Abstract
Objective
One of the main difficulties of vaginoscopy is continuous leakage of distension medium from the introitus hindering proper visualization. This study evaluates the effectiveness and success of performing diagnostic or operative vaginoscopic surgery via a tight self-retaining external vulvar sheet (Darwish sheet) expressed as tight vaginoscopy (TV) compared with conventional vaginoscopy (CV).
Patients and Methods
Females referred for vaginoscopy were initially examined by diagnostic CV followed by TV, and whenever indicated, operative TV via Darwish sheet was performed.
Results
Diagnostic TV was more feasible with excellent visualization if compared with CV. The mean infused distension fluid volume was 325 ml versus 485 ml, and the mean leaked fluid volume was 37 ml versus 94 ml in diagnostic TV versus CV, respectively. Operative TV via Darwish sheet was done in 21 cases (56.7%) that required surgery with 100% success rate without any reported complications.
Conclusions
Accomplishing vulvar tightness using a cheap self-retaining external vulvar sheet (Darwish sheet) during vaginoscopy (TV) is associated with a clearer visualization of vagina or cervix, a lesser amount of irrigating fluid and lesser leakage as compared with CV.
Keywords: Vaginoscopy, Tight, Vaginal lesions, Cervix, Vagina, Darwish sheet
Introduction
Endoscopic examination of the vagina (vaginoscopy) is highly indicated in symptomatizing girls, virgins, nulliparous women with very tight vagina, married women with vaginismus, old postmenopausal patients or postoperative or post-irradiation due to inability to insert a bivalve vaginal speculum in these cases. In addition to the confirmation of diagnosis of suspected vaginal masses or polyps, it can be used to diagnose laceration of the vaginal wall in girls due to foreign body (FB), traumatic injuries, or sexual abuse [1–3]. Despite its importance, vaginoscopy is not a famous procedure due to many factors, one of them is poor visualization due to distension medium leakage. To the best of our knowledge, there is no study addressing a solution to improve the visualization and success of vaginoscopic surgery. This study aims to assess the effectiveness and success of performing diagnostic or operative vaginoscopic surgery via a tight self-retaining external vulvar sheet (Darwish sheet) expressed as tight vaginoscopy (TV) compared with conventional vaginoscopy (CV).
Patients and Methods
A prospective cohort study was performed at the Endoscopy Unit of the Woman’s Health University Hospital, Assiut, Egypt, between July 2014 and January 2020. Participants were symptomatic patients with suspected narrow vagina and consented to participate in this study. They were children, adolescents or nulliparous adult females scheduled for vaginoscopy to confirm the diagnosis and whenever indicated to remove a vaginal or cervical lesion or FB. Multiparous patients or nulliparous patients with normal, patulous or lax vaginas were excluded. All cases underwent a high-resolution 2D transabdominal ultrasonography with full-bladder technique to assess the vaginal integrity, length and width. Children with suspected FB were subjected to plain X-ray. Patients with definite or suspected vaginal or cervical lesions were included in this study. All cases were prepared for a vaginoscopic surgery at the regular endoscopy unit in the immediate postmenstrual period (if postmenarchal), but young girls were operated on at any time.
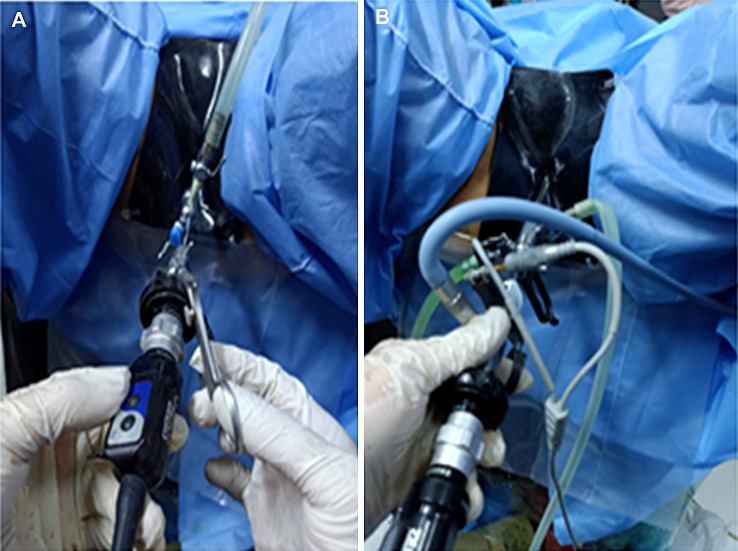
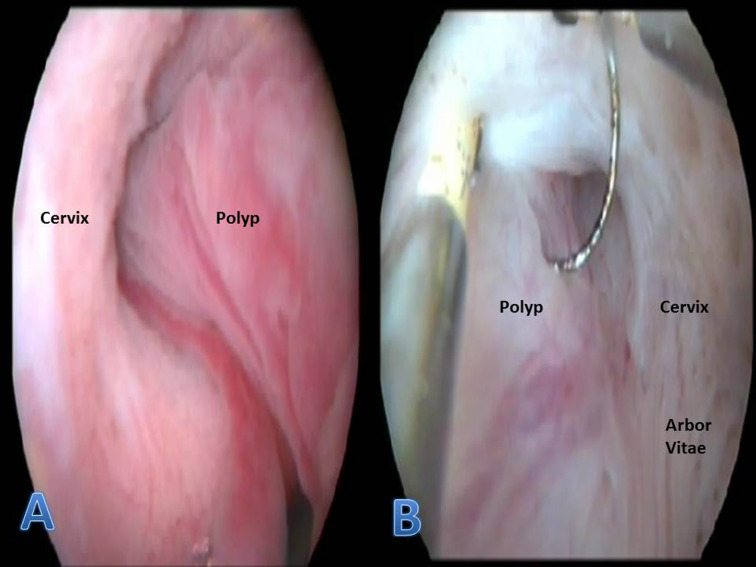
Every patient was subjected to a sequential diagnostic conventional vaginoscopy (CV) followed by tight vaginoscopy (TV), and whenever required operative TV. Vulvar tightness was made using a sterile self-retaining external vulvar sheet (Darwish sheet) (Fig. 1). Under general anaesthesia, all the cases were placed in the dorsal lithotomy position. For adult cases, conventional hysteroscope was used as a vaginoscope. A 4-mm zero-degree telescope loaded inside a 5-mm outer sheath and connected to a light cable, with a pneumatic infusion pump for 0.9% saline irrigation, was inserted inside the vaginal introitus. The vaginoscope was gradually advanced inside the vagina with reporting on the vaginal walls till the ectocervix. Proper examination of the cervix included the endocervical canal and the internal os. On the other hand, for children, office hysteroscope (a 2.6-mm telescope and a 3.2-mm outer sheath) was used. After performing CV, the same patient was re-examined using TV. The vaginoscope penetrates a sterile self-retaining tight external silicone vulvar sheet (Darwish sheet) measuring 20 × 15 cm, which is tied around the patient's waist (Fig. 1) with a central linear incision of 10 mm aiming to minimize the reflux of the irrigating fluid from the vagina. For operative TV, a 27-Fr rotatory resectoscope was loaded inside the sterile self-retaining tight external silicone vulvar sheet (Darwish sheet) (Fig. 1). Glycine 1.5% was used for monopolar resectoscope. FB was extracted in 3 cases using a flexible grasping forceps loaded in the side channel of operative sheath as shown in Fig. 1. A comment on the feasibility of surgery (clarity of visualization and access to the lesion), operative time and any possible complications was made. The amount of irrigated distension medium as well as escaped amount in the suction unit and that collected in a sterile plastic bag embedded under the buttocks of the patient was collected and measured after every case of the diagnostic CV, diagnostic TV and operative TV. All endoscopic equipments were manufactured by Storz Co. (Tuttlingen, Germany). All excised tissues were sent for histopathologic assessment. Figure 2 shows diagnostic and operative vaginoscopy of a case of endocervical polyp after application of Darwish sheet. The main outcome measures included clarity of visualization of the vagina and the cervix, estimation of infused and leaked distension medium before and after application of Darwish sheet and the success rate of operative TV whenever indicated. Postoperatively, the patients were kept under observation for 2–4 h and discharged whenever stable. All cases were followed up at least once after the next menses and examined clinically and by ultrasonography. Data entry and analysis were done using SPSS (Statistical Package for Social Science) version 19. Data were presented as frequency, percentage, mean and standard deviation. Chi-square test and Fisher’s exact tests were used to compare between qualitative variables. Independent samples t-test was used to compare between quantitative variables. P-value was considered statistically significant when P ≤ 0.05.
Fig. 1.
Operative vaginoscopy via a self-retaining vulvar sheet (Darwish sheet) (a: grasping forceps, b: resectoscope)
Fig. 2.
a Vaginoscopic appearance of cervical polyp. b Resectoscopic polypectomy via vaginoscopy
Results
This study comprised 37 consecutive patients referred for vaginoscopy. They were 23 prepubertal girls, 10 adolescent virgins and 4 married nulliparous patients. The mean age of prepubertal girls was 6 ± 2.1 (4–11 years), while it was 18 ± 3.1 (16–22 years) for the rest of cases. The main complaints in the prepubertal girls (23 cases) were persistent vaginal discharge associated with pruritus resistant to all forms of medical treatment (10 cases), which was sometimes bloody (5 cases). Diagnostic vaginoscopy revealed colpitis and cervicitis in 5 cases and cervical polyps in 5 cases and was normal in the remaining 5 cases. FB was seen in 3 cases, which were pen cape in one case, sewing threads in one case and nylon threads in another case (video). Plain X-ray and ultrasonography were normal in the 3 cases. The remaining 5 cases presented with a polypoidal mass protruding from the vulva, which were cervical or vaginal as seen by vaginoscopy. Operative TV succeeded to excise them completely. Adolescent virgins (10 cases) presented mainly with bloody or persistent vaginal discharge or abnormal vaginal bleeding in 4 and 6 cases, respectively. Vaginoscopy diagnosed a cervical or vaginal polyp in 5 cases, endometrial polyp by hysteroscopy in 2 cases and chronic non-specific cervicitis in 3 cases. Married nulliparous patients (4 cases) presented with dyspareunia and contact bleeding in 3 cases and one case, respectively. Vaginoscopy diagnosed a cervical polyp in one case, a vaginal septum in 2 cases and a suspicious cervix in the last case. Operative TV succeeded to treat the first 2 cases. In the last case, vaginoscope was used as a cervicoscopy with staining of the cervix with acetic acid and Lugol's iodine dye, which revealed severe inflammatory picture and immature metaplasia, but punch biopsy was taken. As shown in Table 1, diagnostic CV significantly required more fluid, with more escaped fluid, and took more time with poor visualization due to unsatisfactory vaginal tightness and collapse of the vaginal walls. Duration and fluid requirements for operative procedures (21 cases) are shown in Table 2 without any complications. The histopathologic findings of the excised or biopsied vaginal or cervical lesions were in 17 cases that were benign: 8 inflammatory polyps, 2 multilocular cystic polyps, 3 fibroepithelial (stromal) polyps, 3 hyperplastic polyps and chronic non-specific cervicitis in one case.
Table 1.
Diagnostic vaginoscopy results
| Diagnostic CV | Diagnostic TV | P value | |
|---|---|---|---|
| Distension medium volume | 485 ± 83 ml | 325 ± 46 ml | 0.000 |
| Escaped fluid | 94 ± 33 ml | 37 ± 5 ml | 0.000 |
| Duration of the procedure | 5.7 ± 0.9 min | 3.5 ± 0.6 min | 0.000 |
| Clear visualization | 21(56.7%) | 34(91.8%) | 0.000 |
| Improper visualization | 16 (43%) | 3 (8%) | 0.001 |
| Excessive fluid leakage | 13 (35%) | 1 (2.7%) | 0.000 |
| Excessive cervical, uterine or lesion bleeding | 3 (8%) | 2 (5.4%) | NS |
Table 2.
Surgical outcomes of operative tight vaginoscopy (21 cases)
| Technique | Number of cases | Mean fluid volume | Duration of procedure |
|---|---|---|---|
| Metroplasty (incision) of a vaginal septum | 2 | 752 ± 113 mL | 15.7 ± 3.4 min |
| Polypectomy | 16 | 821 ± 142 mL | 16.5 ± 4.2 min |
| Extraction of a FB | 3 | 556 ± 83 mL | 9.8 ± 2.7 min |
Discussion
In modern practice, clinical use of vaginoscopy is limited due to many factors like the rarity of vaginal lesions, scare publications, lack of experience and orientation and poor visualization due to distending medium leakage via the introitus. In a systematic review [3], only 13 studies on vaginohysteroscopy have been reported. Ten of them (77%) were published after 2005. Eleven papers described a single case report, one paper reported two case reports and one paper reported a case series of 28 cases [4]. Between 2004 and 2013, only 20 girls with persistent vaginal discharge were examined by vaginoscopy at a university hospital [5]. Difficult vaginoscopy is usually expected, particularly in girls due to the natural narrowing of the vagina, their desire to keep intact hymen, and the restricted view [6]. Unlike hysteroscopy, even on maximal fluid flow, vaginal distension is very difficult due to low intravaginal pressure as the vagina is opened to the exterior with continuous leakage of fluid. This study highlights an innovative simple modification to improve visualization and surgical success whenever performing vaginoscopy in girls and nulliparous patients with narrow vaginas.
During vaginoscopy, minimizing fluid leakage from the vagina can be accomplished by manual compression of the labial tissue to narrow the vaginal introitus as recommended by ACOG [7]. Unfortunately, it leads to incomplete elimination of irrigating fluid leakage. Moreover, the surgeon is usually busy during vaginal surgery in a narrow space and usually uses both hands during vaginal resectoscopy. In this study, we used a sterile self-retaining well-fitted external vulvar sheet (Darwish sheet) omitting vulvar tightness by hands. Moreover, there is no need for a nurse or assistant compression of the labia using this technique. This modification allows proper fitting with free hands of the surgeon. Limitations of this study include small sample size, which is attributed to the rarity of cases. The same cause stands behind using the same case to compare CV and TV sequentially without a comparison group. Heterogeneity of cases is another limiting issue of this study. Any research on a novel procedure for rare indications with limited clinical experience would be defective. Although it is a case series with some methodological limitations, it can be helpful in generating a hypothesis that can be tested in further analytic studies [8]. All these limitations would be overcome whenever a large sample-sized multi-centric study would be initiated in future. It is concluded that accomplishing vulvar tightness using a self-retaining tight external vulvar sheet (Darwish sheet) during vaginoscopy (TV) is associated with a better vaginal seal to minimize escape of irrigation fluid, clearer visualization of vaginal or cervical lesions, and lesser requirement of the amount of irrigating fluid as compared to CV. Its routine use as a cheap basic step during diagnostic and therapeutic vaginoscopy is recommended.
Acknowledgements
None.
Abbreviations
- CV
Conventional vaginoscopy
- FB
Foreign body
- TV
Tight vaginoscopy
Atef M. M. Darwish
is currently a Professor and a consultant of Obstetrics and Gynecology, Assiut University, Egypt. He was graduated from the same faulty and completed his MD thesis at Ulm University (Germany). Thereafter he got a PhD degree from Utrecht University (The Netherlands). He joined many centers in the US and Europe concentrating on the reproductive medicine and endoscopic surgery. He is the chief editor or an author of 10 international books and published more than 85 papers in international medical journals.
Authors’ Contributions
AD created the idea, performed the operations and wrote the paper, while DD prepared the cases. All authors have read and approved the manuscript.
Funding
No funding was obtained for this study.
Availability of Data and Materials
The datasets generated and/or analysed during the current study are not publicly available due to [privacy of virgins in a developing country setup] but are available from the corresponding author on reasonable request.
Compliance with Ethical Standards
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Consent to Publish
Consent for the publication of identifying images or other personal or clinical details of participants that compromise anonymity.
Ethical Approval
The study was approved in May 2014 by the local ethical committee of the faculty of Medicine, Assiut University. After detailed explanation of the study, all cases (or parents of young girls) signed an informed consent to participate in this study.
Footnotes
Atef MM Darwish is a Professor, Department of Obstetrics & Gynecology, Woman's Health University Hospital, P.O. Box: (1), 71111, Assiut, Egypt; Dina AM Darwish is a Professor, Department of Obstetrics & Gynecology, Woman's Health University Hospital, P.O. Box: (1), 71111, Assiut, Egypt.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shui LT, Lee CL, Yen CF, et al. Vaginoscopy using hysteroscope for diagnosis of vaginal bleeding during childhood: case report. Changgeng Yi XueZaZhi. 1999;22(2):344–347. [PubMed] [Google Scholar]
- 2.Johary J, Xue M, Xu B, et al. Use of hysteroscope for vaginoscopy or hysteroscopy in adolescents for the diagnosis and therapeutic management of gynecologic disorders: a systematic review. J Pediatr Adolesc Gynecol. 2015;28(1):29–37. doi: 10.1016/j.jpag.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Di Spiezio SA, Zizolfi B, Calagna G, et al. Vaginohysteroscopy for the diagnosis and treatment of vaginal lesions. Int J Gynaecol Obstet. 2016;133(2):146–151. doi: 10.1016/j.ijgo.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Smorgick N, Sheetua A, Lotan G, et al. Diagnosis and treatment of pediatric vaginal and genital tract abnormalities by small diameter hysteroscope. J Pediatr Surg. 2009;44(8):1506–1508. doi: 10.1016/j.jpedsurg.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Ekinci S, Karnak I, Tanyel F, et al. Prepubertal vaginal discharge: vaginoscopy to rule out foreign body. Turk J Pediatr. 2016;58(2):168–71. doi: 10.24953/turkjped.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 6.Moghadami-Tabrizi N, Dabirashrafi H, Mohammad K, et al. Operative vaginoscopy. J Am Assoc Gynecol Laparosc. 1994;1(4 Part 2):S23. doi: 10.1016/s1074-3804(05)80944-2. [DOI] [PubMed] [Google Scholar]
- 7.ACOG Committee opinion on Gynecologic Practice The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology number 800. Obstet Gynecol. 2020;135(3):e138–e148. doi: 10.1097/AOG.0000000000003712. [DOI] [PubMed] [Google Scholar]
- 8.Kooistra B, Dijkman B, Einhorn T, et al. How to design a good case series. Bone Jt Surg Am. 2009;91(Suppl 3):21–26. doi: 10.2106/JBJS.H.01573. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to [privacy of virgins in a developing country setup] but are available from the corresponding author on reasonable request.