Abstract
Background
Since introducing the SARS-CoV-2 vaccination, different adverse effects and complications have been linked to the vaccine. Variable neurological complications have been reported after receiving the COVID-19 vaccine, such as acute encephalopathy.
Case presentation
In this report, we describe a 32-year-old previously healthy man who developed acute confusion, memory disturbances, and auditory hallucination within 24 hours from getting his first dose of the COVID-19 Moderna vaccine.EEG showed features of encephalopathy, CSF investigations were nonspecific, and MRI head did not depict any abnormality. He received five days of ceftriaxone and acyclovir without any benefit.
Discussion
Extensive workup for different causes of acute encephalopathy, including autoimmune encephalitis, was negative. Also, Our patient improved dramatically after receiving methylprednisolone, supporting an immune-mediated mechanism behind his acute presentation. Accordingly, we think the COVID-19 vaccine is the only possible cause of our patient presentation, giving the temporal relationship and the absence of other risk factors for encephalopathy.
Conclusion
the clinician should be aware of the possible neurological complications of the different COVID-19 vaccines. Further research is needed to clarify the pathophysiology of such complications.
Keywords: COVID-19, Vaccination, SARS-CoV-2, Encephalopathy, Adverse reaction, Case report
Highlights
-
•
Neurological complications have been reported in patients who received the COVID-19 vaccine.
-
•
It is still not confirmed if these complications are accidentally or casually related to the COVID-19 vaccine.
-
•
The pathophysiology of those complications is still not established, most likely related to immune mediated mechanism.
-
•
Steroid therapy seems to be effective in the treatment of acute encephalopathy related to COVID-19 vaccination.
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) appeared in December 2019 and caused the coronavirus disease 2019 (COVID‐19). COVID -19 is a systemic disease condition that can lead to various systemic complications affecting almost any system in the body. Recently, different types of COVID-19 vaccines have been distributed worldwide; however, despite the updated studies on these vaccines and their safety, there are several registered complications that can be related to the vaccine [1]. Neurological complications, such as autoimmune encephalitis, demyelination diseases, Guillain‐Barré syndrome (GBS), seizures, and acute encephalopathy, have been reported in patients who received the COVID-19 vaccine. Nevertheless, it is still speculative if these complications are accidentally or casually related to the COVID-19 vaccine. The pathophysiology of those complications is still not well understood and only based on hypotheses [[2], [3], [4]] [[2], [3], [4]] [[2], [3], [4]]. Herein, we report a case of acute encephalopathy within a day of receiving the first dose of the COVID-19 vaccine (Moderna). Extensive workup, including brain imaging and autoimmune disorders investigation, resulted in negative. Notably, our patient responded dramatically to methylprednisolone that might point to an immune-related phenomenon. Accordingly, we believe that the vaccine is the only possible culprit for this acute presentation in our patient. This case report has been reported in line with the SCARE Criteria [5].
2. Presentation of case
A 32-year-old Asian male was brought to the emergency department by his neighbors on May 28th, 2021, because he was seen roaming around his apartment with confusion and agitation. Proper history could not be taken as he was disoriented and amnesic. However, he had no significant past medical history based on his electronic medical record and family information. Also, there was no history of psychiatric illnesses, alcohol use disorder, or other substances abuse. Interestingly, he received the first dose of SARS-Cov-2 vaccination (Moderna vaccine) on May 26th, 2021 (two days before the presentation), and that was the last time seen fine. Upon presentation, he was afebrile and vitally stable. The neurological examination was unremarkable, apart from agitation, disorientation to time, place, person, and memory disturbances.
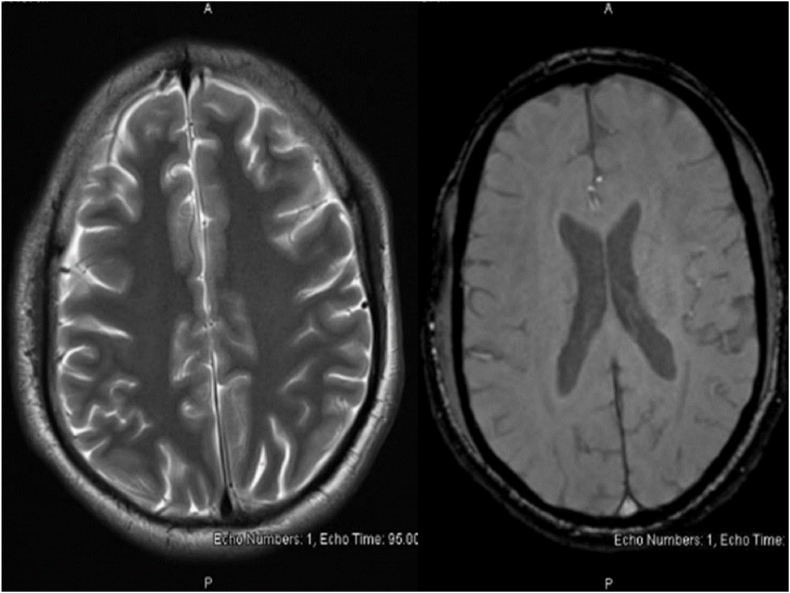
His laboratory results, including alcohol and toxicology screen, were negative. COVID-19 PCR test was negative (repeated twice). Lumbar puncture with Cerebrospinal fluid (CSF) studies was done, and it showed elevated protein levels (0.76 gm/L, reference range = 0.15–0.45) with average cell counts (white blood cells of 3 u/L) and glucose levels. Also, CSF oligoclonal band, HSV PCR, VDRL came negative.EEG showed findings suggestive of acute encephalopathy (slowed background activity). Magnetic resonance imaging (MRI) of the brain did not reveal any acute or chronic abnormality (Fig. 1).
Fig. 1.
MRI of the brain revealed no abnormality.
During his hospital stay, he received a five-day course of ceftriaxone and acyclovir for suspected meningoencephalitis, but his disorientation and aggressiveness got worse. Additionally, he developed auditory hallucinations and abnormal behaviours. He received multiple doses of haloperidol and lorazepam and finally required bed restraints. Based on his clinical manifestations, autoimmune encephalitis was suspected, and empirical intravenous methylprednisolone (1 g/day) was started on day six of the hospital stay. After two doses of methylprednisolone, he showed a dramatic improvement and became able to understand and answer our questions. He confirmed that he started to develop forgetfulness and mood disturbance within 24 hours of receiving the covid-19 vaccine dose, but he did not remember what happened after that. CSF extensive workup for autoimmune encephalitis (including anti-aquaporin-4, anti-myelin basic protein, anti-myelin oligodendrocyte glycoprotein, anti-glial fibrillary acidic protein, anti-NMDAR, anti-GAD, and other autoimmune encephalitis antibodies) was negative. He was discharged from the hospital after receiving three days of methylprednisolone. At follow-up in our outpatient clinic (one month after the discharge), he was asymptomatic and fully oriented.
Patient perspective: “Actually, this was the first time during my life I felt like I could not remember anything. It was a very terrifying period and I hope that it will not happen again. Obviously, I think that the vaccine is the only possible explanation for my disease. Honestly, I am not sure if I will be able to take the second dose of the vaccine”.
3. Discussion
COVID‐19‐related encephalopathy has been reported infrequently since the beginning of the pandemic. Initially, this condition was attributed to direct invasion of the brain by SARS‐CoV‐2; however, SARS‐CoV‐2 RNA usually has not been detected in the cerebrospinal fluid (CSF) of those patients with encephalopathy. In addition to that, CSF analysis, neuroimaging, histopathological findings, and the clinical response to immunosuppressant therapy (such as a steroid), found to be consistent with immune‐related pathogenesis involving the brain rather than a direct infectious process targeting the brain. Thus, a cytokine‐mediated inflammatory process is proposed as the key pathophysiological mechanism for COVID‐19‐related encephalopathy, known as cytokine storm-associated encephalopathy (CySE) [[6], [7], [8]].
Neurological symptoms like pain, headache, dizziness, or muscle spasms are common and self-limited adverse effects after receiving the COVID-19 vaccine. However, major neurological complications, despite the unproven causality, have been reported since the introduction of the COVID-19 vaccine, such as facial palsy, Guillain-Barre syndrome(GBS), seizures, strokes, transverse myelitis, and acute disseminated encephalomyelitis (ADEM) [2].In addition, an unexplained acute encephalopathy state has also been described after receiving the COVID-19 vaccine [3,9]. Regarding the pathogenesis of COVD-19 vaccine-associated complications, It has been proposed that spike protein expression by human cells (after translation of the mRNA COVID-19 vaccine by human cells) might trigger an inflammatory reaction, similar to that induced by the virus itself, leading to those neurological complications [3,6,10]. However, elevated inflammatory markers, including cytokines, were not detected in many reported cases of covid-19 vaccine-related encephalopathy (based on USA's Vaccine Adverse Event Reporting System) [9]; Therefore, we believe that other unknown mechanisms might lead to such complications.
Our patient developed this acute hyperactive encephalopathy (based on clinical presentation, EEG findings, and MRI) within 24 hours of vaccine administration. Initially, meningoencephalitis was suspected; however, despite receiving five days course of ceftriaxone (to cover bacterial meningitis) and parenteral acyclovir (to cover herpes encephalitis), his condition had deteriorated more. We extensively investigated the patient for different causes of an acute encephalopathy, including autoimmune encephalitis work up, without reaching any diagnosis. Also, the patient's dramatic response to methylprednisolone might point to an immune-mediated mechanism behind his condition. Our case nearly resembles a recently reported case by L. Baldelli et al. [8] that describes the occurrence of hyperactive acute encephalopathy post-COVID-19 vaccine. Accordingly, we can link the development of acute encephalopathy in our patient to the vaccine due to the temporal relationship and the absence of other risk factors for encephalopathy in our patient.
4. Conclusion
Up to the best of our knowledge, this is the first reported case presented with acute encephalopathy after receiving the COVID-19 vaccine in Qatar. Our patient markedly improved with corticosteroid therapy supporting immune-mediated pathogenesis behind his clinical presentation. Further studies are required to describe the pathogenesis of COVID-19 vaccination-related complications and their optimal management. Finally, we believe that the vaccine's benefits outweigh the risk of any possible complications associated with its use. Albeit, clinicians should be aware of the COVID-19 vaccine's possible complications, and if they happen, they should not be considered coincident events and should be reported as soon as possible.
Ethical approval
Case report was approved by Hamad Medical Corporation Medical Research Centre.
Sources of funding
Open access funding was provided by Qatar National Library (QNL)
Author contribution
AFA: patient care, data gathering, literature review, manuscript writing. YMA: patient care, manuscript writing. NS: editing and revision of the final manuscript. All authors reviewed, edited, and approved the final version of the manuscript.
Registration of research studies
N/A.
Guarantor
Abdulrahman F. Al-Mashdali.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying image. A copy of the written consent is available for review by the Editor-in-Chief upon request.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and the accompanying image. A copy of the written consent is available for review by the Editor-in-Chief upon request.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
The authors have no competing of interest to declare.
Declaration of competing interest
All authors have no conflict of interest to declare.
Acknowledgments
The authors would like to acknowledge Qatar national library (QNL) for this publication's funding and the HMC internal medicine residency program for scientific support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102803.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Lu L., Xiong W., Mu J., Zhang Q., Zhang H., Zou L., Li W., He L., Sander J.W., Zhou D. The potential neurological effect of the COVID‐19 vaccines: a review. Acta Neurol. Scand. 2021;144:3–12. doi: 10.1111/ane.13417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goss A.L., Samudralwar R.D., Das R.R., Nath A. ANA investigates: neurological complications of COVID-19 vaccines. Ann. Neurol. 2021;89:856–857. doi: 10.1002/ana.26065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu B.D., Ugolini C., Jha P. Two cases of post-moderna COVID-19 vaccine encephalopathy associated with nonconvulsive status epilepticus. Cureus. 2021;13 doi: 10.7759/cureus.16172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao L., Ren L. Acute disseminated encephalomyelitis after severe acute respiratory syndrome coronavirus 2 vaccination: a case report. Acta Neurol. Belg. 2021:1–3. doi: 10.1007/s13760-021-01608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Scare Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Karnik M., Beeraka N.M., Uthaiah C.A., Nataraj S.M., Bettadapura A.D.S., Aliev G., Madhunapantula S.V. A review on SARS-CoV-2-induced neuroinflammation, neurodevelopmental complications, and recent updates on the vaccine development. Mol. Neurobiol. 2021:1–29. doi: 10.1007/s12035-021-02399-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pensato U., Muccioli L., Cani I., Janigro D., Zinzani P.L., Guarino M., Cortelli P., Bisulli F. Brain dysfunction in COVID‐19 and CAR‐T therapy: cytokine storm‐associated encephalopathy. Ann Clin Transl Neurol. 2021;8:968–979. doi: 10.1002/acn3.51348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perrin P., Collongues N., Baloglu S., Bedo D., Bassand X., Lavaux T., Gautier-Vargas G., Keller N., Kremer S., Fafi-Kremer S., Moulin B., Benotmane I., Caillard S. Cytokine release syndrome-associated encephalopathy in patients with COVID-19. Eur. J. Neurol. 2021;28:248–258. doi: 10.1111/ene.14491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldelli L., Amore G., Montini A., Panzera I., Rossi S., Cortelli P., Guarino M., Rinaldi R., D'Angelo R. Hyperacute reversible encephalopathy related to cytokine storm following COVID-19 vaccine. J. Neuroimmunol. 2021;358:577661. doi: 10.1016/j.jneuroim.2021.577661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Umapathi T., Quek W.M.J., Yen J.M., Khin H.S.W., Mah Y.Y., Chan C.Y.J., Ling L.M., Yu W.-Y. Encephalopathy in COVID-19 patients; viral, parainfectious, or both? ENeurologicalSci. 2020;21:100275. doi: 10.1016/j.ensci.2020.100275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.