Abstract
This paper explores and compares health system responses to the COVID-19 pandemic in Denmark, Finland, Iceland, Norway and Sweden, in the context of existing governance features. Content compiled in the Covid-19 Health System Response Monitor combined with other publicly available country information serve as the foundation for this analysis. The analysis mainly covers early response until August 2020, but includes some key policy and epidemiological developments up until December 2020.
Our findings suggest that despite the many similarities in adopted policy measures, the five countries display differences in implementation as well as outcomes. Declaration of state of emergency has differed in the Nordic region, whereas the emphasis on specialist advisory agencies in the decision-making process is a common feature. There may be differences in how respective populations complied with the recommended measures, and we suggest that other structural and circumstantial factors may have an important role in variations in outcomes across the Nordic countries. The high incidence rates among migrant populations and temporary migrant workers, as well as differences in working conditions are important factors to explore further. An important question for future research is how the COVID-19 epidemic will influence legislation and key principles of governance in the Nordic countries.
Keywords: Health policy and administration, Public health, Comparative Research, Governance, System level, influence legislation and key principles of governance in the Nordic countries
Introduction
The health systems in Denmark, Finland, Iceland, Norway and Sweden share a number of common features. They are predominantly tax financed and provide universal coverage to all residents. Health care is a public responsibility and there is a high degree of decentralized management through regional and local level governments. The decentralized governance takes place within a framework of national legislation and negotiated agreements to coordinate strategic policy aims.
The outbreak of the COVID-19 pandemic called for rapid public health responses to avoid spread of the infection and prevent COVID-19 related deaths, and the Nordic region was not an exception. The epidemiological situation has varied across the Nordic countries, which may reflect different policy responses as well as institutional structures. Differences may also reflect the resilience of health systems.
In the past, the structural commonalities have inspired many observers to argue that there is a distinct “Nordic model” of health care, sometimes labelled as an “integrated public corporatist model” [1] or a more decentralized version of the NHS in the UK [2]. Recently, the countries have chosen somewhat diverging paths with regards to the level of centralization or decentralization in the financing and provision of health services [3].
There are constitutional differences and divergence in the traditions of interaction between national governments, state agencies, and decentralized authorities across the five countries which influence the range of policies adopted in a public health crisis. Institutional structures set the boundaries for decision-making and limit the range of likely and possible choices. Institutional veto points and standard operation procedures may on the one hand indicate that radical changes are rare and require substantial external or internal shock to open the political window for action. In more recent contributions to the social science it has, however, been argued that transformations may also be the outcome of more evolutionary developments [4,5]. When studying the impact of the Covid-19 crisis for the healthcare systems it is therefore necessary to understand the context within each system.
The Swedish response to the COVID-19 pandemic has in particular been the subject of an intense academic, as well as political debate [6]. In contrast to most of the EU countries and the Nordic neighbors, the initial lack of more stringent policy measures made Sweden an outlier in terms of both the pandemic response as well as the initial impact on population health, with mortality rates markedly higher than in other Nordic countries [7].
The overall aim of this paper is to explore and compare the Nordic health systems’ responses to the COVID-19 pandemic in the context of governance features and provide insight into differences and similarities in terms of policy responses to the epidemiological situation. This overview not only contributes with comparable information on implementation of policy measures and outcomes, but analyses the role of governance mechanisms and the challenging balance between health policy advice and governmental decisions.
Methods
This analysis builds on the methodology and content compiled in the Covid-19 Health System Response Monitor (HSRM). The HSRM was established in March 2020 and designed to collect and disseminate up-to-date information on how countries, mainly in the WHO European Region, are responding to the crisis (see www.covid19healthsystem.org). The HSRM content is structured around standard health system functions [8], capturing policy responses related to governance, resource generation, financing, and service delivery, as well as measures to prevent transmission of the virus. The information is collected and regularly updated, enabling broad comparisons across countries.
The policy insights emerging from the Nordic countries – Denmark, Finland, Iceland, Norway and Sweden, is focused on the governance and legislation, as well as selected measures of preventing transmission.
The identification of key policy insights from country experiences followed a deliberative process that included extensive review of the HSRM materials and structured discussions among article co-authors, Observatory editors, and other experts. Where relevant, other country material, key documents and literature are used to inform the paper [9], [10], [11], [12], [13].
The aim was not to definitively answer why some countries have dealt better with the pandemic than others, but rather to draw out interesting patterns, key contrasts, and innovative approaches in policy responses aimed at addressing common challenges across countries. Indeed, attributing any causal link between policy response and pandemic outcome is fraught with methodological challenges. Rather, the analysis intended to describe governance and assess policy responses and draw out critical lessons. In turn, this can serve as a basis from which to begin discussions that eventually lead to an understanding of what seems to work, what does not work, and why. The analysis also intended to throw into relief current gaps in policy knowledge i.e. what we still need to know, which can open up areas for future research. Ultimately, this analysis aimed to provide policymakers with policy options as they design their own responses to current and future crises.
The analysis covers mainly the period from February 2020 until August 2020, but also comments on some key policy and epidemiological developments up until the end of December 2020.
Results
Current politics and political background
Denmark, Finland, Iceland, Norway and Sweden share many cultural, historical, social and welfare structure characteristics, and well-established political cooperation in the form of the Nordic Council and the Nordic Council of Ministers [14].
The Nordic countries, with a total population of 27.4 million, are all representative democracies, often led by minority coalitions. Over the course of 2020, Iceland and Finland had majority coalitions, whereas Norway and Sweden had minority coalitions and Denmark was governed by a minority party. Ideologically the governments varied from conservative (Norway), social-democratic in Denmark, and left-green with support of the center parties in Finland and Sweden and center-right parties in Iceland.
All governments had broad support for their initial responses to the pandemic in their respective parliaments as well as among the public. Criticism and political debate emerged in all countries in the late spring, with the easing of the restriction measures.
The development of the pandemic in the Nordic countries and the initial policy responses
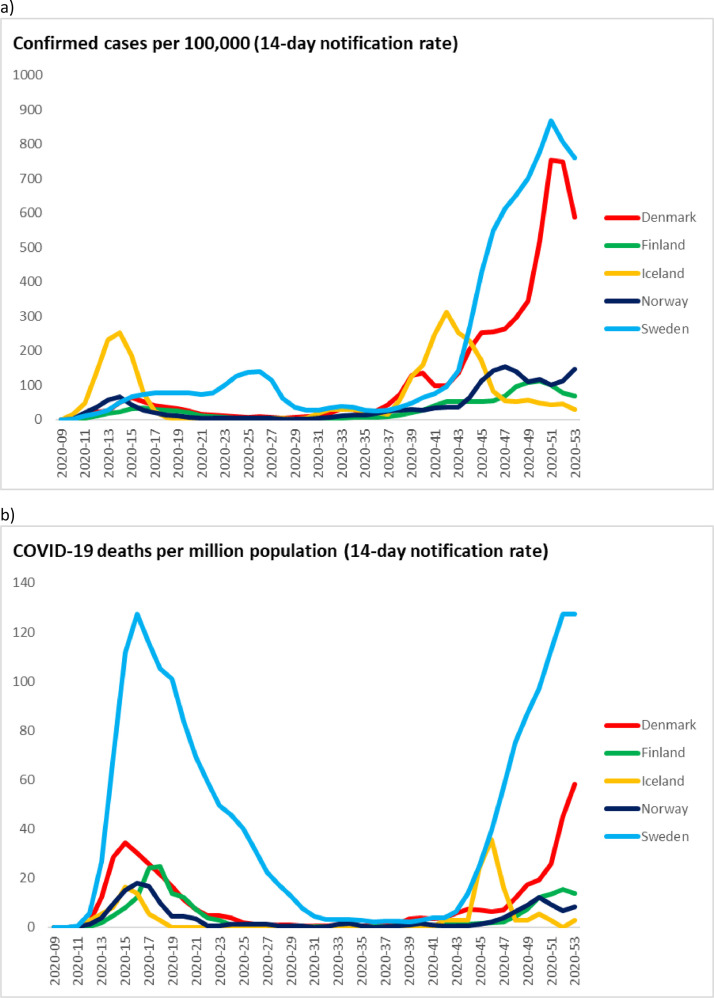
By the last week of February 2020, all five Nordic countries had registered their first COVID-cases. By mid-March Denmark, Finland, Iceland and Norway had implemented a number of strict policy measures such as closure of borders and schools, restriction on social gatherings and access to restaurants etc., whereas Sweden called for caution and remained open. The burden of the pandemic expressed in the number of cases and deaths has not been uniform across the region (Fig. 1 ).
Fig. 1.
Weekly number of COVID-19 cases per 100,000 population (a) and deaths per one million population (b) in the Nordic countries in the period March-December 2020.
Data limitations in terms of comparability of testing and mortality coding notwithstanding [15,16], Sweden appeared to be the outlier in terms of the high incidences rates and the number of COVID-19 deaths in 2020. In the end of July and until early September, the patterns in the Nordic countries became more similar with relatively low incidence rates, before they increased with varying degree in the beginning of autumn. Sweden and Denmark both experienced rapid increase in incident rates which they managed to curb in December 2020.
National legislation underpinning the COVID-19 response
Even though the legal systems in the Nordic countries share many commonalities, the degree to which new or pre-existing legislation allow implementation of strict measures varies. Legislative provisions for infectious disease control can be used to impose far-reaching restrictions on the citizens in order to prevent further spread of diseases. COVID-19 was listed as a communicable disease in the respective infectious disease acts by governmental decrees early in 2020 in all the Nordic countries. Likewise, national disaster or preparedness acts, when invoked, give the national governments extended emergency powers and the right to impose strict emergency regulations on their respective populations (Table 1 ).
Table 1.
Important legislation and pandemic plans underpinning initial COVID-19 response in the Nordic countries.
| Acts and regulations | Denmark | Finland | Iceland | Norway | Sweden |
|---|---|---|---|---|---|
| National Preparedness Acts | 1992 Emergency Management Act Not activated |
2011 The Emergency Powers Act (Activated March 2020) 1994 the Health Protection Act |
2008 Civil Protection Act Activated March 2020 |
1950 Emergency preparedness Act 2000 Emergency Health Preparedness Act Activated March 2020 |
2003 Civil Protection Act (on municipal responsibility) |
| Epidemic Acts | 2009 The Danish Epidemic Act Revised March 2020 (sunset clause March 2021) |
2016 The Communicable Diseases Act Revised several times 2020 |
1997 Act on Health Security and Communicable Diseases | The Act Relating to the Control of Communicable Diseases. Activated February 2020 Revised several times 2020 |
2004 Communicable Diseases Act Revised April 2020 (sunset clause June 2020) |
| COVID-Acts | Enforced 27 March (Sunset clause 27 May) |
||||
| National Emergency Plans | The National Emergency Management Plan 2015 | Regional contingency planning, coordinated at ministerial level | The general contingency plan | National health preparedness plan 2018 | |
| Pandemic Plans | The Pandemic Plan 2013 | National preparedness plan for an influenza pandemic 2013 | Pandemic and Influenza Preparedness Plan Updated 2020 | National plan control communicable diseases 2019 |
21 regional plans 2019 |
Iceland, Finland and Norway invoked national preparedness acts in March 2020. This empowered the government to make country-wide decisions on several restrictions. However, most of the measures were taken in the context of ordinary legislation giving regional/local authorities sufficient powers, such as issuing quarantine or closing public spaces. Additionally, Norway issued a Coronavirus Act (2020), authorising the government to carry out restrictive measures to address the effects of COVID-19.
Neither Denmark nor Sweden invoked a state of emergency in the spring 2020. For Sweden, the legal framework does not allow a declaration of a state of emergency due to a pandemic, but the Parliament has the power to institute new laws very rapidly in case of emergencies. Denmark and Sweden both imposed new policies during the COVID-19 by amending existing legislation. The Danish Epidemic Act (2019) allows the government to temporarily suspend specific rights and obligations outlined by other legislation, when it is necessary to prevent or contain a dangerous contagious disease or to maintain heath care capacity to provide health care services to citizens. In Sweden, a temporary legislation (amendment to Communicable Diseases Act) was invoked from mid-April until the end of June, empowering the government to impose restrictions on restaurants, bars, shopping malls, transportations, etc. in order to contain the spread. This was not utilized, but an amendment to the public order act was used to regulate the number of people permitted to gather in public spaces.
A Nordic Public Health Preparedness Agreement (2002) requires the countries to share information on measures that may influence the cooperation between the countries. This extends to relevant legislative measures, as well as the obligation to facilitate exchange of experiences, cooperation and competence building. The World Health Organisation's International Health Regulation (IHR) from 2005 is incorporated in the national legislation in all the Nordic countries [17]
Governance approaches in practice
During the COVID-19 response, the Nordic countries have been guided by the following principles in terms of emergency management, which are incorporated in national legislation [18]:
-
•
sector responsibility remains in the sector during crises;
-
•
emergency management should reflect standard procedures;
-
•
emergency management should be handled at lowest effective organisational level possible; and
-
•
authorities are responsible for cooperation and coordination with each other in terms of planning and management.
Formal responsibility for the development of policy responses to COVID-19 lies with the respective governments, while any change to the legislation must be adopted by the parliaments in all five Nordic countries, including in an emergency situation. The Ministers of Health are all heads of the ministerial departments (in the case of Finland there are two ministers of Health), and National agencies, subordinate to the Ministries of Health, act independent of their national governments. The ministries may steer them indirectly through instructions, missions and financing.
In Denmark, Finland, Norway, and Sweden the regulatory responsibility of advice on communicable diseases are located in the agencies responsible for monitoring and assessing the situation together with ECDC and WHO. In Iceland, the Chief Epidemiologist, advising and preparing recommendations to the Minister of Health, operates within the Directorate of Health, while the decision-making authority in response to pandemics is centralised and rests with the Minister of Health.
In Norway, the Directorate of Health is in charge of overall coordination of the health and care sector's efforts and implements the necessary measures during an emergency situation. In Sweden, the Public Health Agency (SPHA) with the Chief Epidemiologist, as in Iceland, is responsible for applying the infection control legislation at the national level. In Denmark, The Danish Health Authority and Statens Serum Institute (SSI) are responsible for monitoring and providing recommendations to the Minister of Health. In Finland, the national expert agency is the Finnish Institute for Health and Welfare (THL).
With the exemption of Iceland, regional or local authorities (with respective Chief Medical officers) are responsible for coordinating local policies and recommendations with the state agencies. They are also responsible for necessary precautions against transmission of disease, and the Chief Medical Officers have the power to enforce measures, such as testing and quarantine and/or isolation against individuals, to counter a public health crisis. The responsibility for securing bed and ICU capacity and handling COVID-19 in the hospitals lies in regional organisations in Denmark, Finland, Norway, and Sweden, while in Iceland the responsibility is at the national level.
National guidelines for handling the epidemics are provided in all countries, but the power of enforcing adherence to the guidelines varies with the status of the guidelines as either advisory or mandatory. This is reflected in the national preparedness plans for pandemics in Denmark, Finland, Iceland and Norway. In Sweden, where regions are responsible for handling the pandemic, there is not one national plan, but 21 regional preparedness plans. Regional/local preparedness plans are also present in the other Nordic countries, underpinned by a national plan.
During the first wave of the COVID-19 pandemic, all countries reported the same broad COVID-19 policy aims: to ensure sufficient capacity in the health care system; to prevent deaths due to COVID-19 and to prevent new cases. Broadly, the strategy was to contain and reduce the spread of the virus. Special considerations were given to protect older people and other vulnerable groups in all countries. There were also calls from the countries’ leaderships for solidarity to reduce the risk of infection spread and emphasis on voluntary effort, as all countries communicated a strong reliance on the public to follow the recommendations. Table 2 presents an overview of the main policy measures adopted at population level in all the Nordic countries from March through August 2020.
Table 2.
Selected preventive measures adopted at population level in the Nordic countries during the first 6 months (March through August 2020).
| Denmark | Finland | Iceland | Norway | Sweden | |
|---|---|---|---|---|---|
| Travel restrictions citizens/residents: | |||||
| - International/EU (leisure) | (X) | (X) | (X) | (X) | (X) |
| - Nordic (leisure) | (X) | (X) | (X) | (X) | X |
| - Quarantine upon (re)entry from high risk area | (X) | X | X | X | |
| Travel restrictions EU/EEA citizens– (entry) | |||||
| -Leisure/non-essential purpose | (X) | (X) | (X) | (X) | (X) |
| -Quarantine or negative test | (X) | (X) | (X) | (X) | |
| -Exceptions for migrant workers and other "worthy purposes" | (X) | (X) | (X) | X | |
| Internal mobility restrictions | |||||
| -travel across municipal/regional borders | (X) | (X) | (X) | (X) | |
| -curfew/mobility outside home | |||||
| Childcare and education: | |||||
| - closure of nurseries / kindergartens - remote education in lower primary school |
(X) X |
(X) |
(X) (X) |
||
| - remote education in middle/high schools | X | (X) | (X) | (X) | (X) |
| - remote post-secondary education (e.g. universities) | X | (X) | (X) | (X) | X |
| Recommendation to work from home | |||||
| -private businesses | X | (X) | (X) | X | X |
| -public sector (non-essential) | X | (X) | (X) | X | X |
| Restricting access for visitors | |||||
| -nursing homes and hospitals | X | X | X | X | X |
| Closing or restricting access to | |||||
| -restaurants and bars | (X) | (X) | X | (X) | (X) |
| -Retail shops (non-food) and non-essential retail services | (X) | ||||
| -indoor sports facilities | (X) | (X) | (X) | (X) | (X) |
| -cultural events (concerts, theatres, museums, spectator sports etc) | (X) | (X) | (X) | (X) | (X) |
| Maximum number of persons gathered at Public events | 10 | 10 | 10 | 5 | 50 |
| Maximum number of persons gathered in Private homes | 10 | 10 | 10 | 5 | 50 |
| Contact tracing | X | X | X | X | (X) |
| Self-isolation when infected | X | X | X | X | X |
| Physical distancing | 1 m | 2 m | X | 1m | 2m |
| Face mask required | (X) | (X) | (X) | (X) |
() = temporary + partial, bold=mandated by law, - Regular=recommendation; Physical distancing is highly recommended, whereas wearing a face mask is only recommended when physical distancing is not possible. For gatherings of persons the number is the lowest that have been recommended during the early phase of the pandemic. Source: authors
In the spring 2020, comprehensive national measures were taken in Denmark, Finland and Norway, where the strategy was to stop the spread of the virus by issuing the strictest policy measures taken in times of peace. It was enforced through restrictions on international travel, combined with reduced social interaction in the population (closure of non-essential businesses, schools, public events, etc.). Finland and Norway also had restrictions on internal mobility for a short period of time. It should be noted that curfews have not been imposed in any of the Nordic countries, and many educational facilities and businesses have remained in operation by converting to digital and remote work.
Successive re-opening phases started in late April, as concerns for businesses and the broader economy started to dominate policy discussions, shifting the aim towards controlling the spread of the virus. The gradual reopening prioritised the youngest children, allowing daycare centers and schools to resume activities (in Finland facilities for the youngest children remained open the whole period). School started to open on 15th April in Denmark and on 27th April in Norway. Finland reopened educational facilities on 13th May. In Norway, schools and daycare centers were open for children of essential health care personnel throughout the period and this was also the case for daycare centers for essential personnel in Denmark. In Iceland, childcare and compulsory schools (from 6 to 16 years of age) remained open, subject to infection control measures.
Sweden and Iceland introduced international, while recommending national, restrictions on mobility. In Sweden, the strategy was to issue recommendations aimed at the entire population, besides targeting recommendations for people aged 70+ and those with an underlying disease. High schools and universities were closed and a ban issued in March 2020 on assemblies of more than 50 persons (including for sport and music events) was upheld in the entire period. Museums and amusement parks were also closed.
Further recommendations included working from home if possible, and avoiding public transport, unless absolutely necessary. Non-essential travel from outside the EU/EEA was restricted following the EC recommendations. Later recommendations concerned banning visitors in care homes. In Iceland, people were advised not to travel to countries defined as high-risk zones by the Chief Epidemiologist.
The overall picture of population level measures shows many similarities, despite the more formal differences in instruments. The timing and enforcement of measures varies by country, such as when the limitations on visits to nursing homes were introduced. Internal travel restrictions have been limited in space and time, and lockdowns have not been as strict as in some other European countries, especially on rules for leaving the house. The internal travel ban was enforced more strongly in Finland and Norway, than in Denmark, Iceland and Sweden.
In Denmark and Norway, there have been a shift towards regional or local differentiation in measures based on the local levels of infection by the autumn of 2020. In Finland and Sweden, regional differentiation is the rule by default as it is based on the existing regulation.
Preventing transmission through testing, tracing and isolating
The common strategy across much of Europe for COVID-19 has been to ensure early diagnosis, isolation, as well as quarantining of cases in order to slow the spread as much as possible and to minimize the burden on health services. This is also known as the Find-Test-Trace-Isolate-Support strategy (FTTIS).
The testing capacity was extremely limited across the countries at the beginning of the pandemic. Initially, only people with severe symptoms and more vulnerable groups were referred to testing, followed by a strict testing priority of vulnerable groups and health personnel. With different speed, starting with Iceland, all Nordic countries managed to expand their testing capacity. Once demand for testing was matched, all Nordic countries have relied on incidence figures for municipalities/regions to make informed adjustment of preventive policies.
Regulations for contact tracing differ somewhat between the countries (Table 3 ), and have changed over time. In Denmark, individuals who tested positive for COVID-19 infection were initially requested to track down their own recent contacts. From 12th May 2020, the Danish Patient Safety Authority assumed responsibility for assistance in tracing close contacts. In Finland, Iceland and Norway, contact tracing has been in place since the onset of the epidemic. In Finland and Norway, regional/local authorities are responsible for contact tracing, and in Norway, Norwegian Institute of Public Health (NIPH) may assist in contact tracing and has the authority to obtain contact details about passengers in public transport. In Iceland, a specialised contact tracing team within the Civil Protection Department has the overall responsibility for contact tracing. Norway and Finland launched online educational courses for staff responsible for contact tracing at the local level. In Sweden, SPHA abandoned the strategy of contact tracing as a national level policy in mid-March due to the high number of cases in certain regions. Contact tracing was resumed as a national policy during the summer 2020.
Table 3.
Overview resources and measures for testing, tracing and isolating in the Nordic countries during the first 6 months (March through August).
| Denmark | Finland | Iceland | Norway | Sweden | |
|---|---|---|---|---|---|
|
Testing Resources |
Extremely limited, Sufficient by May 2020 Testing free |
Limited, sufficient by summer 2020 Public testing free |
Limited, sufficient from early spring 2020 | Extremely limited, Sufficient by May Testing free |
Extremely limited. Sufficient by summer 2020 |
|
Testing Local/ regional/ national |
Municipalities | Municipalities and hospital districts Private providers |
National | Municipalities Supported by NIPH | Regions |
| Tracing Apps | Yes, from June 2020 | Yes, from August 2020 | Yes, from April 2020 | Yes, from April. Abandoned June | No |
|
Quarantine Exposed |
Mandatory | Mandatory, Penalty upon violation | Mandatory | Mandatory | No |
| Isolation upon diagnosed with C-19 | Mandatory Penalty upon violation |
Mandatory Penalty upon violation |
Mandatory Penalty upon violation |
Mandatory Penalty upon violation |
Mandatory |
| Isolation upon diagnosed with C-19 | Mandatory | Self-isolation (voluntary) | Mandatory | Mandatory | Adviced |
|
Support Access to quarantine facilities free of charge |
Yes | Yes | Yes | Yes | No |
Mobile apps developed to detect close contacts were introduced in Iceland and Norway in April 2020, followed by Denmark in June and Finland in September. If an app user is diagnosed with COVID-19, other users who have been close contact are informed that they may have been exposed to COVID-19, without revealing the identity of the initial case. Privacy issues were raised about GPS-tracking and central storage of data in Norway, and the initial app use was discontinued. A new app, similar to the Danish one, was developed over the autumn 2020.
Isolation and quarantine are regulated by the infectious disease legislation in all the Nordic countries. Self-isolation is considered mandatory for all patients diagnosed with COVID-19, whereas quarantine is recommended in Sweden and mandatory in the other Nordic countries for people who have been exposed to the virus. Isolation can be enforced in all countries and the patient is entitled to benefits covering income losses. With the exemption of Sweden, isolation is also required for those who have been travelling in specified areas with widespread transmission. In Sweden, only travellers from abroad with symptoms of COVID-19 are advised to quarantine. The Nordic countries have closed their borders to all non-essential travel from countries outside EU/EEA with some exemptions. Denmark, Finland, Iceland and Norway have introduced voluntary testing for COVID-19 for passengers arriving from abroad.
The welfare system ensuring financial support in case of unemployment or sickness has been an important factor for adherence to these measures during the pandemic. In Denmark, Finland, Iceland and Norway, municipalities/health authorities are obliged to provide a place to stay for those who are unable to self-isolate at home, e.g. in hotels. Finland, Iceland and Norway have also defined levels of penalty involved for violation of the isolation rules.
Knowledge behind COVID-19 decisions
Political decisions have in general been informed by advice from the respective national agencies or committees. However, decisions have also been made without clear support or upon conflicting advice from the advisory bodies. Even though access to evidence-based knowledge and clinical guidelines is an important factor in the handling of the pandemic, it appears that ad-hoc independent commissions and expert groups have played an important role. The base for various decisions is not entirely clear.
In Denmark, political decisions are informed by advice from the Danish Health Authority and SSI. The advice is based on the best available evidence. In some cases, the national government has imposed harder restrictions than recommended by the health agencies due to political concerns and as a “cautionary principle”. This was particularly seen in the early phases, where the Danish Health Authority advised against closing borders, schools and day care facilities, since evidence pointed to limited preventive effects on transmission. Yet, the Government decided to impose lock down measures with some support from SSI. This example also illustrates occasional disagreement among the agencies, which have also been criticized for lack of transparency about data and prediction models.
In Finland, it has not been possible to fully assess the knowledge base for the decisions as the Government and the officials the Ministries and the Finnish Institute for Health and Welfare (THL) did not, in the beginning, publish all epidemiological models and other relevant evidence. However, there has been an aim to strive for evidence-based policies as the government has appointed a scientific panel to support the generation of evidence, as well as assembled a number of expert groups to support the governmental decision making [19].
In Iceland, policy decisions are published together with the recommendations from the Chief Epidemiologist and are reported to be based on the best available evidence. A governmental multisector steering group was established to monitor the social and economic impact of the public health responses to the COVID-19 pandemic, and also provide recommendations on policy measures. A council of seven experts appointed by the Minister of Health is overseeing policy and measures taken in response to communicable diseases.
In Norway, NIPH regularly publishes risk-response reports with strategic advice on handling the pandemic. The institute advised against the closure of schools and day care facilities, as well as the national travel ban imposed in the early stages of the pandemic. This was in conflict with the final advice given by the Directorate of Health as advised by the National Preparedness Commission. Information on the agenda and decisions processes in the preparedness commission have not been transparent. An independent expert commission was appointed to assess the socio-economic consequences of implemented policy measures.
The government in Sweden relaied on the principle of delegated authority (responsibility of advice on pandemics) which rests within the Swedish Public Health and Infectious Disease Control Agency.
There have been a number of expert groups appointed to give recommendations and propositions to the government. The Prime Minister's Office and different Ministries have published these, for various restrictive measures such as use of face masks.
Furthermore, Denmark, Finland, Norway and Sweden have all appointed independent national commissions to evaluate the entire course of the COVID-19 crisis. The commissions are set up to evaluate the preparedness for and handling of the COVID-19 pandemic as well as to report on transparency of policies.
Discussion
This paper presents a descriptive analysis of how the Nordic countries compared in terms of governance and policy measures in response to the COVID-19 pandemic at population level mainly from March until August 2020. By mapping legislation and the national governance of pandemic responses, the analysis shows that the initial use of regulatory instruments, as well as in governance of policies differed. The COVID-19 pandemic posed new challenges as it differs somewhat from scenarios described in influenza pandemic preparedness plans.
By the end of February 2020, COVID-cases were registered in all the Nordic countries. In March Finland, Iceland and Norway were in a state of national emergency. Denmark, Finland and Norway had issued a partial national lockdown, whereas Sweden called for caution and remained open.
Governance by recommendations rest on high levels of societal trust
All countries have strong central public administrations with agencies providing oversight and recommendations of pandemics. Measures in general have been similar across the countries (albeit with some variation in timing) and in most cases the authorities relied on recommendations rather than legislation. Recommendations were used to advice on working from home, limiting private and public social gatherings and traveling abroad. Sweden imposed some of the same measures, including transition to online teaching in high schools and universities and recommendations to work from home whenever possible. Policy measures introduced in the autumn of 2020 brought Sweden even closer to the approach adopted in the other Nordic countries.
The extensive reliance on recommendations led to fewer formal restrictions in the first phase of the pandemic in the Nordic countries compared with much of the EU/EEA. In general, the restrictions on internal mobility have been very limited in time and area. Bans on visits to nursing homes and hospitals were only enforced strongly in a few months. There have been no curfews or confinement to homes, with the exception of isolation and quarantine. Restrictions on mass gatherings have been implemented in all countries to reduce contact. Face masks for the population have only been required in specific places when physical distancing is not possible (bars, public transportation, hospitals, nursing homes, etc.).
The public in the Nordic countries generally express a high degree of trust towards fellow citizens and governments which has remained high during the pandemic [20], [21], [22], [23]. All the Nordic governments actively appealed to their population for collective action to fight the pandemic, and appear to have mostly succeeded [24,25]. National media have been perceived as surprisingly supportive of their respective governments in the initial phases [26].
Criticism and political debate have increased as the countries have moved from variations of lockdown towards gradual reopening. Denmark and Sweden are portrayed as two outliers; Danish media were initially perceived to be too consensus-oriented and supportive of national governance, whereas the Swedish media questioned politics and governance, thus fostering more public debate [27]. The latter is not surprising given that Swedish approach has attracted wide international attention.
Nordic countries varied in the use of state of emergency as a legal instrument to centralise power
Declaring a state of emergency allowed the governments’ access to legislative resources they do not possess under normal circumstances. The government temporarily gains the legal means to impose potentially far-reaching policy measures infringing on personal liberties, as well as overriding the decentralisation of power embedded in the governance of the Nordic health care systems. The European Convention of Human Rights (ECHR) safeguards the individual's rights, also against measures that can be invoked under public health epidemic legislation, such as freedom of movement between and within countries [28]. Declaring a state of emergency may be a way to sidestep these rights.
For Sweden, unlike in the other Nordic countries, declaration of a state of emergency limiting the individuals’ liberty is not a legal option in the case of a pandemic. This is in contrast to Iceland where declaration of emergency is a precondition in order to invoke the highest level of response in the contingency plans. Both Finland and Norway chose to declare a state of emergency early on, even though it is not clear whether it was a necessary course of action to implement measures taken. It is, however, clear that the use of emergency powers has limited the decentralised power embedded in the health care systems, and infringed patient rights such as the right to treatment within a specific time frame. Denmark has refrained from its use so far. The use or abuse of emergency powers are increasingly subject of public debate.
It has been argued that Norway and Finland have been more preoccupied with individual rights and constitutional aspects of the chosen policy measures during the pandemic, although in Denmark and Sweden such discussions have also surfaced. Another explanation for the differences in use of emergency powers may lie in the democratic tradition [18,26]. Even though a stronger tradition for the use of legislative measures might have a stronger foothold in some countries than others, it is not evident why an external shock like a pandemic triggered so different legal responses. Another explanation might be differences in emergency preparedness, where civil preparedness seems to have been less prominent on the political agenda in Sweden.
Efforts to coordinate operational and capacity issues, as well as implementation of measures across government levels have been substantial; however, there have been some ongoing challenges, reflecting the broadly decentralised nature of the Nordic health systems’ function. Denmark, Iceland and Norway have all established formal coordination commissions for emergency crisis response, which include relevant national level authorities from different sectors and other relevant stakeholders, in line with existing emergency preparedness plans.
Specialist advisory agencies and expert groups played a strong role in the decision-making, although with varying degree of transparency
Strategic decisions have been made at the national level by politicians, after consultation and advice presented by agencies and commissions, with the exemption of Sweden where the Public Health Agency has been at the centre of strategic decision making. In Norway, the Ministry of Health delegated the powers to the Directorate of Health until April 2020. Overall strategic goals are similar across the Nordic, emphasizing the need to protect vulnerable groups and hospital resources in order to maintain universal access to care. In addition there have been extensive use of ad hoc expert advisory groups and evaluations. These groups may function as a supplement to the existing governance structures, perhaps indicating a more general tendency to initiate expert advice to inform political consensus processes as a tool of support for the regular administration.
Countries faced different conditions for preventing transmission
Another important factor to consider when comparing onset and spread of the pandemic is the changing criteria and volume of testing in the countries. In the first months, the testing strategy only targeted people with obvious symptoms and health personnel at risk, whereas in the autumn testing was available for nearly all. Even though testing strategies were similar, capacity differed and caution should be taken in comparisons before the summer of 2020.
Rigorous contact tracing, followed by self-isolation and quarantine have been particularly strong in Iceland, Norway and Finland during the pandemic. The use of emergency powers ensured access to require hotels as quarantine facilities.
A number of pre-existing factors and chosen responses distinguished Sweden from other Nordic countries
Sweden has been an outlier in the burden of COVID-19 mortality and excess deaths compared to the other Nordic countries. As this analysis shows, there are differences in the legislative frameworks, which did not allow Sweden to declare a state of emergency, leaving the government with fewer instruments to use early on. In addition, responsibility for pandemic emergency planning is decentralised to the 21 regions, whereas in the other Nordic countries decentralised plans are governed by national plans. The level of decentralisation likely contributed to lack of consistency and intensity of response. One potential explanation is that fragmentation and diluted responsibilities between local, regional and state authorities left gaps in times of a crisis, that the government struggled filling fast enough, as expertise and analytical capacity are located in the agencies.
Other factors could also be at play in Sweden. First, there have been reports that herd immunity has been pursued as part of the strategy of handling the virus in Sweden [23]. While the government and SPHA has denied this, herd immunity was nevertheless seen as an outcome of wide societal spread, rather than an official goal, the agency seemed to underestimate the spread of the disease and the potential to halt the spread through strict measures. This could explain the authorities unwillingness to seek ways for stronger implementation of restrictions, in the initial phase of the pandemic. Other Nordic countries sought stricter measures of preventing the spread earlier, a more precautionary-based response of the direct effects of the pandemic. It should be noted that in Sweden a temporary legislation passed in the spring 2020, empowered the government to impose restrictions, such as temporary closure of shopping malls, but the government chose not to invoke it. As such, it was a political (in)decision. Second, a large number of COVID-19 fatalities occurred among residents in long term care settings, reflecting not only the high infection rates in general, but also structural weaknesses in this area (such as the high level of temporary staff not eligible for sickness benefits, larger-size institutions, widespread lack of PPE and guidance on possibility to ban visitors) have had an impact [27]. Finally, another early step, was to abandon contact tracing in the general population, which is considered to be an essential tool to control the spread of the virus [25]. This was explained by the lack of resources to cope with tracing when the incidence started rising rapidly in Stockholm area; however, SPHA hereby put less focus on continued tracing in other regions, where the number of cases was still low.
Conclusions
There have been an abundancy of research trying to link policy measures and outcomes, less research on the overall governance and resilience of health systems or impact of welfare system on the outcome of the pandemic. The welfare systems in the Nordic countries function as a safety net for the population, ensuring less devastating consequences and enables high level of trust.
Our findings suggest that despite the many similarities in policy measures between the five countries, there are also interesting differences in governance of the COVID-19 pandemic, and clear differences in outcomes so far. The differences in governance may be linked to different explanatory models. Sweden and Finland differ from Norway and Denmark in the degree of decentralization. Iceland, Finland and Norway are relying more on the formal legalization of measures than Denmark and Sweden. This analysis of governance is indicative of more diverse responses than anticipated, taken the common background and the common preparedness agreed upon in the Nordic council. This diversity in governance of health systems might reflect more generic response models installed in the different governments.
A common feature for Denmark, Finland, Iceland and Norway is the extensive use of expert advice in and outside the specialist agencies by the political leaders of the country, and reliance on a number of internal coordination fora between ministries, agencies and other relevant public authorities to facilitate a consensus-based development of policy measures. Sweden, on another hand, seems to have relied on technical expertise of the public health agency, with politicians distancing from the decision-making process. While regional/local authorities in Denmark, Finland, Iceland and Norway formally have the power to implement stricter measures when deemed necessary, this is usually coordinated with or even imposed by the national level. Swedish regional/local authorities in practice have more discretion to decide and implement policy measures under the guidance of SPHA.
It also seems plausible that a number of other structural and circumstantial factors have played an important role in variations in outcomes across the Nordic countries. In particular, it is relevant to further explore the importance of housing conditions, population density, and behaviour in particular population groups as potential explanatory factors. Both Denmark, Finland, Norway and Sweden have seen high incidence rates among migrant populations and temporary migrant workers. It should be noted that both Denmark and Sweden managed to curb high levels of infections in the population without enforcing a total lockdown after the initial phase.
Finally, there is a need to call for caution for when and how exceptional emergency powers are invoked. Denmark, Finland, Norway and Sweden have all appointed national commissions to evaluate the entire course of the COVID-19 crisis. The commissions are set up to evaluate the preparedness for and handling of the COVID-19 pandemic as well as to report on transparency of policies. It is a good time to question how the handling of the COVID-19 epidemic will influence future communicable disease control legislation and whether the current crisis have a lasting impact on the key principle of governance in the Nordic countries.
The findings here are based on an analysis of the early stages, and caution must be taken in the interpretation of the results. They do however point to important features of the health systems in the Nordic countries. It would be of interest to compare the Nordic countries’ response to other welfare or health systems, such as the UK or Germany, the states of New England or Kaiser Permanente in the US, the latter two being more of a comparable size.
Further research is necessary to determine the degree to which respective populations comply with the recommended measures. Even though the availability of comparable data within and across the countries are good in terms of testing, incidence rates, mobility and outcomes (COVID-19-related, as well as total mortality), little is known on how compliant the population is in following the advice and regulations.
Declaration of Competing Interest
None.
Funding
This work was partly supported by the European Observatory on Health Systems and Policies, Brussels, Belgia.
Footnotes
This article has been made Open Access through funding by the European Observatory on Health Systems and Policies as part of its Health Systems and Policy Monitor (www.hspm.org), an innovative platform that provides a detailed description of health systems and provides up to date information on reforms and changes that are particularly policy relevant.
Reference
- 1.Magnussen J, Vrangbæk K, Saltman R. Open University Press; 2009. Nordic Health Care Systems: Recent Reforms and Current Policy Challenges. [Google Scholar]
- 2.Byrkjeflot H, Neby S. The end of the decentralised model of healthcare governance?: Comparing developments in the Scandinavian hospital sectors. Journal of Health, Organisation and Management. 2008;22(4):331–349. doi: 10.1108/14777260810893944. [DOI] [PubMed] [Google Scholar]
- 3.Tynkkynen L.K., Alexandersen N., Kaarbøe O., Anell A., Lehto J., Vrangbӕk K. Development of voluntary private health insurance in Nordic countries – An exploratory study on country-specific contextual factors. Health Policy. 2018;122(5):485–492. doi: 10.1016/j.healthpol.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Mahoney J, Thelen K. In: Explaining institutional change: Ambiguity, agency, and power. Mahoney J, Thelen K, editors. Cambridge University Press; 2009. A theory of gradual institutional change; pp. 1–37. [Google Scholar]
- 5.Vogel G. It's been so, so surreal. Critics of Sweden's lax pandemic policies face fierce backlash. Science. 2020 doi: 10.1126/science.abf1247. Oct.6. [DOI] [Google Scholar]
- 6.Ludvigsson JF. The first eight months of Sweden's COVID-19 strategy and the key actions and actors that were involved. Acta Paediatrica. 2020;00:1–13. doi: 10.1111/apa.15582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rechel B, Maresso A, van Ginneken E. World Health Organization (acting as the host for, and secretariat of, the European Observatory on Health Systems and Policies); 2019. Health Systems in Transition. Template for authors. Copenhagen. [Google Scholar]
- 8.Anell A, Glenngård AH, Sweden Merkur S. Health system review. Health Systems in Transition. 2012;14(5):1–159. [PubMed] [Google Scholar]
- 9.Keskimäki I, Tynkkynen LK, Reissell E, Koivusalo M, Syrjä V, Vuorenkoski L, Rechel B, Karanikolos M. Finland: Health system review. Health Systems in Transition. 2019;21(2):1–166. [PubMed] [Google Scholar]
- 10.Olejaz M, Juul Nielsen A, Rudkjøbing A, Okkels Birk H, Krasnik A. Hernández-Quevedo C. Denmark: Health system review. Health Systems in Transition. 2012;14(2):1–192. [PubMed] [Google Scholar]
- 11.Saunes IS, Karanikolos M, Sagan A. Norway: Health system review. Health systems in Transition. 2020;22(1):1–163. [PubMed] [Google Scholar]
- 12.Sigurgeirsdóttir S, Waagfjörð J, Maresso A. Iceland: Health system review. Health Systems in Transition. 2014;16(6):1–182. [PubMed] [Google Scholar]
- 13.Nordic Council of Ministers. Nordic co-operation on COVID-19. Accessed 06.11. 2020. https://www.norden.org/en/news/nordic-co-operation-covid-19.
- 14.Karanikolos M, McKee M. How comparable is COVID-19 mortality across countries? Health System Response Monitor. European Observatory on Health Systems and Policies. 2020 https://analysis.covid19healthsystem.org/index.php/2020/06/04/how-comparable-is-covid-19-mortality-across-countries/ Accessed 09.11.2020. [Google Scholar]
- 15.Karanikolos M, Rajan S, Rechel B. European Observatory on Health Systems and Policies; 2020. How do COVID-19 testing criteria differ across countries? Health System Response Monitor.https://analysis.covid19healthsystem.org/index.php/2020/04/16/how-do-covid-19-testing-criteria-differ-across-countries/ Accessed 09.11. [Google Scholar]
- 16.Nordic Council of Ministers . 2020. Mandate for the Nordic Group for Public Health Preparedness (the Svalbard Group)https://www.norden.org/en/information/mandate-nordic-group-public-health-preparedness-svalbard-group Accessed 06.11. [Google Scholar]
- 17.Eydal GB, Ómarsdóttir IL, Cuadra CB, Dahlberg R, Hvinden B, Rapeli M, Salonen T. Report for the Nordic Council of ministers; 2016. Local Social Services in Nordic Countries in Times of Disaster. [Google Scholar]; https://www.stjornarradid.is/media/velferdarraduneyti-media/media/velferdarvakt09/Local-Services-in-Times-of-Disaster.pdf.
- 18.Tiirinki H, Tynkkynen LK, Sovala M, et al. COVID-19 pandemic in Finland - Preliminary analysis on health system response and economic consequences. Health Policy Technol. 2020;9(4):649–662. doi: 10.1016/j.hlpt.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergh A, Bjørnskov C. Historical Trust Levels Predict the Current Size of the Welfare State. Kyklos. 2011;64:1–19. doi: 10.1111/j.1467-6435.2010.00492.x. [DOI] [Google Scholar]
- 20.Christenson T., Lægreid P. Balancing Governance Capacity and Legitimacy: How the Norwegian Government Handled the COVID-19 Crisis as a High Performer. Public Admin Rev. 2020;80:774–779. doi: 10.1111/puar.13241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esaiasson P, Sohlberg J, Ghersetti M, Hersetti M., Johansson B. How the coronavirus crisis affects citizen trust in institutions and in unknown others: Evidence from ‘the Swedish experiment. European Journal of Political Research. 2020 doi: 10.1111/1475-6765.12419. [DOI] [Google Scholar]
- 22.Holmberg S, Rothstein B. Social Trust – The Nordic Gold? QoG Working Paper Series. 2020 1 January 2020 ISSN 1653-8918. [Google Scholar]
- 23.Strang J. Why do the Nordic countries react differently to the covid-19 crisis? Article in Nordics info 06.04.2020. https://nordics.info/show/artikel/the-nordic-countries-react-differently-to-the-covid-19-crisis/.
- 24.Nordic Council News: Sverige går mot strömmen - också i hur medier i norden bevakar coronakrisen. 30.11.2020. https://www.mynewsdesk.com/se/norden_i_fokus/pressreleases/sverige-gaar-mot-stroemmen-ocksaa-i-hur-medier-i-norden-bevakar-coronakrisen-2986603.
- 25.Martin R, Conseil A, Longstaff A, Kodo J, Siegert J, Duguet A-M, Lobato de Faria P., Haringhuizen G, Espin J, Coker R. Pandemic influenza control in Europe and the constraints resulting from incoherent public health laws. BMC Public Health. 2010;10:532. doi: 10.1186/1471-2458-10-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stenius H. In: Nordic Associations in a European Perspective (Baden-Baden: Nomos) Alapuro R., Stenius H., editors. 2010. Nordic Associational Life in European and Inter-Nordic Perspectives; pp. 29–86. [Google Scholar]
- 27.Brandén M, Aradhya S, Kolk M, Härkönen J, Drefahl S, Malmberg B, Rostila M, Cederström A, Andersson G, Mussino E. Residential context and COVID-19 mortality among adults aged 70 years and older in Stockholm: a population-based, observational study using individual-level data. Lancet Healthy Longev. 2020;1:e80–e88. doi: 10.1016/S2666-7568(20)30016-7. Published Online October 27, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kucharski AJ, Klepac P, Conlan AJK, Kissler SM, Tang ML, Fry H, Gog JR, Edmunds WJ. on behalf of the CMMID COVID-19 working group: Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. 2020;20 doi: 10.1016/S1473-3099(20)30457-6. 1151–60 Published Online June 16, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]