Abstract
During the COVID‐19 pandemic, first responders and health care workers faced elevated virus‐related risks through prolonged contacts with the public. Research suggests that these workers already experienced lower levels of psychological well‐being linked to occupational risks. Thus, the pandemic’s impact might have particularly affected mental health in these groups. This paper analysed data from a large‐scale Welsh population study (N = 12,989) from June to July 2020. Levels of psychological distress were compared across various occupations, including police, fire and rescue, and NHS health care workers. Resilience was also indexed, and its role considered as a protective factor for psychological distress. Surprisingly, health care workers reported lower distress levels than the general population. Further, fire and rescue and police groups had lower distress than most groups and significantly higher resilience. Within police officers, higher resilience levels were protective for distress. Fire and rescue workers were half as likely as others to report distress, even accounting for demographic factors and resilience. The findings offer an optimistic view of psychological resilience in these critical occupations. They illustrate potential benefits to one’s mental health of playing a crucial societal role during crises and reiterate the importance of enhancing resilience within groups who encounter high‐risk situations daily.
Practitioner points
Our findings provide evidence that health care workers and first responders showed lower levels of psychological distress than the general population during the first period of lockdown due to the COVID‐19 pandemic in the United Kingdom. This may indicate that playing a critical role in society during an episode of crisis, and acting to help others, may be protective of one’s own mental health.
The research also provides an optimistic view of the psychological resilience of critical first responders and health care workers during a period early on in the COVID‐19 pandemic (June–July 2020). This highlights the benefits of fostering resilience in those working within high‐risk first responder and health care occupations.
Keywords: COVID‐19, first responders, health care workers, mental wellbeing, pandemic, psychological distress, resilience
Background
During the spring and summer of 2020, cases of COVID‐19 exponentially grew as it spread rapidly from country to country. In efforts to minimize its transmission, governments in many countries issued lockdowns where schools and non‐essential services were ordered to close. While the majority of workers remained at home, many of those employed in roles considered critical in maintaining the supply of essential goods, infrastructure, and public services had to travel to their workplaces to perform their professional duties.
Those working as first responders and health care workers were in frequent close contact with the public, elevating their risk of contracting the virus, which was circulating within the community. Physical proximity to people is an inevitable consequence of these professions, bringing with it occupational physical health risks. Each day emergency and health care professionals face possible injury or death, and exposure to a wide range of diseases and infections (Sawhney, Jennings, Britt, & Sliter, 2017). In fulfilling their roles during 2020, these groups of essential workers have faced an additional and novel occupational health risk: COVID‐19. Inflated case rates were seen in firefighters, police, and medical service providers during the spring and summer of 2020 (Khadse, Gowda, Ganjekar, Desai, & Murthy, 2020; Nguyen et␣al., 2020; Weiden et␣al., 2020). In March 2020, health care workers within the United States and the United Kingdom had a three‐fold increased risk of being infected with COVID‐19 (Nguyen et␣al., 2020), while between March and May, COVID‐19 infection rates were 15 times higher for New York firefighters and emergency medical service providers than that seen in the general public (Weiden et␣al., 2020). By the end of August 2020, infection rates were over eight times higher for members of the Indian Police Force than in the general population of India (Khadse et␣al., 2020).
While professionals in these occupations are undoubtedly aware of the heightened physical dangers they face in doing their jobs, there are also mental health consequences from being at risk, which may amplify during an outbreak of infectious disease such as the COVID‐19 pandemic. The day‐to‐day threat of contracting blood‐borne viral infections from exposure to blood and bodily fluids have been shown to have a detrimental impact on psychological well‐being in these professions (Dunleavy, Taylor, Gow, Cullen, & Roy, 2012; Jahnke, Poston, Jitnarin, & Haddock, 2012; Sawhney et␣al., 2017). However, these exposures relate to encounters with the public outside of a pandemic. During infectious disease outbreaks, first responder and health care staff concerns are likely intensified as close proximity with the public brings heightened health risks. Frontline health care workers during the Severe Acute Respiratory Syndrome (SARS) outbreak of 2002–2004 experienced higher levels of stress and perceived risk than those not involved with direct patient care (Brooks, Dunn, Amlôt, Rubin, & Greenberg, 2018). Additionally, these professionals had a greater likelihood of common mental disorders and displayed higher levels of distress than those not involved in direct care (Brooks et␣al., 2018). Further, the perception of risk was found predictive of post‐traumatic symptoms (Brooks et␣al., 2018). Given the rapid transmission of COVID‐19, and the possible health consequences associating with contracting the disease, both for the individual themselves and their families, it seems likely that first responders and health care workers were alert to being at a greater occupational health risk than usual. This awareness of increased risk would potentially have a negative impact on psychological distress and mental well‐being.
Evidence suggests that first responders and health care workers already had reduced levels of psychological well‐being prior to the pandemic. Members of law enforcement have higher rates of mental health problems and are more likely to experience depression than the general population (Stogner, Miller, & McLean, 2020). Rates of depression and anxiety have been estimated at 15% in ambulance personnel, with 27% experiencing psychological distress (Petrie et␣al., 2018). In firefighters, frequent and repeated exposure to traumatic events through their day‐to‐day work has shown to impact upon mental health and lead to symptoms of post‐traumatic disorder (Jahnke et␣al., 2012; Sawhney et␣al., 2017). Awareness of increased risk to COVID‐19 infection may have compounded these underlying mental health problems and exposure to other occupational risks prevalent across these occupations. Therefore, it seems possible that first responders and health care workers may have been doubly impacted by COVID‐19, given already inflated rates of mental disorder and lower levels of psychological well‐being.
However, the impact of COVID‐19 may not be any greater in these occupational groups than in the general population. Research has repeatedly identified substantial increases in psychological distress and decreases in mental well‐being when comparing population data from 2017 to 2019 against that from 2020 (Lamb, Greenberg, Stevelink, & Wessely, 2020). Several factors have consistently emerged which have been associated with poorer mental health during the pandemic. Those who were younger, experiencing higher levels of deprivation, or who were female reported higher levels of psychological distress and lower levels of mental well‐being in studies across the world (Gray et␣al., 2020; McGinty, Presskreischer, Han, & Barry, 2020; Pierce et␣al., 2020; Wang et␣al., 2020). Subsequent follow‐up studies suggest that lower mental well‐being continued to persist into late summer and that the factors previously identified as being associated with this impact continued to be of importance (e.g., McGinty, Presskreischer, Anderson, Han, & Barry, 2020).
Research comparing psychological distress levels in first responder and health care staff to those in general populations during spring and summer of 2020 has generated mixed findings (Lamb et␣al., 2020). Some studies have identified similar levels of anxiety and depression in health care and non‐health care workers (Barzilay et␣al., 2020), while others have reported higher levels of depression, anxiety and post‐traumatic stress disorder in frontline workers when compared with the general population (Lamb et␣al., 2020). It is therefore unclear if particular occupations have experienced adverse effects of the COVID‐19 pandemic on their psychological well‐being, over and above that evident across community studies.
One variable which has emerged as particularly protective towards psychological distress during COVID‐19 is resilience. This has been defined as a process which facilitates adaptation during difficult times and involves psychologically bouncing back from adversity (Hu, Zhang, & Wang, 2015). Importantly, resilience does not imply that the individual is not negatively impacted by the particular stressor or traumatic event, only that they are able to recover relatively quickly, and return to pre‐stressor levels of functioning (Bonanno, 2005), perhaps even returning to better than premorbid levels of functioning. Across occupations, resilience is well‐established as an important factor for personal well‐being and professional performance (Robertson, Cooper, Sarkar, & Curran, 2015). Resilience is seen as important given the stress and exposure to trauma which are experienced by those in first responder and health care roles.
While resilience can be individual, community, or national, the latter two have not proven to have predictive value for mental distress during the COVID‐19 pandemic (Kimhi, Marciano, Eshel, & Adini, 2020) and will not be considered here. However, studies exploring an individual’s resilience and mental well‐being during the COVID‐19 outbreak have demonstrated its protective importance. In these studies, strong relationships have emerged between being younger, female, or experiencing economic difficulties and higher levels of psychological distress, anxiety, and depression (Barzilay et␣al., 2020; Kavčič, Avsec, & Kocjan, 2020; Kimhi et␣al., 2020). However, the predictive value of these demographic characteristics diminished once resilience was accounted for (Kavčič et␣al., 2020). Levels of resilience were found to correlate moderately with well‐being, and the higher the levels of resilience, the lower the levels of reported distress (Kimhi et␣al., 2020), anxiety, and depression (Barzilay et␣al., 2020). These findings support evidence from previous epidemics and pandemics, where resilience indicators have been identified as protective to psychological functioning in health care workers (Preti et␣al., 2020).
It is possible that despite the additional risks for the first responders and health care workers, through experiencing regular trauma, they have greater resilience. If these groups have enhanced levels of resilience, this may have acted protectively against experiencing elevated levels of psychological distress associated with heightened personal risk from proximity to the public. Thus, while mental well‐being levels in these groups have been reported to be lower (e.g., Petrie et␣al., 2018; Stogner et␣al., 2020), they may have been less affected by the COVID‐19 pandemic than the public.
The present study
The main objective of this study was to assess levels of psychological distress within first responder groups and health care staff during a period of National lock‐down within Wales during the COVID‐19 pandemic (June–July 2020). The study aimed to ascertain if levels of psychological distress differed between these groups of front‐line workers and analyse whether resilience levels moderated the psychological impact of COVID during this time period.
The data used in this study was collected as part of a Wales‐wide project. Findings on the factors of age, gender, and relative deprivation levels have been published elsewhere (Gray et␣al., 2020).
Materials and method
Participants
Supporting health care and first responder organizations publicized the survey, sharing the social media advertisements and disseminating the survey to their staff via email. The project was supported by all four police forces in Wales, the seven National Health Service (NHS) Health Boards in Wales, the three Fire and Rescue Services in Wales, and the Welsh Ambulance Service Trust. Furthermore, third party sector organizations, GPs, the Welsh Farming Union, care homes and a number of large employers and government organizations also supported the study. The participant sample within the general population was recruited online via social media and snowball sampling. Using Twitter, Facebook, and Instagram, advertisements promoted the survey across Wales in Welsh and English language and provided URL links to access it. In addition to social media promotion and access to the survey, it was advertised in newspapers and radio programmes. Paper versions of the survey were provided on request to help support access to the survey by hard‐to‐reach groups of people without access to the internet.
The study was available to complete for those aged 16 and over. A minimum sample size (n = 250) was recruited from each of the 22 Welsh Local Authorities to ensure representation of participants across the population of Wales and in all geographical areas.
The research was registered with ISRCTN (ref: 21598625), and the Research Ethics Committee at the College of Health and Human Sciences, Swansea University granted ethical approval for the research. The study protocol is available online at https://www.swansea.ac.uk/psychology/research‐at‐the‐department‐of‐psychology/research‐protocols/.
Measures
Demographic data were collected including age, relationship status, gender, ethnicity, and deprivation index (calculated from participant postcodes). Participants also provided employment information. Those who indicated they were a critical or ‘key worker’, as defined at the time of the survey by the UK government (UK Government, 2020), were asked to indicate their area of employment (e.g., health care worker, ambulance service employee, police, fire or rescue, transport worker, and education.).
Participant’s mental well‐being and levels of psychological distress were measured using the Kessler Distress Scale (K10; Kessler et␣al., 2002). Resilience was assessed using the ‘stress immunity’ sub‐scale of the Triarchic Psychopathy Measure (TriPM; Patrick, 2010) and a single item of the Brief Resilience Scale (BRS; Smith et␣al., 2008), adapted for the survey.
The K10 was selected as it is a short measure indexing non‐specific psychological distress rather than disorder‐specific mental health issues and designed for use in population health studies (Kessler et␣al., 2002). The ‘stress immunity’ sub‐scale is similarly advantageous in both its brevity and the TriPM demonstrates utility within community samples (van Dongen, Drislane, Nijman, Soe‐Agnie, & van Marle, 2017). Further, the ‘stress immunity’ scale indexes multiple resilience factors. Thus, it is complementary to the item selected from the BRS, which measures an ability to bounce back in the face of adversity, perhaps the most literal interpretation of resilience (Smith et␣al., 2008), and certainly highly relevant in an enduring, global challenge such as a pandemic.
Questions were included about stressors experienced before and since the COVID pandemic along with a mental well‐being measure. Further, participants were asked about aspects of the lockdown which they had enjoyed, corresponding with recent ethical guidance for COVID‐19 research (Townsend, Nielsen, Allister, & Cassidy, 2020). Data and analysis of the mental well‐being measure, stressors, and positive aspects of lockdown are not included in this publication due to the quantity of data generated.
Psychological distress
The K10 (Kessler et␣al., 2002) measures the level of psychological distress over the prior 30 days. It assesses levels of anxiety and depression symptoms and has been used widely across the world (e.g., Donker et␣al., 2010) and in translated forms (e.g., Vissoci et␣al., 2018).
The measure comprises ten questions which focus on experiencing symptoms of anxiety and depression. Respondents indicate how often over the last 30 days they had experienced each symptom on a five‐point Likert Scale (1 = ‘none of the time’ to 5 = ‘all of the time’). To be consistent with other measures taken on the survey, participants were asked to rate their levels of distress over the previous 2 weeks, rather than 30 days. The higher the total score, the higher an individual’s level of psychological distress. Within this sample, the K10 internal consistency was high (Cronbach α = .93).
Resilience
The stress immunity sub‐scale from the Triarchic Psychopathy Measure (TriPM; Patrick, 2010) was one of two measures taken to assess resilience. The 58‐item TriPM indexes three domains associated with psychopathy: disinhibition (20 items), meanness (19 items), and boldness (19 items). Recent analysis has revealed an underlying factor of being ‘stress immune’ within the TriPM boldness domain (Roy et␣al., 2019). Six questions comprise this factor and assess several aspects of resilience: overcoming trauma, a lack of fear, and high self‐confidence levels. Importantly, the stress immunity sub‐scale of the TriPM does not measure current functioning, but rather indexes a stable personality trait measuring how resilient the individual is to stress and trauma (Hu et␣al., 2015).
In the TriPM, participants respond to questions on a four‐point Likert scale (1 = ‘true’ to 4 = ‘false’), with each scored between 0 and 3. The higher the total score, the higher the level of stress immunity or resilience. Within the sample, the internal consistency for stress immunity was high (Cronbach α = .75).
The second resilience measure was an adaptation of the first item from the Brief Resilience Scale (BRS; Smith et␣al., 2008). Using a sliding scale (0 = ‘not at all’ to 10 = ‘completely’) participants indicated the extent to which they felt that ‘Overall, I tend to bounce back quickly after difficult times’. Higher scores indicate higher levels of resilience.
The BRS has previously demonstrated high test‐retest reliability (Chmitorz et␣al., 2018) and good convergent, concurrent, and predictive validity (Rodríguez‐Rey, Alonso‐Tapia, & Hernansaiz‐Garrido, 2016). The item adapted from the BRS had high factor loadings (0.70–0.89) with the total six item scale (Smith et␣al., 2008) and represents an appropriate time sensitive measure of resilience.
Welsh index of multiple deprivation
The Welsh Index of Multiple Deprivation (WIMD; Statistics for Wales, 2019) is the Welsh Government measure of relative deprivation across the country. It combines a range of factors including income, employment, health, housing, and physical environment to measure relative deprivation across Wales. In total, there are 1909 small areas within Wales, determined by residential postcode and each containing approximately 1,600 people. The WIMD ranks these from 1 (‘most deprived’) through to 1909 (‘least deprived’).
Procedure
Data was collected online (Qualtrics, Version: June 2020, Provo, UT, USA, Copyright © 2020) for over 99% of participants, between 9 June 2020 and 13 July 2020. The remainder of responses were completed on paper and sent by post. The survey was available in Welsh and English languages and was designed to take around 10 min to complete. Participants who were unable to access or use the online version were able to call a widely advertised dedicated number to have a paper copy of the survey and a prepaid return envelope.
Interested participants were taken to the online survey. In line with guidance on ethical research on COVID‐19 (Townsend et␣al., 2020), it was highlighted that questions would ask about emotional well‐being and recent experiences during the pandemic. If they provided informed consent and were age 16 or over, participants could continue with the study.
Following the questions, participants were debriefed and thanked for participation. Links to sources of Wales‐wide 24/7 confidential support were provided if participants were experiencing emotional difficulties.
Data analysis plan
To examine differences between employment group on each of the three measures, a series of ANOVAs (analysis of variance) were completed with the significance level set at p <.05. Any significant inter‐group differences were explored using multiple comparisons with Bonferroni corrections. In groups with significantly lower levels of psychological distress, hierarchical logistic regression analyses examined whether additional demographic factors or levels of resilience moderated the relationship between group membership and psychological distress.
Results
Demographics
In total, 15,469 participants consented and commenced the survey. Of these, 2,417 were excluded from further analysis as they did not complete 50% or more of the survey. As the median response time for the survey was 647s (IQR: 510–863), a further 63 participants who completed the survey in <240 s were removed from the analysis as this was considered too quick to have responded carefully to the questions. This process resulted in a final sample size of N = 12,989. However, as not all participants completed each section of the survey, numbers included in each analysis will be stated throughout.
Ambulance, fire and rescue, police, and National Health Service (NHS) health care workers were analysed as individual groups. Other participants identifying as keyworkers were collapsed into a comparison ‘other keyworkers’ group, and non‐keyworkers were grouped as ‘general population’. Table 1 provides summary demographics of age, gender, and ethnicity for these groupings. Table 2 displays the number of participants per employment group along with mean scores for each of the measures of the K10, the Stress Immunity scale and the single item resilience rating. Table 3 illustrates the number and percentage of participants, per employment group, with K10 psychological distress scores falling in the range of 0–19 (psychologically well) 20–24, (mild mental disorder/distress), 25–29 (moderate disorder/distress), and 30 or more (severe mental disorder/distress).
Table 1.
Number of participants (percentage) per gender, per age group and per ethnicity grouping for each employment group
| Employment group | Number of participants (%) | Participant age | Participant ethnicity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 16–24 | 25–34 | 35–44 | 45–54 | 55+ | White – any | Asian – any | Black – any | Mixed – any | Other | Prefer not to say/no response | |
| NHS healthcare | 255 (11.8) | 1,893 (87.4) | 50 | 368 | 527 | 730 | 492 | 2,084 | 43 | 4 | 19 | 3 | 14 |
| Police | 193 (40.5) | 280 (58.8) | 16 | 96 | 148 | 163 | 53 | 465 | 1 | 1 | 2 | 1 | 6 |
| Fire and rescue | 129 (52.2) | 117 (47.4) | 6 | 28 | 71 | 102 | 40 | 244 | 0 | 0 | 0 | 1 | 2 |
| Ambulance | 31 (31.0) | 68 (68.0) | 2 | 14 | 30 | 37 | 17 | 98 | 0 | 0 | 2 | 0 | 0 |
| Other keyworkers | 485 (16.3) | 2,457 (82.7) | 77 | 536 | 770 | 936 | 652 | 2,883 | 17 | 3 | 25 | 20 | 23 |
| General population | 1,397 (19.9) | 5,576 (79.3) | 552 | 828 | 1,101 | 1,286 | 3,261 | 6,779 | 69 | 8 | 62 | 49 | 61 |
Table 2.
Mean scores and standard deviations for the measures of psychological distress, stress immunity, and single item resilience per employment group
| Employment Group | N | K10 (psychological distress) | Single item resilience | Stress immunity (resilience) | |||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | ||
| NHS Healthcare | 2,167 | 2,090 | 21.68 (7.81) | 2,157 | 7.03 (2.18) | 2,070 | 9.40 (3.18) |
| Police | 476 | 458 | 20.94 (7.63) | 473 | 7.25 (2.05) | 465 | 10.39 (3.37) |
| Fire and Rescue | 247 | 241 | 19.23 (6.79) | 244 | 7.64 (1.87) | 238 | 10.62 (3.16) |
| Ambulance | 100 | 99 | 22.88 (9.48) | 100 | 7.05 (2.19) | 99 | 10.19 (3.36) |
| Other keyworkers | 2,971 | 2,860 | 22.57 (7.86) | 2,955 | 6.84 (2.26) | 2,868 | 9.08 (3.36) |
| General population | 7,028 | 6,768 | 22.49 (8.63) | 6,973 | 6.70 (2.45) | 6,750 | 8.91 (3.53) |
| Total | 12,989 | 12,516 | 12,902 | 12,490 | |||
K10 = Kessler Distress Scale; Single item resilience = ‘Overall, I tend to bounce back quickly from difficult times’; Stress Immunity = Stress Immune subscale from Triarchic Psychopathy Measure.
Table 3.
Number of participants (percentage) per psychological distress category, per employment group
| Employment group | K10 (psychological distress) category and score | |||
|---|---|---|---|---|
|
Psychologically well 0–19 |
Mild mental disorder/distress 20–24 |
Moderate mental disorder/distress 25–29 |
Severe mental disorder/distress 30+ |
|
| NHS Healthcare | 977 (46.7) | 409 (19.6) | 327 (15.6) | 377 (18.0) |
| Police | 230 (50.2) | 85 (18.6) | 81 (17.7) | 62 (13.5) |
| Fire and rescue | 143 (57.3) | 46 (19.1) | 29 (12.0) | 23 (9.5) |
| Ambulance | 47 (47.5) | 14 (14.1) | 12 (12.1) | 26 (26.3) |
| Other keyworkers | 1,143 (40.0) | 613 (21.4) | 544 (19.0) | 560 (19.6) |
| General population | 2,913 (43.0) | 1,288 (19.0) | 1,092 (16.1) | 1,475 (21.8) |
| TOTAL | 5,453 (43.6) | 2,455 (19.6) | 2,085 (16.7) | 2,523 (20.2) |
K10 = Kessler Distress Scale.
Across all employment groups, aside from Police and Fire and Rescue, over half of the participants reported psychological distress of varying severity. Moderate levels of resilience indexed by the Stress Immune subscale of the TriPM were reported, given that the sub‐scale score can range from 0 to 18. Similarly, moderate to good levels of the tendency to bounce‐back were reported by the participants on the BRS single‐item as these responses could range from 0 (not at all) to 10 (completely).
Comparisons between groups
A series of ANOVAs (analysis of variance) were completed to analyse between‐employment group differences on each of the three measures.
Psychological distress
Figure 1 shows the levels of psychological distress (K10) for each group. Scores differed significantly between the groups: F(5, 12510) = 12.88, p < .001, = .005. The Ambulance and Other keyworker groups did not differ from the control group in levels of distress. However, several groups reported less psychological distress than the control group: fire and rescue (p < .001), police (p = .001), and NHS health care workers (p = .001).
Figure 1.
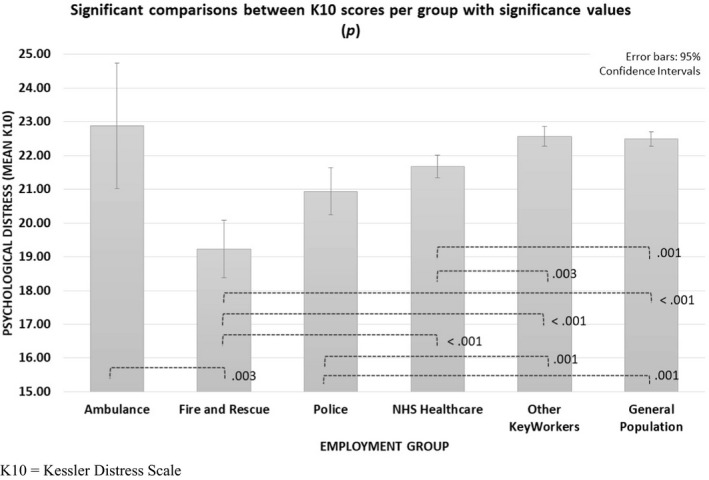
Significant comparisons between employment groups for the K10 measure, showing significant p values. K10 = Kessler Distress Scale.
Resilience
Figure 2 shows the levels of stress‐immunity (TriPM) for each group. Significant differences emerged between group scores: F(5, 12484) = 32.06, p < .001, = .013.
Figure 2.
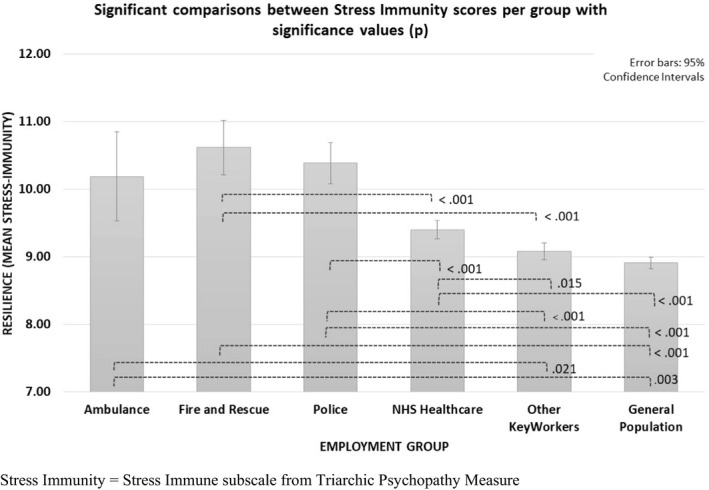
Significant comparisons between employment groups for the Stress Immunity measure, showing significant p values. Stress Immunity = Stress Immune subscale from Triarchic Psychopathy Measure.
Fire and rescue employees and police staff had significantly higher stress‐immunity scores compared with NHS health care workers (p < .001), other keyworkers (p < .001), and the general population group (p < .001). There was no difference in stress‐immunity scores between ambulance workers, police staff, and fire and rescue workers. However, ambulance workers reported significantly higher stress‐immunity scores than other keyworkers (p = .021) and the general population group (p = .003). Similarly, NHS health care workers had higher stress immunity than other keyworkers (p = .015) and the general population (p < .001).
Figure 3 shows the levels of resilience from the brief resilience measure. Scores differed between the groups: F(5, 12896) = 16.74, p < .001, = .006. Fire and rescue workers had significantly higher resilience scores than NHS health care workers (p = .002), other key workers (p < .001), and the general population group (p < .001). NHS health care workers had higher stress immunity than other keyworkers (p = .042), and the general population (p < .001). However, unlike the stress‐immunity scores, there was no difference between police staff and NHS health care workers, and resilience scores did not differ between ambulance workers and any other groups.
Figure 3.
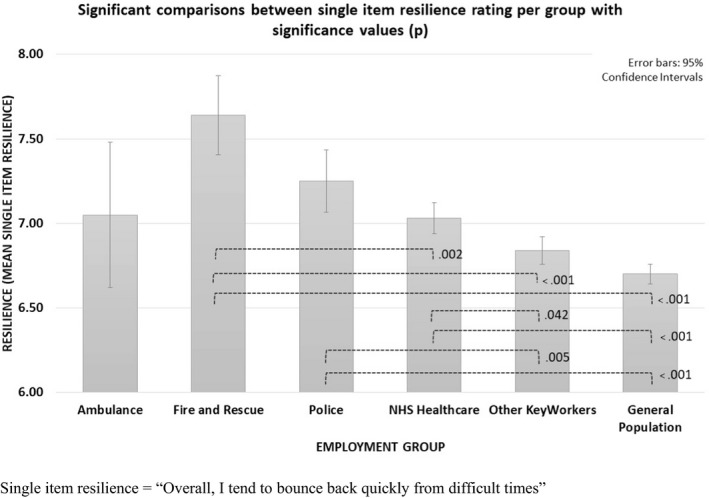
Significant comparisons between employment groups for the single item resilience rating, showing significant p values. Single item resilience = ‘Overall, I tend to bounce back quickly from difficult times’
Regression analyses
As fire service employees had significantly lower levels of psychological distress than all employment groups other than police, logistic regressions were completed for both of these employment groups. K10 scores (‘low’ = less than 25, ‘high’ = 25 or more) were entered as the dependent variable. Employment group (yes, no) was entered as the predictor variable. Separate analyses of the survey data (Gray et␣al., 2020), found that gender, age, and deprivation index were all related to levels of psychological distress. Therefore, models were adjusted for possible effects of these variables. Further, as resilience may relate to levels of psychological distress, scores on the stress immunity scale were added to the models. Table 4 displays the results of these regressions.
Table 4.
Logistic regressions. Numbers in square brackets represent 95% confidence intervals
| Employment group | n | Odds ratio | Adjusted odds ratio (gender, age, deprivation index) | Adjusted odds ratio (gender, age, deprivation index and stress‐immunity) | |
|---|---|---|---|---|---|
| Fire | High distress (K10) | 12,415 | 0.46 (0.33, 0.62)*** | 0.49 (0.34, 0.69) *** | 0.59 (0.41, 0.84)** |
| Police | High distress (K10) | 12,516 | 0.77 (0.63, 0.94)* | 0.76 (0.60, 0.96)* | 0.96 (0.75, 1.24) |
K10 = Kessler Distress Scale.
p < .001; **p < .01, *p < .05.
The regression analyses revealed that those in the fire and rescue services were.46 times as likely to be distressed during the survey period than those not in the fire and rescue services. Adjustment for the effects of the variables, and stress immunity scores had little effect on the model.
Those in the police force were 0.77 times as likely to be distressed during this period than those not in the police force. Adjustments for effects of gender, age, and deprivation index did not affect the overall results. However, the inclusion of the stress immunity scores reduced the odds ratio to no different to 1.0.
Discussion
The data present a generally optimistic picture of levels of psychological distress within first responders during the summer of 2020 in comparison to other groups. However, it should be noted that this is a relative judgment against a population that has been shown to have greatly reduced psychological health (Gray et␣al., 2020) and it seems likely that levels of distress are greater than pre‐COVID levels in all groups.
NHS health care workers reported lower levels of distress than the group of other keyworkers and the general population group, while fire and rescue service employees had significantly lower distress than all other groups, aside from the police. These findings point to an enhanced level of psychological well‐being in these groups, contrasting with other studies suggesting either comparable or lower levels in frontline and health care workers, when compared with the general public (Lamb et␣al., 2020). While it is unknown if these first responder groups were less affected by the COVID‐19 pandemic than the general public, or if they had better mental well‐being prior to the pandemic, these findings are positive regardless.
Levels of resilience, indexed by scores on the stress immunity scale, were significantly higher in fire and rescue, and police employees, when compared with NHS health care workers, other key workers, and the general population group. This may partly relate to the lower levels of psychological distress reported in these groups, as prior research has illustrated the importance of resilience on psychological well‐being (Barzilay et␣al., 2020; Kavčič et␣al., 2020; Kimhi et␣al., 2020). Thus, this may be further evidence that resilience acts protectively against psychological distress. Given the extreme challenges faced by these groups of professionals, heightened during unprecedented times such as the COVID‐19 pandemic, these are reassuring findings. Higher levels of resilience in these professions may stem from greater levels of inherent resilience, particular training programmes, or other factors. These data, again, illustrate the importance of fostering resilience within high‐risk occupations.
Higher resilience appears to have accounted for the lower levels of distress reported by the police group, and interestingly, the fire and rescue group were almost half as likely to suffer from psychological distress. This relationship held even after socio‐economic factors and resilience levels were accounted for. Thus, membership of the fire and rescue group alone accounted for better psychological functioning during this period.
Considering the reasons for lower levels of psychological distress in first responders, one explanation may lie in the factors that are most causal to this psychological distress in the general population. While fear of contracting COVID‐19 is undoubtedly a factor, it appears that social isolation, possible loss of employment, and financial worries may play a greater role (Birditt et␣al., 2021; Wilson et␣al., 2020). The need for first responders to continue in their employment during the crisis may therefore mean that they have less exposure to these particular stressors and hence, suffer a smaller drop in psychological health in comparison to others.
However, the comparatively lower levels of psychological distress in first responders and health care workers may stem from the altruistic nature of these professional roles. Research finds that helping others and performing acts of kindness can boost subjective psychological well‐being with small to medium effect sizes (Curry et␣al., 2018). Such prosocial behaviours have been shown to increase happiness, reduce anxiety, and lead to feelings of connectedness and satisfaction (VanderWeele, 2020). As altruism is central in first responder and health care roles and is a regular part of the day job, it seems feasible that working in such occupations that involve a high degree of assisting others may have minimized psychological distress levels.
It is also possible that the significant differences in psychological distress reported here may have been a compound effect of both of these factors. The controls imposed across people in Wales to limit the transmission of the virus during this period have been restrictive, led to particular stressors and subsequently resulted in a decline in psychological wellbeing. In contrast, those in first responder and health care roles have been able to maintain greater social interactions, experience little change in job and financial securities, and minimize distress through gaining benefit from performing altruism within their professions.
An alternative interpretation of these findings comes from a theoretical model illustrating individual and community emotional responses across phases of disaster situations. Zunin and Mayers (as cited in DeWolfe, 2000) proposed that in the run up to, and immediately following, the impact of a disaster there is an ‘impact’ phase, marked by emotional decline and feelings of confusion, shock, and panic. After this, as people take on selfless and altruistic acts to help those in need, they move into an ‘heroic phase, where accordingly emotional distress lessens. It is possible that our data reflects groups in distinct positions along this trajectory, and that the ‘heroic’ jobs of our first responders have emphasized this ‘heroic’ phase of the emotional response following natural disasters. The general population may have remained in the ‘impact’ phase for longer, as for the majority their confinement prevented them from assisting others and thus they were unable to become ‘heroic’ and engage sufficiently in acts to assist others. Contrastingly, those in first responder roles were able to make a difference and actively treat those who had been infected by the virus. Thus, they could move beyond the ‘impact’ phase of their general population counterparts and into the ‘heroic’ phase, improving their emotional and mental well‐being. Zunin and Mayers’ model has clear applications to the current situation that the global population finds itself in (The Kings Fund, 2021), and this is important to consider when exploring the psychological impact of pandemics such as these. Critically, the model predicts even greater psychological decline than in the ‘impact’ phase later in the natural evolution of psychological response to natural disaster, when there is a lengthy period of ‘disillusionment’. Thus, studies gathering data from late into 2020 and into 2021 may yield levels of psychological distress greater than evidenced here, which may not demonstrate differences between first responders and other occupational groups, or which may even predict a greater rebound effect for the first responder groups.
Limitations
No pre‐COVID data was available for these groups to offer comparisons with current levels of distress and resilience. Thus, this study can only offer a snapshot of the psychological distress within these groups during this period. Further, this was an opportunistic sample and may not be wholly representative of these occupational groups. Additionally, while resilience accounts for some of the differences, the cross‐sectional nature of the data may confound this, where individuals report high resilience because they are currently well (i.e., individuals that were less resilient may have not been able, or inclined, to complete the survey).
This research would benefit from subsequent surveys to gather longitudinal data over an extended period as the COVID‐19 pandemic continues into 2021 and beyond. It would be beneficial to assess how predictive resilience is for reduced psychological distress over time. Further, it may be advantageous to consider incorporating a qualitative element in future longitudinal studies, capturing personal accounts of stress management and coping strategies; gathering such detail may go some way towards elucidating the differences in distress and resilience evident here between occupational groups.
Conclusion
Together, the data provide an encouraging view on the psychological resilience of critical first responder workers and health care staff during a time of great difficulty for the nation and the world. Against predictions, fire and rescue staff, police and NHS health care workers who were dealing face to face with the public reported lower levels of psychological distress than the general population. Police and fire and rescue workers also reported higher resilience levels. Those with responsibility for occupational psychology should look to further enhance resilience within these groups, given the protective nature of resilience within workers who face challenging situations on a daily basis. Future studies should look to explore these factors further, and map resilience and psychological distress over time, given the challenges that the COVID‐19 pandemic has brought upon the world.
Author Contribution
Jennifer Pink: Formal analysis (equal); Investigation (equal); Software (equal); Visualization (equal); Writing – original draft (equal). Nicola S Gray: Conceptualization (equal); Investigation (equal); Methodology (equal); Supervision (equal); Writing – review & editing (equal). Chris O'Connor: Conceptualization (equal); Investigation (equal); Methodology (equal); Writing – review & editing (equal). James R Knowles: Investigation (equal); Software (equal); Writing – review & editing (equal). Nicola J Simkiss: Investigation (equal); Software (equal); Writing – review & editing (equal). Robert J Snowden: Conceptualization (equal); Data curation (equal); Methodology (equal); Supervision (equal); Validation (equal); Writing – review & editing (equal).
Conflicts of interest
All authors declare no conflict of interest.
Acknowledgements
The authors thank Joy Garfitt, Richard Jones, Philip Lewis, David Roberts, Alberto Salmoiraghi, and Ian Wile, who (along with Chris O’Connor) were the Principle Investigators within the seven Health Boards in Wales. Their help and support in disseminating this survey, both to staff within their Health Boards, and to the local populations they serve, was invaluable. Further, we are also very grateful to Jo Jordan, National Programme Director for Mental Health (NHS Wales), for assisting and supporting our endeavours with this research project. Thanks also to Chris Norman at the Portfolio Team at Health Care Research Wales for facilitation of research governance underpinning this mental health survey and for assisting our team in securing local agreements in a timely manner given the need for prompt action. We are also particularly grateful to Stuart Williams who provided web development, and marketing, support throughout our project. Additionally, the authors thank the following organizations and individuals who disseminated the survey: The Institute of Leadership and Management, the Chartered Institute of Personnel and Development, Dyfed Powys Police, Mid and West Wales Fire and Rescue Service, North Wales Fire and Rescue Service, Welsh Ambulance Service Trust, National Farmers’ Union of Cymru, Making Wales Better, Driver and Vehicle Licensing Agency (DVLA), React Support Services, Howell's School, Cancer Pal and the Talyllyn Railway. The authors also thank the many participants who completed the survey.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Barzilay, R. , Moore, T.M. , Greenberg, D.M. , DiDomenico, G.E. , Brown, L.A. , White, L.K. , … Gur, R.E. (2020). Resilience, COVID‐19‐related stress, anxiety and depression during the pandemic in a large population enriched for health care providers. Translational Psychiatry, 10, 291. 10.1038/s41398-020-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt, K.S. , Turkelson, A. , Fingerman, K.L. , Polenick, C.A. , & Oya, A. (2021). Age differences in stress, life changes, and social ties during the COVID‐19 pandemic: Implications for psychological well‐being. The Gerontologist, 61(2), 205–216. 10.1093/geront/gnaa204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno, G. (2005). Resilience in the face of potential trauma. Current Directions in Psychological Science, 14, 135–138. 10.1111/j.0963-7214.2005.00347.x [DOI] [Google Scholar]
- Brooks, S.K. , Dunn, R. , Amlôt, R. , Rubin, G.J. , & Greenberg, N. (2018). A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. Journal of Occupational and Environmental Medicine, 60(3), 248–257. 10.1097/JOM.0000000000001235 [DOI] [PubMed] [Google Scholar]
- Chmitorz, A. , Wenzel, M. , Stieglitz, R.‐D. , Kunzler, A. , Bagusat, C. , Helmreich, I. , … Tüscher, O. (2018). Population‐based validation of a German version of the Brief Resilience Scale. PLoS One, 13(2), e0192761. 10.1371/journal.pone.0192761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry, O.S. , Rowland, L.A. , Van Lissa, C.J. , Zlotowitz, S. , McAlaney, J. , & Whitehouse, H. (2018). Happy to help? A systematic review and meta‐analysis of the effects of performing acts of kindness on the well‐being of the actor. Journal of Experimental Social Psychology, 76, 320–329. 10.1016/j.jesp.2018.02.014 [DOI] [Google Scholar]
- DeWolfe, D.J. (2000). Training manual for mental health and human service workers in major disasters. Washington DC: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. Center for Mental Health Services. [Google Scholar]
- Donker, T. , Comijs, H. , Cuijpers, P. , Terluin, B. , Nolen, W. , Zitman, F. , & Penninx, B. (2010). The validity of the Dutch K10 and extended K10 screening scales for depressive and anxiety disorders. Psychiatry Research, 176, 45–50. 10.1016/j.psychres.2009.01.012 [DOI] [PubMed] [Google Scholar]
- Dunleavy, K. , Taylor, A. , Gow, J. , Cullen, B. , & Roy, K. (2012). Police officer anxiety after occupational blood and body fluid exposure. Occupational Medicine, 62, 382–384. 10.1093/occmed/kqs078 [DOI] [PubMed] [Google Scholar]
- Gray, N.S. , O'Connor, C. , Knowles, J. , Pink, J. , Simkiss, N.J. , Williams, S.D. , & Snowden, R.J. (2020). The influence of the COVID‐19 pandemic on mental well‐being and psychological distress: Impact upon a single country. Frontiers Psychiatry, 11, 1–11. 10.3389/fpsyt.2020.594115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, T. , Zhang, D. , & Wang, J. (2015). A meta‐analysis of the trait resilience and mental health. Personality and Individual Differences, 76, 18–27. 10.1016/j.paid.2014.11.039 [DOI] [Google Scholar]
- Jahnke, S.A. , Poston, W.S.C. , Jitnarin, N. , & Haddock, C.K. (2012). Health concerns of the U.S. fire service: Perspectives from the firehouse. American Journal of Health Promotion, 27(2), 111–118. 10.4278/ajhp.110311-QUAL-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavčič, T. , Avsec, A. , & Kocjan, G.Z. (2020). Psychological functioning of slovene adults during the covid‐19 pandemic: Does resilience Matter? Psychiatric Quarterly, 92(1), 207–216. 10.1007/s11126-020-09789-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R C , Andrews, G. , Colpe, L J , Hiripi, E. , Mroczek, D K , Normand, S.‐l T. , … Zaslavsky, A M (2002). Short screening scales to monitor population prevalences and trends in non‐specific psychological distress. Psychological Medicine, 32, 959–976. 10.1017/s0033291702006074 [DOI] [PubMed] [Google Scholar]
- Khadse, P.A. , Gowda, G.S. , Ganjekar, S. , Desai, G. , & Murthy, P. (2020). Mental health impact of COVID‐19 on police personnel in India. Indian Journal of Psychological Medicine, 42(6), 580–582. 10.1177/0253717620963345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , Marciano, H. , Eshel, Y. , & Adini, B. (2020). Resilience and demographic characteristics predicting distress during the COVID‐19 crisis. Social Science & Medicine, 265, 113389. 10.1016/j.socscimed.2020.113389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb, D. , Greenberg, N. , Stevelink, S.A. , & Wessely, S. (2020). Mixed signals about the mental health of the NHS workforce. The Lancet Psychiatry, 7, 109–1011. 10.1016/S2215-0366(20)30379-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, E.E. , Presskreischer, R. , Anderson, K.E. , Han, H. , & Barry, C.L. (2020). Psychological distress and COVID‐19–related stressors reported in a longitudinal cohort of US adults in April and July 2020. JAMA, 324, 2555. 10.1001/jama.2020.21231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, E.E. , Presskreischer, R. , Han, H. , & Barry, C.L. (2020). Psychological distress and loneliness reported by US Adults in 2018 and April. JAMA, 324(1), 93–94. 10.1001/jama.2020.9740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, L.H. , Drew, D.A. , Graham, M.S. , Joshi, A.D. , Guo, C.‐G. , Ma, W. , … Zhang, F. (2020). Risk of COVID‐19 among front‐line health‐care workers and the general community: A prospective cohort study. Lancet Public Health, 5, e475–e483. 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick, C. J. (2010). Triarchic psychopathy measure (TriPM). In PhenX (Ed.), Toolkit Online assessment catalog. https://www.phenxtoolkit.org/protocols/view/121601 [Google Scholar]
- Petrie, K. , Milligan‐Saville, J. , Gayed, A. , Deady, M. , Phelps, A. , Dell, L. , … Harvey, S.B. (2018). Prevalence of PTSD and common mental disorders amongst ambulance personnel: A systematic review and meta‐analysis. Social Psychiatry and Psychiatric Epidemiology, 53(9), 897–909. 10.1007/s00127-018-1539-5 [DOI] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. , … Abel, K.M. (2020). Mental health before and during the COVID‐19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry, 7, 883–893. 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti, E. , Di Mattei, V. , Perego, G. , Ferrari, F. , Mazzetti, M. , Taranto, P. , … Calati, R. (2020). The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Current Psychiatry Reports, 22, 1–22. 10.1007/s11920-020-01166-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson, I.T. , Cooper, C.L. , Sarkar, M. , & Curran, T. (2015). Resilience training in the workplace from 2003 to 2014: A systematic review. Journal of Occupational and Organizational Psychology, 88, 533–562. 10.1111/joop.12120 [DOI] [Google Scholar]
- Rodríguez‐Rey, R. , Alonso‐Tapia, J. , & Hernansaiz‐Garrido, H. (2016). Reliability and Validity of the Brief Resilience Scale (BRS) Spanish Version. Psychological Assessment, 28(5), e101–e110. 10.1037/pas0000191 [DOI] [PubMed] [Google Scholar]
- Roy, S. , Vize, C. , Uzieblo, K. , van Dongen, J.D.M. , Miller, J. , Lynam, D. , … Neumann, C.S. (2019). Triarchic or septarchic?—Uncovering the Triarchic Psychopathy Measure’s (TriPM) structure. Personality Disorders: Theory, Research, and Treatment, 12(1), 1–15. 10.1037/per0000392 [DOI] [PubMed] [Google Scholar]
- Sawhney, G. , Jennings, K.S. , Britt, T.W. , & Sliter, M.T. (2017). Occupational stress and mental health symptoms: Examining the moderating effect of work recovery strategies in firefighters. Journal of Occupational Health Psychology, 23(3), 443–456. 10.1037/ocp0000091 [DOI] [PubMed] [Google Scholar]
- Smith, B.W. , Dalen, J. , Wiggins, K. , Tooley, E. , Christopher, P. , & Bernard, J. (2008). The brief resilience scale: assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Statistics for Wales . (2019). Welsh Index of Muliple Deprivation (WIMD) 2019 Guidance. Retrieved from https://gov.wales/welsh‐index‐multiple‐deprivation‐index‐guidance#section‐32829 [Google Scholar]
- Stogner, J. , Miller, B.L. , & McLean, K. (2020). Police stress, mental health, and resiliency during the COVID‐19 pandemic. American Journal of Criminal Justice, 45, 718–730. 10.1007/s12103-020-09548-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- The King’s Fund . (2021). Covid‐19 recovery and resilience: what can health and care learn from other disasters?. Retrieved from https://features.kingsfund.org.uk/2021/02/covid‐19‐recovery‐resilience‐health‐care/ [Google Scholar]
- Townsend, E. , Nielsen, E. , Allister, R. , & Cassidy, S.A. (2020). Key ethical questions for research during the COVID‐19 pandemic. The Lancet Psychiatry, 7, 381–383. 10.1016/S2215-0366(20)30150-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UK Government . (2020). Critical workers who can access schools or educational settings. London, UK: UK Government. Retrieved from https://www.gov.uk/government/publications/coronavirus‐covid‐19‐maintaining‐educational‐provision/guidance‐for‐schools‐colleges‐and‐local‐authorities‐on‐maintaining‐educational‐provision [Google Scholar]
- van Dongen, J.D. , Drislane, L.E. , Nijman, H. , Soe‐Agnie, S.E. , & van Marle, H.J. (2017). Further evidence for reliability and validity of the triarchic psychopathy measure in a forensic sample and a community sample. Journal of Psychopathology and Behavioral Assessment, 39(1), 58–66. 10.1007/s10862-016-9567-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele, T.J. (2020). Activities for flourishing: An evidence‐based guide. Journal of Positive School Psychology, 4(1), 79–91. Retrieved from https://www.journalppw.com/index.php/JPPW/article/view/163 [Google Scholar]
- Vissoci, J.R.N. , Vaca, S.D. , El‐Gabri, D. , de Oliveira, L.P. , Mvungi, M. , Mmbaga, B.T. , … Staton, C. (2018). Cross‐cultural adaptation and psychometric properties of the Kessler Scale of psychological distress to a traumatic brain injury population in Swahili and the Tanzanian Setting. Health and Quality of Life Outcomes, 16(147), 10.1186/s12955-018-0973-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C.S. , & Ho, R.C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17, 1229. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiden, M.D. , Zeig‐Owens, R. , Singh, A. , Schwartz, T. , Liu, Y. , Vaeth, B. , … Prezant, D.J. (2020). Pre‐COVID‐19 lung function and other risk factors for severe COVID‐19 in first responders. ERJ Open Research, 7(1), 10.1183/23120541.00610-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, J.M. , Lee, J. , Fitzgerald, H.N. , Oosterhoff, B. , Sevi, B. , & Shook, N.J. (2020). Job insecurity and financial concern during the COVID‐19 pandemic are associated with worse mental health. Journal of Occupational and Environmental Medicine, 62, 686–691. 10.1097/JOM.0000000000001962 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


