Abstract
Objective
Children of parents with mental illness (COPMI) are vulnerable during the COVID-19 pandemic. The study aimed to assess the psychosocial impacts of the pandemic and identify potential factors influencing their mental health.
Method
665 COPMI from six sites including Wuhan in China were enrolled. COPMI's mental health and the impacts of COVID-19 were assessed by an online survey. Univariate and multivariate analyses were performed to examine the association between impact factors and participants’ mental health.
Results
16.1 % of participants were in abnormal range of mental health, with interpersonal relationship being the most common problem. 48.6 % of participants reported quite worried about the epidemic. All aspects of adverse effects of COVID-19 were more prevalent among COPMI in Wuhan than in other sites. Concerns about COVID-19 (OR = 1.7, p = 0.02), decreased family income (OR = 2.0, p = 0.02), being physically abused (OR = 2.1, p = 0.04), witnessing family members being physically abused (OR = 2.0, p = 0.03), and needs for promoting family members' mental health (OR = 2.2, p < 0.01) were independent risk factors for participants' mental health.
Conclusion
The findings raise our awareness of the impacts of COVID-19 pandemic on the wellbeing of COPMI. Multifaceted psychosocial support for COPMI is urgently needed to support them live through the pandemic.
Keywords: Coronavirus disease, Parental mental illness, Children, Psychosocial impacts, Mental health
1. Introduction
The World Health Organization (WHO) declared the outbreak of Coronavirus disease 2019 (COVID-19) as a pandemic in March 2020 (WHO, 2020a). By the end of May 2021, COVID-19 had spread to almost all countries worldwide, affected 110766 individuals in China and nearly 170 million individuals globally. Over 3.5 million deaths have been resulted from COVID-19 (WHO, 2021). Uncertain prognoses of the disease (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020), shortages of protective equipment (Dong and Bouey, 2020), large-scale social distancing measures (Brooks et al., 2020), and growing financial losses are among major stressors which contribute to widespread psychological distress and mental health burden, especially in worst-hit locations (e.g. Wuhan in China, New York City in U.S) (Bao et al., 2020; Pfefferbaum and North, 2020). According to a latest meta-analysis, the overall prevalence of depression was 31.4 %, of anxiety was 31.9 %, and of insomnia was 37.9 % (Wu et al., 2021). The WHO emphasized the significance of mental health wellbeing during the pandemic and promoted the integration of mental health and psychological support into the COVID-19 response efforts (WHO, 2020a). The National Health Commission of China has released several guideline documents and taken measures to mitigate the negative mental health effects of the pandemic (National Health Commission of China, 2020a).
Noteworthily, existing evidence suggests the pandemic could have disproportionate effects on vulnerable populations (Holmes et al., 2020). Though lock down measurements have been challenging for people of all ages, children and adolescents would be more difficult since they highly rely on social connections for their emotional supports and development (Ellis and Zarbatany, 2017). More mental health issues were induced in children and adolescents owing to their unsatisfied educational and developmental needs (Loades et al., 2020). High rates of severe depression, anxiety, fear and dysfunction have been reported across nations (Buzzi et al., 2020; Guessoum et al., 2020; Saurabh and Ranjan, 2020; Zhou et al., 2020).
Meanwhile, patients with existing mental health problems might be particularly suffering due to their susceptibility to stress, disruptions to mental health services, and loss of positive interpersonal activities (Yao et al., 2020). Especially, a previous psychiatric diagnosis has been reported as an independent risk factor for COVID-19 (Taquet et al., 2021). Therefore, children of parents with mental illness (COPMI) might take a double risk and would be of the most vulnerable population in the pandemic. Despite their relatively higher risk of developing mental disorders, living with a parent with mental illness may cause a variety of detrimental social consequences (Bassani et al., 2009; Brockington et al., 2011; Ranning et al., 2016). During the pandemic, COPMI may expose to higher levels of stress and anxiety imposed by their parents (Yao et al., 2020). Heartbreaking news about COPMI in the pandemic have been reported (Tencent News, 2020), which emphasized the significance for providing timely care for this population worldwide.
Understanding psychosocial impacts of COVID-19 on vulnerable groups are the urgent research priority (Holmes et al., 2020). So far little is known about the mental health wellbeing of COPMI in the pandemic. Therefore, we carried out this study to assess the psychosocial impacts of COVID-19 on COPMI and try to identify potential factors influencing their mental health wellbeing. We also hypothesized that the pandemic could affect COPMI living in different locations to different degrees, and COPMI living in worst-hit locations could have more psychological needs and difficulties than other locations.
2. Methods
2.1. Study design and participants
This was a cross-sectional community-based study. Participants were aged 9–18 years old and had been living with their parents of severe mental illness for more than half a year. One of the participant’s parents had a diagnosis of schizophrenia, bipolar disorder, mental retardation with psychotic symptoms, or schizophrenia-like psychosis in epilepsy according to ICD-10 criteria, and had been receiving regular community mental health service provided by the National Continuing Management and Intervention Program (‘686’ Program) (Liu et al., 2011). If any individual was under serious mental or physical conditions which impeded him/her to understand and participate in the study, he/she would be excluded. Ethics approval was obtained from the Institutional Review Board of Peking University Institute of Mental Health.
2.2. Procedures
Data collection took place between March and April 2020, which was considered as the middle period of the pandemic in China. To recruit a representative sample, we selected six geographically and economically diverse sites which were also pilot sites for our COMPI studies based on the ‘686’ Program: Fangshan District from Beijing City (northern area, medium economic development), Zaozhuang City from Shandong Province (northern area, relatively low economic development), Taiyuan City from Shanxi Province (middle area, medium economic development), Mianyang and Zigong City from Sichuan Province (southwestern area, relatively low economic development), Xiamen City from Fujian Province (southeastern area, relatively high economic development), and Wuhan City from Hubei Province, the epicenter of COVID-19 in China (middle area, relatively high economic development) [Fig. 1 ]. At least two communities from each site were involved to represent both urban and rural situations.
Fig. 1.
Distribution of the overall sample (N = 665).
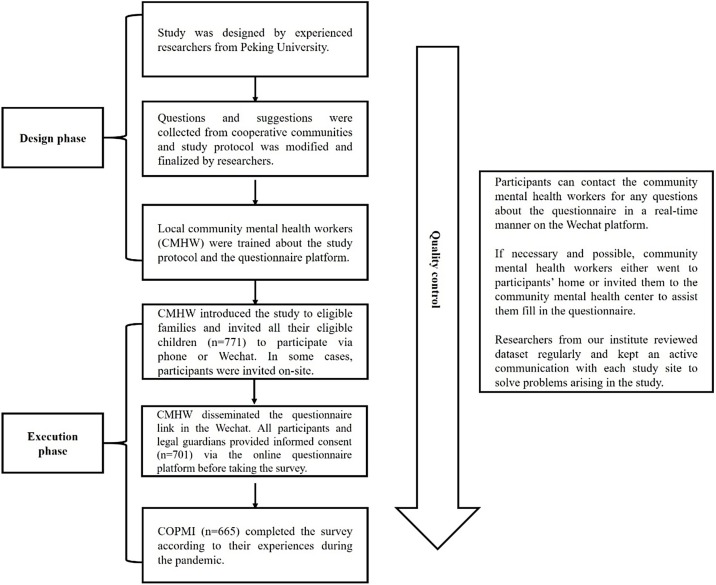
Experienced researchers from our institution, who have extensive experience in working with COPMI, designed the study. The researchers collected questions and suggestions from each study sites, then modified and finalized the research protocol and the questionnaire. 2–4 community mental health workers from each site served as key facilitators and were responsible for working with the study participants after being trained on how to implement the study and use the online questionnaire platform. Those community mental health workers were either psychiatrists in county level hospital, or general practitioners with license for mental health care after receiving basic training in psychiatry. Before joined the study, they had been providing regular follow-ups for the patients based on existing community mental health project.
The sampling was based on a pre-investigation. Patients who had been receiving community mental health service were screened for their fertility situation. Community mental health workers introduced the study to eligible families and invited their children to participant via communications on the phone or through social networking app called Wechat. In some cases the study participants were invited on-site during the mental health care visits. Community mental health workers disseminated the questionnaire link in the Wechat and invited all eligible COPMI to respond to the questions according to their own experiences during the pandemic. All participants and their legal guardians provided informed consent via the online questionnaire platform before taking the survey.
To ensure the study quality, participants can contact the community mental health workers for any questions about the questionnaire in a real-time manner on the Wechat platform. If necessary and possible, community mental health workers either went to participants’ home or invited them to the community mental health center to assist them fill in the questionnaire. Researchers from our institute reviewed dataset regularly and kept an active communication with each study site to solve problems arising in the study [Fig. 2 ].
Fig. 2.
Research flow chart of the study.
2.3. Measurements
We adopted an anonymous online questionnaire (‘Wenjuanxing’ Platform) via social media (Wechat) to facilitate the investigation. The questionnaire consisted of structured questions mainly covering several areas. All measurements, except Strength and Difficulty Questionnaire (SDQ), were made by mental health experts for the purpose of this study.
2.3.1. Mental health status
SDQ was implemented to assess the mental health status of participants. SDQ focuses on difficulties as well as strengths. It measures prosocial activities directly, which might be disturbed seriously during the pandemic. SDQ is a validated 25-item questionnaire which can screen for common emotional and behavioural problems in childhood and adolescence (Du et al., 2008). SDQ is divided into five subscales: emotional symptoms, conduct problems, hyperactivity/inattention, interpersonal relationship problems, and prosocial activities. Each subscale is scored 0−10. The cut-offs for each subscale were 5, 3, 5, 3, 6, respectively. The total difficulty score is the sum of the first four subscales. SDQ obtained in this study were participant self-answered.
2.3.2. Impacts of COVID-19
-
1)
Contact history with COVID-19, including admission to hospital, being quarantined by health authorities, and direct/indirect contact with a confirmed or suspected COVID-19 case.
-
2)
Concerns about COVID-19, which were collected on three self-evaluated questions, "I feel that the pandemic is very close to me." "My family and I are at great risk of being infected." and "People are likely to die if they were infected." Each question was rated on a 5-point scale, with ‘1’ representing ‘strongly disagree’ and ‘5’ representing ‘strongly agree’. Participants who answered ‘4’ or ‘5’ to any question were rated as ‘quite worried’ about the COVID-19, who answered ‘3’ to all questions were rated as ‘moderately worried’, others were rated as ‘not worried’.
-
3)
Adverse effects of COVID-19 in terms of daily life, physical and mental health, family members’ physical and mental health, family relationships, and peer relationships, were assessed on self-rated questions. The participants were asked to answer whether the COVID-19 outbreak had adverse effect on each domain.
-
4)
Experience of domestic violence during the pandemic, i.e., emotional abuse (being insulted, bellowed, ridiculed, cursed or threaten to harm) and physical abuse (being pushed, grabbed, throwed at, beaten or injured) towards young participants and their family members were rated on a 4-point scale, with ‘0’ representing ‘none’, ‘1’ representing ‘only once’, ‘2’ representing ‘several times’, and ‘3’ representing ‘many times’.
-
5)
Difficulties during the pandemic were classified as shortage of living materials, study materials (laptops, internet, etc.), self-protective measurements (masks, medical alcohol, etc.), and difficulties in accessing medical service. The participants were asked to specify the exact problem they encountered.
-
6)
Service needs during the pandemic, including study guidance, living material support, knowledge about COVID-19 protection, accessing health care, and promoting mental health of their parents and themselves, were also collected on self-rated questions.
2.4. Statistical analysis
Data were analyzed using STATA (Statacorp, College Station, TX, US). Differences in measurement data were compared with Student t-test or non-parametric test for continuous variables, and chi-square test for categorical variables. Univariate and multivariate analyses were performed to examine the association between impact factors and participants’ mental health status (classified as ‘well’ with a score of ≤15 in SDQ total difficulties). Odds ratio (OR) and 95 % confidence intervals were used to measure degree of the association. Unadjusted ORs and p-values were reported in univariate analyses. The variable with a p < 0.10 in the univariate analysis was included in the multiple logistic regression. All tests were two-tailed, with a significance level of p<0.05.
2.5. Role of the funding source
This study was supported by the Key Program of Beijing Science and Technology Commission (Z191100006619113, D171100007017002, D121100005012004), and the Capital’s Funds for Health Improvement Research (No.2018-4-4116). The funders had no role in the study design, data collection, data analysis, and data interpretation. The corresponding author had full access to all data in the study and had the final responsibility for decision to submit for publication.
3. Results
3.1. Sociodemographic characteristics
Of the 771 invited individuals, 701 COPMI and their legal guardian gave their informed consents and 665 respondents (86.3 %) completed the survey. Almost half of participants were female, with a mean age of 13.1 years. Parental psychiatric disorder was mainly schizophrenia (78.4 %). 170 (25.6 %) families relied merely on government welfare, and 11 (1.7 %) families did not have any source of income before the epidemic.
Wuhan was the epicenter of China with 50,000 confirmed COVID-19 cases. Other study sites had 16˜35 confirmed cases in total [Table 1 , * The epidemic indicators were references by the end of May 2020 (COVID-19 Map of China, 2020). Therefore, we combined other study sites as a whole and defined as ‘non-epicenter’. In further analysis, we compared the two groups to reflect impacts associated with the severity of the epidemic.
Table 1.
Distribution of participants and Epidemic indicators in study sites.
| Location | Epidemic indicators * |
Study participants |
||
|---|---|---|---|---|
| No. of COVID-19 cases | No. of Deaths due to COVID-19 |
No. of Participants | Response rate (%) | |
| Fangshan district (Beijing) | 16 | 0 | 27 | 93.1 |
| Zaozhuang city (Shandong Province) | 24 | 0 | 58 | 93.5 |
| Taiyuan city (Shandong Province) | 21 | 0 | 31 | 88.6 |
| Xianmen city (Fujian Province) | 35 | 0 | 54 | 90.0 |
| Mianyang, Zigong city (Sichuan Province) | 31 | 0 | 126 | 96.9 |
| Wuhan city (Hubei Province) | 50340 | 3869 | 369 | 81.1 |
| Total | 50467 | 3869 | 665 | 86.3 |
The figures were references by the end of May 202018.
In comparison with other locations, participants from Wuhan were slightly younger, of more parents with schizophrenia, and fewer from families with more than two sources of household income before the epidemic [Table 2 ].
Table 2.
Sociodemographic characteristics of participants.
| Characteristics | Total (N = 665) |
Location |
||
|---|---|---|---|---|
| Epicenter (n = 369) |
Non-Epicenter (n = 296) |
p | ||
| Age [mean ± SD] | 13.1 ± 2.6 | 13.0 ± 2.6 | 13.4 ± 2.6 | 0.05 |
| Female [n(%)] | 322(48.4) | 175(47.4) | 147(49.7) | 0.57 |
| Rural residence [n(%)] | 502(75.5) | 269(72.9) | 233(78.7) | 0.08 |
| Parental psychiatric disorders [n(%)] | ||||
| Schizophrenia | 521(78.4) | 302(81.8) | 219(74.0) | 0.05 |
| Mental retardation with psychotic symptoms |
55(8.3) | 30(8.1) | 25(8.4) | |
| Bipolar disorder | 48(7.2) | 21(5.7) | 27(9.1) | |
| Mental retardation with Schizophrenia-like psychosis in Epilepsy | 41(6.1) | 16(4.3) | 25(8.4) | |
| Household income before the epidemic [n (%)] | ||||
| No income | 11(1.7) | 4(1.1) | 7(2.3) | <0.01 |
| Only Basic Living Allowance | 170(25.6) | 112(30.4) | 58(19.6) | |
| ≥ 2 sources of income | 484(72.8) | 253(68.6) | 231(78.0) | |
| Family members living with COPMI during the epidemic [n (%)] | ||||
| Parents | 477(71.7) | 287(77.8) | 190(64.2) | <0.01 |
| Single parents | 99(14.9) | 51(13.8) | 48(16.2) | |
| Other relatives | 78(11.7) | 24(6.5) | 54(18.2) | |
| Live alone | 11(1.7) | 7(1.9) | 4(1.4) | |
3.2. Mental health wellbeing
Participants showed varying degrees of mental health problems according to SDQ scores. 16.1 % (n = 107) of participants scored higher out of the normal range in total difficulties, with 32.3 % (n = 215) in the subscale of interpersonal relationships, 17.3 % (n = 115) in the subscale of conduct problems, 8.0 % (n = 53) in the subscale of hyperactivity, 5.0 % (n = 33) in the subscale of emotional symptoms. 30.0 % (n = 199) of participants scored lower than the normal range of strengths in the subscale of prosocial activities. Participants from Wuhan scored lower in the strength subscale (p = 0.02). More participants from Wuhan were abnormal in terms of interpersonal relationships (p = 0.04) [Table 3 ].
Table 3.
Mental health status evaluated by SDQ subscales.
| SDQ subscales | Total (N = 665) |
Location |
||
|---|---|---|---|---|
| Epicenter (n = 369) |
Non-Epicenter (n = 296) |
p | ||
| Difficulties | ||||
| 1)Emotional symptoms | ||||
| Median (25 %,75 %) | 2(0,3) | 2(0,3) | 2(0,3) | 0.48 |
| Abnormal [n (%)] | 33(5.0) | 16(4.3) | 17(5.7) | 0.41 |
| 2)Conduct problems | ||||
| Median (25 %,75 %) | 2(1,3) | 2(1,3) | 1.5(1,3) | 0.55 |
| Abnormal [n (%)] | 115(17.3) | 68(18.4) | 47(15.9) | 0.39 |
| 3)Hyperactivity | ||||
| Median (25 %,75 %) | 3(1,4) | 3(2,4) | 3(1,4) | 0.05 |
| Abnormal [n (%)] | 53(8.0) | 31(8.7) | 22(7.1) | 0.46 |
| 4)Interpersonal relationships | ||||
| Median (25 %,75 %) | 3(2,4) | 3(2,4) | 2(2,4) | 0.09 |
| Abnormal [n (%)] | 215(32.3) | 237(35.8) | 83(28.0) | 0.04 |
| Total difficulties | ||||
| Median (25 %,75 %) | 9(5,13) | 9(6,13) | 9(5,12) | 0.17 |
| Abnormal [n (%)] | 107(16.1) | 68(18.4) | 39(13.2) | 0.07 |
| Strengths | ||||
| Prosocial behaviours | ||||
| Median (25 %,75 %) | 7(5,9) | 7(5,9) | 8(5,9) | 0.02 |
| Abnormal [n (%)] | 199(30.0) | 114(30.7) | 86(29.0) | 0.66 |
3.3. Impact of the COVID-19
3.3.1. Contact history with COVID-19
Five participants from Wuhan reported confirmed COVID-19 cases in their families (two fathers, two grandparents, and one aunt). Among them, four reported family members being quarantined by health authorities. No participants from other sites reported any contact history with COVID-19.
3.3.2. Concerns about COVID-19
48.6 % (n = 323) participants reported quite worried, 16.5 % (n = 110) reported moderately worried, and 34.9 % (n = 232) reported slightly or not worried about the epidemic. More participants from the epicenter reported quite worried about COVID-19 than other study sites (53.1 % vs 42.9 %, p < 0.01).
3.3.3. Adverse effects of COVID-19
Daily life was the top rating (72.6 %) of being negatively affected by COVID-19. About half of participants reported their and their family members’ physical health (54.0 % and 49.3 %, respectively) and mental health (52.8 % and 52.2 %, respectively) were negatively affected. 38.0 % (n = 253) reported their peer relationships and 28.0 % (n = 186) reported their family relationships were negatively affected. More participants living in Wuhan reported being adversely affected by the epidemic in each aspect (all p < 0.01).
3.3.4. Experience of domestic violence
118 participants (17.7 %) reported experiencing any form of domestic violence during the epidemic. Among them, 16.2 % (n = 108) reported being emotionally abused and 8.7 % (n = 58) reported being physically abused. Meanwhile, 15.8 % of participants (n = 105) reported witnessing family members being emotionally abused, and 12.5 % (n = 83) reported witnessing family members being physically abused. No significant differences were found between the epicenter and other locations in the frequency of experiencing domestic violence (p = 0.41) or witnessing family members being abused (p = 0.35).12.5 % (n=50) of COPMI reported that their parents’ mental health statuses were getting worse during the epidemic. Participants who reported parents' mental health getting worse were more likely to expose to all forms of domestic violence (all p < 0.01).
3.3.5. Difficulties during the epidemic
55.4 % of participants (n = 366) reported lack of self-protective measurements, 46.2 % (n = 307) reported lack of study materials when being confined at home, 44.2 % (n = 294) reported shortage of living materials, and 26.9 % (n = 179) reported difficulties in accessing medical service during the epidemic. 22.9 % (n = 152) of participants reported decreased household income and relied mainly on government welfare during the epidemic. Difficulties in all aspects were more prevalent in Wuhan than non-epicenters (all p < 0.01).
3.3.6. Service needs during the epidemic
60.0 % of participants (n = 399) expressed their needs for study guidance, 50.4 % (n = 335) for living materials, and 38.2 % (n = 254) for knowledge about the COVID-19 protection. 28.6 % (n = 190) reported they needed help for promoting their family members' mental health, 28.4 % (n = 189) for accessing medical service, and 21.8 % (n = 145) for promoting the mental health of their own. Higher percentage of COPMI from Wuhan expressed needs for living material support and accessing medical service (both p < 0.01) [Table 4 ].
Table 4.
Impacts of COVID-19 on participants@.
| Impacts | Total (N = 665) |
Location |
||
|---|---|---|---|---|
| Epicenter (n = 369) |
Non-epicenter (n = 296) |
p | ||
| Contract history with the COVID-19 [n (%)] | ||||
| Confirmed cases in family | 5(0.8) | 5(1.4) | 0 | |
| Family members being quarantined | 4(0.6) | 4(1.1) | 0 | |
| Concerns about the COVID-19 [n (%)] | ||||
| Quite worried | 323(48.6) | 196(53.1) | 127(42.9) | 0.01 |
| Moderately worried | 110(16.5) | 66(17.9) | 44(14.9) | |
| Slightly or not worried | 232(34.9) | 107(29.0) | 125(42.2) | |
| Adverse effects of COVID-19 [n (%)] | ||||
| Daily life | 483(72.6) | 303(82.1) | 180(60.8) | <0.01 |
| Self-physical health | 359(54.0) | 245(66.4) | 114(38.5) | <0.01 |
| Self-mental health | 351(52.8) | 235(63.7) | 116(39.2) | <0.01 |
| Family members’ mental health | 347(52.2) | 233(63.1) | 114(38.5) | <0.01 |
| Family members’ physical health | 328(49.3) | 219(59.3) | 109(36.8) | <0.01 |
| Peer relationship | 253(38.0) | 173(46.9) | 80(27.0) | <0.01 |
| Family relationship | 186(28.0) | 133(36.0) | 53(17.9) | <0.01 |
| Experience of domestic violence [n (%)] | ||||
| Being emotionally abused | 108(16.2) | 56(15.2) | 52(17.6) | 0.32 |
| Being physically abused | 58(8.72) | 29(7.9) | 29(9.8) | 0.23 |
| Witnessing family members being emotionally abused | 105(15.8) | 58(15.7) | 47(15.9) | 0.62 |
| Witnessing family members being physically abused | 83(12.5) | 50(13.6) | 33(11.1) | 0.46 |
| Difficulties during the epidemic [n (%)] | ||||
| Lack of self-protective measurements | 366(55.4) | 219(59.3) | 147(49.7) | 0.01 |
| Lack of study materials | 307(46.2) | 193(52.3) | 114(38.5) | <0.01 |
| Shortage of living materials | 294(44.2) | 218(59.1) | 74(25.0) | <0.01 |
| Difficulties in accessing medical service | 179(26.9) | 127(34.4) | 52(17.6) | <0.01 |
| Decreased in household income | 152(22.9) | 125(33.9) | 27(9.1) | <0.01 |
| Service needs during the epidemic [n (%)] | ||||
| Study guidance | 399(60.0) | 233(63.1) | 166(56.1) | 0.85 |
| Living material support | 335(50.4) | 246(66.7) | 89(30.1) | <0.01 |
| Knowledge about COVID-19 | 254(38.0) | 145(39.3) | 109(36.8) | 0.25 |
| Promoting family members’ mental health | 190(28.6) | 114(30.1) | 76(25.7) | 0.45 |
| Accessing medical service | 189(28.4) | 131(35.5) | 58(19.6) | <0.01 |
| Promoting self-mental health | 145(21.8) | 81(22.0) | 64(21.6) | 0.22 |
After controlling for household income before the epidemic and family members living with COPMI during the epidemic, which were different between the epicenter and non-epicenters.
3.3.7. Multivariate analysis of impact factors for COPMI's mental health
In univariate analysis, we found quite worried about the COVID-19 (OR = 2.0, p < 0.01), decreased family income (OR=1.8, p = 0.03), being physically abused (OR = 3.4, p < 0.01), witnessing family members being physically abused (OR=3.0, p < 0.01), lack of living materials (OR=3.4, p < 0.01), and needs for promoting family members' mental health (OR=2.7, p < 0.01) were potential risk factors for participants' mental health (‘not well’ classified as with a score of >15 in SDQ total difficulties). The factor of living in or outside the epicenter showed marginal significance (OR=1.5, p = 0.07), which was also included in the multiple logistic regression model.
After controlling for age and gender, quite worried about COVID-19 (OR = 1.7, 95 % CI: 1.1, 2.8, p = 0.02), decreased family income (OR=2.0, 95 % CI(1.1, 3.7), p = 0.02), being physically abused (OR=2.1, 95 % CI(1.0, 4.3), p = 0.04), witnessing family members being physically abused (OR=2.0, 95 % CI(1.1, 3.8), p = 0.03), and needs for promoting family members' mental health (OR = 2.1, 95 % CI(1.4, 3.4), p < 0.01) were independent risk factors for participants' mental health wellbeing [Table 5 ].
Table 5.
Multivariate logistic regression models of independent impact factors for participants’ mental health status.
| Factors | OR | p | 95 % Confidence Interval |
|---|---|---|---|
| Age | 1.0 | 0.95 | (0.9, 1.1) |
| Sex | 1.0 | 0.92 | (0.7, 1.6) |
| Location (Living in the Epicenter) | 1.4 | 0.15 | (0.8, 2.3) |
| Concerns about COVID-19 | 1.7 | 0.02 | (1.1, 2.8) |
| Decreased family income | 2.0 | 0.02 | (1.1, 3.7) |
| Physical abuse towards family members | 2.0 | 0.03 | (1.1, 3.8) |
| Being physically abused | 2.1 | 0.04 | (1.0, 4.3) |
| Needs for promoting family members' mental health | 2.1 | <0.01 | (1.4, 3.4) |
4. Discussion
To the best of our knowledge, this was the first study focusing on mental health of COPMI during the COVID-19 pandemic. Over half of young participants reported being negatively affected by the pandemic in all aspects, and nearly half of them reported quite worried about the pandemic. Our results revealed that COPMI had varying degrees of emotional and behavioral problems, with over 30 % of participants having interpersonal difficulties. After controlling for confounders, concerns about COVID-19, decreased family income, domestic violence, and needs for promoting family members' mental health were independent risk factors for COPMI's mental health wellbeing.
Frequencies of mental health problems in adults were reported to be 16.5 %˜49.8 % during the COVID-19 pandemic (Li et al., 2020; Shi et al., 2020; Wang et al., 2020a). We found the frequencies of mental health problems of COPMI fell in this range during the pandemic. Unfortunately, no longitudinal research assessing the psychosocial impact of the COVID-19 pandemic on children and adolescents have been published to date (Magson et al., 2021). We cannot make direct comparisons to pre-pandemic conditions among this group of participants either. We did observe that COPMI living in the worst-hit area were more likely to be affected in terms of interpersonal relationship and strength subscale based on the comparison of SDQ scores between participants in Wuhan and other study sites. There is additional evidence in the literature that the mental health of family members of patients with mental illness was worsened by the COVID-19 pandemic (Willner et al., 2020).
While previous studies mainly focus on emotional problems, our results suggested that interpersonal problems could be most common for COPMI during the pandemic, which was consistent with previous studies (Zhou et al., 2020). Strict domestic quarantine policies and national school closures were implemented worldwide as emergency measures to prevent the infection (Liu et al., 2020). Children and adolescents confined at home needed to struggle with substantial changes to their daily life and social infrastructure (Wang et al., 2020b). Our data provided evidence that their living condition and interpersonal relationships were significantly affected by the pandemic, reminding that COPMI should be given particular attention for timely psychosocial service to support them maintain meaningful relationships in their communities. Community mental health workers con use existing resources, such as hotlines, to contact COPMI regularly. They can also organize online activities by remote systems to help COPMI obtain interpersonal supports.
Wuhan was the worst-hit location in China. Chinese government declared the lockdown of Wuhan on 23 January 2020 to stop the spread of COVID-19, which affected over 11 million residents (Wikipedia, 2020). 53.1 % of participants from Wuhan reported quite worried about the COVID-19, which was higher than general children from Wuhan (37.3 %) according to a recent study (Xie et al., 2020). In addition, adverse effects of the COVID-19 seemed to be more prevalent among COPMI from Wuhan, which was consistent with previous study (Lai et al., 2020). However, we observed a relatively low frequency of emotional symptoms among COPMI either in or outside Wuhan, which might be due to the fact that this study was carried out in the middle phase of the epidemic in China and multifaceted health interventions might be beneficial for this vulnerable population throughout the country (National Health Commission of China, 2020b).
COPMI are more vulnerable to financial loss due to their already lower socioeconomic positions (Luciano et al., 2014). One in five participants reported decreased family income during the pandemic, which was an independent risk factor for their mental health wellbeing. Meanwhile, almost half of participants were in shortage of living goods and protective measurements, which further aggravated their difficulties in this emergency period. Though home schooling plan (online courses delivered through TV broadcasts and internet) has been implemented all over China, a proportion of COMPI cannot benefit due to their lack of access to digital technologies. We suggest that government agencies should implement enhanced financial assistance to help such families get through the pandemic and support COPMI continue education and development. Significantly, mental health problems may persist for a long time after the pandemic (Mak et al., 2009). COPMI would experience higher levels of depression and anxiety and more difficulties in their adulthood (Mitchell et al., 2018). Therefore, close attention and great efforts are needed to address their specific issues effectively and avoid long-term consequences.
Social distancing measures and rising unemployment levels may lead to increased child abuse and neglect (Teo and Griffiths, 2020; WHO, 2020b). More than one sixth of our participants had ever experienced or witnessed domestic violence during the pandemic. Meanwhile, participants whose parents' mental health condition got worse were more likely to expose to any form of domestic violence. Above factors were associated with more mental health problems in COPMI according to our multivariate analysis, which highlights the importance of taking active actions correspondingly. Healthcare professionals and communities should make effective efforts to ensure the sustainability of mental health care for the parents and to strengthen child protection for this already vulnerable population.
The study has limitations. First, we collect data based on our community mental health network rather than recruiting an additional group without parental mental illness for control purpose. Therefore, we cannot conclude that COPMI were at greater risk during the pandemic than other children. We will make up for it in our follow-up studies. Second, our survey was community-based. Inpatients in psychiatric hospitals, who might be more susceptible to infections due to lack of airflow in confined spaces, were not enrolled in this study. This could bias our results towards a better direction, especially for Wuhan. Third, this was a cross-sectional study designed after the outbreak of COVID-19, we're not able to answer whether the mental health of participants was worsened by the pandemic with a direct comparison to pre-pandemic conditions. Fourth, although the study was based on a pre-investigation to optimize the sampling procedure, the participants were recruited in a convenient manner inevitably. Therefore, the study might subject to selection bias and the findings need to be explained with caution. Finally, due to the limitation of the research conditions owning to the pandemic, our study was carried out using an anonymous online questionnaire and possible information bias might exist.
In conclusion, our findings are enlightening as this is the first study worldwide focused on COPMI in the time of COVID-19. The findings may advance our understanding of the psychosocial impacts of the pandemic on this vulnerable population by directly describing COPMI’s mental health status, difficulties and needs. While keeping limitations in mind, we indicate several risk factors associated with mental health in such children and adolescents. Given that psychosocial support for COPMI is urgently needed but still insufficient until now, multifaceted interventions, which need the cooperation of government and non-government agencies, health authorities, and child welfare workforce, should be implemented to support them live through the pandemic.
Funding
This study was supported by the Key Program of Beijing Science and Technology Commission (Z191100006619113, D171100007017002, D121100005012004), and the Capital’s Funds for Health Improvement and Research (No. 2018-4-4116).
Declaration of Competing Interest
We declared that there are no conflicts of interest in this work.
Acknowledgements
We thank all of the adult children of parents with mental illness involved in this study for participation and their families for t support.
References
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassani D.G., Padoin C.V., Philipp D., Veldhuizen S. Estimating the number of children exposed to parental psychiatric disorders through a national health survey. Child Adolesc. Psychiatry Ment. Health. 2009;3:6. doi: 10.1186/1753-2000-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockington I., Chandra P., Dubowitz H., Jones D., Moussa S., Nakku J., Quadros Ferre I. WPA guidance on the protection and promotion of mental health in children of persons with severe mental disorders. World Psychiatry. 2011;10:93–102. doi: 10.1002/j.2051-5545.2011.tb00023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzzi C., Tucci M., Ciprandi R., Brambilla I., Caimmi S., Ciprandi G., Marseglia G.L. The psycho-social effects of COVID-19 on Italian adolescents’ attitudes and behaviors. Ital. J. Pediatr. 2020;46:69. doi: 10.1186/s13052-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Map of China (in Chinese) https://voice.baidu.com/act/newpneumonia/newpneumonia/?from=osari_pc_3 Accessed June 2, 2020.
- Dong L., Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. J. 2020;26:1616–1618. doi: 10.3201/eid2607.200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y., Kou J., Coghill D. The validity, reliability and normative scores of the parent, teacher and self report versions of the Strengths and Difficulties Questionnaire in China. Child Adolesc. Psychiatry Ment. Health. 2008;2:8. doi: 10.1186/1753-2000-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis W.E., Zarbatany L. Understanding processes of peer clique influence in late childhood and early adolescence. Child Dev. Perspect. 2017;11:227–232. [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. e203976-e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., Li K. Anxiety and depression among general population in China at the peak of the COVID‐19 epidemic. World Psychiatry. 2020;19:249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Ma H., He Y.L., Xie B., Xu Y.F., Tang H.Y., Li M., Hao W., Wang X.D., Zhang M.Y., Ng C.H., Goding M., Fraser J., Herrman H., Chiu H.F., Chan S.S., Chiu E., Yu X. Mental health system in China: history, recent service reform and future challenges. World Psychiatry. 2011;10:210–216. doi: 10.1002/j.2051-5545.2011.tb00059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health. 2020;4:347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59:1218–1239. doi: 10.1016/j.jaac.2020.05.009. e1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciano A., Nicholson J., Meara E. The economic status of parents with serious mental illness in the United States. Psychiatr. Rehabil. J. 2014;37:242–250. doi: 10.1037/prj0000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N.R., Freeman J.Y.A., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell Joseph, M Abraham, Kristen M. Parental mental illness and the transition to college: coping, psychological adjustment, and parent-child relationships. J. Child Fam. Stud. 2018;27:2966–2977. [Google Scholar]
- National Health Commission of China . 2020. Principles for Emergency Psychological Crisis Intervention for the New Coronavirus Pneumonia. (in Chinese). http://www.nhc.gov.cn/xcs/zhengcwj/202001/6adc08b966594253b2b791be5c3b9467.shtml. Accessed March 25, 2020. [Google Scholar]
- National Health Commission of China . 2020. Notice on Strengthening the Treatment and Management for Patients With Severe Mental Illness During the COVID-19 Pandemic. (in Chinese). http://www.nhc.gov.cn/xcs/zhengcwj/202002/f315a6bb2955474c8ca0b33b0c356a32.shtml. Accessed March 25, 2020. [Google Scholar]
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin. J. Epiemiol. 2020;41:145–151. [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Ranning A., Munk Laursen T., Thorup A., Hjorthøj C., Nordentoft M. Children of parents with serious mental illness: with whom do they grow up? A prospective, population-based study. J. Am. Acad. Child Adolesc. Psychiatry. 2016;55:953–961. doi: 10.1016/j.jaac.2016.07.776. [DOI] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. Indian J. Pediatr. 2020;87:532–536. doi: 10.1007/s12098-020-03347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Lu Z.-A., Que J., Huang X.-L., Liu L., Ran M.-S., Gong Y.-M., Yuan K., Yan W., Sun Y.-K., Shi J., Bao Y.-P., Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tencent News . 2020. The Tragic Truth of a Child’s Death at Home in Xiaogan, Hubei Province. (in Chinese). https://new.qq.com/omn/20200315/20200315A0DYIG00.html. Accessed June 15, 2020. [Google Scholar]
- Teo S.S.S., Griffiths G. Child protection in the time of COVID-19. J. Paediatr. Child Health. 2020;56:838–840. doi: 10.1111/jpc.14916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Mental Health and Psychosocial Considerations During the COVID-19. outbreak, 18 March 2020. https://apps.who.int/iris/handle/10665/331490. Accessed March 25, 2020. [Google Scholar]
- WHO . 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-3-april-2020 Accessed June 15, 2020. [Google Scholar]
- WHO . 2021. Coronavirus (COVID-19) Dashboard.https://covid19.who.int/table Accessed June 1, 2021. [Google Scholar]
- Wikipedia . 2020. COVID-19 Pandemic Lockdown in Hubei. (In Chinese). https://en.wikipedia.org/wiki/COVID-19 pandemic_lockdown_in_Hubei. Accessed June 2, 2020. [Google Scholar]
- Willner P., Rose J., Stenfert Kroese B., Murphy G.H., Langdon P.E., Clifford C., Hutchings H., Watkins A., Hiles S., Cooper V. Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2020;33:1523–1533. doi: 10.1111/jar.12811. [DOI] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics. 2020;174:9. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J., Xu Y. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]