Abstract
Falls efficacy is a widely studied construct. The understanding of falls efficacy has evolved over time. Falls efficacy was initially perceived to be suitably used as a measure of fear of falling. However, further research suggested that falls efficacy and fear of falling are distinct constructs, and therefore, would be inappropriate to be used as a proxy. Instead, some researchers posited that falls efficacy is synonymous with balance confidence. Falls efficacy has been conventionally understood as the perceived ability of individuals to perform activities without losing balance or falling. A recently conducted systematic review by the authors on existing falls efficacy related measures had revealed a fresh perspective of recognising falls efficacy as a perceived ability to manage a threat of a fall. Falls efficacy, with a broadened interpreted construct, relates to the individual’s perceived self-efficacy of performing necessary actions needed in different scenarios, including pre-fall, near-fall, fall-landing and completed fall. The conventional interpretation of falls efficacy needs a rethinking of perspective. An extended understanding of falls efficacy would provide an integral approach towards improving the agency of individual to deal with falls and would enhance person-centred care.
Keywords: Falls efficacy, Older Adults, Person-centred care, Physiotherapy, Rehabilitation
Introduction
Falls efficacy was first introduced by Tinetti et al.[1] to our community of clinicians and researchers in the field of gerontology as a potential construct used to determine fear of falling. Using Bandura’s self-efficacy theory[2], fear of falling was interpreted as low perceived self-efficacy in performing various activities, taking into account one’s personal risk to experience a potential fall. The approach of assessing fear of falling was to ask individuals about their confidence in performing various activities without falling. Those who reported a significant lack of confidence were viewed to have a fear of falling[1]. This initial conceptualisation of falls efficacy and fear of falling used in parallel led to much inquiry towards the perceived ability in older adults to manage falls[3]. Over the last three decades, falls-related research has been focused on providing empirical evidence for different rehabilitation approaches on their efficiency and effectiveness towards improving falls efficacy or to address the fear of falling[4,5]. The understanding of falls efficacy has evolved. This article aims to provide a review of falls efficacy, highlight some current rehabilitation practices, and reiterate the importance of person-centred care through our reflection of falls efficacy.
Understanding falls efficacy
Self-efficacy relates to the individual’s perception of one’s capabilities to successfully complete a specific task or perform in a specific scenario[6]. Self-efficacy is viewed as a measurable cognitive mechanism that mediates between thoughts/emotions and actions[7]. In contrast, the construct of fear is accounted for by both emotional aspects, e.g. anxiety and behavioural elements, e.g. activity avoidance[8]. Fear of falling commonly describes an exaggerated concern of falling that leads to excess restriction of activities[9]. Given the different nature of self-efficacy and fear, different authors including Li et al.[10], Hotchkiss et al.[11], Hadjistavropoulos et al.[12] and Hughes et al.[8] have attempted to distinguish between falls efficacy and fear of falling.
Falls efficacy has been defined as the perceived self-efficacy to perform activities of daily living without falling[1]. Stemmed from this perspective, the Falls Efficacy Scale (FES), the first measure of falls efficacy, was developed by clinicians to identify the “most important activities essential to independent living, that while requiring some position change or walking, would be safe and non-hazardous to most elderly persons”[1]. Fear of falling, on the other hand, has been defined as the lasting concerns about falling that leads to an individual avoiding activities that one remains capable of performing[8]. An early measure for this fear, the Falls Efficacy Scale – International (FES-I), was developed by colleagues from the Prevention of Falls Network Europe (ProFaNE). The original FES has been modified to assess the level of concern about falling when carrying out various activities[13]. Another construct, balance confidence, has also been studied closely alongside falls efficacy. The first measure of balance confidence, the Activities-specific Balance Confidence Scale (ABC), was constructed by having similar questions used for falls efficacy posed to clinicians and older adults[14]. Recognising that the measures of falls efficacy and balance confidence had high correlations, Hadjistavropoulos et al.[3] posited that falls efficacy had a tautological relationship to balance confidence and that the two constructs should be viewed to be “equivalent and interchangeable”.
Since the original development of the FES and the ABC, different methodologies have been used to develop other measures for the different falls-related psychological constructs. In essence, measures of falls efficacy or balance confidence have been designed to understand the perceived ability of individuals to maintain balance while performing various activities. On the other hand, measures of fear of falling aim to identify the level of concerns about falling among older adults spanning different activities. Some widely used measures for the different constructs are listed in Table 1. The term “Falls Efficacy” was retained in the title for the measure of fear of falling so as to acknowledge the historical development of the scale[13]. It is necessary to reiterate that the fear measures such as the FES-I[13] and the Iconographical FES (Icon-FES)[15] were conceptualised to measure the concerns of individuals about falling or fear of falling, and not falls efficacy.
Table 1.
List of measures used for different constructs.
| Construct | Definition |
|---|---|
| Falls efficacy | Perceived self-efficacy to perform activities of daily living without falling1 |
| Instruments | |
| FES-101, MFES-1156, MFES-125, MFES-1357, MFES-1458, PAPMFR21, PAMF5 | |
| Construct | Definition |
| Fear of falling | The lasting concerns about falling that leads to an individual avoiding activities that one remains capable of performing8,59 |
| Instruments | |
| FES-I13, Icon-FES15, GFFM60, UIC FFM61, SAFE62, FFABQ63, FFQ-R64 | |
| Construct | Definition |
| Balance confidence | The individual’s belief about their ability to maintain balance whilst performing activities of daily living14 |
| Instruments | |
| ABC-665, ABC-1566, ABC-1614, CONFBal67 | |
FES: Falls Efficacy Scale, MFES: Modified Falls Efficacy Scale, PAPMFR: Perceived Ability to Prevent and Manage Fall Risks, PAMF: Perceived Ability to Manage Risk of Falls or Actual Falls, FES-I: Falls Efficacy Scale – International, Icon-FES: Iconographical Falls Efficacy Scale, GFFM: Geriatric Fear of Falling Measure, UIC FFM: University of Illinois at Chicago Fear of Falling Measure, SAFE: Survey of Activities and Fear of Falling in the Elderly, FFABQ: Fear of Falling Avoidance Behaviour Questionnaire, FFQ-R: Fear of falling questionnaire revised, ABC: Activities specific Balance Confidence Scale, CONFBal: CONFBal scale of balance confidence
As falls-related research advances, the interpretation of falls efficacy has changed. The initial understanding of falls efficacy, which had been interpreted as a measure of fear of falling in the 1990s, had several advantages[1]. First, the operationalisation allowed objective, reliable and valid strategies to be developed based on measuring efficacy across a range of activities. Second, a measure of fear of falling could be made using a continuous scale response option. Third, associating fear with self-efficacy mitigated the perception that fear of falling was a psychiatric condition. However, further research revealed that falls efficacy and fear of falling, despite being highly correlated, were distinct constructs and should be measured separately by different measurement instruments[3]. Falls efficacy was viewed to have a tautological relationship with balance confidence in the 2000s[3] and was addressed through clinical strategies focused on improving balance, strength and increasing the level of physical activities among older adults[16,17]. To avoid any misinterpretation of the construct of interest, several authors such as Jorstad et al.[18], Moore et al.[19] and Hughes et al.[8] called for the clinical and research community to clarify their construct of interest. These included areas in falls efficacy amongst other falls-related psychological constructs, including fear of falling, balance confidence and outcome expectancy, alongside selected measures.
Recently, a systematic review of different falls-efficacy related measurement instruments suggested that the interpretation of falls efficacy should be extended beyond the synonymous interpretation of falls efficacy and balance confidence[20]. To justify that call, two fall efficacy related scales, the “Perceived Ability to Prevent and Manage Fall Risks” (PAMF)[5] and the “Perceived Ability to Manage Risk of Falls or Actual Falls” (PAPMFR)[21], were highlighted among eighteen other measurement instruments. Developers of PAMF and PAPMFR conceptualised falls efficacy based on a formative model, where many measures were developed based on a reflective model to assess falls efficacy. The distinction between formative and reflective models was based on asking oneself whether the indicator “forms” or contributes to an underlying construct or if the indicator “reflects” an underlying construct (using a “thought test”), i.e. do we expect the items to change when the construct changes?[22] The PAMF included the following items: (1) finding ways to get up if they fell; (2) finding ways to reduce falls; (3) protecting themselves if they do fall; (4) increasing their physical strength and (5) getting steadier on their feet. The PAPMFR listed items including: (1) steadiness on their feet; (2) balance while walking; (3) ability to walk in their homes; (4) ability to walk outdoors; (5) ability to prevent falls and (6) ability to find ways to get up if they fell. It was viewed that the items in both measures were used to form an understanding of falls efficacy. Yoshikawa and Smith[21] reported that the items in PAPMFR aimed to cover a wide range of fall-related perceptions, which were addressed through their multi-modal falls management program.
A new perspective of falls efficacy
Drawing upon previous research, Soh et al.[20] proposed that falls efficacy should be considered across a continuum from: (1) pre-fall; (2) near-fall; (3) fall-landing and (4) completed fall (Figure 1) to provide a complete conceptual understanding of falls efficacy. In the pre-fall domain, balance self-efficacy or balance confidence refers to the perceived self-efficacy of performing activities without losing balance or falling. In the near-fall domain, balance recovery self-efficacy or balance recovery confidence relates to the perceived ability to recover balance in response to perturbations. For example, one might quickly grab onto a pole or take a few steps to recover balance after a trip or a slip. When the individual has inadequate reactive balance recovery abilities to regain balance, the fall is viewed as a consequential event[23]. Balance recovery strategies such as compensatory stepping and reach-to-grasp are necessary skills to arrest a fall[24,25]. Balance recovery confidence differs from balance confidence, given that balance recovery confidence focuses on the perceived ability of one’s reactive balance recovery skills to regain balance[26]. Two other domains in the extended interpretation of falls efficacy refer to the fall-landing and the completed-fall. The fall-landing domain attends to the self-efficacy of falling safely onto the ground[27], whereas the completed fall domain relates to the self-efficacy to recover from the fall[28]. Both domains attend to the consequences of an actual fall and should, therefore, be addressed with older adults to adequately deal with the dangers of falling. From this perspective, falls efficacy should be better defined as the perceived ability to manage a potential threat of a fall.
Figure 1.
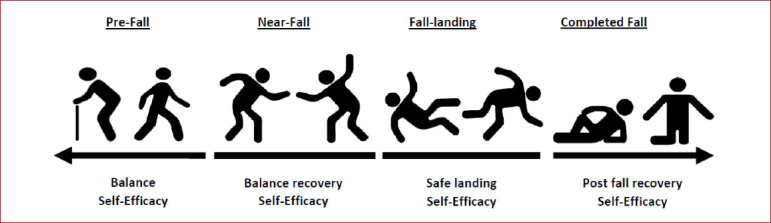
Extended interpretation of falls efficacy from the Falls-related Self-efficacy Continuum Model (Reproduced with permission (20), Copyright 2021, BMC Geriatrics).
An extended interpretation of falls efficacy has its advantages. First, it encourages researchers and clinicians to give greater consideration to the actual construct which they target to address. For example, the goal to improve the reactive balancing ability in response to perturbations; to fall safely on the ground and reduce injurious falls; or perhaps being able to get up or get help effectively after a fall. If so, what would be the appropriate measures used to assess the effectiveness of the rehabilitation program? Second, falls efficacy would not be limited as a “danger-avoidance” approach, i.e. perceived ability to avoid falls. Approaching falls management by avoiding falls provides a lacuna in the understanding for clinicians working with older adults to tackle falls. Falls efficacy should include the perceived ability to address the fall itself (the danger), such as the loss of balance, landing impact, and post-fall recovery.
Hence, a broader interpretation of falls efficacy is needed to comprehensively understand the varying perceived abilities associated with the different demands relating to a fall. Finally, extending the interpretation of falls efficacy allows relevant measurement instruments to be appropriately used in the evaluation of the rehabilitation strategies. Bandura[29] stated that there is no all-purpose measure of perceived self-efficacy. Instead, perceived self-efficacy measures must be tailored to each domain of functioning that is the object of interest.
Current rehabilitation practices for falls efficacy
Contemporary rehabilitation can be categorised based on a broader conceptual understanding of falls efficacy. Approaching current rehabilitation practices from an updated conceptual understanding of falls efficacy would provide a conceptual alignment[30]. A summary of measures suitable for the different domains is provided in Table 2.
Table 2.
List of measures used for the different domains of falls efficacy.
| Domain | Construct | Focus of self-efficacy |
|---|---|---|
| Pre-fall | Balance self-efficacy | On the individual’s perceived performance of activities without losing balance or falling |
| Instruments | ||
| FES-101, MFES-156, MFES-125, MFES-1357, MFES-1458, Five items in PAPMFR21: “Steadiness on their feet”, “Balance while walking”, “Ability to walking in their homes”, “Ability to walk outdoors”, “Ability to prevent falls”, GES-868, GES-1069, Three items in PCOF5: “I can reduce my risk of falling”, “There are things I can do to keep myself from falling”, “Falling is something I can control”, Three items in PAMF5: “Finding ways to reduce falls”, “Increasing their physical strength, “Getting steadier on their feet”, BSPT70, ABC-665, ABC-1566, ABC-1614, CONFBal67 | ||
| Domain | Construct | Focus of self-efficacy |
| Near-fall | Balance recovery self-efficacy | On the individual’s perceived ability to recover balance from different types of perturbations e.g. a slip or a trip or a loss of balance from volitional movements. |
| Instruments | ||
| No measure available. A scale of balance recovery confidence71 has been developed by the authors. The scale is currently evaluated for its psychometric properties. | ||
| Domain | Construct | Focus of self-efficacy |
| Fall-landing | Safe landing self-efficacy | On the individual’s perceived ability to fall on the floor or lower ground safely |
| Instruments | ||
| One item in Perceived Ability to Manage Risk of Falls or Actual Falls (PAMF)5: “Protecting themselves if they do fall” | ||
| Domain | Construct | Focus of self-efficacy |
| Completed fall | Post fall recovery self-efficacy | On the individual’s perceived ability to get up or get help after a fall |
| Instruments | ||
| One item in PAMF5: “Finding a way to get up if they fell”, one item in PAPMFR21: “Ability to find a way to get up if they fall” | ||
FES: Falls Efficacy Scale, MFES: Modified Falls Efficacy Scale, PAPMFR: Perceived Ability to Prevent and Manage Fall Risks, GES: Gait Efficacy Scale, PCOF: Perceived Control over Falling, PAMF: Perceived Ability to Manage Risk of Falls or Actual Falls, BSPT: Balance Self-Perceptions Test, ABC: Activities specific Balance Confidence Scale, CONFBal: CONFBal scale of balance confidence.
Pre-fall domain
Pre-fall relates to the individual performing various activities without losing balance or falling. Much research on falls prevention has focused on this domain by identifying fall risk factors and implementing interventions to address these risks. The evidence-based fall prevention interventions can be broadly categorised as single-component interventions focusing on a specific fall risk factor (e.g. muscle weakness, poor balance, psychoactive medications and home hazards) or multi-component intervention that address several modifiable risk factors[31]. A recent systematic review conducted by Sherrington et al.[32] reported that exercise programs should include aspects of balance, functional exercises and resistance exercises in order to be effective in reducing the rate of falls and the number of older adults experiencing falls living in the community. Community-based interventions promoting behavioural changes, increasing falls-prevention knowledge and reducing home hazards are also well-known approaches when working with older adults to avoid falls[33,34]. In the pre-fall domain, commonly used measurement instruments include the FES, modified FES and the ABC.
Near-fall domain
The near-fall domain is a less studied area compared to the pre-fall domain. A near-fall is defined as a stumble event or loss of balance that would result in a fall if sufficient recovery mechanisms were not activated[35]. Balance recovery abilities are recognised to be crucial skills, given that the inability to recover from the loss of balance or perturbation would be considered the cause of a fall[36]. According to Tokur et al.[37], balance recovery capabilities are needed to respond to perturbations experienced in daily activities. The inability to recover from falls caused by slips, trips and loss of balance are common initiating events leading to falls among older adults[38]. Rubenstein[39] viewed that older adults were stiffer and less coordinated compared to young adults and hence would have impaired ability to arrest a fall in response to an unexpected trip or slip. Older adults with existing comorbidities are known to have poorer balance recovery abilities, risking a higher incidence of falls[40]. Nascent skill-specific rehabilitation interventions (e.g. perturbation-based training) have shown promising results to improve the execution of balance recovery reactive manoeuvres[41,42]. Presently, there is no known measure for balance recovery confidence[20], although a measure has been developed by an international multi-disciplinary study team and is currently under validation[43].
Fall-landing domain
Two other domains of falls efficacy should be considered to prepare older adults to adequately manage an unfortunate fall event following an irrecoverable loss of balance. The fall-landing domain relates to the individual landing at a lower level from an irrecoverable loss of balance. Some ways to minimise physical injuries may include teaching techniques on safe landing[27], as well as the use of hip protectors[44] or appropriately designed flooring[28]. However, passive interventions do not rely on the individual’s perceived ability to successfully complete a task. Therefore, the outcome measures used to evaluate the effectiveness of products should suitably consider the one item from the PAMF scale[5], “Protecting themselves if they do fall”, to identify their sense of self-efficacy or concerns about falling using measures, such as the Falls Efficacy Scale-International[13].
Completed fall domain
When the individual has fallen to the ground or onto a lower level, the individual should have the necessary resources to recover from the fall. The completed fall domain has established rehabilitation strategies which include the training of an older person to get up from the floor[45]. This mode of training instils some degree of confidence in their ability to deal with the “unexpected event” scenario in older adults. The items “Finding a way to get up if they fell” from the PAMF[5] or “Ability to find a way to get up if they fall” from the PAPMFR[21] may be appropriately used to gain a better understanding of the perceived self-efficacy in individuals within this domain.
As there is an absence of empirical evidence in the measurement properties of existing measures to determine the perceived self-efficacy in older people within different domains of falls efficacy (other than balance confidence), clinicians should interpret the results with caution. Researchers and clinicians aiming to develop appropriate measures should conduct a systematic literature review for all existing instruments for the specific constructs[22]. Moving forward with our practice, we reiterate the calls of Jørstad et al.[18], Moore and Ellis[19] and Hughes et al.[8] that researchers and clinicians need to be mindful of the construct of interest, adequately stating them when using the different measurement instruments, so as to avoid research waste and to mitigate the risk of misinterpretation by fellow colleagues[46].
Person-centred care
Applying a new perspective of falls efficacy is important in person-centred care practice (PCC). PCC highlights the importance of knowing the individual as a person and is a key component in engaging the person as an active partner for their care[47]. Clinicians working with older adults should aim to preserve their identity and independence when managing different issues surrounding falls[48]. A comprehensive approach should not only address ways of mitigating the risks of falling, but to advocate a spectrum of strategies, including improving reactive balance recovery abilities, learning skills to be a ‘safe faller’, and knowing the different ways of getting help after a fall. This would allow the older person to lead a fulfilling and flourishing life[28]. Clinicians have acknowledged the importance of working with the older person through a shared decision-making process: the foundation of patient-centred care, and in this case, older person-centred care[49]. To have an effective, shared decision-making session, healthcare providers need to partner with their patients and support their patients in making health care choices consistent with their values and priorities.
The use of appropriate measures to understand specific constructs has been proposed as valuable tools to build mutual understanding between health care professionals and their patients[50]. Improper use of measures, e.g. for other purposes that they are validated for, can risk clinicians making inadequate clinical decisions, leading to patients not receiving the care that they need. Given that person-centred care stems from the proper understanding of patient’s needs, then accurate information of their perceived self-efficacy is required to inform clinicians[51,52].
Moving forward
Working with older adults to deal with a complex phenomenon such as a fall requires a clear and comprehensive approach[53]. A broader perspective of falls efficacy should improve agency in older adults to remain independent and be confident of overcoming the consequences of falling. Falls management is not just about avoiding the risks of falling[28] but should include complementary strategies to deal with the falling process, as well as to recover from a fall. The notion of falls efficacy is a multidimensional construct that would encourage clinicians and researchers to work on specific issues of falls and falling.
Presently, there are well-established measurement instruments available to measure the self-efficacy of performing activities without losing balance or falling (pre-fall domain). Current measures of falls efficacy might suitably measure the construct of balance confidence. There is a need to further investigate the suitability of existing measures for the other domains of falls efficacy. If not, then new measures should be purposefully created. Further research applying appropriate assessments, interventions, and evaluation methods, e.g. COSMIN[54] guide would be needed to have a fuller understanding about the different domains of falls efficacy in various settings. Falls efficacy may not have a tautological relationship with balance confidence. Falls efficacy should be viewed as the perceived self-efficacy to manage a fall, addressing four domains from pre-fall to post-fall. Lach[55] had pointed out the need to consider both efficacy expectations and outcome expectancy in her article “Self-efficacy and fear of falling: in search of complete theory”. It may be plausible that the new perspective of falls efficacy would open the possibility to gain a better understanding of the effect of falling, as well as the effect of falling on the behaviour and health of older adults. An extended understanding of falls efficacy might possibly reshape how clinicians and researchers approach their practice to improve self-efficacy in older adults on falls.
Conclusion
Applying a new perspective towards falls efficacy may potentially drive a more meaningful direction toward falls management. The traditional understanding of falls efficacy has been purposeful in helping older adults maintain their independence. However, it may not be enough in empowering an older person to deal with an actual fall, e.g. improved agency in older adults to arrest a fall upon losing balance, fall safely or recover post-fall. An extended perspective of falls efficacy gives greater attention to the self-efficaciousness of handling a fall if the unfortunate event occurs. There is a need for clinicians and researchers to be explicit about the targeted construct of interest and select suitable self-reported measurement instruments to evaluate the efficacy of rehabilitation approaches for the intended construct.
Footnotes
Edited by: George Lyritis
References
- 1.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol B-Psychol. 1990;45(6):P239–43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 2.Bandura A. Self-efficacy:Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 3.Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualising the role of fear of falling and balance confidence in fall risk. J Aging Health. 2011;23(1):3–23. doi: 10.1177/0898264310378039. [DOI] [PubMed] [Google Scholar]
- 4.Bjerk M, Brovold T, Skelton DA, Bergland A. A falls prevention programme to improve quality of life, physical function and falls efficacy in older people receiving home help services:Study protocol for a randomised controlled trial. BMC Health Serv Res. 2017;17(1) doi: 10.1186/s12913-017-2516-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tennstedt S, Howland J, Lachman M, Peterson E, Kasten L, Jette A. A randomised, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B-Psychol. 1998;53B(6):P384–P92. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]
- 6.Bandura A, &Schunk D. H. Cultivating competence, self-efficacy, and intrinsic interest through proximal self-motivation. Journal of Personality and Social Psychology. 1981;(41):586–98. [Google Scholar]
- 7.Bandura A. Self-efficacy mchanism in human agency. Am Psychol. 1982;37(2):122–47. [Google Scholar]
- 8.Hughes CC, Kneebone II, Jones F, Brady B. A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int Psychogeriatr. 2015;27(7):1071–87. doi: 10.1017/S1041610214002701. [DOI] [PubMed] [Google Scholar]
- 9.Abyad A, Hammami SO. Fear of falling in the elderly - an emerging syndrome. Middle East Journal of Age and Ageing. 2017;14(3):16–25. [Google Scholar]
- 10.Li F, McAuley E, Fisher KJ, Harmer P, Chaumeton N, Wilson NL. Self-efficacy as a mediator between fear of falling and functional ability in the elderly. J Aging Health. 2002;14(4):452–66. doi: 10.1177/089826402237178. [DOI] [PubMed] [Google Scholar]
- 11.Hotchkiss A, Fisher A, Robertson R, Ruttencutter A, Schuffert J, Barker DB. Convergent and predictive validity of three scales related to falls in the elderly. Am J Occup Ther. 2004;58(1):100–3. doi: 10.5014/ajot.58.1.100. [DOI] [PubMed] [Google Scholar]
- 12.Hadjistavropoulos T, Martin RR, Sharpe D, Lints-Martindale AC, McCreary DR, Asmundson GJG. A longitudinal investigation of fear of falling, fear of pain, and activity avoidance in community dwelling older adults. J Aging Health. 2007;19:965–84. doi: 10.1177/0898264307308611. [DOI] [PubMed] [Google Scholar]
- 13.Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age Ageing. 2005;34(6):614–9. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 14.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 15.Delbaere K, Smith ST, Lord SR. Development and initial validation of the Iconographical Falls Efficacy Scale. J Gerontol A Biol Sci Med Sci. 2011;66(6):674–80. doi: 10.1093/gerona/glr019. [DOI] [PubMed] [Google Scholar]
- 16.Arai T, Obuchi S, Inaba Y, Nagasawa H, Shiba Y, Watanabe S, Kimura K, Kojima M. The effects of short-term exercise intervention on falls self-efficacy and the relationship between changes in physical function and falls self-efficacy in Japanese older people:A randomised controlled trial. Am J Phys Med Rehabil. 2007;86(2):133–41. doi: 10.1097/PHM.0b013e31802ef29d. [DOI] [PubMed] [Google Scholar]
- 17.Rochat S, Bula C, Martin E, Ganea R, Hoskovec C, Ionescu A, Seematter-Bagnoud L, Karmaniola A, Piot-Ziegler C, Aminian K, Santos-Eggimann B. Does falls efficacy predict gait performance in high-functioning older people? Gerontologist. 2008;48:536. [Google Scholar]
- 18.Jørstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling:a systematic review. J Am Geriatr Soc. 2005;53(3):501–10. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- 19.Moore DS, Ellis R. Measurement of fall-related psychological constructs among independent-living older adults:a review of the research literature. Aging and Mental Health. 2008;12(6):684–99. doi: 10.1080/13607860802148855. [DOI] [PubMed] [Google Scholar]
- 20.Soh SLH, Lane J, Xu T, Gleeson N, Tan CW. Falls efficacy instruments for community-dwelling older adults:a COSMIN-based systematic review. BMC Geriatr. 2021;21(21):1–10. doi: 10.1186/s12877-020-01960-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoshikawa A, Smith ML. Mediating role of fall-related efficacy in a fall prevention program. Am J Health Behav. 2019;43(2):393–405. doi: 10.5993/AJHB.43.2.15. [DOI] [PubMed] [Google Scholar]
- 22.De Vet HCW, Terwee CB, Mokkink LB, Knol DL. Measurement in medicine:A practical guide. Cambridge: Cambridge University Press; 2011. [Google Scholar]
- 23.Maki BE, Sibley KM, Jaglal SB, Bayley M, Brooks D, Fernie GR, Flint AJ, Gage W, Liu BA, McIlroy WE, Mihailidis A, Perry SD, Popovic MR, Pratt J, Zettel JL. Reducing fall risk by improving balance control:development, evaluation and knowledge-translation of new approaches. J Safety Res. 2011;42(6):473–85. doi: 10.1016/j.jsr.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Gerards MHG, McCrum C, Mansfield A, Meijer K. Perturbation-based balance training for falls reduction among older adults:Current evidence and implications for clinical practice. Geriatr Gerontol Int. 2017;17(12):2294–303. doi: 10.1111/ggi.13082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soh SLH, Tan CW, Lane J, Yeh TT, Soon B. Near falls in Singapore community-dwelling older adults:a feasibility study. Pilot Feasibility Stud. 2021;7(25) doi: 10.1186/s40814-020-00748-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maki BE, McIlroy WE. The role of limb movements in maintaining upright stance:the 'change-in-support'strategy. Phys Ther. 1997;77(5):488–507. doi: 10.1093/ptj/77.5.488. [DOI] [PubMed] [Google Scholar]
- 27.Moon Y, Sosnoff JJ. Safe landing strategies during a fall:systematic review and meta-analysis. Arch Phys Med Rehabil. 2017;98(4):783–94. doi: 10.1016/j.apmr.2016.08.460. [DOI] [PubMed] [Google Scholar]
- 28.Gustavsson J, Jernbro C, Nilson F. There is more to life than risk avoidance - elderly people's experiences of falls, fall-injuries and compliant flooring. Int J Qual Stud Health Well-being. 2018;13(1):1–9. doi: 10.1080/17482631.2018.1479586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bandura A. In: Guide for constructing self-efficacy scales. Pajares F, Urdan TC, editors. Connecticut: Information Age Publishing; 2006. [Google Scholar]
- 30.Terwee CB, Prinsen CAC, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, Bouter LM, de Vet HCW, Mokkink LB. COSMIN methodology for evaluating the content validity of patient-reported outcome measures:a Delphi study. Qual Life Res. 2018;27(5):1159–70. doi: 10.1007/s11136-018-1829-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stevens JA, Sleet DA, Rubenstein LZ. The influence of older adults'beliefs and attitudes on adopting fall prevention behaviors. Am J Lifestyle Med. 2018;12(4):324–30. doi: 10.1177/1559827616687263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb SE. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424. doi: 10.1002/14651858.CD012424.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clemson L, Cumming RG, Kendig H, Swann M, Heard R, Taylor K. The effectiveness of a community-based program for reducing the incidence of falls in the elderly:a randomised trial. J Am Geriatr Soc. 2004;52(9):1487–94. doi: 10.1111/j.1532-5415.2004.52411.x. [DOI] [PubMed] [Google Scholar]
- 34.De Jong LD, Lavender AP, Wortham C, Skelton DA, Haines TP, Hill AM. Exploring purpose-designed audio-visual falls prevention messages on older people's capability and motivation to prevent falls. Health Soc Care Community. 2019;27(4):e471–e82. doi: 10.1111/hsc.12747. [DOI] [PubMed] [Google Scholar]
- 35.Maidan I, Freedman T, Tzemah R, Giladi N, Mirelman A, Hausdorff JM. Introducing a new definition of a near fall:intra-rater and inter-rater reliability. Gait Posture. 2014;39(1):645–7. doi: 10.1016/j.gaitpost.2013.07.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maki BE, Cheng KC, Mansfield A, Scovil CY, Perry SD, Peters AL, McKay S, Lee T, Marquis A, Corbeil P, Fernie GR, Liu B, McIlroy WE. Preventing falls in older adults:new interventions to promote more effective change-in-support balance reactions. J Electromyogr Kinesiol. 2008;18(2):243–54. doi: 10.1016/j.jelekin.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 37.Tokur D, Grimmer M, Seyfarth A. Review of balance recovery in response to external perturbations during daily activities. Hum Mov Sci. 2020;69:102546. doi: 10.1016/j.humov.2019.102546. [DOI] [PubMed] [Google Scholar]
- 38.Timsina LR, Willetts JL, Brennan MJ, Marucci-Wellman H, Lombardi DA, Courtney TK, Verma SK. Circumstances of fall-related injuries by age and gender among community-dwelling adults in the United States. PLoS One. 2017;12(5):e0176561. doi: 10.1371/journal.pone.0176561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rubenstein LZ. Falls in older people:epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 40.Komisar V, McIlroy WE, Duncan CA. Individual, task, and environmental influences on balance recovery:a narrative review of the literature and implications for preventing occupational falls. IISE Trans Occup Ergon Hum Factors. 2019;7(2):91–118. [Google Scholar]
- 41.McCrum C. Falls among older people-are intervention duration and specificity the keys to making a difference? BMJ. 2018;361:k2213. doi: 10.1136/bmj.k2213. [DOI] [PubMed] [Google Scholar]
- 42.Okubo Y, Sturnieks DL, Brodie MA, Duran L, Lord SR. Effect of Reactive Balance Training Involving Repeated Slips and Trips on Balance Recovery Among Older Adults:A Blinded Randomized Controlled Trial. J Gerontol A Biol Sci Med Sci. 2019;74(9):1489–96. doi: 10.1093/gerona/glz021. [DOI] [PubMed] [Google Scholar]
- 43.Soh SLH. Validation of a new scale of balance recovery confidence for community-dwelling older adults US:NIH U.S. National Library of Medicine ClinicalTrials.gov. 2020. [[cited 2021 9 January]]. Available from: https://clinicaltrials.gov/ct2/show/NCT04577365 .
- 44.Cameron ID, Stafford B, Cumming RG, Birks C, Kurrle SE, Lockwood K, Quine S, Finnegan T, Salkeld G. Hip protectors improve falls self-efficacy. Age Ageing. 2000;29(1):57–62. doi: 10.1093/ageing/29.1.57. [DOI] [PubMed] [Google Scholar]
- 45.Adams JMG, Tyson S. The Effectiveness of Physiotherapy to Enable an Elderly Person to Get up from the Floor. Physiotherapy. 2000;86(4):185–9. [Google Scholar]
- 46.Ioannidis JP, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, Schulz KF, Tibshirani R. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–75. doi: 10.1016/S0140-6736(13)62227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fors A. Person-centred care and self-efficacy - Experiences, measures and effects after an event of acute coronary syndrome. Sweden: University of Gothenburg. Sahlgrenska Academy; 2015. [Google Scholar]
- 48.Clancy A, Balteskard B, Perander B, Mahler M. Older persons'narrations on falls and falling-stories of courage and endurance. Int J Qual Stud Health Well-being. 2015;10:26123. doi: 10.3402/qhw.v10.26123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barry MJ, Edgman-Levitan S. Shared decision making - pinnacle of patient centered care. The New England Journal of Medicine. 2012;366(9):780–1. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 50.Kyte DG, Calvert M, Van der Wees PJ, Ten Hove R, Tolan S, Hill JC. An introduction to patient-reported outcome measures (PROMs) in physiotherapy. Physiotherapy. 2015;101(2):119–25. doi: 10.1016/j.physio.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 51.Streiner DL, Norman GR. A practical guide to their development and use. New York: Oxford University Press; 2008. Health measurement scales. [Google Scholar]
- 52.De Leeuw ED, Hox JJ, Dillman DA. International handbook of survey methodology. New York: Psychology Press; 2008. [Google Scholar]
- 53.Avin KG, Hanke TA, Kirk-Sanchez N, McDonough CM, Shubert TE, Hardage J, Hartley G Academy of Geriatric Physical Therapy of the American Physical Therapy A. Management of falls in community-dwelling older adults:clinical guidance statement from the Academy of Geriatric Physical Therapy of the American Physical Therapy Association. Phys Ther. 2015;95(6):815–34. doi: 10.2522/ptj.20140415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, De Vet HCW, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–57. doi: 10.1007/s11136-018-1798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lach HW. Self-efficacy and fear of falling:In search of complete theory. JAGS. 2006;54(2):381. doi: 10.1111/j.1532-5415.2005.00592_11_1.x. [DOI] [PubMed] [Google Scholar]
- 56.Edwards N, Lockett D. Development and validation of a modified falls-efficacy scale. Disability &Rehabilitation:Assistive Technology. 2008;3(4):193–200. doi: 10.1080/17483100801897198. [DOI] [PubMed] [Google Scholar]
- 57.Karström L, Yttergren M, Borgblad M, Stenström CH. The Falls-Efficacy Scale. Nordisk Fysioterapi. 2002;6(2):66–73. [Google Scholar]
- 58.Hill KD, Schwarz JA, Kalogeropoulos AJ, Gibson SJ. Fear of falling revisited. Arch Phys Med Rehabil. 1996;77(10):1025–9. doi: 10.1016/s0003-9993(96)90063-5. [DOI] [PubMed] [Google Scholar]
- 59.Tinetti ME, Powell L. Fear of falling and low self-efficacy:A cause of dependence in elderly persons. The Journals of Gerontology. 1993;48:35–8. doi: 10.1093/geronj/48.special_issue.35. [DOI] [PubMed] [Google Scholar]
- 60.Huang TT. Geriatric Fear of Falling Measure:Development and Psychometric Testing. Int J Nurs Stud. 2005;43(3):357–65. doi: 10.1016/j.ijnurstu.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 61.Velozo CA, Peterson EW. Developing meaningful fear of falling measures for community dwelling elderly. Am J Phys Med Rehabil. 2001;80(9):662–73. doi: 10.1097/00002060-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 62.Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction:The survey of activities and fear of falling in the Elderly (SAFFE) J Gerontol B-Psychol. 1998;53B(1):P43–P50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- 63.Landers MR, Durand C, Powell DS, Dibble LE, Young DL. Development of a scale to assess avoidance behavior due to a fear of falling:the fear of falling avoidance behavior questionnaire. Phys Ther. 2011;91(8):1253–65. doi: 10.2522/ptj.20100304. [DOI] [PubMed] [Google Scholar]
- 64.Bower ES, Wetherell JL, Merz CC, Petkus AJ, Malcarne VL, Lenze EJ. A new measure of fear of falling:psychometric properties of the fear of falling questionnaire revised (FFQ-R) Int Psychogeriatr. 2015;27(7):1121–33. doi: 10.1017/S1041610214001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peretz C, Herman T, Hausdorff JM, Giladi N. Assesing fear of failing:Can a short version of the activities-specific balance confidence scale be useful? Mov Disord. 2006;21(12):2101–5. doi: 10.1002/mds.21113. [DOI] [PubMed] [Google Scholar]
- 66.Filiatrault J, Gauvin L, Fournier M, Parisien M, Robitaille Y, Laforest S, Corriveau H, Richard L. Evidence of the psychometric qualities of a simplified version of the activities-specific balance confidence scale for community-dwelling seniors. Arch Phys Med Rehabil. 2007;88(5):664–72. doi: 10.1016/j.apmr.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 67.Simpson JM, Worsfold C, Fisher KD, Valentine JD. The CONFbal scale:a measure of balance confidence - a key outcome of rehabilitation. Physiotherapy. 2009;95(2):103–9. doi: 10.1016/j.physio.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 68.Rosengren KS, McAuley E, Mihalko SL. Gait adjustments in older adults:activity and efficacy influences. Psychol Aging. 1998;13(3):375–86. doi: 10.1037//0882-7974.13.3.375. [DOI] [PubMed] [Google Scholar]
- 69.McAuley E, Mihalko SL, Rosengren K. Self-efficacy and balance correlates of fear of falling in the elderly. Journal of Aging &Physical Activity. 1997;5(4):329–40. [Google Scholar]
- 70.Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercises on balance, mobility, and fall risk in community-dwelling older adults. Phys Ther. 1997;77(1):46–57. doi: 10.1093/ptj/77.1.46. [DOI] [PubMed] [Google Scholar]
- 71.Soh SLH, Lane J, Tan CW. Researcher as instrument:a critical reflection using nominal group technique for content development of a new patient-reported outcome measure. IPDJ. 2020;10(2):1–9. [Google Scholar]


