Abstract
Background
This study aimed to compare self-reported changes on lifestyle behaviors during two phases of the COVID-19 pandemic in Spain, and to evaluate clinical and sociodemographic factors associated with lifestyles.
Methods
Two cross-sectional web surveys were conducted during lockdown (April 15-May 15, 2020) and seven months later (November 16-December 16, 2020). Lifestyle behaviors were self-reported by a multidimensional scale (SMILE-C). Two separate samples of respondents were analyzed. A multivariate regression model was performed to evaluate the association of SMILE-C scores with demographic and clinical variables.
Results
The sample comprised, 3412 participants from the first survey (S1) and in the S1 and 3635 from the second (S2). SMILE-C score decreased across surveys (p < 0.001). The rates of positive screenings for depression and anxiety were similar between the surveys, whereas those for alcohol abuse decreased (p < 0.001). Most participants in S2 reported that their lifestyle had not changed compared to those before the pandemic. Variables independently associated with an unhealthier lifestyle were working as an essential worker, lower educational level, previous mental disease, worse self-rated health, totally/moderate changes on diet, sleep or social support, as well as positive screenings for alcohol abuse, anxiety and depression.
Limitations
The cross-sectional design and recruitment by non-probabilistic methods limit inferring causality and the external validity of the results.
Conclusions
Overall lifestyle worsened seven months after the lockdown in Spain. Several demographic and clinical factors were associated with lifestyle scores. The contribution of common mental disorders to unhealthier lifestyles should be considered in order to prevent the negative impact of the pandemic.
Keywords: Lifestyle, Mental health, Web survey, General population, COVID-19
1. Introduction
In the last year, the new coronavirus (SARS-CoV-2) has become a global sanitary emergency. The pandemic itself, and the measures adopted to combat it have changed our lifestyle (Crespo-Facorro, 2020). The consequences are not only measured in the number of lives lost, but also in its economic and social impact (Mcbride et al., 2020; Mofijur et al., 2021; Vieta et al., 2020).
Lifestyle is currently considered a multidimensional construct, which integrates behaviors from nutrition, physical activity, restorative sleep, outdoor activities, substance use, stress management and social support (European Lifestyle Medicine Organization, 2021). Meta-analytical evidence supports that several psychiatric disorders are associated with poorer sleep quality, low levels of physical activity, substance abuse and poor nutritional patterns (Firth et al., 2020b) which are the foundations of the emerging fields of Lifestyle Psychiatry (Firth et al., 2019; García et al., 2020), and Positive Psychiatry (Verdolini and Vieta, 2021).
Growing evidence supports that COVID-19 pandemic has a significant impact on most lifestyle behaviors, especially during populations lockdowns (Branchi and Giulani, 2021; Verdolini et al., 2021). For instance, research across the world estimates the prevalence of sleep disturbances between 21.9 and 55.8% (Cellini et al., 2020; Dal Santo et al., 2021; Ernstsen and Havnen, 2020; Fu et al., 2020; Li et al., 2020) which in turn were significantly associated with anxiety and depressive symptoms (Cellini et al., 2020; Ernstsen and Havnen, 2020; Fu et al., 2020; Li et al., 2020; Smith et al., 2020).
Regarding diet, the lockdown has been associated with a greater adherence to Mediterranean diet compared to before the pandemic (Rodríguez-Pérez et al., 2020), whereas according to other studies energy intake and snacking increased, and diet quality worsened (Batlle-Bayer et al., 2020; Sidor and Rzymski, 2020) during COVID-19 confinement.
Regarding exercise, several studies suggest that almost half of the participants became less active during the quarantine, which in turn was associated with lower subjective well-being and lower health-related quality of life (Suzuki et al., 2020). Engaging in physical activity during confinement has been consistently associated with better outcomes on anxiety or mood disorders worldwide (López-Bueno et al., 2020; Maugeri et al., 2020; Meyer et al., 2020; Morrey et al., 2020; Zhang et al., 2020).
Changes in environmental exposures and increased screen time, such as TV, smartphone, and Internet usage, represent an expected consequence of confinement (Colley et al., 2020; Qin et al., 2020; Rolland et al, 2020; Smith et al., 2020; Wiederhold et al., 2020). Moreover, reducing the use of screen-based devices combined with outdoor exercise had more l benefits for mental health than either healthy behavior alone (Colley et al., 2020).
In a web survey in Belgium, 30.3% participants reported consuming more alcohol, 7.4% stated smoking more than before COVID-19 pandemic, while no significant changes in the consumption of cannabis were found. Boredom, lack of social contacts, loss of daily routines, reward after a hard-working day, and loneliness were reported to be the main reasons for a higher substance use during the pandemic (Vanderbruggen et al., 2020). On the contrary, other studies point to the opportunity posed by COVID to motivate smoking cessation (Jaén-Moreno et al., 2020; Klemperer et al., 2020; Pettigrew et al., 2020).
However, most evidence on lifestyle changes is based on cross-sectional studies conducted during the early stages of the pandemic, whereas a few studies exist on its long-term impact on lifestyle (Salfi et al., 2020; Vogel et al., 2021; Zhang et al., 2020). Given the rapidly changing nature of the COVID-19 pandemic, repeated measurements would provide a better insight on the dynamics of its consequences and their relationship with risk and protective factors. For instance, improvement in sleep problems (Beck et al., 2021), increased physical activity (McCarthy et al., 2021), and worsened feelings of loneliness (Killgore et al., 2020) have been described several months after the confinement across the world.
Moreover, most cross-sectional and longitudinal studies have focused on single or a few lifestyle domains. So far, a handful of studies have assessed lifestyle from a comprehensive, multidimensional perspective (Balanzá-Martínez et al., 2021; Rolland et al., 2020; Stanton et al., 2020; Van Rheenen et al., 2020). In sum, the medium to long term impact of the pandemic on lifestyle, from a multidimensional perspective, is yet to be described.
Based on the above, the main study aim was to compare changes on a wide range of lifestyle behaviors (comprising diet/nutrition, substance use, physical activity, stress management, restorative sleep, social support, and environmental exposures) among general population living in Spain, during two phases of the COVID-19 pandemic: under home confinement/lockdown (April-May) and 7 months later. Secondary objectives were (1) to analyze the association of lifestyle behaviors changes with sociodemographic characteristics and previous history of physical and mental health conditions and (2) to analyze the association of lifestyle and positive screenings for concurrent mental health problems (depression, anxiety, and alcohol abuse).
2. Method
2.1. Study design
Two cross-sectional, online surveys were conducted during two periods: April 15-May 15, 2020 (Survey 1, S1) and November 16- December 16, 2020 (Survey 2, S2). The online questionnaires were programmed in SurveyGizmo®.
The S1 took place one month after the declaration of the state of alarm on March 14, 2020. The restrictions included the suspension of all academic activities and Spanish citizens were obliged to stay at home except to purchase essential items, go to work if they were essential workers, or attend emergencies. During the subsequent waves of the pandemic, restrictions such as home confinement were not issued in Spain. However, social distancing measures were reinforced, the curfew was established, and the mandatory use of a mask and restriction of mobility between territories were imposed. After a peak in early November, the incidence fell to the lowest point on December 10, after which it rised again (Centro Nacional de Epidemiología, 2021). The S2 of this study took place during this intercritical period.
2.2. Study population
The study population included individuals from all over Spain, adults over 18 years from both sexes who had access to the Internet and who agreed to participate in the study after reading the informed consent form (Balanzá-Martínez et al., 2021; De Boni et al., 2020).
2.3. Sample size and recruitment
The survey was disseminated through social networks (Twitter, Facebook, and WhatsApp), and mailing lists, using a snowball sampling. Fundamental parameters were unknown at the moment defining sample size on the S1. Previous experiences with similar surveys were able to recruit a significant number of people. For this reason, instead of defining a sample a priori, a 30 day-period of data collection was specified. The S2 followed the same methods aiming to obtain comparability. To avoid repeated responses, at the very beginning of the survey, participants were specifically asked if they had completed the survey previously. Therefore, repeated responses were eliminated from the final sample.
2.4. Outcome
The main outcome was the total score of the Short Multidimensional Inventory Lifestyle Evaluation (SMILE-C) scale (Balanzá-Martínez et al., 2021). This scale was developed, during one week of confinement in Spain, to approach lifestyle from a multidimensional perspective in a pandemic context. This tool was developed from the original SMILE, which is a self-assessed 43-item questionnaire comprising seven lifestyle habits or domains: diet/nutrition, substance abuse, physical activity, stress management, restorative sleep, social support, and environmental exposure. The original SMILE scale was developed to carry out a multidimensional and comprehensive assessment of the seven (healthy) lifestyle during the pandemic self-isolation.
The SMILE-C scale analyzes lifestyle during the previous 30 days, with a 27 items questionnaire comprising seven domains as mentioned above. Multidimensional evaluations of lifestyle are still scarce. Nutrition, physical activity, and restorative sleep are regarded as fundamental aspects of human health, as well as the three pillars of lifestyle (Firth et al., 2019). However, lifestyle as a construct has evolved to include a wider pattern of behaviors, such as stress management, social support, substance avoidance, and environmental exposure such as screen time and contact with natural spaces. This comprehensive approach is aligned with contemporary views about the multidimensional nature of lifestyle, as defined by scientific societies (European Lifestyle Medicine Organization, 2021).
Response options are measured through a 4-point Likert-type scale and the final score is obtained by the sum of all questions (noting that some questions present reverse scores). The higher the score, the healthier the lifestyle (scores range from 27 to 108). The SMILE-C presents an overall Cronbach-α=0.75 and Kaiser-Meyer-Olkin Measure=0.77 (Balanzá-Martínez et al., 2021).
2.5. Variables and measurements
Sociodemographic information included sex, age, educational level, occupational status, being an essential worker (yes/no), number of people living in the house and self-isolation by contagion or high-risk contact. The COVID-19 questions were related to diagnosis (yes/no) and loss of significant ones (yes/no).
Self-rated health (SRH) was measured using the question “How would you rate your health in general?” with possible answer choices of “Very bad”, “Bad”, “Regular”, “Good” and “Very good” (De Salvo et al., 2006; Idler et al., 1997; Jylhä, 2009). Response options were aggregated into “Very good/Good” and “Regular/Bad/Very bad”.
Change in lifestyle behaviors during the COVID-19 pandemic as compared to before the pandemic was assessed by questions such as: “Did you change your (nutritional habits and diet) during the COVID-19 pandemic?”, with a 4-point Likert-type response (Totally, Moderately, Mildly, Not changes), and aggregated into “Totally/Moderately changes” and “Mild/No changes”. In this case, two groups were created, "Totally/Moderately changes" and "Mild/No changes", for all variables related to lifestyle changes, as some variables had sparse classes. Thus, we grouped qualitatively similar values, with new similar categories for all variables for comparison. Sparse classes were grouped into qualitatively similar values to avoid the problems of large confidence intervals.
To retrospectively assess the direction of changes on lifestyle factors, compared to before pandemic, we used the question “You consider that your (nutritional habits and diet) nowadays are…”, with three possible answers, “as healthy as before”, “healthier than before” or “less healthy than before”.
Previously diagnosed conditions were self-reported using the question “In the last 12 months, have you been diagnosed by a medical doctor or health professional, or received treatment for any of the following conditions?”. Possible health problems investigated include diabetes, heart disease, hypertension, anaemia, asthma, depression, anxiety, schizophrenia, bipolar disorder, anorexia/bulimia nervosa, HIV/AIDS, cancer, tuberculosis, cirrhosis, kidney disease and others.
Current depression was screened using the Patient Health Questionnaire-2 (PHQ-2) (Kroenke et al., 2003) using a cut-off ≥ 3, and current anxiety was screened using the Generalized Anxiety Disorder 7-item (GAD-7) (Spitzer et al., 2006) using a cut-off≥ 10. Two dichotomous variables were created “Positive Depression” and “Positive Anxiety”. Then a composite variable was created using the aforementioned variables with the following categories: no positive screening, positive screening for depression only, positive screening for anxiety only, and positive screening for both. Screening for alcohol abuse was performed using the AUDIT-C (Bush et al., 1998) and cut-off was ≥3. The shorter versions of both instruments were chosen to decrease the length of the online questionnaire, which decreases the burden on the participant and increases the overall quality of the answers/completeness (Biffignandi and Bethlehem, 2021).
2.6. Statistical analysis
Sociodemographics, COVID-19 related questions, SRH, change in lifestyle during the COVID-19 pandemic, self-reported diagnosed conditions, as well as screening for alcohol abuse, depression and anxiety were described by absolute and relative frequencies, stratified by groups (S1 and S2). Distributions between groups (S1 and S2) were compared using the Pearson's chi-squared test. Means and standard deviation were summarized for SMILE-C score and age by groups, using Student's t-test and median and interquartile were summarized for number of the people living in the house, by groups, using Mann-Whitney test. A p-value < 0.05 was considered statistically significant for all tests.
Multivariate linear regression model was performed to evaluate the effect of independent factors on the SMILE-C Score, controlled by S1 and S2. Variables presenting p-value < 0.20 at the bivariate tests (Pearson`s chi-squared test, Student's t-test, and Mann-Whitney test) were considered for regression linear model. Sex, age, and the variable of the first and second survey were defined to be included a priori, either by importance in the literature and adjusting a model that indicates cases related to S1 and S2. Stepwise linear models were performed until reaching the most parsimonious model. The fit of the final model was evaluated by graphical analysis of the residuals, with a quantile-quantile graph destined for normal distribution (qq-plot) and a graph of standardized residues versus the adjusted values, the latter to verify the assumption of constant variance. All the analyzes were conducted in SPSS version 20.
2.7. Ethical aspects
The study was approved by the Ethics Committee at the Hospital Universitari i Politècnic La Fe, in Valencia, Spain (2020-149-1). The surveys were anonymous (no identification -name-, city or IP address was collected) and participants read the consent form and confirmed their interest on participating in the first screen of the online questionnaires.
3. Results
The final sample consisted of 7047 answered surveys, 3412 in the S1 and 3635 in the S2. Initially, a total of 7491 answered surveys were obtained. Among them, 444 were not eligible for the study (207 had already participated in the survey, 77 were not living in Spain, and 160 were younger than 18 years).
Sociodemographic and clinical variables (including screening for depression and anxiety) as well as the SMILE-C scores for both surveys are shown in Table 1 . In both cases, there was a predominance of women among the participants, with a mean age of 40 years in S1 and 44 years in S2. In the S1 unemployed participants predominated, followed by non-essential workers and essential workers, while in the S2 the essential workers predominated, followed by the unemployed and non-essential workers. There was a majority of respondents with a university degree or Bachelor/Professional degree (for further details, see Table 1).
Table 1.
Sociodemographic, clinical characteristics and the mean SMILE-C score among participants (n = 7047) between the two surveys.
| Variables/Categories |
Survey |
p-value | ||||||
|---|---|---|---|---|---|---|---|---|
|
First |
Second |
Totally |
||||||
| n | % | N | % | N | % | |||
| SMILE-Ca | 80.3 (8.22) | 78.7 (8.1) | 79.5 (8.2) | <0.001 | ||||
| Sexb | Male | 1123 | 31.8 | 929 | 26.4 | 2052 | 29.1 | <0.001 |
| Female | 2406 | 68.2 | 2588 | 73.6 | 4994 | 70.9 | ||
| Age | 40 (27-52) | 44 (29-53) | 42 (27–53) | <0.001 | ||||
| Working Status | Not working | 1433 | 40.6 | 1221 | 34.7 | 2654 | 37.7 | <0.001 |
| Working (not as an essential worker) | 1007 | 28.5 | 928 | 26.4 | 1935 | 27.5 | ||
| Working (as an essential worker) | 903 | 25.6 | 1320 | 37.5 | 2223 | 31.5 | ||
| Lost the job during the pandemic | 186 | 5.3 | 49 | 1.4 | 235 | 3.3 | ||
| Education level | Primary/Secondary education | 267 | 7.6 | 273 | 7.8 | 540 | 7.7 | <0.001 |
| Bachelor/Professional degree | 959 | 27.2 | 955 | 27.1 | 1914 | 27.2 | ||
| University degree | 1412 | 40.0 | 1593 | 45.3 | 3005 | 42.6 | ||
| Master/Doctorate degree | 891 | 25.2 | 697 | 19.8 | 1588 | 22.5 | ||
| Median # people living in the house (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) | <0.001 | ||||
| Self-isolation | Yes | 1689 | 48.2 | 101 | 2.9 | 1790 | 25.5 | <0.001 |
| No | 1814 | 51.8 | 3417 | 97.1 | 5231 | 74.5 | ||
| Diagnosed with COvid-19 | Yes | 68 | 1.9 | 290 | 8.2 | 358 | 5.1 | <0.001 |
| No | 3455 | 98.1 | 3228 | 91.8 | 6683 | 94.9 | ||
| Lost somebody in the epidemic | Yes | 337 | 9.6 | 382 | 10.9 | 719 | 10.2 | 0.079 |
| No | 3178 | 90.4 | 3136 | 89.1 | 6314 | 89.8 | ||
| Self-rated healthc | Very good or good | 2524 | 71.7 | 2880 | 81.9 | 5404 | 76.8 | <0.001 |
| Regular, bad or very bad | 994 | 28.3 | 638 | 18.1 | 1632 | 23.2 | ||
| Diagnosed or treated for diabetesd | No | 3348 | 95.4 | 3359 | 95.5 | 6707 | 95.5 | 0.93 |
| Diagnosis or treatment | 160 | 4.6 | 159 | 4.5 | 319 | 4.5 | ||
| Diagnosed or treated for heart disease or hypertensione | No | 3398 | 96.6 | 3146 | 89.4 | 6544 | 93.0 | <0.001 |
| Diagnosis or treatment | 119 | 3.4 | 372 | 10.6 | 491 | 7.0 | ||
| Diagnosed or treated for anaemiaf | No | 3278 | 93.2 | 3258 | 92.6 | 6536 | 92.9 | 0.38 |
| Diagnosis or treatment | 241 | 6.8 | 260 | 7.4 | 501 | 7.1 | ||
| Diagnosed or treated for asthma/bronchitisg | No | 3253 | 92.4 | 3329 | 94.6 | 6582 | 93.5 | <0.001 |
| Diagnosis or treatment | 269 | 7.6 | 189 | 5.4 | 458 | 6.5 | ||
| Diagnosed or treated for depressionh | No | 3209 | 92.2 | 3263 | 92.8 | 6472 | 92.5 | 0.37 |
| Diagnosis or treatment | 272 | 7.8 | 255 | 7.2 | 527 | 7.5 | ||
| Diagnosed or treated for anxietyi | No | 2968 | 85.3 | 2941 | 83.6 | 5909 | 84.5 | 0.048 |
| Diagnosis or treatment | 511 | 14.7 | 577 | 16.4 | 1088 | 15.5 | ||
| Diagnosed or treated for Schizophrenia/bipolar disorder/anorexia/bulimiaj | No | 3463 | 98.8 | 3458 | 98.3 | 6921 | 98.5 | 0.095 |
| Diagnosis or treatment | 43 | 1.2 | 60 | 1.7 | 103 | 1.5 | ||
| Diagnosed or treated for others (HIV/SIDA, tuberculosis, cancer, cirrhosis, kidney disease, other)k | No | 2804 | 80.2 | 2855 | 81.2 | 5659 | 80.7 | 0.32 |
| Diagnosis or treatment | 692 | 19.8 | 663 | 18.8 | 1355 | 19.3 | ||
| Screening for depression and anxiety | Negative for depression/anxiety | 2511 | 71.2 | 2571 | 73.1 | 5082 | 72.1 | 0.072 |
| Positive depression only | 293 | 8.3 | 239 | 6.8 | 532 | 7.5 | ||
| Positive anxiety only | 286 | 8.1 | 265 | 7.5 | 551 | 7.8 | ||
| Positive for both | 439 | 12.4 | 443 | 12.6 | 882 | 12.5 | ||
| Screening for alcohol abuse | Negative | 2440 | 69.1 | 3018 | 85.8 | 5458 | 77.5 | < 0.001 |
| Positive | 1089 | 30.9 | 500 | 14.2 | 1589 | 22.5 | ||
| Chronic diseasel | No | 2537 | 72.6 | 2666 | 75.8 | 5203 | 74.2 | 0.002 |
| Yes | 959 | 27.4 | 852 | 24.2 | 1811 | 25.8 | ||
| Mental healthm | No | 2904 | 83.8 | 2904 | 82.5 | 5808 | 83.2 | 0.17 |
| Yes | 562 | 16.2 | 614 | 17.5 | 1176 | 16.8 | ||
| Infectious diseasen | No | 3506 | 99.6 | 3512 | 99.8 | 7018 | 99.7 | 0.11 |
| Yes | 13 | 0.4 | 6 | 0.2 | 19 | 0.3 | ||
Note: missing values (not answered, not saved...) for
:211;
:1;
:11;
21;
:12;
:10;
:7;
: 48;
: 50;
: 23;
:33;
: 33;
:63;
: 10
Consistent with the restrictions, the percentage of self-isolated participants significantly decreased across surveys. Moreover, the prevalence of individuals diagnosed with COVID-19 significantly increased over time, whereas the rate of responders who had lost a significant one due to COVID-19 did not. Self-rated health (SRH) was better seven months later. No significant differences were found for most self-reported conditions in the previous year, except for heart disease/hypertension and asthma/bronchitis.
Overall lifestyle, as measured with the SMILE-C score, differed across surveys, which suggests the existence of unhealthier lifestyles in S2. In both surveys, more than 70% of participants had a negative screening for depression and anxiety. The rate of positive screenings for depression and/or anxiety were similar between the surveys, whereas a significant decrease in positive screening for alcohol abuse was observed.
Table 2 depicts the self-reported changes on each lifestyle behavior during the two surveys of this study. Significant differences were observed over time in all cases, except for substance use. In terms of magnitude, the greatest decrease in the rate of totally / moderate changes were found in environmental exposure, followed by physical activity. Nevertheless, in both domains these rates remained the highest during S2. Significant decreases were also observed in diet/nutrition, social support, stress management, and especially in restorative sleep.
Table 2.
Self-reported changes in lifestyle behaviors between the two surveys (n = 7047).
| Variables/Categories |
Survey |
Totally | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| First | Second | |||||||
| n | % | n | % | N | % | |||
| Diet and nutritiona | Mild/no changes | 2663 | 75.5 | 2802 | 79.6 | 5465 | 77.6 | <0.001 |
| Totally/moderate changes | 864 | 24.5 | 716 | 20.4 | 1580 | 22.4 | ||
| Substance abuseb | Mild/no changes | 3114 | 89.8 | 3147 | 89.5 | 6261 | 89.6 | 0.669 |
| Totally/moderate changes | 355 | 10.2 | 371 | 10.5 | 726 | 10.4 | ||
| Physical activityc | Mild/no changes | 1106 | 31.4 | 2065 | 58.7 | 3171 | 45.0 | <0.001 |
| Totally/moderate changes | 2420 | 68.6 | 1453 | 41.3 | 3873 | 55.0 | ||
| Stress managementd | Mild/no changes | 2393 | 68.2 | 2518 | 71.6 | 4911 | 69.9 | 0.002 |
| Totally/moderate changes | 1114 | 31.8 | 1000 | 28.4 | 2114 | 30.1 | ||
| Restorative sleepe | Mild/no changes | 2239 | 63.5 | 2819 | 80.1 | 5058 | 71.8 | <0.001 |
| Totally/moderate changes | 1287 | 36.5 | 699 | 19.9 | 1986 | 28.2 | ||
| Social supportf | Mild/no changes | 2245 | 64.8 | 2358 | 67.0 | 4603 | 65.9 | 0.045 |
| Totally/moderate changes | 1221 | 35.2 | 1159 | 33.0 | 2380 | 34.1 | ||
| Environmental exposures (pattern of indoor/outdoor)g | Mild/no changes | 285 | 8.1 | 2204 | 62.6 | 2489 | 35.4 | <0.001 |
| Totally/moderate changes | 3229 | 91.9 | 1314 | 37.4 | 4543 | 64.6 | ||
Note: missing value (not answered, not saved...) for
: 2;
: 60;
:3;
: 22;
: 3;
: 64;
: 15
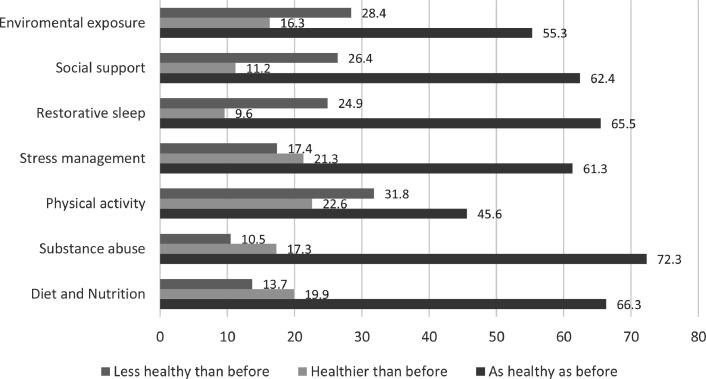
As depicted in Fig. 1 , most participants considered each of their lifestyle behaviors to be as healthy as before the pandemic, except for physical activity (45.6% considered it to be as healthy as before, 31.8% less healthy than before and 22.6% healthier than before).
Fig. 1.
Direction of changes in each lifestyle behavior in the second survey compared to before the pandemic (n = 3635).
Table 3 reports the results obtained from the two surveys for each domain of the SMILE-C. Significant differences were found in all the domain mean scores, except for stress management. In all cases, changes implied a worsening of the lifestyle behaviors, except for environmental exposures, which improved in S2.
Table 3.
Mean scores in the SMILE-C domains in the two surveys (n = 7047).
| Variables/Categories |
Survey |
p-value | |||
|---|---|---|---|---|---|
|
First |
Second |
||||
| n | Mean (SD) | N | Mean (SD) | ||
| Diet and nutritiona | 3497 | 16,01 (2.33) | 3518 | 15.45 (2.16) | <0.001 |
| Substance abuseb | 3509 | 15,34 (1.24) | 3518 | 15.08 (1.39) | <0.001 |
| Physical activityc | 3525 | 2.68 (1.04) | 3518 | 2.52 (0.99) | <0.001 |
| Stress managementd | 3440 | 13.74 (2.71) | 3518 | 13.66 (2.63) | 0.22 |
| Restorative sleepe | 3514 | 11.97 (2.52) | 3518 | 11.83 (2.52) | 0.026 |
| Social supportf | 3443 | 18.82 (3.15) | 3517 | 18.03 (3.40) | <0.001 |
| Environmental exposures (pattern of indoor/outdoor)g | 3529 | 1.84 (0.91) | 3518 | 2.05 (0.97) | <0.001 |
Note: missing value (not answered, not saved...) for
: 32;
: 20;
:4;
: 89;
: 15;
: 87;
: 0
The final adjusted linear regression model is shown in Table 3. The variables that remained independently associated with a healthier lifestyle (i.e., higher SMILE-C scores) were older age, not working, totally/moderate changes on stress management and physical activity, and previous heart disease/hypertension. On the other hand, several variables were independently associated with an unhealthier lifestyle (i.e., lower SMILE-C scores): second survey, working as an essential worker, each educational level below master/doctorate degree, SRH as regular/bad/very bad, totally/moderate changes on diet/nutrition, restorative sleep and social support, as well as previous mental disease. In addition, positive screenings for anxiety, depression (either alone or combined), as well as positive screening for alcohol abuse were associated with lower scores on the SMILE-C.
4. Discussion
The first aim of this study was to compare changes on lifestyle behaviors between two phases of the COVID-19 pandemic in Spain: under confinement and seven months later. Overall lifestyle, evaluated by the SMILE-C scores, worsened in the second survey of this study. To our knowledge, no previous study has evaluated the long-term changes in lifestyle from a multidimensional approach as the pandemic progresses.
Self-reported changes in lifestyle (totally/moderate vs mild /no change) significantly decreased over time for each lifestyle behavior, except for substance use. This might be explained by the strict home confinement measures adopted in Spain early in the pandemic, and the relative softening of the measures seven months later, which allowed a better adaptation to the ‘new normal’.
The most noticeable changes were found in environmental exposures, physical activity and restorative sleep that seem to be the lifestyle behaviors most sensitive to the effects of strict lockdown and mandatory home isolation issued during the early phase of the pandemic. Several studies across the world have also observed the remarkable effects of confinement on these three behaviors (Colley et al., 2020; Dal Santo et al., 2021; Qin et al., 2020; Rolland et al, 2020; Smith et al., 2020; Wiederhold et al., 2020). Moreover, a longitudinal study found a trend towards the disappearance of the sleep disturbances after the lockdown release in France (Beck et al., 2021). Being able to leave the house, either to work, entertain or play sports, seems to be a key change to organize personal routines, which in turn would help to restore sleep-wake rhythms.
Conversely, lesser remarkable changes were observed in diet/nutrition, stress management and social support. A few studies have assessed changes in these lifestyle domains several months apart from the beginning of the current pandemic. For instance, several healthy eating habits that appeared during the early pandemic worsened over time among Chinese population (Zhang et al., 2020), whereas loneliness significantly increased six months later in American general population, which was correlated with depression and suicidal ideation (Killgore et al., 2020).
Regarding the direction of the changes, lifestyle habits during the second survey mostly remained as healthy as before the pandemic. Nevertheless, changes to healthier as well as unhealthier lifestyles were also described by smaller proportions of participants. For behaviors such as environmental exposures, social support, restorative sleep and physical activity, a higher percentage of respondents affirm that their habits were unhealthier than before the pandemic. By contrast, the pandemic would have had a more positive impact on behaviors such as substance abuse, diet/nutrition, and strategies to deal with stress. This variability in responses may result from multiple variables that would act as either risk or resilience factors during the sanitary crisis, as suggested by previous evidence. Indeed, an association was found between pre-pandemic lifestyle and changes on physical activity during the confinement (Martínez-de-Quel et al., 2021; McGrath et al., 2020). Similarly, people with previous obesity showed unhealthier diets, lower rates of physical exercise, and more weight gain during the pandemic (Robinson et al., 2021). According to a longitudinal study, women showed greater long-term resilience than men as the crisis progresses, despite having worse baseline levels of insomnia, anxiety or depression (Salfi et al., 2020). Moreover, sleep disturbances during the early pandemic have been associated with several variables, such as increased worry about COVID-19, lower perceived social support, more severe occupational interference due to COVID-19 and poorer self-reported physical health, the insufficient availability stock of masks (Yu et al., 2020), chronic conditions (Gualano et al., 2020), a higher educational level or a passive coping style (Fu et al., 2020). Further studies are needed to better understand these diverging lifestyle trajectories in order to identify specific vulnerable groups, to whom health promotion actions should be targeted.
After adjusting for confounders, substantial changes in all behaviors except environmental exposures, were associated with lifestyle as a whole, as measured by the SMILE-C scores. On the one hand, totally/moderate changes in restorative sleep, diet/nutrition, social support, and substance use were independently associated with an unhealthier lifestyle. In contrast, changes in strategies to deal with stress and engagement in physical activity were associated with a healthier lifestyle. This interrelation between the different lifestyle behaviors, in response to a stressful situation such as the pandemic, has not received much research attention to date. In this regard, the results suggest that less physical activity, more sedentary behavior (including an increased sleep time) and poorer diet quality would be interconnected (Pellegrini et al., 2020; Vogel et al., 2021; Zheng et al., 2020), a phenomenon known as ‘multiple health behavior change’ (Geller et al., 2017).
One of the secondary aims of the present research was to analyze the association of lifestyle changes with sociodemographic characteristics and previous history of physical and mental health conditions. Being older, but not gender, was associated with a healthier lifestyle. A higher educational level was significantly associated with healthier lifestyle habits. This finding might be explained by the likely higher health literacy among the more educated participants (Yamashita and Kunkel, 2015). The findings regarding working status were more counterintuitive. Unexpectedly, being unemployed was associated with a healthier lifestyle. Having more leisure time for personal care or the absence of stressors associated with work, among other factors, may play a role in this regard.
Regarding previously diagnosed conditions, heart disease/hypertension was associated with a healthier lifestyle, whereas previous mental illness was associated with a poorer lifestyle. In a recent web survey, participants without a psychiatric condition were found to show more adaptive coping strategies such as following a routine, talking to significant ones, engaging in physical exercise or keeping a balanced diet. By contrast, gaining weight, sleep changes, and tobacco smoking were more prevalent among those with a mental illness (Solé et al., 2021).
Finally, poor self-rated health (SRH) was independently associated with an unhealthier lifestyle. Moreover, the improvement in self-perceived health status after seven months of the pandemic is also remarkable, even more taking into account that lifestyle worsened in parallel. SRH is a complex parameter that approaches health from a subjective perspective. Moreover, multiple variables can exert an influence on SRH, which makes obtaining counterintuitive results likely. Previous crises, such as the worldwide financial crisis in 2008, showed that despite the socioeconomic consequences, the SRH improved while the mental health risk increased, for instance in Spain (Urbanos-Garrido and Lopez-Valcarcel, 2014). Conversely, in other European countries, the changes in the SRH were in the opposite direction during the same crisis (Abebe et al., 2016).
In the present study, a global improvement in SRH was observed in the second survey, while the lifestyle worsened. However, we believe that causality cannot be obtained from the coexistence of two temporal trends. Even less when, after controlling the covariates, an independent relationship was found between the worsening of the SRH and the SMILE-C scores.
The current COVID-19 crisis has stressed the primary care health system as never before in Spain (de Nicolás Jiménez et al., 2020) The increase in the caseload focused on the community control of the pandemic might have decreased the healthcare providers´ attention to the diagnosis and treatment of chronic diseases such as hypertension. In addition, being afraid of infection could have limited patients´ attendance at medical appointments during the pandemic, which in turn may have delayed diagnoses or even not detecting them. The results of our study are in line with recent reviews showing a decrease in the number of hospitalizations due to ischemic heart disease during the COVID-19 pandemic (Seidu et al., 2021).
Several observational studies have consistently shown that the relationship between lifestyles and mental health is bidirectional in nature (Firth et al., 2019,2020a). During the COVID-19 pandemic, research has mostly focused on the role of lifestyle behaviors as either risk or protective factors for common mental health symptoms and disorders (Bendau et al., 2021; Cellini et al., 2020; Fullana et al., 2020; Lu et al., 2020; Novotný et al., 2020; Pham et al., 2020; Santabárbara et al., 2020; Stanton et al., 2020). Growing evidence supports that diet (Fullana et al., 2020; Pham et al., 2020), physical activity (Lu et al., 2020), and other lifestyle behaviors (Cellini et al., 2020; Santabárbara et al., 2020; Stanton et al., 2020) are significant predictors of anxiety and/or depression. Conversely, much less studies have examined the reverse direction. Increased depressive and anxiety states early in the pandemic were associated with poorer outcomes in specific lifestyles, e.g. dietary habits and sleep health (Al-Ajlouni et al., 2020; Amatori et al., 2020). In our study, positive screenings for anxiety and/or depression were among the most relevant predictors of an unhealthier lifestyle as a whole. This finding confirms that the concurrent existence of common mental disorders may also influence lifestyles in the general population during pandemic times and expands this relationship from the multidimensional and longer-term perspectives.
The present results should be considered in light of some limitations. Firstly, the non-probabilistic nature of the sample makes it difficult to generalize the results to the entire Spanish population. Moreover, it is likely that a high percentage of participants were healthcare workers, with a higher level of education and a higher gender imbalance. In addition, the limited access to online surveys and the dissemination via social networks may limit the scope of the survey to specific population groups. However, there is growing evidence that supports the usefulness of these sources of information, especially in confined or difficult-to-access populations (Sun et al., 2020), when traditional research is complex to carry out. Secondly, this study uses repeated cross-sectional surveys, with two different samples at two points in time, and does not follow up the same cohort over time. Despite having used the same recruitment method for both surveys, some sociodemographic and clinical variables have been distributed differently between the samples, which could generate a bias when comparing the results. The use of multivariate linear regression would attempt to control a posteriori the possible bias that these differences could generate. Hence, it is not possible to infer causality and the associations must be interpreted cautiously. Thirdly, mental disorders (depression, anxiety, alcohol abuse) were assessed with screening instruments, which are not equivalent to a proper clinical diagnosis. In addition, it should be noted that the scores of the different domains of the SMILE-C should be interpreted with caution, because their psychometric validity to measure each domain independently has not yet been demonstrated. Nevertheless, they are validated for the reference population and are commonly used in web surveys. Fourthly, the formulation of the question about changes in the different lifestyle behaviors (Table 2) is not the most appropriate as it does not accurately reflect the direction of change. Lastly, research based on self-reported data could favor information bias due to the social desirability effect and memory error. In some retrospective questions, such as that about the direction of change, memory bias cannot be entirely ruled out. In this regard, studies with objective measures of lifestyle are needed to provide more valuable information (Sun et al., 2020).
Table 4.
Multivariable linear regression evaluating variables associated with higher SMILE-C score during the two surveys (n = 7047).
| Variables | B |
95.0% C.I. |
p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Survey | <0.001 | |||
| First | Reference | - | - | |
| Second | -2.51 | -2.91 | -2.12 | |
| Sex | 0.57 | |||
| Male | Reference | - | - | |
| Female | 0.11 | -0.26 | 0.47 | |
| Age | 0.02 | 0.01 | 0.03 | 0,004 |
| Working Status | ||||
| Not working | 1.77 | 1.35 | 2.20 | <0.001 |
| Working (not as an essential worker) | Reference | - | - | - |
| Working (as an essential worker) | -0.92 | -1.34 | -0.50 | <0.001 |
| Lost the job during the pandemic | 0.54 | -0.42 | 1.50 | 0.27 |
| Education level | ||||
| Primary/Secondary education | -3.18 | -3.89 | -2.47 | <0.001 |
| Bachelor/Professional degree | -1.82 | -2.31 | -1.34 | <0.001 |
| University degree | -0.85 | -1.27 | -0.43 | <0.001 |
| Master/Doctorate degree | Reference | - | - | - |
| Self-isolation | 0.14 | |||
| No | -0.33 | -0.78 | 0.11 | |
| Yes | Reference | - | - | |
| Self-rated health | <0.001 | |||
| Very good or good | Reference | - | - | |
| Regular, bad or very bad | -4.57 | -4.99 | -4.16 | |
| Screening for depression and anxiety | ||||
| Negative for depression and anxiety | Reference | - | - | - |
| Positive for depression only | -4.31 | -4.93 | -3.68 | <0.001 |
| Positive for anxiety only | -3.48 | -4.10 | -2.86 | <0.001 |
| Positive for depression and anxiety | -7.20 | -7.75 | -6.64 | <0.001 |
| Screening for alcohol abuse | <0.001 | |||
| Negative | Reference | - | - | |
| Positive | -1.1 | -1.50 | -0.71 | |
| Diet and nutrition | ||||
| Mild/no changes | Reference | - | - | |
| Totally/moderate changes | -1.40 | -1.80 | -1.00 | <0.001 |
| Stress management | ||||
| Mild/no changes | Reference | - | - | |
| Totally/moderate changes | 1.54 | 1.16 | 1.91 | <0.001 |
| Restorative sleep | ||||
| Mild/no changes | Reference | - | - | |
| Totally/moderate changes | -2.47 | -2.86 | -2.08 | <0.001 |
| Social support | ||||
| Mild/no changes | Reference | - | - | |
| Totally/moderate changes | -0.521 | -0.87 | -0.17 | 0.004 |
| Physical activity | ||||
| Mild/no changes | Reference | - | - | |
| Totally/moderate changes | 0.48 | 0.13 | 0.84 | 0.007 |
| Mental Disease | ||||
| No | Reference | - | - | |
| Yes | -1.30 | -1.77 | -0.84 | <0.001 |
| Diagnosed/treated for heart disease/hypertension | ||||
| No | Reference | - | - | |
| Diagnosis or treatment | 1.03 | 0.37 | 1.69 | 0.002 |
Positive B indicates increase in the SMILE-C score (better lifestyle), while negative B indicates decrease in the SMILE-C score (worse lifestyle).
Despite these limitations, this is one of the first studies to assess the longer-term impact of the COVID-19 pandemic on lifestyle and mental health in the general population, with important implications for the pandemic aftermath (Vieta et al., 2020). In addition, the use of a multidimensional scale allows a comprehensive and holistic approach to lifestyle, which aligns with contemporary perspectives (European Lifestyle Medicine Organization, 2021). Unlike most web surveys, we also collected health-related data of the participants, including previously diagnosed medical and psychiatric conditions, self-perceived health, and personal information regarding the COVID-19. In the context of a spreading pandemic, the present findings are innovative and timely.
In sum, lifestyle as a whole worsened seven months after the first confinement in Spain. The proportion of relevant changes in most lifestyle behaviors decreased in the second survey. In addition, most of participants in the second survey reported that their habits had not changed from before the pandemic. However, the responses were very heterogeneous, which suggests that the long-term evolution of lifestyles over time may be complex and in no case deterministic but is probably influenced by multiple variables. Moreover, our findings support the bidirectional relationship between lifestyle behaviors and mental health. The specific contribution of common mental disorders to unhealthier lifestyles should be further explored and taken into account when developing public health campaigns addressed to prevent the negative emotional impact of the pandemic.
Role of the Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Jose Cervera-Martínez: Formal analysis, Writing – original draft, Funding acquisition, Writing – review & editing. Beatriz Atienza-Carbonell: Funding acquisition, Writing – review & editing. Jurema C. Mota: Formal analysis, Writing – review & editing. Teresa Bobes-Bascarán: Funding acquisition, Writing – review & editing. Benedicto Crespo-Facorro: Funding acquisition, Writing – review & editing. Cristina Esteban: Funding acquisition, Writing – review & editing. María Paz García-Portilla: Funding acquisition, Writing – review & editing. Susana Gomes-da-Costa: Funding acquisition, Writing – review & editing. Ana González-Pinto: Funding acquisition, Writing – review & editing. M. José Jaén-Moreno: Funding acquisition, Writing – review & editing. Fernando Sarramea: Funding acquisition, Writing – review & editing. Eduard Vieta: Funding acquisition, Writing – review & editing. Iñaki Zorrilla: Funding acquisition, Writing – review & editing. Rafael Tabarés-Seisdedos: Funding acquisition, Writing – review & editing. Flavio Kapczinski: Visualization, Writing – review & editing. Raquel B. De Boni: Visualization, Writing – review & editing. Vicent Balanzá-Martínez: Formal analysis, Writing – original draft, Visualization, Writing – review & editing.
Declaration of Competing Interest
SVBM has received grants and served as consultant, advisor or continuing medical education (CME) speaker during the last 5 years for the following entities: Angelini Spain, Angelini Portugal, Bristol-Myers-Squibb, Ferrer, Janssen, Juste, Lundbeck, Nutrición Médica, and Otsuka.
JC-M has served as continuing medical education (CME) speaker during the last years for Otsuka.
EV has received grants and served as consultant, advisor or CME speaker for the following entities (unrelated to the present work): AB-Biotics, Abbott, Allergan, Angelini, Celon, Dainippon Sumitomo Pharma, Ferrer, Gedeon Richter, GH Research. Janssen, Lundbeck, Otsuka, Sage, Sanofi-Aventis, and Takeda.
SGC has received CME-related honoraria, or consulting fees from Janssen-Cilag, Italfarmaco, Angelini and Lundbeck and reports no financial or other relationship relevant to the subject of this article.
AGP has received grants and served as consultant, advisor or CME speaker for the following entities: Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Sanofi-Aventis, Alter, Angelini, Exeltis, Takeda, the Spanish Ministry of Science and Innovation (CIBERSAM), the Ministry of Science (Carlos III Institute), the Basque Government, and the European Framework Program of Research.
CE has received grants and served as consultant, advisor or CME speaker during the last 5 years for the following entities: Janssen-Cilag, Lundbeck, Otsuka and Casen Recordati.
BCF has received unrestricted research funding from Instituto de Salud Carlos III, MINECO, Gobierno de Cantabria, Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), from the 7th European Union Framework Program and Lundbeck. He has also received honoraria for his participation as a consultant and/or as a speaker at educational events from ADAMED, Mylan, Angelini, Janssen Johnson & Johnson, Lundbeck, and Otsuka Pharmaceuticals.
IZ has received grants and served as consultant, advisor or CME speaker for the following entities: Janssen-Cilag, Lundbeck, Otsuka, Angelini, Takeda
The remaining authors have no conflicts to declare.
Acknowledgments
The authors would like to thank Gabriel Madeira for programming the questionnaires. We are also thankful to all the anonymous individuals and the press departments of Universitat de València and CIBERSAM for their help in disseminating the surveys. We are enormously grateful to all the participants.
VBM acknowledges the national grant PI16/01770 from the Instituto de Salud Carlos III, ISCIII (The PROBILIFE study).
RBDB is grateful for long-term funding from the Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) (E-26/203.154/2017) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (312543/2020-4).
EV thanks the support of the Spanish Ministry of Science and Innovation (PI15/00283, PI18/00805) integrated into the Plan Nacional de I+D+I and co-financed by the ISCIII-Subdirección General de Evaluación and the Fondo Europeo de Desarrollo Regional (FEDER); the Instituto de Salud Carlos III; the CIBER of Mental Health (CIBERSAM); the Secretaria d'Universitats i Recerca del Departament d'Economia i Coneixement (2017 SGR 1365), the CERCA Programme, and the Departament de Salut de la Generalitat de Catalunya for the PERIS grant SLT006/17/00357.
References
- Abebe D.S., Tøge A.G., Dahl E. Individual-level changes in self-rated health before and during the economic crisis in Europe. Int. J. Equity Health. 2016;15(1) doi: 10.1186/s12939-015-0290-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Ajlouni Y.A., Park S.H., Alawa J., Shamaileh G., Bawab A., El-Sadr W.M., Duncan D.T. Anxiety and depressive symptoms are associated with poor sleep health during a period of COVID-19-induced nationwide lockdown: a cross-sectional analysis of adults in jordan. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-041995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amatori S., Donati Zeppa S., Preti A., Gervasi M., Gobbi E., Ferrini F., Sisti D. Dietary habits and psychological states during COVID-19 home isolation in Italian college students: the role of physical exercise. Nutrients. 2020;12(12):3660. doi: 10.3390/nu12123660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balanzá-Martínez V., Kapczinski F., de Azevedo Cardoso T., Atienza-Carbonell B., Rosa A.R., Mota J.C., De Boni R.B. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Rev. Psiquiatr. Salud Ment. 2021;14(1):16–26. doi: 10.1016/j.rpsm.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batlle-Bayer L., Aldaco R., Bala A., Puig R., Laso J., Margallo M., Fullana-I-Palmer P. Environmental and nutritional impacts of dietary changes in Spain during the COVID-19 lockdown. Sci. Total Environ. 2020;748 doi: 10.1016/j.scitotenv.2020.141410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck F., Leger D., Cortaredona S., Verger P., Peretti-Watel P., COCONEL group. Would we recover better sleep at the end of covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2021;78:115–119. doi: 10.1016/j.sleep.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2021;11(2):e01964. doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biffignandi S., Bethlehem J. 2.a ed. Wiley; 2021. Handbook of Web Surveys (Wiley Handbooks in Survey Methodology) (English Edition) [Google Scholar]
- Branchi I., Giuliani A. Shaping therapeutic trajectories in mental health: instructive vs. permissive causality. Eur. Neuropsychopharmacol. 2021;43:1–9. doi: 10.1016/j.euroneuro.2020.12.001. [DOI] [PubMed] [Google Scholar]
- Bush K., Kivlahan D.R., McDonell M.B., Fihn S.D., Bradley K.A. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Arch. Intern. Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020;29(4):e13074. doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centro Nacional de Epidemiología, 2021, COVID-19 en España, Retrieved from https://cnecovid.isciii.es/ (accessed on 31 March 2021).
- Colley R.C., Bushnik T., Langlois K. Exercise and screen time during the COVID-19 pandemic. Health Rep. 2020;31(6):3–11. doi: 10.25318/82-003-x202000600001-eng. [DOI] [PubMed] [Google Scholar]
- Crespo-Facorro B. Mental health and the SARS-CoV-2 pandemic. Rev. Psiquiatr. Salud Ment. 2020;13(2):55–56. doi: 10.1016/j.rpsm.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dal Santo F., González-Blanco L., Rodríguez-Revuelta J., Marina González P.A., Paniagua G., García-Álvarez L., Bobes J. Early impact of the COVID-19 outbreak on sleep in a large Spanish sample. Behav. Sleep Med. 2021:1–16. doi: 10.1080/15402002.2021.1890597. [DOI] [PubMed] [Google Scholar]
- De Boni R.B., Balanzá-Martínez V., Mota J.C., Cardoso T.A., Ballester P., Atienza-Carbonell B., Kapczinski F. Depression, anxiety, and lifestyle among essential workers: a web survey from brazil and Spain during the COVID-19 pandemic. J. Med. Internet Res. 2020;22(10):e22835. doi: 10.2196/22835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Nicolás Jiménez J.M., Blázquez Recio L.M., Fabregat Domínguez M.T., Palomo Cobos L. COVID-19 y esfuerzo asistencial en atención primaria. Aten. Primaria. 2020;52(8):588–590. doi: 10.1016/j.aprim.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSalvo K.B., Bloser N., Reynolds K., He J., Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J. Gen. Intern. Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernstsen L., Havnen A. Mental health and sleep disturbances in physically active adults during the COVID-19 lockdown in Norway: does change in physical activity level matter? Sleep Med. 2020 doi: 10.1016/j.sleep.2020.08.030. [DOI] [PubMed] [Google Scholar]
- European Lifestyle Medicine Organization. What is lifestyle medicine? Retrieved from https://www.eulm.org/what-is-lifestyle-medicine. (Accessed on 3 May 2021).
- Firth J., Gangwisch J.E., Borisini A., Wootton R.E., Mayer E.A. Food and mood: how do diet and nutrition affect mental wellbeing? BMJ. 2020;369:m2382. doi: 10.1136/bmj.m2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Solmi M., Wootton R.E., Vancampfort D., Schuch F.B., Hoare E., Stubbs B. A meta-review of "lifestyle psychiatry": the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 2020;19(3):360–380. doi: 10.1002/wps.20773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Ward P.B., Stubbs B. Editorial: lifestyle psychiatry. Front. Psychiatry. 2019;10:597. doi: 10.3389/fpsyt.2019.00597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., Mao J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry. 2020;10(1):225. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullana M.A., Hidalgo-Mazzei D., Vieta E., Radua J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020;275:80–81. doi: 10.1016/j.jad.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García S., Gorostegi-Anduaga I., García-Corres E., Maldonado-Martín S., MacDowell K.S., Bermúdez-Ampudia C., González-Pinto A. Functionality and neurocognition in patients with bipolar disorder after a physical-exercise program (FINEXT-BD study): protocol of a randomized interventionist program. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.568455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller K., Lippke S., Nigg C.R. Future directions of multiple behavior change research. J. Behav. Med. 2017;40(1):194–202. doi: 10.1007/s10865-016-9809-8. [DOI] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Public Health. 2020;17(13):4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E.L., Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J. Health Soc. Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Jaen-Moreno M.J., Sarramea F., Balanzá-Martínez V. Smoking cessation in severe mental illness: challenges and opportunities in the COVID-19 times. Adicciones. 2020;0(0):1579. doi: 10.20882/adicciones.1579. [Dejar de fumar en el trastorno mental grave: desafíos y oportunidades en tiempos de la COVID-1] [DOI] [PubMed] [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Lucas D.A., Dailey N.S. Loneliness during the first half-year of COVID-19 lockdowns. Psychiatry Res. 2020;294 doi: 10.1016/j.psychres.2020.113551. [DOI] [PubMed] [Google Scholar]
- Klemperer E.M., West J.C., Peasley-Miklus C., Villanti A.C. Change in tobacco and electronic cigarette use and motivation to quit in response to COVID-19. Nicotine Tob. Res. 2020;22(9):1662–1663. doi: 10.1093/ntr/ntaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The patient health questionnaire-2: validity of a two-item depression screener. Med. Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Li D.J., Ko N.Y., Chen Y.L., Wang P.W., Chang Y.P., Yen C.F., Lu W.H. COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: a Facebook survey. Int. J. Environ. Res. Public Health. 2020;17(12):4479. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Bueno R., Calatayud J., Ezzatvar Y., Casajús J.A., Smith L., Andersen L.L., López-Sánchez G.F. Association between current physical activity and current perceived anxiety and mood in the initial phase of COVID-19 confinement. Front. Psychiatry. 2020;11:729. doi: 10.3389/fpsyt.2020.00729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C., Chi X., Liang K., Chen S.T., Huang L., Guo T., Zou L. Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol. Res. Behav. Manag. 2020;13:1223–1233. doi: 10.2147/PRBM.S284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-de-Quel Ó., Suárez-Iglesias D., López-Flores M., Pérez C.A. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: a longitudinal study. Appetite. 2021;158 doi: 10.1016/j.appet.2020.105019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maugeri G., Castrogiovanni P., Battaglia G., Pippi R., D'Agata V., Palma A., Musumeci G. The impact of physical activity on psychological health during covid-19 pandemic in Italy. Heliyon. 2020;6(6):e04315. doi: 10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride O., Murphy J., Shevlin M., Gibson-Miller J., Hartman T.K., Hyland P., Bentall R.P. Monitoring the psychological, social, and economic impact of the COVID-19 pandemic in the population: context, design and conduct of the longitudinal COVID-19 psychological research consortium (C19PRC) study. Int. J. Methods Psychiatr. Res. 2020:e1861. doi: 10.1002/mpr.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy H., Potts H.W.W., Fisher A. Physical activity behavior before, during, and after COVID-19 restrictions: longitudinal smartphone-tracking study of adults in the United Kingdom. J. Med. Internet Res. 2021;23(2):e23701. doi: 10.2196/23701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath A., Murphy N., Richardson N. The impact of the COVID-19 pandemic on the wellbeing of Irish men's shed members. Health Promot. Int. 2020 doi: 10.1093/heapro/daaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J., McDowell C., Lansing J., Brower C., Smith L., Tully M., Herring M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health. 2020;17(18):E6469. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mofijur M., Fattah I.M.R., Alam M.A., Islam A.B.M.S., Ong H.C., Rahman S.M.A., Mahlia T.M.I. Impact of COVID-19 on the social, economic, environmental and energy domains: lessons learnt from a global pandemic. Sustain. Prod. Consum. 2021;26:343–359. doi: 10.1016/j.spc.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrey L.B., Roberts W.O., Wichser L. Exercise-related mental health problems and solutions during the COVID-19 pandemic. Curr. Sports Med. Rep. 2020;19(6):194–195. doi: 10.1249/JSR.0000000000000725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novotný J.S., Gonzalez-Rivas J.P., Kunzová Š., Skladaná M., Pospíšilová A., Polcrová A., Stokin G.B. Risk factors underlying COVID-19 lockdown-induced mental distress. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.603014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini M., Ponzo V., Rosato R., Scumaci E., Goitre I., Benso A., Bo S. Changes in weight and nutritional habits in adults with obesity during the "lockdown" period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7):2016. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew S., Jun M., Roberts I., Bullen C., Nallaiah K., Rodgers A. Preferences for tobacco cessation information and support during covid-19. J. Addict. Med. 2020 doi: 10.1097/ADM.0000000000000743. [DOI] [PubMed] [Google Scholar]
- Pham K.M., Pham L.V., Phan D.T., Tran T.V., Nguyen H.C., Nguyen M.H., Duong T.V. Healthy dietary intake behavior potentially modifies the negative effect of COVID-19 lockdown on depression: a hospital and health center survey. Front. Nutr. 2020;7 doi: 10.3389/fnut.2020.581043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin F., Song Y., Nassis G.P., Zhao L., Dong Y., Zhao C., Zhao J. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in china. Int. J. Environ. Res. Public Health. 2020;17(14):5170. doi: 10.3390/ijerph17145170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., Hardman C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156 doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Pérez C., Molina-Montes E., Verardo V., Artacho R., García-Villanova B., Guerra-Hernández E.J., Ruíz-López M.D. Changes in dietary behaviors during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients. 2020;12(6):1730. doi: 10.3390/nu12061730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: survey study. JMIR Public Health Surveill. 2020;6(3):e19630. doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi F., Lauriola M., Amicucci G., Corigliano D., Viselli L., Tempesta D., Ferrara M. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol. Stress. 2020;13 doi: 10.1016/j.ynstr.2020.100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Lasheras I., Lipnicki D.M., Bueno-Notivol J., Pérez-Moreno M., López-Antón R., Gracia-García P. Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020;109 doi: 10.1016/j.pnpbp.2020.110207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidu S., Kunutsor S.K., Cos X., Khunti K. Indirect impact of the COVID-19 pandemic on hospitalisations for cardiometabolic conditions and their management: a systematic review. Prim. Care Diabetes. 2021;15(4):653–681. doi: 10.1016/j.pcd.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12(6):1657. doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L., Jacob L., Trott M., Yakkundi A., Butler L., Barnett Y., Tully M.A. The association between screen time and mental health during COVID-19: a cross sectional study. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L., Jacob L., Yakkundi A., McDermott D., Armstrong N.C., Barnett Y., Tully M.A. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: a cross-sectional study of UK-based respondents. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solé B., Verdolini N., Amoretti S., Montejo L., Rosa A.R., Hogg B., Torrent C. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY. J. Affect. Disord. 2021;281:13–23. doi: 10.1016/j.jad.2020.11.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stanton R., To Q.G., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., Vandelanotte C. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., Folarin A.A., Ranjan Y., Rashid Z., Conde P., Stewart C., RADAR-CNS Consortium Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J. Med. Internet Res. 2020;22(9):e19992. doi: 10.2196/19992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki Y., Maeda N., Hirado D., Shirakawa T., Urabe Y. Physical activity changes and its risk factors among community-dwelling Japanese older adults during the COVID-19 epidemic: associations with subjective well-being and health-related quality of life. Int. J. Environ. Res. Public Health. 2020;17(18):E6591. doi: 10.3390/ijerph17186591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanos-Garrido R.M., Lopez-Valcarcel B.G. The influence of the economic crisis on the association between unemployment and health: an empirical analysis for Spain. Eur. J. Health Econ. 2014;16(2):175–184. doi: 10.1007/s10198-014-0563-y. [DOI] [PubMed] [Google Scholar]
- Van Rheenen T.E., Meyer D., Neill E., Phillipou A., Tan E.J., Toh W.L., Rossell S.L. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: initial results from the COLLATE project. J. Affect. Disord. 2020;275:69–77. doi: 10.1016/j.jad.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderbruggen N., Matthys F., Van Laere S., Zeeuws D., Santermans L., Van den Ameele S., Crunelle C.L. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur. Addict. Res. 2020:1–7. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdolini N., Amoretti S., Montejo L., García-Rizo C., Hogg B., Mezquida G., Solé B. Resilience and mental health during the COVID-19 pandemic. J. Affect. Disord. 2021;283:156–164. doi: 10.1016/j.jad.2021.01.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdolini N., Vieta E. Resilience, prevention and positive psychiatry. Acta Psychiatr. Scand. 2021;143(4):281–283. doi: 10.1111/acps.13288. [DOI] [PubMed] [Google Scholar]
- Vieta E., Pérez V., Arango C. Psychiatry in the aftermath of COVID-19. Rev. Psiquiatr. Salud Ment. 2020;13(2):105–110. doi: 10.1016/j.rpsm.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel E.A., Zhang J.S., Peng K., Heaney C.A., Lu Y., Lounsbury D., Prochaska J.J. Physical activity and stress management during COVID-19: a longitudinal survey study. Psychol. Health. 2021:1–11. doi: 10.1080/08870446.2020.1869740. [DOI] [PubMed] [Google Scholar]
- Wiederhold B.K. Children's screen time during the COVID-19 pandemic: boundaries and etiquette. Cyberpsychol. Behav. Soc. Netw. 2020;23(6):359–360. doi: 10.1089/cyber.2020.29185.bkw. [DOI] [PubMed] [Google Scholar]
- Yamashita T., Kunkel S.R. An international comparison of the association among literacy, education, and health across the United States, Canada, Switzerland, Italy, Norway, and Bermuda: implications for health disparities. J. Health Commun. 2015;20(4):406–415. doi: 10.1080/10810730.2014.977469. [DOI] [PubMed] [Google Scholar]
- Yu B.Y., Yeung W.F., Lam J.C., Yuen S.C., Lam S.C., Chung V.C., Ho J.Y. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep Med. 2020;74:18–24. doi: 10.1016/j.sleep.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Zhao A., Ke Y., Huo S., Ma Y., Zhang Y., Liu K. Dietary behaviors in the post-lockdown period and its effects on dietary diversity: the second stage of a nutrition survey in a longitudinal Chinese study in the COVID-19 era. Nutrients. 2020;12(11):3269. doi: 10.3390/nu12113269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhang H., Ma X., Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in china. Int. J. Environ. Res. Public Health. 2020;17(10):3722. doi: 10.3390/ijerph17103722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Huang W.Y., Sheridan S., Sit C.H., Chen X.K., Wong S.H. COVID-19 pandemic brings a sedentary lifestyle in young adults: a cross-sectional and longitudinal study. Int. J. Environ. Res. Public Health. 2020;17(17):6035. doi: 10.3390/ijerph17176035. [DOI] [PMC free article] [PubMed] [Google Scholar]