Abstract
Background
High‐intensity occupational therapy can improve arm function after stroke, but many people lack access to such therapy. Home‐based therapies could address this need, but they don’t typically address abnormal muscle co‐activation, an important aspect of arm impairment. An earlier study using lab‐based, myoelectric computer interface game training enabled chronic stroke survivors to reduce abnormal co‐activation and improve arm function. Here, we assess feasibility of doing this training at home using a novel, wearable, myoelectric interface for neurorehabilitation training (MINT) paradigm.
Objective
Assess tolerability and feasibility of home‐based, high‐dose MINT therapy in severely impaired chronic stroke survivors.
Methods
Twenty‐three participants were instructed to train with the MINT and game for 90 min/day, 36 days over 6 weeks. We assessed feasibility using amount of time trained and game performance. We assessed tolerability (enjoyment and effort) using a customized version of the Intrinsic Motivation Inventory at the conclusion of training.
Results
Participants displayed high adherence to near‐daily therapy at home (mean of 82 min/day of training; 96% trained at least 60 min/day) and enjoyed the therapy. Training performance improved and co‐activation decreased with training. Although a substantial number of participants stopped training, most dropouts were due to reasons unrelated to the training paradigm itself.
Interpretation
Home‐based therapy with MINT is feasible and tolerable in severely impaired stroke survivors. This affordable, enjoyable, and mobile health paradigm has potential to improve recovery from stroke in a variety of settings.
Clinicaltrials.gov: NCT03401762.
Introduction
Stroke remains a leading cause of disability worldwide.1, 2 A majority of stroke survivors have impaired upper limb function even after conventional rehabilitation,3 which reduces independence in activities of daily living and quality of life.4 Animal5 and human studies6 have demonstrated that high‐dose rehabilitation, even in the chronic period (more than 6 months after stroke), can improve motor function. However, high‐intensity therapy is not yet integrated into standard clinical practice, and it is unclear how scalable high‐dose, therapist‐led therapy will be. Moreover, in the U.S., only 30% of stroke survivors receive therapy after their acute inpatient stay,7 largely due to socioeconomic factors including cost, transportation, insurance, and availability of rehabilitation services. The situation is similar in the U.K.,8 with much more limited access in low‐to‐moderate income countries.9 Thus, there is a growing interest in developing home‐based therapies, either as an alternative or adjunct to conventional therapies, which could enable high‐dose therapy to be provided more widely and cost effectively.
Design criteria for any include enjoyability and motivation. In any home‐based rehabilitation system, enjoyability and motivation are critical to ensure adherence and effort and thus achieve high doses of therapy.10 While the optimal dose of most therapies is yet unproven, higher dose of therapy largely correlates with better outcomes and improved arm function.6, 11, 12
Various home‐based stroke therapies exist, including telerehabilitation, robot‐assisted therapies, virtual reality (VR) and video gaming.13, 14, 15, 16 Tele‐rehabilitation typically delivers conventional rehabilitation via communication technology.14, 16 Existing home‐based therapies are designed mainly around conventional task‐based practice, which often produces compensatory improvement in function without reducing impairment.17, 18
In addition to muscle weakness, abnormal muscle co‐activation is a major contributor to arm impairment after stroke.19, 20 Examples of abnormal co‐activation include elbow flexion during forward reaching due to abnormal activation of the biceps brachii with the anterior deltoid. In an earlier study, we designed a myoelectric computer interface (MyoCI) to reduce this abnormal co‐activation and associated arm impairment in chronic stroke survivors.21, 22 The MyoCI mapped EMG from abnormally co‐activating muscles to orthogonal components of cursor movements, and the training required decoupling these muscles to successfully acquire targets in those mapping directions. In this study, we have designed a novel, wearable, affordable version of the MyoCI called the Myoelectric Interface for Neurorehabilitation Training (MINT). MINT is designed for home use to enable high‐intensity training that can scale to many users. Here, we describe MINT protocol design and assess tolerability and feasibility in severely impaired, chronic stroke survivors.
Methods
Overview
All procedures were approved by the Northwestern University Institutional Review Board. We recruited participants through the Shirley Ryan AbilityLab Clinical Neuroscience Research Registry, day rehabilitation centers, hospital websites, physician referrals, and word‐of‐mouth. Inclusion criteria for the study were (1) age >18 years, (2) moderately‐severe to severe upper limb impairment (Fugl‐Meyer Assessment of Upper Extremity, FMA‐UE, of 8‐3023) following unilateral ischemic or hemorrhagic stroke occurring at least 6 months before enrollment. Exclusion criteria were (1) significant visual deficit impairing the ability to see a laptop screen, (2) language comprehension deficits (due to aphasia or inability to communicate in English), (3) bilateral stroke, (4) botulinum toxin treatment in the affected arm within 3 months prior to enrollment, (5) starting new physiotherapy within 3 months prior, and (6) participating in any other research studies related to upper limb within 3 months prior.
This is a report on the feasibility and tolerability of MINT therapy in moderately severely to severely impaired stroke survivors. We performed this analysis on participants from an ongoing randomized controlled trial comparing three experimental MINT groups to a sham control (ClinicalTrials.gov NCT03401762). The following is an overview of the training. Two weeks prior to training start, participants were screened in the lab and evaluated for abnormal co‐activation using a reaching task described below. They then participated in 6 weeks of training, 5 days a week at home and one day a week in the lab. Participants were randomized to an experimental or sham group. The goal of the experimental groups was to learn to activate the trained muscles in isolation from each other, while the sham group simply learned to control the EMG amplitude of a single muscle without having to isolate it from other muscles. Although the main study is evaluating efficacy using the Wolf Motor Function Test as primary outcome, we are reporting here only feasibility information, including adherence, motivation survey results, and training performance. Therefore, while we describe the randomization to different groups, we combine all participants for analysis of feasibility in this report.
Enrollment and screening
Occupational therapists evaluated the participants by assessing FMA‐UE at their initial screening visit two weeks prior to starting training. Participants who qualified based on their FMA‐UE scores were randomized to one of four different training groups, with stratification based on age and impairment level. A randomization schedule was generated by a biostatistician using R; group assignment was performed by a member of the team who did not work with, or evaluate, the participants. The groups differed in terms of the methods for controlling the cursor in the game (see Game Design for details): 2 muscles at a time (2D), 2 muscles at a time with full reaching (Reach), 3 muscles at a time (3D), or one muscle at a time (sham control group). Assessing occupational therapists remained blinded to this randomization throughout the study.
During the initial screening visit, participants also performed the reaching task. With the trunk restrained to a chair using Velcro straps, they reached as far as possible to targets placed at waist and shoulder height, in front of and to the side of the impaired arm, to identify abnormally co‐activating muscle groups for each participant.22 We recorded surface EMGs from 12 arm and shoulder girdle muscles (anterior/medial/posterior deltoids, long and lateral heads of the triceps, biceps brachii, brachioradialis, pectoralis major, trapezius, latissimus dorsi, infraspinatus, and pronator quadratus) during the reaching task using active EMG sensors (Trigno, Delsys, Inc.). We identified the muscles with the highest abnormal co‐activation, defined as pairwise correlation coefficients, to customize the training muscle sets for each participant. Co‐activation between the following muscle sets were considered abnormal19, 20: anterior deltoid/biceps, anterior deltoid/posterior deltoid, anterior deltoid/brachioradialis, biceps/triceps, brachioradialis/triceps, pectoralis major/biceps, pec major/brachioradialis, pronator/biceps, anterior deltoid/trapezius. (While deltoid/trapezius often co‐activate in healthy individuals in many movements, we reasoned that they can also be decoupled for certain movements and that this could lead to freer movement of the shoulder.)
Training
On the first training visit (Week 0), we taught participants to place surface EMG sticker electrodes (Bio‐Medical Instruments, Inc.) on the muscles to be trained. Each electrode consisted of 3 snap‐style, 10‐mm diameter Ag‐AgCl coated electrode contacts; two contacts were connected to bipolar leads and the third to a reference lead. The bipolar leads were placed parallel to the long axis of each muscle (Fig. 1). We taught the participants how to place the electrodes correctly and provided a photo of their arm for reference of electrode placement. Alignment marks were made on the sticker and the skin using a skin marker to enable participants to replace the electrodes on the arm as needed. These marks were reinforced each week in the lab and at home when the sticker was replaced. Participants were instructed to use the same electrodes for up to 5 days or until they started to come off, at which point they were replaced. Participants were sent home with a laptop and the MINT device, along with printed instructions for logging into the laptop and using the MINT. When possible, we also educated participants’ family members or caregivers in these procedures, in case they required assistance at home.
Figure 1.
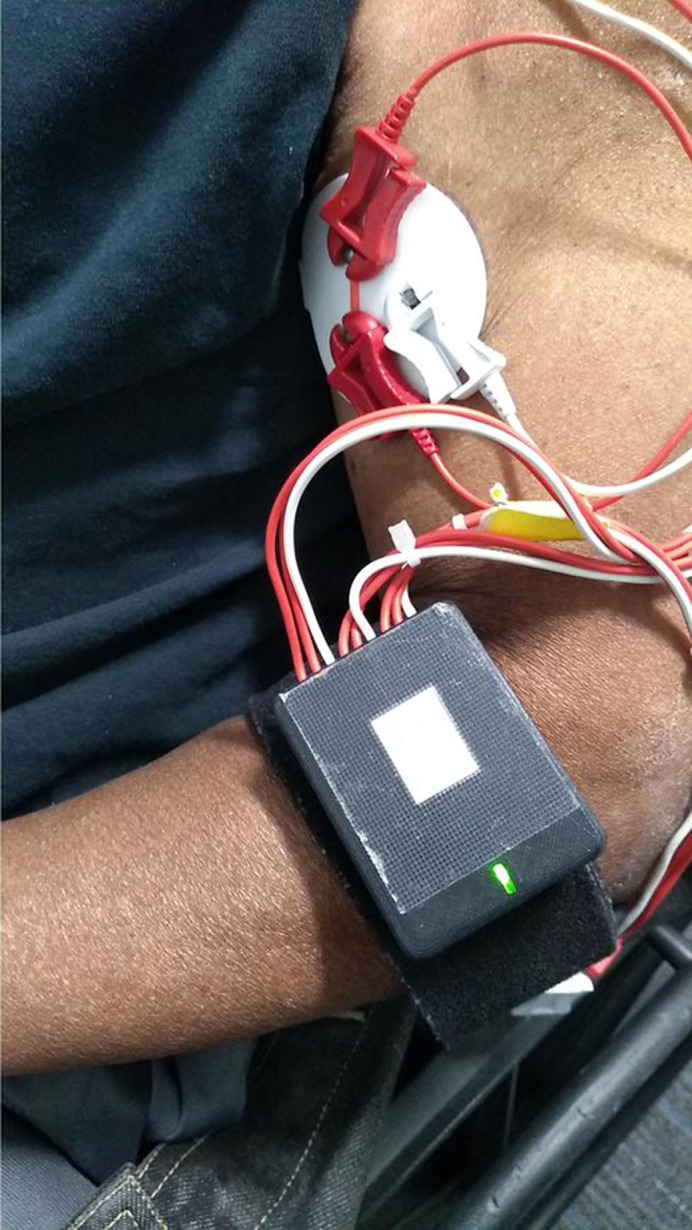
MINT Device and electrodes. The MINT device (black case) was attached to a strap on the participant’s arm. The red line on the EMG sticker was used to guide participants to line up the recording electrodes (red clips) with the long axis of each muscle. The white clip is the reference electrode.
Participants were asked to train with the MINT for 90 min each day, for a period of 36 days over 6 weeks. During this time the participants also made weekly visits to our lab, which we used to monitor training progress, ensure correct training performance and electrode placement, and perform clinical outcome evaluations that will be reported separately upon completing the randomized trial. To help troubleshoot issues remotely in between visits, lab members communicated with the participants or their family members using video call, remote computer access, or by phone when participants did not have home WiFi. Training muscle sets were changed at 3 weeks for the 3D group (who trained on two sets of 3 muscles each), and at Weeks 2 & 4 for the 2D, Reach (three sets of 2 muscles each) and Sham group (three sets of 1 muscle each). We chose to balance the number of total muscles potentially trained in the experimental groups (6 muscles, trained as 3 sets of 2 muscles vs. 2 sets of 3 muscles), rather than the time of training for each muscle set.
MINT device
The custom‐built, wearable MINT device was developed in collaboration with Myomo, Inc. The device, which measures 6 × 4.5 × 1.5 cm, sampled EMGs at 2 kHz and used a Kalman filter to extract the EMG envelopes. These envelope signals were then streamed via Bluetooth at 50 Hz to a laptop, where the signals were used in a Python‐based gaming platform in real time and stored for offline analysis.
EMG calibration
The EMG signals used to control the game were normalized to the EMG value during maximum voluntary contraction (MVC). This served multiple purposes. It equalized the effort needed across muscles, reduced the likelihood of fatigue during training, and enabled comparisons of effort across days and participants. MVC was calculated before training on each day. The MINT game interface prompted participants to produce MVCs using videos demonstrating how to move the arm to activate each muscle trained. Three MVC attempts were made for each muscle. On each attempt, the participant was instructed to relax the muscle for 3 s and then maximally contract the muscle in an isometric manner using readily available props to brace against, such as a desk, wall or the back rest of their chair. For example, for biceps, the participant was instructed to flex the elbow while pushing up against the bottom of a table or desk. The videos were 8–12 s in duration; as participants had variable reaction times in starting to contract, this enabled us to obtain at least a few seconds of maximal contraction in most participants. The MVC was calculated by segmenting the EMG envelope into 500‐ms bins, computing the mean value of each bin, then assigning the maximum of these mean values over all 3 attempts.
Game design
Participants controlled a cursor within a 3D environment created using Blender and Python. Each EMG envelope sample (20 ms) was mapped to one orthogonal component of the cursor’s position (Fig. 2). Participants moved the cursor into the “home” target at the bottom left of the screen by relaxing the controlling muscles. After holding in the home target for 1 s, an outer target appeared near the opposite side of the screen. Participants needed to move the cursor into that target by activating the controlling muscle and hold in the target for 0.5 s. Positive audiovisual feedback was provided for successful trials. If the participant failed to acquire the target within 7 s, the trial ended and was labeled a failure.
Figure 2.

MINT training group screenshots and cursor mappings. Examples of screenshots and cursor mapping for the different MINT training groups. (A) In the sham control, participants controlled the cursor with one muscle in one direction (red arrow indicates mapping direction of increasing EMG activity). (B) The 2D group controlled the cursor as a vector sum of the two muscles (red arrows indicate mapping directions). (C) The Reach group provided similar feedback to the 2D group with the addition of prompting the participants to reach out in a direction using the targeted muscle (e.g., elbow flexion for biceps, green arrow). (D) The 3D group controlled the cursor as a vector sum of three muscles (dashed arrow, mapping into the screen). The game “skins” changed with each different set of muscles trained.
The cursor position was determined by the vector sum of the EMG components. There were two components for the 2D and Reach groups, three components for the 3D group, and one component for the sham control. Thus, to acquire targets on the cardinal axes, participants in the experimental groups had to activate the targeted muscle in isolation from the other muscles (those in the sham did not).
We normalized the components of cursor position according to the following equation:
| (1) |
where P was the position of each component, EMG was the EMG envelope amplitude, EMGB was the mean EMG during a 1‐s baseline (rest) period at the start of each trial, M was the MVC, W was the width of the game window on the screen, and fM and fB were the MVC factor and baseline factor, respectively. The MVC factor scaled the effort required to acquire the targets so that participants did not fatigue too quickly. The baseline was subtracted from the EMGs to enable participants to play the game despite having some difficulty relaxing the muscles, as tonic muscle contraction is a common issue among stroke survivors.
To keep participants engaged and challenged, the difficulty level increased steadily as performance improved. Each time the participant performed 2 consecutive 10‐minute runs with 70% or higher success rate, the level was incremented; a success rate below 50% in a single run caused the level to decrement. Increases in difficulty level corresponded to changes in 5 factors: increasing the angular distance of the outer target from the diagonal, decreasing cursor size, decreasing target size, decreasing the baseline factor (which required the participant to relax the arm muscles more after each trial), and increasing the MVC factor (which required more activation on each trial). We initialized the MVC factor to 0.15 for the first level (meaning that outer targets were placed at a distance of 15% of MVC from the home target), with steady increments thereafter. The outer targets were generated at a random angle within a selected range of angles, starting close to the 45° diagonal between muscles (allowing for more co‐activation) and moving farther away from the diagonal as the level increased, thereby requiring more isolation of muscles.
Adherence, motivation, and performance measures
We defined adherence as the amount of time trained by each participant, which was recorded by the MINT software. We computed the mean training time per day over all participants. To assess enjoyment, motivation and effort during the training protocol, we surveyed participants using a modified version of the Intrinsic Motivation Inventory (IMI)24 at the end of the 6‐week training. This was a questionnaire with 18 questions graded on a 7‐point Likert scale, with 1 being the lowest rating (‘Strongly Disagree’), 7 the highest (‘Strongly Agree’), and 4 indicating a neutral response. The wording of these questions was modified from the original IMI to reflect the participants’ experience as it related to the MINT training (Supplementary Material). The questions were stratified into categories reflecting enjoyment, effort, perceived benefit, and satisfaction. We computed the mean of these scores over all participants, over the complete survey and within each category. Certain questions in the survey were worded negatively; the scores on these questions (n) were reversed (8‐n) to calculate the means. Our focus for this paper was on the first two categories of enjoyment and effort, as a measure of feasibility. This survey was added to the protocol after the start of the study for enhanced participant feedback and has been completed by 15 participants to date.
Game performance metrics
We measured training game performance using the time‐to‐target (TTT; mean time to acquire each target) divided by the difficulty level in each run. We computed TTT separately for each muscle set—i.e., every two weeks for the sham, 2D, and Reach groups. To simplify our analysis, we combined the data across groups and muscle sets. For the 3D group, which trained for 3 weeks on each muscle set, we report only the first two weeks of each set to enable combination with the other groups. We also report the change co‐activation for the experimental groups as a whole, during the last day of training of each muscle set compared to the baseline co‐activation during the reaching task. Because sham only recorded from one muscle, we cannot report co‐activation changes in that group.
Results
Participants
A total of 60 stroke survivors have enrolled in the main study to date; 17 were screened out (Fig. 3). Five participants dropped from the study after screening but before starting training, and 13 dropped after beginning training. Reasons for dropout (and number of participants) included the following: computer illiteracy preventing sufficient training (3), personal reasons/transportation issues (6), insufficient compensation (2), development of other health problems or excessive fatigue (4), and inability to communicate and comply with training schedule (3). We had to suspend training for two participants due to COVID‐19‐related restrictions on research.
Figure 3.
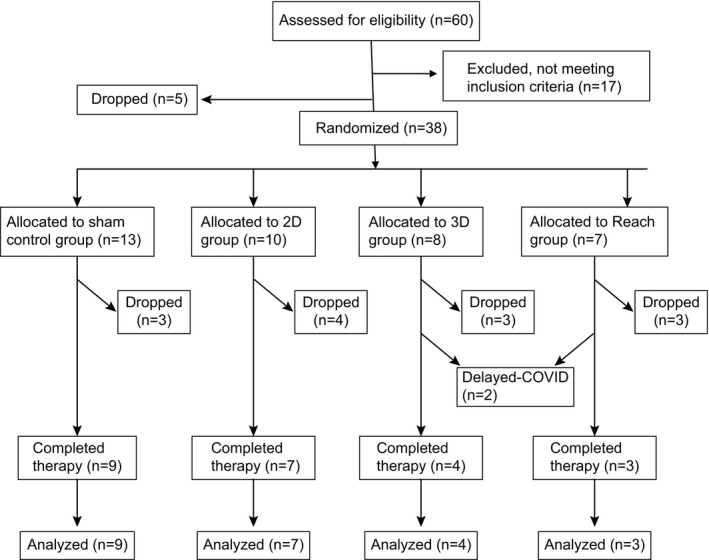
CONSORT flowchart.
The 23 participants who completed training were 58 ± 15 years of age (mean ± SD); 10 were male and 13 female. Their baseline FMA‐UE was 17.8 ± 5.7, indicating severe impairment.23 The 13 participants who dropped out of the study after starting training did not differ significantly in either age (62 ± 11, p = 0.3, t‐test) or FMA‐UE (18.1 ± 6.7, p = 0.8) from those who completed the study. Here, we report qualitative feedback from participants regarding the MINT protocol and quantitative outcomes in the form of adherence, IMI survey responses and game performance metrics.
Training was feasible and highly adhered to
Training adherence was high overall. Participants trained 82 ± 18 min of the required 90 minutes per day. While only 30% of participants averaged at least 90 min per day, 96% were able to train for at least 60 min/day. Some training was missed due to software or hardware malfunctions (n = 6 participants, 30‐270 min each), or a family‐related issue (n = 1, 270 min). Importantly, participants performed a high number of movements for a daily, home‐based therapy: 299 ± 8 repetitions per day.
Most participants were able to set up the MINT device independently. Two participants required daily assistance from their caregivers to connect the device to the electrodes on their arm. Five participants received intermittent assistance from family members, primarily for help with logging into the laptop or carrying the device, but also with placement of electrodes on posterior muscles such as posterior deltoid and infraspinatus.
Participant experience
During the period of training, we actively asked for anecdotal feedback from the participants during lab visits and phone calls. Examples of such feedback included: “The concept for this game is definitely good”, “I get frustrated when I cannot control the cursor like how I wanted”, and “This is the best game for arm movement.” In addition, seven participants stated that they were able to move and use their affected arm more in activities of daily living. Eight participants expressed interest in continuing MINT training after completing the study. Muscle fatigue was mentioned by three participants following training on 1–4 days each, two of whom had more muscle pain than their usual amount. However, allowing flexibility in choosing the day off and spreading training over multiple sessions within each day mitigated the effects of fatigue, enabling these participants to complete the desired duration of training. The fatigue largely correlated with having too much tonic contraction on those days, leading to difficulty relaxing completely and spending a great deal of effort trying to reposition their arm to start a new trial. This was only a problem when the MVC for that muscle was also low, because this limited the dynamic EMG range between home and outer targets, and thus any tiny fluctuation made it more difficult for the cursor to remain in the home target. Accurately measuring MVC was an important, and yet difficult, aspect of training. The electrodes used were not designed for long‐term home use and thus often needed to be replaced by participants, due to loss of adhesion. This sometimes led to inaccurate MVC estimates and was particularly an issue in 4 participants who trained on the brachioradialis, due to the high arm curvature near the muscle. Excess fat over the target muscles, e.g., triceps, also reduced MVC in some participants. Four participants described difficulty in relaxing the arm during training. Seven participants complained that the login experience was difficult, largely due to the university‐mandated security software on the laptop that required frequent updates and more elaborate login procedures. In addition, the MINT devices occasionally had either Bluetooth or electrode connection issues. Finally, three participants experienced transient skin irritation from the electrodes, which did not cause them to drop out of the study or miss significant amounts of training.
MINT training was motivating and enjoyable
The modified IMI results showed that participants largely enjoyed the training and were highly motivated to train (Fig. 4). Ninety‐two percent of the surveyed participants agreed at least slightly that the MINT was enjoyable (mean ± SD score of 5.7 ± 1.0) and motivating (6.4 ± 0.6). Keeping track of their high score was motivating for most participants (6.5 ± 1.1). The training was enjoyed by participants in the experimental groups (5.8 ± 1.2, n = 10) as well as in the sham control group (5.4 ± 0.6, n = 5); there was no significant difference between experimental and sham groups (p = 0.4, t‐test). Eighty‐five percent of participants felt the training was more enjoyable than standard physiotherapy (6.4 ± 1.1). Ninety‐three percent of participants rated themselves as exerting high effort, with a mean score of 6.4 ± 0.6 in effort. Overall, 60% of participants thought MINT training improved their arm function (mean score of 5.6 ± 1.4), and 87% said they would recommend it to other stroke survivors (mean score of 6.3 ± 1.0).
Figure 4.
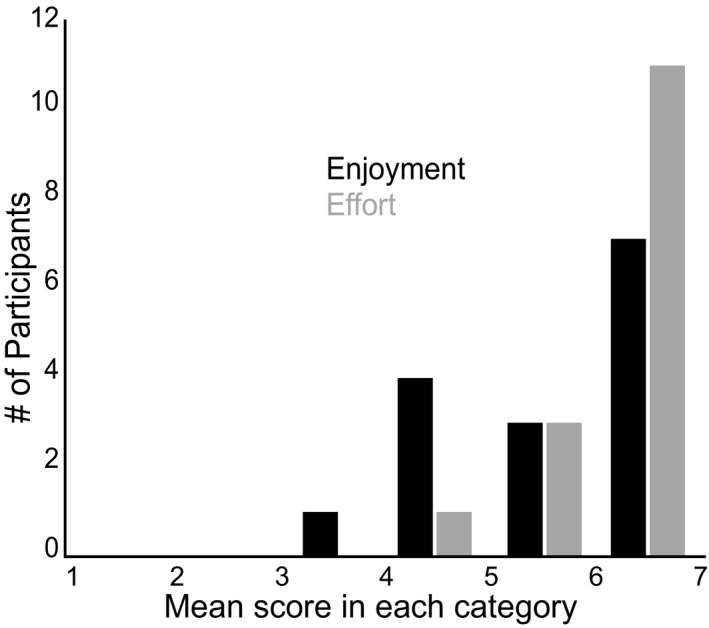
Histogram of responses to questions assessing enjoyment (black) and effort (gray) from the modified IMI survey. Almost all participants enjoyed the training to some extent and were motivated to exert high effort.
Participants learned to perform the task efficiently
Participants in the experimental groups reached 49 ± 10% (mean ± SE over all groups) of the maximum game difficulty level and those in the sham group all reached the maximum level. Weighted TTT decreased steadily over all three muscle sets combined (R = −0.77, p = 0.003; Fig. 5A). There was higher variability in the last 3 days due to three participants training only 8 or 9 days on the first muscle set. Overall, participants succeeded more quickly as training progressed, which suggested that they were engaged with training and learned to reduce co‐activation, at least in the experimental group. Indeed, in the experimental group, co‐activation declined by 54 ± 10% over all three muscle sets combined, compared to the baseline reaching task (p = 0.04, t‐test; Fig. 5B). Co‐activation decreased as early as the first day of training.
Figure 5.

Game performance and co‐activation improved with training. (A) Mean (±SE) performance (weighted TTT) over all trials on each day over participants from all groups, over all three muscle sets combined. Gray dashed line is best‐fit linear regression, R = −0.77, p = 0.008. (B) Co‐activation (R) over all experimental groups decreased significantly (*) from baseline (blue) to the last day of training (black). Data are combined over all three muscle sets.
Discussion
We designed and tested a novel, wearable, high‐dose, home‐based therapy to reduce abnormal co‐activation in chronic stroke survivors. We found that participants adhered very well to the training protocol and rated MINT as enjoyable and motivating. Anecdotal reports largely supported the formal survey results. Participants improved in their training performance over time. This indicates that they were engaged in learning the games. In addition, participants in the experimental groups learned to reduce co‐activation between the targeted muscles. The number of daily repetitions (299) was very high compared to standard therapy (typically 3225). This demonstrates that high‐intensity MINT training is feasible, motivating, and enjoyable in people with severe arm impairment from stroke.
The potential to help people with severe impairment is particularly important. Conventional rehabilitation techniques work better in patients with less severe impairments,26, 27 largely because the subjects must have sufficient remaining function to participate.28, 29 Unfortunately, severely impaired patients are the most in need of new therapies, yet are often excluded from clinical trials,29 including most telerehabilitation trials.9, 13 MINT only requires electrical muscle activity, not movement, which allows severely impaired patients to participate. Moreover, these patients also have the most abnormal co‐activation.17 Although we excluded people with FMA‐UE less than 8 due to their extremely limited mobility for this study, it is possible that they might be able to benefit as well, since only some EMG modulation is required. However, outcome metrics that are used in clinical trials are very insensitive to improvement at the very low end of the scale, which makes it problematic to include such patients in rehabilitation trials without negatively biasing results.
Enjoyability and motivation are critical to participant engagement,30, 31 which leads to greater therapy doses, which in turn may lead to better outcomes.6, 10 Greater adherence also correlates with greater functional improvement.32, 33 A randomized clinical trial of home‐based gaming therapy for subacute stroke showed that telerehabilitation was noninferior to in‐clinic therapy in terms of adherence (40 out of 70 min/day) and reduction in impairment.10 Adherence rates among our participants, in a more time‐intensive protocol (6 days/week compared to 3 days/week), were high, with a mean of 82 min/day of training. This is especially encouraging in a severely impaired population. Fewer than a third of conventional home‐based stroke rehabilitation therapy programs are reported to achieve an adherence rate of 75% or higher,34, 35 while partial adherence to home exercise programs has been reported as 65%.36 Our results (96% completed two‐thirds of the requested dose of therapy) thus compare favorably with conventional home exercise programs, as well as with the aforementioned trial of telerehabilitation (93% completed 57% of requested dose10). Several features of the MINT paradigm were designed to increase adherence. The use of video games was designed to increase enjoyability, as has been reported before.31, 37, 38 Our games also tracked high scores, which participants rated as motivating in and of themselves. Overall, the MINT helped motivate participants to engage in therapy, as indicated by the survey results. Part of this motivation may have been simply providing detailed feedback about the muscles, which is often lacking in participants with very little motion in the limb.39 In addition, the ability to play the games at home likely improved adherence compared to having to come to a lab or clinic daily for 6 weeks. We also enabled participants to split up training into multiple sessions per day if desired, and we communicated frequently with participants. Finally, while some of the IMI survey questions try to distinguish between intrinsic and extrinsic motivation, it is difficult to make definitive conclusions from a limited survey. An additional survey early on in training might provide more information about how much intrinsic vs. extrinsic motivation affected enjoyment, participation, and functional improvement.
This study did identify several challenges for this version of MINT. While partial adherence was high, 70% of participants did not achieve the requested 90 min/day of therapy. This is not entirely surprising, given that other home‐based therapies also had difficulty ensuring participant adherence to the full amount of practice time instructed.16, 37 There was also a high rate of attrition; however, this was largely due to factors other than the MINT paradigm itself, as documented above. In a minority of dropouts, there was some limitation in participation due to computer literacy or motivation. Thus, making a wider variety of games may help enable motivation. Participants who dropped out during training did not differ in age or impairment from those that completed training. Thus, older, severely impaired patients could use the technology, which bodes well for MINT feasibility in general. The current version is somewhat limited by the need to clip wired leads to EMG electrodes. Future MINT versions will aim to improve on the design, with one near‐term goal being a completely wireless system, with no need to clip wires on, to make it even easier to use. EMG electrodes that require less frequent replacement would help ensure reliable recordings. Laptop security/login issues and computer literacy can be easily remedied by designing a phone or tablet app. We continue streamlining the current system as much as possible. Finally, fatigue may be an issue in severely impaired patients, especially when concurrently working and receiving conventional therapy, as were many of our participants. Thus, finding an optimal dose for MINT therapy is an important future goal.
Conflict of Interest
Dr. Slutzky reports non‐financial support from Myomo, Inc during the conduct of the study. In addition, Dr. Slutzky has a patent issued related to the MINT device, and has consulted for Battelle on their Strategic Advisory Board.
Supporting information
Supplementary Material
Acknowledgments
We thank Samuel Kesner and Richard Harvey for device and study design assistance, respectively. This study was supported by NIH grants R01NS099210 and R01NS112942.
Funding Statement
This work was funded by NIH grants R01NS099210 and R01NS112942.
References
- 1.Cramer SC. Brain repair after stroke. N Engl J Med 2010;362(19):1827–1829. [DOI] [PubMed] [Google Scholar]
- 2.Virani Salim S, Alonso A, Benjamin Emelia J, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 2020;141(9):e139–e596. [DOI] [PubMed] [Google Scholar]
- 3.Dobkin BH. Rehabilitation after stroke. N Engl J Med 2005;352(16):1677–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sveen U, Bautz‐Holter E, Margrethe Sodring K, Bruun Wyller T, Laake K. Association between impairments, self‐care ability and social activities 1 year after stroke. Disabil Rehabil 1999;21(8):372–377. [DOI] [PubMed] [Google Scholar]
- 5.Nudo RJ, Wise BM, SiFuentes F, Milliken GW. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science 1996;272(5269):1791. [DOI] [PubMed] [Google Scholar]
- 6.Ward NS, Brander F, Kelly K. Intensive upper limb neurorehabilitation in chronic stroke: outcomes from the Queen Square programme. J Neurol Neurosurg Psychiatry 2019;90(5):498–506. [DOI] [PubMed] [Google Scholar]
- 7.Ayala C, Fang J, Luncheon C, et al. Use of outpatient rehabilitation among adult stroke survivors—20 states and the District of Columbia, 2013, and four states, 2015. Morb Mortal Weekly Rep 2018;67(20):575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKevitt C, Fudge N, Redfern J, et al. Self‐reported long‐term needs after stroke. Stroke 2011;42(5):1398–1403. [DOI] [PubMed] [Google Scholar]
- 9.Kamalakannan S, Gudlavalleti Venkata M, Prost A, et al. Rehabilitation needs of stroke survivors after discharge from hospital in India. Arch Phys Med Rehabil 2016;97(9):1526–32.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cramer SC, Dodakian L, Le V, et al. Efficacy of home‐based telerehabilitation vs in‐clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol 2019;76(9):1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta‐analysis. PLoS ONE 2014;9(2):e87987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsieh Y‐W, Wu C‐Y, Liao W‐W, Lin K‐C, Wu K‐Y, Lee C‐Y. Effects of treatment intensity in upper limb robot‐assisted therapy for chronic stroke: a pilot randomized controlled trial. Neurorehabil Neural Repair 2011;25(6):503–511. [DOI] [PubMed] [Google Scholar]
- 13.Chen Y, Abel KT, Janecek JT, Chen Y, Zheng K, Cramer SC. Home‐based technologies for stroke rehabilitation: a systematic review. Int J Med Informatics 2019;123:11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buick AR, Kowalczewski J, Carson RG, Prochazka A. Tele‐supervised FES‐assisted exercise for hemiplegic upper limb. IEEE Trans Neural Syst Rehabil Eng 2016;24(1):79–87. [DOI] [PubMed] [Google Scholar]
- 15.Wolf SL, Sahu K, Bay RC, et al. The HAAPI (Home Arm Assistance Progression Initiative) trial: a novel robotics delivery approach in stroke rehabilitation. Neurorehabil Neural Repair 2015;29(10):958–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dodakian L, McKenzie AL, Le V, et al. A home‐based telerehabilitation program for patients with stroke. Neurorehabil Neural Repair 2017;31(10–11):923–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krakauer JW. Arm function after stroke: from physiology to recovery. Semin Neurol 2005;25(4):384–395. [DOI] [PubMed] [Google Scholar]
- 18.Kitago T, Liang J, Huang VS, et al. Improvement after constraint‐induced movement therapy: recovery of normal motor control or task‐specific compensation? Neurorehabil Neural Repair 2013;27(2):99–109. [DOI] [PubMed] [Google Scholar]
- 19.Dewald J, Pope PS, Given JD, Buchanan TS, Rymer WZ. Abnormal muscle coactivation patterns during isometric torque generation at the elbow and shoulder in hemiparetic subjects. Brain 1995;118(2):495. [DOI] [PubMed] [Google Scholar]
- 20.Roh J, Rymer WZ, Perreault EJ, Yoo SB, Beer RF. Alterations in upper limb muscle synergy structure in chronic stroke survivors. J Neurophysiol 2013;109(3):768–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright ZA, Rymer WZ, Slutzky MW. Reducing abnormal muscle coactivation after stroke using a myoelectric‐computer interface: a pilot study. Neurorehabil Neural Repair 2014;28(5):443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mugler EM, Tomic G, Singh A, et al. Myoelectric computer interface training for reducing co‐activation and enhancing arm movement in chronic stroke survivors: a randomized trial. Neurorehabil Neural Repair 2019;33(4):284–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woytowicz EJ, Rietschel JC, Goodman RN, et al. Determining levels of upper extremity movement impairment by applying a cluster analysis to the Fugl‐Meyer assessment of the upper extremity in chronic stroke. Arch Phys Med Rehabil 2017;98(3):456–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McAuley E, Duncan T, Tammen VV. Psychometric properties of the intrinsic motivation inventory in a competitive sport setting: a confirmatory factor analysis. Res Q Exerc Sport 1989;60(1):48–58. [DOI] [PubMed] [Google Scholar]
- 25.Lang CE, MacDonald JR, Reisman D, et al. Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil 2009;90(10):1692–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parry R, Lincoln N, Vass C. Effect of severity of arm impairment on response to additional physiotherapy early after stroke. Clin Rehabil 1999;13(3):187–198. [DOI] [PubMed] [Google Scholar]
- 27.Winstein CJ, Rose DK, Tan SM, Lewthwaite R, Chui HC, Azen SP. A randomized controlled comparison of upper‐extremity rehabilitation strategies in acute stroke: a pilot study of immediate and long‐term outcomes. Arch Phys Med Rehabil 2004;85(4):620–628. [DOI] [PubMed] [Google Scholar]
- 28.Nowak DA, Grefkes C, Ameli M, Fink GR. Interhemispheric competition after stroke: brain stimulation to enhance recovery of function of the affected hand. Neurorehabil Neural Repair 2009;23(7):641. [DOI] [PubMed] [Google Scholar]
- 29.Buch ER, Modir Shanechi A, Fourkas AD, Weber C, Birbaumer N, Cohen LG. Parietofrontal integrity determines neural modulation associated with grasping imagery after stroke. Brain 2012;135(2):596–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.King M, Hijmans JM, Sampson M, Satherley J, Hale L. Home‐based stroke rehabilitation using computer gaming. New Zealand J Physiother. 2012;40:128+. [Google Scholar]
- 31.Warland A, Paraskevopoulos I, Tsekleves E, et al. The feasibility, acceptability and preliminary efficacy of a low‐cost, virtual‐reality based, upper‐limb stroke rehabilitation device: a mixed methods study. Disabil Rehabil 2019;41(18):2119–2134. [DOI] [PubMed] [Google Scholar]
- 32.Duncan PW, Horner RD, Reker DM, et al. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke 2002;33(1):167–178. [DOI] [PubMed] [Google Scholar]
- 33.Benvenuti F, Stuart M, Cappena V, et al. Community‐based exercise for upper limb paresis: a controlled trial with telerehabilitation. Neurorehabil Neural Repair 2014;28(7):611–620. [DOI] [PubMed] [Google Scholar]
- 34.Donoso Brown EV, Nolfi D, Wallace SE, Eskander J, Hoffman JM. Home program practices for supporting and measuring adherence in post‐stroke rehabilitation: a scoping review. Top Stroke Rehabil 2020;27(5):377–400. [DOI] [PubMed] [Google Scholar]
- 35.Jurkiewicz MT, Marzolini S, Oh P. Adherence to a home‐based exercise program for individuals after stroke. Top Stroke Rehabil 2011;18(3):277–284. [DOI] [PubMed] [Google Scholar]
- 36.Miller KK, Porter RE, DeBaun‐Sprague E, Van Puymbroeck M, Schmid AA. Exercise after stroke: patient adherence and beliefs after discharge from rehabilitation. Top Stroke Rehabil 2017;24(2):142–148. [DOI] [PubMed] [Google Scholar]
- 37.Proffitt R, Lange B. Feasibility of a customized, in‐home, game‐based stroke exercise program using the Microsoft Kinect® Sensor. Int J Telerehabil 2015;7(2):23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lewis GN, Woods C, Rosie JA, McPherson KM. Virtual reality games for rehabilitation of people with stroke: perspectives from the users. Disabil Rehabil Assist Technol 2011;6(5):453–463. [DOI] [PubMed] [Google Scholar]
- 39.Young SJ, van Doornik J, Sanger TD. Visual feedback reduces co‐contraction in children with dystonia. J Child Neurol 2011;26(1):37–43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


