Abstract
Background: Black mothers in the United States have shorter breastfeeding (BF) durations and less exclusive breastfeeding (EBF) than others. The factors underlying these disparities require investigation.
Methods: Using longitudinal data from a CDC-sponsored birth cohort in Cincinnati, Ohio, we analyzed the factors mediating racial disparity in BF outcomes. Study mothers were enrolled in prenatal clinics associated with two large birth hospitals. Analysis was restricted to racial groups with sufficient numbers in the cohort, non-Hispanic Black (n = 92) and White (n = 113) mothers, followed to at least 6 months postpartum.
Results: Black mothers were 25 times more likely to reside in socioeconomically deprived neighborhoods and 20 times more likely to have an annual household income <$50,000/year than White mothers (p < 0.001). The gap in EBF for 6 weeks was 45 percentage points by racial group (13%—Black mothers versus 58%—White mothers, p < 0.001); in any BF at 6 months was 37 percentage points (28%—Black mothers versus 65%—White mothers, p < 0.001); and in mothers meeting their own intention to BF at least 6 months was 51 percentage points (29%—Black mothers versus 80%—White mothers, p < 0.001). Racial disparity in EBF at 6 weeks was mediated in logistic regression models by inequities in socioeconomic position, maternal hypertension, and BF intention. Racial disparities in BF at 6 months or meeting 6-month BF intention were mediated by inequities in socioeconomic position, maternal obesity, and EBF at 6 weeks. Not all BF disparities could be explained by models used in these analyses.
Conclusions: Efforts to lessen BF disparities should address the underlying structural inequities that disproportionately affect Black mothers and children, should incorporate maternal health, and focus on breastfeeding exclusivity and duration. Few Black mothers achieved EBF at 6 weeks, which contributed to disparity in BF duration. Greater attention to Black mother–infant pairs is a public health priority.
Keywords: breastfeeding, race, equity, health disparity, social determinants of health
Introduction
With sustained public health focus on breastfeeding (BF) in hospitals and communities over the past decades, breastfeeding rates have been steadily increasing in the United States. As of 2020, 84% of U.S. infants were ever breastfed, with 58% still breastfeeding at 6 months of life.1 While the United States has exceeded the 2020 Healthy People breastfeeding initiation goal of 81.5%, the Healthy People goals for breastfeeding duration and exclusivity have yet to be met, and beneath the overall 2020 national breastfeeding attainment lies a persistent disparity: Breastfeeding rates in the first 6 months of life have been reported to be 16–17% lower among non-Hispanic Black women compared with other U.S. populations.1–5
Disparity in breastfeeding by racial group raises a powerful call for equity, as lack of breastfeeding conveys immediate and long-term health risks to both mothers and infants. Lack of breastfeeding is associated with significantly increased infant morbidity due to a variety of infectious diseases and immune conditions, infant adiposity, and reduced cognitive development.5–8 Several studies report an association between lack of breastfeeding and increased infant mortality in the United States.9,10 There are also consequences for mothers: Lack of breastfeeding is associated with increased maternal postpartum blood loss, risk of breast and ovarian cancer, and may lead to postpartum weight retention.6–8,11
To ultimately eliminate disparity between racial groups in breastfeeding outcomes, it is critical to delineate the mediating influences. Historically, Black mothers have had a lower intention to breastfeed associated with negative perceptions of breastfeeding, though recent qualitative research in Cincinnati and elsewhere indicates that many Black mothers hold positive attitudes and intention to breastfeed along with concerns about barriers and their ability to meet their goals.12,13 Black mothers have been marginalized, and have experienced less health system support for breastfeeding, fewer role models, and reduced exposure to evidence-based interventions that promote and enable breastfeeding due to structural racism.3,5,14 Black women in the United States are also disproportionately affected by conditions that can impair their pregnancy and breastfeeding outcomes, including hypertension, diabetes, obesity, low birth weight, and premature deliveries.15–19 Understudied in relation to racial disparities in breastfeeding in the United States are the profound racial differences in circumstance and social determinants of health, including stressors, home and workplace expectations, and socioeconomic resources, which are products of systemic racism and its policies. To respond to the need for research relevant to equity in breastfeeding, we analyzed longitudinal data from a CDC-sponsored birth cohort study conducted in Cincinnati, Ohio. Our aims were to compare breastfeeding patterns in non-Hispanic Black and White mothers in the first 6 months of life and identify underlying contributors that may mediate breastfeeding disparities.
Methods
Study design
This is a secondary analysis of the PREVAIL (Pediatric Respiratory and Enteric Virus Acquisition and Immunogenesis Longitudinal) cohort, a prospective, observational study of mother–child pairs in Cincinnati, Ohio. The cohort included generally healthy mothers and child pairs followed actively from the third trimester of pregnancy until the child's second birthday. This study was reviewed and approved by Institutional Review Boards (IRB) at the CDC, Cincinnati Children's Hospital Medical Center (CCHMC) and the hospitals where maternal enrollment and delivery occurred. The overall study methods are described elsewhere20; here we provide a description of study methods relevant to this analysis.
Enrollment
Study mothers were enrolled from March 2017 through July 2018 in obstetrical clinics associated with the two study birth hospitals, University of Cincinnati Medical Center (UCMC) and The Christ Hospital (TCH) in Cincinnati, Ohio. The UCMC is a public hospital that is certified as a Baby-Friendly Hospital, and a participant in the CDC's Best Fed Beginnings program designed to support Baby-Friendly status.21 TCH is a private hospital that does not have Baby-Friendly Hospital status but has a “three-star” ranking from the Ohio First Steps for Healthy Babies program, which recognizes facilities with one star for every two of the Ten Steps to Successful Breastfeeding achieved.22
Mothers were screened for eligibility based on medical records. Eligible pregnant women who were at least 34 weeks of gestation were approached during an outpatient obstetric visit and invited to participate. Enrollment required written, informed consent. Inclusion criteria for enrollment included singleton pregnancy, maternal age ≥18 years, and delivery at either study hospital. Participation also required a cell phone that could be used for text messaging to maintain communication. Exclusion criteria were living more than 20 miles from the birth hospital, illicit drug use, HIV infection, delivery of multiples, stillborn infant, a major congenital anomaly, and failure to participate in the week 2 postnatal research visit.
Based on review of obstetrical records, 1,206 pregnant women were identified as potentially eligible for inclusion. Screened patients were 50% Black race, 47% White race, and 3% “other race,” which were largely Asian, with a few Native, Pacific Islanders, or unspecified. Only 27 (2%) potentially eligible subjects were identified as Hispanic. Of the potentially eligible, 265 pregnant women consented to participate before delivery and 245 met the postpartum criteria to complete enrollment. Among the 245 enrolled mothers, 104 (42%) self-identified their race/ethnicity as non-Hispanic Black, 126 (51%) as non-Hispanic White, and 9 (4%) as non-Hispanic and biracial, Asian, Native or Pacific Islander. Only six (2%) mothers identified as Hispanic, of whom three were Black race, one was White race, and two did not specify their race. This racial and ethnic distribution was similar to that identified at initial subject screening, with somewhat higher representation of Black mothers and lower representation of White mothers compared to the region. For this secondary analysis, we excluded the 15 enrolled mothers who identified as biracial, Asian, Native, Pacific Islander or Hispanic, due to their low numbers, and an additional 25 enrolled mothers who failed to complete the month 6 visit. This left a total of 205 study mothers in the current analysis, 92 (45%) Black race and 113 (55%) White race.
Data collection
During the prenatal enrollment visit, a baseline questionnaire was administered to mothers regarding their breastfeeding intentions, race and ethnicity, health, and factors influencing their socioeconomic position. Socioeconomic position is defined as the range of social and economic factors that influence what positions individuals or groups hold within the structure of a society.23,24 Breastfeeding intention was asked using a previously published and validated instrument, with a 5-point Likert scale ranging from “very much agree” to “very much disagree” regarding mothers' intention to initiate exclusive breastfeeding (EBF) and to continue EBF at least 1, 3, or 6 months.25 Household composition questions determined the total number of persons in the household. Socioeconomic position questions included family annual income and insurance status, defined as public or private, with mothers reporting both classified as public. Mothers were asked to self-identify their race as White, Black, Asian, Pacific Islander, Native American, or Other, and as Hispanic or non-Hispanic ethnicity.
During postnatal research visits at weeks 2 and 6 and month 6, participants were administered standardized questionnaires in person. At month 4, participants were contacted and administered an interim questionnaire by phone. The series of questionnaires were used to determine any change in breastfeeding, health status, residence, or contact information. Breastfeeding status was self-reported by study mothers on each questionnaire for the interval preceding the current time point (birth–week 2, week 2–week 6, week 6–month 4, and month 4–month 6). Mothers who previously reported breastfeeding were asked about whether their feeding practice had been EBF, defined as feeding human milk without the addition of any infant formula during the study interval; partial breastfeeding, any combination of human milk and formula feeding during the interval; or exclusive formula feeding, defined as no human milk fed during the interval. Within this definition, mothers who had reported partial breastfeeding in a previous interval could return to EBF status if no supplemental formula was given during the interval in question. When breastfeeding ceased, the date of cessation was recorded. Maternal work status was also self-reported at the research visits, indicating whether or not the mother had worked outside of the home during the interval between clinic visits. Workplace breastfeeding behaviors were not investigated in this study.
After mothers were enrolled in the study, their obstetrical and health histories, including weights and heights, were abstracted from hospital records by the obstetrics team. Body mass index (BMI) was calculated as kg/m2 using the weight from the obstetrics record and presence of obesity was defined as a BMI of ≥30. Maternal weight was recorded in the first trimester for most (88%) mothers. When this time point was not available, the prepregnancy weight was used. The proportion of mothers whose weights were recorded in prepregnancy or in the first trimester of pregnancy was not associated with maternal race or obesity status.
Data management
Study data were entered directly into the REDCap database26 by study staff. The REDCap database system included logic checks at the point of data capture. Data management staff systematically reviewed completed questionnaires to ensure completion of missing data and verification or correction of improbable values.
Neighborhood ecological socioeconomic position was quantified using the Deprivation Index,27 a validated measure of neighborhood (census tract-level) socioeconomic position that was determined for the residence of each mother. The Deprivation Index uses six U.S. census Bureau American Community Survey28 measures, including percentage of homes in the tract that are vacant, median home value, the fraction of the population without a high school diploma, who have used any government social-services or income support within 12 months, without health insurance, and who meet the federal definition of poverty. The scores for each tract were standardized into a scale between 0 and 1, with increasing score representing increasing neighborhood deprivation. Current maternal residential addresses were geocoded using DeGAUSS software29 to the corresponding U.S. census tract and assigned a Deprivation Index score.
Statistical considerations
Descriptive analyses were undertaken to compare socioeconomic determinants (Table 1) with the breastfeeding patterns of Black and White mothers over the first 6 months after delivery. Sankey diagrams30 were used to visualize the flow in change in breastfeeding status between EBF, partial breastfeeding, and exclusive formula feeding at each study visit. Fisher's exact test was used to compare socioeconomic, demographic, and breastfeeding support and intention factors in relation to race and breastfeeding outcomes.
Table 1.
Characteristics of the 205 Black and White Mothers Enrolled in the PREVAIL Cohort from Birth to 6 Months
| Maternal–Infant characteristic | Description | Black (n = 92), n (%) | White (n = 113), n (%) | p |
|---|---|---|---|---|
| Health-related factors | ||||
| Maternal age, years | 18–24 | 27 (29.4) | 9 (8.0) | <0.001 |
| 25–34 | 52 (56.5) | 80 (70.8) | ||
| ≥35 | 13 (14.1) | 24 (21.2) | ||
| First child (primiparous) | Yes | 31 (33.7) | 55 (48.7) | 0.026 |
| No | 61 (66.3) | 58 (51.3) | ||
| Delivery mode | Cesarean | 33 (35.9) | 45 (39.8) | 0.674 |
| Vaginal | 59 (64.1) | 68 (60.2) | ||
| Diabetesa | Yes | 14 (15.2) | 21 (18.8) | 0.588 |
| No | 78 (84.8) | 92 (81.2) | ||
| Hypertensiona | Yes | 27 (29.3) | 19 (16.8) | 0.035 |
| No | 65 (70.7) | 94 (83.2) | ||
| Obese (prepregnancy) | Yes | 63 (68.5) | 33 (29.2) | <0.001 |
| No | 29 (31.5) | 80 (70.8) | ||
| Preterm delivery | Term (37–42 weeks) | 85 (92.4) | 110 (97.4) | 0.191 |
| Preterm (35–36 weeks) | 7 (7.6) | 3 (2.7) | ||
| Infant birthweight, g | <2,500 | 10 (10.9) | 2 (1.8) | 0.019 |
| 2,500–3,999 | 79 (85.9) | 104 (92.0) | ||
| ≥4,000 | 3 (3.3) | 7 (6.2) | ||
| Breastfeeding support and related factors | ||||
| Received breastfeeding counseling in pregnancy | Yes | 54 (58.7) | 53 (49.9) | 0.216 |
| No | 38 (41.3) | 60 (53.1) | ||
| Delivery hospital is Baby-Friendly | Yes | 66 (71.7) | 35 (31.0) | <0.001 |
| No | 26 (28.3) | 78 (69.0) | ||
| Worked outside the home | By 6 weeks postpartum | 16 (17.4) | 12 (10.6) | <0.001 |
| >6 weeks to 4 months | 37 (40.2) | 77 (68.1) | ||
| After 4 months if at all | 39 (42.4) | 24 (21.2) | ||
| Marital status | Married/part of a couple | 37 (40.2) | 104 (92.0) | <0.001 |
| Single/divorced/separated | 55 (59.8) | 9 (8.0) | ||
| Breastfeeding intention | ||||
| Intended to initiate BF | Yes | 76 (82.6) | 106 (93.8) | 0.014 |
| No | 16 (17.4) | 7 (6.2) | ||
| Intended to BF for 3 months | Yes | 44 (47.8) | 80 (70.8) | 0.002 |
| No | 48 (52.2) | 33 (29.2) | ||
| Intended to BF for 6 months | Yes | 41 (44.6) | 71 (62.8) | 0.011 |
| No | 51 (55.4) | 42 (37.2) | ||
| Socioeconomic position | ||||
| Maternal education | ≤ High school graduate | 72 (78.3) | 19 (16.8) | <0.001 |
| Beyond high school | 20 (21.7) | 94 (83.2) | ||
| Insurance type | Public | 89 (96.7) | 21 (18.6) | <0.001 |
| Private | 3 (3.3) | 92 (81.4) | ||
| Household income (annual) | <$25,000 | 53 (57.6) | 8 (7.1) | <0.001 |
| $25,000–49,999 | 24 (26.2) | 15 (13.3) | ||
| ≥$50,000 | 9 (9.8) | 88 (77.9) | ||
| Unknown | 6 (6.5) | 2 (1.8) | ||
| Residential neighborhood deprivation index | Quartile 1: Least deprived | 8 (8.7) | 50 (44.3) | <0.001 |
| Quartile 2 | 13 (14.1) | 36 (31.9) | ||
| Quartile 3 | 27 (29.4) | 23 (20.4) | ||
| Quartile 4: Most deprived | 44 (47.8) | 4 (3.5) | ||
Gestational and prepregnancy combined.
BF, breastfeeding; PREVAIL, Pediatric Respiratory and Enteric Virus Acquisition and Immunogenesis Longitudinal.
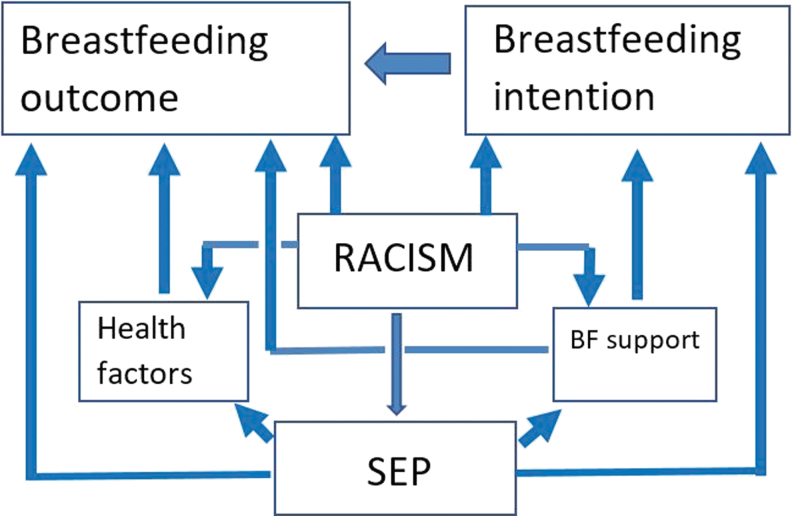
Mediation analysis was applied by conducting a series of logistic regression models.31 Mediators are not confounders or nuisance parameters but potential causal pathways, and in our analyses, they represent pathways of systemic racism. All variables listed in Table 1 were considered potential mediators of breastfeeding outcomes, as each were considered to have the potential to differ by race, occurred before breastfeeding, and could serve as the means by which race could influence breastfeeding outcomes.31 Evidence of racial disparity was taken as a significant (p ≤ 0.05) odds ratio (OR) signifying reduced breastfeeding outcomes associated with being Black, hereafter referred to as the disparity ratio. Multiple logistic regression was used to model the disparity ratio with other covariates in relation to EBF at 6 weeks, any breastfeeding at 6 months, and whether mothers who prenatally intended to BF a minimum of 6 months met their goal (Fig. 1). Variables were grouped by general mediator domains representing socioeconomic position, maternal–infant health characteristics, breastfeeding intention, and factors related to breastfeeding support. Income level was limited to <$50,000/year, as this represents the standard to which a family of four would qualify for most Federal aid. Mediation models compared logistic models of outcome by race only, the potential mediator by race only, and the outcome by race and the mediator to determine the average causal mediation effect (ACME) and the estimated percent mediation effect using a 1,000 simulation bootstrap approach.32 ACME represents the average indirect effect of the independent variable on the outcome through the mediator.
FIG. 1.
Conceptual model of the influence of structural racism on breastfeeding intention and outcomes. SEP, socioeconomic position.
Variables with a statistically significant ACME or a percent mediation effect above 10% were considered potentially causal and added into a full multiple regression model. In the event that two highly correlated mediators met inclusion criteria, the mediator with the higher percent mediation effect was used. All potential mediators not initially identified for inclusion in the multiple regression model were then added one at a time to the regression model to test its effect on the disparity ratio. Statistically significant mediators or mediators that altered the OR for Black race by ≥10% were kept and a final “best fit” regression model was fit. Finally, each regression model was modified by adding prenatal breastfeeding intention, EBF at 6 weeks, or both to determine the effect of prenatal intention and exclusivity on breastfeeding duration and meeting prenatal breastfeeding goals. All analyses were performed using R Statistical Software,33 with mediation analysis performed using the mediation package.34
For purposes of modeling, data were imputed for less than 5% of missing values for obesity or income data. Presence of obesity was imputed based on maternal age, race, and Deprivation Index quartile. Income category was imputed using the median income category of the subject's Deprivation Index quartile. Sensitivity analysis found no significant differences in the results for any models using the imputed data.
Results
Study population
All 205 women included in this analysis were enrolled from the same birth hospital-associated clinics and were active participants in the PREVAIL cohort. Nevertheless, Black mothers and White mothers differed in most of the health, support, intentions, and socioeconomic factors measured (Table 1). Black mothers were younger (p < 0.001), more likely to be multiparous (p = 0.026), hypertensive (p = 0.035), and to deliver a low birthweight infant (<2,500 g, p = 0.019) compared to White mothers. The 12 low birthweight infants in this study had a median hospital stay of 4 days, which did not differ by maternal race (p = 0.30). Obesity was greater in Black mothers than in White mothers (66% versus 29%, p < 0.001), though both groups had similar prevalence of diabetes (17%) and Cesarean section delivery (38%).
While enrollment was evenly split between study hospitals, mothers delivering at the Baby-Friendly-certified public hospital, UCMC, were more likely to be Black (69%), publicly insured (67%), and have an income below $50,000/year (66%, all p < 0.001). Black mothers reported work outside of the home before 6 weeks postpartum more often than White mothers, but only 15% of all mothers met this criterion, which did not reach statistical significance (OR 1.8, p = 0.220). Black mothers were 17 times more likely to be single or divorced (p < 0.001) and to have not completed any studies past high school (p < 0.001). Only about half of Black and White mothers reported to have received breastfeeding counseling during pregnancy, with no significant difference by race.
Socioeconomic position differed profoundly between Black and White mothers. Annual household income below $50,000 was reported by 84% of Black mothers but only 20% of White mothers (p < 0.001). Health insurance type was public for 97% of Black mothers but only 19% of White mothers (p < 0.001). Black mothers were far more likely than White mothers to be living in the most socioeconomically deprived (quartile 4) neighborhoods (48% versus 4%, p < 0.001) and far less likely to be living in the least deprived (quartile 1) neighborhoods (9% versus 44%, p < 0.001).
Breastfeeding patterns
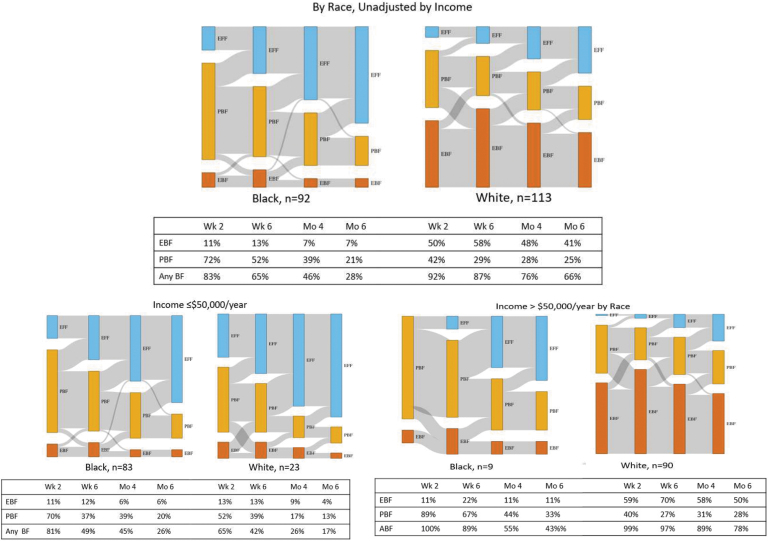
Breastfeeding intentions (Table 1) differed between Black and White mothers, specifically, intention to ever breastfeed (p = 0.014), intention to breastfeed to 3 months (p = 0.002), and intention to breastfeed to 6 months (p = 0.011). The breastfeeding outcomes for Black and White mothers (Fig. 2) differed significantly at all time points (p < 0.001), with the percentage point disparity being the smallest at the time of breastfeeding initiation and worsening over time. The flow toward increasing exclusive formula feeding was found most dramatically in Black mothers. The Sankey diagram transitions between visits indicate that mothers typically transition from exclusive to partial breastfeeding and then to exclusive formula feeding, and that the transition to exclusive formula feeding happens more rapidly among Black mothers and low income White mothers due to their lower EBF.
FIG. 2.
Sankey diagram and table of breastfeeding mode frequencies comparing Black and White mothers over the first 6 months of life. In this Sankey diagram (18), bars represent the relative frequency of the infant feeding behaviors at four time points, left to right: Week 2, week 6, month 4, and month 6. EBF is represented in dark orange, PBF in dark yellow, and EFF in blue. The gray lines between bars indicate the proportion of individuals who transition from one infant feeding state to another across the time points measured. EBF, exclusive breastfeeding; EFF, exclusive formula feeding; PBF, partial breastfeeding.
At week 6 postpartum, EBF was at its peak, yet exhibited a 45-percentage point disparity: 13% among Black mothers and 58% among White mothers (p < 0.001). Any breastfeeding was also significantly (p < 0.001) lower among Black mothers when compared to White mothers at all time points. Among Black mothers, breastfeeding initiation was reported by 83%; continued breastfeeding was reported by 65% at the week 6 visit, 46% at the month 4 visit; and 28% at the month 6 visit. Among White mothers, breastfeeding initiation was reported by 92%; continued breastfeeding was reported by 88% at the week 6 visit, 74% at the month 4 visit; and 66% at the month 6 visit.
In addition to being less likely to intend breastfeeding and to have lower EBF and breastfeeding duration, Black mothers were less likely to be able to meet their own breastfeeding goals. For example, of the 41 Black mothers and 71 White mothers who indicated the intention to breastfeed to at least 6 months, only 12 (29%) Black mothers compared to 57 (80%) White mothers met their prenatal goal (p < 0.001).
Mediation analysis
We found a number of factors, including breastfeeding intention, support, health, and socioeconomic position variables, to be potential mediators of the Black-White disparity ratio for our primary outcomes (Table 2). In relation to EBF at 6 weeks, the strongest mediators were socioeconomic position factors; the percent of disparity explained ranged from 45% to 72% for maternal education, private versus public insurance, and household income. Individual variables that each explained 14–19% of the Black-White disparity in EBF at 6 weeks included breastfeeding intention, and support-related variables (delivery hospital being Baby-Friendly or not, and being married or part of an unmarried couple). Delivery of a low birthweight infant explained 10% of the disparity, and maternal history of hypertension explained 6% of the disparity in EBF at 6 weeks.
Table 2.
Potential Mediators of Black-White Disparity Identified from Logistic Regression Models
| Type of factor | Potential mediator | EBF at 6 weeks, n = 205 |
BF at 6 months, n = 205 |
Met 6 months intention to BF, n = 112a |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ACMEb | Effect,c | p | ACME | Effect, % | p | ACME | Effect, % | p | ||
| Intention | BF initiation | −0.07 | 15.9 | 0.01 | −0.063 | 16.9 | 0.006 | — | — | — |
| Intention | BF to 3 months | −0.062 | 13.9 | 0.004 | −0.071 | 18.9 | 0.01 | — | — | — |
| Intention | BF to 6 months | −0.008 | 16.0 | 0.05 | −0.053 | 16.6 | 0.04 | — | — | — |
| Support | Baby Friendly Hospital | −0.062 | 13.5 | 0.036 | −0.050 | 13.1 | 0.098 | 0.013 | −2.6 | 0.73 |
| Support | Married/part of a couple | −0.076 | 16.6 | 0.11 | −0.022 | 6.0 | 0.55 | −0.0056 | 1.1 | 0.91 |
| Health | Hypertension | −0.028 | 6.1 | 0.060 | −0.016 | 4.3 | 0.080 | −0.005 | 1.1 | 0.45 |
| Health | Obesity | −0.013 | 2.9 | 0.630 | −0.083 | 21.7 | 0.006 | −0.12 | 22.9 | 0.020 |
| Health | Low birthweight | −0.043 | 9.5 | 0.016 | −0.018 | 4.8 | 0.086 | −0.056 | 11.1 | <0.001 |
| SEP | >HS education | −0.213 | 45.9 | <0.001 | −0.213 | 42.4 | 0.002 | −0.038 | 7.4 | 0.650 |
| SEP | Private insurance | −0.32 | 71.5 | <0.001 | −0.368 | 91.4 | <0.001 | −0.16 | 31.0 | 0.390 |
| SEP | Income <$50,000/year | −0.215 | 46.0 | <0.001 | −0.215 | 56.5 | <0.001 | −0.072 | 14.1 | 0.330 |
Bold value indicates p < 0.05.
Includes only the 112 subjects who prenatally indicated an intention to breastfeed at least 6 months.
The ACME represents the average difference in the regression coefficient for race due to the presence of the mediating variable.
Effect represents the percentage of the race effect that is mediated by the presence of the mediating variable.
ACME, average causal mediation effect; BF, breastfeeding; EBF, exclusive breastfeeding; HS, high school; SEP, socioeconomic position.
In relation to any breastfeeding at 6 months, we again found socioeconomic position factors to have the largest mediating influence, greater than 40%—maternal education, private versus public insurance, and household income. The other major mediator of breastfeeding to 6 months was maternal obesity, which explained 22% of the Black-White breastfeeding disparity, while breastfeeding intention and delivery at the Baby-Friendly hospital each explained 13–19% of the Black-White breastfeeding disparity. Maternal hypertension and having a low birthweight infant each explained 4–5% of racial disparity in any breastfeeding at 6 months. Finally, in relation to mothers meeting their own intention to breastfeed to 6 months, the only significant mediating factors were maternal obesity, which explained 23% of the Black-White disparity, and delivery of a low birthweight infant, which explained 11% of the Black-White disparity.
In crude logistic regression models, the Black-White disparity ratio was extremely strong, indicating that Black mothers were 9 to 10 times less likely to exclusively breastfeed to 6 weeks, continue any breastfeeding to 6 months, or meet their own goal to breastfeed for 6 months (p < 0.001, model 1, Table 3). However, in multiple logistic regression models that included the potential mediators listed in Table 2, the Black-White disparity ratio was lessened and no longer statistically significant (models 2 and 3, Table 3). The primary mediators of EBF at 6 weeks were socioeconomic position factors (maternal education and private versus public insurance), maternal hypertension, and breastfeeding intention to 3 months. In multiple logistic regression models of any BF at 6 months and meeting the prenatal 6 month BF intention (model 2, Table 3), private versus public insurance and obesity remained significant mediators. Once EBF to 6 weeks and intention variables were added to these models (model 3, Table 3), only obesity remained a significant predictor. Two factors that were found to be significant mediators in the univariate mediation analyses (Table 2), did not remain in multiple logistic regression models (Table 3); in some cases this might have been due to statistical collinearity with other factors (Baby Friendly Hospital) or insufficient numbers to support multiple regression (low birthweight).
Table 3.
Crude and Best Fit Multiple Logistic Regression Models
| Factors | EBF at 6 weeks, n = 205 |
BF at 6 months, n = 205 |
Met 6 months intention to BF, n = 112 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | p | OR | 95% CI | p | |
| Model 1: Crude | |||||||||
| Black-White | 0.11 | 0.05–0.21 | <0.001 | 0.19 | 0.10–0.35 | <0.001 | 0.10 | 0.04–0.24 | <0.001 |
| Model 2: Multiple Regression Best fit | |||||||||
| Black-White | 0.89 | 0.26–3.36 | 0.860 | 1.53 | 0.48–5.26 | 0.476 | 0.44 | 0.076–2.26 | 0.331 |
| Married/part of a couple | 1.49 | 0.50–4.41 | 0.464 | ||||||
| Hypertension | 0.40 | 0.15–1.00 | 0.054 | 0.69 | 0.29–1.59 | 0.394 | |||
| Diabetes | 0.52 | 0.14–1.87 | 0.218 | ||||||
| C section | 0.60 | 0.22–1.57 | 0.306 | ||||||
| Obesity | 0.80 | 0.37–1.77 | 0.570 | 0.32 | 0.15–0.66 | 0.002 | 0.36 | 0.12–0.92 | 0.033 |
| Low birthweight | 0.21 | 0.01–1.29 | 0.160 | ||||||
| >HS education | 3.44 | 1.27–9.43 | 0.015 | 2.01 | 0.76–5.27 | 0.155 | |||
| Private insurance | 4.09 | 1.27–14.00 | 0.019 | 5.82 | 1.93–19.51 | 0.002 | 4.04 | 0.71–21.19 | 0.096 |
| Highest deprivation index |
|
|
|
1.44 |
0.53–4.07 |
0.479 |
|
|
|
| |
Intention to BF to 3 months |
Intention to BF to 6 months and EBF to 6 weeks |
EBF to 6 weeks |
||||||
| Model 3: Best fit modela | |||||||||
| Black-White |
0.88 |
0.24–3.53 |
0.855 |
1.88 |
0.45–8.51 |
0.393 |
0.68 |
0.09–5.05 |
0.703 |
| Married/part of a couple |
1.70 |
0.56–5.19 |
0.346 |
|
|
|
|
|
|
| Hypertension |
0.36 |
0.13–0.96 |
0.044 |
1.00 |
0.35–2.81 |
1.0 |
|
|
|
| Diabetes |
|
|
|
|
|
|
0.33 |
0.06–1.58 |
0.182 |
| C section |
|
|
|
|
|
|
0.82 |
0.25–2.61 |
0.741 |
| Obesity |
0.71 |
0.31–1.63 |
0.417 |
0.18 |
0.07–0.46 |
<0.001 |
0.35 |
0.10–1.18 |
0.090 |
| Low birthweight |
|
|
|
0.29 |
0.01–2.00 |
0.292 |
|
|
|
| >HS education |
2.82 |
0.96–8.32 |
0.057 |
1.14 |
0.33–3.76 |
0.834 |
|
|
|
| Private insurance |
3.44 |
0.95–13.08 |
0.063 |
3.34 |
0.82–14.48 |
−0.095 |
1.95 |
0.26–13.82 |
0.500 |
| Highest deprivation index |
|
|
|
2.33 |
0.68–8.24 |
0.181 |
|
|
|
| EBF to 6 weeks |
|
|
|
14.13 |
5.70–38.21 |
<0.001 |
21.67 |
6.57–89.16 |
<0.001 |
| Intention to BF ≥3 months |
5.52 |
2.43–13.35 |
<0.001 |
|
|
|
|
|
|
| Intention to BF ≥6 months | 5.47 | 2.33–13.62 | <0.001 | ||||||
The model 3 best fit model includes the same variables as model 2, but with the addition of EBF to 6 weeks or intention variables, as indicated for each column.
Bold text represents the significant values (p < 0.05).
BF, breastfeeding; CI, confidence interval; EBF, exclusive breastfeeding; HS, high school; OR, odds ratio.
Discussion
Black women continue to have the lowest rates of breastfeeding in the United States, compared with women from all other racial/ethnic groups. Although breastfeeding rates continue to improve, the disparity in breastfeeding among Black women has continued for decades.4 The PREVAIL birth cohort includes infants born in 2017 and 2018 in Cincinnati, Ohio. In the analysis of this cohort, we used a longitudinal approach to compare breastfeeding patterns of non-Hispanic Black and White women from birth to 6 months, and we considered a number of factors involved in breastfeeding intention and support, maternal–infant health, and socioeconomic position as potential mediating or explanatory factors.
In our cohort, breastfeeding initiation was 83% in Black women, and 92% in White women, a modest disparity of 9 percentage points, but a rapid drop-off in breastfeeding was observed: Only 28% of Black mothers compared to 65% of white mothers continued breastfeeding to 6 months, a disparity of 37 percentage points. And, at 6 weeks of infant age, EBF was reported by only 13% of Black women, compared to 58% of White women, a disparity of 45 percentage points.
Intention to breastfeed follows a similar pattern to actual breastfeeding behavior. The racial disparity in intention to ever breastfeed is only 11 percentage points, whereas the disparity in intention to breastfeed to 6 months is larger, 18 percentage points (Table 1). While for Black women, intention to breastfeed to 6 months far exceeded the practice of breastfeeding at 6 months, for White women, there was only a small gap between intention and practice. It is a disturbing disparity that Black women face persistent barriers in meeting their own goals for breastfeeding duration.
Measures of socioeconomic position—maternal education, public/private insurance, household income, or the deprivation index of the mother's neighborhood—strongly mediated the Black-White disparity in breastfeeding outcomes in our cohort. Our findings regarding the importance of socioeconomic position are consistent with national data analyzed by Li et al., who found that controlling for income reduced the Black-White breastfeeding disparity.4 Our analysis differs by treating socioeconomic position factors not as confounders, but as potential mediators of racial disparity. Nevertheless, the relationship between race, income, and breastfeeding is complex. Although sample size limits inference, higher income alone did not appear to strongly influence EBF among the 9 Black women when compared to the 90 White women in the >$50,000 income bracket (Fig. 2).
Racial disparities in maternal health also mediated racial disparity in breastfeeding outcomes: Greater frequency of hypertension in Black mothers appeared to partially mediate lower EBF at 6 weeks. Greater frequency of obesity in Black mothers strongly mediated disparities in breastfeeding at 6 months. Breastfeeding intention also differed by race and mattered for BF and EBF outcomes. Disparity in EBF at 6 weeks strongly influenced disparity in breastfeeding duration. Each of these factors interrelate in the complex causal web that is systemic racism. For example, higher obesity and hypertension in Black mothers also have underpinnings in systemic racism.
Mediation modeling indicated that for some outcomes, notably, breastfeeding at 6 months, the adjusted Black-White disparity ratio was well above 1.0, suggesting that if socioeconomic position and maternal health were equalized, breastfeeding durations might also equalize. However, for other outcomes, notably, EBF at 6 weeks and mothers meeting their own 6-month intention to breastfeed, the disparity ratio, while no longer statistically significant after adjusting for covariates, did not reach parity (OR = 1.0), suggesting that some of the racial difference remained unaccounted for by the variables measured and the models used.
Qualitative studies involving Black mothers help provide perspective. Based on focus groups conducted in Cincinnati, McClain reported that low-income Black mothers had positive attitudes and intentions toward breastfeeding initiation but were far less confident about breastfeeding at 3 and 6 months.12 Mothers frequently mentioned pumping and supplementing breast milk rather than exclusive feeding at the breast as they anticipated returning to work and/or school. Mention of pumping and supplement usage increased when mothers were asked about EBF. An ethnographic study conducted in northern California by Asiodu et al. reported that while half of the mothers intended to exclusively breastfeed, few mothers accomplished their goals due to life barriers and stressors.13 While these qualitative studies support our findings, the question remains: What are the structural inequities in the lived experiences of Black mothers that impedes BF, particularly EBF? Our current study is not designed to address this important question, nor does it address cultural issues such as attitudes toward the breast.
It is important to place our findings in context. Cincinnati has an informal coalition of academics and advocates to effect improvement in breastfeeding outcomes, which includes a regional quality improvement collaborative for improving the Joint Commission Perinatal Core Measure 05 for exclusive breast milk feedings. The forum provides an opportunity for representatives from multiple facilities, including the two study hospitals, to share ideas facilitating implementation of evidence-based breastfeeding practices. These hospitals participate in Ohio First Steps for Healthy Babies,17 a state-wide breastfeeding initiative, which recognizes progress in achieving the Ten Steps to Successful Breastfeeding through one star for every two steps achieved.16 UCMC, the certified Baby-Friendly Hospital in our study, met all Ten Steps and thus achieved a five-star ranking in Ohio First Steps. This achievement was enabled by UCMC's active participation in the CDC Best Fed Beginnings program. TCH, the other hospital in our study, instead focused on achieving a three-star ranking from the Ohio First Steps program in recognition of its adherence to six of the Ten Steps.
Baby-Friendly hospital practices are known to significantly improve breastfeeding exclusivity and duration.35,36 While racial disparities remain in maternal exposure to evidence-based practices that support breastfeeding,14 a large study of 33 hospitals in the southern United States found that launching the Baby-Friendly hospital program improved breastfeeding outcomes overall and significantly reduced Black-White disparities in breastfeeding.36 Similarly, we found a significant mediation effect on reduced Black-White disparities in EBF at 6 weeks associated with delivery at the Baby-Friendly hospital, but our cohort was limited in its ability to examine this question. The certified Baby-Friendly Hospital in our study was also the public hospital, and thus, correlated with race, insurance, and income, causing the birth hospital to be lost from multivariable regression models due statistical collinearity.
Prior research has also identified returning to work before 3 months postpartum as a predictor for early breastfeeding cessation.37 While return to work at any time point was not a significant predictor or mediator in our models, our analysis was limited by sample size; we did identify a trend in our data toward early return to work and reduced breastfeeding, consistent with the literature.
Racial differences in breastfeeding initiation and support are known to occur throughout the United States.2,4,14,36 That we did not find great racial differences in breastfeeding initiation or support should be interpreted in light of our region's continuing efforts to reach all women, particularly, low-income Black mothers. For three consecutive years, co-authors on this article and community groups have collaborated to host a regional conference to address racial inequities in breastfeeding and infant mortality.38 Ongoing outreach efforts to Black mothers in Cincinnati include a nonprofit organization, Breastfeeding Outreach to Our Beautiful Sisters (BOOBS),39 an academic-community partnership, All Moms Empowered to Nurse (AMEN),40 and a reproductive justice project, Queens Village/Cradle Cincinnati.41 Ongoing community efforts of these groups have engaged Black women prenatally and postnatally in a variety of ways, including social media and peer support with educational sessions to increase breastfeeding intention and initiation. The impact of these initiatives is evident with continued growth of each program and the increase in breastfeeding intention and initiation among low-income Black women served by these programs.38,39 Cincinnati is located within Hamilton County, and data obtained from the county health department42 indicates that between 2015 and 2019, the increase in breastfeeding initiation was greater for non-Hispanic Black mothers, 16 percentage points, compared to an increase of only 5 percentage points for non-Hispanic White mothers. We are encouraged that in Hamilton County, the 23 percentage points Black-White disparity in breastfeeding initiation reported in 2015 declined to a 12 percentage points disparity by 2019. Our experience suggests that community-based outreach, combined with hospital-based programs, such as is being undertaken in our region, can have impact and needs to be continued.
Our study cohort is representative of the mothers attending the clinics from which we recruited, but it is not fully representative of the Cincinnati (Hamilton County) population. Per 2019 census estimates,43 27% of Hamilton County Black families are below the poverty threshold (∼$26,000/year for a family of four), while about twice as many Black mothers in our cohort reported that level of household income. Conversely, 9% of the region's White families meet poverty criteria, close to the 7% of White families in our cohort who reported that level of income. Since we found socioeconomic position to be strongly associated with disparities in breastfeeding, these differences by race between the Greater Cincinnati population and our cohort may have inflated the crude (unadjusted) estimates of race on outcomes. However, the internal validity of our study remains, as does the importance of our findings about socioeconomic position and other mediating factors. Our study did not investigate work-related breastfeeding behaviors or barriers. Our study was also limited in measures of breastfeeding support, which included only questions about delivery hospital and whether mothers had received breastfeeding counseling in pregnancy. Furthermore, this study included only 205 mothers, which limited our ability to look at subgroups, such as higher income Black mothers. Nevertheless, the offset of these limitations are the comprehensive sets of factors measured and the longitudinal view of breastfeeding obtained from this cohort of study infants born in 2017–2018.
Conclusions
Our study of racial disparity in breastfeeding included a range of influences and has several key findings. First, the Black-White breastfeeding disparity is modest in initiation, but increases over time, with significant and large differences between races in exclusivity, duration, and the ability of mothers to meet their own breastfeeding goals. Second, Black mothers are significantly disadvantaged in socioeconomic position, which in turn contributes to racial disparities in breastfeeding. Third, racial disparities in maternal health—notably, obesity and hypertension—also appear to be key drivers in racial disparities in breastfeeding and deserve greater attention. Fourth, disparity in breastfeeding intention mediated about 15–19% of the Black-White disparity in BF in our cohort, supporting ongoing efforts to influence breastfeeding intention. Fifth, the Black-White disparity in EBF in turn contributes to disparity in breastfeeding duration. Finally, not all racial disparity was explained by the factors we measured.
Our findings support the notion that efforts to promote breastfeeding among Black mothers are succeeding in Cincinnati, similar to the U.S. overall, but more needs to be done. Efforts should focus on reducing the underlying systemic structural inequities that disproportionately affect Black mothers and children, address maternal health disparities and focus on increasing breastfeeding exclusivity and duration. Greater attention to breastfeeding and the overall health of Black mother–infant pairs should be a public health priority.
Acknowledgments
We gratefully acknowledge the participation of the PREVAIL birth cohort families. The authors also wish to thank our researchers at the University of Cincinnati, Cincinnati Children's Hospital, and The Christ Hospital–Cincinnati. We also gratefully acknowledge the hard work of the dedicated PREVAIL staff.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Disclosure Statement
Ardythe L. Morrow has research funding from FrieslandCampina and Abbott to study human milk components, and serves on the Scientific Advisory Boards of Biostime Institute for Nutrition and Care and Glycosyn LLC. No other authors have financial interests to disclose.
Funding Information
This work was funded by a cooperative agreement from the U.S. Centers for Disease Control and Prevention (IP16-004), the Molecular Epidemiology in Children’s Environmental Health Training program (Grant 5 T32 ES 10957-18), and the Center for Clinical and Translational Science and Training at the University of Cincinnati and Cincinnati Children’s Hospital Medical Center (Grant 2UL2TROO1425-05A1).
References
- 1.National Immunization Survey. Children born in 2019. [Internet]. Available at https://www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-socio-dem-2017.html (accessed October1, 2020)
- 2.Beauregard JL, Hamner HC, Chen J, et al. Racial disparities in breastfeeding initiation and duration among U.S. infants born in 2015. MMWR Morb Mortal Wkly Rep 2019;68:745–748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med 2015;10:186–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li R, Perrine CG, Anstey EH, et al. Breastfeeding trends by race/ethnicity among US children born from 2009 to 2015. JAMA Pediatr 2019;173:e193319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Louis-Jacques A, Deubel TF, Taylor M, et al. Racial and ethnic disparities in U.S. breastfeeding and implications for maternal and child health outcomes. Semin Perinatol 2017;41:299–307 [DOI] [PubMed] [Google Scholar]
- 6.Dieterich CM, Felice JP, O'Sullivan E, et al. Breastfeeding and health outcomes for the mother-infant dyad. Pediatr Clin North Am 2013;60:31–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartick MC, Jegier BJ, Green BD, et al. Disparities in breastfeeding: impact on maternal and child health outcomes and costs. J Pediatr 2017;181:49–55.e6 [DOI] [PubMed] [Google Scholar]
- 8.Ip S, Chung M, Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007:1–186 [PMC free article] [PubMed] [Google Scholar]
- 9.Chen A, Rogan WJ. Breastfeeding and the risk of postneonatal death in the United States. Pediatrics 2004;113:e435–e439 [DOI] [PubMed] [Google Scholar]
- 10.Ware JL, Chen A, Morrow AL, et al. Associations between breastfeeding initiation and infant mortality in an urban population. Breastfeed Med 2019;14:465–474 [DOI] [PubMed] [Google Scholar]
- 11.Baker JL, Gamborg M, Heitmann BL, et al. Breastfeeding reduces postpartum weight retention. Am J Clin Nutr 2008;88:1543–1551 [DOI] [PubMed] [Google Scholar]
- 12.McClain JS.Pregnant African American Women Breastfeeding Intentions, Beliefs Attitudes and Perspectives [dissertation]. ProQuest Dissertations Publishing, 2019 [Google Scholar]
- 13.Asiodu I, Waters C, Dailey D, et al. Infant feeding decision-making and the influences of social support persons among first-time African American mothers. Matern Child Health J 2017;21:863–872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sipsma H, Rabinowitz M, Young D, et al. Exposure to hospital breastfeeding support by maternal race and ethnicity: A pilot study. J Midwifery Womens Health 2019;64:743–748 [DOI] [PubMed] [Google Scholar]
- 15.Nommsen-Rivers LA, Chantry CJ, Peerson JM, et al. Delayed onset of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. Am J Clin Nutr 2010;92:574–584 [DOI] [PubMed] [Google Scholar]
- 16.Strapasson MR, Ferreira CF, Ramos JGL. Feeding practices in the first 6months after delivery: Effects of gestational hypertension. Pregnancy Hypertens 2018;13:254–259 [DOI] [PubMed] [Google Scholar]
- 17.Marshall NE, Lau B, Purnell JQ, et al. Impact of maternal obesity and breastfeeding intention on lactation intensity and duration. Matern Child Nutr 2019;15:e12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grobman WA, Parker CB, Willinger M, et al. Racial disparities in adverse pregnancy outcomes and psychosocial stress. Obstet Gynecol 2018;131:328–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belgrave FZ, Abrams JA. Reducing disparities and achieving equity in African American women's health. Am Psychol 2016;71:723–733 [DOI] [PubMed] [Google Scholar]
- 20.Morrow A, Staat M, DeFranco E, et al. The Pediatric Respiratory and Enteric Virus Acquisition and Immunogenesis Longitudinal (PREVAIL) cohort of U.S. mothers and their children 0–2years: Methods. JMIR Res Protoc 2021;10:e22222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baby Friendly USA [Internet]. Available at www.babyfriendlyusa.org (accessed October1, 2020)
- 22.Ohio Hospital Association [Internet]. Available at www.ohiohospitals.org (accessed October1, 2020)
- 23.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annu Rev Public Health 1997;18:341–378 [DOI] [PubMed] [Google Scholar]
- 24.Galobardes B, Shaw M, Lawlor DA, et al. Indicators of socioeconomic position (part 1). J Epidemiol Commun Health 2006;60:7–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nommsen-Rivers LA, Cohen RJ, Chantry CJ, et al. The Infant Feeding Intentions scale demonstrates construct validity and comparability in quantifying maternal breastfeeding intentions across multiple ethnic groups. Matern Child Nutr 2010;6:220–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brokamp C, Beck AF, Goyal NK, et al. Material community deprivation and hospital utilization during the first year of life: An urban population–based cohort study. Ann Epidemiol 2019;30:37–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Community Survey [Internet]. Available at https://www.census.gov/programs-surveys/acs (accessed July5, 2020)
- 29.Brokamp C. DeGAUSS: Decentralized geomarker assessment for multi-site studies. J Open Source Softw 2018;3:812 [Google Scholar]
- 30.Rpubs—Communicating And Vizualizing Conraceptive Dynamics Data Using A Sankey Diagram [Internet]. Available at https://rpubs.com/YJ_Choi/PAA2020 (accessed October12, 2020)
- 31.VanderWeele TJ, Robinson WR. On the causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology 2014;25:473–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods 2010;15:309–334 [DOI] [PubMed] [Google Scholar]
- 33.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing Vienna, Austria [Internet]. 2018. Available at https://www.R-project.org/ (accessed October12, 2020)
- 34.Tingley D, Yamamoto T, Hirose K, et al. mediation: R Package for Causal Mediation Analysis. J Statist Softw 2014;59:1–38 [Google Scholar]
- 35.Jung S, Nobari TZ, Whaley SE. Breastfeeding outcomes among WIC-participating infants and their relationships to Baby-Friendly Hospital practices. Breastfeed Med 2019;14:424–431 [DOI] [PubMed] [Google Scholar]
- 36.Merewood A, Bugg K, Burnham L, et al. Addressing racial inequities in breastfeeding in the southern United States. Pediatrics 2019;143:e20181897. [DOI] [PubMed] [Google Scholar]
- 37.Langellier BA, Langellier BA, Pia Chaparro M, et al. Social and institutional factors that affect breastfeeding duration among WIC participants in Los Angeles County, California. Matern Child Health J 2012;16:1887–1895 [DOI] [PubMed] [Google Scholar]
- 38.Knox-Kazimierczuk F, Nommsen-Rivers L, Graham C, et al. Eliminating racial disparities in breastfeeding and infant mortality—A qualitative analysis of conference proceedings. Breastfeed Med 2018;13(Suppl 2):S38 [Google Scholar]
- 39.Breastfeeding Outreach for Our Beautiful Sisters (B.O.O.B.S.) [Internet]. Available at https://www.breastfeeding-boobs.com/ (accessed October29, 2020)
- 40.Ware JL, Love D, Ladipo J, Paddy K, et al. African American Breastfeeding Peer Support: All Moms Empowered to Nurse. Breastfeed Med 2021;16:156–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shockley-Smith M.Local Black Women in the Fight for Reproductive Justice. Cincinnati, OH: The Cincinnati Herald, 2020 [Google Scholar]
- 42.Ohio Department of Health (ODH). Ohio Public Health Information Warehouse Birth Data Set. 2006. –2019. “These data were provided by the Ohio Department of Health. The Department specifically disclaims responsibility for any analyses, interpretations or conclusions, prepared by Hamilton County Public Health”
- 43.Quick Facts. Hamilton County, OH [Internet]. Available at https://www.census.gov/quickfacts/hamiltoncountyohio (accessed October14, 2020)