Abstract
Background:
Azerbaijan is an upper middle-income country in South Caucasus with an area of 86,600 km2 and a total population of 10 million people and gross domestic product of US $4480 per capita. The aim of this research is to estimate fungal infection burden and highlight the problem at national and international levels.
Methods:
Fungal infection burden was estimated using data from epidemiological papers and population at risk and LIFE (Leading International Fungal Education) modelling.
Results:
The number of people living with human immunodeficiency virus (PLHIV) in 2018 was 6193, 29% of them not receiving antiretroviral therapy. Based on 90% and 20% rates of oral and oesophageal candidiasis in patients with CD4 cell count <200 µl–1 we estimate 808 and 579 patients with oral and oesophageal candidiasis, respectively. The annual incidences of cryptococcal meningitis and Pneumocystis pneumonia are 5 and 55 cases, respectively. We estimated 2307 cases of chronic pulmonary aspergillosis (CPA), 4927 patients with allergic bronchopulmonary aspergillosis (ABPA), and 6504 with severe asthma with fungal sensitization (SAFS). Using data on chronic obstructive pulmonary diseases (COPD), lung cancer, acute myeloid leukaemia rates, and number of transplantations, we estimated 693 cases of invasive aspergillosis following these conditions. Using a low-European rate for invasive candidiasis, we estimated 499 and 75 patients with candidemia and intra-abdominal candidiasis respectively. The number of adult women (15–55 years) in Azerbaijan is ~2,658,000, so it was estimated that 159,490 women suffer from recurrent vulvovaginal candidiasis (rVVC).
Discussion:
In total, the estimated number of people suffering from fungal diseases in Azerbaijan is 225,974 (2.3% of the population). However, the fungal rate is underestimated due to lack of epidemiological data. The most imminent need is improvement in diagnostic capabilities. This aim should be achieved via establishing a reference laboratory and equipping major clinical centers with essential diagnostics assays.
Keywords: aspergillosis, Azerbaijan, candidiasis, cryptococcal meningitis, fungal infections, Pneumocystis pneumonia
Introduction
Only about 300 out of 100,000 known species of fungi can cause disease in humans.1 Over 90% of reported deaths from fungal diseases are caused by Aspergillus spp., Candida spp., Cryptococcus, and Pneumocystis spp.2 Many infections are missed completely because the clinical features are subtle early in disease and non-specific, and, if sensitive diagnostics are not used, the aetiology is usually mistaken.3–5 The incidence of invasive fungal infections has increased over the past decades,6–9 partly because of improved recognition, but also because of additional risk groups – ibrutinib treatment of cancer patients and severe influenza being good examples.10 Several trends in epidemiology have emerged: increased incidence of mold infection (caused by Aspergillus spp. in particular) in patients with chronic obstructive pulmonary disease (COPD) exacerbations and lung cancer patients,11,12 and increase of non-Candida spp. and Zygomyces-associated infections.13,14 Other risk groups include acute leukaemia (AL), hematopoietic stem cell transplant (HSCT) and solid organ transplant recipients, HIV/AIDS (acquired immune deficiency syndrome), COPD, and intensive care unit (ICU) patients.
Chronic and allergic fungal infections are now recognized and appreciated more widely. Disfiguring skin mycetoma and chromoblastomycosis are recognized by the World Health Organization (WHO) as neglected tropical diseases (NTD).15 Chronic pulmonary aspergillosis (CPA), often either following pulmonary tuberculosis (PTB) as a complication or mimicking it, is thought to affect about 3 million people worldwide with an annual mortality of 15%.16 Chronic and allergic fungal rhinosinusitis are common in the community.17,18 Allergic bronchopulmonary aspergillosis (ABPA) complicates asthma at rate of approximately 2.5% and may eventually lead to CPA,19 while the rate of severe asthma with fungal sensitisation (SAFS) is 33% in the most poorly controlled group.20 Invasive aspergillosis (IA) is a life-threatening infection occurring both in immunocompromised and immunocompetent patients. The frequency of IA among acute myeloid leukemia (AML) patients is approximately 10%,21 whereas the frequency among patients with lung cancer is 2.6%.21 IA may also develop in patients without immunosuppression; in particular, IA complicates COPD in approximately 3% of patients with exacerbations,11 and in 19% of those with influenza.10
According to the United States (US) Centres for Disease Control and Prevention (CDC), fungal infections remain the major opportunistic infections in people living with human immunodeficiency virus (PLHIV).22 Cryptococcal meningitis (CM) and Pneumocystis pneumonia (PCP) are AIDS-defining illnesses and are uniformly fatal without treatment. Unfortunately, more than 50% cases of CM and PCP are diagnosed post-mortem.5
Currently, the emergence of azole and echinocandin resistance in Candida spp. and azole resistance in Aspergillus spp. has worsened treatment outcomes.23,24 Mortality rates from azole-resistant mold infections vary between 50% and 100%.23
Globally, the burden of fungal diseases is underestimated due to the complexity of diagnosis and paucity of national surveillance programs.1,14 Life-threatening fungal infections are thought to develop in immune compromised or ICU patients. However, these pathologies tend to develop as underlying conditions in immune competent people as well. Underestimation of fungal diseases leads to poor recognition of the problem and increase of patients suffering from invasive and non-invasive fungal pathologies.
Azerbaijan is an upper middle-income country in South Caucasus with land area of 86,600 km2 located between the Caspian Sea and the Caucasian Mountains (Figure 1).25 It has a total population of 10 million people and gross domestic product of US $4480 per capita in 2019.26 The aim of this research is to estimate fungal infection burden in Azerbaijan. To the best of our knowledge, such work has never been done before; our results highlight the problem at national and international levels.
Figure 1.
Geography of Azerbaijan.25
Methods
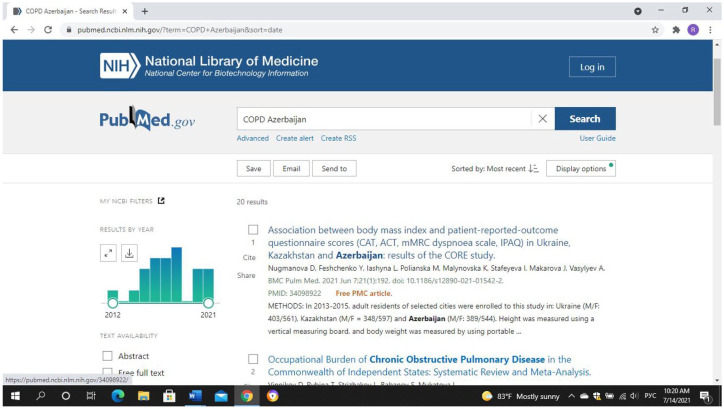
In order to evaluate burden of fungal diseases, epidemiological papers were searched in international databases (PubMed, Google Scholar, and elibrary.ru). The search terms included ‘fungal infections and Azerbaijan’, specific underlying conditions (e.g., “bronchial asthma”, “chronic obstructive pulmonary disease”, etc.), and specific fungal infections (e.g., “invasive aspergillosis”) (Figure 2). The time period for the search was all dates up to December 2019. Since no papers on burden of fungal infection were found, the LIFE (Leading International Fungal Education) model was utilized, which uses population at-risk to estimate the burden of fungal infections.
Figure 2.
Search of publications related to fungal diseases in international databases.
Results
A total burden of fungal diseases, rate per 100,000 population in relevance to underlying pathological conditions are given in Table 1. In 2018, there were total of 48,685 patients with cancer (487.7 per 100,000), 8684 – with tuberculosis (87 per 100,000), 208,300 with respiratory system disorders (2087 per 100,000) and 6193 with HIV/AIDS (62 per 100,000) in Azerbaijan.
Table 1.
Estimated burden of serious fungal infections in Azerbaijan.
| Number of patients with underlying disorder |
Rate per 100,000 | Total burden | |||||
|---|---|---|---|---|---|---|---|
| Nonea | Respiratory | HIV/AIDS | Cancer/Tx | ICU | |||
| Oesophageal candidiasis | – | – | 579 | – | – | 5.8 | 579 |
| Oral candidiasis | – | – | 808 | – | – | 8.1 | 808 |
| Candidemia | – | – | – | – | 499 | 5 | 499 |
| Candida peritonitis | – | – | – | – | 75 | 0.75 | 75 |
| RVVC | 159,489 | – | – | – | – | 3196 | 159,489 |
| ABPA | – | 4927 | – | – | – | 49.37 | 4927 |
| SAFS | – | 6504 | – | – | – | 65.16 | 6504 |
| CPA after TB | – | 577 | – | – | – | 5.8 | – |
| CPA total | – | 2307 | – | – | – | 86.8 | 2307 |
| IA | – | 36 | – | 81 | 577 | 7.0 | 693 |
| Cryptococcal meningitis | – | – | 5 | – | – | 0.05 | 5 |
| Pneumocystis pneumonia | – | – | 55 | – | – | 0.55 | 55 |
| Mucormycosis | – | – | – | 20 | – | 0.2 | 20 |
| Fungal keratitis | unk | – | – | ? | – | 0.12 | 12 |
| Allergic fungal sinusitis | 50,000 | – | – | – | – | 50 | 50,000 |
| Estimated total burden | 209,489 | 14,351 | 1447 | 101 | 1151 | – | 225,974 |
Population at risk without underlying condition.
ABPA, allergic bronchopulmonary aspergillosis; AIDS, acquired immune deficiency syndrome; CPA, chronic pulmonary aspergillosis; HIV, human immune deficiency virus; IA, invasive aspergillosis; ICU, intensive care unit; SAFS, severe asthma with fungal sensitization; RVVC, recurrent vulvovaginal candidiasis; unk, unknown.
We used data provided by Republican Centre for Combating AIDS in Azerbaijan for the number of patients with HIV/AIDS.27 The number of PLHIV in 2018 was 6193 (62 per 100,000 population), among which 71% (4397) received antiretroviral therapy (ARV). The total number of AIDS patients was 1629. Considering 90% and 20% rates of oral and oesophageal candidiasis in patients with CD4 cell count <200 µl−1,28–30 we estimated 808 (8.1 per 100,000 population) and 579 (5.8 per 100,000 population) cases of oral and oesophageal candidiasis respectively. The number of patients with PCP is 55 (0.55 per 100,000 population). Assuming a cryptococcal antigen prevalence of 2.9%,31 we estimated the number of patients with CM to be 5 (0.05 per 100,000 population).
The prevalence of COPD and bronchial asthma were calculated on the basis of research by Aliyeva et al.32 According to their investigation conducted in 933 adults, the prevalence of bronchial asthma and COPD were 2680 and 430 per 100,000 population, respectively. However, the prevalence of “wheezing symptoms” during the study period was 12,340 per 100,000 (973,056) persons and the prevalence of COPD diagnosed and confirmed by spirometry – 3750 per 100,000 persons. It shows that individuals with asthma and COPD do not go to the doctors despite the presence of symptoms, and these values are likely to be underestimated. Taking into account that not all “wheezing symptoms” are due to asthma, we used doctor-diagnosed cases for asthma prevalence estimation and calculated that there were 197,097 (2680 per 100,000) patients with asthma in 2018. Considering a rate of ABPA in asthma patients of 2.5%,19 we estimated that there were 4927 (49.37 per 100,000) patients with ABPA in Azerbaijan. The proportion of severe asthma is thought to be 10%; among these patients, 33% have severe asthma SAFS.20 We calculated the number of patients with SAFS in Azerbaijan in 2018 was 6504 (65.16 per 100,000 population). Assuming prevalence of allergic sinusitis being 10% of the population,33 and the prevalence of allergic fungal sinusitis of 5%,34,35 we estimate approximately 50,000 people (50 per 100,000 population) suffering from allergic fungal rhinosinusitis.
Considering the low sensitivity of doctor-diagnosed COPD diagnosis (0.11) reported by Toren et al.,36 we used spirometry results (3750 per 100,000) by Aliyeva et al. and estimated the number of COPD patients as 295,701.32 The probability of IA in COPD patients varies between 1.3% and 3.9%.11,37 We used the rate of 3.9% determined by Xu et al.11 Taking into account that 5% of COPD patients are admitted to hospital annually,38 we assumed that 577 patients had IA complicating COPD. The 5-year prevalence of cancer was 25,091 and annual incidence of lung cancer was 1380 cases.39 Applying a 2.6% rate of IA in lung cancer patients,21 we estimated 36 cases in this group of patients. The rate of IA in AML patients is 10%40; thus, applying the annual incidence of AML – 379 cases (3.8 per 100,000) – predicts 38 IA cases among patients with hematological malignancies. The number of transplantation operations carried out in Azerbaijan in 2018 was 181 (116 kidney, 30 bone marrow, 23 liver, and 12 corneal transplants). It means that there were 81 IA cases in this group of patients. Thus, we estimated the total annual incidence of IA in Azerbaijan to be 694.
Azerbaijan is among the 18 high-priority countries to fight tuberculosis (TB) in the WHO European Region and among 30 high multidrug-resistant TB (MDR-TB) burden countries in the world.41 CPA develops in 13–23% of PTB.16 The number of new PTB cases and overall TB prevalence were taken from data provided by the Information and Statistics Department of the Health Ministry.42 The total number of TB patients in 2018 was 8684, with an annual incidence 3792; 85% (7380) of all cases were PTB. The number of new PTB cases was 2859. The frequency of post-treatment cavitation was estimated to be 22%. We assumed that the percentage of CPA case development was 22% in patients with pulmonary cavities and 2% in those without cavities. The burden of CPA was estimated assuming a 15% attrition rate, including a resection rate of 6%.16 We therefore estimated the annual incidence of post PTB CPA at 183 cases and the 5-year prevalence at 577. Assuming that TB is the underlying condition for CPA in 33% of cases,43 we estimated the total CPA prevalence as 2307 cases.
Estimation of candidemia was based on low-average rate for European countries (5 per 100,000).44 The number of Candida peritonitis cases was derived from the assumption that 50% of patients with candidemia in ICU have Candida peritonitis,45 and 33% of candidemia cases are observed in ICU.46 Thus, we estimate that the annual incidences of candidemia and Candida peritonitis are 499 and 75 cases, respectively.
Recurrent vulvovaginal candidiasis (rVVC) is defined as having at least four episodes per year. According to research by Foxman et al. rVVC affects about 6% of women between 15 and 50 years.46 Based on data from the Azerbaijan State Statistical Information Service,47 we estimated that the number of women of major risk age (between 15 and 50) is 2,658,156. After applying a rate of 6%, we estimated the number of women with rVVC to be approximately 159,489 (3195.7 per 100,000 women). Hormone replacement in post-menopausal women increases rVVC rates, so our estimate may be an underestimate. There is no epidemiological data on mucormycosis. Considering a rate of 2 per 1,000,000,48 we estimated 20 cases annually. As 95% of fungal keratitis cases are caused by Aspergillus spp., Candida spp., and Fusarium spp., we estimated 12 cases of fungal keratitis using rates of 0.12 per 100,000 population.49
We found no data on dermatophytosis (“tinea capitis”), mycetoma, chromoblastomycosis, histoplasmosis as there are no local data or specific populations at-risk for these conditions.
Discussion
In Azerbaijan, currently the only means of making a diagnosis of fungal disease is microscopy, culture, blood and urine culture and biopsy with histopathology. Sensitization to fungi is diagnosed via skin prick tests or measuring of specific IgE levels as a part of food and respiratory allergy screening. The lack of non-culture diagnostics such as antigen testing for cryptococcal and Aspergillus infections, limits current datasets and experience in the country. This is the primary reason we have adopted a deterministic estimation approach, rather than a series of formal surveillance studies.
The estimated total burden of serious fungal diseases was 225,974 (2.3% of the population) and, in addition, there are skin hair and nail infections, which we have not estimated. Our estimates of mucosal candidiasis are limited to HIV patients (and excludes cancer, corticosteroid, diabetes and age-related age groups) and rVVC in women in their fertile years. While mucosal candidiasis may be regarded as trivial, it is not in the immunocompromized patient, and rVVC is associated with reactive depression, lost days of work, and relationship issues for those affected.
We have estimated a relatively high burden of HIV-associated fungal infection, namely oral and esophageal candidiasis, CM, and PCP.
Rates of respiratory conditions, namely asthma and COPD, are high in Azerbaijan. This may be partially attributed to mountain geography and high rates of smoking – more than 13% of the population are smokers (35.3% of men).50 This leads to higher rates of COPD and probably exacerbates the impact of asthma. The high burden of PTB in Azerbaijan is a reflection of poor access to diagnostic and treatment facilities. This leads to higher rates of PTB complications, namely CPA.
A comparison of fungal infection burden with Eastern European and Middle Asian countries is provided in the Tables 2–4.
Table 2.
Comparison of the burden of fungal infections in Eastern European and Middle Asian countries: estimated number of patients with fungal diseases and rate per 100,000 population.
| Azerbaijan |
Kazakhstan |
Kyrgyzstan |
Russian Federation |
Kazakhstan |
Russian Federation |
Uzbekistan |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | n | Rate | |
| Oesophageal candidiasis | 579 | 5.8 | 1042 | 5.9 | 294 | 4.9 | 490 | 5.5 | 490 | 5.5 | 13,727 | 30.1 | 2066 | 6.7 |
| Oral candidiasis | 808 | 8.1 | 4393 | 24.8 | 787 | 13.1 | 1260 | 14.1 | 1260 | 14.1 | 50,847 | 112 | 4950 | 16 |
| Candidemia | 499 | 5 | 765 | 4.3 | 250 | 4.2 | 371 | 4.2 | 371 | 4.2 | 2278 | 5 | 1825 | 5.9 |
| Candida peritonitis | 75 | 0.75 | 376 | 0.8 | 50 | 0.8 | 74 | 0.8 | 74 | 0.8 | 376 | 0.8 | ||
| RVVC | 159,489 | 3196 | 273,258 | 2985 | 175,949 | 5865 | 168,834 | 3794 | 168,834 | 3794 | 893,579 | 3923 | 513,600 | 3339 |
| ABPA | 4927 | 49.4 | 306 | 1.7 | 2205 | 36.8 | 6008 | 67.5 | 6008 | 67.5 | 28,447 | 62.4 | 879 | 2.9 |
| SAFS | 6504 | 65.2 | 422 | 2.4 | 2911 | 48.5 | 7930 | 89.1 | 7930 | 89.1 | 37,491 | 82.3 | 1147 | 3.7 |
| CPA total | 2307 | 86.8 | 6231 | 35.5 | 3097 | 51.6 | 4161 | 46.8 | 4161 | 46.8 | 10,054 | 22.1 | 1941 | 6.3 |
| IA | 693 | 7.0 | 511 | 2.8 | 292 | 4.9 | 283 | 3.2 | 283 | 3.2 | 1233 | 2.7 | 1521 | 4.8 |
| Cryptococcal meningitis | 5 | 0.05 | 78 | 0.4 | 25 | 0.4 | 41 | 0.5 | 41 | 0.5 | 101 | 0.2 | 65 | 0.2 |
| Pneumocystis pneumonia | 55 | 0.55 | 1956 | 11.1 | 101 | 1.7 | 210 | 2.4 | 210 | 2.4 | 6152 | 13.5 | 1650 | 5.4 |
| Mucormycosis | 20 | 0.2 | 16 | 0.1 | unk | unk | unk | unk | unk | unk | 90 | 0.2 | 27 | 0.1 |
| Fungal keratitis | 12 | 0.12 | unk | unk | unk | unk | unk | unk | unk | unk | unk | unk | unk | unk |
| Allergic fungal sinusitis | 50000 | 50 | unk | unk | unk | unk | unk | unk | unk | unk | unk | unk | unk | unk |
| Total burden | 225,974 | 999,152 | 300,824 | 3,082,907 | 189,662 | 999,152 | 536,978 | |||||||
ABPA, allergic bronchopulmonary aspergillosis; CPA, chronic pulmonary aspergillosis; IA, invasive aspergillosis; RVVC, recurrent vulvovaginal candidiasis; SAFS, severe asthma with fungal sensitization; unk, unknown.
Table 3.
Comparison of the burden of fungal infections in Eastern European and Middle Asian countries: estimated number of patients with fungal diseases.
| Azerbaijan | Kazakhstan | Kyrgyzstan | Russian Federation | Tajikistan | Ukraine | Uzbekistan | |
|---|---|---|---|---|---|---|---|
| Oesophageal candidiasis | 579 | 1042 | 294 | 11,444 | 490 | 13,727 | 2066 |
| Oral candidiasis | 808 | 4393 | 787 | 48,469 | 1260 | 50,847 | 4950 |
| Candidemia | 499 | 765 | 250 | 11,840 | 371 | 2278 | 1825 |
| Candida peritonitis | 75 | 376 | 50 | 74 | 74 | 376 | |
| RVVC | 159,489 | 273,258 | 175,949 | 2, 487, 215 | 168,834 | 893,579 | 513,600 |
| ABPA | 4927 | 306 | 2205 | 175,082 | 6008 | 28,447 | 879 |
| SAFS | 6504 | 422 | 2911 | 231,000 | 7930 | 37,491 | 1147 |
| CPA total | 2307 | 6231 | 3097 | 52,311 | 4161 | 10,054 | 1941 |
| IA | 693 | 511 | 292 | 3238 | 283 | 1233 | 1521 |
| Cryptococcal meningitis | 5 | 78 | 25 | 296 | 41 | 101 | 65 |
| Pneumocystis pneumonia | 55 | 1956 | 101 | 1414 | 210 | 6152 | 1650 |
| Mucormycosis | 20 | 16 | unk | 232 | unk | 90 | 27 |
| Fungal keratitis | 12 | unk | unk | unk | unk | unk | unk |
| Allergic fungal sinusitis | 50,000 | unk | unk | unk | unk | unk | unk |
| Total burden | 225,974 | 300,824 | 189,961 | 3,082,907 | 189,662 | 999,152 | 536,978 |
ABPA, allergic bronchopulmonary aspergillosis; SAFS, severe asthma with fungal sensitization; IA, invasive aspergillosis; CPA, chronic pulmonary aspergillosis; RVVC, recurrent vulvovaginal candidiasis; unk, unknown.
Table 4.
Comparison of the burden of fungal infections in Eastern European and Middle Asian countries: estimated rate of fungal diseases per 100,000 population.
| Azerbaijan | Kazakhstan | Kyrgyzstan | Russian Federation | Tajikistan | Ukraine | Uzbekistan | |
|---|---|---|---|---|---|---|---|
| Oesophageal candidiasis | 5.8 | 5.9 | 4.9 | 8 | 5.5 | 30.1 | 6.7 |
| Oral candidiasis | 8.1 | 24.8 | 13.1 | 33.9 | 14.1 | 112 | 16 |
| Candidemia | 5 | 4.3 | 4.2 | 8.3 | 4.2 | 5 | 5.9 |
| Candida peritonitis | 0.75 | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 | |
| RVVC | 3196 | 2985 | 5865 | 3481 | 3794 | 3923 | 3339 |
| ABPA | 49.4 | 1.7 | 36.8 | 122.5 | 67.5 | 62.4 | 2.9 |
| SAFS | 65.2 | 2.4 | 48.5 | 161.7 | 89.1 | 82.3 | 3.7 |
| CPA total | 86.8 | 35.5 | 51.6 | 126.2 | 46.8 | 22.1 | 6.3 |
| IA | 7.0 | 2.8 | 4.9 | 2.3 | 3.2 | 2.7 | 4.8 |
| Cryptococcal meningitis | 0.05 | 0.4 | 25 | 0.2 | 0.5 | 0.2 | 0.2 |
| Pneumocystis pneumonia | 0.55 | 11.1 | 101 | 1 | 2.4 | 13.5 | 5.4 |
| Mucormycosis | 0.2 | 0.1 | unk | 0.2 | unk | 0.2 | 0.1 |
| Fungal keratitis | 0.12 | unk | unk | unk | unk | unk | unk |
| Allergic fungal sinusitis | 50 | unk | unk | unk | unk | unk | unk |
| Total burden | 225,974 | 300,824 | 185,961 | 3,082,907 | 189,662 | 999,152 | 536,978 |
ABPA, allergic bronchopulmonary aspergillosis; CPA, chronic pulmonary aspergillosis; IA, invasive aspergillosis; RVVC, recurrent vulvovaginal candidiasis; SAFS, severe asthma with fungal sensitization; unk, unknown.
The burden of infections may be underestimated, as there are few epidemiological publications in this topic area from the Caucasus. Military action in 2020 in Azerbaijan highly likely led to an increase of fungal infections due to blast injuries.51,52 However, due to near absence of case reporting, estimation of these infections is not possible. We consider that the coronavirus disease 2019 (COVID-19) pandemic has had impact on fungal infections rate as well. Another issue is the complexity of differential diagnosis between fungal pathologies and underlying conditions related to their similar clinical manifestations. Thus, often a complex of diagnostic investigations should be performed for correct and timely diagnosis. Fungal culture methodology is considered by many as the “gold” standard of diagnosis but has low sensitivity and should be combined with other diagnostic procedures to identify cases. PCR has better sensitivity compared with culture for diagnosing invasive candidiasis and onychomycosis.53,54 Antigen testing, including galactomannan and β-d-glucan are essential for timely diagnostic of many invasive mycoses, which is crucial for improved patient outcomes.55 Recent developments such as high-volume culture of respiratory samples,56 or the use of chromogenic agar to presumptively identify Candida spp.,57–59 are welcome. Matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) identification of fungi is now much improved, with better algorithms for culture age and media to be used.60,61
However, for many infections, either PCR or antigen testing is critical for early diagnostics of invasive infection. One example is example is Aspergillus antigen, which is released during invasive fungal infection. This marker allows early and non-invasive diagnostics of invasive aspergillosis. In ICU patients with medical problems and severe influenza, bronchial samples can be tested for Aspergillus antigen and provide an immediate diagnosis of invasive aspergillosis.62 There is also evidence that galactomannan levels may be used to monitor therapeutic response.63
Another example of a rapid and sensitive test is β-d-glucan, which is a pan-fungal marker found in deep layers of a cell wall and released during infection after phagocytic damage. Since a β-d-glucan assay is highly sensitive, this test has a very high negative predictive value, so negative results allow physicians to exclude invasive fungal infection with a high level of certainty (reducing unnecessary antifungal therapy).64 Combined use of galactomannan and β-d-glucan assays provides best diagnostic value.65
Molecular methods, namely qPCR, have shown good diagnostic value in patients with invasive candidiasis and, especially, in early detection of Pneumocystis pneumonia.53,66 PCR can be used on expectorated sputum as well as bronchoscopy samples.67 PCR can also be used on oropharyngeal and nasopharyngeal swabs, which is very useful in pediatric patients since obtaining sputum or bronchoalveolar lavage (BAL) is challenging in younger children.68
Observation of tissue invasion by filamentous fungi in biopsy/autopsy specimens provides a definitive (proven) diagnosis of invasive fungal infection. When it is impossible to identify fungi by microscopy, confirmation using culture or molecular methods is required. However, culture methods have low reported sensitivity (17%) for detection of fungi in specimens.69 On the other hand, tissue biopsy and histopathological examination is not possible in immunosuppressed patients with low platelet counts. Moreover, patients sometimes refuse invasive procedures. Serological diagnostic methods like galactomannan and β-d-glucan are very helpful in this situation. These tests greatly aid the conduct of local epidemiological investigations, and national reporting of such data and publication would be valuable for guiding antimicrobial policies and empiric choices in the clinical setting. Better recognition of the pervasive problem of fungal infections would help to develop preventive and therapeutic measures and support funding for establishment of mycological reference laboratory in Azerbaijan.
The public health system in Azerbaijan consists of two main structures: The Ministry of Health and The State Agency on Mandatory Health Insurance (started functioning in 2016). The Administration of the Regional Medical Divisions established in 2018 is responsible for supervision in the area of implementation of mandatory health insurance. Mandatory health insurance is implemented as a pilot scheme starting from January 2016 in some regions. Many essential antifungals are not available in Azerbaijan, e.g., conventional and liposomal amphotericin B, flucytosine, and echinocandins are not registered. Although some azoles, namely fluconazole, itraconazole, and voriconazole are registered, only fluconazole is procured by the Ministry of Health while all other antifungal medications have to be paid for by patients.
The limitations of our methodology include the uncertainty around incidence and prevalence estimates, which are often taken from countries remote to the Caucasus. Even the underlying disease statistics, such as asthma prevalence and lung cancer cases, as examples, may not be very accurate due to inaccurate and missing data on underlying conditions. However, the purpose of this research is to understand the scale of the problem in Azerbaijan to inform local and international healthcare authorities and plan appropriate actions to address current situation.
The most imminent need is improvement of diagnostic capabilities. This aim should be achieved via two routes: (a) establishing a reference laboratory; (b) equipping major clinical centres with essential diagnostics assays.
Footnotes
Author contribution statement: This manuscript is submitted with the knowledge and on behalf of the co-authors. All the listed co-authors have made substantial contributions to the manuscript and approved the final version to be published.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: RMH, SSJ, AO, SK, SRV, and EA declare no conflicts of interest related to this work. DWD and family hold Founder shares in F2G Ltd, a University of Manchester spin-out antifungal discovery company. He acts or has recently acted as a consultant to Scynexis, Cidara, Quintiles, Pulmatrix, Pulmocide, Zambon, iCo Therapeutics, Roivant, and Fujifilm. In the last 3 years, he has been paid for talks on behalf of Astellas, Dynamiker, Gilead, Merck, Mylan, and Pfizer. He is a longstanding member of the Infectious Disease Society of America Aspergillosis Guidelines group, the European Society for Clinical Microbiology, Infectious Diseases Aspergillosis Guidelines group, and the British Society for Medical Mycology Standards of Care committee
ORCID iD: Ravil M. Huseynov  https://orcid.org/0000-0002-7381-5740
https://orcid.org/0000-0002-7381-5740
Contributor Information
Ravil M. Huseynov, The Department of Medical Microbiology and Immunology, Azerbaijan Medical University, Mardanov Qardashlari 98, Baku, Azerbaijan.
Samir S. Javadov, The Department of Medical Microbiology and Immunology, Azerbaijan Medical University, Baku, Azerbaijan
Ali Osmanov, Global Action Fund for Fungal Infections, Geneva, Switzerland.
Shahin Khasiyev, The Department of Informatics and Statistics, Ministry of Health of Azerbaijan Republic, Baku, Azerbaijan.
Samira R. Valiyeva, Republican Centre for Combating AIDS, Ministry of Health of Azerbaijan Republic, Baku, Azerbaijan
Esmira Almammadova, Republican Centre for Combating AIDS, Ministry of Health of Azerbaijan Republic, Baku, Azerbaijan.
David W. Denning, Global Action Fund for Fungal Infections, Geneva, Switzerland Faculty of Biology, Medicine and Health, University of Manchester, Manchester Academic Health Science Centre, Manchester, UK; National Aspergillosis Centre, Wythenshawe Hospital, Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, Manchester, UK.
References
- 1.Schmiedel Y, Zimmerli S.Common invasive fungal diseases: an overview of invasive candidiasis, aspergillosis, cryptococcosis, and Pneumocystis pneumonia. Swiss Med Wkly 2016; 146: w14281. [DOI] [PubMed] [Google Scholar]
- 2.Brown GD, Denning DW, Gow NA, et al. Hidden killers: human fungal infections. Sci Transl Med 2012; 4: 165rv13. [DOI] [PubMed] [Google Scholar]
- 3.Dignani MC.Epidemiology of invasive fungal diseases on the basis of autopsy reports. F1000Prime Rep 2014; 6: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winters B, Custer J, Galvagno SM, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Qual Saf 2012; 21: 894. [DOI] [PubMed] [Google Scholar]
- 5.Antinori S, Nebuloni M, Magni C, et al. Trends in the postmortem diagnosis of opportunistic invasive fungal infections in patients with AIDS: a retrospective study of 1,630 autopsies performed between 1984 and 2002. Am J Clin Pathol 2009; 132: 221–227. [DOI] [PubMed] [Google Scholar]
- 6.Webb BJ, Ferraro JP, Rea S, et al. Epidemiology and clinical features of invasive fungal infection in a US health care network. Open Forum Infect Dis 2018; 5: ofy187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kousha M, Tadi R, Soubani AO.Pulmonary aspergillosis: a clinical review. Eur Respir Rev 2011; 20: 156–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suzuki Y, Kume H, Togano T, et al. Epidemiology of visceral mycoses in autopsy cases in Japan: the data from 1989 to 2009 in the annual of Pathological autopsy cases in Japan. Med Mycol 2013; 51: 522–526. [DOI] [PubMed] [Google Scholar]
- 9.Bitar D, Lortholary O, Le Strat Y, et al. Population-based analysis of invasive fungal infections, France, 2001-2010. Emerg Infect Dis 2014; 20: 1149–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schauwvlieghe A, Rijnders BJA, Philips N, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med 2018; 6: 782–792. [DOI] [PubMed] [Google Scholar]
- 11.Xu H, Li L, Huang WJ, et al. Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: a case control study from China. Clin Microbiol Infect 2012; 18: 403–408. [DOI] [PubMed] [Google Scholar]
- 12.Denning DW, Cadranel J, Beigelman-Aubry C, et al. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J 2016; 47: 45–68. [DOI] [PubMed] [Google Scholar]
- 13.Low CY, Rotstein C.Emerging fungal infections in immunocompromised patients. F1000 Med Rep 2011; 3: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Enoch DA, Yang H, Aliyu SH, et al. The changing epidemiology of invasive fungal infections. Methods Mol Biol 2017; 1508: 17–65. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Control of neglected tropical diseases, https://www.who.int/neglected_diseases/diseases/en/ (accessed 22 February 2020).
- 16.Denning DW, Pleuvry A, Cole DC.Global burden of chronic pulmonary aspergillosis as a sequel to pulmonary tuberculosis. Bull World Health Organ 2011; 89: 864–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dykewicz MS, Rodrigues JM, Slavin RG.Allergic fungal rhinosinusitis. J Allergy Clin Immunol 2018; 142: 341–351. [DOI] [PubMed] [Google Scholar]
- 18.Suresh S, Arumugam D, Zacharias G, et al. Prevalence and clinical profile of fungal rhinosinusitis. Allergy Rhinol (Providence) 2016; 7: 115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denning DW, Pleuvry A, Cole DC.Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adults. Med Mycol 2013; 51: 361–370. [DOI] [PubMed] [Google Scholar]
- 20.Denning DW, Pashley C, Hartl D, et al. Fungal allergy in asthma-state of the art and research needs. Clin Transl Allergy 2014; 4: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yan X, Li M, Jiang M, et al. Clinical characteristics of 45 patients with invasive pulmonary aspergillosis: retrospective analysis of 1711 lung cancer cases. Cancer 2009; 115: 5018–5025. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Fungal diseases [Internet], https://www.cdc.gov/fungal/infections/hiv-aids.html (2017, accessed 21 February 2020).
- 23.Lestrade PPA, Meis JF, Melchers WJG, et al. Triazole resistance in Aspergillus fumigatus: recent insights and challenges for patient management. Clin Microbiol Infect 2019; 25: 799–806. [DOI] [PubMed] [Google Scholar]
- 24.Beardsley J, Halliday CL, Chen SCA, et al. Responding to the emergence of antifungal drug resistance: perspectives from the bench and the bedside. Future Microbiol 2018; 13: 1175–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azerbaijan - location map, https://commons.wikimedia.org/wiki/File:Azerbaijan_-_Location_Map_(2013)_-_AZE_-_UNOCHA.svg (accessed 21 February 2020).
- 26.GNI per capita. Atlas method (current US $), https://data.worldbank.org/indicator/NY.GNP.MKTP.PP.CD (accessed 3 January 2021).
- 27.Press release of Republican Center for Combating AIDS on HIV/AIDS problem in Azerbaijan, http://aids.az/az/qics_uzre_epid_veziyyet/azerbaycanda_epid_veziyyet/Press%20reliz%202018/ (2018, accessed 9 November 2019).
- 28.Smith E, Orholm M.Trends and patterns of opportunistic diseases in Danish AIDS patients 1980-1990. Scand J Infect Dis 1990; 22: 665–672. [DOI] [PubMed] [Google Scholar]
- 29.Buchacz K, Baker RK, Palella FJ, Jr, et al. AIDS-defining opportunistic illnesses in US patients, 1994-2007: a cohort study. Aids 2010; 24: 1549–1559. [DOI] [PubMed] [Google Scholar]
- 30.Yang YL, Lo HJ, Hung CC, et al. Effect of prolonged HAART on oral colonization with Candida and candidiasis. BMC Infect Dis 2006; 6: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rajasingham R, Smith RM, Park BJ, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis 2017; 17: 873–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aliyeva G, Akhundova I, Mammadbayov E, et al. Prevalence of bronchial asthma and COPD in Baku. Eur Respir J 2018; 52(Suppl. 62): PA4487. [Google Scholar]
- 33.Pearce N, Aït-Khaled N, Beasley R, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2007; 62: 758–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferguson B, Barnes L, Bernstein J, et al. Geographic variation in allergic fungal rhinosinusitis. Otolaryngol Clin North Am 2000; 33: 441–449. [DOI] [PubMed] [Google Scholar]
- 35.Dall’Igna C, Palombini BC, Anselmi F, et al. Fungal rhinosinusitis in patients with chronic sinusal disease. Braz J Otorhinolaryngol 2005; 71: 712–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Toren K, Murgia N, Olin AC, et al. Validity of physician-diagnosed COPD in relation to spirometric definitions of COPD in a general population aged 50-64 years - the SCAPIS pilot study. Int J Chron Obstruct Pulmon Dis 2017; 12: 2269–2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guinea J, Torres-Narbona M, Gijon P, et al. Pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: incidence, risk factors, and outcome. Clin Microbiol Infect 2010; 16: 870–877. [DOI] [PubMed] [Google Scholar]
- 38.Polatli M, Ben Kheder A, Wali S, et al. Chronic obstructive pulmonary disease and associated healthcare resource consumption in the Middle East and North Africa: the BREATHE study. Respir Med 2012; 106(Suppl. 2): S75–S85. [DOI] [PubMed] [Google Scholar]
- 39.Globocan 2018: Azerbaijan, http://gco.iarc.fr/today/data/factsheets/populations/31-azerbaijan-fact-sheets.pdf (accessed 6 November 2019).
- 40.Chen CY, Sheng WH, Tien FM, et al. Clinical characteristics and treatment outcomes of pulmonary invasive fungal infection among adult patients with hematological malignancy in a medical centre in Taiwan, 2008-2013. J Microbiol Immunol Infect 2018; 53: 106–114. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Tuberculosis, http://www.euro.who.int/en/health-topics/communicable-diseases/tuberculosis/tuberculosis-read-more (accessed 6 November 2019).
- 42.The form#8: “Tuberculosis report” 2018. Information and Statistics Department of Ministry of Health of Azerbaijan Republic, Baku, 2018, https://www.stat.gov.az/menu/4/e-reports/az/12/012.php (accessed 6 November 2019). [Google Scholar]
- 43.Smith NL, Denning DW.Underlying conditions in chronic pulmonary aspergillosis including simple aspergilloma. Eur Respir J 2011; 37: 865–872. [DOI] [PubMed] [Google Scholar]
- 44.Rodriguez-Tudela JL, Alastruey-Izquierdo A, Gago S, et al. Burden of serious fungal infections in Spain. Clin Microbiol Infect 2015; 21: 183–189. [DOI] [PubMed] [Google Scholar]
- 45.Montravers P, Mira JP, Gangneux JP, et al. A multicentre study of antifungal strategies and outcome of Candida spp. peritonitis in intensive-care units. Clin Microbiol Infect 2011; 17: 1061–1067. [DOI] [PubMed] [Google Scholar]
- 46.Foxman B, Muraglia R, Dietz JP, et al. Prevalence of recurrent vulvovaginal candidiasis in 5 European countries and the United States: results from an internet panel survey. J Low Genit Tract Dis 2013; 17: 340–345. [DOI] [PubMed] [Google Scholar]
- 47.Demographic indicators. Azerbaijan statistical information service, https://www.azstat.org/portal/tblInfo/TblInfoList.do#994_001 (accessed 6 November 2019).
- 48.Rees JR, Pinner RW, Hajjeh RA, et al. The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992-1993: results of population-based laboratory active surveillance. Clin Infect Dis 1998; 27: 1138–1147. [PubMed] [Google Scholar]
- 49.Brown L, Leck AK, Gichangi M, et al. The global incidence and diagnosis of fungal keratitis. Lancet Infect Dis 2021; 21: e49–e57. [DOI] [PubMed] [Google Scholar]
- 50.Tobacco control fact sheet - Azerbaijan, http://www.euro.who.int/__data/assets/pdf_file/0009/337428/Tobacco-Control-Fact-Sheet-Azerbaijan.pdf (accessed 27 February 2020).
- 51.Rodriguez C, Weintrob AC, Dunne JR, et al. Clinical relevance of mold culture positivity with and without recurrent wound necrosis following combat-related injuries. J Trauma Acute Care Surg 2014; 77: 769–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fochtmann A, Forstner C, Hagmann M, et al. Predisposing factors for candidemia in patients with major burns. Burns 2015; 41: 326–332. [DOI] [PubMed] [Google Scholar]
- 53.Clancy CJ, Nguyen MH.Diagnosing invasive candidiasis. J Clin Microbiol 2018; 56: e01909–e01917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gupta AK, Mays RR, Versteeg SG, et al. Update on current approaches to diagnosis and treatment of onychomycosis. Expert Rev Anti Infect Ther 2018; 16: 929–938. [DOI] [PubMed] [Google Scholar]
- 55.Lamoth F.Galactomannan and 1,3-β-d-glucan testing for the diagnosis of invasive aspergillosis. J Fungi (Basel) 2016; 2: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vergidis P, Moore C, Rautemaa-Richardson R, et al. High-volume sputum culture for the diagnosis of pulmonary aspergillosis. Open Forum Infect Dis 2017; 4(Suppl. 1): S609. [Google Scholar]
- 57.Vecchione A, Florio W, Celandroni F, et al. Comparative evaluation of six chromogenic media for presumptive yeast identification. J Clin Pathol 2017; 70: 1074–1078. [DOI] [PubMed] [Google Scholar]
- 58.Pravin Charles MV, Kali A, Joseph NM.Performance of chromogenic media for Candida in rapid presumptive identification of Candida species from clinical materials. Pharmacognosy Res 2015; 7(Suppl. 1): S69–S73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leena Sankari S, Mahalakshmi K, Naveen Kumar V. Chromogenic medium versus PCR-RFLP in the speciation of Candida: a comparative study. BMC Res Notes 2019; 12: 681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cassagne C, Normand A-C, L’Ollivier C, et al. Performance of MALDI-TOF MS platforms for fungal identification. Mycoses 2016; 59: 678–690. [DOI] [PubMed] [Google Scholar]
- 61.Bader O.Fungal species identification by MALDI-ToF mass spectrometry. Methods Mol Biol 2017; 1508: 323–337. [DOI] [PubMed] [Google Scholar]
- 62.Meersseman W, Lagrou K, Maertens J, et al. Galactomannan in bronchoalveolar lavage fluid: a tool for diagnosing aspergillosis in intensive care unit patients. Am J Respir Crit Care Med 2008; 177: 27–34. [DOI] [PubMed] [Google Scholar]
- 63.Kovanda L, Desai A, Hope W.Prognostic value of galactomannan: current evidence for monitoring response to antifungal therapy in patients with invasive aspergillosis. J Pharmacokinet Pharmacodyn 2017; 44: 143–151. [DOI] [PubMed] [Google Scholar]
- 64.Rautemaa-Richardson R, Rautemaa V, Al-Wathiqi F, et al. Impact of a diagnostics-driven antifungal stewardship programme in a UK tertiary referral teaching hospital. J Antimicrob Chemother 2018; 73: 3488–3495. [DOI] [PubMed] [Google Scholar]
- 65.Kumar M, Mugunthan M.β-d-Glucan and Aspergillus Galactomannan assays in the diagnosis of invasive fungal infections. Med J Armed Forces India 2019; 75: 357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Song Y, Ren Y, Wang X, et al. Recent advances in the diagnosis of pneumocystis pneumonia. Med Mycol J 2016; 57: E111–E116. [DOI] [PubMed] [Google Scholar]
- 67.Nowaseb V, Gaeb E, Fraczek MG, et al. Frequency of Pneumocystis jirovecii in sputum from HIV and TB patients in Namibia. J Infect Dev Ctries 2014; 8: 349–357. [DOI] [PubMed] [Google Scholar]
- 68.Morrow BM, Samuel CM, Zampoli M, et al. Pneumocystis pneumonia in South African children diagnosed by molecular methods. BMC Res Notes 2014; 7: 26–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barton RC.Laboratory diagnosis of invasive aspergillosis: from diagnosis to prediction of outcome. Scientifica (Cairo) 2013; 2013: 459405. [DOI] [PMC free article] [PubMed] [Google Scholar]