Abstract
Social capital aspects are playing an important role in activities of daily living (ADL) performance, thus on independent living. This paper was aimed to present an overview of the associations and adverse effects between social capital aspects and disability in ADL and health-related quality of life (HRQoL) in an older population aged 65 years old and over. Α scoping review was designed following the guidelines of PRISMA Extension for Scoping Reviews (PRISMA-ScR) and the review was conducted by 3 authors. A total of 185 primary studies were extracted and, finally, 40 studies did meet the inclusion criteria and critically appraised in two main categories; Category 1(29 studies) ‘social capital and disability in ADL’ deducing that as greater a social capital as better ADL performance and Category 2 (11 studies) ‘Social capital and HRQoL’ concluding that people 65 years old and over with lower social capital were presented with a poor HRQoL. Study synthesis highlights the impact of social capital suggesting that nurses caring for older people must focus on their engagement in terms of social diversity and trust in the community.
Keywords: Disability in ADL, Healthy aging, Health-related quality of life, Independence, Social capital
Introduction
Rationale
Aging may lead to the development of disability in ADL, which consists of the difficulty or need of help for the individual to perform typical self-care activities (the basic activity of daily living, or ADL) or more complex ones (the instrumental ADL, or IADL). On the one hand, predisposing factors (sociodemographic characteristics), intraindividual (lifestyle, behavior or diseases) and external factors (interventions from health services, use of medication, external support in conjunction with the natural and social environment) affect the disability process[1].
On the other hand, social capital is described as a collection of norms, networks and trust that may improve the effectiveness of the community[2]. Social capital may be defined as the characteristics of social organizations such as trust, norms and social networks that facilitate coordinated action and bring benefits which can be determined through social relationships[3]. Although social capital is seen as a multidimensional concept, the two most commonly used indicators of social capital in the empirical literature are participation in voluntary associations and generalized social trust[4]. According to the Puntam[2], social capital is distinguished in the bonding social capital which refers to trust and cooperation among members of a network and is characterized by strong ties and close social contacts and the bridging social capital which mentions to relationships of respect and reciprocity between people who are not identical in sociodemographic terms (e.g., social identity, age, ethnicity, etc.)[5]. The first form of social capital “bonding social capital” includes three elements: social participation (e.g., how often they go to church or participate in leisure activities outside the home if during the last month to have someone visit or they has visited someone), social diversity (if grandchildren, siblings, relatives, friends or acquaintances have visited the last month) and the level of satisfaction with social relations. The second form of social capital “bridging social capital” refers to the level of crime and violence in the municipalities, and the linkage of mutual trust within a community[6]. Additionally, Szreter and Woolcock[5] introduced the concept of “Social Cohesion” (linking-social capital) which refers to relationships of respect and trust of people with formal and institutionalized power in the community. Specifically, linking social capital includes four elements: expression of trust to the home care services in the municipality, voting rate for the senior council in the community, the politicians’ attitude towards older people in the community and health and social expenses for people >65 years old in the community[6].
In the international literature, there is limited evidence for the positive links between social capital and health of older people in the general context of developing countries. Indeed, many of the details of recent research in China, where measurements of social capital have been found to have different effects, which depend on how one measures the social capital and the used measure of health, stressing the need to take into account specific circumstances[7]. Especially, higher social capital indicators contribute to the “better” mental and physical quality of life (QoL)[8]. Social engagement was important to maintain and strengthen the social ties that promote health and functional well-being[9]. The non-participation and mistrust in the community were associated with disability in ADL and/or physical limitations[10].
Objectives
The initiatives of the European Innovation Partnership on Active and Healthy Ageing (EIPonAHA), pointed out that a necessary condition for achieving the goal of active and healthy ageing is “a person to live independently”[11]. On the other hand, “engagement” of an older person in social activities in the community required a “physical capacity”. Therefore, we hypothesized that high social capital may have an important role in this assumption regarding active role living a healthier, more active and independent living.
The aim of this paper is to summarize and synthesize new evidence in the field of active and healthy ageing highlighting possible associations and adverse effects between social capital aspects and disability in ADL and HRQoL in an older population aged 65 years old and over.
Methods
Research strategy
This scoping review was conducted according to guidelines PRISMA Extension for Scoping Reviews (PRISMA-ScR)[12], to identify articles published from 2006 to 2020 that explore the association between social capital and disability in ADLs; a review protocol was developed in a three-step search process.
The study’s eligibility criteria included published articles; investigated the relationship between social capital and disability in ADLs; original articles in a cross-section and prospective design to obtain only primary research data focusing on ADL indexes (Barthel, SMAF, Katz index); participants aged over 65 years and the free full text written in the English language. Given the fact that chronic conditions, in particular cerebrovascular disease, arthritis and coronary heart disease, are important predictors of functional limitation, articles concerning these chronic conditions were not excluded but only the original studies which did control for them were included.
To provide a comprehensive approach and data analysis[13] in the field of active and healthy ageing we focused mainly on primary and prospective studies. Within a framework, the search strategy was properly configured to initially identify the main initiatives of the EIPonAHA[11]. Specifically, the search followed the inclusion criteria that have been raised using Medical Subjects Headings terms, such as: ‘ADL’ or ‘Functional decline’ or ‘disability’, and terms ‘Social capital’ ‘bonding’, ‘bridging’, ‘linking’ referred to aspects of social capital. Moreover, the term both ‘HRQoL’ and ‘QoL’ were also used in the advanced search method and applying filters (AND, OR, NOT). Interestingly, data were mainly retrieved by PubMed and Scopus databases due to their biomedical character.
In the first step, a limited primary search of the PubMed and Scopus databases was carried out to extract articles based on our MeSH terms included in the ‘title’, the ‘abstract’ and ‘keywords’ with special attention to ‘disability in ADL’, ‘independence’ and ‘QoL’ were applied. Secondly, the search aimed to identify the keywords of the text associated with aspects of social capital [bonding, bridging and linking] following the recommendation of Poulsen et al[6]. More specifically, the following pattern was applied:
‘social capital’ [Title/Abstract] OR ‘social participation’ [Title/Abstract] OR ‘social diversity’ [Title/Abstract] OR ‘satisfaction with social relationships’ [Title/Abstract] OR ‘bridging social capital-social support '[Title/Abstract] OR 'linking social capital-social cohesion’ [Title/Abstract] AND ‘activities of daily living-ADL’ [Title/Abstract] OR ‘independence’ [Title/Abstract] OR ‘health-related quality of life-–‘physical and mental health’ [Title/Abstract] AND ‘older adults’ [Title/Abstract] OR ‘elderly’ [Title/Abstract] OR ‘aged’ [Title/Abstract]. Keywords combined in searches.
In the second step extensive electronic search was conducted using the same search strategy in both databases, where if the initial review of the first step suggested that the study was ‘relevant’, then in this second step the “full text” of the article was under review for final selection.
In the third step, the articles retrieved, stored and were documented for the final selection. Procedurally, they were checked for duplicate studies which were excluded and then reviewed in order to withdraw any irrelevant articles that arose. If it was difficult to determine the relevance of the article based only on its summary, the full text was recovered and examined by two independent researchers using the inclusion criteria. Disagreements among researchers resolved through discussion and constructive argument.
Data extraction and analysis
To derive data, a summary table was developed and piloted by the research team. Then based on the table, the full text of the included articles was tested and data was extracted by the three authors. The lack of consensus between the three researchers was resolved with full discussion and argument. The data extracted included the title, the year of publication of the article, the study design, the characteristics of participants in the study, the sources of data, the validity and reliability of the design tools, the measurements of social capital, the disability in ADL and the HRQoL.
The data obtained are analyzed using a narrative presentation. As the studies were highly heterogeneous, a meta-analysis was not conducted. The findings drawn from the data of studies that critically analyzed are presented in the respective tables, providing useful information on the “home country”, the “number and characteristics of the ‘participants’ studied”, the “instrument”, the “study type” and the “main findings”. The studies reviewed were published between 2006 and 2020 and included 34 cross-sectional and 6 prospective cohort studies
Results
A total of 40 articles were included in this scoping review. In the flow diagram (Figure 1) the selection process is shown in studies according to the criteria placed.
Figure 1.
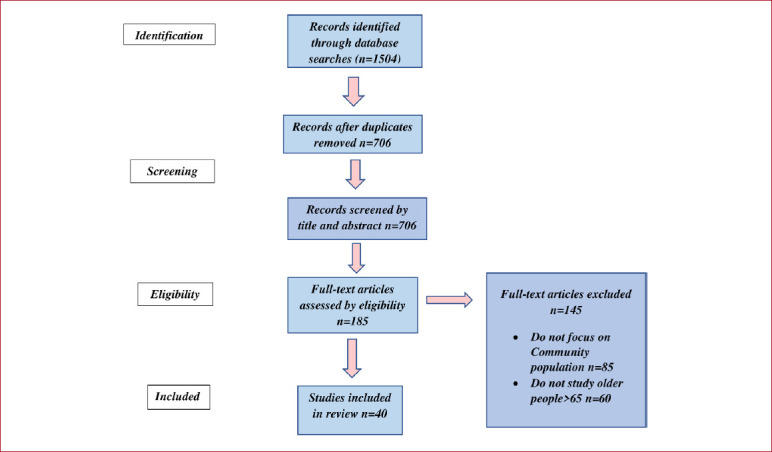
PRISMA flow Diagram for Literature.
The Methodological quality of the included studies
The evaluation of the quality of the studies was conducted using the quality assessment tool of descriptive and cross-sectional studies (QAT-OCCSS, Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies)[14]. The QAT-OCCSS is an assessment tool that sorts 14-point quality study based on several methodological and mentioned parameters. The evaluation of the quality of each study was conducted by the two independent writers according to the guidelines on evaluation instructions.
The methodological quality of the included studies was generally low (total quality score 3-8 with an average of 5,8 from a possible average 14). Concerning the specific points mentioned in QAT-OCCSS, all studies (100%) had clearly formulated a research question, clearly identified the study population, and adequately described the inclusion and exclusion criteria. Additionally, none of the studies did attempt to justify the sample size or the power of the analysis.
Characteristics of included studies
The majority of studies were conducted in the USA (8 articles), in Europe (9 articles), in Japan (6 articles) and China (5 articles). As far as deviations of the outcome, the disability in ADL was the primary outcome in 29 articles while the HRQoL was evaluated in 11 articles although mentioned in previous studies. The size of the study sample ranged from 155-33.744 persons, while the age range of participants from 60-100 years.
The included studies evaluated the disability in ADL performance, functional capacity, independence exclusively with instruments such as ADL, IADL, Katz Index, the Barthel Index or the Functional Autonomy Measurement System (SMAF).
In particular, the Activity of Daily Living Index (to being fed one by himself, moving from bed to chair, getting dressed, walking between two rooms on the same floor, using the toilet and bathe) is a commonly used tool to assess functional disability in geriatric populations. Additionally, IADL Index is used to measure IADL (to prepare the food itself, taking care of his own money, performing basic household chores, taking medications and shopping by himself).
Furthermore, the Katz Index is the most appropriate tool to determine the functional status of the individual. The Index assesses the adequacy of executing six functions (doing one bathroom, getting dressed, going to the toilet, move, eat alone, and have voluntary control of urination and defecation)[15].
On the other hand, the Barthel ADL index is commonly used to assess the degree of independence from any help, physical or verbal, any size and for any reason. In particular, the Index considers “what the patient does” and not “what the patient could do”. The need for supervision renders the person non-independent. The greatest advantage of the Barthel Index is its simplicity[16].
Additionally, the Functional Autonomy Measurement System (SMAF) is a 29-item scale developed following the classification of impotence by the World Health Organization. It measures functional ability in five areas: ADL (7 items), mobility (6 items), communication (3 items), mental functions (5 items) and IADL (8 items)[17].
Finally, studies reported on the relationship between social capital with HRQoL were also included. More specifically, it is mainly the QoL rating scales developed by the World Health Organization as the Older’s People QoL Questionnaire (OPQOL) and the Short Form-36 (SF-36). All questionnaires were focused on two areas: physical and mental health[18].
From the methodological approach applied, 40 articles were derived which were classified into two main categories based on indexes that were used for the assessment of the relation between social capital and disability in ADL performance. Specifically, it resulted in category a) Social Capital and disability in ADL (Table 1) and b) Social Capital and HRQoL (Table 2). Moreover, it was considered appropriate to present separate the aspects of Social capital in each of the categories which are directly linked to the achievement of the target process for active and healthy ageing (Table 3 and 4).
Table 1.
Presentation of the main findings between social capital and disability in ADL/IADL.
| Original research | Participants | Instrument | Study type | Main findings |
|---|---|---|---|---|
| Aranda et al[24] 2011, US | 2,069 Mexico-Americans aged >75 years old | ADL Index | Prospective | The protective factors of the neighborhood effect against increased vulnerability condition are positively associated with functional capacity |
| Bowling et al[25] 2006, UK | 999 people aged>65 years old | ADL Index | Cross-sectional | High social participation and emotional support were strongly and independently associated with a reduced functional disability |
| Brown et al[26] 2008, US | 273 Hispanic people aged >70 years | ADL Index | Cross-sectional | Neighborhood may be more walkable when allows more personal interactions that increase physical functionality |
| Chen et al[27] 2015, China | 14292 people aged ≥60 years old | Katz Index | Cross-sectional | Functional disability was associated with female sex, older age, unmarried status, illiteracy and poor economic status and feelings of loneliness |
| Clarke et al[28] 2005, US | 4162 community residents >65 years | Katz Index | Cross-sectional | Neighborhoods more accessible to pedestrians and friendly public transport are associated with greater independence in the ability to perform basic daily activities |
| Contijo et al[29] 2016, Brazil | 1,995 elderly in the community | ADL Index IADL Index |
Cross-sectional | Functional disability was positively correlated with low level of social capital |
| Cramm et al[30] 2011, Netherlands | 270 elderly >70 years | Katz Index | Cross-sectional | Older and vulnerable people living alone had poor functional capacity which was the main risk factor in the need for services in the community |
| Feng et al[31] 2014, China | 741 elderly 60-89 years | ADL Index | Cross-sectional | Functional Disability was correlated inversely with social support to rural population |
| Ferreira et al[32] 2010, Brazil | 1611 people aged >60 years old | ADL Index IADL Index |
Cross-sectional | Independence in basic daily activities was associated with male sex, better education, working in a job, being the head of household, no report of chronic illness, not being concerned about going out of home due to fear of falling because of sidewalk defects |
| Grundy et al[33] 2012, UK | 8780 people aged>60 years | ADL Index |
Cross-sectional | Larger family size was positively associated with receiving of help from a child by parents with activities of daily living (ADL) or instrumental activities of daily living (IADL) limitations |
| Hironaka et al[34] 2015, Japan | 1377 people aged>65 years old | IADL Index | Cross-sectional | Higher social capital was associates with satisfactory masticatory function which was positively related to a self-reliant life and an active life expectancy which can be extended |
| Imamura et al[10] 2016, Japan | 984 people aged>65 years old | Katz Index | Cross-sectional | Non-participation and level of trust at the community were associated with an increased risk of functional decline or death |
| Kanamori et al[21] 2014, Japan | 12951 older people mean age 72 years old | ADL Index | Prospective | Social participation may decrease the risk of incidence of functional disability in elderly |
| Levasseur et al[35] 2011, Canada | 554 elderly >65 years old | SMAF | Cross-sectional | Perceived proximity to neighborhood resources has a modest effect on the correlation between functional disability and social participation for men but not for women |
| Levasseur et al36 2010, Canada | 155 people with mean age 73,7 years old | SMAF | Cross-sectional | Reduced satisfaction with social participation is associated with limitations in daily activities in elderly |
| Litwin[37] 2010, Mediterranean | 9,154 people aged >60 years | ADL Index IADL Index |
Cross-sectional | Variations of the social network had different results in functional well-being of older people |
| Maciel et al[38] 2010, Brazil | 310 people aged >65 database sample | Katz Index | Prospective | The sociodemographic differences affect cognitive impairment, limitations in basic activities of daily living |
| Pavela[39] 2015, USA | 9,447 people aged >70 years old | ADL Index IADL Index |
Cross-sectional | Functional limitations (mobility) was associated with reduced likelihood of social contacts with friends |
| Rose et al[40] 2008, Latin America | 10500 people aged≥60 years old | ADL Index | Cross-sectional | Largest social network was associated with less disability in performing of basic daily activities |
| Rosso et al[9] 2013, US | 676 people aged >65 years old | ADL Index | Cross-sectional | Social engagement is important to maintain and strengthen one’s social ties that promote health and functional well-being |
| Satariano et al[41] 2016, US | 884 people aged ≥ 65 years | ADL Index IADL Index |
Cross-sectional | Older people with poor lower physical function reported difficulty in walking and low accessibility to goods and services |
| Somrongthong et al[42] 2017, Thailand | 1678 people ≥60 years | Barthel Index | Cross-sectional | Socio-economic factors were significantly associated with functional capacity |
| Tomioka et al[43] 2017, Japan | 17.680 people aged ≥ 65 years old | IADL Index | Cross-sectional | Social participation in older age is positively associated with IADL Index |
| Tomioka et al[44] 2016, Japan | 14956 people aged >65 years old | Barthel Index | Cross-sectional | The beneficial effects of frequent participation on IADL may be stronger for females than for males |
| Tomioka et al[45] 2015, Japan | 4588 people aged ≥65 years old | ADL Index IADL Index |
Prospective | The health impact of social participation on the functional efficiency can be stronger for women than older men |
| Ugargol et al[46] 2016, India | 9850 people aged ≥60 years old | Katz Index | Cross-sectional | Living arrangements were associated with functional decline, disability and decreased health outcomes |
| Vergara et al[47] 2014, Spain | 638 people aged ≥65 years | Barthel Index | Prospective | Social factors and living circumstances affect the functional recovery after an accidental hip fracture |
| Wee et al[48] 2012, Singapore | 909 people aged≥60 years old | Barthel Index | Cross-sectional | Living conditions in low socioeconomic status are associated with cognitive impairment and functional decline |
| Xu et al[49] 2015, US | 9237 Americans aged >65 years | Katz Index | Cross-sectional | Lower level of education and income were associated with greater disability in physical, emotional and cognitive functioning |
Table 2.
Presentation of the main findings among social capital aspects and HRQoL of older adults.
| Participants | Instrument | Study Type | Main findings | |
|---|---|---|---|---|
| Belanger, et al[50] 2016, Canada | 1600 people aged 65-74 years old | QOL | Cross-sectional | The effects of social support on physical and mental health and QoL depend on the sources of support and vary by social general framework |
| Belvis et al[51] 2008, Italy | 33744 people aged ≥60 years old | SF-12 | Cross-sectional | Some dimensions of social relationships were significantly associated with better HRQoL |
| Bowling et al[52] 2011, UK | 999 people aged >65 years old | OPQoL | Cross-sectional | Only the psychological approach to successful ageing independently predicted better HRQoL |
| Deshmukh et al[53] 2015, India | 900 people aged >60 years old | WHOQoL-brief | Cross-sectional | The social and cultural capital contributed significantly to quality of life (physical health) |
| Henning-Smith[54] 2016, US | 4862 people aged >65 years old | 5-item Likert scale | Cross-sectional | Older adults living alone are at greater risk for psychological distress and worse QoL |
| Lukumi et al[8] 2015, Spain | 1907 adults>60 years old | Spanish version of the SF-8 | Cross-sectional | Higher social capital indicators were positively associated with mental and physical dimension of HRQoL. |
| Ma et al[55] 2015, China | 214 people aged >65 years old | SF-36 | Cross-sectional | Greater social support was positively associated with better quality of life in elderly |
| Machon et al[56] 2017, Spain | 634 people aged ≥65 years old | EuroQol-5D Scale | Cross-sectional | Low social support was associated with poor HRQoL |
| Norstrand et al[7] 2012, China | 2,344 adults aged>65 years | 5-item Likert scale | Prospective | Social capital was associated with significantly better physical and emotional QoL |
| Tiraphat et al[57] 2017, Thailand | 4183 people aged≥60 years | WHOQoL-br | Cross-sectional | Age-friendly environments for elderly were associated with better QoL |
| Woo et al[58] 2010, China | 4000 people aged>65 years | SF-36 | Cross-sectional | A healthy lifestyle and socioeconomic status were associated with better physical and mental HRQoL |
Table 3.
Disability in ADL studies explored specific aspects of social capital.
| Elderly with poor functional disability (ADL/IADL) | Bonding | Bridging | Linking | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Social ties | Social support | Social cohesion | |||||||
| Social participation | Social diversion | Level of satisfaction with social relations | Mutual trust within a community | Social environment and level of crime in the community | Expression of trust to the home care | Voting rate for senior council in the community | The politicians’ attitude towards the older people in the community | Health expenses in the community for people >65 yrs | |
| 16 (articles) | 18 | 25 | 6 | 5 | 10 | 2 | 7 | 10 | |
| Aranda et al[24] 2011, US | ✓ | ✓ | ✓ | ||||||
| Bowling et al[25] 2006, UK | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Brown et al[26] 2008, USA | ✓ | ✓ | ✓ | ✓ | |||||
| Chen et al[27] 2015, China | ✓ | ✓ | ✓ | ||||||
| Clarke et al[28] 2005, US | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Contijo et al[29] 2016, Brazil | ✓ | ✓ | ✓ | ||||||
| Cramm et al[30] 2011, Netherlands | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Feng et al[31] 2014, China | ✓ | ✓ | ✓ | ✓ | |||||
| Ferreira et al[32] 2009, Brazil | ✓ | ✓ | ✓ | ✓ | |||||
| Grundy et al[33] 2012, UK | ✓ | ✓ | |||||||
| Hironaka et al[34] 2015, Japan | ✓ | ✓ | ✓ | ||||||
| Imamura et al[10] 2016, Japan | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Itziar Vergara et al[47] 2014, Spain | ✓ | ✓ | |||||||
| Kanamori et al[21] 2014, Japan | ✓ | ✓ | |||||||
| Levasseur et al[36] 2010, Canada | ✓ | ✓ | ✓ | ||||||
| Levasseur et al[35] 2011, Canada | ✓ | ✓ | ✓ | ✓ | |||||
| Litwin[37] 2010, Mediterranean countries | ✓ | ✓ | ✓ | ✓ | |||||
| Maciel et al[38] 2010, Brazil | ✓ | ✓ | ✓ | ||||||
| Pavela[39] 2015, US | ✓ | ✓ | |||||||
| Rose et al[40] 2008, Latin America | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Rosso et al[9] 2013, US | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Satariano et al[41] 2016, US | ✓ | ✓ | ✓ | ||||||
| Somrongthong et al[42] 2017, Thailand | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Tomioka et al[43] 2017, Japan | ✓ | ||||||||
| Tomioka et al[44] 2016, Japan | ✓ | ✓ | ✓ | ||||||
| Tomioka et al[45] 2015, Japan | ✓ | ✓ | ✓ | ||||||
| Ugargol et al[46] 2016, India | ✓ | ✓ | |||||||
| Wee et al[48] 2012, Singapore | ✓ | ✓ | ✓ | ✓ | |||||
| Xu et al[49] 2015, US | ✓ | ||||||||
Notes:(✓) indicates significantly associated.
Table 4.
HRQoL studies explored specific aspects of social capital.
| Older adults with “good” HRQoL | Bonding | Bridging | Linking | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Social ties | Social support | Social cohesion | |||||||
| High social participation | High social diversion | Level of satisfaction with social relations | Mutual trust within a community | Social environment and level of crime in the community | Expression of trust to the home care | Voting rate for senior council in the community | The politicians’ attitude towards the older people in the community | Health expenses in the community for people>65 years | |
| 10 (articles) | 11 | 10 | 4 | 2 | 5 | 4 | 5 | 7 | |
| Belanger, et al[50] 2016, Canada | ✓ | ✓ | ✓ | ||||||
| Belvis et al51 2008, Italia | ✓ | ✓ | ✓ | ||||||
| Bowling et al[52] 2011, UK | ✓ | ✓ | ✓ | ||||||
| Deshmukh et al[53] 2015, India | ✓ | ✓ | ✓ | ||||||
| Henning-Smith[54] 2016, US | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Lukumi et al[8] 2015, Spain | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Ma et al[55] 2015, China | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Machon et al[56] 2017, Spain | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Norstrand et al[7] 2012, China | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Tiraphat et al[57] 2017, Thailand | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Woo et al58 2010, China | ✓ | ✓ | ✓ | ||||||
Notes: (✓) indicates significantly associated.
Associations between Disability in ADL and Social Capital
Table 1 summarizes the results of the 29 included studies in terms of the relationship between social capital and disability in ADL in older adults, presenting the main findings of each article. Disability in ADL was positively associated with the low level of social capital while decreased social contact was correlated with functional limitations. Furthermore, high social contact and support and high self-efficacy had a strong independent association with better physical functioning.
Table 3 presents the disability in ADL studies explored specific aspects of social capital. The majority of the studies (25/29, 86,20%) shows a reverse association suggesting that increasing the level of satisfaction as reducing the disability in ADL. Additionally, a significant number of studies (18/29, 62,6%) concludes that high social diversity plays a key role in the reduced functional disability, thus the independence of the older. On the other hand, the variable of high social participation in 16 of the 29 studies (55,17%) is associated with the reduction of disability in ADL and increased autonomy of the older person. Fewer studies (6/29, 20,6%) correlate the feeling of trust in the community with a disability in ADL while 5/29 studies (17,2%) discuss the role of the level of violence and crime in the community with the functional disability of the seniors. Finally, 10 of 29 studies (34,5%) discuss trust of the older person to the home care, 2 of 29 (7%) the voting rate of the older adult in the community, 7 of the 29 (24,1%) the politicians’ social attitude towards the older people in the community and 10 of the 29 (34,5%) the health expenses for people>65 years in the community.
Associations between HRQoL and Social Capital
Studies on social capital and HRQoL try to score participants’ physical and mental health status. Social capital was analyzed concerning HRQOL in 11 studies. Table 2 summarizes the results of the included studies in terms of the relationship between social capital and HRQoL presenting similarly main findings. Generally, the majority of the main findings showed significant and reversely associations reporting that older person with high social capital presented with improved QoL in both domains mental and physical. Notably, in a few studies was found that social support was associated with less depression and better QoL, only in the domain of physical health.
Table 4 shows HRQoL studies explored specific aspects of social capital. Specifically, 11 of the 11 studies (100%) discuss the high social diversity, 10 of the 11 studies (90,9%) the high social participation and 10 of the 11 (90,9%) the level of satisfaction with social relations. Additionally, a smaller percentage of studies 4 of 11 (36,3%) refer to the feeling of trust in the community and only 2 of the 11 studies (18,1%) in the social environment and the level of violence and crime in the community. Finally, aspects of social cohesion (linking aspect) discuss 7 of the 11 studies (63,6%) health expenses for people >65 yrs in the community, 5 of the 11 studies (45,4%) trust of the older person to the home care, 5 of the 11 (45,4%) the politicians’ social attitude towards the older people in the community and 4 of the 11 (36,3%) the voting rate for senior council in the community and active participation in the political life of the community.
Discussion
The objective of this scoping review was to present an overview exploring the impact of social capital aspects on disability in ADL and HRQoL in a framework of achieving the goal of active and healthy ageing.
More specifically, the process of achieving active and healthy ageing is oriented to enhancing and improving the functionality and thus the QoL so that older adults to live independently. Despite them, prevention of syndromes and pathologies seems to be not enough to achieve the objective of active and healthy ageing as well as several factors such as the aspects of social capital are associated inextricably with disability in ADL, physical HRQoL and the general health status. It becomes obvious that to achieve this specific goal should primarily assess aspects that probably affect the independence and degree of independence of the older people[19,20].
It has been proposed several methods to assess social capital as its aspects vary according to age group study, with individual level (culture, education, beliefs, etc.) and the degree of influence in the community (crime, violence, social network, etc.) However, in this review, we focus on the three aspects of social capital (social ties-bonding, support-bridging and social cohesion-linking) that focus on gerontology, according to Pulsen et al.[6]. According to the synthesis of the new evidence presenting in this scoping review, it is demonstrated that high social aspects and particular social engagement reduces disability in ADL and improves the independence and the HRQoL.
More specifically, social ties (bonding) keep older adults active and promotes their physical function. On the other hand, the support older people take from their family, friends and their social participation plays a crucial role in their daily independence and prevents their functional decline[21]. Also, social capital positively affects the mental and physical dimensions of HRQoL. All of these are prerequisites for the achieving process of active and healthy ageing[11,19].
Consequently, European, national and regional policies for the promotion of healthy and active ageing must concentrate all aspects of social capital in their implementation. Policies should also shift the focus from hospital-based and acute care to self-care, empowerment and home care services. Thus, strengthen national, regional and local actions means that they must turn on the development and implementation policies and best practices which reassure older adult’s active ageing in the community which promotes social ties; the engagement of community nursing services to older people motivation and empowerment for active community participation (volunteering, activation, life-long learning, new technologies, etc.); the crucial action of reinforcing local services to improve collaboration and synergies between health and social services for the older people and long-term health and social care.
It is recently reported that ageing has a major impact on public and private expenditures. Keeping older adults healthy and active is a measure to control these high costs of care[22]. Thus, focusing on home care, technology solutions and community nursing services as well as on social inclusion, even though paid and unpaid work, are the perfect solutions to keep older people in their homes and to satisfy their health and social needs in their community. These kinds of services provide holistic human approach, prevent or delay the progression of the disease and dependency and also reduce frailty[22].
Interestingly, added value can be formed through a better understanding of the key relationship between social capital and independence and HRQoL by health professionals working in the community; paying special attention to the contribution of community nursing services to detect older adult’s social isolation/exclusion and stimulate their self-participation and connection with their local community; and increasing collaboration of national health and social care services for optimal physical health, HRQoL, and independence.
Since most of the studies focus on the effect of social ties (bonding aspect) on disability in ADL and HRQoL thus these associations cannot be discussed extensively as regards other aspects of social linking and bridging.
Given these findings, the current scoping review suggests some opportunities for future research. First, the development of reliable tools which measure systematically social capital. The lack of some clear, valid and reliable scales of social capital was a consistent methodological bias of the included studies which limits the confidentiality of their findings. Second, conducting more research using a comprehensive approach to clear up potential causal contributions of social capital on active and healthy ageing is recommended. Additionally, chronic medical conditions are important predictors of functional constraints[23]. In this context, future research should focus on the investigation of how chronic diseases affect social support with an emphasis on the expression of trust to the home care within the community.
The strength of this scoping review is its comprehensive approach to the appraisal regarding the relationship between social capital and ageing. This scoping review is more informational reflecting the functions of social capital and how it affects disability in ADL and HRQoL. Indeed, although there are many studies that refer to different aspects of social capital, the use of social capital as a general concept is relatively recent. For this reason, the research could be a turning point for the immediate future exploration of the relationship of social capital with active and healthy ageing. Another strong point of the scoping review is the search strategy in biomedical (PubMed and Scopus) databases according to the guidelines of PRISMA Extension for Scoping Reviews (PRISMA-ScR) to assure comprehensive coverage of literature in different fields. Additionally, the biases and prejudices of the evaluators in this scoping review were minimized with the participation of two independent reviewers which used the same data extraction forms. Therefore, we compose focused “new evidence” regarding the impact of Social Capital on the degree of disability in ADL of older people.
Limitations
Despite the useful findings, the present scoping review is subject to several limitations. Particularly, there is a possibility of bias in the publication as no grey literature was searched and non-English language publications were excluded. Additionally, all data were based on those reported by the authors, and no contact was carried out for incomplete information in the articles, the results may be subject to bias. In this scoping review, we are not able to answer “clearly formulated research question” because we held “synthesis” of the main findings and not “metanalysis”.
However, all articles in which social capital was in the title, the abstract, or used as a keyword were appraised. The reference lists of articles that met inclusion criteria were investigated. Consequently, it was argued that the strategy of this scoping review had covered most of the available literature.
Conclusions
This paper highlights the important role of specific social capital aspects on active and healthy ageing. It is also suggesting that older people with lower levels of social capital are more likely to experience to some degree difficulty in performing ADL particularly regarding the concept of cohesion in the neighbourhood. Preventive interventions should focus on prevention of disability, enhancing independence, and encouraging older people to participate more actively in social activities at the community level. Finally, health professionals caring for older people should first understand the importance of social capital in the effort to promote active and healthy ageing.
Footnotes
Edited by: George Lyritis
References
- 1.Verbrugge L, &Jette A. The disablement process. Social Science and Medicine. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 2.Puntam R, Leonardi R, Nanetti R. Making Democracy work.:civic traditions in modern Italy. Princeton: Princeton University Press; 1993. [Google Scholar]
- 3.Han S. Compositional and contextual associations of social capital and self-related health in Seoul, South Korea:A multilevel analysis of longitudinal evidence. Social Science and Medicine. 2013;80(3):113–120. doi: 10.1016/j.socscimed.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Cao J, Rammohan A. Social capital and healthy ageing in Indonesia. BMC Public Health. 2016;16:631–644. doi: 10.1186/s12889-016-3257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szreter S, Woolcock M. Health by association?Social capital, social theory and the political economy of public health. International Journal of Epidemiology. 2004;33(4):650–67. doi: 10.1093/ije/dyh013. [DOI] [PubMed] [Google Scholar]
- 6.Poulsen T, Christensen U, Lund R, Avlund K. Measuring aspects of social capital in a gerontological perspective. European Journal of Ageing. 2011;8(4):221–232. doi: 10.1007/s10433-011-0205-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norstrand J, Xu Q. Social capital and health outcomes among older adults in China:The Urban-Rural Dimension. The Gerontologist. 2012;52(3):325–334. doi: 10.1093/geront/gnr072. [DOI] [PubMed] [Google Scholar]
- 8.Lukumi D, Gomez L, Brownson R, Parra D. Social capital, socioeconomic status and health-related quality of life among older adults in Bogota (Colombia) Journal of Aging and Health. 2015;27(4):730–750. doi: 10.1177/0898264314556616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosso A, Taylor J, Tabb L, Michael Y. Mobility, disability and social engagement in older adults. Journal of Aging and Health. 2013;25(4):617–637. doi: 10.1177/0898264313482489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imamura H, Hamano T, Michikawa T, Takeda-Imai F, Nakamura T, Takebayashi T, Nishiwaki Y. Relationships of community and individual level social capital with activities of daily living and death by gender. International Journal of Environmental Research and Public Health. 2016;13(9):860–71. doi: 10.3390/ijerph13090860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.EIPonAHA. What is the European Innovation Partnership on Active and Healthy Ageing (EIP on AHA)? 2016. Retrieved at https: //ec.europa.eu/eip/ageing/about-the-partnership_en .
- 12.Tricco A, Lillie E, Zarin W, O'Brien K, Colquhoun H, Levac D, Straus S. PRISMA Extension for Scoping Reviews (PRISMA-ScR):Checklist and Explanation. Annals of Internal Medicine. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 13.Arksey H, O'Malley L. Scoping studies:towards a methodological framework. International journal of social research methodology. 2005;8(1):19–32. [Google Scholar]
- 14.NHLBI. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. 2014. Retrieved at https: //www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort .
- 15.Hartigan I. A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Int J Older People Nurs. 2007;2(3):204–212. doi: 10.1111/j.1748-3743.2007.00074.x. [DOI] [PubMed] [Google Scholar]
- 16.Prodinger B, O'Connor RJ, Stucki G, Tennant A. Establishing score equivalence of the functional independence measure motor scale and the Barthel Index, utilizing the International Classification of Functioning, Disability and Health and Rasch measurement theory. J Rehabil Med. 2017;49(5):416–422. doi: 10.2340/16501977-2225. [DOI] [PubMed] [Google Scholar]
- 17.Hopman-Rock M, van Hirtum H, De Vreede P, Freiberger E. Activities of daily living in older community-dwelling persons:a systematic review of psychometric properties of instruments. Aging Clin Exp Res. 2019;31(7):917–925. doi: 10.1007/s40520-018-1034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire:normative data for adults of working age. BMJ. 1993;306(6890):1437–40. doi: 10.1136/bmj.306.6890.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO. Active Aging:A Policy Framework. Geneva: WHO; 2002. [Google Scholar]
- 20.Council of the European Union. Council Declaration on the European Year for Active Ageing and Solidarity between Generations:The Way Forward. 2012. Retrieved from http: //register.consilium.europa.eu/doc/srv?l=EN&f=ST%2017468%202012%20INIT .
- 21.Kanamori S, Kai Y, Aida J, Kondo K, Kawachi I, Hirai H, JAGES Group. Social participation and the prevention of functional disability in older Japanese:The JAGES Cohort Study. PloS One. 2014;9(6):1–10. doi: 10.1371/journal.pone.0099638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cylus J, Figueras J, Normand C, Sagan A, Richardson E, North J, White C. Will population ageing spell the end of the welfare state?a review of evidence and policy options. Copenhagen: World Health Organization; 2019. [PubMed] [Google Scholar]
- 23.Boult C, Kane R, Louis T, Boult L, McCaffrey D. Chronic conditions that lead to functional limitation in the elderly. Journal of Gerontology. 1994;49(1):28–36. doi: 10.1093/geronj/49.1.m28. [DOI] [PubMed] [Google Scholar]
- 24.Aranda M, Ray L, Snih S, Ottenbacher K, Markides K. The protective effect of neighborhood composition on increasing frailty among older Mexican Americans:A barrio advantage? Journal Aging Health. 2011;23(7):1189–1217. doi: 10.1177/0898264311421961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowling A, Barber J, Morris R, Ebrahim S. Do perceptions of neighbourhood environment influence health?Baseline findings from a British survey of aging. J Epidemiol Community Health. 2006;60(6):476–483. doi: 10.1136/jech.2005.039032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown S, Mason C, Perrino T, Lombard J, Martinez F, Plater-Zyberk E, Szapocznik J. Built environment and physical functioning in Hispanic elders:the role of “eyes on the street”. Environmental Health Perspectives. 2008;116(10):1300–1307. doi: 10.1289/ehp.11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen W, Fang Y, Mao F, Hao S, Chen J, Yuan M, Hong A. Assessment of Disability among the elderly in Xiamen of China:A representative sample survey of 14.292 older adults. PloS One. 2015;10(6):1–12. doi: 10.1371/journal.pone.0131014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clarke P, George L. The role of the Built environment in the Disablement Process. American Journal of Public Health. 2005;95(11):1933–1939. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Contijo C, Mambrini J, Luz T, Filho A. Association between disability and social capital among community-dwelling elderly. Revista Brasileira de Epidemiologia. 2016;19(3):471–483. doi: 10.1590/1980-5497201600030001. [DOI] [PubMed] [Google Scholar]
- 30.Cramm J, Dijk H, Lotters F, Exel J, Nieboer A. Evaluating an integrated neighbourhood approach to improve well-being of frail elderly in a Dutch community:a study protocol. BMC Research Notes. 2011;4:532–540. doi: 10.1186/1756-0500-4-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng D, Ji L, Xu L. Mediating effect of social support on the association between functional disability and psychological distress in older adults in rural China:Does Age make a difference? PloS One. 2014;9(6):1–7. doi: 10.1371/journal.pone.0100945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferreira F, Cesar C, Passos V, Lima-Costa M, Proietti F. Aging and Urbanization:the neighborhood perception and functional performance of elderly persons in Belo Horizonte Metropolitan Area-Brazil. Journal of Urban Health. 2010;87(1):54–66. doi: 10.1007/s11524-009-9406-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grundy E, Read S. Social contacts and receipt of help among older people in England:are there benefits of having more children? The Journal of Gerontologists Series B Psychological Sciences and Social Sciences. 2012;67(6):742–754. doi: 10.1093/geronb/gbs082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hironaka M, Kayama Y, Misaka Y, Akifusa S. Relationship between self-rated masticatory ability and independent life in community-dwelling older adults. Gerontology and Geriatric Medicine. 2015;1:1–8. doi: 10.1177/2333721415603193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levasseur M, Gauvin L, Richard L, Kestens Y, Daniel M, Payette H. Associations between perceived proximity to neighborhood resources, disability, and social participation among community-dwelling older adults:results from the Voisi Nu Age Study. Archives of Physical Medicine and Rehabilitation. 2011;92(12):1979–1986. doi: 10.1016/j.apmr.2011.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levasseur M, Desrosiers J, Whiteneck G. Accomplishment level and satisfaction with social participation of older adults:association with quality of life and best correlates. Quality of Life Research. 2010;19(5):665–675. doi: 10.1007/s11136-010-9633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Litwin H. Social Networks and well-being:a comparison of older people in Mediterranean and non-Mediterranean countries. The Journals of Gerontology Series B:Psychological Sciences and Social Sciences. 2010;65(B):599–608. doi: 10.1093/geronb/gbp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maciel A, Guerra R. Influence of biopsychosocial factors on the survival of the elderly in Northeast Brazil- A prospective study. Current Gerontology and Geriatrics Research. 2010;1:1–8. doi: 10.1155/2010/127605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pavela G. Functional status and social contact among older adults. Research on Aging. 2015;37(8):815–836. doi: 10.1177/0164027514566091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rose A, Hennis A, Hambleton I. Sex and the city:Differences in disease- and disability-free life years and active community participation of elderly men and women in 7 cities in Latin America and the Caribbean. BMC Public Health. 2008;8:127–137. doi: 10.1186/1471-2458-8-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Satariano W, Kealey Μ, Hubbard A, Kurtovich E, Ivey S, Bayles CN, Bayles C, Prohaska T. R. Mobility disability in older adults:at the intersection of people and places. The Gerontologist. 2016;56(3):525–534. doi: 10.1093/geront/gnu094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Somrongthong R, Wongchalee S, Ramakrishna C, Hongthong D, Yodmai K, Wongtongkam N. Influence of socioeconomic factors on daily life activities and quality of life of Thai elderly. The Journal of Public Health Research. 2017;6(1):49–55. doi: 10.4081/jphr.2017.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tomioka Κ, Kurumatani Ν, Hosoi Η. Age and gender differences in the association between social participation and instrumental activities of daily living among community-dwelling elderly. BMC Geriatrics. 2017;17:99–108. doi: 10.1186/s12877-017-0491-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tomioka K, Kurumatani N, Hosoi H. Association between social participation and instrumental activities of daily living among community-dwelling older adults. Journal of Epidemiology. 2016;26(10):553–561. doi: 10.2188/jea.JE20150253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tomioka Κ, Kurumatani Ν, Hosoi Η. Social Participation and the prevention of decline in effectance among community-dwelling elderly:a population-based cohort study. PloS One. 2015;10(9):1–13. doi: 10.1371/journal.pone.0139065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ugargol AP, Hutter I, James KS, Bailey A. Care Needs and Caregivers:Associations and Effects of Living Arrangements on Caregiving to Older Adults in India. Ageing international. 2016;41:193–213. doi: 10.1007/s12126-016-9243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana J. Factors related to functional prognosis in elderly patients after accidental hip fractures:a prospective cohort study. BMC Geriatrics. 2014;14:124–132. doi: 10.1186/1471-2318-14-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wee L, Yeo W, Yang G, Hannan N, Lim K, Chua C, Shen HM. Individual and area level socioeconomic status and its association with cognitive function and cognitive impairment (Low MMSE) among community-dwelling elderly in Singapore. Dementia and Geriatrics Cognitive Disorders Extra. 2012;2(1):529–542. doi: 10.1159/000345036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu X, Liang J, Bennett J, Botoseneanu A, Allore H. Socioeconomic stratification and multidimensional health trajectories:evidence of convergence in later old age. The Journals of Gerontology Series B:Psychological Sciences and Social Sciences. 2015;70(4):661–671. doi: 10.1093/geronb/gbu095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Belanger E, Ahmed T, Vafaei A, Curcio C, Philips S, Zunzunegui M. Sources of social support associated with health and quality of life:a cross-sectional study among Canadian and Latin American older adults. BMJ Open. 2016;6(6):1–10. doi: 10.1136/bmjopen-2016-011503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Belvis A, Avolio M, Sicuro L, Rosano A, Latini E, Damiani G, Ricciardi W. Social relationships and HRQL:a cross-sectional survey among older Italian adults. BMC Public Health. 2008;8:348–358. doi: 10.1186/1471-2458-8-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bowling A, Iliffe S. Psychological approach to successful ageing predicts future quality of life in older adults. Health and Quality of Life Outcomes. 2011;9(13):1–10. doi: 10.1186/1477-7525-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Deshmukh P, Dongre A, Rajendran K, Kumar S. Role of social, cultural and economic capitals perceived quality of life among old age people in Kerala, India. Indian Journal of Palliative Care. 2015;21(1):39–44. doi: 10.4103/0973-1075.150175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Henning-Smith C. Quality of Life and Psychological Distress among older adults:The Role of Living Arrangements. Journal of Applied Gerontology. 2016;35(1):39–61. doi: 10.1177/0733464814530805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma L, Li Y, Wang J, Zhu H, Yang W, Cao R, Feng M. Quality of Life is related to social support in elderly osteoporosis patients in a Chinese population. PloS One. 2015;10(6):1–10. doi: 10.1371/journal.pone.0127849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Machon M, Larranaga I, Dorronsoro M, Vrotsou K, Vergara I. Health-related quality of life and associated factors in functionally independent older people. BMC Geriatrics. 2017;17:19–27. doi: 10.1186/s12877-016-0410-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tiraphat S, Peltzer K, Thamma-Aphiphol K, Suthisukon K. The Role of Age -Friendly Environments on Quality of Life among Thai older adults. International Journal of Environmental Research and Public Health. 2017;14(3):282–294. doi: 10.3390/ijerph14030282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Woo J, Chan R, Leung J, Wong M. Relative contributions of geographic, socioeconomic and lifestyle factors to quality of Life, Frailty and Mortality in elderly. PloS One. 2010;5(1):1–11. doi: 10.1371/journal.pone.0008775. [DOI] [PMC free article] [PubMed] [Google Scholar]


