Abstract
Background and Aims:
The simultaneous use of alcohol and cannabis (“simultaneous alcohol and marijuana [SAM] use”) is common among young adults and associated with negative substance-related consequences. SAM use may be tied to fluctuating mood states such as negative affect and individual characteristics including trait level of anxiety and sex. However, little is understood about their collective role. In this study, we sought to understand the daily link between SAM use and negative affect and whether this link might differ by both trait anxiety and sex.
Method:
Participants were 154 young adults (57.8% female, 72.7% White, M age = 20.2) who completed baseline surveys on trait anxiety symptoms and up to 14 consecutive daily surveys on their substance use and affective states.
Results:
Multilevel models tested for associations of type of substance use day (i.e., alcohol-only days, cannabis-only days, and no use days relative to SAM use days) with next-day negative affect. Three-way and lower order interactions were tested for substance use day type, anxiety, and sex. Two three-way interactions between cannabis-only days, anxiety, and sex and between alcohol-only days, anxiety, and sex emerged such that SAM use was associated with greater next-day negative affect relative to single substance use days particularly among female participants with elevated anxiety.
Conclusions:
Anxiety and sex are salient factors in the link between SAM use relative to single-substance use and daily negative affect. Study findings reinforce the need to account for all of these factors in order to develop maximally efficacious substance use interventions.
Keywords: simultaneous alcohol and cannabis use, daily diary, affect, anxiety, sex differences
Young adult substance use patterns have shifted in recent years. While rates of heavy drinking have plateaued or declined, rates of regular cannabis use have increased among individuals in this age group (Schulenberg et al., 2020). Historical changes have also been observed for the way in which young adults use alcohol and cannabis. Combining alcohol and cannabis such that the effects of both substances overlap – or simultaneous alcohol and marijuana (SAM) use – is reported by 30% of adult drinkers in their early 20s and is on the rise among early- and mid-young adults who use alcohol (Terry-McElrath & Patrick, 2018). Individuals who report SAM use tend to engage in heavier substance use and tend to be at greater risk for negative consequences (e.g., Jackson et al., 2020; Linden-Carmichael et al., 2019; Midanik et al., 2007; Terry-McElrath et al., 2014; Yurasek et al., 2017). Recent diary work has extended between-person comparisons by conducting within-person comparisons of days when the same individual used only alcohol or only cannabis and days the same individual used both simultaneously, documenting poorer outcomes on SAM days such as heavier substance use (Lee et al., 2020) and increased risk for acute harms (Linden-Carmichael et al., 2020; Sokolovsky et al., 2020). While examining the role of SAM use on level of substance use and acute harms is critical for identifying potentially higher-risk substance use days, far less attention has been placed on identifying day- and person-level factors associated with SAM use.
Numerous well-established theories including the self-medication hypothesis (Khantzian, 1997), tension-reduction hypothesis (Conger, 1956), and motivational model of alcohol use (Cooper et al., 1995; Cox & Klinger, 1988), theorize a strong link between negative affect (NA) and substance use. These theoretical models posit that individuals may drink or use other substances to alleviate negative mood states. Indeed, in diary studies, affect is an established correlate of alcohol use at the within-person level among undergraduate student and community samples (e.g., Armeli et al., 2003; Bresin et al., 2018; Russell et al., 2020). Affect is also linked to cannabis use at the within-person level among diverse community samples and young adult medical outpatients (e.g., Buckner et al., 2015; Ross et al., 2018). A growing body of work evaluating existing theories such as the tension reduction hypothesis have examined the cyclical process in which using alcohol to cope is negatively reinforced (Baker et al., 2004; Hussong et al., 2001), documenting that NA may also increase following heavy substance use (e.g., Hussong et al., 2001). Gleaning from theoretical models of relapse prevention (Collins, 1993; Marlatt & Gordon, 1980, 1985), some individuals may experience a limit violation effect whereby they experience higher levels of NA following particularly heavy or excessive use occasions. Indeed, recent work examining substance use and next-day NA has found decreases in NA during/shortly after using alcohol but increases in NA the following day (Cronce et al., 2020; Devenney et al., 2019).
While the cyclical process of NA and substance use has been observed when studying heavy drinking occasions and next-day NA among social drinkers (e.g., Muraven et al., 2005) and evening heavy drinking and cannabis use predicting next-day emotion regulation strategies (Weiss et al., 2017), limited work has examined the link between SAM use and NA. Of the limited work available, it appears that affect may be particularly tied to SAM use. Specifically, findings from a laboratory-based study of healthy volunteers revealed that alcohol and cannabis use can interact to alter mood at the within-person level, producing positive subjective mood states shortly after combining (Lukas & Orozco, 2001). Cross-sectional evidence concurs with these findings: broadly defined, polysubstance use is associated with poorer mental health, including anxiety (Morley et al., 2015). Although no studies have examined associations between anxiety and SAM use specifically, anxiety disorders often co-occur with alcohol and cannabis use disorders (Lai et al., 2015). Data from the National Alcohol Study revealed SAM use was strongly associated with increased odds of depression relative to heavy alcohol use alone, which was unassociated with depression (Midanik et al., 2007). In a recent diary study of community-recruited young adults, higher motivations of using substances to cope, such as to reduce anxiety, were associated with increased odds of within-person SAM use relative to alcohol use alone (Patrick et al., 2019). Although these findings may suggest that engagement in SAM use is perceived to acutely alleviate NA states, when assessed across a longer time scale SAM use may actually increase NA states relative to individual substances. This seems particularly likely given the other acute harms such as adverse physical effects (e.g., hangover), social-interpersonal consequences (e.g., arguments), and negative cognitive outcomes (e.g., blacking out) that have been documented to be more prevalent on SAM days relative to single-substance use days (Linden-Carmichael et al., 2020; Sokolovsky et al., 2020). The role of SAM use relative to individual substance use or no substance use has not yet been examined.
In investigating the association between SAM use and NA, it is also imperative to identify for whom the association between SAM use and NA is most salient. As noted, polysubstance use is associated with poorer mental health symptoms including anxiety (Morley et al., 2015) and may be a critical factor in the link between SAM use and NA. Trait anxiety in particular refers to an individual’s predisposition to experience anxious states, characterized by physiological arousal and feelings of apprehension, fear, nervousness, and tension (Spielberger, 1966). In addition to the strong association between trait and state anxiety, individuals with elevated trait anxiety also experience more general negative affective states such as anger, disgust, and guilt in daily life (Merz & Roesch, 2011). Drawing upon alcohol literature, trait anxiety has been shown to moderate the association between negative mood and alcohol use, such that higher trait anxiety levels were associated with greater decreases in nervousness after alcohol consumption (Swendsen et al., 2000). Trait anxiety may, therefore, exacerbate the daily links between SAM use and NA. Further, sex has also been observed as a significant moderator of the NA and alcohol use link, such that alcohol use was associated with lower NA in moments of distress, but only among female participants (Simons et al., 2017). Addressing for whom the link between SAM use and NA is most relevant will aid in refining and targeting interventions for young adults who may be motivated to use substances to cope.
Current Study
The current study examined associations between SAM use and next-day NA. Using daily diary data, we contrasted level of NA on days when the same individuals reported no substance use, only alcohol use, only cannabis use, or SAM use. Aim 1 was to examine the association between SAM use and next-day NA. Given prior work suggesting that SAM days are associated with poorer next-day outcomes, it was hypothesized that NA would be higher following SAM days relative to no substance use days and other substance use days. Aim 2 sought to test trait anxiety and sex as moderators of the link between SAM use and next-day NA. We tested two-way interactions between type of substance use day (SAM vs. alcohol-only; SAM vs. cannabis-only; SAM vs. no substance use) and anxiety, and three-way interactions between type of use day, anxiety, and sex, predicting next-day NA. Drawing from separate lines of work indicating that the links among trait anxiety, day-level NA, and day-level substance use vary as a function of sex (e.g., Simons et al., 2017, Swendsen et al., 2000), we hypothesized that the association between SAM use and next-day NA would be stronger for individuals with higher trait levels of anxiety, particularly female participants.
Material and Methods
Participants and Procedure
Participants were young adults (ages 18–25) who reported past-month SAM use and past-two-week binge drinking (4+/5+ drinks in one sitting for female/male participants) to ensure we would obtain enough reports substance use days across the two-week period to be powered for statistical analyses. Participants were recruited via flyers and a university online research database in the Northeastern region of the U.S., near a large, public university. Interested individuals completed a brief online screener to determine eligibility and, if eligible and consented to participate, were immediately invited to complete a baseline survey. After completing the baseline survey, participants were e-mailed instructions for completing the daily diary portion of the study.
Brief, daily online surveys were collected across 14 consecutive days in October 2018-March 2019 in a state where recreational cannabis use was illegal. Participants were sent e-mail/text reminders to complete their survey at 9:00 AM regarding yesterday’s behaviors and today’s mood with 95% of daily surveys completed between 9:00 AM and 12:00 PM. Participants received up to $48 for completing the baseline and daily surveys. Compliance for the daily surveys was high with participants completing an average of 13.13 (SD = 1.95) surveys per person. One hundred and sixty-one eligible participants completed the baseline survey. Only participants who completed 1+ daily survey were included in analyses (n = 154). Of our analytic sample, participants were primarily female (57.8%). M age was 20.24 (SD = 1.45) years. Regarding race/ethnicity, 72.7% of participants identified as Non-Hispanic/Latinx (NHL) White, 11.7% identified as NHL Asian, 6.5% identified as NHL Black, 3.3% identified as NHL multiracial, 3.9% identified as Hispanic/Latinx White, and 2.0% did not report on their racial/ethnic identity. Regarding college status, 88.3% were currently attending college and 11.7% were not currently attending or had never attended college. Additional details can be found in the description of the parent study (Linden-Carmichael et al., 2020).
Baseline Measures
Trait anxiety.
The Brief Symptom Inventory (BSI-18; Derogatis, 2001) assessed past-two-week anxiety, depression, and somatic symptoms. Participants indicated how much each problem bothered or distressed them with responses ranging from 0 (not at all) to 4 (extremely). The six-item anxiety subscale was used for the current study by summing scores across items such as “feeling fearful”, “feeling tense or keyed up,” or “nervousness or shakiness inside.” Cronbach’s α was 0.87.
Daily Measures
Type of substance use day.
Provided with a list of a wide range of substances, participants checked all substances they used the day prior. Days when participants did not indicate any substance use (including alcohol, cannabis, nicotine, etc.) were coded as non-substance use days. Days when participants reported alcohol use and no other substance use were coded as alcohol-only days. Days with cannabis use and no other substance use were coded as cannabis-only days. On days when participants reported alcohol and cannabis use, they were asked a follow-up question of, “Did you use alcohol and marijuana together at the same time, such that the effects overlapped?” Days when they positively endorsed this item were coded as SAM days1.
Negative affect.
Each day, participants were provided with the 20-item Positive and Negative Affect Schedule (Watson et al., 1988). Participants indicated the extent to which they currently experienced different feelings and emotions with responses ranging from 1 (very slightly/not at all) to 5 (extremely). Ten items assessing NA (e.g., irritable, nervous) were summed to form the daily NA score (Cronbach’s α = 0.90).
Covariates.
Day of the week was included as a covariate: Thursday-Saturday were coded as weekend days (1); Sunday-Wednesday were coded as weekdays (0; e.g., Del Boca et al., 2004). Person-specific proportions of cannabis-only and alcohol-only days were calculated as a ratio of the individual’s number of that type of substance use day relative to their total number of cannabis-only, alcohol-only, or SAM use days. Sex was coded as 0 = female, 1 = male.
Analytic Plan
Multilevel modeling was used to address both research aims as it accounts for nonindependence of observations and can accommodate unequal numbers of measurement occasions across individuals (Hox, 2010). First, we calculated descriptive statistics for study variables across only days when participants reported no substance use, alcohol-only, cannabis-only, or SAM use, yielding 1,833 person-days across 154 individuals. We then modeled next-day NA as a function of type of day (no substance use vs. any [alcohol-only, cannabis-only, SAM] substance use). Specifically, day t NA was reported on day t, and day t substance use was reported on day t +1.
To address Aim 1, a main-effect model (Model 1) was estimated to examine differences in next-day NA, respectively, on alcohol-only days, cannabis-only days, and no substance use days relative to SAM days. In these models, Level-1 predictors were indicators of alcohol-only day, cannabis-only day, no substance use day, and weekend. Alcohol-only, cannabis-only, and no substance use day indicators were dummy-coded such that SAM days were the reference day type. To separate within-person and between-person effects for type of substance use day, three variables representing person-specific proportions of cannabis-only days, alcohol-only days, and no substance use days were included as covariates at Level-2. Models were based on data from person-days on which individuals reported alcohol-only use, cannabis-only use, SAM use, or no substance use, resulting in 1830 observations from 154 individuals. Random intercepts were included in models to allow person-mean level of NA to vary across individuals.
To address Aim 2 regarding differences in associations between type of substance use day and next-day NA as a function of trait anxiety level and sex, we estimated models in a stepwise manner. Random intercepts were estimated to allow mean NA to vary between individuals. Level-1 predictors were within-person indicators of alcohol-only day, cannabis-only day, no substance use day, and weekend, and Level-2 predictors were trait anxiety, sex (0 = female, 1 = male), and person-specific proportions of cannabis-only, alcohol-only days, and no substance use days. In Model 2, two-way cross-level interactions between alcohol-only days and anxiety, cannabis-only days and anxiety, and no substance use days and anxiety were added to predict next-day NA. In Model 3, the three three-way interactions between type of substance use day, anxiety, and sex, and lower order interactions were included to predict next-day NA.
Results
Descriptive statistics are reported in Table 1. Results from a descriptive multilevel model in which next-day NA was regressed onto substance use day (0 = no substance use, 1 = alcohol-only, cannabis-only, or SAM use) revealed that on average, NA was higher following non-substance use days relative to days when individuals engaged in alcohol-only, cannabis-only, or SAM use (γ = −0.69, SE = 0.24, p = .005).
Table 1.
Descriptive Statistics of Key Study Variables
| n days | M (SD) | Range | |
|---|---|---|---|
| Day-Level Variables | |||
| No Substance Use | 871 | -- | -- |
| Alcohol-only | 377 | -- | -- |
| Cannabis-only | 368 | -- | -- |
| SAM Use | 217 | -- | -- |
| Negative Affect (females) | -- | 16.22 (6.61) | 10.00 – 47.00 |
| Negative Affect (males) | -- | 15.37 (6.09) | 10.00 – 39.00 |
| Baseline Variables | |||
| Trait Anxiety (females) | -- | 4.43 (4.35) | 0.00 – 18.00 |
| Trait Anxiety (males) | -- | 3.45 (3.98) | 0.00 – 18.00 |
Notes. Means and standard deviations for negative affect are aggregated across all person-days. SAM use = simultaneous alcohol and marijuana use. Statistics are based on N=154 individuals across 1,833 person-days.
Aim 1: SAM Use and Next-Day NA
As shown in Table 2, overall associations between both Level-1 (substance use day type, weekend) and Level-2 (proportion of substance use day type) predictors with next-day NA (Model 1) were not significant. Specifically, in Model 1, the non-significant within-person effect for alcohol-only days suggests that next-day NA did not significantly differ on alcohol-only and SAM days after adjusting for day of the week and individuals’ person-specific proportion of alcohol-only days. Similarly, the within-person effect for cannabis-only days suggests that next-day NA did not differ between cannabis-only and SAM days after adjusting for day of the week and individuals’ person-specific proportion of cannabis-only days. The within-person effect for no substance use days suggests that there was no difference in next-day NA between no substance use and SAM days after adjusting for day of the week and individuals’ person-specific proportion of no substance use days. Further, the proportions of alcohol-only/cannabis-only/no substance use days that a given individual reported was unassociated with next-day NA.
Table 2.
Associations between Type of Substance Use Day, Anxiety, and Sex and Next-Day Negative Affect
| Next-Day Negative Affect | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| γ | SE | γ | SE | γ | SE | |
| Fixed Effects | ||||||
| Intercept | 14.74*** | 2.70 | 11.61*** | 2.37 | 11.08*** | 2.43 |
| Level 1 | ||||||
| Alc Only | 0.16 | 0.43 | 0.06 | 0.58 | 1.54† | 0.80 |
| Can Only | −0.05 | 0.39 | 0.13 | 0.52 | 1.13 | 0.77 |
| No SU | 0.57 | 0.41 | 0.88 | 0.54 | 1.37† | 0.75 |
| Weekend | −0.33 | 0.21 | −0.31 | 0.21 | −0.31 | 0.21 |
| Level 2 | ||||||
| Prop. Alc | −0.30 | 3.27 | −1.28 | 2.80 | −1.25 | 2.79 |
| Prop. Can | 0.00 | 4.04 | 0.17 | 3.44 | 0.16 | 3.42 |
| Prop. No SU | 2.59 | 2.93 | 3.26 | 2.51 | 3.27 | 2.50 |
| Anxiety | 0.66*** | 0.10 | 0.71*** | 0.14 | ||
| Sex | 0.54 | 0.73 | 1.59 | 1.27 | ||
| Cross-Level | ||||||
| Alc X Anxiety | 0.02 | 0.09 | −0.16 | 0.12 | ||
| Can X Anxiety | −0.04 | 0.08 | −0.22† | 0.12 | ||
| No SU X Anxiety | −0.07 | 0.09 | −0.13 | 0.11 | ||
| Alc X Sex | −3.22** | 1.15 | ||||
| Can X Sex | −1.82† | 1.02 | ||||
| No SU X Sex | −0.86 | 1.05 | ||||
| Anxiety X Sex | −0.12 | 0.21 | ||||
| Alc X Anxiety X Sex | 0.45* | 0.20 | ||||
| Can X Anxiety X Sex | 0.34* | 0.17 | ||||
| No SU X Anxiety X Sex | 0.11 | 0.18 | ||||
| Random Effects | ||||||
| Intercept Variance | 24.33*** | 2.98 | 17.05*** | 2.13 | 16.90*** | 2.11 |
| Residual Variance | 17.01*** | 0.59 | 16.97*** | 0.59 | 16.85*** | 0.58 |
Note.
p < .001.
p <.01.
p < .05.
p < .10.
Data are limited to person-days on which individuals reported using alcohol-only, cannabis-only, alcohol and cannabis simultaneously (SAM), or no substance use. Alc = Alcohol-only day; coded 1 = alcohol-only day, 0 = SAM day. Can = Cannabis-only day; coded 1 = cannabis-only, 0 = SAM day. No SU = No substance use day; coded 1 = no substance use, 0 = SAM day. Prop. Alc/Can/No SU = Person-specific proportion of alcohol-only/cannabis-only/no substance use days; person i’s number of alcohol-only/cannabis-only/No SU days divided by the total number of days person i reported alcohol-only, cannabis-only, SAM use, or no substance use. Sex is coded 0 = female, 1 = male. Weekend is coded 0 = Sunday – Wednesday, 1 = Thursday – Saturday. Models predicting next-day negative affect were based on 1830 observations from 154 individuals.
Aim 2: Moderation by Anxiety and Sex
The results for the stepwise models used to test hypotheses regarding differential links between type of substance use day and NA based on trait anxiety and sex are shown in Table 2 (Models 2 and 3, respectively).
For Model 2, only trait anxiety was significantly associated with next-day NA: on average, each unit increase in anxiety was associated with NA that was 0.66 units higher the following day, adjusting for covariates. None of the two-way interactions added in Model 2 (alcohol-only day X anxiety, cannabis-only day X anxiety, no substance use day X anxiety) were statistically significant.
In Model 3, there were trends for within-person effects for alcohol only days and no substance use days, and as in Model 2, trait anxiety was statistically significant. There were also trend-level two-way interactions between cannabis-only days and anxiety (γ = −0.22, SE = 0.12, p = .06) and between cannabis-only days and sex (γ = −1.82, SE = 1.02, p = .08), and a significant two-way interaction between alcohol-only days and sex (γ = −3.22, SE = 1.15, p = .005). These effects were qualified by a statistically significant three-way interaction between cannabis-only days, anxiety, and sex (γ = 0.34, SE = 0.17, p = .039) and between alcohol-only days, anxiety, and sex (γ = 0.45, SE = 0.20, p = .026). As demonstrated in Figure 1, the simple slopes for the three-way interaction between cannabis-only days, anxiety, and sex revealed that for female participants, a one-unit increase in trait anxiety was associated with NA that was 0.71 units higher following SAM days, and 0.49 units higher following cannabis-only days. In contrast, for male participants, a one-unit increase in anxiety symptoms was associated with NA that was 0.59 units higher following SAM days, and 0.71 units higher following cannabis-only days. As shown in Figure 2, the simple slopes for the three-way interaction between alcohol-only days, anxiety, and sex suggested that for female participants, a one-unit increase in anxiety corresponded to NA that was 0.55 units higher following alcohol-only days, and for male participants, a one-unit increase in anxiety corresponded to NA that was 0.88 units higher following alcohol-only days.
Figure 1.
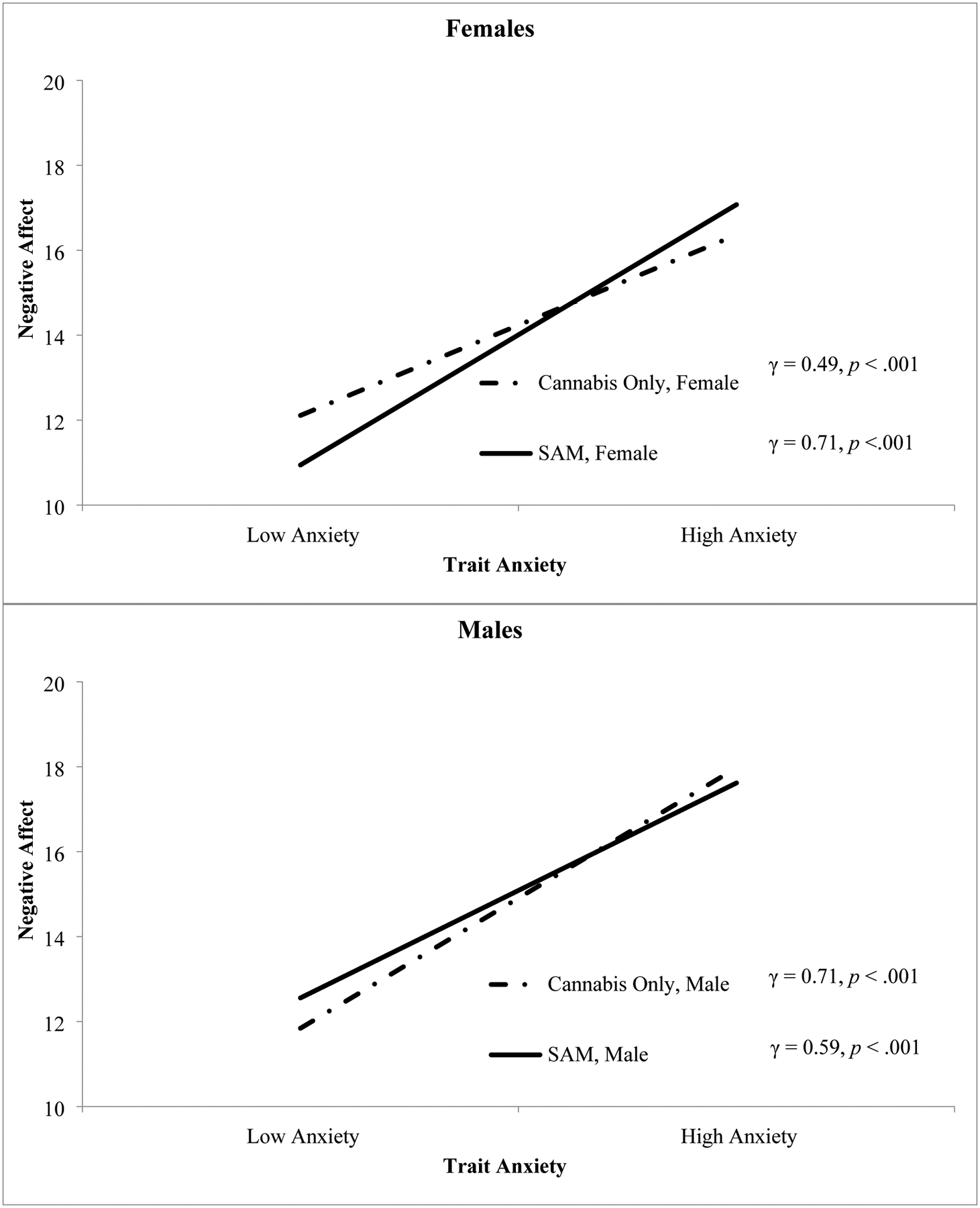
Simple slopes derived from Model 3 to facilitate interpretation of the three-way interaction between cannabis-only days, trait anxiety, and sex predicting next-day negative affect. Low and high anxiety were defined as one standard deviation below and above the mean, respectively.
Figure 2.
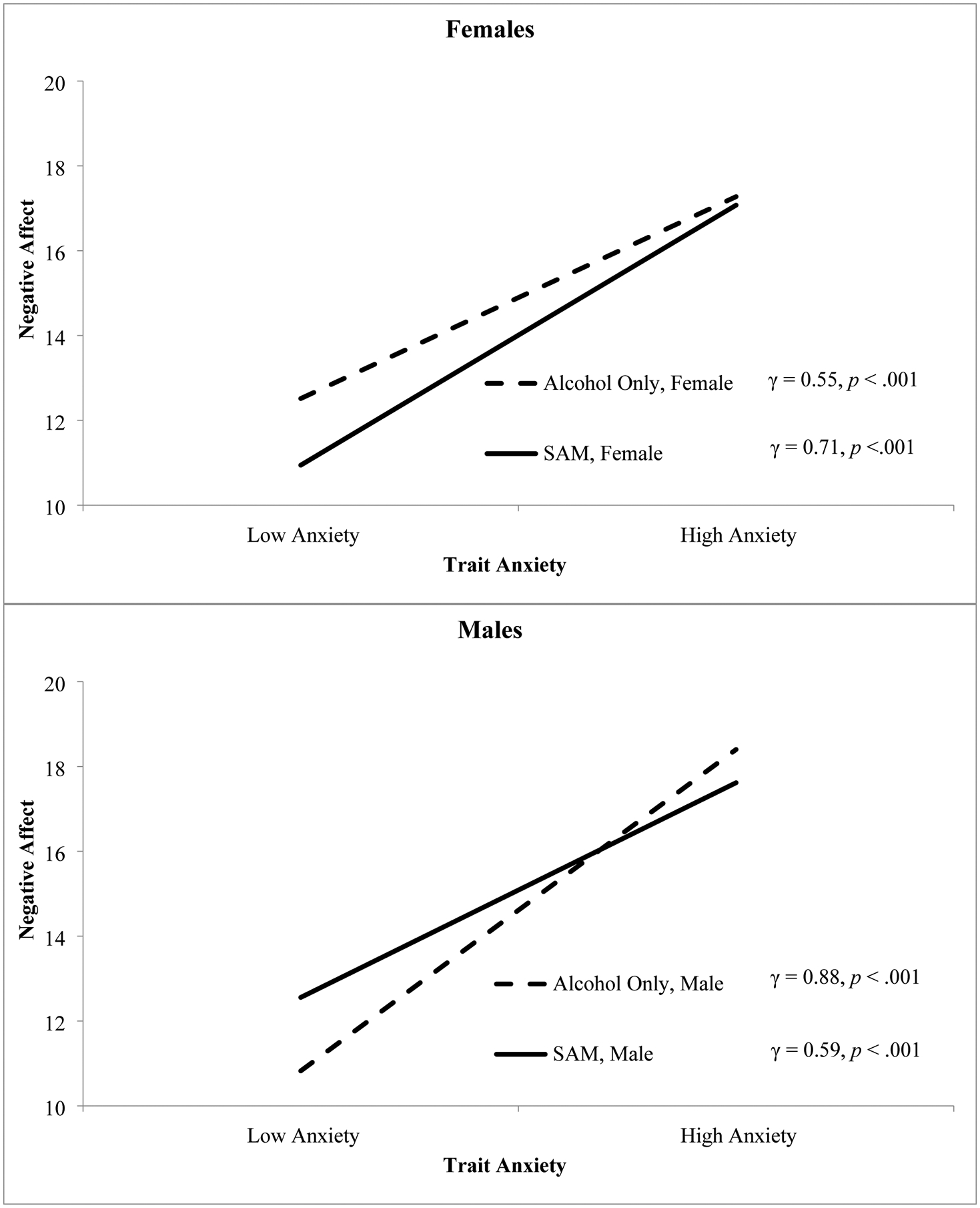
Simple slopes derived from Model 3 to facilitate interpretation of the three-way interaction between alcohol-only days, trait anxiety, and sex predicting next-day negative affect. Low and high anxiety were defined as one standard deviation below and above the mean, respectively.
Conclusions
The current study examined day-level associations between SAM use and NA and the role of trait anxiety and sex in this association. Findings revealed that the interaction between anxiety and SAM use relative to cannabis-only days and relative to alcohol-only days was significantly different for male and female participants. Specifically, SAM use was particularly associated with greater next-day NA among female participants with elevated anxiety. Although there was a main effect of trait anxiety on next-day NA, the lack of main effects for SAM use suggests that SAM use was unrelated to elevated next-day NA relative to alcohol-only, cannabis-only, or no substance use days. By itself, the lack of statistically significant main effects of SAM use on NA might suggest individuals who engage in SAM use experience similar levels of NA following different types of substance use and no substance use days. However, the significant three-way interaction predicting next-day NA highlights that such an interpretation overlooks key subgroup differences in who is experiencing NA, and when this occurs in relation to their substance use.
Based on prior work showing worsened affect and compounded negative consequences on SAM use days relative to days where either substance is used independently (Linden-Carmichael et al., 2020; Patrick et al., 2019), SAM use days were expected to be linked with greater next-day NA. The broader literature on anxiety, NA, and sex in relation to alcohol or cannabis use further suggested two- and three-way interactions (Cooper & Haney, 2014; Khan et al., 2013; Patrick et al., 2016; Wycoff et al., 2018). The significant three-way interaction supports this literature, indicating sex differences in the compounding effect of using alcohol and cannabis simultaneously on next-day NA. For female participants, elevated anxiety was associated with worsened NA following SAM days relative to cannabis-only or alcohol-only days. Male participants had an opposite pattern, such that anxiety was associated with worsened next-day NA more so following alcohol-only or cannabis-only days relative to SAM days. Recent work has shown that female young adults’ NA may be exacerbated by rumination, female young adults may experience greater momentary NA relief from alcohol or cannabis consumption, and female young adults are more likely to develop use-related disorders through internalizing pathways (Cooper & Haney, 2014; Simons et al., 2017). While the results of the current study are preliminary, it appears that among female participants with elevated anxiety, SAM use may be particularly linked to experiences of next-day NA. Future work would benefit from examining the long-term impacts of SAM use and NA in this population.
The current findings may have intervention implications targeting high-risk substance use among young adults with elevated anxiety. To date, prior work has noted that some promising interventions that have effectively reduced either alcohol or cannabis use, have not effectively reduced use of both substances (e.g., Stein et al., 2018; White et al., 2015). Likewise, substance use interventions that do not account for sex or pre-existing anxiety may be less effective. A large body of work has highlighted the consequences of SAM use and regular binge drinking (Jackson et al., 2020; Linden-Carmichael et al., 2019; Yurasek et al., 2017). Our findings extend this work on more general associations to offer implications for targeted intervention efforts for young adults who may perceive these behaviors to be normative and benign (White et al., 2019). For example, findings indicate a specific effect of SAM use on next-day NA among female participants with elevated trait anxiety; understanding sex differences in these associations may inform best practices to help young adults reduce high-risk use behaviors and avoid increasing their NA. Female participants with elevated anxiety, who may present with more severe, treatment-resistant substance use problems, may benefit more from approaches other than common group therapy formats for substance use (Book et al., 2009; Buckner & Carroll, 2010; Sherman et al., 2017). The current findings reinforce the need to account for all of these factors to effectively intervene (Turner et al., 2018). Consistent with evidence that substance use and NA vary considerably within and across days, a clear next step is to evaluate these patterns with more fine-grained assessments (e.g., ecological momentary assessment; Bekiroglu et al., 2017; Slavish et al., 2019). Such momentary designs could capture NA and substance use multiple times throughout a day to examine potential reciprocal associations between NA and SAM use as the episode unfolds, and how these associations differ for other types of use episodes such as cannabis only. Analyzing such data using a cross-lagged panel model, while taking into account the multilevel structure with days nested within individuals and potential unequal spacing between observations, could advance understanding of directionality of the SAM-NA association.
The current study should be considered in light of several limitations. First, while daily diary data may have limited retrospective self-report biases, evidence suggests that momentary fluctuations in affect may provide key insight into periods of risk for, and reinforcement of, substance use patterns (Goodman et al., 2018; Simons et al., 2017). It is possible that NA immediately preceding a use event would have differentiated SAM use from alcohol-only or cannabis-only use occasions. As noted, future work that incorporates more fine-grained assessments with higher-risk populations such as young adults who engage in SAM use, is needed. Such work would also be poised to consider the role of social contexts as well as more specific anxiety profiles/symptom clusters at the person (e.g., generalized anxiety vs. social anxiety), day, and momentary (e.g., social anxiety in response to a specific context/interaction) levels (Armeli et al., 2003; Wycoff et al., 2018). Second, cannabis use was conceptualized by any use, yet a growing body of work indicates that the amount (e.g., hits, grams), cannabinoid composition (e.g., THC to CBD ratios), and mode of administration (e.g., vaping vs. blunts) all influence the experience of a cannabis use event (Andrade et al., 2019; Cloutier et al., 2021; Prince & Conner, 2019; Zuardi et al., 1982). Third, data were collected in a state where cannabis had been legalized for medical, but not recreational, use and the current study did not assess whether participants were using cannabis medicinally, which may impact the strength and generalizability of the study findings (Kerr et al., 2017). Fourth, our sample was predominantly NHL-White (73%) and we did not assess other critical identities (e.g., gender vs. sex, sexual orientation) nor their intersection (e.g., gay Black cismen). More specifically, our binary treatment of sex (male/female) may not accurately reflect heterogeneity and potentially the unique needs in college healthcare and other counseling settings. Our sample also consisted of primarily college-attending young adults (88%). More diverse samples that consider systemic factors and education differences (Carter et al., 2010) are needed to better characterize individuals at greatest risk for specific consequences of SAM use (e.g., access; policing possession of paraphernalia). Relatedly, our findings may not generalize to treatment-seeking individuals or individuals presenting with severe substance use disorder; this remains an important area of future study. Lastly, our findings were based on individuals who reported frequent heavy drinking and recently engaged in SAM use; findings may not necessarily generalize to individuals who do not drink heavily or engage in less frequent heavy drinking.
Our results add to the larger body of literature on SAM use by demonstrating specific consequences of SAM use on next-day NA for female participants with elevated anxiety who engage in SAM use. Thus, beyond the consequences generally experienced by young adults who engage in SAM use on SAM use days, female participants with elevated anxiety experienced worsened next-day NA. The current findings also reinforce that interventions targeting SAM use may have particular benefits for young adult female participants with elevated anxiety. By improving daily affect through reduced SAM use, young adult female participants may also experience improvements in existing anxiety while preventing the emergence of longer-term problems.
Highlights.
Negative affect was higher on no substance use days relative to alcohol-only, cannabis-only, or SAM use days.
SAM use was associated with higher next-day negative affect for female participants with higher anxiety.
Anxiety and sex are critical factors in the link between SAM use and affect.
Role of Funding Sources
This work was supported by the National Institute on Drug Abuse (NIDA) [P50 DA039838, T32 DA017629, F31DA051118], the National Institute on Alcohol Abuse and Alcoholism (NIAAA) [K01 AA026854], and the National Science Foundation (NSF) [DGE1255832]. The NIDA, NIAAA, and NSF did not have any role in study design, collection, analysis, and interpretation of the data; writing the report; and the decision to submit the report for publication. The authors have no conflicts of interest to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
The authors declare that they have no competing financial interests or personal relationships that have influenced the work reported in this paper.
All other days (n = 189 days) were excluded. Specifically, days on which participants used only substances other than alcohol or cannabis (e.g., days with nicotine); days on which participants used alcohol and cannabis, but not simultaneously; and days on which participants used alcohol or cannabis with another substance (e.g., days with alcohol and nicotine) were excluded from analyses.
References
- Andrade AK, Renda B, & Murray JE (2019). Cannabinoids, interoception, and anxiety. Pharmacology Biochemistry and Behavior, 180, 60–73. [DOI] [PubMed] [Google Scholar]
- Armeli S, Tennen H, Todd M, Carney MA, Mohr C, Affleck G, & Hromi A (2003). A daily process examination of the stress-response dampening effects of alcohol consumption. Psychology of Addictive Behaviors, 17(4), 266–276. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. [DOI] [PubMed] [Google Scholar]
- Bekiroglu K, Russell MA, Lagoa CM, Lanza ST, & Piper ME (2017). Evaluating the effect of smoking cessation treatment on a complex dynamical system. Drug and Alcohol Dependence, 180, 215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Book SW, Thomas SE, Dempsey JP, Randall PK, & Randall CL (2009). Social anxiety impacts willingness to participate in addiction treatment. Addictive Behaviors, 34(5), 474–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresin K, Mekawi Y, & Verona E (2018). The effect of laboratory manipulations of negative affect on alcohol craving and use: A meta-analysis. Psychology of Addictive Behaviors, 32(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, & Carroll KM (2010). Effect of anxiety on treatment presentation and outcome: Results from the Marijuana Treatment Project. Psychiatry Research, 178(3), 493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Crosby RD, Wonderlich SA, Ecker AH, & Richter A (2015). Antecedents and consequences of cannabis use among racially diverse cannabis users: An analysis from ecological momentary assessment. Drug and Alcohol Dependence, 147, 20–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AC, Obremski Brandon K, & Goldman MS (2010). The college and noncollege experience: A review of the factors that influence drinking behavior in young adulthood. Journal of Studies on Alcohol and Drugs, 71, 742–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloutier RM, Calhoun BH, & Linden-Carmichael AN (2021). Associations of mode of administration on cannabis consumption and subjective intoxication in daily life. Psychology of Addictive Behaviors. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL (1993). Drinking restraint and risk for alcohol abuse. Experimental and Clinical Psychopharmacology, 1, 44–54. [Google Scholar]
- Conger JJ (1956). II. Reinforcement Theory and the Dynamics of Alcoholism. Quarterly Journal of Studies on Alcohol, 17(2), 296–305. [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, & Mudar P (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69, 990–1005. [DOI] [PubMed] [Google Scholar]
- Cooper ZD, & Haney M (2014). Investigation of sex-dependent effects of cannabis in daily cannabis smokers. Drug and Alcohol Dependence, 136, 85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox WM, & Klinger E (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97, 168–180. [DOI] [PubMed] [Google Scholar]
- Cronce JM, Zimmerman L, Rhew IC, Cadigan JM, Atkins DC, & Lee CM (2020). Does it work and does it last? Effects of social and drinking behavior on same- and next-day mood. Addictive Behaviors, 100, 106111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J, Greenbaum PE, & Goldman MS (2004). Up close and personal: Temporal variability in the drinking of individual college students during their first year. Journal of Consulting and Clinical Psychology, 72, 155–164. [DOI] [PubMed] [Google Scholar]
- Derogatis L (2001). Brief Symptoms Inventory 18: Administration, Scoring, and Procedures Manual. Minneapolis, MN: NCS Pearson. [Google Scholar]
- Devenney LE, Coyle KB, & Verster JC (2019). Cognitive performance and mood after a normal night of drinking: A naturalistic alcohol hangover study in a non-student sample. Addictive Behavior Reports, 10, 100197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman FR, Stiksma MC, & Kashdan TB (2018). Social anxiety and the quality of everyday social interactions: The moderating influence of alcohol consumption. Behavior Therapy, 49(3), 373–387. [DOI] [PubMed] [Google Scholar]
- Hox JJ (2010). Multilevel analysis: Techniques and applications, 2nd ed. New York, NY, US: Routledge/Taylor & Francis Group. [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, & Curran PJ (2001). Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology, 110(3), 449–461. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sokolovsky AW, Gunn RL, & White HR (2020). Consequences of alcohol and marijuana use among college students: Prevalence rates and attributions to substance-specific versus simultaneous use. Psychology of Addictive Behaviors, 34(2), 370–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr DC, Bae H, Phibbs S, & Kern AC (2017). Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon. Addiction, 112(11), 1992–2001. [DOI] [PubMed] [Google Scholar]
- Khan SS, Secades-Villa R, Okuda M, Wang S, Pérez-Fuentes G, Kerridge BT, & Blanco C (2013). Gender differences in cannabis use disorders: Results from the National Epidemiologic Survey of Alcohol and Related Conditions. Drug and Alcohol Dependence, 130(1), 101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ (1997). The self-medication hypothesis of substance use disorders: Reconsideration and recent applications. Harvard Review of Psychiatry, 4, 231–244. [DOI] [PubMed] [Google Scholar]
- Lai HMX, Cleary M, Sitharthan T, & Hunt GE (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13. [DOI] [PubMed] [Google Scholar]
- Lee CM, Patrick ME, Fleming CB, Cadigan JM, Abdallah DA, Fairlie AM, & Larimer ME (2020). A daily study comparing alcohol-related positive and negative consequences for days with only alcohol use versus days with simultaneous alcohol and marijuana use in a community sample of young adults. Alcoholism: Clinical and Experimental Research, 44(3), 689–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Stamates AL, & Lau-Barraco C (2019). Simultaneous use of alcohol and marijuana: Patterns and individual differences. Substance Use and Misuse, 54(13), 2156–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Van Doren N, Masters LD, & Lanza ST (2020). Simultaneous alcohol and marijuana use in daily life: Implications for level of use, subjective intoxication, and positive and negative consequences. Psychology of Addictive Behaviors, 34(3), 447–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukas SE, & Orozco S (2001). Ethanol increases plasma Delta(9)-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers. Drug and Alcohol Dependence, 64(2), 143–149. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, & Gordon JR (1980). Determinates of relapse: Implications for the maintenance of behavior change. In Davidson PO & Davidson MS (Eds.), Behavioral medicine: Changing health lifestyles (pp. 410–452). New York: Brunner/Mazel. [Google Scholar]
- Marlatt GA, & Gordon JR (1985). Relapse prevention. New York: Guilford Press. [Google Scholar]
- Merz EL, & Roesch SC (2011). Modeling trait and state variation using multilevel factor analysis with PANAS daily diary data. Journal of Research in Personality, 45(1), 2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Tam TW, & Weisner C (2007). Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence, 90(1), 72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley KI, Lynskey MT, Moran P, Borschmann R, & Winstock AR (2015). Polysubstance use, mental health and high-risk behaviours: Results from the 2012 Global Drug Survey. Drug and Alcohol Review, 34(4), 427–437. [DOI] [PubMed] [Google Scholar]
- Muraven M, Collins RL, Morsheimer ET, Shiffman S, & Paty JA (2005). The morning after: Limit violations and the self-regulation of alcohol consumption. Psychology of Addictive Behaviors, 19(3), 253–262. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Fairlie AM, Cadigan JM, Abdallah DA, Larimer ME, & Lee CM (2019). Daily motives for alcohol and marijuana use as predictors of simultaneous use among young adults. Journal of Studies on Alcohol and Drugs, 80(4), 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Yeomans-Maldonado G, & Griffin J (2016). Daily reports of positive and negative affect and alcohol and marijuana use among college student and nonstudent young adults. Substance Use and Misuse, 51(1), 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince MA, & Conner BT (2019). Examining links between cannabis potency and mental and physical health outcomes. Behaviour Research and Therapy, 115, 111–120. [DOI] [PubMed] [Google Scholar]
- Ross CS, Brooks DR, Aschengrau A, Siegel MB, Weinberg J, & Shrier LA (2018). Positive and negative affect following marijuana use in naturalistic settings: An ecological momentary assessment study. Addictive Behaviors, 76, 61–67. [DOI] [PubMed] [Google Scholar]
- Russell MA, Linden-Carmichael AN, Lanza ST, Fair EV, Sher KJ, & Piasecki TM (2020). Affect relative to day-level drinking initiation: Analyzing ecological momentary assessment data with multilevel spline modeling. Psychology of Addictive Behaviors, 34(3), 434–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, & Patrick ME (2020). Monitoring the Future national survey results on drug use, 1975–2019: Volume II, college students and adults ages 19–60. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Sherman BJ, McRae-Clark AL, Baker NL, Sonne SC, Killeen TK, Cloud K, & Gray KM (2017). Gender differences among treatment-seeking adults with cannabis use disorder: Clinical profiles of women and men enrolled in the achieving cannabis cessation-evaluating N-acetylcysteine treatment (ACCENT) study. American Journal on Addictions, 26(2), 136–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Emery NN, Simons RM, Wills TA, & Webb MK (2017). Effects of alcohol, rumination, and gender on the time course of negative affect. Cognition and Emotion, 31(7), 1405–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavish DC, Scaglione NM, Hultgren BA, & Turrisi R (2019). An ecological momentary assessment of affect, mental health symptoms, and decisions to drink among first-year college women: A pilot study. Prevention Science, 20(5), 753–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokolovsky AW, Gunn RL, Micalizzi L, White HR, & Jackson KM (2020). Alcohol and marijuana co-use: Consequences, subjective intoxication, and the operationalization of simultaneous use. Drug and Alcohol Dependence, 212, 107986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD (1966). The effects of anxiety on complex learning and academic achievement. In Spielberger CD (Ed.), Anxiety and behavior (pp. 361–398). New York, NY: Academic Press. [Google Scholar]
- Stein MD, Caviness CM, Morse EF, Grimone KR, Audet D, Herman DS, Moitra E, & Anderson BJ (2018). A developmental-based motivational intervention to reduce alcohol and marijuana use among non-treatment-seeking young adults: A randomized controlled trial. Addiction, 113(3), 440–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, & Hromi A (2000). Mood and alcohol consumption: An experience sampling test of the self-medication hypothesis. Journal of Abnormal Psychology, 109(2), 198–204. [PubMed] [Google Scholar]
- Terry-McElrath YM, O’Malley PM, & Johnston LD (2014). Alcohol and marijuana use patterns associated with unsafe driving among U.S. high school seniors: High use frequency, concurrent use, and simultaneous use. Journal of Studies on Alcohol and Drugs, 75(3), 378–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath YM, & Patrick ME (2018). Simultaneous alcohol and marijuana use among young adult drinkers: Age-specific changes in prevalence from 1977 to 2016. Alcoholism: Clinical and Experiment Research, 42(11), 2224–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S, Mota N, Bolton J, & Sareen J (2018). Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and Anxiety, 35(9), 851–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Bold KW, Sullivan TP, Armeli S, & Tennen H (2017). Testing bidirectional associations among emotion regulation strategies and substance use: A daily diary study. Addiction, 112(4), 695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Jiao Y, Ray AE, Huh D, Atkins DC, Larimer ME, Fromme K, Corbin WR, Baer JS, Labrie JW, Mun E-Y (2015). Are there secondary effects on marijuana use from brief alcohol interventions for college students? Journal of Studies on Alcohol and Drugs, 76(3), 367–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Kilmer JR, Fossos-Wong N, Hayes K, Sokolovsky AW, & Jackson KM (2019). Simultaneous alcohol and marijuana use among college students: Patterns, correlates, norms, and consequences. Alcoholism: Clinical and Experimental Research, 43(7), 1545–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wycoff AM, Metrik J, & Trull TJ (2018). Affect and cannabis use in daily life: A review and recommendations for future research. Drug and Alcohol Dependence, 191, 223–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurasek AM, Merrill JE, Metrik J, Miller MB, Fernandez AC, & Borsari B (2017). Marijuana use in the context of alcohol interventions for mandated college students. Journal of Substance Abuse Treatment, 79, 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuardi AW, Shirakawa I, Finkelfarb E, & Karniol IG (1982). Action of cannabidiol on the anxiety and other effects produced by Δ 9-THC in normal subjects. Psychopharmacology, 76(3), 245–250. [DOI] [PubMed] [Google Scholar]


