Summary
Background
COVID‐19 school closures pose a threat to children's wellbeing, but no COVID‐19‐related studies have assessed children's behaviours over multiple years .
Objective
To examine children's obesogenic behaviours during spring and summer of the COVID‐19 pandemic compared to previous data collected from the same children during the same calendar period in the 2 years prior.
Methods
Physical activity and sleep data were collected via Fitbit Charge‐2 in 231 children (7–12 years) over 6 weeks during spring and summer over 3 years. Parents reported their child's screen time and dietary intake via a survey on 2–3 random days/week.
Results
Children's behaviours worsened at a greater rate following the pandemic onset compared to pre‐pandemic trends. During pandemic spring, sedentary behaviour increased (+79 min; 95% CI = 60.6, 97.1) and MVPA decreased (−10 min, 95% CI = −18.2, −1.1) compared to change in previous springs (2018–2019). Sleep timing shifted later (+124 min; 95% CI = 112.9, 135.5). Screen time (+97 min, 95% CI = 79.0, 115.4) and dietary intake increased (healthy: +0.3 foods, 95% CI = 0.2, 0.5; unhealthy: +1.2 foods, 95% CI = 1.0, 1.5). Similar patterns were observed during summer.
Conclusions
Compared to pre‐pandemic measures, children's PA, sedentary behaviour, sleep, screen time, and diet were adversely altered during the COVID‐19 pandemic. This may ultimately exacerbate childhood obesity.
Keywords: accelerometry, children, diet, physical activity, screen time, sleep
List of Abbreviations
- 95% CI
95% confidence interval
- BMI
body mass index
- COVID‐19
coronavirus disease 2019
- HRR
heart rate reserve
- MVPA
moderate‐to‐vigorous physical activity
- PA
physical activity
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic resulted in widespread health, social and economic consequences, particularly in the United States. Globally, approximately 1.5 billion elementary school‐age children (ages 5–12) were impacted by school closures and began virtual learning in March and April 2020. 1 The school closures enacted to limit the spread of COVID‐19 pose a potential threat to children's physical and mental wellbeing. Structured environments such as school and extracurricular activities provide opportunities for positive health behaviours (e.g., minimal screen time, nutritious meals, physical activity [PA] opportunities and a regular sleep schedule) which reduce the risk of overweight and obesity. 2 , 3 During summer months, obesogenic behaviours increase and ultimately lead to unhealthy weight gain. 4 This effect is more pronounced among low‐income, as well as Black and Hispanic families. 5 , 6 COVID‐19‐related closures and mitigation strategies may inadvertently alter children's health behaviours by mimicking an ‘extended summer vacation’ environment, largely devoid of external structure that school or extracurricular activities provide. The lack of structure may exacerbate obesogenic behaviours and ultimately lead to unhealthy weight gain. 7
Concerns about children's health behaviours during the pandemic have been reflected through commentaries forecasting the immediate and distal effects of COVID‐19 on children's activity, sleep, dietary intake, and screen time. 8 Initial cross‐sectional and longitudinal studies indicate children are less active, 9 , 10 , 11 , 12 consume more snacks, 11 , 13 and engage in more screen time 10 , 11 , 12 compared to retrospective recall of pre‐pandemic behaviours or self‐reported behaviours. Although effects of the pandemic on sleep duration and quality have been mixed, 12 , 13 , 14 , 15 there is a shift towards later bed/wake times, 14 , 15 , 16 which is concerning given the link between later bedtimes and negative health indicators. 17
No current COVID‐19 related studies have assessed children's behaviours across multiple years. This is particularly relevant as both seasonality and developmental changes are known to impact children's levels of PA, 18 sedentary behaviour, 18 sleep, 18 screen time, 19 and dietary intake. 20 Furthermore, relatively fewer studies to date have reported on multiple health behaviours (i.e., PA, sleep, screen time and diet) within the same sample. 11 , 13 , 21 The purpose of this study was thus to examine children's obesogenic behaviours during the COVID‐19 pandemic compared to previous data collected from the same children during the same calendar period in each of the 2 years prior (i.e., 2018, 2019). Specifically, behaviours in spring and summer of 2020 were compared to spring and summer of 2019, after accounting for yearly maturational changes measured from 2018 to 2019. This interrupted time series design is strengthened by the repeated measures of behaviours among the same children, 22 the use of objective measures of PA and sleep, and methods used to reduce recall bias to measure screen time and dietary intake.
2. METHODS
2.1. Study design
This quasi‐experimental interrupted time series study is an extension of a larger, longitudinal study to examine changes in body mass index (BMI) and fitness of children (age 7–12 years) attending year‐round and traditional schools. 23 , 24 When traditional randomized controlled trials are not possible, a quasi‐experimental interrupted time series is a strong alternative design, 25 and can uniquely inform public health research. With this design, the specific time point in the series at which an “exposure” (i.e., pandemic) occurred must be known, and subsequent causal hypotheses about the effect of the pandemic can be tested by examining trends before and after that point in time. Using multiple observations prior to pandemic onset is a strength of this design and reduces threats to internal validity, most notably the threats of maturation (i.e., study outcomes being a result of natural change over time) and history (i.e., the potential for variables other than the pandemic to influence the outcome). This allows us to compare natural changes prior to the pandemic (i.e., “maturation” to changes that occurred during the pandemic above and beyond what would have been considered a natural change over time (i.e., pandemic + maturation).
Participant recruitment took place in 2018 and 2019. Schools were matched on school‐day structure, start and end times, enrollment, and student demographics. All children attending these three schools in kindergarten through third grade were invited to participate in behavioural measures in spring of 2018. 24 Parents were asked to return a consent form to the child's school to indicate their interest in participating. Of those who expressed interest, children were randomly selected to participate in the longitudinal study (Table 1). The current study leveraged this existing cohort and added additional measurement time points for a subsample of participants during the COVID‐19 pandemic in 2020. At the initiation of this extension of the original cohort study (April 2020), all participating schools had adopted the same virtual learning schedule 5 days per week (Figure S1), so participants from different schools were combined for this analysis. All measurements were collected in six‐week “sprints” during the school year and summer. For these analyses, only measurements collected during overlapping segments were included (i.e., April/May and June/July).
TABLE 1.
Participation of children in sample by year
| 2018 | 2019 a | 2020 b | |
|---|---|---|---|
| Participants invited | 240 | 168 | 157 |
| Provided valid data | 182 | 127 | 74 |
| No response | 10 | 7 | 63 |
| Opted out | 7 | 6 | 14 |
| No data | 2 | 2 | 0 |
| Moved away | 39 | 26 | 6 |
Note: Please see Table S1 for a detailed breakdown of the number of children who provided valid data across time points.
Sample was refreshed n = 50.
Only children with valid data in 2018 and/or 2019 were invited.
2.2. Participants
Two hundred thirty‐one unique children from the southeastern United States provided data in 2018 and/or 2019. Children from the existing cohort with valid 2018 and/or 2019 data were invited to participate in additional measurement time points (referred to as “2020 subsample”) during the pandemic unless they had moved out of the area, opted out of the study, or no longer responded to phone communication. Parents opted into this extension of the original study by responding to a brief online survey. Of the 157 invited, 74 enrolled and provided valid data (Table S1).
2.3. Measures
Upon opting in (mid‐April), and consistent with previous data collection waves, participants were mailed an envelope with study information, a Fitbit and charger, and a pre‐stamped envelope to return their device in August. PA and sleep were measured via a wrist‐worn Fitbit Charge‐2 (Fitbit Inc., San Francisco, CA). Children were asked to wear the device every day over each six‐week measurement period in spring and summer each year (i.e., 2018–2020). Fitbit devices that integrate heart rate and accelerometry provide good agreement with polysomnography and electrocardiography. 26 , 27 Parents were instructed to sync their child's Fitbit via the Fitbit app installed on their mobile phone. Parents were sent reminders to sync three times per week. Upon syncing, data were stored on the cloud‐based Fitabase platform (Small Steps Lab, LLC, San Diego, CA). Data processing for PA and sleep have been previously described elsewhere. 24 , 28 Briefly, PA intensity was calculated from heart rate data. 29 Children's resting heart rate was ascertained from their daily lowest average heart rate over ten consecutive minutes. 30 , 31 , 32 , 33 From this, children's PA intensity was determined using percent of heart rate reserve (HRR) where 0%–19.9% HRR is classified as sedentary activity, 20.0%–49.9% HRR is classified as light PA and ≥50% HRR is classified as MVPA. 34 Days in which children had at least 10 h of waking wear time were considered valid days and included in analyses.
Sleep outcomes of interest included nocturnal sleep duration (i.e., total sleep time, in minutes), sleep timing (sleep onset, offset, midpoint) and sleep variability (i.e., individual standard deviation of sleep midpoint). Sleep onset occurred in the first minute that the child's nocturnal sleep episode began while offset occurred when the last minute of the sleep episode was recorded. Sleep midpoint, which is an indicator of timing shifts, 35 was calculated as the time halfway between onset and offset. For this analysis, nocturnal sleep was defined as a sleep period lasting >240 min with sleep onset between 7 PM–6 AM and offset between 5 AM‐1 PM. Sleep periods that fell outside these criteria were flagged as invalid. Sensitivity analyses were conducted to examine the influence of invalid sleep periods on outcomes of interest. Because we hypothesized that children's nocturnal sleep patterns may shift during the COVID‐19 pandemic, only daytime sleep periods (i.e., onset between 6 AM–7 PM) were excluded.
During each 6‐week measurement period, parents reported children's consumption of healthy and unhealthy foods as well as screen use in a survey (<5 min) sent via text on two to three random days each week. 23 Parents received the survey in the evening and were instructed to report based on their child's activities on that day. Healthy and unhealthy food consumption was assessed with the Beverage and Snack Questionnaire. 36 The Healthy Meal Index informed categorization of foods into healthy (i.e., fruit, vegetables, unsweetened dairy) and unhealthy (i.e., convenience foods, sweets/desserts, salty snacks, sugar‐sweetened beverages) foods. 37 Foods consumed were dichotomized into did or did not consume categories. Values for healthy and unhealthy foods were summed and represent the number of foods consumed per day with a range from 0 to 3 for healthy foods and 0 to 14 for unhealthy foods consumed. Parents were also asked to report their child's total daily screen use (i.e., watching TV/movies, playing video games, using a smartphone, tablet, or computer), as well as screen use after 8:00 PM, and after 8:00 PM in the bedroom (hereafter referred to as bedroom screen time). 38 , 39
2.4. Statistical analyses
Demographic variables of participants in the 2020 subsample were compared with the larger sample using chi‐square tests. Logistic regression models were used to predict the likelihood of participating in the 2020 subsample from pre‐pandemic behaviours. Missing data patterns were examined along with associations with demographic variables. All outcome variables were examined for normality. Variables that were skewed (i.e., greater than absolute value of two) were winsorized at 5%. Multilevel mixed models were used to account for the repeated measures of the data (days nested within measurement periods which were then nested within children). Time points were treated as categorical, and dummy coded with spring 2018 as the reference point. To assess typical maturational changes, we used linear combinations to compare differences in means between 2019 and 2018 for each behavioural outcome. We then compared the difference in change between years (i.e., change from 2020 to 2019 compared to typical maturational changes from 2019 to 2018). This allowed for interpretation of pandemic‐related changes above and beyond what we would have expected with maturation over time. To investigate potential moderation, we included a sex‐by‐age interaction term in all models. Children's age, sex and race were included as covariates in all statistical models. Age and sex were included as covariates to account for previously documented differences in PA. 40 Race was included as a covariate to account for the well‐documented effects of structural racism on health behaviours which underlie health disparities. 41 Race was included in the model as a dichotomous variable (white vs. historically minoritized groups [i.e., Black, Hispanic, more than one race]) to account for the effects of identifying as a historically minoritized group in the context of a society that favours ‘whiteness.’ Children's wear time and mean sleep duration were also included in activity and sleep variability models, respectively. All participants who provided valid data at any point were included in the model and maximum likelihood estimation was used to account for missingness. The Benjamini–Hochberg procedure was used to account for multiple comparisons. 42 All statistical analyses were completed in Stata (Version 16.1, College Station, TX).
3. RESULTS
In 2018 and/or 2019, 231 children provided valid data, 74 of which re‐enrolled in the 2020 subsample. Children provided an average of 19 valid days and nights of Fitbit wear for PA and sleep measures during each measurement period. Demographics for the 2020 subsample and the larger cohort are presented in Table 2. Raw estimates of children's behaviours can be found in Table 3. Only MVPA and bedroom screen time were not normally distributed and therefore winsorized results are presented. Children who re‐enrolled in the 2020 subsample did not differ from the larger cohort sample in terms of sex [χ 2 (1) = 0.30, p > 0.05] grade in school [χ 2 (4) = 9.25, p > 0.05] or school attended [χ 2 (2) = 2.43, p > 0.05]. Children who re‐enrolled in the 2020 subsample consumed more unhealthy foods (2.96 ± 0.09 vs. 2.69 ± 0.08) compared to those who did not re‐enroll (t[461] = −2.27, p = 0.02). There was no significant clustering at the school level on any variables of interest (all ICC < 0.006). Sensitivity analyses demonstrated that sleep parameterization did not change the direction or significance of results, thus all nocturnal sleep periods were analysed. When assessing for potential moderation, all sex‐by‐age interactions were non‐significant (p > 0.05) indicating no differential effects for boys and girls over time (data not shown).
TABLE 2.
Descriptive characteristics of participants with only pre‐pandemic measures and those enrolled in the subsample
| 2020 Subsample (n = 74) | Pre‐pandemic only (n = 157) | |||
|---|---|---|---|---|
| N | % or M ± SD | N | % or M ± SD | |
| Parent sociodemographic Info | ||||
| Relationship to child | ||||
| Mother | 67 | 90.5% | 111 | 91.0% |
| Father | 4 | 5.4% | 4 | 3.3% |
| Grandmother | 3 | 4.1% | 6 | 4.9% |
| Aunt | 0 | 0.0% | 1 | 0.8% |
| Education | ||||
| <High school | 3 | 4.1% | 6 | 4.2% |
| High school | 16 | 21.6% | 33 | 27.1% |
| Some college | 34 | 46.0% | 43 | 35.4% |
| 2‐year degree | 5 | 6.8% | ‐ | ‐ |
| 4‐year degree | 9 | 12.2% | 27 | 22.1% |
| Graduate or professional degree | 7 | 9.5% | 13 | 10.7% |
| Marital status | ||||
| Married | 32 | 43.2% | 52 | 42.6% |
| Single | 18 | 24.3% | 34 | 27.9% |
| Living with partner | 8 | 10.8% | 15 | 12.3% |
| Widowed/divorced/separated | 16 | 21.6% | 21 | 17.2% |
| Household income | ||||
| <$20, 000 | 22 | 30.1% | 35 | 28.7% |
| $20, 001–$40, 000 | 27 | 37.0% | 40 | 32.8% |
| $40, 001–$60, 000 | 7 | 9.6% | 22 | 18.0% |
| $60, 001–$80, 000 | 8 | 11.0% | 10 | 8.2% |
| >$80, 000 | 9 | 12.3% | 15 | 12.3% |
| Child sociodemographic info | ||||
| Age (years) | 74 | 9.8 ± 1.5 | 154 | 10.0 ± 1.1 |
| Sex | ||||
| Male | 39 | 53% | 72 | 45.9% |
| Female | 35 | 47% | 85 | 54.1% |
| Race | ||||
| White | 25 | 34% | 53 | 33.8% |
| Historically minoritized groups | 49 | 66% | 104 | 66.2% |
| Household Makeup | ||||
| Number of people | 74 | 4.2 ± 1.1 | 122 | 4.4 ± 1.5 |
| Number of children | 74 | 2.4 ± 0.9 | 121 | 2.7 ± 1.4 |
Note: Historically minoritized groups included children whose parent reported their race as Black, Hispanic, or more than one race.
TABLE 3.
Raw estimates of children's health behaviours across measurement periods (2018–2020)
| Spring 2018 | Spring 2019 | Spring 2020 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subsample | Pre‐pandemic only | Subsample | Pre‐pandemic only | Subsample | ||||||
| N | M ± SD | N | M ± SD | N | M ± SD | N | M ± SD | N | M ± SD | |
| Physical activity (min) | ||||||||||
| Light PA | 45 | 488.8 ± 84.0 | 123 | 499.6 ± 100.3 | 59 | 478.8 ± 110.3 | 33 | 484.1 ± 101.9 | 70 | 394.4 ± 109.4 |
| MVPA | 45 | 78.7 ± 31.1 | 123 | 78.5 ± 36.1 | 59 | 71.2 ± 38.9 | 33 | 63.9 ± 38.7 | 70 | 60.5 ± 33.3 |
| Sedentary behaviour (min) | 45 | 313.8 ± 95.6 | 123 | 293.3 ± 112.8 | 59 | 327.2 ± 119.5 | 33 | 329.6 ± 123.9 | 70 | 465.9 ± 145.1 |
| Sleep | ||||||||||
| Minutes asleep | 44 | 470.9 ± 37.9 | 125 | 465.0 ± 50.1 | 58 | 462.7 ± 45.2 | 37 | 475.6 ± 46.1 | 61 | 476.0 ± 52.0 |
| Bedtime | 44 | 10:42 PM ± 51.5 | 125 | 10:50 PM ± 64.7 | 58 | 10:40 PM ± 62.0 | 37 | 10:30 PM ± 57.0 | 61 | 12:27 AM ± 115.7 |
| Wake time | 44 | 7:05 AM ± 43.0 | 125 | 7:07 AM ± 52.7 | 58 | 6:58 AM ± 45.7 | 37 | 6:57 AM ± 49.6 | 61 | 8:57 AM ± 109.6 |
| Midpoint | 44 | 2:53 AM ± 44.0 | 125 | 2:58 AM ± 52.8 | 58 | 2:48 AM ± 49.8 | 37 | 2:43 AM ± 48.2 | 61 | 4:37 AM ± 109.1 |
| Midpoint ISD | 43 | 73.0 ± 30.5 | 117 | 73.9 ± 38.8 | 55 | 65.1 ± 32.3 | 32 | 63.3 ± 36.4 | 60 | 89.6 ± 60.5 |
| Screen time (min) | ||||||||||
| Total ST | 45 | 100.5 ± 75.3 | 83 | 88.1 ± 65.5 | 70 | 105.3 ± 68.7 | 50 | 110.9 ± 79.7 | 74 | 220.2 ± 121.9 |
| Evening ST | 42 | 25.8 ± 38.3 | 82 | 15.0 ± 21.5 | 69 | 34.4 ± 34.8 | 49 | 34.2 ± 37.4 | 74 | 60.4 ± 56.0 |
| Bedroom ST | 41 | 13.9 ± 29.1 | 82 | 5.4 ± 11.9 | 68 | 16.5 ± 28.0 | 49 | 12.5 ± 18.0 | 74 | 25.6 ± 35.0 |
| Diet | ||||||||||
| Healthy foods | 45 | 1.5 ± 0.8 | 84 | 1.3 ± 0.7 | 71 | 1.5 ± 0.8 | 50 | 1.4 ± 0.7 | 74 | 2.0 ± 0.8 |
| Unhealthy foods | 45 | 2.9 ± 1.4 | 84 | 2.6 ± 1.3 | 71 | 2.8 ± 1.2 | 50 | 2.7 ± 1.3 | 73 | 4.4 ± 1.6 |
| Summer 2018 | Summer 2019 | Summer 2020 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subsample | Pre‐pandemic only | Subsample | Pre‐pandemic only | Subsample | ||||||
| Physical activity (min) | ||||||||||
| Light PA | 34 | 471.6 ± 78.5 | 54 | 475.2 ± 113.0 | 43 | 445.1 ± 108.6 | 17 | 478.4 ± 111.3 | 57 | 416.1 ± 112.9 |
| MVPA | 34 | 88.1 ± 44.8 | 54 | 74.1 ± 43.3 | 43 | 68.7 ± 39.1 | 17 | 102.7 ± 60.1 | 57 | 67.7 ± 38.5 |
| Sedentary behaviour (min) | 34 | 322.5 ± 107.1 | 54 | 315.6 ± 132.9 | 43 | 358.5 ± 134.3 | 17 | 287.8 ± 147.9 | 57 | 493.0 ± 169.4 |
| Sleep | ||||||||||
| Minutes asleep | 35 | 473.1 ± 60.3 | 55 | 492.0 ± 45.0 | 43 | 474.9 ± 54.6 | 19 | 490.3 ± 50.4 | 52 | 485.8 ± 49.4 |
| Bedtime | 35 | 11:38 PM ± 83.3 | 55 | 11:32 PM ± 76.6 | 43 | 12:02 AM ± 93.9 | 19 | 11:47 PM ± 68.9 | 52 | 12:50 AM ± 103.6 |
| Wake time | 35 | 8:03 AM ± 87.1 | 55 | 8:17 AM ± 80.1 | 43 | 8:35 AM ± 99.4 | 19 | 8:32 AM ± 69.6 | 52 | 9:30 AM ± 116.1 |
| Midpoint | 35 | 3:47 AM ± 79.6 | 55 | 3:47 AM ± 75.2 | 43 | 4:20 AM ± 92.9 | 19 | 4:03 AM ± 63.2 | 52 | 5:10 AM ± 106.5 |
| Midpoint ISD | 33 | 72.6 ± 41.4 | 53 | 75.8 ± 51.8 | 41 | 68.2 ± 39.9 | 17 | 60.3 ± 38.1 | 51 | 103.9 ± 89.0 |
| Screen time (min) | ||||||||||
| Total ST | 40 | 139.4 ± 89.6 | 70 | 123.7 ± 88.4 | 66 | 154.1 ± 97.1 | 37 | 174.2 ± 90.2 | 69 | 185.7 ± 119.3 |
| Evening ST | 40 | 44.9 ± 53.1 | 63 | 36.2 ± 44.0 | 65 | 57.8 ± 51.4 | 37 | 51.5 ± 47.8 | 69 | 62.3 ± 63.1 |
| Bedroom ST | 40 | 16.5 ± 33.5 | 63 | 12.5 ± 27.1 | 65 | 23.2 ± 33.3 | 37 | 24.3 ± 27.7 | 69 | 25.9 ± 33.4 |
| Diet | ||||||||||
| Healthy foods | 39 | 1.3 ± 0.8 | 70 | 1.2 ± 0.8 | 66 | 1.5 ± 0.9 | 38 | 1.6 ± 0.8 | 68 | 2.0 ± 0.8 |
| Unhealthy foods | 39 | 2.8 ± 1.3 | 70 | 2.6 ± 1.2 | 66 | 3.3 ± 1.4 | 38 | 3.0 ± 1.3 | 68 | 4.1 ± 1.3 |
Note: Pre‐pandemic only measures include children who did not re‐enroll in the 2020 subsample. Healthy foods ranged from 0 to 3 and unhealthy foods ranged from 0 to 14 with higher values indicating greater daily consumption. MVPA and Bedroom ST were winsorized at 5% due to high skew.
Abbreviation: ISD, individual standard deviation; MVPA, moderate to vigorous physical activity; PA, physical activity; ST, screen time.
Before the pandemic, children naturally increased sedentary time from spring 2018 to spring 2019 by +25 min and reduced light PA and MVPA by −17 and −8 min, respectively. Total screen time increased by +22 min, evening screen time by +19 min and bedroom screen time by +7 min. There were no changes in sleep or diet from spring 2018 to 2019 (Table 4, spring maturation change). Similar trends in activity and screen time were observed in the summers prior to the pandemic. However, children slept −17 min less, went to bed +12 min later and consumed more healthy and unhealthy foods from summer 2018 to summer 2019 (Table 4, summer maturation change).
TABLE 4.
Linear mixed model estimates for behavioural outcomes adjusted for age, sex and race (Spring 2018–2020)
| Spring maturation change | Pandemic additional change | Summer maturation change | Pandemic additional change | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spring 2019–Spring 2018 | (Spring 2020‐Spring 2019)—(Maturation) | Summer 2019–Summer 2018 | (Summer 2020‐Summer 2019)—(Maturation) | |||||||||
| Coefficient | SE | 95% CI | Coefficient | SE | 95% CI | Coefficient | SE | 95% CI | Coefficient | SE | 95% CI | |
| Physical activity (min) | ||||||||||||
| Light PA | −17.1 | 4.0 | (−25.0, −9.3) | −68.9 | 7.7 | (−83.9, −53.9) | −25.3 | 5.8 | (−36.6, −14.0) | −26.9 | 10.5 | (−47.4, −6.4) |
| MVPA | −7.5 | 1.8 | (−11.1, −3.9) | −7.9 | 3.5 | (−14.9, −1.0) | −3.9 | 2.7 | (−9.1, 1.4) | −11.4 | 4.9 | (−20.9, −1.9) |
| Sedentary behaviour (min) | 24.8 | 4.8 | (15.4, 34.3) | 78.8 | 9.3 | (60.6, 97.1) | 26.5 | 7.0 | (12.8, 40.2) | 44.2 | 12.7 | (19.3, 69.2) |
| Sleep | ||||||||||||
| Minutes asleep | −2.9 | 2.8 | (−8.4, 2.6) | 17.4 | 5.6 | (6.4, 28.4) | −17.3 | 4.2 | (−25.5, −9.0) | 35.9 | 7.8 | (20.6, 51.3) |
| Bedtime | −2.1 | 3.1 | (−8.2, 5.0) | 117.9 | 6.2 | (105.7, 130.1) | 11.6 | 4.6 | (2.5, 20.6) | 40.1 | 8.6 | (23.3, 57.0) |
| Waketime | −3.2 | 3.4 | (−9.8, 4.4) | 130.4 | 6.8 | (117.1, 143.6) | 1.0 | 5.0 | (−9.8, 10.9) | 59.5 | 9.4 | (41.1, 77.9) |
| Midpoint | −2.7 | 2.9 | (−8.4, 4.0) | 124.2 | 5.8 | (112.9, 135.5) | 6.3 | 4.3 | (−3.1, 14.7) | 49.8 | 8.0 | (34.2, 65.5) |
| Midpoint ISD | −8.0 | 6.1 | (−19.9, 3.9) | 33.4 | 11.7 | (10.5, 56.4) | −9.1 | 7.7 | (−24.2, 6.0) | 47.0 | 14.2 | (19.2, 74.8) |
| Screen time (min) | ||||||||||||
| Total ST | 22.1 | 6.2 | (9.8, 34.3) | 97.2 | 9.3 | (79.0, 115.4) | 30.7 | 5.8 | (19.4, 42.0) | 18.3 | 8.8 | (1.1, 35.4) |
| Evening ST | 19.2 | 3.4 | (12.5, 25.9) | 9.7 | 5.0 | (0.0, 19.52) | 20.9 | 3.2 | (14.7, 27.0) | −7.1 | 4.8 | (−16.4, 2.3) |
| Bedroom ST | 6.5 | 1.9 | (2.9, 10.2) | 1.6 | 2.7 | (−3.8, 6.9) | 8.4 | 1.7 | (5.0, 11.7) | −1.4 | 2.6 | (−6.5, 3.7) |
| Diet | ||||||||||||
| Healthy foods | 0.1 | 0.1 | (0.0, 0.2) | 0.3 | 0.1 | (0.2, 0.5) | 0.1 | 0.1 | (0.0, 0.2) | 0.2 | 0.1 | (0.1, 0.3) |
| Unhealthy foods | 0.1 | 0.1 | (−0.1, 0.2) | 1.2 | 0.1 | (1.0, 1.5) | 0.5 | 0.1 | (0.3, 0.6) | 0.2 | 0.1 | (0.0, 0.5) |
Note: Bolded values indicate p < 0.05. Healthy foods ranged from 0 to 3 and unhealthy foods ranged from 0 to 14 with higher values indicating greater daily consumption. Wear time was included as a covariate for PA and sedentary behaviour models. Mean minutes asleep was included as a covariate for the sleep midpoint ISD model. MVPA and Bedroom ST were winsorized at 5% due to high skew.
Abbreviation: ISD, individual standard deviation; MPVA, moderate‐to‐vigorous physical activity; PA, physical activity; ST, screen time.
During the pandemic, behavioural changes accelerated compared to pre‐pandemic changes. Sedentary behaviour increased by an additional +79 min, light PA and MVPA decreased by an additional −69 and −8 min, respectively (Figure 1A, and Table 2, pandemic spring additional change). Children slept an additional +17 min and sleep midpoint shifted later by an additional +124 min, reflected in later bed and wake times (Figure 2A,B). Individual variability in sleep midpoint increased by +33 min. Total screen time increased by an additional +97 min, while evening and bedroom screen time were consistent with previous maturational trends (Figure 1B). Consumption of both healthy and unhealthy foods increased by an additional +0.3 and +1.2 foods, respectively (Figure 1C). A similar, but less dramatic pattern of results was observed for summer, except for unhealthy food consumption where increases were not above what might have been expected given previous trends in summer eating habits (Table 4, pandemic summer additional change).
FIGURE 1.
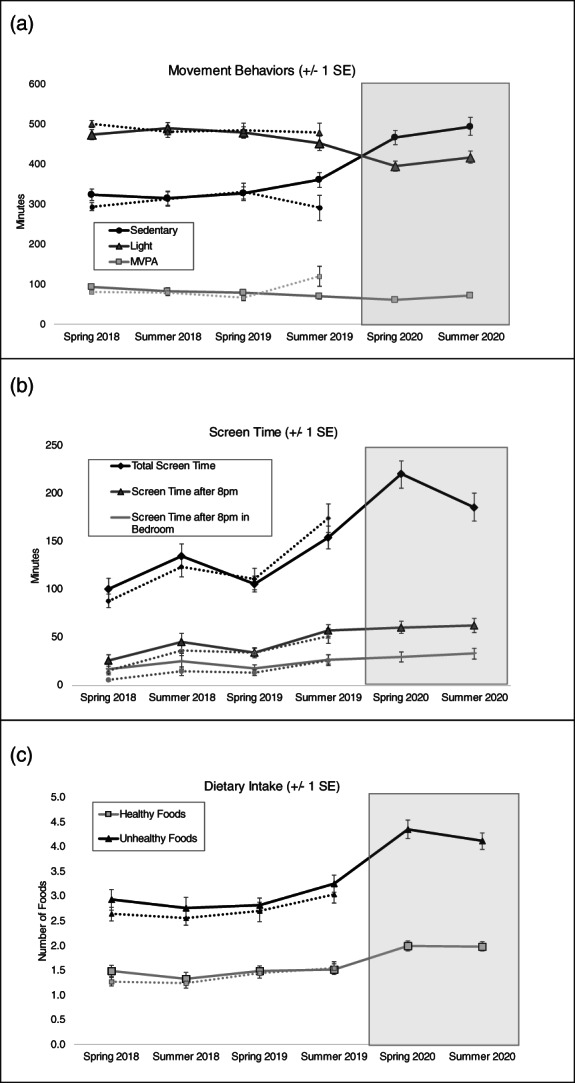
Mean estimates of (A) physical activity and sedentary behaviour, (B) screen time, and (C) dietary intake. Dotted lines indicate the trajectory for children who only provided data in 2018 and/or 2019. Solid lines indicate the trajectory for children who participated in the 2020 subsample. Raw means and standard deviations are presented in Table 3
FIGURE 2.
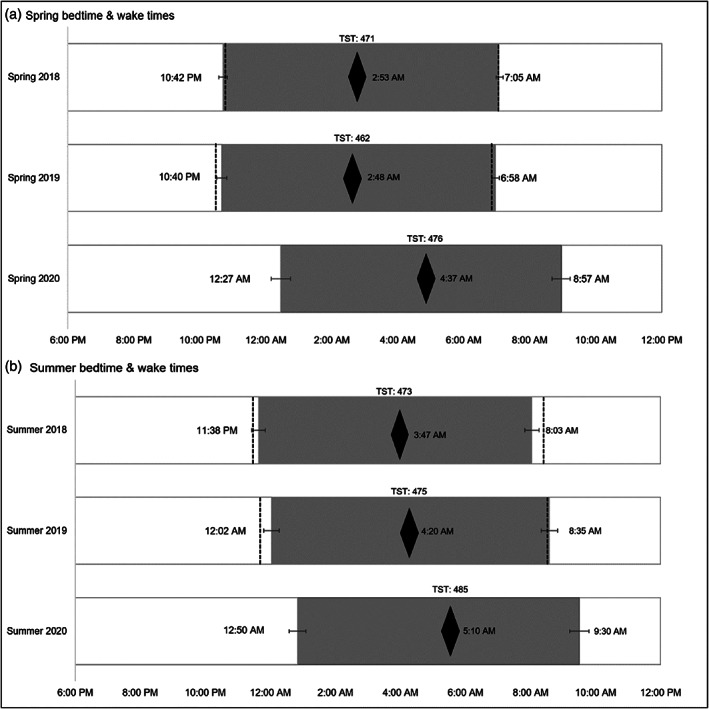
Bedtime, wake time and sleep midpoint by year. Black diamonds, sleep midpoint; TST, total sleep time in minutes. Dotted lines indicate the bed and wake times for children who only provided data in 2018 and/or 2019. Grey boxes represent children who participated in the 2020 subsample
4. DISCUSSION
This is one of the first studies to report objective data on the degradation of elementary schoolers' behaviours during the COVID‐19 pandemic. Compared to pre‐pandemic measures, children's PA, sleep timing, screen time, and diet were significantly worsened during the COVID‐19 pandemic, even after accounting for previous maturational trends from years prior. Our findings are generally in line with initial cross‐sectional and retrospective studies, that support, and even exceed the prediction that the COVID‐19 pandemic will “exacerbate all of the risk factors for weight gain associated with summer recess.” 7 While any one of these behavioural changes might be concerning, their confluence for such an extended period of time may have significant health impacts, including dramatic increases in childhood obesity. 43
Our findings are among the first to provide objective data that support retrospective parental perceptions of decreased activity and increased sedentary behaviour among pre‐adolescents (age 8–12), 9 and are among the first conducted in the United States. 9 , 44 While the increase in springtime screen use is largely influenced by virtual learning, patterns established in the spring persisted into summer, even in the absence of virtual school. While high levels of sedentary behaviour and screen time along with reduced PA levels could be attributed to continued pandemic restrictions and potential relaxed parental rules to allow children to connect with friends virtually, they might reflect new entrenched behaviour patterns that persist even in the absence of pandemic restrictions. Although there were minor changes in sleep duration, the dramatic shift in timing is concerning. On average, children's sleep timing was shifted by nearly 2 hours during the spring, likely attributable to the lack of external structure provided by in‐person school. Mounting evidence of shifted sleep timing is worrisome, 14 , 15 , 16 as sleep timing, independent of sleep duration, is linked with overweight and obesity. 43
Evidence for potential health impacts of changes in children's health behaviours stems from previous work examining behavioural changes during extended breaks from the structured school year (e.g., summer vacation), weekends and short breaks (e.g., spring/winter break). Later shifts in sleep timing and reductions in PA levels are evident during school breaks as little as one week in length and even more so during a three‐week break. 28 In a natural experiment examining children's obesogenic behaviours during structured and unstructured periods, children's sedentary behaviour, screen time, and sleep timing worsened during a traditional 12‐week summer vacation compared to those who remained in more structured settings (i.e., children attending year‐round school with a shorter 5‐week summer vacation). These behavioural changes corresponded to a statistically significant acceleration in zBMI gain in children during the traditional 12‐week summer vacation suggesting that structured environments have a protective effect on children's health outcomes. 24
It is possible that the pandemic‐related behaviour changes observed in the present study mimic an extended summer vacation period, and thus, potential health impacts would align with observed trends in accelerated weight gain during the summer months. 45 In addition to obesity risk, children who exhibit poor health behaviours (e.g., low PA, high sedentary behaviour, high screen time, poor sleep) compared to those meeting recommended levels of health behaviours have lower aerobic fitness, worse cardiometabolic indicators such as systolic blood pressure, insulin and triglycerides, 46 and poor mental and social health. 47 In a longitudinal study of 8–11 year old children followed over 6.5 months, children who experienced unfavourable changes in physical activity, sleep duration and sedentary time had an increased cardiometabolic risk profile (e.g., higher HOMAIR and lower HDL‐C) compared to those who experienced favourable changes over the same time period. 48 Therefore, it is imperative that intervention strategies target behavioural changes observed during the pandemic to limit the risk of associated poor health outcomes in children.
The results of this study should be interpreted within the context of its limitations. Although this is one of the first studies to report objectively measured sleep and PA in elementary schoolers during the COVID‐19 pandemic, diet and screen time were parent‐reported. However, by conducting surveys on multiple random days at each time point over the course of three years, we reduced the threat of recall bias, a limitation of many existing screen time and diet measures. While it is surprising that no significant increases were observed for nighttime and bedroom screen use, this may reflect parents limited awareness of their child's nighttime screen habits, especially in the context of our delayed bedtime findings which is often linked with increased screen time. 17 Along similar lines, it is also notable that parents reported children ate both more healthy and unhealthy foods during the pandemic. While parents may have been unaware of evening screen time, it is possible that they were more aware of their child's eating habits during the pandemic given the increase in daily time spent together and at home. 11 Our study did not differentiate between academic and non‐academic screen use, and it remains unclear if screen content impacts the well‐documented link between screen time and negative health outcomes. 49 As necessity of screens has been firmly established, future research should emphasize the quality and function of screen time, as well as the potential displacement of other healthy behaviours. It is also worth noting the limited retention for the 2020 subsample. While there were no significant differences in behaviour pre‐pandemic between those who did and did not participate in the additional measurements, this study is subject the potential threat of selection bias. Finally, although we were able to statistically control for one year of maturation using multiple measurement time periods prior to the pandemic onset, it is possible that some degree of maturation was not accounted for and could influence the results. For example, our model implies that the pre‐pandemic maturational changes are of similar magnitude to those that would occur due to maturation during the pandemic. However, it is possible that children's behaviours may change at a faster rate as they age, which may impact the results.
4.1. Future directions
It is unclear if the behavioural patterns observed in the spring and summer of 2020 will persist, even after the re‐introduction of structured environments (i.e., in‐person school, extracurricular activities, summer camps). Health behaviours like engaging in PA, limiting screen time, or practicing good sleep hygiene need to be completed frequently and consistently. Lapses in health behaviours, even for short periods of time, can have immediate negative physical and mental health consequences. Of greater concern is that they can increase vulnerability to the development of unhealthy behaviour patterns that become entrenched. 50 The longer unhealthy habits are practiced (i.e., through multiple days of unstructured social distancing measures) the more ingrained they become. Continued longitudinal data following the eventual relaxation of these precautions is needed to understand the acute as well as potential long‐term impacts of removing external structure on children's health behaviour patterns. The significant degradation in children's PA, sleep timing, screen time, and diet in addition to preliminary reports of drastic increases in childhood obesity 43 highlights the need for swift and resounding intervention efforts to stimy and repair the devastating trajectory of children's behavioural health.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Sarah Burkart revised data collection materials, collected data, conducted statistical analyses, led the interpretation of data, drafted the initial manuscript and revised the final manuscript. Hannah Parker conducted initial analyses, drafted the initial manuscript and revised the manuscript. R. Glenn Weaver conceptualized and designed, obtained funding and coordinated data collection for the original study, contributed to data interpretation and critically reviewed and revised the manuscript. Michael W. Beets assisted with conceptualization of the original study, contributed to data interpretation, and critically reviewed and revised the manuscript. Elizabeth L. Adams, Jean‐Philippe Chaput, Alexis Jones contributed to the interpretation of data and critically revised the manuscript for important intellectual content. Bridget Armstrong conceptualized and designed the ancillary study, obtained funding for the ancillary study, revised data collection instruments, contributed to interpretation of data, drafted the initial manuscript and revised the final manuscript. All authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Supporting information
Table S1. Number of children with valid measures by year
Figure S1. Overlapping timeline of study‐related events and South Carolina's COVID‐19 response
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R21HD095164 and a COVID‐19 Research Initiative grant from the Office of the Vice President for Research at the University of South Carolina. Work on this article was supported in part by the National Institute of General Medical Sciences for the UofSC Research Centre for Child Well‐Being (P20GM130420; Armstrong & Weaver), the National Institute of General Medical Sciences (T32GM081740; Jones) and the National Heart, Lung and Blood Institute (F32HL154530; Burkart) of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Burkart S, Parker H, Weaver RG, et al. Impact of the COVID‐19 pandemic on elementary schoolers' physical activity, sleep, screen time and diet: A quasi‐experimental interrupted time series study. Pediatric Obesity. 2022;17(1):e12846. 10.1111/ijpo.12846
Funding information Eunice Kennedy Shriver National Institute of Child Health and Human Development, Grant/Award Number: R21HD095164; National Heart, Lung, and Blood Institute, Grant/Award Number: F32HL154530; National Institute of General Medical Sciences, Grant/Award Numbers: P20GM130420, T32GM081740; Office of the Vice President for Research, University of South Carolina, Grant/Award Number: COVID‐19 Research Initiative
REFERENCES
- 1. Couzin‐Frankel J, Vogel G, Weiland M. Not open and shut: School openings across globe suggest ways to keep coronavirus at bay, despite outbreaks. American Association for the Advancement of Science, 369; 2020:241‐245. [DOI] [PubMed]
- 2. Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act. 2017;14(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nicholson LM, McLeod Loren D, Reifenberg A, Beets MW, Bohnert AM. School as a protective setting for excess weight gain and child obesity: a meta‐analysis. J Sch Health. 2021;91(1):19‐28. [DOI] [PubMed] [Google Scholar]
- 4. Baranowski T, O'Connor T, Johnston C, et al. School year versus summer differences in child weight gain: a narrative review. Child Obes. 2014;10(1):18‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. von Hippel PT, Workman J. From kindergarten through second grade, US children's obesity prevalence grows only during summer vacations. Obesity. 2016;24(11):2296‐2300. [DOI] [PubMed] [Google Scholar]
- 6. Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11:E101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID‐19–related school closings and risk of weight gain among children. Obesity. 2020;28(6):1008‐1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chulvi‐Medrano I, Villa‐González E, Rebullido TR, Faigenbaum AD. The impact of COVID‐19 quarantine on youth: from physical inactivity to pediatric depreobesity. J Movement Health. 2020;18(1):1–4. [Google Scholar]
- 9. Dunton GF, Do B, Wang SD. Early effects of the COVID‐19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20:(1). 10.1186/s12889-020-09429-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID‐19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carroll N, Sadowski A, Laila A, et al. The impact of COVID‐19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12(8):2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mitra R, Moore SA, Gillespie M, et al. Healthy movement behaviours in children and youth during the COVID‐19 pandemic: exploring the role of the neighbourhood environment. Health Place. 2020;65:102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28(8):1382‐1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gruber R, Saha S, Somerville G, Boursier J, Wise MS. The impact of COVID‐19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 2020;76:33‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu Z, Tang H, Jin Q, et al. Sleep of preschoolers during the coronavirus disease 2019 (COVID‐19) outbreak. J Sleep Res. 2020;30:e13142. [DOI] [PubMed] [Google Scholar]
- 16. Cellini N, Di Giorgio E, Mioni G, Di Riso D. Sleep quality, timing, and psychological difficulties in Italian school‐age children and their mothers during COVID‐19 lockdown. J Pediatr Psychol. 2021;46(2):153‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Olds TS, Maher CA, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34(10):1299‐1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hjorth MF, Chaput J‐P, Michaelsen K, Astrup A, Tetens I, Sjödin A. Seasonal variation in objectively measured physical activity, sedentary time, cardio‐respiratory fitness and sleep duration among 8–11 year‐old Danish children: a repeated‐measures study. BMC Public Health. 2013;13(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Twenge JM, Campbell WK. Associations between screen time and lower psychological well‐being among children and adolescents: evidence from a population‐based study. Prev Med Rep. 2018;12:271‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tăut D, Băban A, Giese H, de Matos MG, Schupp H, Renner B. Developmental trends in eating self‐regulation and dietary intake in adolescents. Appl Psychol Health Well Being. 2015;7(1):4‐21. [DOI] [PubMed] [Google Scholar]
- 21. Evans S, Mikocka‐Walus A, Klas A, et al. From ‘it has stopped our lives’ to ‘spending more time together has strengthened bonds': the varied experiences of Australian families during COVID‐19. Front Psychol. 2020;11:2906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Biglan A, Ary D, Wagenaar AC. The value of interrupted time‐series experiments for community intervention research. Prev Sci. 2000;1(1):31‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weaver RG, Hunt E, Rafferty A, et al. The potential of a year‐round school calendar for maintaining children's weight status and fitness: preliminary outcomes from a natural experiment. J Sport Health Sci. 2020;9(1):18‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weaver RG, Armstrong B, Hunt E, et al. The impact of summer vacation on Children's obesogenic behaviors and body mass index: a natural experiment. Int J Behav Nutr Phys Act. 2020;17(1):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cook TD, Campbell DT, Shadish W. Experimental and Quasi‐Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- 26. Zhang Y, Weaver RG, Armstrong B, Burkart S, Zhang S, Beets MW. Validity of wrist‐worn photoplethysmography devices to measure heart rate: a systematic review and meta‐analysis. J Sports Sci. 2020;38(17):2021‐2034. [DOI] [PubMed] [Google Scholar]
- 27. de Zambotti M, Baker FC, Willoughby AR, et al. Measures of sleep and cardiac functioning during sleep using a multi‐sensory commercially‐available wristband in adolescents. Physiol Behav. 2016;158:143‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weaver RG, Beets MW, Perry M, et al. Changes in children's sleep and physical activity during a 1‐week versus a 3‐week break from school: a natural experiment. Sleep. 2019;42(1):zsy205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Epstein LH, Paluch RA, Kalakanis LE, Goldfield GS, Cerny FJ, Roemmich JN. How much activity do youth get? A quantitative review of heart‐rate measured activity. Pediatrics. 2001;108(3):e44. [DOI] [PubMed] [Google Scholar]
- 30. Welk GJ, Corbin CB. The validity of the Tritrac‐R3D activity monitor for the assessment of physical activity in children. Res Q Exerc Sport. 1995;66(3):202‐209. [DOI] [PubMed] [Google Scholar]
- 31. Sallis JF, Buono MJ, Roby JJ, Carlson D, Nelson JA. The Caltrac accelerometer as a physical activity monitor for school‐age children. Med Sci Sports Exerc. 1990;22(5):698. [DOI] [PubMed] [Google Scholar]
- 32. Janz KF. Validation of the CSA accelerometer for assessing children's physical activity. Med Sci Sports Exerc. 1994;26(3):369‐375. [PubMed] [Google Scholar]
- 33. Simons‐Morton BG, Taylor WC, Huang IW. Validity of the physical activity interview and Caltrac with preadolescent children. Res Q Exerc Sport. 1994;65(1):84‐88. [DOI] [PubMed] [Google Scholar]
- 34. Tudor‐Locke C, Barreira TV, Schuna JM, et al. Improving wear time compliance with a 24‐hour waist‐worn accelerometer protocol in the international study of childhood obesity, lifestyle and the environment (ISCOLE). Int J Behav Nutr Phys Act. 2015;12(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bei B, Wiley JF, Trinder J, Manber R. Beyond the mean: a systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med Rev. 2016;28:108‐124. [DOI] [PubMed] [Google Scholar]
- 36. Neuhouser ML, Lilley S, Lund A, Johnson DB. Development and validation of a beverage and snack questionnaire for use in evaluation of school nutrition policies. J Am Diet Assoc. 2009;109(9):1587‐1592. [DOI] [PubMed] [Google Scholar]
- 37. Kasper N, Mandell C, Ball S, Miller AL, Lumeng J, Peterson KE. The healthy meal index: a tool for measuring the healthfulness of meals served to children. Appetite. 2016;103:54‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Eisenmann JC, Bartee RT, Wang MQ. Physical activity, TV viewing, and weight in US youth: 1999 youth risk behavior survey. Obes Res. 2002;10(5):379‐385. [DOI] [PubMed] [Google Scholar]
- 39. Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children's physical activity, sedentary time, and screen time by socioeconomic status. Int J Behav Nutr Phys Act. 2012;9(1):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963‐975. [DOI] [PubMed] [Google Scholar]
- 41. Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57(8):1152‐1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B Stat Methodol. 1995;57(1):289‐300. [Google Scholar]
- 43. Weaver RG, Hunt ET, Armstrong B, et al. COVID‐19 school closures Lead to a 10‐fold increase in BMI z‐score gain: an interrupted time‐series study. Am J Prev Med. 2021;S0749‐3797(21):00236‐00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Garcia JM, Lawrence S, Brazendale K, Leahy N, Fukuda D. Brief report: the impact of the COVID‐19 pandemic on health behaviors in adolescents with autism Spectrum disorder. Disabil Health J. 2020;14:101021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Weaver RG, Beets MW, Brazendale K, Brusseau TA. Summer weight gain and fitness loss: causes and potential solutions. Am J Lifestyle Med. 2019;13(2):116‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Carson V, Chaput J‐P, Janssen I, Tremblay MS. Health associations with meeting new 24‐hour movement guidelines for Canadian children and youth. Prev Med. 2017;95:7‐13. [DOI] [PubMed] [Google Scholar]
- 47. Janssen I, Roberts KC, Thompson W. Is adherence to the Canadian 24‐hour movement behaviour guidelines for children and youth associated with improved indicators of physical, mental, and social health? Appl Physiol Nutr Metab. 2017;42(7):725‐731. [DOI] [PubMed] [Google Scholar]
- 48. Hjorth MF, Chaput J‐P, Damsgaard CT, et al. Low physical activity level and short sleep duration are associated with an increased cardio‐metabolic risk profile: a longitudinal study in 8‐11 year old Danish children. PloS One. 2014;9(8):e104677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Carson V, Hunter S, Kuzik N, et al. Systematic review of sedentary behaviour and health indicators in school‐aged children and youth: an update. Appl Physiol Nutr Metab. 2016;41(6):S240‐S265. [DOI] [PubMed] [Google Scholar]
- 50. Dunton GF, Rothman AJ, Leventhal AM, Intille SS. How intensive longitudinal data can stimulate advances in health behavior maintenance theories and interventions. Transl Behav Med. 2019;11(1):281‐286. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Number of children with valid measures by year
Figure S1. Overlapping timeline of study‐related events and South Carolina's COVID‐19 response


