Abstract
Objective
To determine the ability of the Activity Measure for Post-Acute Care (AM-PAC) "6-Clicks" assessments of mobility and activity to predict key clinical outcomes in patients hospitalized with coronavirus disease 2019 (COVID-19).
Design
Retrospective cohort study.
Setting
An academic health system in the United States consisting of 5 inpatient hospitals.
Participants
Adult patients (N=1486) urgently or emergently admitted who tested positive for COVID-19 and had at least 1 AM-PAC assessment.
Interventions
Not applicable.
Main Outcome Measures
Discharge destination, hospital length of stay, in-hospital mortality, and readmission.
Results
A total of 1486 admission records were included in the analysis. After controlling for covariates, initial and final mobility (odds ratio, 0.867 and 0.833, respectively) and activity scores (odds ratio, 0.892 and 0.862, respectively) were both independent predictors of discharge destination with a high accuracy of prediction (area under the curve [AUC]=0.819-0.847). Using a threshold score of 17.5, sensitivity ranged from 0.72-0.79, whereas specificity ranged from 0.74-0.83. Both initial AM-PAC mobility and activity scores were independent predictors of mortality (odds ratio, 0.885 and 0.877, respectively). Initial mobility, but not activity, scores were predictive of prolonged length of stay (odds ratio, 0.957 and 0.980, respectively). However, the accuracy of prediction for both outcomes was weak (AUC=0.659-0.679). AM-PAC scores did not predict rehospitalization.
Conclusions
Functional status as measured by the AM-PAC “6-Clicks” mobility and activity scores are independent predictors of key clinical outcomes individual hospitalized with COVID-19.
Keywords: Length of stay, Morbidity, Mortality, Prognosis, Rehabilitation
List of abbreviations: AM-PAC, Activity Measure for Post-Acute Care; AUC, area under the curve; CI, confidence interval; COVID-19, coronavirus disease 2019; ICU, intensive care unit; LOS, length of stay; ROC, receiver operating characteristic; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; UPHS, University of Pennsylvania Health System
The outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has had a significant effect on health care delivery throughout the world, with over 175 million cases and nearly 4 million deaths worldwide.1 Infection with SARS-CoV-2 leads to coronavirus disease 2019 (COVID-19), which is highly variable in terms of clinical presentation and severity.2 Although some will present with no or minimal symptoms, 20% of infected individuals develop severe COVID-19, and a significant fraction will require prolonged hospitalization, placement in a postacute care facility, or readmission to the hospital.3 , 4 Early identification of individuals at risk for such outcomes may help reduce the burden imposed on health care systems.
The risks of infection, hospitalization, and death due to COVID-19 are higher in older persons, those with medical comorbidities,5 and in the Black and Hispanic-Latino populations.6 However, other factors may be necessary to identify individuals who require additional services in the acute and early postacute phase. For example, 3 recent studies have reported significant associations between impairments in physical function and important outcomes such as discharge destination,7 hospital readmission,8 and mortality9 in this population. These results are consistent with a small but growing number of reports highlighting prognostic significance of physical function in hospitalized patients,10 suggesting that routine assessment of physical function in the hospital may help guide the delivery of care, particularly during a pandemic when resources are stretched.
The Activity Measure for Post-Acute Care (AM-PAC) “6-Clicks” assessments of basic mobility and activities of daily living are specific measures of patient functioning that have been adopted by numerous health care systems. The tools are quick and easy to implement and predict discharge destination in a variety of hospitalized populations.11, 12, 13 The association between AM-PAC scores and clinical outcomes in COVID-19, however, have not been fully investigated. Therefore, the purpose of this study was to test the hypothesis that AM-PAC “6-Clicks” activity and mobility scores would predict discharge disposition, hospital length of stay (LOS), in-hospital mortality, and 30-day readmission in individuals hospitalized with COVID-19.
Methods
Study design, setting, and participants
This retrospective observational cohort study used an inpatient COVID-19 registry composed of medical record data of patients admitted to 5 hospitals within the University of Pennsylvania Health System (UPHS). The UPHS includes both community and academic medical centers in urban and suburban areas across the greater metropolitan Philadelphia region. The records from individuals 17 years or older who were urgently or emergently admitted to one of the 5 hospitals from March 1 to July 31, 2020, who tested positive for COVID-19 during their admission and who had at least 1 AM-PAC “6 Clicks” rating were included in the analysis. Hospice or psychiatric admission records were excluded. The study protocol was approved by the University of Pennsylvania Institutional Review Board (protocol #843920).
Variables
Outcome variables included discharge destination (home vs facility, including long-term acute hospitals, skilled nursing facilities, and inpatient rehabilitation facilities), hospital LOS (dichotomized by 75th percentile; 11 days), in-hospital mortality, and 30-day readmission. The analysis of discharge destination only included those who were discharged from the hospital alive. Readmission data were retrieved more than 30 days after the end of the observation period and included individuals who were readmitted to one of the 5 hospitals in the system within 30 days of discharge from the index admission, excluding hospice admissions or patients admitted within 6 hours from discharge.
Our predictor variables were AM-PAC “6-Clicks” mobility and activity scores. Each assessment consists of 6 items scored on a 1-4 scale, producing an overall score of 6-24, with lower scores indicating poorer performance. The mobility assessment includes the following tasks: (1) turning over in bed; (2) sitting down and standing up from a chair; (3) moving from lying to sitting; (4) moving to and from a bed to a chair; (5) walking in the room; and (6) climbing 3-5 steps. The activity assessment includes items related to activities of daily living: (1) putting on and taking off lower body clothing; (2) bathing; (3) toileting; (4) putting on and taking off upper body clothing; (5) grooming; and (6) eating meals. Previous studies have demonstrated the validity of the assessments in the hospital environment14 and that they can be assessed by multiple disciplines with excellent reliability.15 , 16 In the UPHS system, nurses, physical therapists, and occupational therapists are all trained to use the assessments, and assessments from all 3 disciplines were included in this data set. The patient's initial AM-PAC score was used to predict mortality and hospital LOS, whereas the final score was used to predict readmission. Both initial and final scores were used to predict discharge destination in separate analyses.
Demographic variables considered as potential covariates include age (>75 or ≤75y),17 sex, race (Black, White, other),18 ethnicity (Hispanic/Latino vs not), and insurance status (uninsured, Medicaid, Medicare, private, other). The admitting hospital was also included to account for variation across facilities.19 Clinical variables included primary/admitting diagnosis (COVID-19 vs other), admission to the intensive care unit (ICU) (yes vs no), mechanical ventilation (yes vs no), and hospital LOS (days). The Charlson Comorbidity Index20 was included because the presence of medical comorbidities increases the risk and severity of infection with COVID-19.5 Preliminary analysis suggested a significant effect of admission date on several variables, including mortality21; as a result, the sample was divided into 2 cohorts based on whether their admission date was in the first (3/1 to 5/17) or second (5/18 to 7/31) half of the study time period. Because of the variability in the timing of the AM-PAC assessments, the number of days between admission and initial AM-PAC score was included as a covariate for the prediction of mortality, hospital LOS, and discharge destination. Similarly, the number of days between the final AM-PAC assessment and discharge was used as a covariate in the prediction of discharge destination and readmission.
Analysis
Continuous variables are expressed as median and interquartile range because the distribution of most variables is skewed, whereas categorical variables are expressed as frequencies and percentages. Participant characteristics were compared between subsets (COVID as admitting/primary diagnosis vs COVID as secondary diagnosis, first cohort vs second cohort, included vs excluded) using the Mann-Whitney U test for continuous variables and chi-square test for categorical variables. Preliminary bivariate analysis demonstrated that all potential covariates were significantly associated with at least 2 of the 4 outcome measures, so all were included in the multivariate analyses. The assumption of linearity of each of the continuous predictor variables with the logit was assessed using the Box-Tidwell procedure with Bonferroni correction.22
Separate multivariate logistic regression models were generated for each combination of AM-PAC (mobility, activity) and outcome variable (mortality, LOS, discharge destination, readmission). All variables were entered using the forced-entry method in 2 steps; the first step included just the covariates, whereas the second included covariates and the AM-PAC score of interest (eg, mobility or activity, initial or final). Receiver operating characteristic (ROC) curves were created for each step using the predicted probabilities from each model, and change in the area under the curve (AUC) was used to evaluate the effect of the addition of the AM-PAC score on the overall prediction of the model. Additionally, separate ROC curves were created using only the raw AM-PAC scores to determine the AUC for prediction and identify threshold scores for predicting each of the outcome variables. Stratified analyses, using identical regression models, were performed to further explore the effect of admitting/primary diagnosis (COVID vs other), date of admission (first vs second cohort), admission to the ICU (yes vs no), medical comorbidity (dichotomized by the median), and race (Black vs White+other). The effect of selection bias on the relationship between the covariates and the dependent variables was explored using separate regression models including only covariates as predictors for included and excluded participants. All analyses were conducted using SPSS v26,a and the level of significance was set at P<.05.
Results
Participants
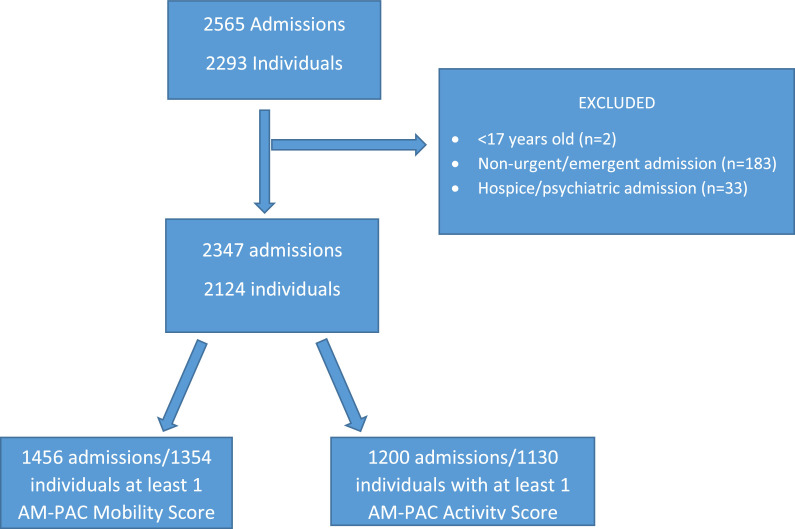
Participant flow is shown in figure 1 , and demographics are shown in table 1 . A total of 62% (n=1456) of adult urgent/emergent admissions had at least 1 AM-PAC mobility score, whereas 51% (n=1200) had at least 1 AM-PAC activity score. Physical and/or occupational therapy was consulted in 861 of the 1456 records with at least 1 AM-PAC mobility score. A total of 74% (n=635) of those with a physical therapy consult had at least 1 AM-PAC mobility score entered by a physical therapist, whereas 68% (n=584) of those with an occupational therapy consult had at least 1 AM-PAC activity score entered by an occupational therapist. Compared with participants who had at least 1 AM-PAC score in their record, excluded participants were younger, had fewer comorbidities, had shorter LOS, were less likely to be admitted to the intensive care unit, and were more likely to be discharged to home but were also more likely to die in the hospital (supplemental table S1, available online only at http://www.archives-pmr.org/).
Fig 1.
Flow diagram of inclusion criteria.
Table 1.
Participant characteristics
| Characteristics | All (N=1456) | COVID-19 as Primary/Admitting Diagnosis (n=690) | COVID-19 as Secondary Diagnosis (n=766) | P Value (COVID-19 as Primary vs Secondary) |
|---|---|---|---|---|
| Age (y), median (IQR) | 64 (26) | 65 (25) | 64 (26) | .079 |
| Sex (female), n (%) | 723 (49.7) | 348 (50.4) | 375 (49.0) | .573 |
| Race, n (%) | .673 | |||
| Black | 791 (54.3) | 375 (54.3) | 416 (54.3) | |
| White | 440 (30.2) | 203 (29.4) | 237 (30.9) | |
| Other | 225 (15.5) | 112 (16.2) | 113 (14.8) | |
| Ethnicity (Hispanic/Latino), n (%) | 144 (9.9) | 71 (10.3) | 73 (9.5) | .628 |
| BMI, median (IQR) | 28.2 (10.4) | 28.7 (10.2) | 27.5 (10.5) | <.001 |
| Charlson Comorbidity Index, median (IQR) | 4 (5) | 4 (4) | 4 (5) | .560 |
| Insurance, n (%) | .002 | |||
| Uninsured | 38 (2.6) | 29 (4.2) | 9 (1.2) | |
| Medicaid | 271 (18.2) | 119 (17.2) | 144 (18.8) | |
| Medicare | 795 (53.5) | 362 (52.5) | 421 (55.0) | |
| Private | 314 (21.1) | 154 (23.3) | 150 (19.6) | |
| Other | 68 (4.6) | 26 (3.8) | 42 (5.5) | |
| ICU (admitted), n (%) | 521 (35.8) | 206 (29.9) | 315 (41.1) | <.001 |
| Mechanical ventilation (yes), n (%) | 263 (18.1) | 93 (13.5) | 170 (22.2) | <.001 |
| Mortality, n (%) | 129 (8.9) | 59 (8.6) | 70 (9.1) | .682 |
| Length of stay (d), median (IQR) | 7 (10) | 7 (9) | 7(11) | . 017 |
| Discharge, n (%) home | 890 (61.1) | 461 (66.8) | 429 (56.0) | <.001 |
| Readmission, n (%) | 166 (11.4) | 69 (10.0) | 97 (12.7) | .110 |
| AM-PAC mobility, median (IQR) | ||||
| Initial score | 18 (14) | 18 (12) | 15 (15) | <.001 |
| Days to initial score | 1 (3) | 1 (2) | 1 (4) | <.001 |
| Final score | 18 (13) | 18 (13) | 17 (15) | <.001 |
| Days from final to discharge | 1 (3) | 1 (3) | 1 (3) | .190 |
| AM-PAC activity, median (IQR) | ||||
| Initial score | 18 (14) | 19 (10) | 16 (13) | <.001 |
| Days to initial score | 1 (3) | 1 (2) | 1 (4) | .001 |
| Final score | 18 (13) | 19 (10) | 17 (12) | <.001 |
| Days from final to discharge | 1 (3) | 2 (4) | 2 (4) | .992 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
Supplemental Table 1.
Characteristics for included and excluded participants
| Excluded from AM-PAC Mobility (n=891) | Included AM-PAC Mobility (n=1456) | P Value | |
|---|---|---|---|
| Age, med (IQR) | 61 (30) | 64.5 (26) | <0.001 |
| Sex, n (%) female | 453 (50.8) | 723 (49.7) | 0.577 |
| Race, n (%) | 0.057 | ||
| Black | 441 (49.5) | 791 (54.3) | |
| White | 288 (32.3) | 440 (30.2) | |
| Other | 163 (18.2) | 225 (9.6) | |
| Ethnicity, n (%) Hispanic/Latino | 88 (9.9) | 144 (9.9) | 0.991 |
| Hospital, n (%) | <0.001 | ||
| 0 | 169 (18.9) | 143 (9.8) | |
| 1 | 251 (28.2) | 399 (27.4) | |
| 2 | 165 (18.5) | 333 (22.9) | |
| 3 | 196 (22.0) | 399 (27.4) | |
| 4 | 111 (12.5) | 183 (7.8) | |
| BMI, kg/m2, med (IQR) | 30.0 (10.1) | 28.2 (10.4) | 0.018 |
| Cohort, n (%) first | 574 (64.4) | 847 (58.2) | 0.003 |
| COVID adm or primary dx, n (%) yes | 450 (50.5) | 690 (47.4) | 0.143 |
| Charlson Comorbidity Index | 3 (5) | 4 (5) | <0.000 |
| Insurance, n (%) | 0.003 | ||
| Uninsured | 26 (2.9) | 38 (2.6) | |
| Medicaid | 186 (20.9) | 263 (18.1) | |
| Medicare | 410 (46.0) | 783 (53.8) | |
| Private | 233 (26.2) | 304 (20.9) | |
| Other | 36 (4.0) | 68 (4.7) | |
| ICU, n (%) admitted | 268 (29.4) | 521 (35.8) | <0.001 |
| Mechanical Ventilation, n (%) yes | 142 (15.9) | 263 (18.1) | 0.186 |
| Mortality, n (%) | 192 (21.5) | 129 (8.9) | <0.001 |
| Length of stay, days, med (IQR) | 4 (5) | 7 (10) | <0.001 |
| Discharge, n (%) home | 562 (87.1) | 890 (71.4) | <0.001 |
| Readmission, n (%) | 51 (5.7) | 136 (9.3) | 0.002 |
Med = median; IQR = interquartile range; BMI = body mass index; ICU = intensive care unit
P-values from Mann-Whitney U for continuous variables or Chi-square for categorical variables.
COVID-19 was the admitting or primary diagnosis for 48.6% (n=690) of included participants. Primary diagnoses varied for the remainder of the sample, with the most common being infection/sepsis (27% of the total), pneumonia (1.6%), gastrointestinal issues (1.4%), and trauma/fracture (1.3%). Those with COVID as an admitting or primary diagnosis were more likely to be discharged home, less likely to be admitted to the ICU or require mechanical ventilation, and had higher AM-PAC scores than those with COVID as a secondary diagnosis. As seen in supplemental table 2 (available online only at http://www.archives-pmr.org/), participants in the first cohort were more likely to have COVID as an admitting or primary diagnosis, require mechanical ventilation, have a longer hospital LOS, die in the hospital, and be discharged to a postacute care facility that those in the second cohort.
Supplemental Table 2.
Characteristics for participants in First and Second Cohorts
| First Cohort (n=847) | Second Cohort (n=609) | p | |
|---|---|---|---|
| Age, med (IQR) | 66 (23) | 62 (28) | 0.009 |
| Sex, n (%) female | 408 (48.2) | 315 (51.7) | 0.181 |
| Race, n (%) | 0.813 | ||
| Black | 458 (54.1) | 333 (54.7) | |
| White | 261 (30.8) | 179 (29.4) | |
| Other | 128 (15.1) | 97 (15.9) | |
| Ethnicity, n (%) Hispanic/Latino | 76 (9.0) | 68 (11.2) | 0.167 |
| BMI, kg/m2, med (IQR) | 29.8 (11.3) | 28.2 (10.3) | 0.561 |
| Charlson Comorbidity Index | 4 (4) | 4 (6) | 0.766 |
| Insurance, n (%) | 0.017 | ||
| Uninsured | 21 (2.5) | 17 (2.8) | |
| Medicaid | 131 (15.5) | 132 (21.7) | |
| Medicare | 468 (55.3) | 315 (51.7) | |
| Private | 191 (22.6) | 113 (18.6) | |
| Other | 36 (4.3) | 32 (5.3) | |
| COVID adm or primary dx, n (%) yes | 455 (53.7) | 235 (38.6) | <0.001 |
| ICU, n (%) admitted | 315 (37.2) | 206 (33.8) | 0.187 |
| Mechanical Ventilation, n (%) yes | 197 (23.3) | 66 (10.8) | <0.001 |
| Mortality, n (%) | 104 (12.3) | 25 (4.1) | <0.001 |
| Length of stay, days, med (IQR) | 8 (13) | 6 (7) | <0.001 |
| Discharge, n (%) home | 479 (68.8) | 411 (74.6) | 0.025 |
| Readmission, n (%) | 81 (9.6) | 55 (9.0) | 0.731 |
| AM-PAC MOBILITY, med (IQR) | |||
| Initial score | 17 (16) | 18 (13) | 0.004 |
| Days to initial score | 1 (3) | 1 (2) | 0.638 |
| Final score | 17 (15) | 18 (12) | <0.001 |
| Days from final to discharge | 1 (3) | 1 (3) | 0.774 |
| AM-PAC Activity, med (IQR) | 0.012 | ||
| Initial score | 18 (13) | 19 (18) | <0.001 |
| Days to initial score | 1 (5) | 1 (2) | 0.016 |
| Final score | 17 (12) | 19 (10) | <0.001 |
| Days from final to discharge | 2 (4) | 2 (4) | 0.044 |
Med = median; IQR = interquartile range; BMI = body mass index; ICU = intensive care unit
P-values from Mann-Whitney U for continuous variables or Chi-square for categorical variables.
Main results
The results of the stepwise logistic regression analyses are presented in table 2 , and the result of the stratified analyses are displayed in tables 3 -5. For discharge destination, the predictive ability of initial and final AM-PAC scores was assessed in separate regression models. After controlling for the influence of covariates, AM-PAC mobility and activity scores were both independent predictors of discharge destination (see table 3). Furthermore, their addition significantly improved the accuracy of prediction of the model, as shown by the change in AUC (see table 2). Each 1-point decrease in initial AM-PAC score increased the odds of discharge to a facility by 1.15-fold (1.12-1.19) and 1.12-fold (1.08-1.12) for mobility and activity, respectively. A 1-point decrease in final AM-PAC score increased the odds of being discharged to a facility by 1.20-fold (1.16-1.23) and 1.16-fold (1.12-1.20) for mobility and activity, respectively. Stratified analysis revealed similar results regardless of primary/admitting diagnosis (COVID vs other), cohort (date of admission in first vs second half of specified time period), ICU status (yes vs no), number of medical comorbidities, and race (supplemental table 3, available online only at http://www.archives-pmr.org/). In addition, the comparison of regression models including only covariates for included and excluded individuals suggest similar relationships between each of the covariates and discharge destination in the 2 groups (supplemental table 4, available online only at http://www.archives-pmr.org/).
Table 2.
Results of stepwise logistic regression models
| Outcome Variable | Regression Model | R2 | Sp | Sn | ROC AUC (95% CI) | AUC Diff (95% CI) |
|---|---|---|---|---|---|---|
| Discharge destination | Covariates | 0.421 | 91.9 | 50.0 | 0.853 (0.831 to 0.876) | 0.028* (0.016 to 0.040) |
| Covariates+initial mobility | 0.489 | 93.3 | 59.3 | 0.882 (0.863 to 0.901) | ||
| Covariates | 0.454 | 91.8 | 51.2 | 0.868 (0.845 to 0.891) | 0.018* (0.008 to 0.028) | |
| Covariates+initial activity | 0.497 | 91.1 | 57.6 | 0.886 (0.865 to 0.907) | ||
| Covariates | 0.438 | 91.3 | 52.1 | 0.856 (0.834 to 0.878) | 0.039* (0.025 to 0.053) | |
| Covariates+final mobility | 0.533 | 90.3 | 62.6 | 0.895 (0.877 to 0.913) | ||
| Covariates | 0.481 | 91.8 | 52.4 | 0.876 (0.854 to 0.898) | 0.020* (0.010 to 0.031) | |
| Covariates+final activity | 0.532 | 90.9 | 58.7 | 0.896 (0.876 to 0.916 | ||
| Length of stay | Covariates | 0.475 | 93.7 | 57.4 | 0.849 (0.827 to 0.871) | 0.006† (0.000 to 0.012) |
| Covariates+initial mobility | 0.483 | 93.4 | 58.6 | 0.856 (0.834 to 0.877) | ||
| Covariates | 0.508 | 92.4 | 61.1 | 0.863 (0.840 to 0.886) | 0.001 (−0.001 to 0.004) | |
| Covariates+initial activity | 0.509 | 92.3 | 61.1 | 0.863 (0.380 to 0.884) | ||
| Mortality | Covariates | 0.424 | 98.3 | 27.9 | 0.905 (0.878 to 0.931) | 0.007 (−0.002 to 0.017) |
| Covariates+initial mobility | 0.457 | 98.6 | 29.5 | 0.912 (0.886 to 0.938) | ||
| Covariates | 0.449 | 98.2 | 23.8 | 0.917 (0.892 to 0.941) | 0.010 (−0.001 to 0.021) | |
| Covariates+initial activity | 0.493 | 98.3 | 37.1 | 0.927 (0.905 to 0.949) | ||
| Readmission | Covariates | 0.098 | 99.8 | 0.60 | 0.698 (0.658 to 0.738) | 0.002 (−0.005 to 0.009) |
| Covariates+final mobility | 0.100 | 99.7 | 0.60 | 0.700 (0.660 to 0.740) | ||
| Covariates | 0.102 | 99.8 | 0.70 | 0.706 (0.664 to 0.749) | 0.000 (−0.004 to 0.003) | |
| Covariates+final activity | 0.102 | 99.8 | 0.70 | 0.706 (0.663 to 0.749) |
NOTE. Results of stepwise logistic regression are presented separately for each combination of outcome variable and predictor (eg, covariates, AM-PAC mobility, AM-PAC activity); R2=Nagelkerke R2 from regression model; specificity and sensitivity assume a predicted probability cutoff of 0.5; AUC Diff=AUC for model 2 (covariates+AM-PAC score) − model 1 (only covariates).
Abbreviations: Sn, sensitivity; Sp, specificity.
P<.001.
P<0.05;
Table 3.
Logistic regression results for predicting discharge
| Predictor | Sample | Odds Ratio | 95% CI | P Value |
|---|---|---|---|---|
| Initial AM-PAC Mobility | All (n=1246) | 0.867 | 0.841-0.893 | <.001 |
| COVID-19 as primary/admitting | ||||
| Yes (n=604) | 0.858 | 0.817-0.901 | <.001 | |
| No (n=641) | 0.869 | 0.837-0.903 | <.001 | |
| ICU | ||||
| Yes (n=419) | 0.861 | 0.818-0.906 | <.001 | |
| No (n=823) | 0.867 | 0.835-0.901 | <.001 | |
| Cohort | ||||
| First (n=696) | 0.883 | 0.848-0.919 | <.001 | |
| Second (n=550) | 0.844 | 0.806-0.884 | <.001 | |
| Initial AM-PAC activity | All (n=1029) | 0.892 | 0.862-0.923 | <.001 |
| COVID-19 as primary/admitting | ||||
| Yes (n=494) | 0.868 | 0.817-0.922 | <.001 | |
| No (n=516) | 0.896 | 0.857-0.937 | <.001 | |
| ICU | ||||
| Yes (n=365) | 0.889 | 0.840-0.940 | <.001 | |
| No (n=643) | 0.891 | 0.852-0.935 | <.001 | |
| Cohort | ||||
| First (n=560) | 0.904 | 0.864-0.946 | <.001 | |
| Second (n=469) | 0.855 | 0.810-0.901 | <.001 | |
| Final AM-PAC mobility | All (n=1242) | 0.837 | 0.812-0.86 | <.001 |
| COVID-19 as primary/admitting | ||||
| Yes (n=600) | 0.852 | 0.745-0.836 | <.001 | |
| No (n=641) | 0.806 | 0.770-0.843 | <.001 | |
| ICU | ||||
| Yes (n=392) | 0.789 | 0.745-0.836 | <.001 | |
| No (n=823) | 0.865 | 0.832-0.90 | <.001 | |
| Cohort | ||||
| First (n=685) | 0.842 | 0.808-0.876 | <.001 | |
| Second (n=512) | 0.818 | 0.778-0.860 | <.001 | |
| Final AM-PAC activity | All (n=999) | 0.862 | 0.832-0.893 | <.001 |
| COVID-19 as primary/admitting | ||||
| Yes (n=483) | 0.873 | 0.824-0.925 | <.001 | |
| No (n=516) | 0.848 | 0.806-0.892 | <.001 | |
| ICU | ||||
| Yes (n=356) | 0.813 | 0.759-0.870 | <.001 | |
| No (n=643) | 0.884 | 0.844-0.927 | <.001 | |
| Cohort | ||||
| First (n=557) | 0.852 | 0.813-0.893 | <.001 | |
| Second (n=442) | 0.829 | 0.782-0.879 | <.001 |
NOTE. Results of the main (sample=all) and subanalyses on different subsets of the cohort (eg, only those with COVID-19 as a primary or admitting diagnosis, etc). Model P<.001 for all analyses. Nagelkerke R2 ranged from 0.482-0.552.
Table 5.
Logistic regression results for predicting mortality
| Predictor | Sample (n) | Odds Ratio | 95% CI | P Value |
|---|---|---|---|---|
| Initial AM-PAC mobility | All (n=1453) | 0.885 | 0.846-0.925 | <.001 |
| COVID as primary/admitting diagnosis | ||||
| Yes (n=690) | 0.883 | 0.825-0.945 | <.001 | |
| No (n= 761) | 0.883 | 0.830-0.939 | <.001 | |
| ICU | ||||
| Yes (n=519) | 0.940 | 0.885-0.998 | .043 | |
| No (n=929) | 0.867 | 0.809-0.929 | <.001 | |
| Cohort | ||||
| First (n=847) | 0.884 | 0.842-0.929 | <.001 | |
| Second (n=606) | 0.955 | 0.864-1.055 | .362 | |
| Initial AM-PAC Activity | All (n=1200) | 0.877 | 0.835-0.921 | <.001 |
| COVID as primary/admitting diagnosis | ||||
| Yes (n=566) | 0.867 | 0.803-0.937 | <.001 | |
| No (n=613) | 0.878 | 0.820-0.940 | <.001 | |
| ICU | ||||
| Yes (n=447) | 0.907 | 0.843-0.975 | .009 | |
| No (n=730) | 0.862 | 0.803-0.926 | <.001 | |
| Cohort | ||||
| First (n=686) | 0.856 | 0.823-0.917 | <.001 | |
| Second (n=514) | 0.959 | 0.841-1.093 | .533 |
NOTE. Results of the main (sample=all) and subanalyses on different subsets of the cohort (eg, only those with COVID-19 as a primary or admitting diagnosis, etc). Model P<.001 for all analyses. Nagelkerke R2 ranged from 0.449-0.512.
Supplemental Table 3.
Impact of race and medical comorbidities on the prediction of Discharge Destination.
| Predictor | Sample | Odds Ratio | 95% CI | P Value |
|---|---|---|---|---|
| AM-PAC Initial Mobility | Medical Comorbidity | |||
| CCI<=3 (n=624) | 0.818 | 0.772, 0.866 | <0.001 | |
| CCU >=3 (n=618) | 0.898 | 0.865, 0.932 | <0.001 | |
| Race | ||||
| Black (n=699) | 0.890 | 0.856, 0.926 | <0.001 | |
| White + Other (n=543) | 0.844 | 0.805, 0.885 | <0.001 | |
| AM-PAC Initial Activity | Medical Comorbidity | |||
| CCI<=3 (n=523) | 0.806 | 0.751, 0.865 | <0.001 | |
| CCI>3 (n=502) | 0.927 | 0.889, 0.967 | <0.001 | |
| Race | ||||
| Black (n=568) | 0.904 | 0.862, 0.948 | <0.001 | |
| White + Other (n=457) | 0.857 | 0.812, 0.904 | <0.001 |
Supplemental Table 4.
Results of covariate logistic regression model for prediction of Discharge Destination for excluded and included subjects.
| Excluded (n=641) |
Included (n=1242) |
|||||
|---|---|---|---|---|---|---|
| Variable | B | SE | p | B | SE | p |
| Age | 0.841 | 0.362 | 0.020 | 0.542 | 0.190 | 0.004 |
| Sex | 0.189 | 0.332 | 0.569 | 0.084 | 0.162 | 0.605 |
| Race | 0.595 | 0.078 | ||||
| 1 | -0.511 | 0.708 | 0.470 | -0.420 | 0.302 | 0.164 |
| 2 | -0.098 | 0.707 | 0.889 | 0.013 | 0.303 | 0.996 |
| Ethnicity | -0.664 | 0.945 | 0.482 | -1.683 | 0.473 | 0.000 |
| Hospital | 0.000 | 0.000 | ||||
| 1 | -2.008 | 0.534 | 0.000 | -1.345 | 0.299 | 0.000 |
| 2 | -1.687 | 0.516 | 0.001 | -0.444 | 0.284 | 0.119 |
| 3 | -1.499 | 0.527 | 0.004 | -0.444 | 0.298 | 0.136 |
| 4 | -2.876 | 1.110 | 0.010 | -0.457 | 0.323 | 0.157 |
| Length of Stay | 0.072 | 0.028 | 0.009 | 0.075 | 0.010 | 0.000 |
| Cohort | 0.467 | 0.346 | 0.177 | 0.098 | 0.165 | 0.553 |
| COVID Dx | -0.171 | 0.334 | 0.609 | -0.353 | 0.160 | 0.028 |
| Ventilator | 3.309 | 1.335 | 0.013 | 0.703 | 0.307 | 0.022 |
| ICU | -2.528 | 0.865 | 0.003 | 0.139 | 0.210 | 0.509 |
| Insurance | 0.016 | 0.000 | ||||
| 1 | 17.522 | 8072 | 0.998 | 2.373 | 1.868 | 0.204 |
| 2 | 19.263 | 8072 | 0.998 | 3.470 | 1.865 | 0.063 |
| 3 | 15.128 | 8072 | 0.998 | 2.267 | 1.863 | 0.224 |
| 4 | 18.796 | 8072 | 0.998 | 2.391 | 1.926 | 0.214 |
| BMI | -0.005 | 0.020 | 0.801 | 0.005 | 0.009 | 0.564 |
| CCI | 0.149 | 0.057 | 0.009 | 0.067 | 0.026 | 0.010 |
| Constant | -20.25 | 8072 | 0.998 | -4.589 | 1.971 | 0.17 |
For EXCLUDED, Model p <0.001; Nagelkerke R2 = 0.565; Sp = 96.4; Sn = 54.2. For INCLUDED, Model p<0.001; Nagelkerke R2 = 0.419; Sp = 92.1; Sn = 50.0. CODING: Discharge destination (0=home, 1=facility), Age (1=>75); Sex (1=female); Race (0=other, 1=Black, 2=White); Ethnicity (0=non-hispanic, 1=Hispanic); Length of stay (continuous); Cohort (1=second); COVID Dx (1=COVID as admitting or primary diagnosis); Vent (1=yes); ICU (1=yes); Insurance (0=none, 1=Medicaid, 2=Medicare, 3=Private, 4=Other), BMI (continuous), CCI (continuous).
After controlling for the influence of covariates, initial AM-PAC mobility, but not activity, was a significant independent predictor of hospital LOS (see table 4 ). However, its addition to the model had only a modest effect on the accuracy of prediction (see table 2). Each point decrease in mobility score increased the odds that the hospital LOS would be 11 days or longer by 1.04-fold (95% confidence interval [CI], 1.02-1.07). Stratified analysis revealed similar results for AM-PAC mobility score regardless of primary/admitting diagnosis (COVID vs other) and cohort (date of admission in first vs second half of specified time period). However, mobility scores were no longer predictors when the analysis was restricted to those who were admitted to the ICU. Because AM-PAC activity was not a predictor in the primary analysis, additional stratified analyses were not conducted.
Table 4.
Logistic regression results for predicting length of stay
| Predictor | Sample | Odds Ratio | 95% CI | P Value |
|---|---|---|---|---|
| Initial AM-PAC mobility | All (n=1453) | 0.957 | 0.933-0.982 | <.001 |
| COVID-19 as primary/admitting | ||||
| Yes (n=690) | 0.946 | 0.906-0.988 | .012 | |
| No (n=761) | 0.953 | 0.922-0.985 | .004 | |
| ICU | ||||
| Yes (n=519) | 0.983 | 0.944-1.023 | .389 | |
| No (n=929) | 0.930 | 0.899-0.962 | <.001 | |
| Cohort | ||||
| Cohort (n=847) | 0.958 | 0.926-0.991 | .014 | |
| Cohort (n=606) | 0.952 | 0.914-0.991 | .018 | |
| Initial AM-PAC activity | All (n=1200) | 0.980 | 0.951-1.011 | .209 |
| COVID-19 as primary/admitting (n=566) | 0.978 | 0.930-1.029 | .392 |
NOTE. Results of the main (sample=all) and subanalyses on different subsets of the cohort (eg, only those with COVID-19 as a primary or admitting diagnosis, etc). Additional subanalyses using AM-PAC activity score were not conducted because of the lack of significance of the main analysis. Model P<.001 for all analyses. Nagelkerke R2 ranged from 0.481-0.525.
After controlling for the influence of covariates, initial AM-PAC mobility and activity scores were both independent predictors of mortality (see table 5 ). However, their addition did not significantly improve the overall prediction of the model (see table 2). Each point decrease in the initial AM-PAC score increased the odds of in-hospital mortality by 1.13-fold (95% CI, 1.08-1.18) or 1.14-fold (95% CI, 1.09-1.20) for mobility and activity, respectively. Subgroup analysis revealed that AM-PAC demonstrated similar results regardless of primary/admitting diagnosis (COVID vs other), whether or not the individual was admitted to the ICU, and when the analysis was restricted to those in the first cohort. Neither AM-PAC score (mobility or activity) was a predictor of mortality when the analysis was restricted to those in the second cohort. Neither AM-PAC mobility (odds ratio, 0.986; 95% CI, 0.952-1.017) nor activity (odds ratio, 0.989; 95% CI, 0.952-1.027) scores were predictors of readmission.
ROC curves were constructed to evaluate the prognostic ability of AM-PAC mobility and activity scores alone to predict key clinical outcomes, and the results are shown in table 6 . The AUC indicates that AM-PAC mobility and activity scores are strong predictors of discharge destination (0.819-0.847) but weak to moderate predictors of mortality and hospital LOS (0.659-0.679) A threshold score of 17.5 provided a balance of sensitivity and specificity for both mobility and activity scores for predicting discharge destination. ROC curves were not constructed for readmission because the logistic regression indicated AM-PAC scores were not significant predictors of readmission.
Table 6.
Accuracy of prediction from ROC curve analysis
| Outcome | Predictor (Score=17.5) | Area Under the Curve (95% CI) | Sensitivity | Specificity |
|---|---|---|---|---|
| Discharge Destination | Initial mobility | 0.819 (0.781-0.856) | 0.720 | 0.790 |
| Initial activity | 0.822 (0.779-0.864) | 0.769 | 0.743 | |
| Final mobility | 0.840 (0.806-0.874) | 0.774 | 0.832 | |
| Final activity | 0.847 (0.810-0.883) | 0.790 | 0.779 | |
| Length of stay | Mobility | 0.671 (0.627-0.716) | 0.636 | 0.602 |
| Activity | 0.659 (0.611-0.707) | 0.700 | 0.543 | |
| Mortality | Mobility | 0.670 (0.599-0.741) | 0.593 | 0.712 |
| Activity | 0.679 (0.594-0.764) | 0.647 | 0.604 |
NOTE. Accuracy of AM-PAC prediction of key outcomes using AM-PAC mobility and activity scores. Sensitivity and specificity are for a cutoff score of 17.5.
Discussion
These results indicate that AM-PAC “6-Clicks” mobility and activity scores are strong predictors of discharge destination in individuals hospitalized with COVID-19. Strengths of the study include a large sample size from a health system consisting of multiple centers serving urban and suburban areas, including community hospitals and academic medical centers. The results suggest that simple measures of physical function can help guide discharge planning to maximize the efficiency of care delivery in the setting of a global pandemic.
Our results confirm and extend those of other studies demonstrating a link between functional impairments and discharge destination in COVID-19,7 as well those supporting the prognostic significance of AM-PAC scores in mixed13 , 23 and diagnosis-specific patient groups.11 , 24 The similarity in the threshold scores and accuracy of prediction between this and others11, 12, 13 demonstrate that the relationship between AM-PAC scores and discharge destination is robust, and applicable even in the setting of a global pandemic.
We are unaware of other studies assessing the association between physical function and LOS in COVID-19, but Laosa et al9 reported that poor function on admission predicted mortality in those hospitalized in the first month of the pandemic. Although we found AM-PAC scores to be poor predictors of mortality overall, the strength of the association was substantially higher in the first cohort than the second. Thus, the improvements in medical management of COVID-19 appear to have blunted to association between physical function and mortality, which may contribute to the discrepancy. The lack of association between physical function and readmission differs from the results of Bowles et al,8 who studied individuals discharged to home after hospitalization for COVID-19. In contrast, nearly 40% of the individuals in the current study were discharged to a postacute care facility, where it is likely that their medical status was closely monitored, decreasing their risk of rehospitalization. In addition, only readmission to 1 of the 5 hospitals in the UPHS would be captured by our registry. Therefore, our data may underestimate the readmission rate, which may limit our ability to draw conclusions about the relationship between in-hospital physical function and readmission.
Overall, the results of this investigation suggest that AM-PAC scores provide important information that can guide discharge planning, which may reduce costly delays in the transitioning of patients to the appropriate next level of care25 and the rate of hospital readmission.26 Early assessment of mobility can also guide resource allocation decisions. For example, Johnson et al27 found that increased frequency of rehabilitation services improved function at the time of hospital discharge and increased the likelihood of discharge to home. The fact that AM-PAC scores were assessed by multiple disciplines, including nursing, suggests that mobility assessment can provide important information even when physical or occupational therapy are not involved in a patient's care.
Study limitations
Several limitations of this study must be considered. First, all individuals with a positive COVID test were considered for eligibility, regardless of the severity of their COVID-specific symptoms. As a result, some individuals in our sample may have had no or minor symptoms specifically related to COVID-19. However, our sensitivity analysis demonstrated similar results when the analysis was restricted to those whose admitting or primary diagnosis was COVID-19, all of whom presumably had a severe presentation. Second, we did not have information on other factors known to affect the outcomes of interest. Prior living and functional status, marital status, and baseline cognition are all known to affect discharge destination, but those data were not available in our registry. In addition, medical complications that did not require admission to the intensive care or mechanical ventilation were not captured in our data set, and we cannot assess the effect of these factors on our results. Third, only including individuals who had an AM-PAC score documented in their medical record may limit the generalizability of our results to all individuals hospitalized with COVID-19. Although it is unclear what factors might make a clinician more or less likely to implement the AM-PAC assessment in a given patient, the results of our analysis suggest that the potential for significant selection bias is small. Finally, our readmission rates may be underestimates because our registry only included readmission data from hospitals in our system.
Conclusions
In conclusion, AM-PAC “6-Clicks” assessments of mobility and activity are easy to implement, can be completed by multiple disciplines, and provide important prognostic information. Consistent application of the AM-PAC assessments may help to maximize the efficiency of care delivery in this and future pandemics. Future research should assess the ability of other functional measures to predict short- and long-term outcomes in individuals hospitalized with COVID-19. In addition, efforts should be focused on incorporating preexisting guidelines28 for consistent outcome measure use and reporting in this population, which may ultimately improve patient outcomes.
Supplier
-
a
SPSS v26; IBM Corp.
Acknowledgments
We thank William Schweickert, MD; Mark Mikkelsen, MD, MSCE, FCCM; Julianne Jablonski, DNP, RN; Venkat Panchanadam, PhD; Erik Hossain, BS, all from the University of Pennsylvania Health System; Melissa Miller, PhD, MPH and Arteid Memaj, MS, of Arcadia University.
Footnotes
Michael A. Tevald's contribution is supported, in part, by the Foundation for Physical Therapy Research (Acute Care Research Grant 2019), which had no role in the design, conduct, analysis, or interpretation of this study.
Disclosures: none
References
- 1.Johns Hopkins University & Medicine Coronovarus Resource Center. COVID-19 dashboard. Available at: https://coronavirus.jhu.edu/map.html. Accessed June 16, 2021.
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Somani SS, Richter F, Fuster V, et al. Characterization of patients who return to hospital following discharge from hospitalization for COVID-19. J Gen Intern Med. 2020;35:2838–2844. doi: 10.1007/s11606-020-06120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. COVID-19 mortality overview. Available at: https://www.cdc.gov/nchs/covid19/mortality-overview.htm. Accessed June 25, 2021.
- 6.Centers for Disease Control and Prevention. Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Available at:https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed June 25, 2021.
- 7.Roberts P, Wertheimer J, Park E, Nuno M, Riggs R. Identification of functional limitations and discharge destination in patients with COVID-19. Arch Phys Med Rehabil. 2021;102:351–358. doi: 10.1016/j.apmr.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowles KH, McDonald M, Barron Y, Kennedy E, O'Connor M, Mikkelsen M. Surviving COVID-19 after hospital discharge: symptom, functional, and adverse outcomes of home health recipients. Ann Intern Med. 2021;174:316–325. doi: 10.7326/M20-5206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laosa O, Pedraza L, Alvarez-Bustos A, Carnicero JA, Rodriguez-Artalejo F, Rodriguez-Manas L. Rapid assessment at hospital admission of mortality risk from COVID-19: the role of functional status. J Am Med Dir Assoc. 2020;21:1798–1802. doi: 10.1016/j.jamda.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.So C, Lage DE, Slocum CS, Zafonte RD, Schneider JC. Utility of functional metrics assessed during acute care on hospital outcomes: a systematic review. PM R. 2019;11:522–532. doi: 10.1002/pmrj.12013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez N, Gore S, Benson S, Blackwood J. Use of AM-PAC “6 Click” socres to predict discharge location post-hospitalization in adults with cardiovascular disease: a retrospective cohort study. Cardiopulm Phys Ther J. 2020;31:152–158. [Google Scholar]
- 12.Warren M, Knecht J, Verheijde J, Tompkins J. Association of AM-PAC “6-Clicks” basic mobility and daily activity scores with discharge destination. Phys Ther. 2021;101 doi: 10.1093/ptj/pzab043. pzab043. [DOI] [PubMed] [Google Scholar]
- 13.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94:1252–1261. doi: 10.2522/ptj.20130359. [DOI] [PubMed] [Google Scholar]
- 14.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014;94:379–391. doi: 10.2522/ptj.20130199. [DOI] [PubMed] [Google Scholar]
- 15.Hoyer EH, Needham DM, Atanelov L, Knox B, Friedman M, Brotman DJ. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9:277–282. doi: 10.1002/jhm.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jette DU, Stilphen M, Ranganathan VK, Passek S, Frost FS, Jette AM. Interrater reliability of AM-PAC “6-Clicks” basic mobility and daily activity short forms. Phys Ther. 2015;95:758–766. doi: 10.2522/ptj.20140174. [DOI] [PubMed] [Google Scholar]
- 17.Hagg S, Jylhava J, Wang Y, et al. Age, frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. J Am Med Dir Assoc. 2020;21:1555–1559. doi: 10.1016/j.jamda.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiley Z, Ross-Driscoll K, Wang Z, Smothers L, Mehta AK, Patzer RE. Racial and ethnic differences and clinical outcomes of COVID-19 patients presenting to the emergency department. Clin Infect Dis. 2021 Apr 2 doi: 10.1093/cid/ciab290. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asch DA, Islam MN, Sheils NE, et al. Patient and hospital factors associated with differences in mortality rates among Black and White US Medicare beneficiaries hospitalized with COVID-19 infection. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.12842. [DOI] [PubMed] [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Anesi GL, Jablonski J, Harhay MO, et al. Characteristics, outcomes, and trends of patients with COVID-19-related critical illness at a learning health system in the United States. Ann Intern Med. 2021;174:613–621. doi: 10.7326/M20-5327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tabachnick BG, Fidell LS. 4th ed. Allyn and Bacon; Boston: 2001. Using multivariate statistics. [Google Scholar]
- 23.Pfoh ER, Hamilton A, Hu B, Stilphen M, Rothberg MB. The Six-Clicks mobility measure: a useful tool for predicting discharge disposition. Arch Phys Med Rehabil. 2020;101:1199–1203. doi: 10.1016/j.apmr.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 24.Menendez ME, Schumacher CS, Ring D, Freiberg AA, Rubash HE, Kwon YM. Does “6-Clicks” day 1 postoperative mobility score predict discharge disposition after total hip and knee arthroplasties? J Arthroplasty. 2016;31:1916–1920. doi: 10.1016/j.arth.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 25.Raut M, Schein J, Mody S, Grant R, Benson C, Olson W. Estimating the economic impact of a half-day reduction in length of hospital stay among patients with community-acquired pneumonia in the US. Curr Med Res Opin. 2009;25:2151–2157. doi: 10.1185/03007990903102743. [DOI] [PubMed] [Google Scholar]
- 26.Henke RM, Karaca Z, Jackson P, Marder WD, Wong HS. Discharge planning and hospital readmissions. Med Care Res Rev. 2017;74:345–368. doi: 10.1177/1077558716647652. [DOI] [PubMed] [Google Scholar]
- 27.Johnson JK, Lapin B, Green K, Stilphen M. Frequency of physical therapist intervention is associated with mobility status and disposition at hospital discharge for patients with COVID-19. Phys Ther. 2021;101:pzaa181. doi: 10.1093/ptj/pzaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martin R, Botkin R, Campbell A, et al. COVID-19 core outcome measures: American Physical Therapy Association Academies and Sections Consensus Statement. Available at:https://www.apta.org/your-practice/outcomes-measurement/covid-19-core-outcome-measures. Accessed April 14, 2021.