single TG measurement, which could have allowed for inclusion of individuals in these cohorts who had only transiently elevated TG levels. However, TG levels in this range, even transiently can expose an individual to the risk of pancreatitis. Furthermore, literature supports day-to-day variability in TG of approximately 20% [33], therefore even accounting for maximal variability, TG levels are likely to remain elevated on subsequent tests. Information on pharmacological treatment was limited to a subset of the VS-HTG cohort, limiting the usefulness and generalizability of this data. The use of over the counter supplements could not be captured with our data sources. Certain susceptibility states, such as obesity and alcohol abuse, may be underestimated in the administrative data due to low coding sensitivity, which may have underestimated their contribution to HTG. Individuals with poor access to healthcare may be under-represented in the study sample as they would be less likely to obtain a lipid profile. Similarly, it is possible that including these patients with undetected VS-HTG may have resulted in lower follow-up rates than seen in this VS-HTG cohort. Additionally, data regarding visits to some specialists that may be involved in the management of VS-HTG, such as cardiologists or gastroenterologists, was not captured. While it was concluded that there was no significant care gap, it could be argued that specialist referral would be most appropriate for anyone with a history of VS-HTG, given it is a rare condition with potentially serious side effects, suggesting that there may still be a gap in appropriate care within Ontario. There were overall low numbers in the VS-HTG cohort, but only 10 predictors were chosen and there should have had sufficient statistical power. Additionally, the baseline rates of pancreatitis and use of fibrates were high in those with VS-HTG, suggesting that these may not have all been incident cases. Finally, given the observational nature of the data set, causality cannot be determined, and the findings may not be generalizable outside Ontario.
Conclusions
In conclusion, this study shows that ~ 1/400 adults in Ontario have S-HTG and ~ 1/2500 had new evidence of VS-HTG from 2010 to 2015. Peak incidence occurs between the ages of 30 and 65 years. Conditions that are most strongly associated with VS-HTG include diabetes, male sex, alcohol, chronic liver disease, hypertension, obesity and chronic kidney disease. No significant care gap was identified for individuals in Ontario with identified VS-HTG and the majority had repeat TG below the threshold for pancreatitis risk.
These findings may assist clinicians in recognizing individuals at heightened risk for VS-HTG, who may benefit from increased surveillance. Male patients with diabetes, obesity and alcohol abuse are at the highest risk; early attention to these patients may assist in developing an individualized treatment plan to monitor for HTG and prevent associated adverse outcomes.
Supplementary Information
Additional file 1: Supplemental Table 1. Databases Utilized. Supplemental Table 2. RECORD checklist (from (17)). Supplementary Table 3. Incidence of severe (S-HTG; TG >10-20mmol/L) and very severe (VS-HTG; TG>20mmol/L) hypertriglyceridemia in Ontario by age group and gender. Supplemental Table 4. Prescription characteristics of VS-HTG and comparison cohorts
Disclosures
R.A.H. is supported by the Jacob J. Wolfe Distinguished Medical Research Chair, the Edith Schulich Vinet Research Chair in Human Genetics, and the Martha G. Blackburn Chair in Cardiovascular Research. R.A.H. has also received operating grants from the Canadian Institutes of Health Research (Foundation award), the Heart and Stroke Foundation of Ontario (G-18-0022147).
Abbreviations
- S-HTG
Severe hypertriglyceridemia
- VS-HTG
Very severe hypertriglyceridemia
- TG
Triglyceride
- OR
Odds ratio
- SD
Standard deviation
- LPL
Lipoprotein lipase
- APOC2
Apolipoprotein C-II
- APOA5
Apolipoprotein A-V
- LMF1
Lipase maturation factor 1
- GPIHBP1
Glycosylphosphatidylinositol-anchored high density lipoprotein binding protein 1
- OHIP
Ontario Health Insurance Program
- RPDB
Registered Persons Database
- CAPE
Client Agency Program Enrolment
- CIHI-DAD
Canadian Institutes for Health Information’s Discharge Abstract Database
- NACRS
National Ambulatory Care Reporting System
- ICD-10
International Classification of Diseases 10th Revision (ICD-10)
- CCI
Canadian Classification of Health Interventions
- HYPER
Hypertension database
- ODD
Ontario Diabetes Database
- ODB
Ontario Drug Benefit
- DIN
Drug Identification Number
- IQR
Interquartile range
- StDiff
Standardized differences
- CI
Confidence intervals
- HTN
Hypertension
- FP
Family physician
Authors’ contributions
AJB conceived the project, with assistance from RAH. All authors planned the experiment and data analysis. KKC planned the protocol, with input from all other authors. AMO conducted the analysis with support from SZS. AJB wrote the manuscript with support from RAH, KKC and AMO. All authors provided critical feedback and helped shape the research, analysis and manuscript. The authors read and approved the final manuscript.
Funding
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The study was completed at the ICES Western site, where core funding is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine and Dentistry, Western University, and the Lawson Health Research Institute. R.A.H. is supported by the Jacob J. Wolfe Distinguished Medical Research Chair, the Edith Schulich Vinet Research Chair in Human Genetics, and the Martha G. Blackburn Chair in Cardiovascular Research. R.A.H. has also received operating grants from the Canadian Institutes of Health Research (Foundation award), the Heart and Stroke Foundation of Ontario (G-18-0022147).
Parts of this material are based on data and information compiled and provided by CIHI and the MOHLTC. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. We thank IQVIA Solutions Canada Inc. for the use of their Drug Information File.
Availability of data and materials
The analysis was conducted by members of the ICES Western facility (London, Ontario). Alexandra Ouédraogo is responsible for the data analysis. The protocol can be obtained by emailing Dr. Kristin Clemens at Kristin.Clemens@sjhc.london.on.ca.
Declarations
Ethics approval and consent to participate
ICES is a prescribed entity under section 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects conducted under section 45, by definition, do not require review by a Research Ethics Board. This project was conducted under section 45, and approved by ICES’ Privacy and Compliance Office.
Consent for publication
Not applicable.
Competing interests
KC received a research award that was sponsored in part by Astra Zeneca. She has attended Merck sponsored medical conferences. She has received honoraria for delivering Certified Medical Education talks from Sutherland Global Services Canada ULC, the Toronto Ontario Knowledge Translation Working Group, and the Canadian Medical and Surgical Knowledge Translation Research Group.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Sacks F, Murad MH, et al. Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(9):2969–2989. doi: 10.1210/jc.2011-3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy MJ, Sheng X, MacDonald TM, Wei L. Hypertriglyceridemia and acute pancreatitis. JAMA Intern Med. 2013;173(2):162–164. doi: 10.1001/2013.jamainternmed.477. [DOI] [PubMed] [Google Scholar]
- 3.Yuan G, Al-Shali KZ, Hegele RA. Hypertriglyceridemia: its etiology, effects and treatment. CMAJ. 2007;176(8):1113–1120. doi: 10.1503/cmaj.060963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pedersen SB, Langsted A, Nordestgaard BG. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis. JAMA Intern Med. 2016;176(12):1834–1842. doi: 10.1001/jamainternmed.2016.6875. [DOI] [PubMed] [Google Scholar]
- 5.Wolska A, Yang ZH, Remaley AT. Hypertriglyceridemia: new approaches in management and treatment. Curr Opin Lipidol. 2020;31(6):331–339. doi: 10.1097/MOL.0000000000000710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brahm AJ, Hegele RA. Chylomicronaemia--current diagnosis and future therapies. Nat Rev Endocrinol. 2015;11(6):352–362. doi: 10.1038/nrendo.2015.26. [DOI] [PubMed] [Google Scholar]
- 7.Stahel P, Xiao C, Hegele RA, Lewis GF. Polygenic risk for hypertriglyceridemia can mimic a major monogenic mutation. Ann Intern Med. 2017;167(5):360–361. doi: 10.7326/L17-0182. [DOI] [PubMed] [Google Scholar]
- 8.Paquette M, Bernard S, Hegele RA, Baass A. Chylomicronemia: differences between familial chylomicronemia syndrome and multifactorial chylomicronemia. Atherosclerosis. 2019;283:137–142. doi: 10.1016/j.atherosclerosis.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 9.Hegele RA, Ginsberg HN, Chapman MJ, Nordestgaard BG, Kuivenhoven JA, Averna M, et al. The polygenic nature of hypertriglyceridaemia: implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014;2(8):655–666. doi: 10.1016/S2213-8587(13)70191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dron JS, Wang J, Cao H, McIntyre AD, Iacocca MA, Menard JR, et al. Severe hypertriglyceridemia is primarily polygenic. J Clin Lipidol. 2019;13(1):80–88. doi: 10.1016/j.jacl.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Johansen CT, Kathiresan S, Hegele RA. Genetic determinants of plasma triglycerides. J Lipid Res. 2011;52(2):189–206. doi: 10.1194/jlr.R009720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chait A, Eckel RH. The Chylomicronemia syndrome is Most often multifactorial: a narrative review of causes and treatment. Ann Intern Med. 2019;170(9):626–634. doi: 10.7326/M19-0203. [DOI] [PubMed] [Google Scholar]
- 13.Brunzell JD. Clinical practice. Hypertriglyceridemia. N Engl J Med. 2007;357(10):1009–1017. doi: 10.1056/NEJMcp070061. [DOI] [PubMed] [Google Scholar]
- 14.Retterstol K, Narverud I, Selmer R, Berge KE, Osnes IV, Ulven SM, et al. Severe hypertriglyceridemia in Norway: prevalence, clinical and genetic characteristics. Lipids Health Dis. 2017;16(1):115. doi: 10.1186/s12944-017-0511-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Hypertriglyceridemia and its pharmacologic treatment among US adults. Arch Intern Med. 2009;169(6):572–578. doi: 10.1001/archinternmed.2008.599. [DOI] [PubMed] [Google Scholar]
- 16.Esparza MI, Li X, Adams-Huet B, Vasandani C, Vora A, Das SR, et al. Very severe hypertriglyceridemia in a large US County health care system: associated conditions and management. J Endocr Soc. 2019;3(8):1595–1607. doi: 10.1210/js.2019-00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christian JB, Bourgeois N, Snipes R, Lowe KA. Prevalence of severe (500 to 2,000 mg/dl) hypertriglyceridemia in United States adults. Am J Cardiol. 2011;107(6):891–897. doi: 10.1016/j.amjcard.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 18.International statistical classification of diseases and related health problems, 10th revision, 5th edition. World Health Organization; 2016. Available from: https://apps.who.int/iris/handle/10665/246208.
- 19.Canadian Classification Of Health Interventions 2015. Available from: https://www.cihi.ca/sites/default/files/cci_volume_four_2015_en_0.pdf. Accessed 5 Mar 2020.
- 20.Lipscombe LL, Hwee J, Webster L, Shah BR, Booth GL, Tu K. Identifying diabetes cases from administrative data: a population-based validation study. BMC Health Serv Res. 2018;18(1):316. doi: 10.1186/s12913-018-3148-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tu K, Chen Z, Lipscombe LL. Canadian hypertension education program outcomes research T. prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ. 2008;178(11):1429–1435. doi: 10.1503/cmaj.071283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iskander C, McArthur E, Nash DM, Gandhi-Banga S, Weir MA, Muanda FT, et al. Identifying Ontario geographic regions to assess adults who present to hospital with laboratory-defined conditions: a descriptive study. CMAJ Open. 2019;7(4):E624–E6E9. doi: 10.9778/cmajo.20190065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ontario Lab Data and Your EMR. eHealth Ontario; 2016. Available from: https://ehealthontario.on.ca/files/public/support/OLIS_EMR_ProviderGuide_EN.pdf. Accessed 5 Mar 2020.
- 24.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat. 2009;38(6):1228–1234. doi: 10.1080/03610910902859574. [DOI] [Google Scholar]
- 25.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 27.Morkos M, Amblee A, Henriquez A, Basu S, Fogelfeld L. External validation of a predictive model for acute pancreatitis risk in patients with severe hypertriglyceridemia. Endocr Pract. 2019;25(8):817–823. doi: 10.4158/EP-2018-0599. [DOI] [PubMed] [Google Scholar]
- 28.Canadian Health Measures Survey. 2017. Available from: https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2018033-eng.htm Accessed 28 July 2020..
- 29.Canada D. Diabetes in Canada. 2021. [Google Scholar]
- 30.Immigration and Ethnocultural Diversity Highlight Tables. 2016. Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/imm/Table.cfm?Lang=E&T=41&Geo=00&SP=1&vismin=2&age=1&sex=1. Accessed 28 July 2020.
- 31.Overweight and obesity - BMI statistics. 2019. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Overweight_and_obesity_-_BMI_statistics. Accessed 28 July 2020.
- 32.Obesity and overweight. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 28 July 2020.
- 33.Bookstein L, Gidding SS, Donovan M, Smith FA. Day-to-day variability of serum cholesterol, triglyceride, and high-density lipoprotein cholesterol levels. Impact on the assessment of risk according to the National Cholesterol Education Program guidelines. Arch Intern Med. 1990;150(8):1653–1657. doi: 10.1001/archinte.1990.00040031653012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplemental Table 1. Databases Utilized. Supplemental Table 2. RECORD checklist (from (17)). Supplementary Table 3. Incidence of severe (S-HTG; TG >10-20mmol/L) and very severe (VS-HTG; TG>20mmol/L) hypertriglyceridemia in Ontario by age group and gender. Supplemental Table 4. Prescription characteristics of VS-HTG and comparison cohorts
Data Availability Statement
The analysis was conducted by members of the ICES Western facility (London, Ontario). Alexandra Ouédraogo is responsible for the data analysis. The protocol can be obtained by emailing Dr. Kristin Clemens at Kristin.Clemens@sjhc.london.on.ca.