Abstract
Aim
This study gives insights into the association between the use of personal protective equipment (PPE), wearing time of masks and stress among frontline nursing staff during the COVID‐19 pandemic.
Background
PPE can have physical consequences like headache and pain, which could result in increased nurse stress levels.
Methods
A total of 2600 nurses participated in this online survey. The questionnaire is based on literature and includes the perceived level of stress scale.
Results
We found no significant association between the use of PPE and stress. Nurses who wore masks for more than 8 h had significant higher stress levels than those who used the masks for a shorter period.
Conclusions
The duration of wearing masks is associated with nurse's stress level. Our findings can help nurses to argue a higher frequency of breaks and a maximum duration of mask usage in their organisations.
Implications for Nursing Management
We recommend that nursing managers implement practical strategies such as a mask break task force. This task force could promote awareness for mask breaks and recommend and allocate rooms or locations such as balconies for mask breaks.
Keywords: COVID‐19, nurses, personal protective equipment, psychological stress
1. INTRODUCTION
In March 2020, the Wold Health Organisation (WHO) assessed that COVID‐19 and the underlying severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) was characterized as a pandemic. Authors of a systematic review describe the main symptoms of COVID‐19 as fever and cough followed by fatigue (Grant et al., 2020). The WHO stated on 28 June 2020 that more than 9,840,000 confirmed cases, with nearly 500,000 deaths in 216 countries/areas, had been reported (WHO, 2020c). This pandemic has been internationally recognized as the biggest pandemic since the 1918 influenza pandemic.
One main challenge for each affected country has been to protect high‐risk groups and prevent a collapse of the health care system, and especially the intensive care system. This was done by, for example, social distancing, working in home office (if possible) and restricting treatments in hospitals insofar as possible.
Nevertheless, nursing staff are neither able to use social distancing nor to work in home office as preventive strategies. Beyond other health care professionals, they have to be available at the patients' bedsides 24/7. Therefore, it is of utmost importance to provide nursing staff with personal protective equipment (PPE), such as gloves or eyewear, including surgical face masks (SFM) and filtering facepiece masks (FFP masks), as the virus is distributed by contact or droplet transmission (WHO, 2020b). (Inter‐)national organisations have launched investigations on or even created regulations for the use of PPE (WHO, 2020e). An example would be McGilton et al who provide a list of considerations for infection control management in nursing homes, which might differ from, for example, acute care, based on (inter) national recommendations (McGilton et al., 2020). They noted a need to prepare and distribute videos or other resources to nursing home staff in order to provide them with information about the adequate and correct use and disposal of PPE as well as SFM/FFP masks and to update these as needed. They also recommended that experienced nurses teach nursing home staff how to follow the PPE and SFM/FFP masks guidelines and how to put on and take off the PPE and SFM/FFP masks safely. These guidelines often also include the maximum wearing time of the PPE and SFM/FFP masks. In April 2020, the WHO recommended the use of SFM masks without removing for up to 6 h during severe shortages, when caring for a cohort of COVID‐19 patients (WHO, 2020e). More recently, the WHO and the International Labour Organisation have described that due to, for example, PPE shortages and high workload, wearing a PPE for extended periods of time may be required (WHO & International Labour Organisation, 2021). This is similar to the recommendations made by the National Institute for Occupational Safety and Health regarding the extended use of N95 masks (National Institute for Occupational Safety and Health, 2020). These recommendations state that such masks should be used for extended periods, as touching them less frequently might result in a lower risk of contact transmission as opposed to taking the mask off and putting the same mask back on (National Institute for Occupational Safety and Health, 2020).
On the other hand, regulations with regard to occupational safety state a maximum wearing time of FFP masks up to 2 h, depending on the type, followed by a break of 30 min (Deutsche gesetzliche Unvallversicherung, 2011). In Austria, in February 2021, a new legal provision was adopted determining a maximum wearing time for masks of 3 h, followed by a 10‐min break (Federal Ministry for Labour, 2021).
However, several studies, letters and commentaries on PPE in general have been published since the COVID‐19 outbreak (Cook, 2020; Lockhart et al., 2020; Ong et al., 2020). It is known that wearing PPE, and specifically SFM/FFP masks, can have physical consequences like headache and pain among frontline health care workers (Ong et al., 2020). Even though the majority (64.6%) of the before mentioned study were nurses, the authors did not report their results separated for the different frontline health care workers (nurses, doctors, etc.). In addition, studies have found an association between headache and stress (Alkhudhairy et al., 2018; Krøll et al., 2017). Therefore, the use of SFM/FFP masks can potentially increase the stress levels among nursing staff over the long run, through, for example, headache. Moreover, a recent study with 20 healthy persons showed that the stress level measured with heart rate variability was increased by wearing masks (Tian et al., 2020). However, they also highlighted that wearing the mask for a long time can cause poor breathing and even hypoxia, which can lead to an increased level of stress (Tian et al., 2020). This is of interest because high levels of perceived stress can result in burnout and increase the risk that staff leave the nursing profession, an important consideration in light of the expected worldwide nursing shortage (Catton, 2020; WHO, 2016).
However, none of these studies placed a focus on SFM/FFP masks usage and wearing time and frontline nursing staff stress, even though the use of PPE and SFM/FFP masks is considered the only way to protect frontline nursing staff against COVID‐19 infection. Therefore, this study was carried out to give first insights into the association between the use of PPE including SFM/FFP masks, as well as wearing time of masks, and stress levels among frontline nursing staff, including registered nurses, nursing aids nursing students and specialized social carers, during the COVID‐19 pandemic.
2. METHODS
2.1. Design
This study employed a cross‐sectional design by using an online questionnaire. The online questionnaire was distributed through the open‐source, online statistical web survey app LimeSurvey. The link for the online survey was distributed by applying a snowball sampling technique. The link was posted on the first author's personal Twitter account and the official Facebook page of the respective Institute of Nursing Science.
2.2. Setting and sample
We included Austrian nursing staff from different settings (e.g., hospital and long‐term care) who worked at the frontline during the COVID‐19 pandemic. Frontline nursing staff were registered nurses, nursing aids, nursing students as well as specialized social carers. Because Austrian nurses are by law permitted to delegate certain tasks to nursing aids, we also included them in this survey. In addition, we also included, for example, nursing students, as they have also been working with COVID‐19 affected persons during the COVID‐19 pandemic in Austria, due to nursing staff shortage. Managers or nursing directors were not included in the data collection process, as the aim of the study was to gain insights into frontline nursing care during this pandemic.
2.3. Data collection instrument
Data were collected on sample characteristics such as age and gender. In addition, we collected information on the type of health care institution (e.g., hospital, long‐term care and rehabilitation), professional qualifications held by the staff member (i.e., registered nurse, nursing aid, nursing student and specialized social carers) and years of nursing experience (i.e., <5, 5–10, 11–20 or >20 years) even though these professionals are, by law, not included in the group of nursing professions. However, as nurses and nursing aids are allowed to delegate certain tasks to specialized social carers, we also included them in the analysis.
The questionnaire used was developed on the basis of Donabedian's quality of health care model (Donabedian, 1966), which includes three levels: the structural, process and outcome levels. The questions asked on the structural and process levels were developed on the basis of official recommendations from the WHO (WHO, 2020a, 2020d), the Austrian Government (Federal Ministry for Social Affairs, Health Care and Consumer Protection, 2020a, 2020b), or similar guidelines extracted from international publications (Mo et al., 2020; Ong et al., 2020).
Questions on the structural level related for example to the availability of PPE, such as SFM, FFP masks and eyewear. On the process level, we asked the participants whether they were using PPE, such as the use of SFM, FFP masks and eyewear (Yes/No). In order to avoid ambiguity, we inserted pictures of the various mask types in the online survey. In addition, the following note regarding FFP masks were incorporated in the online survey: ‘FFP masks are tested and licensed in Europe according to the EN 149 standard. A print on the mask indicates compliance with the EN 149 norm, the respective protective level (FFP1, FFP2 or FFP3) and the CE‐sign followed by a 4‐digit number.’
Moreover, we asked how long the participants wore the SFM as well as the FFP mask, before using a new one. They could choose from among the following options: less than 4 h, 4–8 h, more than 8 h or I do not use them.
On the outcome level, we used the validated perceived stress scale (PSS) to measure stress levels among the nursing staff (Cohen et al., 1983).
The PSS is available in the German language (Schneider et al., 2017) and shows good psychometric properties. Previous studies of the German PSS reported a good internal consistency with a Cronbach's alpha of 0.84 and good fit indices for construct validity (Klein et al., 2016). The Cronbach's alpha for our sample is similar with 0.866. Moreover, another study reported that the German PSS showed significant results for almost all associations with regard to concurrent validity (Reis et al., 2019). In addition, because it only includes 10 items, its use is highly practical (Klein et al., 2016). Each item was rated on a 5‐point Likert scale (0 = never; 1 = almost never; 2 = sometimes; 3 = fairly often; 4 = very often) (Klein et al., 2016). We used the sum score of all items to differentiate between 0–13 points indicating low stress, 14–26 moderate stress and 27–40 for high‐perceived stress, respectively, in accordance with various former studies (Alharbi & Alshehry, 2019; Drachev et al., 2020; Wiriyakijja et al., 2020).
The PSS has been used internationally in several studies with different samples, including pharmacy students, informal caregivers, nursing students and nursing staff (Falzarano & Siedlecki, 2021; Hirsch et al., 2020; Senocak & Demirkiran, 2020; Teresi et al., 2020).
2.4. Data analysis
We used SPSS version 26 for data analysis (IBM Corp. Released, 2019). We expressed categorical variables as frequencies and metric variables as means. To investigate associations between the use/wearing time of SFM/FFP masks and the staff member's stress level, we performed a chi‐square test. For the association between the wearing time of SFM/FFP masks and stress, we used Cramer's V as a measure of the effect size.
In order to give detailed insights into the results, we also performed Kruskal–Wallis tests, which can be used to make pairwise comparisons between categorical variables (wearing time less than 4 h vs. wearing time 4–8 h), with the PSS sum score as a metric variable. We considered a p value of <.05 as statistically significant.
2.5. Ethics
The study was approved by a responsible ethical committee (32–386 ex 19/20). On the first page of the documentation provided, all participants were informed of the aim of the study, the responsible organisation and the contact persons as well as data security. All data collected were anonymized, and IP addresses were not stored. In addition, the data created were stored on the server of the Medical University of Graz. All participants were asked to provide their written informed consent in the first question of the online survey, by means of ticking the respective box, to comply with the General Data Protection Regulation issued by the European Union.
3. RESULTS
Five participants out of the entire sample of 2602 individuals were 65 years or older, which is above the Austrian retirement age; therefore, data from these participants were excluded from this analysis. The majority of the participating nurses worked in hospitals (73.3%, n = 1903), followed by long‐term care institutions (17.2%, n = 447). Almost 80% (n = 2058) of the participants were nurses. Table 1 displays the sample characteristics.
TABLE 1.
Sample characteristics
| Nursing staff (N = 2597) | |
|---|---|
| Female % (n) | 83.8 (2175) |
| Mean age in years (SD) | 38 (11) |
| Area of work % (n) | |
| Hospital | 73.3 (1903) |
| Nursing home | 17.2 (447) |
| Other | 9.5 (247) |
| Professional qualification % (n) | |
| Nurse | 79.2 (2058) |
| Nursing aid | 11.9 (308) |
| Nursing student | 6.5 (170) |
| Specialized social carers | 2.3 (61) |
| Experience % (n) | |
| <5 years | 27.1 (704) |
| 5–10 years | 19.5 (506) |
| 11–20 years | 20.9 (543) |
| >20 years | 32.5 (844) |
Table 2 describes the main variables of interest. Nearly all participating nurses used SFM (97.9%, n = 2542) and protective gloves (95.6%, n = 2482) during their daily work. In addition, about three‐quarters (74.2, n = 1927) of the staff used FFP masks, and 55% (n = 1450) used protective eyewear such as glasses. Nearly half of the nursing staff wore the SFM (48.3%, n = 1254) and, respectively, the FFP masks (45.1%, n = 1172) for more than 8 h continuously. More than half of the nursing staff had moderate stress levels (56.8%, n = 1476), and 10.5% (n = 272) reported experiencing high stress levels.
TABLE 2.
Use of different PPE, SFM/FFP‐masks‐wearing time and perceived stress levels
| Nursing staff (N = 2597) | |
|---|---|
| Use of PPE % (n) | |
| SFM | 97.9 (2542) |
| FFP mask | 74.2 (1927) |
| Protective eyewear | 55.8 (1450) |
| Protective gloves | 95.6 (2482) |
| Protective gowns | 27.1 (1892) |
| Average wearing time of SFM % (n) | |
| Less than 4 h | 11.3 (293) |
| 4–8 h | 38.2 (993) |
| More than 8 h | 48.3 (1254) |
| I do not use them | 2.3 (57) |
| Average wearing time of FFP mask % (n) | |
| Less than 4 h | 8.0 (208) |
| 4–8 h | 24.8 (645) |
| More than 8 h | 45.1 (1172) |
| I do not use them | 22.0 (572) |
| PSS categories % (n) | |
| Low | 32.7 (849) |
| Moderate | 56.8 (1476) |
| High | 10.5 (272) |
| Mean PSS sum score (SD) | 16.9 (7.3) |
Abbreviations: FFP mask, filtering facepiece mask; PPE, personal protective equipment; PSS, perceived stress scale; SD, standard deviation; SFM, surgical face mask.
We found no statistically significant association between the use of masks, eyewear, gloves or gowns and stress (Table 3). However, one‐third of the nursing staff who used SFM/FFP masks experienced a low stress level (SFM 33.0%, n = 839; FFP mask 32.1%, n = 618). In contrast, less than 20% of nursing staff who did not wear SFM experienced a low stress level (18.2%, n = 10). Among the nurses who used gloves, 56% (n = 1404) reported experiencing a moderate stress level. This finding differed from that for nurses who did not wear gloves, of which 62% (n = 72) of whom experienced a moderate stress level.
TABLE 3.
Association of the use of different PPE and stress level
| Nursing staff perceived stress level % (n) | p value of effect size | Effect size Cramer | |||
|---|---|---|---|---|---|
| Low | Moderate | High | |||
| Use of SFM | |||||
| Yes (n = 2542) | 33.0 (839) | 56.6 (1438) | 10.4 (265) | .069 | 0.045 |
| No (n = 55) | 18.2 (10) | 69.1 (38) | 12.7 (7) | ||
| Use of FFP mask | |||||
| Yes (n = 1927) | 32.1 (618) | 57.5 (1108) | 10.4 (201) | .462 | 0.024 |
| No (n = 670) | 34.5 (231) | 54.9 (368) | 10.6 (71) | ||
| Use of protective eyewear | |||||
| Yes (n = 1436) | 32.6 (472) | 57.2 (830) | 10.2 (148) | .831 | 0.011 |
| No (n = 1141) | 32.9 (377) | 56.3 (646) | 10.8 (124) | ||
| Use of protective gloves | |||||
| Yes (n = 2482) | 32.8 (814) | 56.6 (1404) | 10.7 (264) | .306 | 0.030 |
| No (n = 115) | 30.4 (35) | 62.6 (72) | 7.0 (8) | ||
| Use of protective gowns | |||||
| Yes (n = 1892) | 32.8 (620) | 57.1 (1080) | 10.1 (192) | .663 | 0.017 |
| No (n = 705) | 32.5 (229) | 56.2 (396) | 11.3 (80) | ||
Abbreviations: FFP mask, filtering facepiece mask; PPE, personal protective equipment; SFM, surgical face mask.
Due to the fact, that even the wearing of the SFM or FFP does not influence the stress level, we also had a look at the association between the duration of wearing SFMor FFP masks and stress (Figure 1). The highest stress level was reported by nurses who wore masks for longer than 8 h (SFM 14.3%, n = 618; FFP mask 13.1%, n = 618).
FIGURE 1.
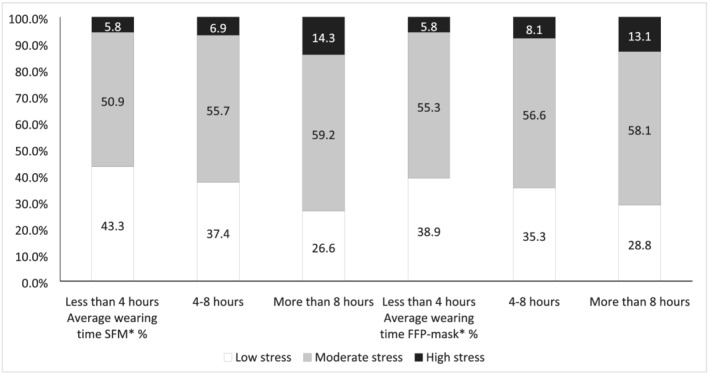
Association of duration of SFM/FFP‐mask usage and stress (*p value < .05). FFP mask, filtering facepiece mask; SFM, surgical face mask
According to the Kruskal–Wallis tests, comparing different wearing times with each other, we found the following results. Nurses who wore SFM masks for more than 8 h had statistically significant higher stress levels than those who used the SFM masks for less than 4 h (p value = .000) or from 4 to 8 h (p value = .000). Nurses who wore FFP masks for more than 8 h had statistically significantly higher stress levels than those who used these types of masks for less than 4 h (p value = .000) or from 4 to 8 h (p value = .000).
4. DISCUSSION
This study was carried out to investigate the association between the use of PPE including SFM/FFP masks, as well as wearing time of masks, and stress among nursing staff during the COVID‐19 pandemic.
Nearly all staff who participated in our online survey used SFM, and nearly 75% used FFP masks. The fact that not all participants wore masks is in contrast with the findings of a recent study, in which health care workers from a national university hospital in Singapore were investigated, placing a focus on PPE use and headaches (Ong et al., 2020). In this study, all participants wore FFP masks.
One possible reason for the differences in the use of masks is that most of the health care workers in the former study worked on high‐risk hospital wards, such as the isolation wards, emergency rooms—including a fever facility—and the medical intensive care unit (Ong et al., 2020). In contrast, our study included all types of health care institutions and wards. This might explain the higher rate of wearing masks and eyewear in the Singapore study.
In addition, we show that more than two‐thirds of the participants had moderate or even high‐perceived stress levels. There might be three possible explanations for not identifying a statistically significant association between the use of SFM/FFP masks and stress.
First, wearing masks and gloves is common in nursing practice, and wearing SFM and FFP masks has been/is mandatory during the COVID‐19 pandemic. Nurses generally have to be fully aware of the importance of PPE usage because it constitutes the only way to protect both themselves and the patients and residents they are caring for from infectious diseases. We are drawing on literature pertaining to norovirus to illustrate our points, as nurses are familiar with it and building knowledge around Covid‐19 is still ongoing. Being familiar with infectious viruses may be the reason why the usage of PPE itself was not associated with the perceived stress of nursing staff. Additionally, the pandemic itself might have caused stress for the nursing staff, which the usage of PPE might have not increased.
Second, viral illnesses are a highly prevalent in the hospital as well in the nursing home setting, in which more than 90% of our participating nursing staff were working. As an example, in a UK nursing home study, 257 outbreaks with a single viral cause pathogen were identified, of which 181 (70.4%) were caused by norovirus (Inns et al., 2019). So we assume that most of the participating staff is familiar with being exposed to a virus and therefore, not perceived the wearing of PPE as a stressful event.
Third, the interventions, recommended for limiting the spread of norovirus the prevention, include the use of gloves and masks, for example, when cleaning up vomit (Barclay et al., 2014), but also gowns and goggles, if a risk of splashing exists (Barclay et al., 2014). Being used to wearing PPE and being familiar with exposition to a virus was also frequently mentioned from nursing home staff, in an interview study, which is currently being analysed (Hoedl & Schoberer, 2020).
However, we could show that a statistically significantly association existed between the duration of the use of masks and stress.
Most of our study participants wore SFM and the FFP masks for more than 4 h (86.5% vs. 69.9%). This finding is in line with those for the health care staff working in high‐risk wards, who stated that they used the N95 masks on average 5.9 h each day (Ong et al., 2020). Such N95 masks can be considered as comparable with the FFP masks from the European Union (3M Personal Safety Division, 2020).
Two studies have been carried out to investigate the wearing time of N95 masks among health care workers (Radonovich et al., 2009; Rebmann et al., 2013). In the first study, the sample included 27 health care workers, 22 of which were nursing staff, and the median wearing time for eight different N95 masks ranged between 4.1 and 7.7 h (Radonovich et al., 2009), findings that are in line with our results focusing on FFP masks. The second study was carried out to investigate the levels of compliance regarding mask usage and compare this with physiological effects and subjective symptoms (Rebmann et al., 2013). In this study, 10 nurses participated, who had an average of 11 years of experience with wearing an N95 mask (Rebmann et al., 2013). The authors reported that the daily average wearing time ranged between 2.5 and 3.7 h and that 90% of the nurses tolerated the use of the mask for two 12‐h shifts (Rebmann et al., 2013). This different finding could be explained by the fact that our study was conducted during the COVID‐19 pandemic, when the risks and consequences of wearing or not wearing the masks were onmipresent. The former study by Rebmannet al., in contrast, was performed in 2013 at a time when no worldwide pandemic was ongoing; therefore, the results are not completely comparable.
We could show that nurses who wore a SFM less than 4 h and up to 8 h per day reported lower stress levels more often than nurses who wore the FFP mask for a longer time period. Similar results were found by Rebmann et al., which show that the daily average wearing time of an N95 mask alone was higher than the combination of wearing an N95 with a mask overlay (Rebmann et al., 2013). This finding might be explained by the fact that the N95 mask described by Rebmann et al. is thinner than an FFP mask in our study. In addition, these authors showed that wearing an N95 masks with an extra overlay statistically significantly increases CO2, nausea and visual challenges as compared with wearing a N95 mask alone (Rebmann et al., 2013).
Among the nursing staff, between 5.8% and 14.3% experienced high stress levels. Regardless of the type of masks, the perceived level of stress was statistically significant and positively correlated with the increased mask‐wearing time. Other studies have shown that mask‐wearing for more than 4 h per day is associated with headaches (Ong et al., 2020), increased levels of CO2, perceived exertion, shortness of breath, reported headaches, dizziness and communication difficulties (Rebmann et al., 2013). All of these effects can lead to discomfort, pain and consequently, an increase in the stress levels of nursing staff.
In another study, 59% of the participating nurses refused to wear the masks for more than 8 h. Their stated reasons included an intolerance to heat, pressure, or pain, dizziness, difficulties concentrating and interference with communication (Radonovich et al., 2009). Nevertheless, we conducted this study to provide an insight into the use of SFM/FFP masks in Austrian health care institutions during the COVID‐19 pandemic. We did not specifically assess the reasons for compliance or non‐compliance with the rules for PPE use or the reasons for limiting this use, which highlights the need to carry out qualitative studies on this topic in the future.
4.1. Strengths and limitations
The first strength of this study is that it is the first one, to our knowledge, that describes the influence of wearing PPE during the COVID‐19 pandemic in Austria. Another strength is that our sample included more than 2500 nurses. One limitation of our study might be that we started the survey in mid‐May, nearly 2 months after the COVID‐19 pandemic had begun in Austria. Because we asked nurses retrospectively about their SFM/FFP mask usage during the COVID‐19 pandemic, some perceptions could have been distorted. We also have to mention that working during the pandemic as a frontline nurse might be stressful, independently of wearing a PPE or not. This could have influenced our results, as the high stress level might be a result of the ‘new pandemic’ and not only of PPE. Another aspect that should be mentioned is that we did not ask explicitly whether the nurses had opportunities to take a break, when wearing a mask for a longer period of time. However, we specifically asked the nursing staff how long they wore their masks before using a new one, which implies at least a short break.
Another limitation that has to be mentioned is that our data were obtained via an online survey that had been distributed mainly by using social media and a snowball technique. Therefore, it might have been possible that somebody participated in the study even if they were not frontline nursing staff during the COVID‐19 pandemic in Austria. We also have to mention that we did not stratify this analysis by the participant's professional qualification. This was decided for two reasons. As the aim was to obtain first insights into the association between the use of PPE, as well as the wearing time of masks, and stress levels among frontline nursing staff, analysing associated factors that predispose to the use of PPE among nursing staff was beyond the scope of the paper. However, we want to add that we are currently analysing data from the first and the second COVID‐19 waves that might answer this specific question. Second, as the use of masks is and was mandatory in Austrian health care institutions during the COVID‐19 pandemic, all health care providers were legally obliged to wear masks. Therefore, the level of qualification did not seem to constitute a confounder.
We also have to mention that we did not include physical consequences, such as headache and dizziness, even though this might have strengthened the study. However, we were able to conduct two interview studies, one with nursing staff from hospitals and one with nursing home staff, focusing on physical, psychological and social consequences for nursing staff during this pandemic. The results of these studies are currently in process of being analysed to be published at a later stage.
5. CONCLUSIONS
This study was carried out to investigate the association between PPE as well as wearing time of masks and stress levels among nursing staff during the COVID‐19 pandemic in Austria. Nearly all participating nurses used SFM or FFP masks. This might be an indication of a high level of compliance among Austrian nurses regarding the national as well as international regulations and highlights the key role played by nurses in such pandemics. Our results also show that increased mask‐wearing time led to increased levels of stress. These results suggest that (inter‐)national regulations on how and when to use masks should also include a maximum duration of time for wearing each type of mask. Such regulations could help to prevent work‐related stress, particularly in the case of future epidemics, and avoid nurses leaving their jobs. The consequences of both of these negative outcomes should be considered in light of the predicted future shortage of health care workers.
6. IMPLICATIONS FOR NURSING MANAGEMENT
Even when it is mandatory to wear PPE in times of a pandemic, our findings highlight that nursing managers should introduce a maximum wearing time for masks in their organisations, specifically in times of PPE shortage, when (inter‐)national recommendations cannot be followed anymore. Additionally, nursing managers could implement practical strategies such as a mask break task force. This task force could promote awareness for mask breaks and recommend and allocate rooms or locations such as balconies for mask breaks. This can help them, especially in times of an (inter‐)national nursing shortage, to increase work satisfaction and consequently to keep nurses in their organisation.
CONFLICT OF INTEREST
None declared.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
AUTHOR CONTRIBUTIONS
All above listed as authors (M. Hoedl, D. Eglseer & S. Bauer) are qualified for authorship by meeting all four of the following criteria:
Have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data;
Been involved in drafting the manuscript or revising it critically for important intellectual content;
Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and
Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hoedl M, Eglseer D, Bauer S. Associations between personal protective equipment and nursing staff stress during the COVID‐19 pandemic. J Nurs Manag. 2021;29:2374–2382. 10.1111/jonm.13400
DATA AVAILABILITY STATEMENT
Due to legal regulations, data cannot be made available.
REFERENCES
- 3M Personal Safety Division . (2020). Comparison of FFP2, KN95, and N95 filtering facepiece respirator classes. Retrieved from https://multimedia.3m.com/mws/media/1791500O/comparison-ffp2-kn95-n95-filtering-facepiece-respirator-classes-tb.pdf:
- Alharbi, H. , & Alshehry, A. (2019). Perceived stress and coping strategies among ICU nurses in government tertiary hospitals in Saudi Arabia: A cross‐sectional study. Annals of Saudi Medicine, 39(1), 48–55. 10.5144/0256-4947.2019.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhudhairy, M. W. , Al Ramel, F. , Al Jader, G. , Al Saegh, L. , Al Hadad, A. , Alalwan, T. , Al Shaikh, D. , & Al Bandar, M. (2018). A self‐reported association between temporomandibular joint disorders, headaches, and stress. Journal of International Society of Preventive & Community Dentistry, 8(4), 371–380. 10.4103/jispcd.JISPCD_177_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barclay, L. , Park, G. W. , Vega, E. , Hall, A. , Parashar, U. , Vinjé, J. , & Lopman, B. (2014). Infection control for norovirus. Clinical Microbiology and Infection, 20(8), 731–740. 10.1111/1469-0691.12674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catton, H. (2020). Global challenges in health and health care for nurses and midwives everywhere. International Nursing Archive, 67(1), 4–6. 10.1111/inr.12578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cook, T. M. (2020). Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic—A narrative review. Anaesthesia, 75(7), 920–927. 10.1111/anae.15071 [DOI] [PubMed] [Google Scholar]
- Deutsche gesetzliche Unvallversicherung . Benutzung von Atemschutzgeräten (DGUV Regel 112–190), (2011).
- Donabedian, A. (1966). Evaluating the quality of medical care. The Milbank Memorial Fund Quarterly, 44(3), 166–206. [PubMed] [Google Scholar]
- Drachev, S. N. , Stangvaltaite‐Mouhat, L. , Bolstad, N. L. , Johnsen, J.‐A. K. , Yushmanova, T. N. , & Trovik, T. A. (2020). Perceived stress and associated factors in Russian medical and dental students: A cross‐sectional study in north‐West Russia. BMC Oral Health, 17(15), 5390. 10.3390/ijerph17155390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falzarano, F. , & Siedlecki, K. L. (2021). Differences in cognitive performance between informal caregivers and non‐caregivers. Neuropsychology, Development, and Cognition. Section B, Aging, Neuropsychology and Cognition, 28(2), 284–307. 10.1080/13825585.2020.1749228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Ministry for Social Affairs, Health Care and Consumer Protection . (2020a). Übersicht Einsatzbereiche verschiedener Maskenarten und Mund‐ Nasen‐Schutzes im Gesundheits‐ /Sozialbereich. Vienna: Republic Austria; Retrieved from. https://www.sozialministerium.at/Informationen-zum-Coronavirus/Coronavirus---Fachinformationen.html [Google Scholar]
- Federal Ministry for Social Affairs, Health Care and Consumer Protection . (2020b). Empfehlung zu COVID‐19 Schutzmaßnahmen für Pflege und Betreuung [in German]. Retrieved from https://www.sozialministerium.at/Informationen-zum-Coronavirus/Coronavirus---Fachinformationen
- Grant, M. C. , Geoghegan, L. , Arbyn, M. , Mohammed, Z. , McGuinness, L. , Clarke, E. L. , & Wade, R. G. (2020). The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS‐CoV‐2; COVID‐19): A systematic review and meta‐analysis of 148 studies from 9 countries. PLoS ONE, 15(6), e0234765. 10.1371/journal.pone.0234765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch, J. D. , Nemlekar, P. , Phuong, P. , Hollenbach, K. A. , Lee, K. C. , Adler, D. S. , & Morello, C. M. (2020). Patterns of stress, coping and health‐related quality of life in doctor of pharmacy students. American Journal of Pharmaceutical Education, 84(3), 7547. 10.5688/ajpe7547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoedl, M. , & Schoberer, D. (2020). ARbeitsanfOrderungen von PflegeperSonen im PflEgeheim während der COVID‐19 PaNdemie (ROSEN‐Projekt).
- IBM Corp. Released . (2019). IBM SPSS statistics for windows version 26.0. NY: IBM Corp. [Google Scholar]
- Inns, T. , Wilson, D. , Manley, P. , Harris, J. P. , O'Brien, S. J. , & Vivancos, R. (2019). What proportion of care home outbreaks are caused by norovirus? An analysis of viral causes of gastroenteritis outbreaks in care homes, north East England, 2016–2018. BMC Infectious Diseases, 20(1), 2. 10.1186/s12879-019-4726-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein, E. M. , Brähler, E. , Dreier, M. , Reinecke, L. , Müller, K. W. , Schmutzer, G. , Wölfling, K. , & Beutel, M. E. (2016). The German version of the perceived stress scale—Psychometric characteristics in a representative German community sample. BMC Psychiatry, 16, 159. 10.1186/s12888-016-0875-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krøll, L. S. , Hammarlund, C. S. , Westergaard, M. L. , Nielsen, T. , Sloth, L. B. , Jensen, R. H. , & Gard, G. (2017). Level of physical activity, well‐being, stress and self‐rated health in persons with migraine and co‐existing tension‐type headache and neck pain. The Journal of Headache and Pain, 18(1), 46. 10.1186/s10194-017-0753-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockhart, S. L. , Duggan, L. V. , Wax, R. S. , Saad, S. , & Grocott, H. P. (2020). Personal protective equipment (PPE) for both anesthesiologists and other airway managers: Principles and practice during the COVID‐19 pandemic. Canadian Journal of Anesthesia, 67(8), 1005–1015. 10.1007/s12630-020-01673-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGilton, K. , Escrig‐Pinol, A. , Gordon, A. , Chu, C. , Zúñiga, F. , Sanchez, M. , Boscart, V. , Meyer, J. , Corazzini, K. N. , Jacinto, A. F. , Spilsbury, K. , Backman, A. , Scales, K. , Fagertun, A. , Wu, B. , Edvardsson, D. , Lepore, M. J. , Leung, A. Y. M. , Siegel, E. O. , … Bowers, B. (2020). Uncovering the devaluation of nursing home staff during COVID‐19: Are we fuelling the next health care crisis? Journal of the American Medical Directors Association, 21(7), 962–956. 10.1016/j.jamda.2020.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo, Y. , Deng, L. , Zhang, L. , Lang, Q. , Liao, C. , Wang, N. , Qin, M. , & Huang, H. (2020). Work stress among Chinese nurses to support Wuhan for fighting against the COVID‐19 epidemic. Journal of Nursing Management, 28, 1002–1009. 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health . (2020). Recommended guidance for extended use and limited reuse of N95 filtering facepiece respirators in healthcare settings. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
- Ong, J. , Bharatendu, C. , Goh, Y. , Tang, J. Y. , Sooi, K. , Tan, Y. , Tan, B. Y. Q. , Teoh, H.‐L. , Ong, S. T. , Allen, D. M. , & Sharma, V. (2020). Headaches associated with personal protective equipment—A cross‐sectional study among frontline healthcare workers during COVID‐19. Headache, 60, 864–877. 10.1111/head.13811 [DOI] [PubMed] [Google Scholar]
- Radonovich, L. J. Jr. , Cheng, J. , Shenal, B. V. , Hodgson, M. , & Bender, B. S. (2009). Respirator tolerance in health care workers. Journal of the American Medical Association, 301(1), 36–38. 10.1001/jama.2008.894 [DOI] [PubMed] [Google Scholar]
- Rebmann, T. , Carrico, R. , & Wang, J. (2013). Physiologic and other effects and compliance with long‐term respirator use among medical intensive care unit nurses. American Journal of Infection Control, 41(12), 1218–1223. 10.1016/j.ajic.2013.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis, D. , Lehr, D. , Heber, E. , & Ebert, D. D. (2019). The German version of the perceived stress scale (PSS‐10): Evaluation of dimensionality, validity, and measurement invariance with exploratory and confirmatory bifactor modeling. Assessment, 26(7), 1246–1259. 10.1177/1073191117715731 [DOI] [PubMed] [Google Scholar]
- Schneider, E. E. , Schönfelder, S. , Wolf, M. , & Wessa, M. (2017). All stressed out? Introducing a German version of the perceived stress scale: Validation, psychometric properties and sample differences in healthy and clinical populations. Psychoneuroendocrinology, 83, 21. 10.1016/j.psyneuen.2017.07.296 [DOI] [Google Scholar]
- Senocak, S. U. , & Demirkiran, F. (2020). Subjective well‐being and influencing factors in Turkish nursing students: A cross‐sectional study. Journal of the Pakistan Medical Association, 70(4), 630–635. 10.5455/jpma.11398 [DOI] [PubMed] [Google Scholar]
- Teresi, J. A. , Ocepek‐Welikson, K. , Ramirez, M. , Kleinman, M. , Ornstein, K. , Siu, A. , & Luchsinger, J. (2020). Evaluation of the measurement properties of the perceived stress scale (PSS) in Hispanic caregivers to patients with Alzheimer's disease and related disorders. International Psychogeriatrics, 1–12. 10.1017/s1041610220000502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian, Z. , Kim, B.‐Y. , & Bae, M.‐J. (2020). A study on the effect of wearing masks on stress response. International Journal of Engineering Research and Technology, 13, 807–813. 10.37624/IJERT/13.4.2020.807-813 [DOI] [Google Scholar]
- WHO . (2016). The global strategic directions for strengthening nursing and midwifery: 2016–2020. Retrieved from Geneva: https://www.who.int/hrh/nursing_midwifery/global-strategic-midwifery2016-2020.pdf?ua=1
- WHO . (2020a). Advice on the use of masks in the context of COVID‐19: Interim guidance, 6 April 2020. Retrieved from https://apps.who.int/iris/handle/10665/331693
- WHO . (2020b). Coronavirus disease (COVID‐19): How is it transmitted?
- WHO . (2020c). COVID‐19 dashboard. Retrieved from https://covid19.who.int/?gclid=EAIaIQobChMIo53W7Zaa6wIVg9eyCh2t4wnHEAAYASAAEgIiN_D_BwE:
- WHO . (2020d). Infection prevention and control during health care when COVID‐19 is suspected: Interim guidance, 19 March 2020. Retrieved from https://www.who.int/publications/i/item/10665-331495https://www.who.int/publications/i/item/10665-331495
- WHO . (2020e). Rational use of personal protective equipment for coronavirus disease (COVID‐19) and considerations during severe shortages: Interim guidance, 6 April 2020. Retrieved from https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortageshttps://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages
- WHO & International Labour Organisation . (2021). COVID‐19: Occupational health and safety for health workers Interim guidance. Retrieved from https://www.who.int/publications/i/item/WHO-2019-nCoV-HCW_advice-2021.1:
- Wiriyakijja, P. , Porter, S. , Fedele, S. , Hodgson, T. , McMillan, R. , Shephard, M. , & Ni Riordain, R. (2020). Validation of the HADS and PSS‐10 and a cross‐sectional study of psychological status in patients with recurrent aphthous stomatitis. Journal of Oral Pathology & Medicine, 49(3), 260–270. 10.1111/jop.12991 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to legal regulations, data cannot be made available.


