Abstract
Objectives:
Sarcopenia is prevalent among geriatric patients and it has a high rate of negative health related outcomes. Diagnostic and assessment approaches are not always feasible. The aim of the study was to detect a valid screening tool for sarcopenia that could be used easily in acute care setting.
Methods:
A cross sectional study was conducted in Geriatrics department, Ain Shams University Hospital. 127 inpatient elderly participants were recruited. Sarcopenia was defined according to the European Working Groups on Sarcopenia in Older People (EWGSOP) criteria as low skeletal muscle mass with either low handgrip strength or slow gait speed. Muscle mass was measured by bioelectrical impedance analysis (BIA). Two screening methods for sarcopenia were investigated, namely SARC-F questionnaire and Ishii equation including age, handgrip, and calf circumference (CC).
Results:
Both SARC-F questionnaire and Ishii equation can detect sarcopenia in both genders and both showed good agreement with the standard diagnostic method. Combining SARC-F to Ishii equation improved the diagnostic accuracy, with a higher sensitivity and specificity.
Conclusions:
SARC-F and Ishii equation could be used as a valid simple screening tool in acute hospital setting. Combing these two screening tools resulted in better diagnostic accuracy with higher sensitivity and specificity.
Keywords: Elderly, Hospitalized, Sarcopenia, Screening, Tool
Introduction
Sarcopenia is one of the new geriatric giants. Sarcopenia was defined as ‘’a syndrome characterized by progressive and generalized loss of skeletal muscle mass and strength with an appreciated risk of adverse outcomes including physical disability, poor quality of life and death’’[1].
Sarcopenia is an under-diagnosed. Elderly subjects who have a history of recent significant weight loss or those who appear malnourished including alcoholics and those with chronic medical conditions associated with loss of muscle (e.g. diabetes, chronic heart, lung, kidney and liver disorders) should be screened for sarcopenia[2].
The diagnosis of sarcopenia depends mainly on low muscle strength as a key characteristic of sarcopenia, uses detection of low muscle quantity and quality to confirm the sarcopenia diagnosis, and identifies poor physical performance as indicative of severe sarcopenia[3].
Muscle mass could be assessed by a wide range of techniques. Three imaging techniques have been used to estimate muscle mass: computed tomography (CT scan), magnetic resonance imaging (MRI) and dual energy X-ray absorptiometry (DXA)[4]. Bioelectrical impedance analysis (BIA) is used to estimate the volume of fat and lean body mass. The test is inexpensive, easy to use, readily reproducible, and appropriate for both ambulatory and bedridden patients. BIA measurement techniques have been found to correlate well with MRI predictions[5].
Muscle strength assessment could be done through handgrip strength measurement. Low handgrip strength (HGS) is a clinical marker of poor mobility and a better predictor of clinical outcomes than low muscle mass[6]. Physical performance could be assessed by the Short Physical Performance Battery (SPPB)[7], the usual gait speed[8], or the timed get-up-and-go (TUG) test[9].
Due to its clinical importance, screening methods for sarcopenia were created to avoid complex measurements, which may not be feasible everywhere and hard to apply on a wide base. Examples of these screening methods include SARC-F questionnaire[10-13] Ishii equation[14] and another tool by Goodman et al[15].
Although sarcopenia has clear deleterious effects, most of clinicians appear unaware of its existence and rarely make the diagnosis[16]. Clinicians need simple and quick tool to screen for sarcopenia. Most of the existing sarcopenia screening methods were not tested in acute setting. We aimed to detect a valid and feasible sarcopenia screening method to be used in everyday practice.
Material and methods
This was a single center cross sectional study that included 127 older adults, both men and women, 60 years old and above, who were admitted to Ain Shams University Hospital (El-Demerdash), Cairo, Egypt. All elderly patients who were admitted during the time from January 2018 to August 2018 were considered potentially eligible for the study. Then we excluded those patients who refused to participate in the study, patients with significant cognitive impairment (MMSE ≥24), delirium, patients with end stage disease or terminal illness, and patients on chemotherapy or other medications that could affect muscle assessment. Flowchart of subjects’ recruitment was illustrated (Figure 1).
Figure 1.
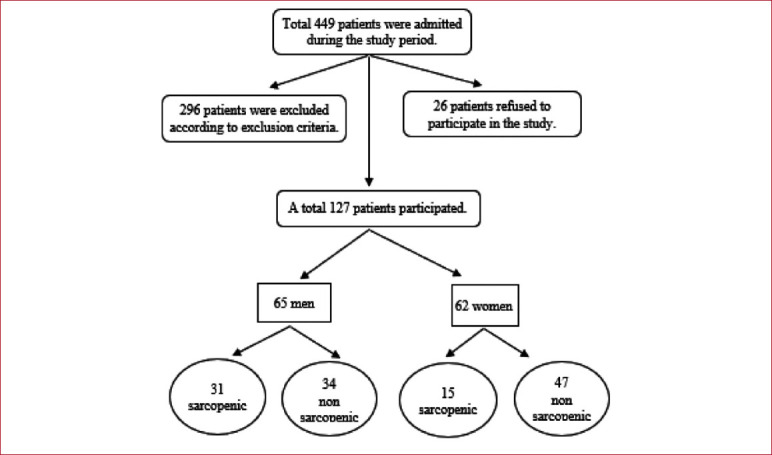
Flowchart of subject’s recruitment.
Working protocol
Screening for sarcopenia was done at first by using the two screening tools; SARC-F questionnaire and Ishii equation the include age, handgrip, and calf circumference (CC). Then, the diagnosis of sarcopenia was done using a standardized method. We were attempting to compare these two screening tools with the standardized method in diagnosis of sarcopenia. The standardized method is done according to European Working Groups on Sarcopenia in Older People (EWGSOP) in older population by measuring muscle mass, muscle strength and muscle performance.
The screening methods that we used were chosen out of a five known screening tests for sarcopenia; (a) SARC-F questionnaire[10,17]; (b) a screening grid for low muscle mass by age and body mass index (BMI)[15]; (c) Ishii equation for prediction of sarcopenia using age, handgrip strength and calf circumference[14]; (d) an anthropometric prediction equation in combination with a measure of muscle function (ASMPE)[18]; and (e) a two-step algorithm using gait speed assessment and handgrip strength[1].
A pilot study was done initially, in which these five screening methods were applied on 15 cases. The results of this pilot study were in favor of SARC-F questionnaire and Ishii equation. According to this pilot study, we found that SARC-F had the highest sensitivity (100%) compared to other screening tests, with high negative predictive value (100%). The sum score of the Ishii equation (including age/grip strength/CC) had the highest specificity (100%) with a high positive predictive value (100%).
Assessment / Diagnosis of sarcopenia
The workup for assessment /diagnosis of sarcopenia was carried out for every participant within the first 48 hours of admission to the inpatient unit in the Geriatrics department. All the assessment tests were performed during daytime from 09:00-16:00., by one of this study authors.
A. Diagnosis of sarcopenia was done according to EWGSOP by presence of low muscle mass and either low muscle strength or poor physical performance
1. Measurement of muscle mass:
This was done by bioelectrical Impedance Analysis (BIA) using beurer Glass diagnostic scale (BG42, Germany). It measures the volume of fat and the lean body mass. The subjects stood over the scale after filling in data as age, height, gender, and level of activity (scored form a minimum of 1 and a maximum of 5). Absolute muscle mass was measured, and total skeletal muscle mass index (TSMMI) was calculated. TSMMI=absolute muscle mass/ height in m2. The cut off points for low muscle mass was ≤10.75 kg/m2 in men and ≤6.75 kg/m2 in women[5].
2. Measurement of Muscle Strength:
A handheld dynamometer (Jamar Hydraulic hand dynamometer; 5030J1, USA) was used to assess muscle strength. Participants were instructed to keep their arms by the sides of their body. The participant squeezed the dynamometer with the dominant hand using maximum isometric effort. No other body movement was allowed and the better performance of the three trials was used[19]. Low muscle strength was defined as hand grip strength less than 30 kg in men and 20 kg in women[6].
3. Physical performance:
This was assessed by usual gait speed. Each Participant was instructed to walk over a 10-m straight course at their usual speed. Usual gait speed is derived from 4 m divided by the time in seconds spent in the middle 4 m. Good reproducibility of this measurement was reported previously. Usual gait speed values in the lowest quintile were classified as low physical performance. Cut-off values are 0.8 m/s for both genders)[6].
B. Sarcopenia screening:
This was done by using two screening tools: the Ishii equation and a SARC-F questionnaire.
(a) Ishii et al, Equation:
They found that the probability of sarcopenia could be estimated using a score chart, which includes three variables: age, grip strength, and calf circumference but essentially this tool worked best to rule-out those at risk of sarcopenia[14].
Score in men= [0.62×(age-64)] – [3.09×(grip strength-50)] – [4.64×(calf circumference-42)]. Score in women= [0.80×(age-64)] – [5.09×(grip strength-34)] – [3.28×(calf circumference-42)]. Sum score above 105 in men and 120 in women determines people having a high probability of sarcopenia[14]. Calf circumference is measured on the right calf, while the subject is sitting. The measuring tape is placed around the calf and moved up and down to locate the maximum circumference in a plane perpendicular to the long axis of the calf, then its wrapped around the calf but not tight and the calf circumference is recorded to the nearest 0.1 cm20.
(b) SARC-F questionnaire:
SARC-F questionnaire is a screening tool for sarcopenia. It Assesses 5 domains: Strength, assistance in walking, rising from a chair, climbing stairs, and history of falls[10].
Strength: how much difficulty do you have in lifting and carrying 5 Kg (None: 0; Some: 1; A lot or unable: 2); Assistance in walking: how much difficulty do you have walking across a room (none: 0; some: 1; a lot, use aids, or unable: 2); Rise from a chair: how much difficulty do you have transferring from a chair or bed (none: 0; some: 1; a lot or unable without help: 2); Climb stairs: how much difficulty do you have climbing a flight of 10 stairs (none: 0; some: 1; a lot or unable: 2); History of falls: how many times have you fallen in the past year (none: 0; 1-3 falls: 1; >4 falls: 2). Participants with a total score ≥4 were classified as positive screening for sarcopenia. SARC-F is recommended as a screening tool for sarcopenia in the EWGSOP2 consensus[3].
The strength of SARC-F screening tool is related to the simplicity of its questions, it does not require complex measurements of strength or gait speed. In addition, this tool has been linked to predicting clinical outcome and therefore, has clinical relevance when it comes positive[11]. SARC-F questionnaire has been validated in many studies among community dwellers elderly. The results of these studies are comparable and consistently showed good diagnostic accuracy characterized by low sensitivity and high specificity[21].
Covariates:
Socio-demographic variables as age and gender were assessed. Participants were screened for cognitive impairment by MMSE[22] and screened for depression by PHQ9 where scores of equal or more than three considered positive[23]. Functional assessment was done by ADL and IADL depending on the participants’ self-reported difficulty in performing different activities[24,25]. Nutritional assessment was done using the mini nutritional assessment form[26] and risk of falls[27].
Statistical analysis
Analysis of data was performed by using the Statistical Package for Social Science (SPSS16). Description of all data in the form of mean (M) and standard deviation (SD) for all quantitative variables was done. Frequency and percentage were done for all qualitative variables. Comparison between quantitative variables was done using t-test to compare two groups. Comparison of qualitative variables was done using the Chi-square or Fisher exact tests when appropriate. Significant level was measured according to P value (probability). P>0.05 is insignificant, p<0.05 is significant and p<0.01 is highly significant.
Results
This study included 65 men in whom 31 were diagnosed as sarcopenic and 62 women in whom 15 were diagnosed as sarcopenic by the standard diagnostic method. Sarcopenic participants were older and less educated (p<0.05). No significant differences between sarcopenic and non-sarcopenic participants regarding smoking, alcohol intake (p>0.05). Charlson comorbidity index was significantly higher in sarcopenic compared to non-sarcopenic only in women but not in men (p <0.05) (Table 1).
Table 1.
Demographic and clinical characteristics.
| Men (n=65) | Women (n=62) | ||||
|---|---|---|---|---|---|
| Sarcopenic (n=31) | Non-Sarcopenic (n= 34) | Sarcopenic (n= 15) | Non-Sarcopenic (n= 47) | ||
| Age in years (mean ± SD) | 70.23 ± 6.37 | 62.03 ± 3.01 | 67.33 ± 6.7 | 63.5 ± 3.1 | |
| p-value | <0.001 (T) | 0.004 (T) | |||
| Smoking | Non-smoker (N %) | 19 (61.3%) | 13 (48.2%) | 13 (86.7%) | 74 (100.0%) |
| Current smoker (N %) | 12 (38.7%) | 21 (61.8%) | 2 (13.3%) | 0 (0.0%) | |
| p-value | 0.175 (F) | 0.01 (F) | |||
| Alcohol intake | Consumer (N %) | 2 (6.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Non-consumer (N %) | 29 (93.5%) | 34 (100.0%) | 15 (100.0%) | 47 (100.0%) | |
| p-value | 0.224 (F) | --- | |||
| Years of education | < 6 years | 14 (45.2%) | 3 (8.8%) | 13 (86.7%) | 13 (28.3%) |
| ≥ 6 years | 17 (54.8%) | 31 (91.2%) | 2 (13.3%) | 33 (71.7%) | |
| p-value | 0.001 (F) | 0.000 (F) | |||
| Charlson Comorbidity index | 2.77 ± 1.59 | 2.26 ± 1.40 | 3 ± 1.1 | 1.19 ± 0.97 | |
| p-value | 0.174 (T) | 0.001 (T) | |||
Data are presented as mean ± SD or %. Independent student ‘t’ test (t), Chi-square test (c), and Fisher’s Exact test (F) were used. Significant p-value if p<0.05.
SARC-F questionnaire’s total score could differentiate sarcopenic from non-sarcopenic in both men and women. SARC-F questionnaire’s individual items were also significantly different in both genders (P<0.05). Ishii equation showed a statistically significant difference between sarcopenic and non-sarcopenic in both men and women as well (Table 2).
Table 2.
SARC-F questionnaire and Equation among participants.
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Sarcopenic (by standard) (n= 31) | Non-sarcopenic (by standard) (n= 34) | p-value | Sarcopenic (by standard) (n=15) | Non-sarcopenic (by standard) (n= 47) | p-value | |||
| SARCF total score (mean± SD) | 4.52 ± 2.64 | 0.56 ± 1.24 | <0.001(T) | 5.8 ± 2.17 | 2.3 ± 1.5 | <0.001(T) | ||
| SARC-F Items | Strength score | 0.00 | 8 (25.8%) | 31 (91.2%) | <0.001(C) | 1 (6.7%) | 18 (38.3%) | 0.000(c) |
| 1.00 | 14 (45.2%) | 3 (8.8%) | 4 (26.7%) | 27 (57.4%) | ||||
| 2.00 | 9 (29.0%) | 0 (0.0%) | 10 (66.7%) | 2 (4.3%) | ||||
| Assistance in walking score | 0.00 | 12 (38.7%) | 32 (94.1%) | <0.001(C) | 1 (6.7%) | 38 (80.9%) | 0.001(F) | |
| 1.00 | 16 (51.6%) | 2 (5.9%) | 14 (93.3%) | 9 (19.1%) | ||||
| 2.00 | 2 (6.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||||
| Rise from chair score | 0.00 | 14 (45.2%) | 32 (94.1%) | <0.001(C) | 2 (13.3%) | 31 (66%) | 0.001(F) | |
| 1.00 | 15 (48.4%) | 2 (5.9%) | 13 (86.7%) | 16 (34%) | ||||
| 2.00 | 2 (6.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||||
| Climbing stairs score | 0.00 | 1 (3.2%) | 26 (76.5%) | <0.001(C) | 0 (0.0%) | 6 (12.8%) | 0.005(F) | |
| 1.00 | 17 (54.8%) | 6 (17.6%) | 6 (40%) | 37 (78.7%) | ||||
| 2.00 | 13 (41.9%) | 2 (5.9%) | 9 (60%) | 4 (8.5%) | ||||
| Falls score | 0.00 | 16 (51.6%) | 34 (100.0%) | <0.001(C) | 8 (53.3%) | 44 (93.6%) | <0.001(F) | |
| 1.00 | 7 (22.6%) | 0 (0.0%) | 3 (20%) | 0 (0%) | ||||
| 2.00 | 8 (25.8%) | 0 (0.0%) | 4 (26.7%) | 3 (6.4%) | ||||
| Screening by SARC-F | Sarcopenic | 20 (64.5%) | 3 (8.8%) | <0.001(F) | 14 (93.3%) | 10 (21.3%) | 0.001(F) | |
| Not sarcopenic | 11 (35.5%) | 31 (91.2%) | 1 (6.7%) | 37 (78.7%) | ||||
| Equation Score (mean± SD) | 133±36.9 | 59.2±43 | 0.000(T) | 138±19 | 82.7±29.7 | 0.000(T) | ||
| Screening by Equation | Sarcopenic (N %) | 27 (87.1%) | 9 (26.5%) | <0.001(F) | 12 (80%) | 4 (8.5%) | 0.002(C) | |
| Not sarcopenic (N %) | 4 (12.9%) | 25 (73.5%) | 3 (20%) | 43 (91.5%) | ||||
Data are presented as mean ± SD or %. Independent student ‘t’ test (T), Chi-square test (C), and Fisher’s Exact test (F) were used. Significant p-value if p<0.05.
All muscle assessment tools (namely, hand grip, BMI, calf circumference (CC), BIA, and gait speed) were significantly affected in sarcopenic participants in both gender (p<0.05). All these differences were statistically significant except gait speed in women (Table 3).
Table 3.
Muscle assessment tools for all participants.
| Men | Women | ||||||
|---|---|---|---|---|---|---|---|
| Sarcopenic (by standard) (n= 31) | Non-sarcopenic (by standard) (n= 34) | p-value | Sarcopenic (by standard) (n= 15) | Non-sarcopenic (by standard) (n= 47) | p-value | ||
| Hand grip (Kg) (mean± SD) | 20.32 ± 8.06 | 36.35 ± 11.34 | <0.001(T) | 11± 3.9 | 19.6± 5.1 | 0.01(T) | |
| Hand grip cut off | Sarcopenic (N %) | 28 (90.3%) | 7 (20.6%) | <0.001(C) | 14 (93.3%) | 16 (34%) | 0.001(F) |
| Non- sarcopenic (N %) | 3 (9.7%) | 27 (79.4%) | 1 (6.7%) | 31 (66%) | |||
| Body mass index (BMI) (Kg/m2) (mean± SD) | 23.48 ± 3.02 | 27.72 ± 4.45 | 0.000(T) | 27.8 ± 5.1 | 34.58 ± 6.4 | 0.000(T) | |
| Calf muscle circumference (cm) (mean± SD) | 33.94 ± 4.47 | 38.06 ± 2.99 | <0.001(T) | 36.5± 2.6 | 38.9 ± 4.2 | 0.03(T) | |
| Bioelectrical impedance analysis (BIA) (mean± SD) | 8.50 ± 1.08 | 9.92 ± 1.64 | <0.001(T) | 6.8 ± 1.8 | 9.5 ± 1.48 | <0.001(T) | |
| BIA cut off | Sarcopenic (N %) | 31 (100.0%) | 20 (58.8%) | <0.001(C) | 7 (46.7%) | 0 (0%) | <0.001(F) |
| Non-sarcopenic (N %) | 0 (0.0%) | 14 (41.2%) | 8 (53.3%) | 47 (100%) | |||
| Gait speed (m/sec) (mean± SD) | 0.44 ± 0.21 | 0.84 ± 0.20 | <0.001(T) | 0.36 ± 0.21 | 0.59 ± 0.21 | 0.001(T) | |
| Gait speed cut off | Sarcopenic (N %) | 28 (90.3%) | 6 (17.6%) | <0.001(C) | 14(93.3%) | 40 (85.1%) | 0.372(F) |
| Non-sarcopenic (N %) | 3 (9.7%) | 28 (82.4%) | 1 (6.7%) | 7 (14.9%) | |||
Data are presented as mean ± SD or %. Independent student ‘t’ test (t), Chi-square test (C), and Fisher’s Exact test (F) were used. Significant p-value if p<0.05.
Table 4.
ROC curve analysis for the screening tools used for detecting sarcopenia.
| Tools | AUC (95% CI) | Cut-off value | Senst. | Specif. | PPV | NPV | p-value | |
|---|---|---|---|---|---|---|---|---|
| SARC-F | Men | 0.93 (0.84 to 0.98) | ≥ 3 | 62% | 91% | 90.9% | 74.4% | 0.0001 |
| Women | 0.93(0.8374 to 1) | ≥ 4 | 93% | 80% | 58.3% | 97.4% | 0.001 | |
| Equation | Men | 0.93 (0.83 to 0.98) | ≤100 | 87% | 75% | 75% | 86% | 0.00 |
| Women | 0.86 (0.79 to 0.98) | ≤115 | 80% | 78% | 93% | 76.6% | 0.001 | |
| SARC-F + Equation | Men | 0.92(0.87-0.97) | 0.38 | 96% | 75% | 91.3% | 76.2% | 0.000 |
| Women | 0.95(0.89-1) | 0.5 | 96% | 87% | 86.7% | 95.7% | 0.001 | |
| CC | Men | 0.77 (0.65 to 0.86) | ≤36 | 77.4% | 70.6% | 70.6% | 77.4% | 0.001 |
| Women | 0.63 (0.4 to 0.67) | ≤36.5 | 60% | 47% | 40% | 77.2% | 0.76 | |
| SARC-F + CC | Men | 0.93(0.89-0.98) | 0.41 | 96% | 75% | 91% | 76% | 0.000 |
| Women | 0.95(0.88-1) | 0.43 | 95% | 80% | 85.7% | 93.8% | 0.00 | |
ROC; receiver operating characteristic, AUC; Area under the curve, CC; Calf Circumference, PPV; positive predictive value, NPV; negative predictive value.
Comparing the screening methods (SARC-F and Ishii equation) to the standard diagnosis for sarcopenia showed good agreement with the standard diagnostic method. SARC-F questionnaire had agreement of 78.46% in men and 82.25% in women, while the equation had agreement of 80% in men and 88% in women.
A receiver operating characteristic curve (ROC curve) was performed to reveal accuracy of screening tests in detecting sarcopenia. SARC-F showed a good discriminative property to predict sarcopenia in general nonetheless with a better performance in women than in men. Ishii equation showed a good discriminative property in both genders likewise. Combining these two screening methods improved the diagnostic accuracy in detecting sarcopenia, with a higher sensitivity and specificity in both genders. While calf circumference alone was found to be just a fair discriminative test to detect sarcopenia only in men (Τable 4).
Discussion
Sarcopenia is an important and prevalent health problem in older adults that carries a high rate of negative health related outcomes. In this study, we investigated the two well-known screening tools for sarcopenia, SARC-F and Ishii et al equation to detect a simple and valid screening tool that could be used in recognition of sarcopenia in acute hospital setting aside from the standard diagnostic methods.
Regarding SARC-F tool, we found that SARC-F scores were significantly higher in sarcopenic compared to non-sarcopenic participants. Besides, SARC-F’s individual items (namely, strength score, assistance in walking score, rise from chair score, climbing stairs score, and falls score) showed significant differences between sarcopenic and non-sarcopenic participants in both men and women.
In the current study, SARC-F questionnaire showed good agreement with the standard method for diagnosis of sarcopenia in both men and women (78.46% in men and 82.25% in women). ROC curve analysis of SARC-F revealed that the area under the curve was the same in both genders (0.93). The sensitivity was higher in women compared to men (93% vs 62% respectively), while the specificity was higher in men compared to women (91% vs 80% respectively). This could be related to the subjective element of the test and little prevalence of sarcopenia among picked women in this study.
In agreement with the previous findings, Malmstrom et al., 2016[10] reported that SARC-F questionnaire is internally consistent and valid for detecting persons at risk for adverse outcomes from sarcopenia. Moreover, SARC-F questionnaire has been validated as a screening tool among community dwellers elderly by Woo et al, and their results showed good diagnostic accuracy, low sensitivity, and high specificity[28].
Additionally, Yang et al, 2018 found that using only 3 items (strength, ability to climb stairs and need for assistance in walking) of the 5 item questionnaire improved the diagnostic area under the curve values and had the highest predictive value of adverse outcomes[17]. SARC-F questionnaire is easier and requires no instruments and highly recommended by EWGSOP and Society of Sarcopenia, cachexia and Wasting Disorders[16,18].
The second screening tool addressed in our study was the equation of Ishii et al. This equation tool worked best to rule-out those at-risk of sarcopenia as was proved by the study done by Ishii et al[14], that resulted in selection of three easily obtainable variables (age, grip strength and calf circumference) that were significantly associated with sarcopenia. This model with the three variables had excellent discrimination for sarcopenia based on more stringent cut-off levels for grip strength and usual gait speed. However, it needs complex calculation and time.
In our study, we found that the equation scores showed significant differences between sarcopenic and non-sarcopenic participants in both genders. The agreement between the equation and the standard diagnostic method was also found good, with better agreement in women compared to men (86% vs 80%). The ROC curve analysis of the equation for sarcopenia screening showed sensitivity at 87% and specificity 80% in men participants. while in women participants it showed a bit lower results with sensitivity at 80% and specificity 78%. Meanwhile, the area under the curve was 0.93, 0.86 in men and women, respectively.
We combined the two screening tools (Ishii et al equation and SARC-F questionnaire), as a trial to improve the screening performance, we found that sensitivity increased to 96% in both men and women, while specificity improved to 75%, 87% in men and women respectively. Also, to improve the specificity of SARC-F questionnaire, we add calf circumference measurement to SARC-F questionnaire, and this improved the screening performance in both men and women as sensitivity raised to 96% in men (area under the curve: 0.93 (95% CI 0.89- 0.98), and 95% in women (area under the curve: 0.95 (95% CI 0.88-1). Our results were similar to Barbosa et al[29], and Bahat et al[30], who had the same results when they combined SARC- F to calf circumference as this increased diagnostic accuracy of this screening test among community dwellers.
Based on Area under the Curve (AUC) calculation, both SARC-F and the equation of Ishii et al showed excellent discrimination property between sarcopenic and non-sarcopenic participants in men (AUC=0.93 for both tests), while in women, SARC-F showed a better discriminative property compared to the equation (AUC=0.93 vs 0.86).
As a conclusion, both SARC-F questionnaire and Ishii equation are easy and reliable screening methods for sarcopenia in acute hospital settings. Combing SARC-F questionnaire and the equation improved diagnostic accuracy in both genders. Also, combined SARC-F questionnaire with Calf Circumference measurement improved diagnostic accuracy in both genders. The Ishii equation was reliable screening test in both genders as an objective screening tool. Combining two screening methods, either SARC-F plus the equation or SARC-F plus CC measurement increase the diagnostic property for detecting sarcopenia. The clinical benefit of implementing this simple and cheap screening tools is detection of sarcopenia among hospitalized, elderly patients, especially in case of patient’s inability to stand unsupported on BIA device or unavailability of diagnostic devices such as ultrasound or CT. Early diagnosis of sarcopenia among older adult patients, in acute hospital settings, will result in early implementation of the proper intervention plan aiming to improve their functional status and health-related outcome.
The main limitations in our study were its relatively small sample size and the exclusion criteria that resulted in excluding those subjects who were unable to complete the tests for assessment of sarcopenia such as terminally ill patients, patients with end-organ failure, and those receiving chemotherapy or other medications that potentially have a negative effect on muscle. The exclusion of such high number of the admitted patients (total 296) lowered our sample size and may cause underestimation of sarcopenia in our study.
Clinical application
We need to incorporate an objective sarcopenia screening tool to comprehensive geriatric assessment for elderly.
Ethical approval
Approval was obtained from the ethics committee of Ain Shams University. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgements
Authors appreciate the role of the elderly participants who participated effectively in this research. Appreciation to the Geriatrics and gerontology department, Ain Shams University hospitals, Cairo, Egypt, for facilitating the procedures of this work.
Footnotes
Edited by: Yannis Dionyssiotis
References
- 1.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia:European consensus on definition and diagnosis:Report of the European Working Group on Sarcopenia in Older People. Age Aging. 2010;39(4):412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali S, Garcia JM. Sarcopenia, cachexia and aging:diagnosis, mechanisms and therapeutic options-a mini-review. Gerontology. 2014;60(4):294–305. doi: 10.1159/000356760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cruz-Jentoft AJ, Landi F, Schneider SM, Clemente Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults:a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS) Age Ageing. 2014;43(6):748–59. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chien MY, Huang TY, Wu YT. Prevalence of sarcopenia estimated using a bioelectrical impedance analysis prediction equation in community-dwelling elderly people in Taiwan. J Am Geriatr Soc. 2008;56(9):1710–15. doi: 10.1111/j.1532-5415.2008.01854.x. [DOI] [PubMed] [Google Scholar]
- 5.Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol. 2000;89(2):465–71. doi: 10.1152/jappl.2000.89.2.465. [DOI] [PubMed] [Google Scholar]
- 6.Lauretani F1, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, et al. Age-associated changes in skeletal muscles and their effect on mobility:an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95(5):1851–60. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- 7.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function:association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology. 1994;49(2):85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 8.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability:consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. The Journals of Gerontology Series A. J Gerontol A Biol Sci Med Sci. 2000;55(4):221–31. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 9.Mathias S, Nayak US, Isaacs B. Balance in elderly patients:the“get-up and go”test. Arch Phys Med Rehabil. 1986;67(6):387–9. [PubMed] [Google Scholar]
- 10.Malmstrom TK, Morley JE. SARC-F:a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14(8):531–32. doi: 10.1016/j.jamda.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Cao L, Chen S, Zou C, Ding X, Gao L, Liao Z, et al. A pilot study of the SARC-F scale on screening sarcopenia and physical disability in the Chinese older people. J Nutr Health Aging. 2014;18(3):277–83. doi: 10.1007/s12603-013-0410-3. [DOI] [PubMed] [Google Scholar]
- 12.Parra-Rodriguez L, Szlejf C, Garcia-Gonzalez AI, Malmstrom TK, Esteban Cruz-Arenas E, Oscar Rosas-Carrasco O. Cross-cultural adaptation and validation of the Spanish-language version of the SARC-F to assess sarcopenia in Mexican community-dwelling older adults. J Am Med Dir Assoc. 2016;17(12):1142–11. doi: 10.1016/j.jamda.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Rolland Y, Dupuy C, Abellan Van Kan G, Cesari M, Vellas B, Faruch M, et al. Sarcopenia screened by the SARC-F questionnaire and physical performances of elderly women:A cross-sectional study. J Am Med Dir Assoc. 2017;18(10):848–52. doi: 10.1016/j.jamda.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Ishii S, Tanaka T, Shibasaki K, Ouchi Y, Kikutani T, Higashiguchi T, et al. Development of a simple screening test for sarcopenia in older adults. Geriatr Gerontol Int. 2014;14(1):93–101. doi: 10.1111/ggi.12197. [DOI] [PubMed] [Google Scholar]
- 15.Goodman MJ, Ghate SR, Mavros P, Sen S, Marcus RL, Joy E, et al. Development of a practical screening tool to predict low muscle mass using NHANES, 1999–2004. J Cachexia Sarcopenia Muscle. 2013;4(3):187–97. doi: 10.1007/s13539-013-0107-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. The Lancet. 2019;393(10191):2636–46. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 17.Yang M, Hu X, Xie L, Zhang L, Zhou J, Lin J, et al. SARC-F for sarcopenia screening in community-dwelling older adults:Are 3 items enough? Medicine. 2018;97(30):e11726. doi: 10.1097/MD.0000000000011726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, et al. International clinical practice guidelines for sarcopenia (ICFSR):Screening, Diagnosis and Management. Journal Nutr Health Aging. 2018;22(10):1148–61. doi: 10.1007/s12603-018-1139-9. [DOI] [PubMed] [Google Scholar]
- 19.Yu S, Appleton S, Chapman I, Adams R, Wittert G, Visvanathan T, et al. An anthropometric prediction equation for appendicular skeletal muscle mass in combination with a measure of muscle function to screen for sarcopenia in primary and aged care. J Am Med Dir Assoc. 2015;16(1):25–30. doi: 10.1016/j.jamda.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 20.Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies:towards a standardized approach. Age Ageing. 2011;40(4):423–9. doi: 10.1093/ageing/afr051. [DOI] [PubMed] [Google Scholar]
- 21.Rolland Y, Lauwers-Cances V, Cournot M, Nourhashémi F, Reynish W, Rivière D, et al. Sarcopenia, calf circumference, and physical function of elderly women:a cross-sectional study. J Am Geriat Soc. 2003;51(8):1120–4. doi: 10.1046/j.1532-5415.2003.51362.x. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. Mini Mental State:a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams J. Validation and utility of a self-report Version of PRIME-MD:the PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 24.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged:The index of ADL:A standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–19. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 25.Lawton MP, Brody EM. Assessment of older people:self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 26.Vellas B, Villars H, Abellan G, Soto ME, Rolland Y, Guigoz Y, et al. Overview of the MNA - Its History and Challenges. J Nutr Health Aging. 2006;10(6):456–65. [PubMed] [Google Scholar]
- 27.Podsiadlo D, Richardson S. (1991):“The timed 'Up &Go':A test of basic functional mobility for frail elderly persons”. J Am Geriat Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 28.Woo J, Leung J, Morley JE. Validating the SARC-F:a suitable community screening tool for sarcopenia. J Am Med Dir Assoc. 2014;15(9):630–34. doi: 10.1016/j.jamda.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 29.Barbosa-Silva TG, Menezes AM, Bielemann RM, Malmstrom TK, Gonzalez MC. Enhancing SARC-F:Improving sarcopenia screening in the clinical practice. J Am Med Dir Assoc. 2016;17(12):1136–41. doi: 10.1016/j.jamda.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Bahat G, Oren MM, Yilmaz O, Kılıç C, Aydin K, Karan MA. Comparing SARC-F with SARC-CalF to screen sarcopenia in community living older adults. J Nutr Health Aging. 2018;22(9):1034–38. doi: 10.1007/s12603-018-1072-y. [DOI] [PubMed] [Google Scholar]


