Abstract
A trimalleolar ankle fracture is considered unstable and treatment is generally performed operatively. Computed tomography is important for the operative planning by providing an elaborated view of the posterior malleolus.
Trimalleolar ankle fractures have a rising incidence in the last decade with up to 40 per 100,000 people per year. With a growing number of elderly patients, trimalleolar ankle injuries will become more relevant in the form of fragility fractures, posing a particular challenge for trauma surgeons.
In patients with osteoporotic trimalleolar ankle fractures and relevant concomitant conditions, further evidence is awaited to specify indications for open reduction and internal fixation or primary transfixation of the ankle joint.
In younger, more demanding patients, arthroscopic-assisted surgery might improve the outcome, but future research is required to identify patients who will benefit from assisted surgical care.
This review considers current scientific findings regarding all three malleoli to understand the complexity of trimalleolar ankle injuries and provide the reader with an overview of treatment strategies and research, as well as future perspectives.
Cite this article: EFORT Open Rev 2021;6:692-703. DOI: 10.1302/2058-5241.6.200138
Keywords: ankle joint, fibula, fracture fixation, tibia, trimalleolar ankle fractures
Anatomy
The human ankle joint complex can be divided in a talocrural, a talocalcaneonavicular and a subtalar part.1 The talocrural (TC) joint is formed by three bones and a complex ligamentous apparatus. Tibia, fibula and talus are interconnected through collateral ligaments and the syndesmotic ligament complex.2,3
From the tibia, the facies articularis medialis (pilon) and the facies articularis inferior are connected to the talus. Looking at the coronal plane, the tibia shows a slight slope from medial to lateral and is concave-shaped in the sagittal plane (Fig. 1B). Considering the bone mineral density of the tibia, the articular site shows a higher density in comparison to the metaphysis.4–6 Besides the connection between tibia and talus, there exists a close interaction between tibia and fibula. The concave-shaped incisura tibialis matches the convex shape of the fibula (Fig. 1C). The incisura tibialis is formed by the anterior (Chaput’s tubercle) and posterior tubercle of the tibia (Fig. 1C). Likewise, the anterior (Le Fort-Wagstaffe tubercle) and posterior tubercle of the fibula form a convex triangle. The contact zone between tibia and fibula is covered by a thin layer of cartilage forming the syndesmotic recess.7
Fig. 1.
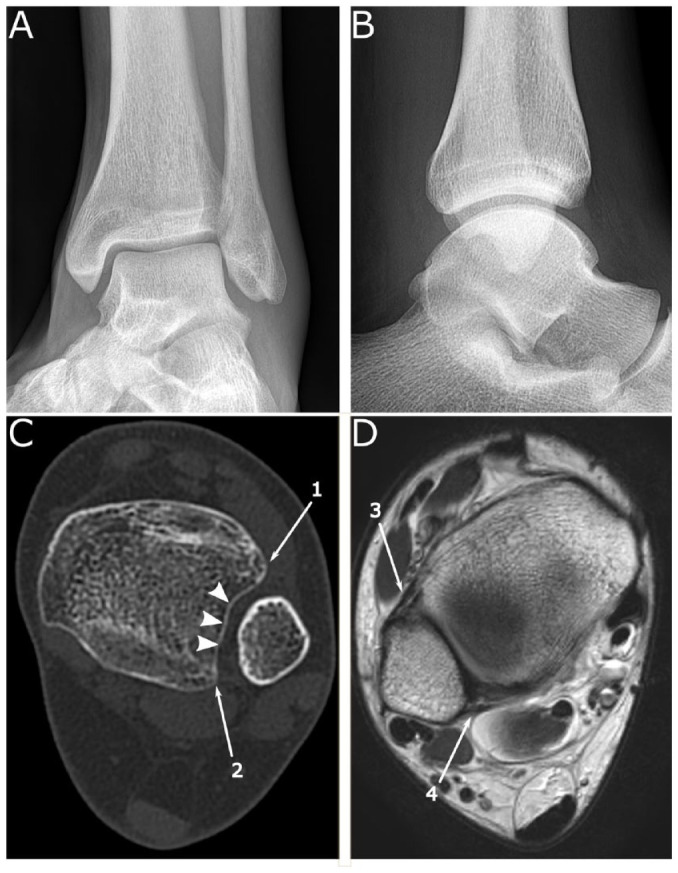
(A) Ankle anteroposterior (AP) mortise view of a healthy young male showing the configuration between distal tibia, distal fibula and talus. Regarding the length of the fibula, the articular portion reaches further in distal direction in comparison to the medial malleolus. (B) Lateral radiograph of the ankle of the same patient of (A). The tibia is concave-shaped in the sagittal plane and the arc length of the talus with around 120° is greater in comparison to the tibia with its 80°. (C) Axial computerized tomography (CT) image at the level of the distal tibiofibular. The concave-shaped incisura tibialis (filled arrowhead) matches the convex shape of the fibula. The incisura tibialis is formed by the anterior (Chaput’s tubercle) (1) and posterior tubercle (2) of the tibia. (D) Oblique magnetic resonance image at the level of the tibiotalar joint with distal anterior tibiofibular ligament (ATIFL) (3) and the distal posterior tibiofibular ligament (PTIFL) (4).
Furthermore, the fibula is connected with the corresponding articular surface of the talus.8 Due to the length of the fibula, the articular portion reaches further in distal direction in comparison to the medial malleolus.2 Via the syndesmotic complex, the fibula is dynamically fixed to the tibia (Fig. 1 D).9
Over half of the surface of the talus is covered with cartilage without any tendon insertions.10 The shape of the talus is complex, resulting in a changing axis of rotation.11 Looking from above at the trochlea tali, it is wedge-shaped with a broader anterior portion.3 On the medial side, the articulation between talus and malleolus shows a larger contact surface.5,12 In the sagittal plane, there also exists an incongruity between the articular surface of the talus and the distal tibia. The convex-shaped talus has a greater articular surface than the corresponding concave-shaped facies articularis inferior of the tibia (Fig. 1B).13
In the frontal plane, the trochlea of the talus shows a lateral slope of about nine degrees.12 The surface of the talus forms an arched deepening from ventral to dorsal direction, ensuring a rotational stability in dorsoplantar movements.3,12
The ligamentous apparatus of the TC joint can be differentiated into the lateral (LCL), the medial (MCL) and the tibiofibular ligament complex. Among the ligamentous structures of the syndesmosis are the distal anterior tibiofibular ligament (ATIFL), the distal posterior tibiofibular ligament (PTIFL), the transverse ligament and the interosseous ligament (Fig. 1D). Proximal to that, the interosseus membrane forms also part of the tibiofibular complex.7 All of these structures stabilize the ankle mortise and at the same time allow movements of the fibula in relation to the tibia.14 The ATIFL is trapezoidal-shaped and extends from the Chaput tubercle to the Wagstaff tubercle.15 In the literature, an accessory ligament, called Bassett’s ligament, running inferior and parallel to the ATIFL is described.16 Between the fascicles of the ATIFL lie perforating branches of the peroneal artery.14 In comparison to the interosseous ligament, the ATIFL is weaker, contributing to the fact that the ATIFL can be ruptured, but the interosseus ligament with the osseous membrane remains intact.17 The interosseus ligament is the distal continuation of the osseous membrane and is pyramid-shaped.18 The PTIFL is a strong ligament running from the posterior tibia in distal-lateral direction to the posterior tubercle of the fibula.7 It can be differentiated into a superficial and a deep part, also called the transverse ligament. The transverse ligament runs more horizontally and forms a labrum analogue.7 A frequent anatomic variation is the intermalleolar ligament between PTIFL and transverse ligament.19,20
The LCL complex consists of the anterior talofibular (ATFL), the calcaneofibular (CFL), and the posterior talofibular (PTFL) ligaments. The ATFL typically shows a double-banded morphology and is separated by vascular branches.14,21 It is almost horizontally located to the ankle in neutral position and depending on the position of the foot, one band tightens while the other relaxes.14 Due to its characteristics, it limits anterior displacement of the talus and plantar flexion of the ankle.22 The CFL originates below the ATFL at the fibula and inserts at the posterior region of the lateral surface of the calcaneus.14 Its fibres run obliquely backwards/downwards and the CFL is located directly underneath the peroneal tendons. It is the only ligament of the LCL complex that bridges the TC and subtalar joint.14 The PTFL runs almost horizontally from the fibula to the posterior process of the talus. Single fibres can reinforce the intermalleolar ligament. In neutral position, the PTFL is relaxed and tightens in dorsiflexion.14
The MCL complex (deltoid ligament) consists of a superficial and deep layer. It is a fan-shaped complex reaching from the medial malleolus to the talus, calcaneus and navicular bone, bridging the TC and subtalar joint.23 The sheaths of the tibialis posterior and flexor hallucis tendons pass above the MCL complex.14
The ankle joint is not solely a hinge joint around a constant axis, but rather allows combined rotatory and hinge movements. The axis of rotation changes depending on the degree of dorsiflexion/plantarflexion, leading to a complex movement of the talus in sagittal, coronal and frontal plane.24,25 Due to the interactions between tibia and fibula, the subtalar joint and the Chopart joint, the dorsiflexion leads to an internal rotation, valgization of the rear foot and pronation of the forefoot, whereas in plantarflexion, it comes to an external rotation, varization of the rear foot and supination of the forefoot.2,11,25,26 The normal range of motion in the sagittal plane is 13–33° of dorsiflexion and 23–56° of plantarflexion. Motions in the transverse (internal/external rotation) and coronal plane (varus/valgus) are coupled with motions in the sagittal plane.24
Epidemiology
Ankle fractures are common and account for up to 10% of all bone injuries with a rising incidence over the last decades.27,28 According to a nationwide population study in Sweden, closed bi- or trimalleolar fractures had an annual incidence rate of 33 per 100,000 person-years and 20 to 40 per 100,000 persons-years in Denmark.28,29 Interestingly, the peak incidence of trimalleolar fractures is in the age from 60 to 69 years, becoming the second most common ankle fracture type in this age group.28 Elderly women are especially at risk, since women over 60 years with bi- or trimalleolar fracture have the highest incidence of open ankle fractures.29 Due to the predominance in elderly women, some authors claim that trimalleolar fractures should be regarded as fragility fractures.28 There also exists a seasonal variation with increased incidences for ankle fractures during cold winters.28
Different mechanisms, ranging from low to high-energy trauma, can lead to complex ankle fractures with falls from standing heights in combination with ankle distortion presenting the most common cause.28,29 Especially in women over 60 years, falls from a standing position account for over two-thirds of all cases.29 Trimalleolar ankle fractures are typically the result of a low-energy trauma.30
Classification
A trimalleolar ankle fracture typically involves the distal fibula (lateral malleolus), medial and posterior malleolus. The first ankle fracture classification system developed by Percival Pott differentiated between uni-, bi- and trimalleolar ankle fractures.31 Despite the reproducibility, the classification system lacks the distinction between stable and unstable fractures.32,33 Lauge-Hansen developed a classification system for ankle fractures based on the mechanism of injury.34 It describes the position of the foot at the time of trauma and the direction of the deforming force.35 Depending on the severity of the ankle injury, different stages (I-IV) can be distinguished. Providing further information about the stability of the injury, the Lauge-Hansen classification had become a widely used classification system for ankle injuries.32 According to the Lauge-Hansen classification, a trimalleolar fracture of the ankle can either be classified as SE IV or PE IV. But the Lauge-Hansen classification system has been challenged due to a poor reproducibility and low inter- and intraobserver reliability.36–39
One of the most commonly used classifications for ankle fractures is the Weber classification, which differentiates fibular fractures relevant to the tibiofibular syndesmosis.40 Despite the fact that the Weber classification system has a high inter- and intraobserver reliability, it is inadequate for multimalleolar fractures.41,42
Biomechanical and clinical research led to the development of classification systems of the medial and posterior malleolus. Medial malleolar fractures can be classified according to Herscovici et al, who differentiate between four types (A–D) of fractures based on the anteroposterior radiograph.43 It is the current standard system regarding the medial malleolus, but inadequate for multimalleolar fractures.44 Indication for operative treatment of medial malleolus fractures rather depends on the degree of displacement and whether it is part of an unstable ankle fracture.44
The posterior malleolus can be classified according to Haraguchi, Bartoníček or Mason. The former developed a computerized tomography (CT)-based classification system for posterior malleolus fractures depending on transverse CT sections.45 Mason et al modified the Haraguchi classification indicating the severity and pathomechanism of the fracture.46 Bartoníček et al postulated a more specific CT-based classification system that also takes the stability of the tibiotalar joint and the integrity of the fibular notch into consideration.47 These classification systems of the posterior malleolus can guide further operative or non-operative treatment, but fail to fully characterize the kind of trimalleolar fracture.
The AO/OTA classification distinguishes between Type A (infra-syndesmotic), B (trans-syndesmotic) and C (supra-syndesmotic) fibular fractures.48 Furthermore, AO/OTA Type B2.3 or B3.3 fractures are trans-syndesmotic fibular fractures with a fracture of the posterolateral rim and medial malleolus. The same applies for AO/OTA type C1.3 and C2.3 fractures involving all three malleoli. Additional qualifications can be added to specify the stability of the syndesmosis or concomitant injuries (e.g. Le Fort-Wagstaffe tubercle). The AO/OTA classification lacks a description of the fracture configuration of the medial and posterior malleolus. This is noteworthy, since the size of the posterior fragment and displacement are factors to consider for the choice of treatment.49
Ideally, a classification system should have a high inter-/intraobeserver reliability, be widely recognized, relevant for prognosis and applicatory in research and clinic. The most comprehensive classification system is the AO/OTA classification. It is widely recognized, easy to use in clinical practice and provides information about the kind of trimalleolar fracture with focus on the fibula. However, an important factor, the configuration of the posterior malleolus fragment, is not represented in the AO/OTA classification.
Non-operative treatment
In general, it is accepted that trimalleolar fractures are treated operatively.50,51 But in selected groups, where satisfactory initial closed reduction is possible, a conservative treatment can lead to a comparable outcome.52 A randomized controlled trial comparing close contact casting with surgery of unstable ankle fractures among 620 older adults found satisfactory results following conservative treatment.53 Even after three years of non-operative treatment, the equivalence in function between both groups remained.54 The conservative therapy consisted of a close contact cast below the knee applied under anaesthesia, non-weight-bearing for four weeks and full weight-bearing by week six to eight. Regular radiographs were conducted to monitor joint congruency.53 Nineteen percent of patients needed conversion to internal fixation due to a loss of fracture reduction, and the non-operative group had a six times higher probability of a radiologic malunion.53 Unfortunately, the type of malleolar fracture was only described as relevant to the syndesmosis and not classified according to one of the common classification systems. Due to that fact and the exclusion criteria of the study, the results should be interpreted with caution and cannot simply be transferred to the management of trimalleolar ankle fractures.
In contrast, a prospective randomized study of 43 patients with displaced ankle fractures in patients aged over 55 years showed an inferior outcome for non-operative treatment.55 Thirty-eight percent of the conservative group showed a loss of reduction and a limited range of motion in comparison to the open reduction and internal fixation (ORIF) group at follow-up.55
A retrospective study of 19 patients with non-operatively treated displaced bimalleolar and trimalleolar fractures reported an excellent functional outcome after 20 years.56 However, it is not feasible to draw reliable conclusions for the treatment of trimalleolar fractures, because only four patients with a trimalleolar fracture were available for final clinical and radiological evaluation.
The current literature strongly advocates the operative treatment of ankle fractures involving the posterior malleolus. In their critical review, Rammelt and Bartoníček analysed the importance of the posterior malleolus with conclusive data supporting the direct open reduction and fixation of posterior malleolar fragments.57 Vacas-Sánchez et al proposed a CT-based algorithm for fixation of the posterior malleolus and Wang et al showed good functional outcomes following operative treatment of the posterior malleolus.58,59
Operative treatment
Timing to surgery
Depending on the fracture configuration, the management and timing to definite surgery can differ significantly. Dislocated trimalleolar ankle fractures should be reduced immediately, re-establishing joint congruity and reducing concomitant soft tissue injury.60 If closed reduction is unsatisfactory, an immediate open reduction should be achieved. Furthermore, emergency indications for an operative treatment are:
severe soft tissue injury,
compartment syndrome,
open fracture with/without concomitant vascular or nerve injury.60–62
Despite the emergency operative treatment, there is a controversy about the optimal timing of surgery of closed trimalleolar ankle fractures. It spans from the period of a few hours up to several days of delay in order to minimize soft tissue swelling.63 A retrospective cohort study in Norway with 1011 patients showed no difference regarding postoperative length of stay, complications, and functional outcomes in patients with closed ankle fractures treated with ORIF during the first 8h, 8h to 6 days and > 6 days.64 Other studies are in line with these findings, reporting no difference regarding postoperative wound infections between early and delayed surgery groups.65–67 In contrast, a case series of Schepers et al found a significant difference regarding wound complications between patients treated within one day and with delay.68 They also performed a literature review including six studies showing a significant increase of wound complications when surgery was delayed.63,66,68-73 Considering the published studies, their heterogeneity and partially low quality, there is no definite recommendation for the optimal timing of the operative treatment of closed ankle fractures (Table 1). In clinical practice, the evaluation of soft tissue status is still an important piece of information and can lead to a delayed surgery in case of excess soft tissue swelling.66 Latest studies showed no difference regarding different time categories and further studies are necessary to determine the best timing of surgery. In clinical practice, the time of surgery also depends on staff and operating capacities so that definite operative treatment is neither feasible nor successful in many cases.
Table 1.
Overview timing to surgery of closed ankle fractures
| Author | Journal/Year | Timing to surgery |
|---|---|---|
| Naumann64 | Injury 2017 | Up to 6 days |
| Breederveld65 | Injury 1988 | 5 to 8 days |
| Singh66 | Journal of Orthopaedic Surgery 2015 | Within 24 hours |
| Schepers68 | International Orthopaedics 2013 | Within 24 hours |
| Saithna63 | European Journal of Orthopaedic Surgery & Traumatology 2009 | Up to 6 days |
| Carragee69 | The Journal of Bone and Joint Surgery [Br] 1991 | Up to 4 days |
| Carragee70 | The Journal of Trauma 1993 | Within 24 hours |
| Høiness71 | Annales Chirurgiae et Gynaecologiae 2000 | Within 8 hours |
| Adamson72 | Injury Extra 2009 | Within 24 hours |
| Sukeik73 | Orthopaedic Proceedings 2011 | Within 24 hours |
Surgical technique
For choosing the optimal surgical treatment and implants, there are some important factors to be considered:
Soft tissue injury
Bone mineral density (non-osteoporotic vs. osteoporotic)
Fracture configuration
Functional demand of the patients
Trimalleolar ankle fractures with severe soft tissue injury or open fractures pose a particular challenge. The incidence of open ankle fractures is about 3%, but is expected to increase especially in older patients.29,74,75 An open ankle fracture is an independent risk factor for wound complications and thus for a poorer outcome.76 Concomitant conditions such as diabetes, smoking or vascular diseases increase postoperative wound complications and can lead to an amputation below the knee.77–80 In these selected cases with severe soft tissue injury and relevant concomitant injuries, an external fixation might be a viable option for fracture treatment.81
The management of osteoporotic ankle fractures is challenging and internal fixation is associated with an increased risk of sepsis, nonunion, malunion and delayed wound healing.82–84 In elderly patients, tibio-talo-calcaneal (TTC) nailing is an alternative surgical treatment option.85–87 A prospective randomized control trial by Georgiannos et al showed that elderly patients following tibio-talo-calcaneal nailing had fewer postoperative complications in comparison to open reduction and internal fixation.85 The mean age of patients treated with TTC ranged from 77 to 82 years with an Olerud and Molander ankle score of < 60, representing an elderly low-demanding patient population.85–87 The peak incidence of trimalleolar fractures is in the age from 60 to 69 years and thus primary ankle transfixation with TTC does not present the optimal operative treatment in these cases. In the following, the surgical options to anatomically restore the ankle joint function in trimalleolar ankle fractures will be outlined.
Lateral malleolus
The standard approach is a lateral incision above the distal fibula. In the classical AO technique, open anatomical reduction is secured, fixed with a lag screw and a lateral neutralization plate (e.g. one-third tubular plate).40,60 Today, this technique and implants are commonly used in daily routine.88
In elderly patients with reduced bone mineral density, lateral locking plates can be advantageous in comparison to traditional compression plating when soft tissue coverage is sufficient.89 Biomechanical studies showed that locking plates provide a higher construct stability in specimens with reduced bone mineral density.90,91 In trimalleolar ankle fractures with normal bone mineral density, fibular locking plates do not show a mechanical advantage.92 But the use of locking compression plates results in a better clinical and radiological outcome in comparison to standard one-third tubular plates.93 The level and extent of fibular injury needs to be considered when choosing the adequate plating system. Disadvantages of locking plates are that they provide minimal compression across the fracture (without lag screw), higher costs and ‘thicker’ plate size, causing a possibly higher wound complication rate.89,94,95 But in a randomized control trial comparing locking and non-locking neutralization plates, there was no difference regarding the complication rates.96 Minimally invasive locking plate osteosynthesis of distal fibular fractures may be a viable option in critical soft tissue conditions.97 Therefore, a smaller incision is made at the distal end of the fibula and the locking plate is inserted from the distal side in a proximal direction using a locking drill sleeve.97 Furthermore, a locking plate system allows to safely fix distal fragments with small fragment locking screws in distal fibular fractures.89
Beside the standard lateral plating, posterolateral antiglide plate fixation is an alternative. Biomechanical studies showed an improved construct stability in comparison to lateral locking plates in osteoporotic bone.98 Posterolateral and posterior antiglide plate fixation led to satisfactory clinical and radiological outcome comparable to lateral plating.99–101 A significant complication of posterolateral plating is a peroneal tendon lesion, that can lead to high rates of hardware removal.102 But the more currently conducted studies report a low complication rate, including minimal presence of peroneal lesions.99,103 The antiglide plate can be inserted via a lateral or posterolateral approach, depending on the fracture configuration. A posterolateral approach is used in case of a concomitant fracture of the posterior malleolus requiring open reduction and internal fixation.100,104 The distal fibula is openly reduced and fixed from the posterior side with a neutralizing one-third tubular plate with or without lag screw.100
In contrast to open surgical fixation of distal fibular fractures, a percutaneous method was developed to minimize soft tissue stress while providing a reliable fixation method. Biomechanically, an intramedullary fibular nail provides a robust construct stability with a greater torque-to-failure compared to standard plating.105 A prospective randomized control study in elderly patients showed a lower wound infection rate of fibular nailing in comparison to standard ORIF and a superior cost-effectiveness.95 Especially in high risk patients, fibular nailing seems to be a safe treatment choice with a low infection complication rate.106 A review of 1008 patients treated with intramedullary fixation of distal fibular fractures states excellent clinical and functional outcomes.107 Due to the closed reduction and mini-incision technique at the distal tip of the fibula, comminuted fractures pose a difficulty, whereas intramedullary nailing can be impossible and conversion to plate fixation is mandatory.108 There are some technical difficulties that need to be taken into consideration. The distal fibular entry point is crucial, the base of the nail should be left flush with the cortex at the tip of the fibula, one distal locking screw is sufficient and the careful placement of one or two proximal locking screws is essential.109 Modern fibular nail implants provide several options for distal locking screws.110
Posterior malleolus
The indications for fixation of the posterior malleolus are disputed.111–114 A review about the long-term outcome of 866 posterior malleolar fractures reported comparable results of operatively and non-operatively treated patients.112 If a stable ankle mortise can be achieved through medial and lateral fixation and there is no joint impaction or a large intercalated fragment, patients may not benefit from posterior plating considering the additional risks.114
For a long time, the extent and displacement of the posterior malleolus fragment was decisive for indication to surgery. A fragment displacement of more than 2 mm or the involvement of one-quarter to one-third of the articular surface on the lateral radiograph were critical indications for operative treatment.115–118 CT-based classifications of the posterior malleolus were developed, since the interpretation of plain radiographs poorly assess the posterior fragment size and configuration.47,119,120 The proposed classification by Bartoníček and Rammelt may be used as a guide for decision making, but important factors have to be considered. Operative treatment aims to re-establish posterior stability while restoring the size and articular surface of the tibial pilon, the stabilizing function of the posterior tibiofibular ligament and the integrity of the fibular notch.121 The quality of reduction and joint congruity are significant factors influencing prognosis.122 To achieve these goals, there are different operative strategies depending on the fragment configuration and concomitant injuries. Open reduction and internal fixation can be performed direct or indirect.121,123 Indirect methods involve anterior to posterior (AP) screw fixation and transfibular reduction with AP screws.123
AP screws are indicated in non-displaced single, large fragments of the posterior malleolus without intercalary fragment (Bartoníček and Rammelt Type 4).121 The posterior malleolus is reduced by ligamentotaxis and secured with a pointed reduction clamp between the anterior and posterior tibial tubercles. Following radiographic confirmation and ideally direct visualization of the reduction, the fragment is fixed with anterior to posterior screws.57 Biomechanical and clinical studies showed that AP screw fixation seems to be inferior compared to buttress/posterolateral plating.115,116,124 This is a fact the surgeon has to consider before choosing the fixation method, but also weighing the contributed risks of the different approaches.
Direct reduction of the posterior malleolus can be achieved via a posteromedial or posterolateral approach. The posterolateral approach is indicated in posterior malleolus fractures with relatively small diameter (Bartoníček and Rammelt Type 2 & 4) and the presence of intercalary fragments.121 According to the Mason classification, Mason Type 2 and 3 posterior malleolar fractures are treated with a posterolateral approach and only Type 1 fractures with trans-syndesmotic fixation.125 The posterolateral approaches allow open reduction and internal fixation of the posterior malleolus as well as the treatment of distal fibular fractures.99 Open reduction and internal fixation of the posterior malleolus can be performed with posterior screw or plate fixation depending on the fracture configuration and bone quality.121 There is no uniform recommendation for when to use screws, e.g. 3.5 mm lag screws, one-third tubular plates or locking plates. In osteoporotic bone, a locking plate fixation might be advantageous.126 Important structures that are at risk are the sural nerve, peroneal tendons and the flexor hallucis longus muscle.121,127 In a cadaveric study, lesions to the tibialis anterior tendon were seen through posterior to anterior K-wires.128 The posterolateral approach offers advantages over indirect fixation methods involving direct visualization and reduction as well as the possibility to remove small osteochondral fragments.121 Clinical studies showed a better outcome of direct posterior in comparison to indirect reduction with comparable complication rates.129–132 In comparison to the indirect fixation method, the posterolateral approach is currently endorsed, but large randomized control trials are needed to prove its superiority.
The posteromedial approach is useful in posterior malleolus fractures with a posteromedial fragment involving the medial malleolus (Bartoníček and Rammelt Type 3).104,121 It can also be combined with a posterolateral approach to treat trimalleolar fractures with the involvement of the entire posterior plafond.133,134 Similar to the posterolateral approach, open fracture reduction of the posterior and medial malleolus can be secured with screws and/or plates.135 Structures at special risk are the tibialis posterior tendon, flexor digitorum longus muscle and the neurovascular bundle.121 If an appropriate reduction can be achieved, the outcome is satisfactory with low complication rates.104,133,135 But the studies included only small patient numbers and long-term outcomes are missing.
In trimalleolar ankle fractures, the trend goes towards directly fixing the posterior malleolus fragment since it leads to a superior quality of reduction and better clinical outcome.131,132,136 Direct fixation can prevent syndesmotic diastasis and thus contributes to prompt rehabilitation.113,137 In a current study, Yang et al propose that in cases without fixation of the posterior malleolus, the syndesmotic screw should be removed three months postoperatively since early removal led to a higher rate of syndesmotic diastasis.137 Open reduction and internal fixation of the posterior fragment restores the integrity of the posterior portion of the syndesmosis and thereby reduces the need for trans-syndesmotic fixation.57,131,136,138,139 But if the intraoperative testing after fracture fixation shows a syndesmotic instability, an additional trans-syndesmotic fixation is necessary. Trans-syndesmotic fixation can be achieved through dynamic or static fixation. A meta-analysis of 11 cadaveric studies showed that a dynamic fixation system (suture button) provides less rigidity in comparison to metal screws.140 Looking at the clinical and radiological outcome, the dynamic fixation for acute syndesmotic injuries is superior compared to static screw fixation.141–144 But these studies included mainly syndesmotic injuries with or without a unilateral malleolar fracture.141–144 Thus, these results cannot simply be transferred to the treatment of trimalleolar ankle fractures and future studies need to prove superiority of dynamic stabilization devices.
Medial malleolus
Traditionally, open reduction and internal fixation of medial malleolus fractures is indicated in trimalleolar ankle fractures.44 Considering the age distribution and peak incidence of trimalleolar ankle fractures, fixation of the medial malleolus may provide an additional stability in these osteoporotic bones.50 But Hoelsbrekken et al showed that non-operative management of minimally displaced medial malleolus fractures after fracture reduction in bi- or trimalleolar ankle fractures results in equivalent outcomes.145 A prospective randomized controlled trial regarding the management of medial malleolus fractures in unstable ankle fractures is awaited, hopefully providing further Level I evidence.146
Operative management includes open and percutaneous techniques with tension-band wiring, plate and/or screw fixation. Open surgical approaches are the anteromedial and direct medial approach. Advantages are the direct visualization of the fracture, inspection of the articular surface and possibility to retrieve interposing reduction obstacles.44 Due to the extensile approach, soft tissue is more likely compromised and the great saphenous vein and nerve are at special risk when performing an anteromedial approach.44 This has led to the development of minimally invasive and solely percutaneous techniques. With a minimally invasive approach, the articular surface can be inspected via a mini-arthrotomy, fracture reduction visualized and fixation performed through percutaneous screw fixation.147 Advantages are the reduced soft tissue stripping, but especially purely percutaneous screw fixation can compromise bone union due to interposing periosteal flaps.148 The choice of implant depends on fracture configuration, bone quality and soft tissue injury. Screws are the most frequently used implant and are indicated in oblique fractures of the medial malleolus.149 Following the traditional AO technique, two parallel partially threaded cancellous lag screws are inserted – preferably into the anterior colliculus.44 This classic approach is challenged by a randomized control trial by Buckley et al, who compared double to single-screw fixation and found comparable results.150 In osteoporotic bone, fully threaded screws or even bicortical fixation can provide more compression and lower rates of radiological loosening.151,152
In cases of distal avulsions (Herscovici type B) or severe comminution, stainless steel tension-band wiring (TBW) constructs are superior in comparison to screws.153 Also, in transverse fractures of the medial malleolus (Herscovici type C), TBW seems to be advantageous.149 The disadvantage of TBW is the frequently observed wire migration in up to one fifth of patients and prominent metalwork causing medial pain and implant removal.154,155 Due to these associated complications, new low-profile knotless systems were developed that still need to prove their reliability.156
In vertical fractures (Herscovici type D) of the medial malleolus, antiglide plating provides a biomechanical superior fixation compared to screws.157 Due to a higher load to failure and increased compression of the fracture, antiglide plating should be used with additional lag screws.44 The disadvantage of plate fixation is a larger exposure, as compared to screws requiring good soft tissue conditions.
New implants, such as headless or bioabsorbable screws were developed to reduce medial site pain and supersede implant removal, but prospective studies with a high scientific quality are missing to justify routine clinical use.44
Arthroscopic-assisted open reduction and internal fixation (AORIF)
In recent years, there has been a growing number of studies regarding arthroscopic-assisted open reduction and internal fixation (AORIF) in acute ankle fractures.158–160 A review analysing the long-term outcome after 1822 operatively treated ankle fractures showed that only 79.2% of the optimally reduced fractures showed a good to excellent long-term outcome.51 Due to the arthroscopic findings in acute ankle fractures, the unsatisfactory results in optimally reduced fractures are attributed to traumatic chondral lesions.161–164 But the majority of studies performing AORIF included isolated malleolar fractures 158. Only one study compared ORIF and AORIF in bimalleolar or trimalleolar ankle fractures.158,160 Baumbach et al showed that patients with bimalleolar or trimalleolar ankle fractures following AORIF in comparison to ORIF had a significantly better outcome regarding the functional score four years after surgery.160 The median age of the included patients undergoing AORIF was 46 years, representing a younger and higher-demand patient population, in which arthroscopic-assisted ankle surgery is typically performed.158,160 Due to the fact that there only exists one comparative study regarding AORIF in trimalleolar ankle fractures, further studies providing Level I evidence for indications of arthroscopic-assisted surgery in trimalleolar ankle fractures are awaited.
Perspective
In the authors’ opinion, future research regarding trimalleolar ankle fractures will need to focus on two different patient populations and their distinct characteristics to derive appropriate treatment protocols. On the one side, there is a growing number of elderly patients with osteoporotic fractures and relevant concomitant conditions in which internal fixation to restore anatomical ankle joint congruity poses a particular challenge. Future studies need to provide further evidence to specify indications for open reduction and internal fixation or primary transfixation of the ankle joint in these elderly patients. On the other side, the current trend towards direct fixation of the posterior malleolus needs to prove superiority regarding the long-term outcome in comparison to indirect surgical techniques in trimalleolar ankle fractures. In younger, higher-demanding patients, arthroscopic-assisted open reduction and internal fixation might improve the outcome, but studies are needed to identify patients who will benefit from assisted surgical care.
Conclusion
Trimalleolar ankle fractures are unstable and their treatment is generally facilitated operatively. Computed tomography is essential for classification and operative planning. The posterior malleolus gained in importance in the last few years and current clinical evidence is endorsing direct open reduction and internal fixation to provide a stable and accurate reduction. Incidence of trimalleolar fractures peaks in higher age groups and is becoming more relevant in fracture care in the future due to the demographic development. Elderly patients with osteoporotic trimalleolar ankle fractures and concomitant conditions pose a particular challenge and further evidence is needed regarding the optimal surgical treatment.
Acknowledgments
The authors would like to thank Fritz Seidl, M.A. Interpreting and Translating, for proof-reading and language-editing the manuscript.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthop Trauma 2016;30:232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knupp M, Valderrabano V, Hintermann B. Anatomische und biomechanische uberlegungen zur sprunggelenkprothetik. Orthopade 2006;35:489–494. [DOI] [PubMed] [Google Scholar]
- 3.Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg [Am] 1956;38-A:761–781. [PubMed] [Google Scholar]
- 4.Knupp M, Ledermann H, Magerkurth O, Hinterman B. The surgical tibiotalar angle: a radiologic study. Foot Ankle Int 2005;26:713–716. [DOI] [PubMed] [Google Scholar]
- 5.Inman V. Biomechanics of the ankle and subtalar joint. Inman’s joints of the ankle. Baltimore, MD: Williams and Wilkins, 1991:31–74. [Google Scholar]
- 6.Lowery RB. Fractures of the talus and os calcis. Curr Opin Orthop 1995;6:25–34. [Google Scholar]
- 7.Hermans JJ, Beumer A, de Jong TA, Kleinrensink GJ. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat 2010;217:633–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rothkötter H-J. Anatomie und Biomechanik von Sprunggelenk und Rückfuß. AE-Manual der Endoprothetik. Berlin, Heidelberg: Springer, 2011:3–8. [Google Scholar]
- 9.Hintermann B, Nigg BM. In vitro kinematics of the axially loaded ankle complex in response to dorsiflexion and plantarflexion. Foot Ankle Int 1995;16:514–518. [DOI] [PubMed] [Google Scholar]
- 10.Adelaar RS, Madrian JR. Avascular necrosis of the talus. Orthop Clin North Am 2004;35:383–395. [DOI] [PubMed] [Google Scholar]
- 11.Barnett CH, Napier JR. The axis of rotation at the ankle joint in man; its influence upon the form of the talus and the mobility of the fibula. J Anat 1952;86:1–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Seiler H. Biomechanics and functional anatomy of the upper ankle. Orthopade 1999;28:460–468. [DOI] [PubMed] [Google Scholar]
- 13.Pretterklieber ML. Anatomy and kinematics of the human ankle joint [Anatomie und Kinematik der Sprunggelenke des Menschen]. Radiologe 1999;39:1–7. [DOI] [PubMed] [Google Scholar]
- 14.Golanó P, Vega J, de Leeuw PA, et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc 2010;18:557–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lilyquist M, Shaw A, Latz K, Bogener J, Wentz B. Cadaveric analysis of the distal tibiofibular syndesmosis. Foot Ankle Int 2016;37:882–890. [DOI] [PubMed] [Google Scholar]
- 16.Subhas N, Vinson EN, Cothran RL, Santangelo JR, Nunley JA, II, Helms CA. MRI appearance of surgically proven abnormal accessory anterior-inferior tibiofibular ligament (Bassett’s ligament). Skeletal Radiol 2008;37:27–33. [DOI] [PubMed] [Google Scholar]
- 17.Hoefnagels EM, Waites MD, Wing ID, Belkoff SM, Swierstra BA. Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int 2007;28:602–604. [DOI] [PubMed] [Google Scholar]
- 18.Bartonícek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat 2003;25:379–386. [DOI] [PubMed] [Google Scholar]
- 19.Oh C-S, Won H-S, Hur M-S, et al. Anatomic variations and MRI of the intermalleolar ligament. AJR Am J Roentgenol 2006;186:943–947. [DOI] [PubMed] [Google Scholar]
- 20.Seifarth A. Anatomy and pathology of the ligaments in the upper and lower ankle joints. Arthroskopie 2019;32:125–132. [Google Scholar]
- 21.Milner CE, Soames RW. Anatomical variations of the anterior talofibular ligament of the human ankle joint. J Anat 1997;191:457–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Bekerom MP, Oostra RJ, Golanó P, van Dijk CN. The anatomy in relation to injury of the lateral collateral ligaments of the ankle: a current concepts review. Clin Anat 2008;21:619–626. [DOI] [PubMed] [Google Scholar]
- 23.Milner CE, Soames RW. Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int 1998;19:757–760. [DOI] [PubMed] [Google Scholar]
- 24.Castro MD. Ankle biomechanics. Foot Ankle Clin 2002;7:679–693. [DOI] [PubMed] [Google Scholar]
- 25.Leardini A, O’Connor JJ, Catani F, Giannini S. A geometric model of the human ankle joint. J Biomech 1999;32:585–591. [DOI] [PubMed] [Google Scholar]
- 26.Lundberg A, Goldie I, Kalin B, Selvik G. Kinematics of the ankle/foot complex: plantarflexion and dorsiflexion. Foot Ankle 1989;9:194–200. [DOI] [PubMed] [Google Scholar]
- 27.Heckman JD, McKee M, McQueen MM, Ricci W, Tornetta P, III. Rockwood and Green’s fractures in adults. Philadelphia, PA: Lippincott Williams & Wilkins, 2014. [Google Scholar]
- 28.Elsoe R, Ostgaard SE, Larsen P. Population-based epidemiology of 9767 ankle fractures. Foot Ankle Surg 2018;24:34–39. [DOI] [PubMed] [Google Scholar]
- 29.Thur CK, Edgren G, Jansson K-Å, Wretenberg P. Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: a population-based study of 91,410 Swedish inpatients. Acta Orthop 2012;83:276–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Juto H, Nilsson H, Morberg P. Epidemiology of adult ankle fractures: 1756 cases identified in Norrbotten County during 2009–2013 and classified according to AO/OTA. BMC Musculoskelet Disord 2018;19:441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pott P. Some few general remarks on fractures and dislocations. 1758. Clin Orthop Relat Res 2007;458:40–41. [DOI] [PubMed] [Google Scholar]
- 32.Bugler K, Watson CD, Hardie AR, et al. The treatment of unstable fractures of the ankle using the Acumed fibular nail J Bone Joint Surg [Br] 2012;94:1107–1112. [DOI] [PubMed] [Google Scholar]
- 33.Tartaglione JP, Rosenbaum AJ, Abousayed M, DiPreta JA. Classifications in brief: Lauge-Hansen classification of ankle fractures. Clin Orthop Relat Res 2015;473:3323–3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lauge-Hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg 1950;60:957–985. [PubMed] [Google Scholar]
- 35.Russo A, Reginelli A, Zappia M, et al. Ankle fracture: radiographic approach according to the Lauge-Hansen classification. Musculoskelet Surg 2013;97:S155–S160. [DOI] [PubMed] [Google Scholar]
- 36.Michelson J, Solocoff D, Waldman B, Kendell K, Ahn U. Ankle fractures. The Lauge-Hansen classification revisited. Clin Orthop Relat Res 1997;345:198–205. [PubMed] [Google Scholar]
- 37.Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: an MRI study. J Orthop Trauma 2006;20:267–272. [DOI] [PubMed] [Google Scholar]
- 38.Nielsen JØ, Dons-Jensen H, Sørensen HT. Lauge-Hansen classification of malleolar fractures: an assessment of the reproducibility in 118 cases. Acta Orthop Scand 1990;61:385–387. [DOI] [PubMed] [Google Scholar]
- 39.Thomsen NO, Overgaard S, Olsen LH, Hansen H, Nielsen ST. Observer variation in the radiographic classification of ankle fractures. J Bone Joint Surg [Br] 1991;73-B:676–678. [DOI] [PubMed] [Google Scholar]
- 40.Weber BG. Die Verletzungen des Oberen Sprunggelenkes. (Aktuelle Probleme in der Chirurgie). Bern: Huber, 1966. [Google Scholar]
- 41.Kennedy JG, Johnson SM, Collins AL, et al. An evaluation of the Weber classification of ankle fractures. Injury 1998;29:577–580. [DOI] [PubMed] [Google Scholar]
- 42.Malek IA, Machani B, Mevcha AM, Hyder NH. Inter-observer reliability and intra-observer reproducibility of the Weber classification of ankle fractures. J Bone Joint Surg [Br] 2006;88-B:1204–1206. [DOI] [PubMed] [Google Scholar]
- 43.Herscovici D, Jr, Scaduto JM, Infante A. Conservative treatment of isolated fractures of the medial malleolus. J Bone Joint Surg [Br] 2007;89-B:89–93. [DOI] [PubMed] [Google Scholar]
- 44.Carter TH, Duckworth AD, White TO. Medial malleolar fractures: current treatment concepts. J Bone Joint Surg [Br] 2019;101-B:512–521. [DOI] [PubMed] [Google Scholar]
- 45.Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg [Am] 2006;88-A:1085–1092. [DOI] [PubMed] [Google Scholar]
- 46.Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int 2017;38:1229–1235. [DOI] [PubMed] [Google Scholar]
- 47.Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 2015;135:505–516. [DOI] [PubMed] [Google Scholar]
- 48.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium—2018. J Orthop Trauma 2018;32:S1–S170. [DOI] [PubMed] [Google Scholar]
- 49.Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg 2016;55:140–145. [DOI] [PubMed] [Google Scholar]
- 50.White T, Carter T. Ankle fractures: facts and fiction. Bone & Joint 3602018;7:3–8. [Google Scholar]
- 51.Stufkens SA, van den Bekerom MP, Kerkhoffs GM, Hintermann B, van Dijk CN. Long-term outcome after 1822 operatively treated ankle fractures: a systematic review of the literature. Injury 2011;42:119–127. [DOI] [PubMed] [Google Scholar]
- 52.Larsen P, Rathleff MS, Elsoe R. Surgical versus conservative treatment for ankle fractures in adults: a systematic review and meta-analysis of the benefits and harms. Foot Ankle Surg 2019;25:409–417. [DOI] [PubMed] [Google Scholar]
- 53.Willett K, Keene DJ, Mistry D, et al. ; Ankle Injury Management (AIM) Trial Collaborators. Close contact casting vs surgery for initial treatment of unstable ankle fractures in older adults: a randomized clinical trial. JAMA 2016;316:1455–1463. [DOI] [PubMed] [Google Scholar]
- 54.Keene DJ, Lamb SE, Mistry D, et al. ; Ankle Injury Management (AIM) Trial Collaborators. Three-year follow-up of a trial of close contact casting vs surgery for initial treatment of unstable ankle fractures in older adults. JAMA 2018;319:1274–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Makwana NK, Bhowal B, Harper WM, Hui AW. Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age: a prospective, randomised study. J Bone Joint Surg [Br] 2001;83:525–529. [DOI] [PubMed] [Google Scholar]
- 56.Wei SY, Okereke E, Winiarsky R, Lotke PA. Nonoperatively treated displaced bimalleolar and trimalleolar fractures: a 20-year follow-up. Foot Ankle Int 1999;20:404–407. [DOI] [PubMed] [Google Scholar]
- 57.Rammelt S, Bartoníček J. Posterior malleolar fractures: a critical analysis review. JBJS Rev 2020;8:00207. [DOI] [PubMed] [Google Scholar]
- 58.Vacas-Sánchez E, Olaya-González C, Abarquero-Diezhandino A, Sánchez-Morata E, Vilá-Rico J. How to address the posterior malleolus in ankle fractures? A decision-making model based on the computerised tomography findings. Int Orthop 2020;44:1177–1185. [DOI] [PubMed] [Google Scholar]
- 59.Wang Z, Sun J, Yan J, et al. Comparison of the efficacy of posterior-anterior screws, anterior-posterior screws and a posterior-anterior plate in the fixation of posterior malleolar fractures with a fragment size of ≥ 15% and < 15%. BMC Musculoskelet Disord 2020;21:570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rammelt S, Grass R, Zwipp H. Ankle fractures. Unfallchirurg 2008;111:421–437. [DOI] [PubMed] [Google Scholar]
- 61.Zwipp H. Chirurgie des fußes. Berlin, Heidelberg: Springer-Verlag, 2013. [Google Scholar]
- 62.Bennett A, Smith K. (ii) Open fractures. Orthop Trauma 2013;27:9–14. [Google Scholar]
- 63.Saithna A, Moody W, Jenkinson E, Almazedi B, Sargeant I. The influence of timing of surgery on soft tissue complications in closed ankle fractures. Eur J Orthop Surg Traumatol 2009;19:481–484. [Google Scholar]
- 64.Naumann MG, Sigurdsen U, Utvåg SE, Stavem K. Associations of timing of surgery with postoperative length of stay, complications, and functional outcomes 3–6 years after operative fixation of closed ankle fractures. Injury 2017;48:1662–1669. [DOI] [PubMed] [Google Scholar]
- 65.Breederveld RS, van Straaten J, Patka P, van Mourik JC. Immediate or delayed operative treatment of fractures of the ankle. Injury 1988;19:436–438. [DOI] [PubMed] [Google Scholar]
- 66.Singh RA, Trickett R, Hodgson P. Early versus late surgery for closed ankle fractures. J Orthop Surg (Hong Kong) 2015;23:341–344. [DOI] [PubMed] [Google Scholar]
- 67.Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg [Am] 2012;94-A:2047–2052. [DOI] [PubMed] [Google Scholar]
- 68.Schepers T, De Vries MR, Van Lieshout EM, Van der Elst M. The timing of ankle fracture surgery and the effect on infectious complications: a case series and systematic review of the literature. Int Orthop 2013;37:489–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carragee EJ, Csongradi JJ, Bleck EE. Early complications in the operative treatment of ankle fractures: influence of delay before operation. J Bone Joint Surg [Br] 1991;73-B:79–82. [DOI] [PubMed] [Google Scholar]
- 70.Carragee EJ, Csongradi JJ. Increased rates of complications in patients with severe ankle fractures following interinstitutional transfers. J Trauma 1993;35:767–771. [DOI] [PubMed] [Google Scholar]
- 71.Høiness P, Strømsøe K. The influence of the timing of surgery on soft tissue complications and hospital stay: a review of 84 closed ankle fractures. Ann Chir Gynaecol 2000;89:6–9. [PubMed] [Google Scholar]
- 72.Adamson S, Trickett R, Hodgson P, Mohanty K. Ankle fractures: impact of timing of surgery. Inj Extra 2009;10:224. [Google Scholar]
- 73.Sukeik M, Qaffaf M, Ferrier G. Ankle fractures: impact of swelling on timing of surgery, length of hospital stay and the economic burden. Orthop Proc 2011;93-B(Supp II). [Google Scholar]
- 74.Court-Brown CM, Biant LC, Clement ND, Bugler KE, Duckworth AD, McQueen MM. Open fractures in the elderly: the importance of skin ageing. Injury 2015;46:189–194. [DOI] [PubMed] [Google Scholar]
- 75.Ovaska MT, Madanat R, Honkamaa M, Mäkinen TJ. Contemporary demographics and complications of patients treated for open ankle fractures. Injury 2015;46:1650–1655. [DOI] [PubMed] [Google Scholar]
- 76.Hulsker CC, Kleinveld S, Zonnenberg CB, Hogervorst M, van den Bekerom MP. Evidence-based treatment of open ankle fractures. Arch Orthop Trauma Surg 2011;131:1545–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ovaska MT, Madanat R, Mäkinen TJ. Predictors of postoperative wound necrosis following primary wound closure of open ankle fractures. Foot Ankle Int 2016;37:401–406. [DOI] [PubMed] [Google Scholar]
- 78.White CB, Turner NS, Lee G-C, Haidukewych GJ. Open ankle fractures in patients with diabetes mellitus. Clin Orthop Relat Res 2003;414:37–44. [DOI] [PubMed] [Google Scholar]
- 79.Ovaska MT, Mäkinen TJ, Madanat R, et al. Risk factors for deep surgical site infection following operative treatment of ankle fractures. J Bone Joint Surg [Am] 2013;95:348–353. [DOI] [PubMed] [Google Scholar]
- 80.Wukich DK, Kline AJ. The management of ankle fractures in patients with diabetes. J Bone Joint Surg Am 2008;90:1570–1578. [DOI] [PubMed] [Google Scholar]
- 81.El-Shazly M, Dalby-Ball J, Burton M, Saleh M. The use of trans-articular and extra-articular external fixation for management of distal tibial intra-articular fractures. Injury 2001;32:SD99–SD106. [DOI] [PubMed] [Google Scholar]
- 82.Salai M, Dudkiewicz I, Novikov I, Amit Y, Chechick A. The epidemic of ankle fractures in the elderly: is surgical treatment warranted? Arch Orthop Trauma Surg 2000;120:511–513. [DOI] [PubMed] [Google Scholar]
- 83.Beauchamp CG, Clay NR, Thexton PW. Displaced ankle fractures in patients over 50 years of age. J Bone Joint Surg [Br] 1983;65-B:329–332. [DOI] [PubMed] [Google Scholar]
- 84.Srinivasan CM, Moran CG. Internal fixation of ankle fractures in the very elderly. Injury 2001;32:559–563. [DOI] [PubMed] [Google Scholar]
- 85.Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury 2017;48:519–524. [DOI] [PubMed] [Google Scholar]
- 86.Jonas SC, Young AF, Curwen CH, McCann PA. Functional outcome following tibio-talar-calcaneal nailing for unstable osteoporotic ankle fractures. Injury 2013;44:994–997. [DOI] [PubMed] [Google Scholar]
- 87.Al-Nammari SS, Dawson-Bowling S, Amin A, Nielsen D. Fragility fractures of the ankle in the frail elderly patient: treatment with a long calcaneotalotibial nail. J Bone Joint Surg [Br] 2014;96-B:817–822. [DOI] [PubMed] [Google Scholar]
- 88.Goost H, Wimmer MD, Barg A, Kabir K, Valderrabano V, Burger C. Fractures of the ankle joint: investigation and treatment options. Dtsch Arztebl Int 2014;111:377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Konopitski A, Boniello AJ, Shah M, Katsman A, Cavanaugh G, Harding S. Techniques and considerations for the operative treatment of ankle fractures in the elderly. J Bone Joint Surg [Am] 2019;101:85–94. [DOI] [PubMed] [Google Scholar]
- 90.Zahn RK, Frey S, Jakubietz RG, et al. A contoured locking plate for distal fibular fractures in osteoporotic bone: a biomechanical cadaver study. Injury 2012;43:718–725. [DOI] [PubMed] [Google Scholar]
- 91.Bariteau JT, Fantry A, Blankenhorn B, Lareau C, Paller D, Digiovanni CW. A biomechanical evaluation of locked plating for distal fibula fractures in an osteoporotic sawbone model. Foot Ankle Surg 2014;20:44–47. [DOI] [PubMed] [Google Scholar]
- 92.Nguyentat A, Camisa W, Patel S, Lagaay P. A biomechanical comparison of locking versus conventional plate fixation for distal fibula fractures in trimalleolar ankle injuries. J Foot Ankle Surg 2016;55:132–135. [DOI] [PubMed] [Google Scholar]
- 93.Huang Z, Liu L, Tu C, et al. Comparison of three plate system for lateral malleolar fixation. BMC Musculoskelet Disord 2014;15:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schepers T, Van Lieshout EM, De Vries MR, Van der Elst M. Increased rates of wound complications with locking plates in distal fibular fractures. Injury 2011;42:1125–1129. [DOI] [PubMed] [Google Scholar]
- 95.White TO, Bugler KE, Appleton P, Will E, McQueen MM, Court-Brown CM. A prospective randomised controlled trial of the fibular nail versus standard open reduction and internal fixation for fixation of ankle fractures in elderly patients. J Bone Joint Surg [Br] 2016;98-B:1248–1252. [DOI] [PubMed] [Google Scholar]
- 96.Tsukada S, Otsuji M, Shiozaki A, et al. Locking versus non-locking neutralization plates for treatment of lateral malleolar fractures: a randomized controlled trial. Int Orthop 2013;37:2451–2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hess F, Sommer C. Minimally invasive plate osteosynthesis of the distal fibula with the locking compression plate: first experience of 20 cases. J Orthop Trauma 2011;25:110–115. [DOI] [PubMed] [Google Scholar]
- 98.Minihane KP, Lee C, Ahn C, Zhang L-Q, Merk BR. Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma 2006;20:562–566. [DOI] [PubMed] [Google Scholar]
- 99.Kilian M, Csörgö P, Vajczikova S, Luha J, Zamborsky R. Antiglide versus lateral plate fixation for Danis-Weber type B malleolar fractures caused by supination-external rotation injury. J Clin Orthop Trauma 2017;8:327–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Vance DD, Swindell HW, Greisberg JK, Vosseller JT. Outcomes following posterior and posterolateral plating of distal fibula fractures. Foot Ankle Spec 2019;12:246–252. [DOI] [PubMed] [Google Scholar]
- 101.Lamontagne J, Blachut PA, Broekhuyse HM, O’Brien PJ, Meek RN. Surgical treatment of a displaced lateral malleolus fracture: the antiglide technique versus lateral plate fixation. J Orthop Trauma 2002;16:498–502. [DOI] [PubMed] [Google Scholar]
- 102.Weber M, Krause F. Peroneal tendon lesions caused by antiglide plates used for fixation of lateral malleolar fractures: the effect of plate and screw position. Foot Ankle Int 2005;26:281–285. [DOI] [PubMed] [Google Scholar]
- 103.Ahn J, Kim S, Lee J-S, Woo K, Sung K-S. Incidence of peroneal tendinopathy after application of a posterior antiglide plate for repair of supination external rotation lateral malleolar fractures. J Foot Ankle Surg 2016;55:90–93. [DOI] [PubMed] [Google Scholar]
- 104.Weber M. Trimalleolar fractures with impaction of the posteromedial tibial plafond: implications for talar stability. Foot Ankle Int 2004;25:716–727. [DOI] [PubMed] [Google Scholar]
- 105.Smith G, Mackenzie SP, Wallace RJ, Carter T, White TO. Biomechanical comparison of intramedullary fibular nail versus plate and screw fixation. Foot Ankle Int 2017;38:1394–1399. [DOI] [PubMed] [Google Scholar]
- 106.Karkkola S, Kortekangas T, Pakarinen H, Flinkkilä T, Leskelä H-V, Niinimäki J. Fibular nailing for fixation of ankle fractures in patients at high risk of surgical wound infection. Foot Ankle Surg 2019;26:784–789 [DOI] [PubMed] [Google Scholar]
- 107.Jain S, Haughton BA, Brew C. Intramedullary fixation of distal fibular fractures: a systematic review of clinical and functional outcomes. J Orthop Traumatol 2014;15:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Asloum Y, Bedin B, Roger T, Charissoux J-L, Arnaud J-P, Mabit C. Internal fixation of the fibula in ankle fractures: a prospective, randomized and comparative study: plating versus nailing. Orthop Traumatol Surg Res 2014;100:S255–S259. [DOI] [PubMed] [Google Scholar]
- 109.Carter TH, Mackenzie SP, Bell KR, et al. Optimizing long-term outcomes and avoiding failure with the fibula intramedullary nail. J Orthop Trauma 2019;33:189–195. [DOI] [PubMed] [Google Scholar]
- 110.Bäcker HC, Vosseller JT. Fibular nail fixation: topical review. Foot Ankle Int 2019;40:1331–1337. [DOI] [PubMed] [Google Scholar]
- 111.van den Bekerom MP, Haverkamp D, Kloen P. Biomechanical and clinical evaluation of posterior malleolar fractures: a systematic review of the literature. J Trauma 2009;66:279–284. [DOI] [PubMed] [Google Scholar]
- 112.Veltman ES, Halma JJ, de Gast A. Longterm outcome of 886 posterior malleolar fractures: a systematic review of the literature. Foot Ankle Surg 2016;22:73–77. [DOI] [PubMed] [Google Scholar]
- 113.Solan MC, Sakellariou A. Posterior malleolus fractures: worth fixing. J Bone Joint Surg [Br] 2017;99-B:1413–1419. [DOI] [PubMed] [Google Scholar]
- 114.White TO. In defence of the posterior malleolus. J Bone Joint Surg [Br] 2018;100-B:566–569. [DOI] [PubMed] [Google Scholar]
- 115.O’Connor TJ, Mueller B, Ly TV, Jacobson AR, Nelson ER, Cole PA. ‘A to p’ screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J Orthop Trauma 2015;29:e151–e156. [DOI] [PubMed] [Google Scholar]
- 116.De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 2005;44:211–217. [DOI] [PubMed] [Google Scholar]
- 117.Hartford JM, Gorczyca JT, McNamara JL, Mayor MB. Tibiotalar contact area: contribution of posterior malleolus and deltoid ligament. Clin Orthop Relat Res 1995;320:182–187. [PubMed] [Google Scholar]
- 118.Tejwani NC, Pahk B, Egol KA. Effect of posterior malleolus fracture on outcome after unstable ankle fracture. J Trauma 2010;69:666–669. [DOI] [PubMed] [Google Scholar]
- 119.Ferries JS, DeCoster TA, Firoozbakhsh KK, Garcia JF, Miller RA. Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma 1994;8:328–331. [DOI] [PubMed] [Google Scholar]
- 120.Rammelt S, Boszczyk A. Computed tomography in the diagnosis and treatment of ankle fractures: a critical analysis review. JBJS Rev 2018;6:e7–e. [DOI] [PubMed] [Google Scholar]
- 121.Bartoníček J, Rammelt S, Tuček M, Naňka O. Posterior malleolar fractures of the ankle. Eur J Trauma Emerg Surg 2015;41:587–600. [DOI] [PubMed] [Google Scholar]
- 122.Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. Results of ankle fractures with involvement of the posterior tibial margin. J Trauma 2002;53:55–60. [DOI] [PubMed] [Google Scholar]
- 123.Bartoníček J, Rammelt S, Tuček M. Posterior malleolar fractures: changing concepts and recent developments. Foot Ankle Clin 2017;22:125–145. [DOI] [PubMed] [Google Scholar]
- 124.Bennett C, Behn A, Daoud AI, Dikos G, Bishop J, Sangeorzan B. Buttress plating versus anterior-to-posterior lag screws for fixation of the posterior malleolus: a biomechanical study. J Orthop Trauma 2016;30:664–669. [DOI] [PubMed] [Google Scholar]
- 125.Mason LW, Kaye A, Widnall J, Redfern J, Molloy A. Posterior malleolar ankle fractures: an effort at improving outcomes. JBJS Open Access 2019;4:e0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hartwich K, Lorente Gomez A, Pyrc J, Gut R, Rammelt S, Grass R. Biomechanical analysis of stability of posterior antiglide plating in osteoporotic pronation abduction ankle fracture model with posterior tibial fragment. Foot Ankle Int 2017;38:58–65. [DOI] [PubMed] [Google Scholar]
- 127.Little MT, Berkes MB, Lazaro LE, Sculco PK, Helfet DL, Lorich DG. Complications following treatment of supination external rotation ankle fractures through the posterolateral approach. Foot Ankle Int 2013;34:523–529. [DOI] [PubMed] [Google Scholar]
- 128.Karbassi JA, Braziel A, Garas PK, Patel AR. Open reduction internal fixation of posterior malleolus fractures and iatrogenic injuries: a cadaveric study. Foot Ankle Spec 2016;9:527–533. [DOI] [PubMed] [Google Scholar]
- 129.Shi HF, Xiong J, Chen YX, et al. Comparison of the direct and indirect reduction techniques during the surgical management of posterior malleolar fractures. BMC Musculoskelet Disord 2017;18:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vidović D, Elabjer E, Muškardin IVA, Milosevic M, Bekic M, Bakota B. Posterior fragment in ankle fractures: anteroposterior vs posteroanterior fixation. Injury 2017;48:S65–S69. [DOI] [PubMed] [Google Scholar]
- 131.Baumbach SF, Herterich V, Damblemont A, Hieber F, Böcker W, Polzer H. Open reduction and internal fixation of the posterior malleolus fragment frequently restores syndesmotic stability. Injury 2019;50:564–570. [DOI] [PubMed] [Google Scholar]
- 132.Verhage SM, Hoogendoorn JM, Krijnen P, Schipper IB. When and how to operate the posterior malleolus fragment in trimalleolar fractures: a systematic literature review. Arch Orthop Trauma Surg 2018;138:1213–1222. [DOI] [PubMed] [Google Scholar]
- 133.Wang L, Shi ZM, Zhang CQ, Zeng BF. Trimalleolar fracture with involvement of the entire posterior plafond. Foot Ankle Int 2011;32:774–781. [DOI] [PubMed] [Google Scholar]
- 134.Amorosa LF, Brown GD, Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma 2010;24:188–193. [DOI] [PubMed] [Google Scholar]
- 135.Bois AJ, Dust W. Posterior fracture dislocation of the ankle: technique and clinical experience using a posteromedial surgical approach. J Orthop Trauma 2008;22:629–636. [DOI] [PubMed] [Google Scholar]
- 136.Ribeiro HM, Silva J, Teixeira R, Fernandes P, Sobral L, Rosa I. Clinical outcomes and trans-syndesmotic screw frequency after posterior malleolar fracture osteosynthesis. Injury 2021;52:633–637. [DOI] [PubMed] [Google Scholar]
- 137.Yang T-C, Tzeng Y-H, Wang C-S, Lin C-C, Chang M-C, Chiang C-C. Untreated small posterior fragment of ankle fracture with early removal of syndesmotic screw is associated with recurrent syndesmotic instability. Injury 2021;52:638–643. [DOI] [PubMed] [Google Scholar]
- 138.Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res 2010;468:1129–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Miller MA, McDonald TC, Graves ML, et al. Stability of the syndesmosis after posterior malleolar fracture fixation. Foot Ankle Int 2018;39:99–104. [DOI] [PubMed] [Google Scholar]
- 140.Lee JS, Curnutte B, Pan K, Liu J, Ebraheim NA. Biomechanical comparison of suture-button, bioabsorbable screw, and metal screw for ankle syndesmotic repair: a meta-analysis. Foot Ankle Surg 2021;27:117–122. [DOI] [PubMed] [Google Scholar]
- 141.Ræder BW, Figved W, Madsen JE, Frihagen F, Jacobsen SB, Andersen MR. Better outcome for suture button compared with single syndesmotic screw for syndesmosis injury: five-year results of a randomized controlled trial. J Bone Joint Surg [Br] 2020;102-B:212–219. [DOI] [PubMed] [Google Scholar]
- 142.Andersen MR, Frihagen F, Hellund JC, Madsen JE, Figved W. Randomized trial comparing suture button with single syndesmotic screw for syndesmosis injury. J Bone Joint Surg [Am] 2018;100-A:2–12. [DOI] [PubMed] [Google Scholar]
- 143.Colcuc C, Blank M, Stein T, et al. Lower complication rate and faster return to sports in patients with acute syndesmotic rupture treated with a new knotless suture button device. Knee Surg Sports Traumatol Arthrosc 2018;26:3156–3164. [DOI] [PubMed] [Google Scholar]
- 144.Laflamme M, Belzile EL, Bédard L, van den Bekerom MP, Glazebrook M, Pelet S. A prospective randomized multicenter trial comparing clinical outcomes of patients treated surgically with a static or dynamic implant for acute ankle syndesmosis rupture. J Orthop Trauma 2015;29:216–223. [DOI] [PubMed] [Google Scholar]
- 145.Hoelsbrekken SE, Kaul-Jensen K, Mørch T, et al. Nonoperative treatment of the medial malleolus in bimalleolar and trimalleolar ankle fractures: a randomized controlled trial. J Orthop Trauma 2013;27:633–637. [DOI] [PubMed] [Google Scholar]
- 146.Carter TH, Oliver WM, Graham C, Duckworth AD, White TO. Medial malleolus: operative Or Non-operative (MOON) trial protocol – a prospective randomised controlled trial of operative versus non-operative management of associated medial malleolus fractures in unstable fractures of the ankle. Trials 2019;20:565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Saini P, Aggrawal A, Meena S, Trikha V, Mittal S. Miniarthrotomy assisted percutaneous screw fixation for displaced medial malleolus fractures: a novel technique. J Clin Orthop Trauma 2014;5:252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Weinraub GM, Levine P, Shi E, Flowers A. Comparison of medial malleolar fracture healing at 8 weeks after open reduction internal fixation versus percutaneous fixation: a retrospective cohort study. J Foot Ankle Surg 2017;56:277–281. [DOI] [PubMed] [Google Scholar]
- 149.Ebraheim NA, Ludwig T, Weston JT, Carroll T, Liu J. Comparison of surgical techniques of 111 medial malleolar fractures classified by fracture geometry. Foot Ankle Int 2014;35:471–477. [DOI] [PubMed] [Google Scholar]
- 150.Buckley R, Kwek E, Duffy P, et al. Single-screw fixation compared with double screw fixation for treatment of medial malleolar fractures: a prospective randomized trial. J Orthop Trauma 2018;32:548–553. [DOI] [PubMed] [Google Scholar]
- 151.Parker L, Garlick N, McCarthy I, Grechenig S, Grechenig W, Smitham P. Screw fixation of medial malleolar fractures: a cadaveric biomechanical study challenging the current AO philosophy. J Bone Joint Surg [Br] 2013;95-B:1662–1666. [DOI] [PubMed] [Google Scholar]
- 152.Ricci WM, Tornetta P, Borrelli J, Jr. Lag screw fixation of medial malleolar fractures: a biomechanical, radiographic, and clinical comparison of unicortical partially threaded lag screws and bicortical fully threaded lag screws. J Orthop Trauma 2012;26:602–606. [DOI] [PubMed] [Google Scholar]
- 153.Johnson BA, Fallat LM. Comparison of tension band wire and cancellous bone screw fixation for medial malleolar fractures. J Foot Ankle Surg 1997;36:284289. [DOI] [PubMed] [Google Scholar]
- 154.Georgiadis GM, White DB. Modified tension band wiring of medial malleolar ankle fractures. Foot Ankle Int 1995;16:64–68. [DOI] [PubMed] [Google Scholar]
- 155.Ostrum RF, Litsky AS. Tension band fixation of medial malleolus fractures. J Orthop Trauma 1992;6:464–468. [DOI] [PubMed] [Google Scholar]
- 156.Downey MW, Duncan K, Kosmopoulos V, et al. Comparing the knotless tension band and the traditional stainless steel wire tension band fixation for medial malleolus fractures: a retrospective clinical study. Scientifica (Cairo) 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wegner AM, Wolinsky PR, Robbins MA, Garcia TC, Maitra S, Amanatullah DF. Antiglide plating of vertical medial malleolus fractures provides stiffer initial fixation than bicortical or unicortical screw fixation. Clin Biomech (Bristol, Avon) 2016;31:29–32. [DOI] [PubMed] [Google Scholar]
- 158.Chen X-Z, Chen Y, Liu C-G, Yang H, Xu X-D, Lin P. Arthroscopy-assisted surgery for acute ankle fractures: a systematic review. Arthroscopy 2015;31:2224–2231. [DOI] [PubMed] [Google Scholar]
- 159.Gonzalez TA, Macaulay AA, Ehrlichman LK, Drummond R, Mittal V, DiGiovanni CW. Arthroscopically assisted versus standard open reduction and internal fixation techniques for the acute ankle fracture. Foot Ankle Int 2016;37:554–562. [DOI] [PubMed] [Google Scholar]
- 160.Baumbach SF, Urresti-Gundlach M, Braunstein M, et al. Propensity score-matched analysis of arthroscopically assisted ankle facture treatment versus conventional treatment. Foot Ankle Int 2021;42:400–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hintermann B, Regazzoni P, Lampert C, Stutz G, Gächter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg [Br] 2000;82-B:345–351. [DOI] [PubMed] [Google Scholar]
- 162.Fuchs DJ, Ho BS, LaBelle MW, Kelikian AS. Effect of arthroscopic evaluation of acute ankle fractures on PROMIS intermediate-term functional outcomes. Foot Ankle Int 2016;37:51–57. [DOI] [PubMed] [Google Scholar]
- 163.Braunstein M, Baumbach SF, Böcker W, Mutschler W, Polzer H. [Arthroscopically assisted treatment of ankle fractures]. Unfallchirurg 2016;119:92–98. [DOI] [PubMed] [Google Scholar]
- 164.Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg [Am] 2009;91-A:333–339. [DOI] [PubMed] [Google Scholar]


