Abstract
Background
The mental health response to the coronavirus (COVID‐19) pandemic–related product shortages in those living with chronic gastrointestinal (GI) disorders has received little attention. We aimed to explore the association between the pandemic‐related product shortages and psychological distress in people with GI disorders.
Methods
This online cross‐sectional survey was nested within an ongoing, international, prospective study of well‐being in people with GI disorders. The study was advertised in multiple countries in May‐September 2020 via patient organizations and social media. The primary outcome measure was distress, evaluated by the Depression Anxiety Stress Scale. We utilized linear regressions, adjusting for covariates and testing individual moderation effects.
Key Results
Overall, 831 people completed the survey from 27 countries, of whom 82% were female (mean age = 49 years). The most common disorders included inflammatory bowel disease (n = 322), celiac disease (n = 273), and irritable bowel syndrome (n = 260). Significant problems accessing food were reported by 19.8%, non‐medical therapies by 16%, toilet paper by 10.8%, and essential medication by 8.9% of the sample (>5% pain medication). There was a positive association between toilet paper and pain medication shortages and distress, and a negative association between food shortages and distress. Significant moderation effects were identified for COVID‐19 prevalence and toilet paper and food shortages, and between COVID‐19 fear and pain medication shortages.
Conclusions and Inferences
The study documented a significant relationship between product shortages and psychological distress, which were associated with COVID‐19 prevalence and fear. Strategies addressing COVID‐19 fear could potentially modify the relationship between shortages and distress.
Keywords: COVID‐19, distress, gastrointestinal disorders, product shortages, psychological distress
Product shortages were associated with psychological distress in people with gastrointestinal disorders at the time of the COVID‐19 pandemic. The relationship between product shortages and distress was moderated by COVID‐19 prevalence and fear.

Key Points.
The first study to explore the relationship between product shortages and distress among adults living with GI disorders during the COVID‐19 pandemic.
The study documented a significant relationship between personal product shortages, specifically toilet paper, pain medication, and food shortages, and psychological distress.
The relationship between product shortages and distress was moderated by COVID‐19 prevalence and fear.
1. INTRODUCTION
To date, the novel coronavirus (SARS‐CoV‐2) has caused over 3 million deaths, with over 170 million people infected worldwide, and infection and death rates rising daily. 1 The coronavirus (COVID‐19) pandemic has put significant pressure on health services, often limiting access to routine and preventive care, and in some cases limiting access to urgent care needed for acutely ill patients. The pandemic has also interrupted supply chains, particularly at production and distribution levels, at times resulting in shortages of items such as medications and personal hygiene products. 2 , 3 , 4
While the burden of the pandemic on the global economy 5 and society well‐being 6 , 7 is indisputable, it has been further amplified for those living with gastrointestinal (GI) disorders. GI disorders affect at least one third of the population worldwide, with functional gastrointestinal disorders, such as irritable bowel syndrome (IBS), being the largest contributor to overall prevalence. 8 , 9 GI disorders are debilitating, costly, 10 and responsible for more than a quarter million deaths each year in the United States alone. 11 GI disorders are also frequently accompanied by anxiety and depression, which are known to be significantly associated with the GI symptoms and illness severity. 12 , 13 , 14 , 15 GI disorders are often managed by daily medication use, with some of the affected populations requiring immunosuppressive therapies, complex dietary approaches, and high demand for personal hygiene products, the latter related to the nature of the symptoms, such as diarrhea.
The COVID‐19 pandemic has caused major shortages of medical products such as ventilators, 16 medication, 17 acute beds, 18 face masks, 19 face shields, 20 and hand sanitizer 21 as well as supply fluctuations resulting in access to more mundane products such as toilet paper and certain foods. 2 , 3 , 4 In addition to supply or production shortages, stockpiling and panic buying have been well documented during the pandemic. 22 This behavior is hypothesized to provide short‐term reduction in anxiety, 23 , 24 by offering a sense of control during unpredictable times. However, while stockpiling may temporarily relieve anxiety in some people, it may aggravate it for those who need the products urgently. Difficulty accessing healthcare services, shortages of medication used to manage GI symptoms, and other co‐morbid conditions, together with food (eg, specialty food such as lactose‐, gluten‐free), protective equipment (eg, masks), and personal hygiene product shortages (eg, toilet paper and stoma appliance supplies), may therefore further exacerbate psychological distress and undermine coping in this population. However, the mental health response to the shortages of products and services has received little attention thus far, with the effect of shortages on those living with chronic GI disorders unexplored to date. The present study aimed to:
Aim 1: explore the association between the COVID‐19 pandemic–related product shortages and symptoms of stress, anxiety, and depression (collectively called psychological distress) in people with GI disorders.
Aim 2: identify vulnerable subgroups who were most affected by the product shortages.
We hypothesized that there is a positive relationship between the COVID‐19 pandemic–related product shortages and psychological distress in people with GI disorders.
2. MATERIALS AND METHODS
2.1. Design
This online cross‐sectional survey was nested within an ongoing, international, prospective study of well‐being in people with GI disorders during the COVID‐19 pandemic.
2.2. Participants, recruitment, and procedure
The study was advertised to potential participants in multiple countries around the world in May‐September 2020 via gastrointestinal‐specific patient organizations and associated social media.
Participants needed to meet the following eligibility criteria: (a) ≥18 years of age, (b) diagnosed (self‐reported) by a physician with a GI disorder, and (c) able to provide informed consent. While the study was advertised broadly, it required understanding English as the questionnaire was provided in this language only. Consent was obtained by the participant's decision to complete the questionnaire. This study was approved by the Swinburne University of Technology Human Research Ethics Committee on May 25, 2020 (Ref: 20202978–4430).
2.3. Measures
Patient demographics and health characteristics were collected with a questionnaire developed by the investigators. Income data were provided in the local currency and converted to US dollars using an approximate average conversion rate for the study period. 25 Income was ranked into percentiles: 5th, 10th, 25th, 50th, 75th, 90th, and 95th. GI disorders were self‐reported.
2.3.1. Depression, anxiety, and stress scale (DASS‐21)
The DASS is a 21‐item self‐report scale that measures symptoms of distress (ie, stress, anxiety, and depression) over the past week. Each question is rated on a 4‐point Likert scale from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time). The DASS‐21 has been shown to possess adequate construct validity and reliability for measuring the dimensions of depression, anxiety, and stress. 26
2.3.2. Gastrointestinal symptom rating scale (GSRS)
The 15‐item GSRS is a widely used and reliable self‐report measure that captures the severity of GI symptoms across a range of GI conditions. 27 Respondents rate their level of discomfort for a range of GI symptoms over the past week, using a 7‐point Likert scale with anchor points of “no discomfort at all” to “very severe discomfort.” The total score ranges from 15 to 105, with higher scores reflecting more severe symptoms.
2.3.3. COVID prevalence
Average COVID cases per million between March and November 2020 were estimated using the online coronavirus pandemic data explorer. 28 Participant nations were then ranked according to lowest prevalence in that time frame (New Zealand, Australia, Canada) to highest (Belgium, United States, Switzerland). England, Northern Ireland, Scotland, and Wales were pooled to align with estimates from the data explorer.
2.3.4. COVID Infection
Participants reported whether they or someone from their household had been diagnosed with COVID‐19, and responses were dichotomized to reflect participants who reported self/familial infection and those who did not.
2.3.5. The brief illness perception questionnaire (Brief IPQ)
Brief IPQ is a widely used and reliable measure of illness perception. 29 This 8‐item measure asks the respondents to rate their views regarding their level of concern in living with their illness (eg, controllability, impact, severity, duration) on a scale from 0 to 10, with 0 = no concern and 10 = extremely concerned. The authors of the scale encourage its adaptation to other illness settings. 30 Therefore, in the present study, we adapted the Brief IPQ to the COVID context, utilizing two IPQ subscales: GI‐specific (IPQ‐GI, 8 items) and COVID‐19–specific (IPQ‐COVID, five items). In the first subscale (IPQ‐GI), to ensure that the scale assessed GI‐specific perceptions, the word “illness” was replaced with “gastrointestinal condition,” for example, “How much control do you feel you have over your illness?” became “How much control do you feel you have over your gastrointestinal condition?” The 8‐item scale has a strong reliability (α = .83). A second version of this scale (IPQ‐COVID) was used to assess perceptions relating to COVID‐19. For each of the original items, the word “your illness” was replaced with “COVID‐19,” for example “How much control do you feel you have over your illness?” became “How much control do you feel you have over COVID‐19?”. After three items (4, 5, and 7) were discarded based on Cronbach's alpha, the reliability was good (α = .75). IPQ‐GI and IPQ‐COVID totals were created by averaging items, with higher scores indicating poorer GI illness perceptions or poorer perceptions relating to COVID‐19 respectively.
2.3.6. Perception of COVID spread
Participants were asked to give their perception of the current state of coronavirus in their state or province (“What is your sense of the COVID‐19 pandemic spread in your state/province?”), on a four‐point scale: 1 = “Cases of COVID‐19 are rising quickly”; 2 = “Cases of COVID‐19 are rising slowly”; 3 = “Cases of COVID‐19 have flattened out with only a few new cases each time”; and 4 = “No cases of COVID‐19.”
2.3.7. The fear relating to COVID‐19 Scale (COVID‐19 fear)
The Fear Relating to COVID‐19 Scale is derived from the Fear of AIDS Scale, 31 has been validated in the IBD population, and showed excellent psychometric properties. 32 This 14‐item scale asks respondents to indicate the level of fear/concern they are experiencing regarding different situations, such as contracting COVID‐19 or having contact with health professionals. For the present study, five GI‐amplified items were added regarding (a) whether COVID will worsen the GI disorder; (b) whether COVID will affect access to medical care; (c) whether COVID will affect the management of the GI disorder; (d) whether the GI disorder will increase the risk of contracting COVID; and (e) whether having a GI disorder will increase the risk of death from COVID. All items are rated on a 5‐point scale from 1 (no fear) to 5 (very much fear). Scale scores ranged from 14 to 70, and higher scores indicated greater fear/concern about COVID‐19. The scale presents two factors: General Fear of COVID and GI‐amplified Fear of COVID, both with acceptable internal reliability (α = .93 and α = .88, respectively).
Product shortages were evaluated with a series of 4‐point Likert scales ranging from “no problem at all” to “serious problem.” This measure was developed by the investigators, utilizing multi‐country experiences to date and the unique context of a global pandemic. Items included shortages of medications, pain medications, food, toilet paper, and non‐medical therapies. Scores ranged from 1 to 4, with higher scores reflecting greater difficulties with product shortages.
2.4. Statistical analysis
Missing data were deemed to be missing at random with no evidence of systematic missingness. Data met assumptions of linearity and independence of errors and fell within acceptable ranges of normal distribution. Bivariate correlations were performed for all variables in the model, using Pearson's r for continuous variables and Spearman's rho for ordinal variables.
To explore whether specific vulnerable populations would experience stronger associations between COVID shortages and psychological distress, we performed a series of linear regressions, adjusting for the presence of other variables and testing individual moderation effects. The total distress score was the dependent variable in all models, and we examined five specific shortages common to gastrointestinal patients. The moderator variables entered into the models were as follows: parent/caregiver status, chronic condition, employed, COVID prevalence, perception of COVID spread, COVID fear, income, diarrhea severity, COVID infection, IPQ‐COVID, IPQ‐GI, GSRS, and age.
To accommodate the number of model effects and control the type I error rate, we developed our final model by running individual moderator‐specific models that contained all univariate main effects, and the interactions of a single moderator variable with each of the shortage variables. All analyses were performed in R 31 and Jamovi, 33 using the car 34 (Fox & Weisberg, 2018) and emmeans packages. 35
3. RESULTS
Overall, 831 people completed the survey, of whom 82% were female and were, on average, 49 years old (SD = 16.5). The majority were married (56%), had a university degree (60%), and came from the United Kingdom (n = 365); see Tables 1 and 2.
TABLE 1.
Sample characteristics
| N (%) | Missing | Mean | Standard deviation | Minimum | Maximum | |
|---|---|---|---|---|---|---|
| Age | 793 | 38 | 49.1 | 16.1 | 18 | 94 |
| Dependents | 569 | 262 | 0.866 | 1.16 | 0 | 9 |
| USD Income | 424 | 407 | 75015 | 84456 | 0 | 1,103,832 |
| Distress | 831 | 0 | 26.9 | 25.4 | 0 | 126 |
| GI disorder activity | 831 | 0 | 36.2 | 16.6 | 15 | 97 |
| Illness perception of GI | 831 | 0 | 5.3 | 1.73 | 1.25 | 9.5 |
| Illness perception of COVID | 831 | 0 | 4.7 | 1.19 | 1.13 | 8.25 |
| Perception of COVID spread | 831 | 0 | 2.54 | 0.865 | 1 | 4 |
| Fear related to COVID scale | 831 | 0 | 26.51 | 8.5 | 9 | 45 |
| Self/familial COVID infection (yes/no) | 34/797 (4.1) | 0 |
TABLE 2.
Demographic characteristics
| Gender | Counts | % of total | Marital status | Counts | % of total | Nation | Counts | % of total | COVID prevalence ranka | Condition | Counts |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | 142 | 17.1% | Single | 232 | 27.9% | Australia | 101 | 12.2% | 1 | Celiac disease | 273 |
| Female | 684 | 82.3% | Married | 464 | 55.8% | Austria | 2 | 0.2% | 15 | Colonic inertia | 9 |
| Equally/neither/unsure/prefer not to say | 5 | 0.6% | De facto | 54 | 6.5% | Belgium | 1 | 0.1% | 20 | Diverticular diseases | 54 |
| Widowed | 19 | 2.3% | Brazil | 1 | 0.1% | 13 | Functional dyspepsia | 20 | |||
| Divorced | 50 | 6.0% | Canada | 28 | 3.4% | 3 | Gallstones | 35 | |||
| Separated | 12 | 1.4% | Denmark | 34 | 4.1% | 5 | Gastroparesis | 18 | |||
| England | 313 | 37.7% | 7 | GERD/GORD | 96 | ||||||
| Education levels | Counts | % of Total | Employment levels | Counts | % of Total | France | 1 | 0.1% | 16 | Globus | 5 |
| Elementary to 8th grade | 7 | 0.8% | Full‐time employed | 270 | 32.5% | Germany | 8 | 1.0% | 4 | Hemorrhoids | 74 |
| Some high school, no diploma | 39 | 4.7% | Part‐time employed | 109 | 13.1% | Ireland | 4 | 0.5% | 7 | IBS | 260 |
| High school degree or equivalent (eg, GED) | 84 | 10.1% | Casually employed | 14 | 1.7% | The Netherlands | 38 | 4.6% | 14 | Crohn's disease | 177 |
| Some college credit, no degree | 75 | 9.0% | Other | 49 | 5.9% | New Zealand | 69 | 8.3% | 1 | Ulcerative colitis | 123 |
| Trade/technical/vocational training | 89 | 10.7% | Self‐employed | 49 | 5.9% | Poland | 79 | 9.5% | 11 | Indeterminate colitis | 22 |
| Associate degree (eg, AA, AS) | 39 | 4.7% | Unemployed | 63 | 7.6% | Portugal | 8 | 1.0% | 12 | Other: | 129 |
| Bachelor's degree (eg, BA, BS, BBA) | 279 | 33.6% | Retired | 153 | 18.4% | Romania | 11 | 1.3% | 9 | ||
| Master's degree (eg, MA, MS, MEng, MSW, MBA) | 150 | 18.1% | Pensioner | 48 | 5.8% | Scotland | 32 | 3.9% | 7 | ||
| Professional degree (eg, MD, DDS, JD, DVM) | 36 | 4.3% | Home duties | 38 | 4.6% | Sweden | 4 | 0.5% | 8 | ||
| Doctoral degree (eg, PhD) | 33 | 4.0% | Student | 38 | 4.6% | Switzerland | 1 | 0.1% | 18 | ||
| United States of America | 63 | 7.6% | 19 | ||||||||
| Wales | 16 | 1.9% | 7 | ||||||||
| Spain | 8 | 1.0% | 10 | ||||||||
| Northern Ireland | 4 | 0.5% | 7 | ||||||||
Variable is ranked 1 to 20, with higher values indicative of greater COVID prevalence among the countries reported in the sample.
The most common GI disorder types included IBD (n = 322), celiac disease (n = 273), and IBS (n = 260), with 448 (53.9%) identifying living with a co‐morbid chronic illness (see Table 2). The mean scores for distress symptoms were within the normal range, and the severity of GI symptoms was also low (M = 36.2, SD = 16.6).
Product shortages data are presented in Table 3. Moderate serious problems accessing food were reported by almost one in five of the sample, with 16% affected by shortages of non‐medical therapies and 10.8% by toilet paper shortages, while essential medication shortages affected 8.9% of the sample.
TABLE 3.
COVID‐19–related product shortages
| No problem at all | % | Minor problem | % | Moderate problem | % | Serious problem | % | |
|---|---|---|---|---|---|---|---|---|
| Medication | 499 | 67.9% | 170 | 23.1% | 51 | 6.9% | 15 | 2.0% |
| Toilet paper | 501 | 63.7% | 201 | 25.5% | 64 | 8.1% | 21 | 2.7% |
| Food | 352 | 43.8% | 292 | 36.4% | 134 | 16.7% | 25 | 3.1% |
| Pain medication | 566 | 82.4% | 83 | 12.1% | 28 | 4.1% | 10 | 1.5% |
| Non‐medical therapies | 303 | 55.5% | 154 | 28.2% | 59 | 10.8% | 30 | 5.5% |
3.1. Aim 1
3.1.1. Correlations
The univariate correlations between the variables of interest are presented in Table 4. Diarrhea severity, illness perceptions of COVID and gastrointestinal illness, total gastrointestinal symptom severity, and shortages of medications, toilet paper, special diet food, pain medication, and non‐medication therapies were each significantly and positively correlated with distress, with the strongest association observed for fear of COVID.
TABLE 4.
Univariate correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DISTRESS | — | |||||||||||||||||
| PARENT/CAREGIVER | 0.006 | — | ||||||||||||||||
| CHRONIC CONDITION | −0.02 | −0.076 | — | |||||||||||||||
| EMPLOYED | 0.034 | 0.208c | −0.146aa | — | ||||||||||||||
| COVID PREVALENCE | −0.023 | −0.009 | −0.001 | −0.033 | — | |||||||||||||
| COVID PERCEPTION OF SPREAD | 0.036 | −0.016 | −0.043 | 0.008 | 0.133c | — | ||||||||||||
| COVID FEAR | 0.307 | −0.047 | 0.076a | −0.075a | 0.077a | 0.203c | — | |||||||||||
| INCOME | −0.076 | 0.106 | −0.147c | 0.199c | −0.067 | −0.009 | −0.054 | — | ||||||||||
| DIARRHEA SEVERITY | 0.29 | 0.003 | −0.062 | −0.059 | 0.057 | 0.052 | 0.16c | −0.062 | — | |||||||||
| COVID INFECTION | −0.093 | −0.011 | 0.028 | −0.036 | 0.001 | 0.007 | 0.025 | 0.016 | −0.061 | — | ||||||||
| IPQ_GI | 0.496c | 0.04 | −0.057 | −0.001 | 0.07 | 0.063 | 0.283c | −0.018 | 0.479c | −0.027 | — | |||||||
| IPQ_COVID | 0.458 | 0.037 | 0.033 | 0.023 | −0.03 | 0.14c | 0.572c | −0.063 | 0.157c | −0.133c | 0.385c | — | ||||||
| GSRS_BASE_COVID | 0.484 | 0.014 | 0.025 | −0.026 | 0.034 | 0.069a | 0.249c | −0.081 | 0.676c | −0.051 | 0.653c | 0.288c | — | |||||
| AGE | −0.198 | −0.064 | 0.354c | −0.358c | −0.042 | −0.143c | −0.03 | −0.161c | −0.112b | 0.002 | −0.123c | −0.074a | −0.133c | — | ||||
| MEDICATIONS | 0.219 | 0.013 | 0.041 | 0.039 | 0.022 | 0.081a | 0.222c | 0.044 | 0.161c | −0.024 | 0.248c | 0.175c | 0.24c | −0.12c | — | |||
| TOILET PAPER | 0.171c | −0.041 | 0.028 | 0.046 | −0.191c | 0.03 | 0.122c | 0.006 | 0.048 | −0.031 | 0.105b | 0.172c | 0.163c | −0.135c | 0.283c | — | ||
| FOOD | 0.108b | 0.027 | 0.065 | 0.058 | −0.044 | 0.055 | 0.154c | 0.001 | −0.054 | −0.075 | 0.054 | 0.209c | 0.08a | −0.072a | 0.33c | 0.505c | — | |
| PAIN MEDICATION | 0.175c | 0.003 | −0.004 | 0.054 | 0.05 | 0.077 | 0.15c | −0.015 | 0.088 | −0.008 | 0.162c | 0.122b | 0.191c | −0.079a | 0.517c | 0.227c | 0.319c | — |
| NON‐MEDICATION THERAPIES | 0.211c | 0.056 | 0.055 | −0.028 | −0.047 | 0.063 | 0.168c | −0.009 | 0.06 | −0.064 | 0.162c | 0.201c | 0.21c | −0.004 | 0.352c | 0.201c | 0.312c | 0.365c |
p < 0.05.
p < 0.01.
p < 0.001.
Age was the sole negative correlate with distress, meaning that younger participants reported greater distress, and frequently observed to negatively correlate with other variables except for chronic condition diagnosis.
Interestingly, we observed a weak negative association between current employment status and annual pre‐tax household income, suggesting that a not‐insubstantial number of participants had lost employment during the COVID crisis. Each of the five shortage variables was positively correlated with the others, generally with small but robust associations. The strongest associations were between toilet paper and special food shortages (r = .505), and between general medications and pain medications (r = .517).
3.1.2. Regression models
The COVID‐19 pandemic–related product shortages of toilet paper, pain medication, and food were significantly associated with distress. In particular, there was a positive association between toilet paper and pain medication shortages and distress, and there was a negative association between food shortages and distress (Table 5, the final regression model).
TABLE 5.
Final regression model of the association between shortages and mental health
| Estimate | SE | T | p | Beta | Lower | Upper | |
|---|---|---|---|---|---|---|---|
| Intercept | −109.364 | 44.593 | −2.452 | 0.016 | |||
| Age | −1.491 | 0.132 | −1.33 | 0.260 | −0.0846 | −0.4098 | 0.112 |
| Income | 0.597 | 1.126 | 0.531 | 0.597 | 0.0375 | −0.10253 | 0.1776 |
| COVID prevalence | 2.776 | 1.900 | 1.461 | 0.147 | 0.0669 | −0.07302 | 0.2068 |
| Perception of COVID spread | 0.442 | 2.037 | 0.217 | 0.829 | 0.0144 | −0.11674 | 0.1455 |
| Employed | −3.913 | 4.154 | −0.942 | 0.348 | −0.0674 | −0.20917 | 0.0743 |
| Chronic condition | 2.997 | 4.078 | 0.735 | 0.464 | 0.0536 | −0.09087 | 0.1981 |
| Parent/caregiver | 3.597 | 3.722 | 0.966 | 0.336 | 0.0650 | −0.06820 | 0.1981 |
| GI disorder activity | 0.270 | 0.185 | 1.458 | 0.147 | 0.1575 | −0.05644 | 0.3715 |
| COVID fear | 2.664 | 1.112 | 2.396 | 0.018 | 0.0205 | −0.14536 | 0.1864 |
| Illness perception of GI | 4.672 | 1.498 | 3.119 | 0.002 | 0.2634 | 0.09613 | 0.4306 |
| Illness perception of COVID | 7.071 | 1.953 | 3.621 | <.001 | 0.3202 | 0.14501 | 0.4953 |
| Diarrhea | 2.446 | 5.226 | 0.468 | 0.641 | 0.0263 | −0.14652 | 0.1991 |
| COVID infection | 4.677 | 11.319 | 0.413 | 0.680 | 0.0288 | −0.10923 | 0.1668 |
| Medication shortages | −18.459 | 9.537 | −1.935 | 0.055 | −0.0534 | −0.23946 | 0.1326 |
| Toilet paper shortages | 20.605 | 5.993 | 3.438 | <.001 | 0.0614 | −0.10923 | 0.2321 |
| Food shortages | −13.495 | 5.620 | −2.401 | 0.018 | −0.0594 | −0.23948 | 0.1208 |
| Pain medication | 34.320 | 14.844 | 2.312 | 0.023 | 0.0267 | −0.16132 | 0.2148 |
| Non‐medical therapies shortages | 1.622 | 2.538 | 0.639 | 0.524 | 0.0483 | −0.10145 | 0.1981 |
| Age × Medications | 0.334 | 0.178 | 1.879 | 0.063 | 0.1339 | −0.00724 | 0.2750 |
| COVID Prevalence × Toilet paper | −2.690 | 0.832 | −3.233 | 0.002 | −0.3191 | −0.51462 | −0.1236 |
| COVID Prevalence × Food | 1.669 | 0.633 | 2.635 | 0.010 | 0.1999 | 0.04962 | 0.3502 |
| COVID Fear × Pain Medications | −1.151 | 0.513 | −2.244 | 0.027 | −0.2259 | −0.42537 | −0.0265 |
| Diarrhea × Pain Medications | −0.903 | 2.344 | −0.385 | 0.701 | −0.0353 | −0.21717 | 0.1465 |
In comparing geographic regions, we observed that the most variation in serious shortages was reported by participants for special diet food products and toilet paper. Participants from North America reported the highest proportion of food shortages (10.9%), followed by Australia and New Zealand (4.2%). Reports of serious toilet paper shortages were highest in North America, Australia, and New Zealand (between 6% and 7%).
In a comparative examination of specific gastrointestinal diagnoses, we also observed that participants with a diagnosis of celiac disease were more likely to report moderate or serious food shortages (24% and 5.5%, respectively) compared to those with other GI diagnoses (13% and 1.7%). Participants with a celiac diagnosis were also more likely to report moderate, but not serious, shortages of toilet paper (10.1%) compared to those without a diagnosis (6.7%). Participants with celiac disease in all regions were more likely to report serious shortages of any type, though some variation was identified. Participants from continental Europe with a diagnosis of celiac disease were significantly more likely to report moderate or serious shortages of medication and non‐medication therapies compared to participants with other GI disorders from that region (16.7% to 7%). In North America, the same comparison between celiac diagnoses and other diagnoses revealed substantial differences in those reporting moderate or serious shortages of toilet paper and food (25.84% to 13.3%; 52.7% to 23.4%, respectively), and a comparable proportion of responses was observed for participants from the UK and Republic of Ireland for food shortages (28.1% to 16.9%). Interestingly, participants from Australia and New Zealand with a diagnosis of celiac disease were less likely to report shortages of pain medication and non‐medication therapies (2.3% to 9.52%; 13.8% to 17.2%, respectively).
3.2. Post hoc subgroup analyses
To account for heterogeneity of effects across different diagnoses, we performed subgroup analyses of the final regression model for participants who reported diagnoses of celiac, IBS, or IBD. The regression models and coefficients can be viewed in Supplemental Tables S1–S3. In contrast to the whole sample, no individual variable or interaction between variables was predictive of psychological distress in participants who reported a diagnosis of celiac, and the model was non‐significant. Most variables only changed slightly, few changed directions. In contrast to the celiac analysis, participants who reported a diagnosis of IBS shared many similarities with the overall model but produced some unique results. The associations of COVID fear, perception of COVID, and pain medication shortages with distress did not retain significance within the IBS sample, but a positive association between fears of non‐medication therapy shortages and distress emerged (b = 13.44, t = 2.21, p = 0.034). The interaction effect between age and medication was also not retained with the IBS sample.
Analysis of the participants reporting a diagnosis of IBD revealed several differences from the overall sample. The associations between distress and employment, IPQ‐COVID, pain medication shortages, and toilet paper shortages were not retained, nor the interaction effects between COVID fear and pain medications, and COVID prevalence and toilet paper shortages. In contrast, we observed significant associations between distress and age (b = −1.77, t = −2.65, p = 0.012), and diarrhea symptom severity (b = 33.63, t = 2.31, p = 0.028). We also observed significant interaction effects for age and medication shortage fears (b = 0.666, t = 2.53, p = 0.017), and between diarrhea symptom severity and pain medication shortage fears (b = −15.647, t = −2.24 p = 0.033).
We also examined mean differences between these three diagnostic subgroups across all variables entered into the model (See Supplementary Table S4 for full results). Adjusting for multiple comparisons using the Bonferroni corrections, each of the summarized differences here is significant at the p < 0.05 level. The IBD group was significantly younger and more distressed than the other two groups. The IBS group reported the highest levels of GSRS, followed by the IBD group, and reported the highest levels of IPQ‐COVID scores. Neither coeliac nor IBD groups differed on the IPQ‐COVID measure. The celiac group reported the lowest levels of IPQ‐GI symptoms, COVID fear, and diarrhea symptoms, while the IBS and IBD groups did not differ on these measures. Finally, the celiac group reported the highest fear of food shortages, but was only statistically distinct from the IBD group, which reported the lowest.
3.3. Aim 2
Significant moderation effects were identified for COVID‐19 prevalence and toilet paper and food shortages, and between COVID‐19 fear and pain medication shortages (Table 6).
TABLE 6.
Simple effects for moderations
| Moderator | Estimates | SE | Lower | Upper | Df | T | p |
|---|---|---|---|---|---|---|---|
| COVID Prevalence × Toilet paper | |||||||
| Mean−1·SD | 13.14 | 4.14 | 4.95 | 21.337 | 115 | 3.177 | 0.002 |
| Mean | 2.12 | 2.98 | −3.77 | 8.016 | 115 | 0.713 | 0.477 |
| Mean+1·SD | −8.90 | 4.88 | −18.57 | 0.772 | 115 | −1.823 | 0.071 |
| COVID Prevalence × Food | |||||||
| Mean−1·SD | −8.87 | 4.26 | −17.31 | −0.421 | 115 | −2.080 | 0.040 |
| Mean | −2.03 | 3.11 | −8.19 | 4.129 | 115 | −0.653 | 0.515 |
| Mean+1·SD | 4.81 | 3.82 | −2.77 | 12.381 | 115 | 1.257 | 0.211 |
| COVID Fear × Pain Medication | |||||||
| Mean−1·SD | 0.7610 | 0.342 | 0.0836 | 1.439 | 115 | 2.225 | 0.028 |
| Mean | 0.0634 | 0.259 | −0.4488 | 0.576 | 115 | 0.245 | 0.807 |
| Mean+1·SD | −0.6343 | 0.458 | −1.5420 | 0.273 | 115 | −1.384 | 0.169 |
Interestingly, as COVID‐19 prevalence per 1 million population increased (average since March 2020), the association between toilet paper shortages and distress became negative. Participants from nations with the highest COVID‐19 prevalence (Belgium, United States, Switzerland) did not achieve statistically significant associations between distress and toilet paper shortages, while nations with low prevalence (New Zealand, Australia, Canada) had strong positive associations. An almost symmetrical moderation effect was detected for the association between food shortages and distress, where nations with lower COVID‐19 prevalence reported negative associations, while no associations were observed for nations with average or higher COVID‐19 prevalence (Figure 1).
FIGURE 1.
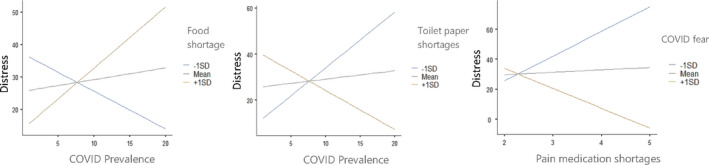
Distress and moderation simple slopes
Regarding the moderation of the association between distress and pain medication shortages by COVID‐19 fear, where COVID‐19 fear is highest, the association between pain medication shortages and distress is negative, and where COVID fear is low, the association between distress and pain medication shortages is positive.
4. DISCUSSION
This international survey is the first to explore the relationship between product shortages and distress among adults living with GI disorders during the COVID‐19 pandemic. The study documented a significant relationship between personal product shortages, specifically toilet paper, pain medication, and food shortages, and psychological distress. This relationship was significantly moderated by COVID‐19 prevalence and COVID‐19 fear.
People living with GI disorders have a higher risk of distress, compared with healthy controls 36 ; however, given the anxiety surrounding it, the COVID‐19 pandemic is likely to exacerbate this risk. Impaired psychological functioning in the general population has been reported during this pandemic. 7 This worsening well‐being has been hypothesized to stem from prolonged isolation, as people in self‐isolation or under quarantine appear to have a higher risk of developing anxiety and/or depression, 37 or the loss of employment/income and rising rates of domestic violence. 38 In addition, parents have been shown to be under particular distress as they struggle combining at home work with at home schooling of their children. 39 However, ours is the first study documenting the role of product shortages in this context. Availability of products, such as toilet paper and pain medication, is essential to well‐being, particularly for this population, whose symptoms often include pain, diarrhea, and/or frequent trips to the bathroom. Interestingly, we did not find a relationship between other medications and non‐medical treatments and distress despite these shortages being more commonly reported than pain medication. This might be due to immediate sense of control provided by pain medication not offered by other treatments, which usually require time to work.
Paradoxically, we documented a negative association between food shortages and distress, where nations with lower COVID‐19 prevalence reported negative associations. Nearly 20% of this study's respondents experienced moderate serious food shortages due to the COVID‐19 pandemic, but it seems that those most affected by the food shortages tended not to be reporting current distress. It is possible that these participants were able to adapt, eating a more monotonous diet or simply reducing their food intake, which provided some sense of control and reduced distress. Previous studies have documented higher external locus of control in people with GI disorders such as IBD and functional gut disorders than in the healthy controls. 40 It could also be that those living in the countries with high COVID‐19 prevalence such as the United States could be more focused on the virus itself, and its impact on their health, than on food shortages. Food is also a more generic category of item, and supermarkets were not completely sold out of food; responses may have been elevated if preferred foods were not able to be obtained. However, a complete lack of toilet paper for periods of time has been a feature of this pandemic. Further, the timing of the present study may also explain that, because distress due to food shortages was likely higher during the first wave of COVID‐19 earlier in the year than during the second wave which is documented in the present study. Moreover, in a comparative examination of specific gastrointestinal diagnoses, we observed that participants with a diagnosis of celiac disease were more likely to report moderate or serious food shortages compared to those without those diagnoses. Due to the necessity of a specialized diet requiring strict avoidance of food with gluten, people with celiac disease would arguably be most affected by shortages of gluten‐free products.
Further, our study demonstrated that participants from nations with highest prevalence of COVID‐19 reported negative associations between distress and toilet paper shortages, while nations with low prevalence (New Zealand, Australia, Canada) had strong positive associations. One potential interpretation of this finding could be that the low prevalence of COVID‐19 in nations such as New Zealand, Australia, and Canada was aided by this positive association—citizens from these countries had a greater distress response to COVID shortages and participated in suppression/elimination strategies more enthusiastically. Taking Australia as a case study, 17% of shoppers reported panic buying in April 2020 versus 6% in June 2020, 41 while another study demonstrated that Australians had one of the highest rates of COVID‐19–related panic buying worldwide, 42 associated with government announcements on tightening physical distancing rules. 43 Since Australia has experienced only economic growth in the last 30 years, shortages are largely unknown at the population level and their sudden appearance could have resulted in widespread panic. Another driver of this finding may be the severity of the lockdown measures, with Australia and New Zealand introducing some of the harshest lockdowns worldwide. Lockdown measures make it more difficult to shop and communicate the seriousness of the virus. In addition, countries with a high prevalence of COVID‐19 could have been more concerned about the risk of hospitalization or death rather than the pandemic's effects on lifestyle.
In addition, analysis of the diagnostic subgroups revealed some distinctive patterns of distress between the largest diagnoses. Interestingly, our attempts to predict distress within the celiac sample were largely unsuccessful compared with IBS or IBD, though our analyses suggest that reported distress within this group was significantly lower than the other groups with less than half the variance present. Our lack of an overall significant model predicting distress within this diagnostic subgroup may also suggest that the experience of distress is experientially distinct from those with IBS or IBD. The presence of significant models for IBS and IBD, as well as the individually predictive variables, in contrast, allows exploration of key features of distress within each group. For example, we see that the IBS group was uniquely distressed by concerns related to non‐medication therapies. Within the IBD group, we observed that younger age and lower diarrhea severity predicted fewer distress symptoms and that with increasing age came increased distress associated with fears of medication shortage. Curiously, the negative interaction effect between diarrhea severity and pain medication suggests that each of these variables had an inverse effect upon the association of the other with distress—that is, those with higher levels of diarrhea severity reported negative associations between distress and fears of pain medication shortages, and vice versa. One explanation for this interaction effect could be immediacy, where the more proximal concern to a participant (diarrhea symptoms) reduces concern about the more distal.
Finally, we showed that those with a higher level of concern about their GI illness or about COVID‐19 and with higher levels of COVID‐19–related fear reported higher distress. However, when COVID‐19 fear is highest, the association between pain medication shortages and distress is negative, whereas when COVID fear is low, more pain medication shortages are associated with higher distress. Therefore, strategies addressing COVID‐19 fear, such as educational campaigns or psychological interventions improving coping strategies and fostering a greater sense of self‐efficacy, could potentially modify the relationship between shortages and distress.
4.1. Limitations
This survey used a convenience and un‐controlled sample recruited online, and therefore, participant demographics may not correspond to those seen in clinical populations. However, since recruitment for research studies at health clinics has become impractical (due to lockdown of clinics/research labs), given the risk of the virus for researchers, and also due to the burden of the pandemic on health practitioners, we opted to conduct the study online and recruit via GI‐related groups and social media. Arguably, this sample might be more representative of the general population. This is supported by the sample's reported low levels of GI symptoms and good mental health. On the other hand, our sample had a high proportion of persons with university education, which makes it more educated than the general population. In addition, the participants were predominantly female, which limits the generalizability of its findings to males with GI disorders. Nevertheless, for many of these conditions (eg, IBS), the prevalence is much higher among females. For practical reasons, we relied on self‐report measures. We relied on a self‐reported diagnosis, which was not confirmed by a physician since this was most practical during the pandemic. In addition, while some of the scales we used are well‐standardized (eg, DASS‐21), others have not yet undergone a proper psychometric evaluation. For example, our adaptation of the Brief IPQ to the COVID context, while necessary for the study, has not been validated. We have, however, provided reliability scores for this scale. Nonetheless, to undertake our survey on COVID pandemic issues, especially regarding stresses experienced, as close to the time of the pandemic onset as possible, it was necessary to adapt already validated scales in other diseases for our study. Further, while we advertised widely, our inclusion criteria meant we only included people who speak English, which reduces the study's generalizability. We also collected a sample not reflective of the prevalence of specific GI disorders, with IBD and celiac disease overrepresented and IBS underrepresented, most likely due to more effective advertising via these consumer organizations. Finally, the countries of origin of our sample are not equally represented, and therefore, cross‐country comparisons were not practical.
5. CONCLUSION
This international survey documented a significant relationship between personal product shortages, specifically toilet paper, pain medication, and food shortages, and psychological distress in people living with GI conditions at the time of the COVID‐19 pandemic. This relationship was significantly moderated by COVID‐19 prevalence and COVID‐19 fear. Since COVID‐19 fear is a potentially modifiable moderator of this relationship, interventions, and strategies addressing COVID‐19 fear, such as educational campaigns or psychological interventions improving coping and fostering a greater sense of self‐efficacy, could potentially modify the relationship between shortages and distress.
CONFLICT OF INTEREST
The authors have no conflict of interests in relation to this study.
DISCLOSURES
The other authors have nothing to report.
AUTHORS’ CONTRIBUTIONS
AMW conceived and drafted the manuscript and is the guarantor of the article. DS analyzed and interpreted all data. All authors contributed to study design, promotion, and data collection, commented on drafts of the paper, and approved the final draft of the manuscript. SK ran the final check of the data accuracy and manuscript and provided final approval for the study.
Supporting information
Table S1‐S4
ACKNOWLEDGEMENTS
Outside the present work, A. Mikocka‐Walus served as an invited speaker at IBD‐related conferences co‐organized by Crohn's & Colitis Australia (a charity), Janssen and Ferring, and received a speaker's fee. M. Barreiro‐de Acosta has served as a speaker, consultant, and advisory member for or has received research funding from MSD, AbbVie, Janssen, Kern Pharma, Celltrion, Takeda, Gilead, Pfizer, Ferring, Faes Farma, Shire Pharmaceuticals, Dr. Falk Pharma, Chiesi, Gebro Pharma, Adacyte, and Vifor Pharma. Ch. Bernstein has served on advisory Boards for AbbVie Canada, Amgen Canada, Bristol Myers Squibb Canada, Janssen Canada, Roche Canada, Sandoz Canada, Takeda Canada, and Pfizer Canada; consultant for Mylan Pharmaceuticals and Takeda; educational grants from AbbVie Canada, Pfizer Canada, Takeda Canada, and Janssen Canada; speaker’s panel for AbbVie Canada, Janssen Canada, Takeda Canada, and Medtronic Canada; and received research funding from AbbVie Canada. L. Graff has served as a consultant for Roche Canada. R. Gearry has served on advisory boards for AbbVie New Zealand and Australia, Janssen New Zealand; speaker’s panel for AbbVie New Zealand and Australia, Janssen New Zealand, Takeda Australia; and educational grants from AbbVie, New Zealand. A. Stengel has worked as consultant for a + r Berlin, Boehringer Ingelheim, Dr. Wilmar Schwabe, Microbiotica, and Takeda. I. Trindade has received consultancy fees from Pfizer Inc. M van Tilburg has served as a consultant for Mahana Therapeutics, Inc. Outside the present work, S.R Knowles served as an invited speaker at IBD‐related conferences co‐organized by Crohn's & Colitis Australia (a charity) and Coeliac Australia (a charity), is a member of the Medical Advisory Committee for Glutagen Pty Ltd, and has received consultancy fees from AbbVie Pty Ltd and Janssen‐Cilag Pty Ltd.
Mikocka‐Walus A, Skvarc D, van Tilburg MAL, et al. COVID‐19–related personal product shortages are associated with psychological distress in people living with gastrointestinal disorders: A cross‐sectional survey. Neurogastroenterology & Motility.2022;34:e14198. 10.1111/nmo.14198
Funding information
This study received no external funding.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on a reasonable request from the senior author, SK. The data are not publicly available due to restrictions.
REFERENCES
- 1. ECDC . Download today’s data on the geographic distribution of COVID‐19 cases worldwide Stockholm European centre for disease prevention and control. 2020. https://www.ecdc.europa.eu/en/publications‐data/download‐todays‐data‐geographic‐distribution‐covid‐19‐cases‐worldwide
- 2. Davis J, Jasper C, McCarthy M. Shoppers urged to be patient as Victorian coronavirus restrictions impact food supply. ABC Rural. 2020. [Google Scholar]
- 3. Truu M. Half of Australian women were impacted by period product shortages during coronavirus. SBS News. 2020. [Google Scholar]
- 4. Wright P. Coronavirus COVID‐19: why is everyone buying toilet paper? ABC Life. 2020. [Google Scholar]
- 5.Article No. 8383: Over two‐thirds of working Australians have had their employment impacted by the ‘Coronavirus Crisis’ [press release]. 2020.
- 6. Torales J, O'Higgins M, Castaldelli‐Maia JM, Ventriglio A. The outbreak of COVID‐19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317‐320. 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- 7. Sibley CG, Greaves LM, Satherley N, et al. Effects of the COVID‐19 pandemic and nationwide lockdown on trust, attitudes toward government, and well‐being. Am Psychol. 2020;75(5):618‐630. [DOI] [PubMed] [Google Scholar]
- 8. Sperber AD, Bangdiwala SI, Drossman DA, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome foundation global study. Gastroenterology. 2020;160(1):99‐114.e3. [DOI] [PubMed] [Google Scholar]
- 9. Farthing M, Roberts SE, Samuel DG, et al. Survey of digestive health across Europe: Final report. Part 1: The burden of gastrointestinal diseases and the organisation and delivery of gastroenterology services across Europe. United European Gastroenterology J. 2014;2(6):539‐543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther. 2014;40(9):1023‐1034. [DOI] [PubMed] [Google Scholar]
- 11. Everhart JE. The burden of digestive diseases in the United States. Washington, DC: Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease. 2008. [Google Scholar]
- 12. Gracie DJ, Guthrie EA, Hamlin PJ, Ford AC. Bi‐directionality of Brain‐gut interactions in patients with inflammatory bowel disease. Gastroenterology. 2018;154(6):1635‐1646.e3. [DOI] [PubMed] [Google Scholar]
- 13. Koloski N, Holtmann G, Talley NJ. Is there a causal link between psychological disorders and functional gastrointestinal disorders? Expert Rev Gastroenterol Hepatol. 2020;14(11):1047‐1059. [DOI] [PubMed] [Google Scholar]
- 14. Koloski NA, Jones M, Kalantar J, Weltman M, Zaguirre J, Talley NJ. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12‐year prospective population‐based study. Gut. 2012;61(9):1284‐1290. [DOI] [PubMed] [Google Scholar]
- 15. Koloski NA, Jones M, Talley NJ. Evidence that independent gut‐to‐brain and brain‐to‐gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1‐year population‐based prospective study. Aliment Pharmacol Ther. 2016;44(6):592‐600. [DOI] [PubMed] [Google Scholar]
- 16. Iyengar K, Bahl S, Raju V, Vaish A. Challenges and solutions in meeting up the urgent requirement of ventilators for COVID‐19 patients. Diabetes Metab Syndr. 2020;14(4):499‐501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pulk RA, Leber M, Tran L, et al. Dynamic pharmacy leadership during the COVID‐19 crisis: optimizing patient care through formulary and drug shortage management. Am J Health Syst Pharm. 2020;77(22):1874‐1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vincent JL, Creteur J. Ethical aspects of the COVID‐19 crisis: how to deal with an overwhelming shortage of acute beds. Eur Heart J Acute Cardiovasc Care. 2020;9(3):248‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rowan NJ, Laffey JG. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic–Case study from the Republic of Ireland. Sci Total Environ. 2020;725:138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gomes BA, Queiroz FLC, Pereira PLO, et al. In‐House three‐dimensional printing workflow for face shield during COVID‐19 pandemic. J Craniofac Surg. 2020;31(6):e652‐e653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Berardi A, Perinelli DR, Merchant HA, et al. Hand sanitisers amid CoViD‐19: a critical review of alcohol‐based products on the market and formulation approaches to respond to increasing demand. Int J Pharm. 2020;584:119431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Arafat SMY, Kar SK, Menon V, et al. Panic buying: an insight from the content analysis of media reports during COVID‐19 pandemic. Neurol Psychiatry Brain Res. 2020;37:100‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tolin DF, Abramowitz JS, Brigidi BD, Foa EB. Intolerance of uncertainty in obsessive‐compulsive disorder. J Anxiety Disord. 2003;17(2):233‐242. [DOI] [PubMed] [Google Scholar]
- 24. Castriotta N, Dozier ME, Taylor CT, Mayes T, Ayers CR. Intolerance of uncertainty in hoarding disorder. J Obsessive Compuls Relat Disord. 2019;21:97‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. OzForex . Yearly average rates. https://www.ofx.com/en‐au/forex‐news/historical‐exchange‐rates/yearly‐average‐rates/2020
- 26. Henry JD, Crawford JR. The short‐form version of the depression anxiety stress scales (DASS‐21): construct validity and normative data in a large non‐clinical sample. Br J Clin Psychol. 2005;44(Pt 2):227‐239. [DOI] [PubMed] [Google Scholar]
- 27. Dimenäs E, Glise H, Hallerbäck B, Hernqvist H, Svedlund J, Wiklund I. Well‐being and gastrointestinal symptoms among patients referred to endoscopy owing to suspected duodenal ulcer. Scand J Gastroenterol. 1995;30(11):1046‐1052. [DOI] [PubMed] [Google Scholar]
- 28. Roser M, Ritchie H, Ortiz‐Ospina E, Hasell J. COVID‐19 Data Repository: "Coronavirus Pandemic (COVID‐19)". In: University TCfSSaECaJH. Published online at OurWorldInData.org2020.
- 29. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631‐637. [DOI] [PubMed] [Google Scholar]
- 30. Moss‐Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D. The revised illness perception questionnaire (IPQ‐R). Psychol Health. 2002;17:1‐16. [Google Scholar]
- 31. Arrindell WA, Ross MW, Bridges R, Hout W, Hofman A, Sanderman R. Fear of aids: are there replicable, invariant questionnaire dimensions? Adv Behav Res Ther. 1989;11:69‐115. [Google Scholar]
- 32. Trindade IA, Ferreira NB. COVID‐19 Pandemic's Effects on disease and psychological outcomes of people with inflammatory bowel disease in Portugal: a preliminary research. Inflamm Bowel Dis. 2020;izaa261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. The jamovi project . 2021. jamovi (Version 1.6) [Computer Software]. Retrieved from https://www.jamovi.org
- 34. Fox J, Weisberg S. Car: Companion to Applied Regression. [R package]. 2018.
- 35. Lenth R. Emmeans: Estimated Marginal Means, aka Least‐Squares Means. [R package]. 2018.
- 36. Mikocka‐Walus A, Knowles SR, Keefer L, Graff L. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2016;22(3):752‐762. [DOI] [PubMed] [Google Scholar]
- 37. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. IASC . Addressing mental health and psychosocial aspects of COVID‐19 outbreak Version 1.5. Geneva: United Nations Inter‐Agency Standing Committee (IASC); 2020.Reference Group on Mental Health and Psychosocial Support in Emergency Settings. 2020.
- 39. A.L. van Tilburg M, Edlynn E, Maddaloni M, van Kempen K, Díaz‐González de Ferris M, Thomas J. High levels of stress due to the SARS‐CoV‐2 pandemic among parents of children with and without chronic conditions across the USA. Children. 2020;7(10):193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hobbis IC, Turpin G, Read NW. Abnormal illness behaviour and locus of control in patients with functional bowel disorders. Br J Health Psychol. 2003;8(Pt 4):393‐408. [DOI] [PubMed] [Google Scholar]
- 41. O'Connor P, Anglim J, Smillie L. Disagreeability, neuroticism and stress: what drives panic buying during the COVID‐19 pandemic. The Conversation. 2020.
- 42. Australia tops coronavirus consumer panic [press release]. Sydney, NSW: UNSW. 2020. https://newsroom.unsw.edu.au/news/business‐law/australia‐tops‐coronavirus‐consumer‐panic [Google Scholar]
- 43. Prentice C, Chen J, Stantic B. Timed intervention in COVID‐19 and panic buying. J Retail Consum Serv. 2020;57:102203. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S4
Data Availability Statement
The data that support the findings of this study are available on a reasonable request from the senior author, SK. The data are not publicly available due to restrictions.


