Abstract
We measured contact patterns using online diaries for 304 employees of 3 U.S. companies working remotely. The median number of daily contacts was 2 (IQR 1–4); majority were conversation (55 %), occurred at home (64 %) and lasted >4 h (38 %). These data are crucial for modeling outbreak control among the workforces.
Keywords: Infectious diseases, Social contact surveys, Social mixing, Social contact patterns
1. Introduction
The workplace is a key setting for social interactions and respiratory infection transmission, where 16 % (range 9–33 %) of influenza transmission is estimated to occur (Edwards et al., 2016). Accordingly, the workplace is an important setting to reduce severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) transmission through policies including remote work. In models of infection transmission, the force of infection depends on the rate of inter-personal social contacts and an estimate of the probability of virus transmission during contact. The potential impact of remote work on SARS-COV-2 transmission can be quantified by assessing changes in social contact patterns (Del Fava et al., 2020; Zhang et al., 2020). Contact patterns are used to parameterize mathematical models and may be used to forecast epidemics and simulate the effects of interventions. Models are highly sensitive to the nature and frequency of contacts that individuals make within different settings.
There is a dearth of social contact data for the United States, especially in workplaces. One published telephone study from one US state reported variation by age, day of the week and holiday period (Destefano et al., 2011). Along with households, adults spend most of their time at work (American Time Use Survey Home Page, 2020) where 20–25 % of their contacts are with individuals from diverse ages and neighborhoods (Edwards et al., 2016). In mid-April 2020, 62 % of employed adults in the US reported working remotely in response to the COVID-19 pandemic (PWC’s US Remote Work Survey, 2020). Our study aimed to characterize social contact patterns among employees in the US during the COVID-19 pandemic.
2. Methods
Researchers in this study partnered with the Rollins School of Public Health, Emory University, to recruit 3 companies in Atlanta Georgia, through convenience sampling. Two of these offer consulting services (N1 = 275, N2 = 3000) with employees across all US states while the third offers administrative services to a university (N3 = 560), where Ni represents number of employees per company. Company officials sent emails inviting all staff working in their US offices to participate. Participants opted into the study by consenting online. Each participant completed an enrolment survey which collected information on socio-demographics, the workplace, and household structure. Participants were expected to complete two consecutive days of online diaries through a personalized emailed survey link. Multiple daily contacts with the same person were recorded once, as well as the total time spent with that person. Contact with the same person on both days was counted as two contacts. A contact was defined as either non-physical (a two-way conversation with three or more words exchanged in the physical presence of another person) or physical (directly touching someone, either skin-to-skin or over the clothes). Remote work was defined as working from a location outside their designated site of work, including home or a public space. Each contact was characterized by age, sex, duration and location. For the second day of contact diary, we asked if each contact was repeated from the first day to assess contact persistence. Data were collected from April to June 2020.
We summarized the median number of contacts per person per day stratified by age group, sex, race and household structure of the participant. Contact matrices were calculated by dividing the age group-specific number of contacts by the number of participants in that age group and stratified by contact type, location and repeat. We used four age groups for the participants (20–29, 30–39, 40–59, 60+ years) and six age groups for the contacts (0–9, 10–19, 20–29, 30–39, 40–59, 60+ years). We assessed mixing within same age groups (assortative mixing) using the Q index (Iozzi et al., 2010) (Supplementary text 1). To make our results representative of age-specific mixing patterns among US office workers during the pandemic, we weighted the contact matrix with age-specific employee data for office workers from the US Bureau of Labor Statistics (U.S. Bureau of Labor Statistics, 2021). Analyses were done in R v3.6.2. Ethical approval was given by Yale University (IRB# 2000026906).
3. Results
The overall response rate for the first day of the contact diary was 9.3 % (357/3,835), of which 304 (85 %) participants completed both days of contact diary. Because we found no substantial differences in characteristics between participants who completed one day only and both days, main results are summarized for the individuals who completed both.
The median age of the participants was 36 years (range 21–78) with around 50 % aged 20–39 years and 10 % older than 60 years (Table 1). The majority self-identified as white (58 %) and women (61 %). Most participants reported at least a bachelor’s degree (94 %), and all worked in office-based roles such as analysts, consultants, and managers. Household structures ranged from living with spouse only (32 %), spouse and children only (25 %), parent (8%), roommate or sibling (13 %) or alone (15 %); the most common state of residence was Georgia (49 %). Almost all participants worked remotely on the day of diary completion (95 %).
Table 1.
Distribution of participant characteristics (n = 304) and the median and interquartile range (IQR) of contacts reported on the first day and over the two study days, April to June 2020.
| Total (%) | Median (IQR) Contacts – First day | Daily Median (IQR) Contacts – over two days | ||
|---|---|---|---|---|
| Company | Accenture | 39 (12.8 %) | 2 (1–3.5) | 2 (1–3) |
| Guidehouse | 178 (58.6 %) | 2 (1–4) | 2 (1–4) | |
| Emory 1599 | 87 (28.6 %) | 2 (1–4) | 2 (1–4) | |
| Sex | Women | 184 (60.5) | 2 (1–4) | 2 (1–4) |
| Men | 116 (38.2) | 2 (1–4) | 2 (1–4) | |
| Prefer not to answer | 4 (1.3) | 0.5 (0–1.5) | 1 (0–1.5) | |
| Age Group (years) | 20–29 | 90 (29.6) | 2 (1–3) | 2 (1–3) |
| 30–39 | 76 (25.0) | 2 (1–3) | 2 (1–3) | |
| 40–49 | 60 (19.7) | 3 (2–5) | 3 (1–5) | |
| 50–59 | 49 (16.1) | 2 (1–3) | 2 (1–3) | |
| 60+ | 29 (9.5) | 2 (1–4) | 2 (1–4) | |
| Race | Black | 26 (8.6) | 2.5 (1–4) | 2 (1–4) |
| White | 174 (57.2) | 2 (1–4) | 2 (1–4) | |
| Asian | 48 (15.8) | 2 (0.8–3) | 1 (1–3) | |
| Mixed | 52 (17.1) | 2 (1–4) | 2 (1–4) | |
| Other | 4 (1.3) | 3 (1.8–4.3) | 3 (1–4) | |
| Hispanic or Latino | Yes | 14 (4.6) | 3 (1.3–5) | 3 (1–4) |
| No | 290 (95.4) | 2 (1–4) | 2 (1–4) | |
| Household structurea | Live alone | 44 (14.5) | 0.5 (0–2) | 0 (0–2) |
| Live with parent | 26 (8.6) | 3 (2–5.8) | 3 (2–5) | |
| Roommate or sibling | 39 (12.8) | 3 (2–5) | 3 (1–4) | |
| Spouse and children | 76 (25.0) | 3 (2–5) | 3 (2–4) | |
| Spouse only | 97 (31.9) | 1 (1–2) | 1 (1–2) | |
| Otherb | 22 (7.2) | 3 (2–4) | 1 (1–4) |
Household structure was considered as living with parent if the participant lived with parent regardless of who else was in the house. This category includes households with parents, participant, spouse; parents, participant, children etc.
Others are living with children only, grandchildren, grandparents, friends, niece, nephew, tenant and au pair.
A median of 2 contacts (IQR: 1–4, range: 0–21) was reported per respondent on both days. Over both days, a median of 2 contacts (IQR: 1–4) was reported. The number of contacts differed by household structure but not by sex, age group, race or ethnicity. Individuals living alone or living with their spouse only reported a median of 0 contacts (IQR: 0–2) which was lower than individuals living with spouse and children, sibling or roommate or with at least a parent (median 3; Table 1).
Of the 608 diary-days, 202 (33 %) were collected in April and 406 (67 %) were collected in May and June. Among the 1,548 social contacts reported across two days of data collection, 54 % were conversation only, 12 % were physical contact only, and 34 % were conversation and physical contact (Fig. 1). Among these, 64 % occurred at home, 14 % on the streets or at stores, 6 % at work, and 5% at another person’s home (Fig. 1 Panel A). We report both long lasting (38 % of contacts lasting >4 h) and short (32 % lasting <15 min) contacts: 97 % of long-lasting contacts occurred at the participant’s home while 78 % of short contacts occurred outside. Sixty two percent of contacts were repeated over both days of data collection and 87 % of repeat contacts occurred in the participant’s home.
Fig. 1.
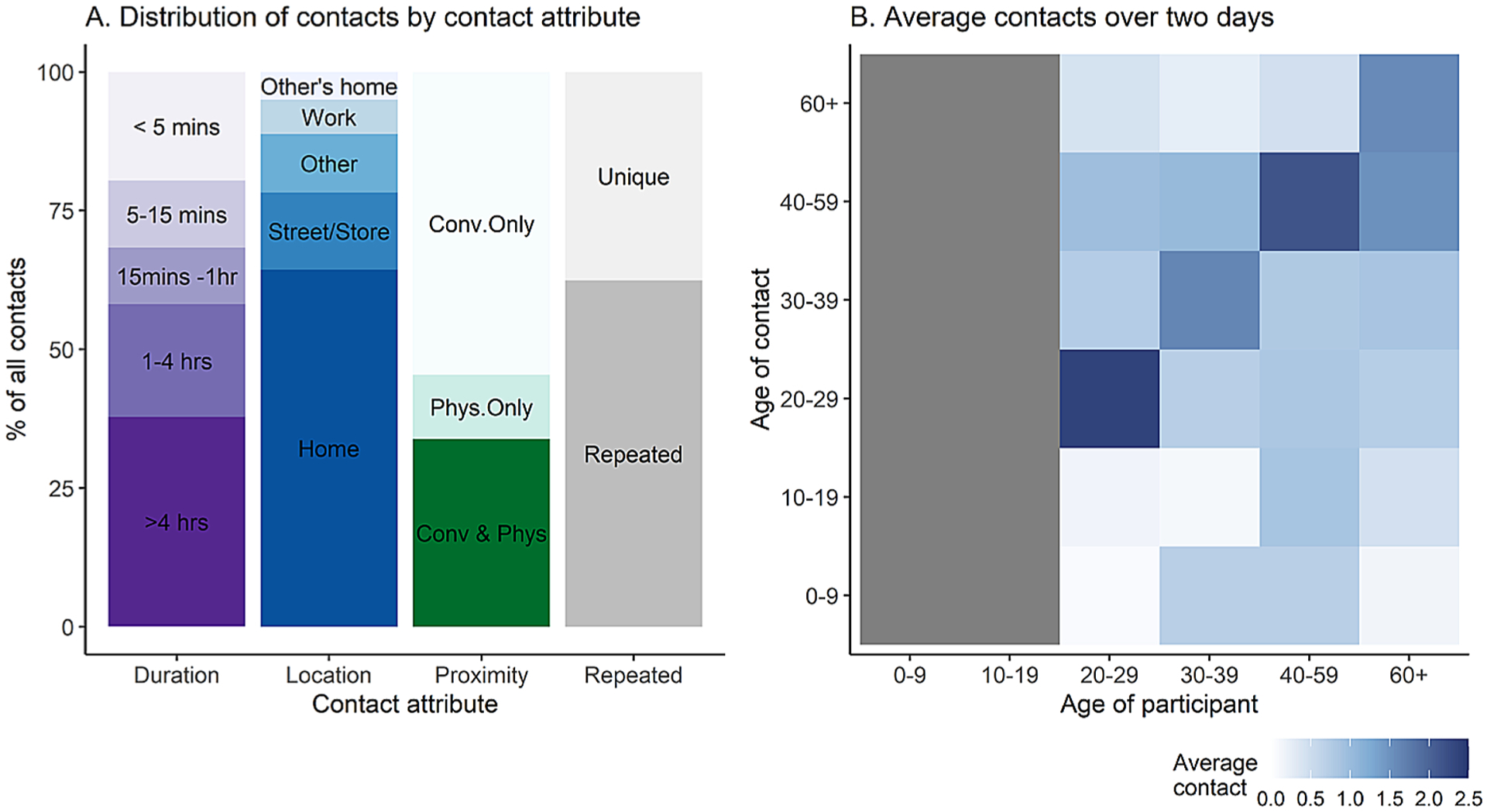
Distribution of contacts. Fig. 1A shows the distribution of contacts by attributes: duration (in minutes (mins) or hours (hr)). Types of contact were conversation with physical touch (Conv & Phys), physical only (Phys), or non-physical/conversation only (Conv only). A contact was repeated if observed on both days or unique if observed on only one day. Fig. 1B shows the age-stratified average number of contacts over two study days (numerical values available in Supplementary Information 1). The gray area on the x-axis indicates that all respondents were over the age of 19, however they were able to report contacts under the age of 19 years. Data shown in the graphs are for 1,548 contacts recorded by 304 participants over 608 diary-days.
The age-stratified contact matrix (Fig. 1 Panel B) details average contacts made by participants and contacts within and across age groups. The peak mean numbers of contacts were on the main diagonal, indicating preferential mixing among individuals of the same age group. However, there was little evidence of assortative mixing by age for contacts above 20 years (Q index = 0.27). The mixing matrix also shows inter-generational mixing involving 30–59-year-old participants and children.
4. Discussion
Participating study employees reported few contacts during this time when shelter-in-place orders were in effect in Georgia and most other states. The majority of the contacts occurred at home and were repeated rather than new, which may reduce the overall size of an outbreak (Smieszek, 2009). As such, employees in this survey were not making many new contacts outside the household during this phase of the pandemic, which could limit community transmission risk but increase risk of infections clustered in the households. The duration of contact is important in models to define heterogeneous transmission probabilities based on age-specific exposure-time to infectious agents during contacts (Smieszek, 2009). The duration of contact can also be used in network models of transmission dynamics. Network models represent persistent contacts, in order to explicitly represent the repeated set of exposures between the same set of persons in the population over time (Jenness et al., 2020). Persistent contacts are important to incorporate in settings or situations where the assumptions of standard compartmental models (a homogenous well-mixed population) may be violated. By disentangling one-time versus repeated exposures in this data, we provide the necessary empirical framework for parameterizing these models.
Employees from 3 companies were recruited online; employees opted-in the study which elicited fewer responses than expected despite regular reminders and monetary incentives. Employees interested in public health or who adhered to social distancing policies may have been more likely to respond to our surveys. Public health messaging calling for social distancing may have also created stigma around reporting high contact rates resulting in the low contact rates reported in this study. This study purposively selected individuals from job categorized as management occupations, business and financial operations occupations, computer and mathematical occupations and life physical and social science occupations (U.S. Bureau of Labor Statistics, 2021). Nevertheless, the distribution of population by age and job category is similar to the overall distribution of employees aged >16 years, thus we represent a diverse cross-section of the working population as shown in Table 1. To account for the non-probability sampling, we performed post hoc weighting and adjusted for reciprocity similar to other studies (Supplementary Information 2). This resulted to a symmetric matrix with lower contact rates along the diagonal.
We lack pre-pandemic data from this specific population for direct comparison, but other studies in the UK (Klepac et al., 2020) and China (Zhang et al., 2020) report reduced contact rates by office workers during the pandemic. Data provided from this study can be combined with other population-based data sources from earlier studies (such as POLYMOD (Mossong et al., 2008) or studies by UC Berkeley (Feehan and Mahmud, 2021) to represent general community. Similarly, many U.S. companies instituted work-from-home policies (PWC’s US Remote Work Survey, 2020), likely reducing total number of contacts in workplaces and non-household settings, while increasing the intensity and duration of household contacts. In subsequent rounds of the study, we will assess changes in contact patterns as physical distancing restrictions are eased and employees return to work in office settings. We will also adjust for sex, age group and region based on company-specific data or nationally representative census data. In future, we will use the contact pattern data to parameterize mathematical models describing risk of disease transmission and investigate prevention and control strategies in the home and workplace.
Supplementary Material
Acknowledgment
We thank the employees of the three companies that participated in this study.
Funding statement
This work was supported by CDC/NCEZID (5U01CK00057) and NIH/NICHD (5R01HD097175). The authors declare no conflict of interest.
Footnotes
Transparency document
The Transparency document associated with this article can be found in the online version.
Declaration of Competing Interest
The authors report no declarations of interest.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.epidem.2021.100481.
References
- American Time Use Survey Home Page. 2020. [cited 1 Jun 2020]. Available: https://www.bls.gov/tus/.
- Del Fava E, Cimentada J, Perrotta D, Grow A, Rampazzo F, Gil-Clavel S, et al. , 2020. The Differential Impact of Physical Distancing Strategies on Social Contacts Relevant for the Spread of COVID-19: Evidence from a Multi-country Survey. 10.1101/2020.05.15.20102657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Destefano F, Haber M, Currivan D, Farris T, Burrus B, Stone-Wiggins B, et al. , 2011. Factors associated with social contacts in four communities during the 2007–2008 influenza season. Epidemiol. Infect 139, 1181–1190. 10.1017/S095026881000230X. [DOI] [PubMed] [Google Scholar]
- Edwards CH, Tomba GS, De Blasio BF, 2016. Influenza in workplaces: transmission, workers’ adherence to sick leave advice and European sick leave recommendations. Eur. J. Public Health 26, 478–485. 10.1093/eurpub/ckw031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feehan DM, Mahmud AS, 2021. Quantifying population contact patterns in the United States during the COVID-19 pandemic. Nat. Commun 12. 10.1038/s41467-021-20990-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iozzi F, Trusiano F, Chinazzi M, Billari FC, Zagheni E, Merler S, et al. , 2010. Little Italy: an agent-based approach to the estimation of contact patterns-fitting predicted matrices to serological data. PLoS Comput. Biol 6. 10.1371/journal.pcbi.1001021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenness SM, Willebrand KS, Malik AA, Lopman BA, Omer SB, 2020. Dynamic network strategies for SARS-CoV-2 control on a cruise ship. medRxiv, 2020.08.26.20182766.Available: http://medrxiv.org/content/early/2020/10/06/2020.08.26.20182766.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klepac P, Kucharski A, Conlan AJ, Kissler S, Tang M, Fry H, et al. , 2020. Contacts in Context: Large-Scale Setting-specific Social Mixing Matrices from the BBC Pandemic Project, pp. 1–17. 10.1101/2020.02.16.20023754. [DOI] [Google Scholar]
- Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. , 2008. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 5, 0381–0391. 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PWC’s US Remote Work Survey. 2020. [cited 1 Jun 2020]. Available: https://www.pwc.com/us/en/library/covid-19/us-remote-work-survey.html.
- Smieszek T, 2009. A mechanistic model of infection: why duration and intensity of contacts should be included in models of disease spread. Theor. Biol. Med. Model 6, 25. 10.1186/1742-4682-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. 2021. [cited 1 Apr 2021]. Available: https://www.bls.gov.
- Zhang J, Litvinova M, Liang Y, Wang Y, Wang W, Zhao S, et al. , 2020. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science (80-) 368, 1481–1486. 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


