Abstract
Aim
To understand the impact of professional stressors on nurses' and other health care providers' professional quality of life and moral distress as they cared for patients during the COVID‐19 pandemic.
Background
Health care providers caring for patients during the COVID‐19 pandemic are at increased risk of decreased professional quality of life and increased moral distress.
Methods
A convergent mixed‐methods design and snowball sampling was used to collect survey data (n = 171) and semi‐structured interviews (n = 23) among health care providers working in the inpatient setting.
Results
Perceived lack of support from executive leadership, access to personal protective equipment and constantly changing guidelines led to decreased professional quality of life and increased moral distress among health care providers.
Conclusion
Findings from this study indicate that shared governance, disaster management training and enhanced communication may assist executive leadership to reduce the likelihood of decreased professional quality of life and increased moral distress in front line health care providers.
Implications for Nursing Management
Following the principles of shared governance may assist executive leadership to promote and acknowledge the significance of the role of health care providers at the bedside. Additionally, disaster management training and open communication are crucial to ensure that health care providers are adequately informed and supported at the bedside.
Keywords: health care providers, leadership, moral distress, nurses, professional quality of life
1. INTRODUCTION
The coronavirus disease (COVID‐19) pandemic has led to unexpected ethical and logistical challenges, creating significant disruptions in the provision of health care in the United States (U.S.) and worldwide (Dudzinski et al., 2021; Fernandez et al., 2020; Lam et al., 2020; Li et al., 2021). Even as countries around the globe begin to distribute and administer a vaccine for COVID‐19, new cases continue to emerge, placing increased strain on hospitals, nurses and other health care providers (HCPs; Ulrich et al., 2020). The COVID‐19 pandemic has led to social distancing policies and shortages of personal protective equipment (PPE), potentially leading to increased demand on front line HCPs as hospitals work to provide safe, urgent care to patients in need (Sheehan et al., 2020). As the volume of patients infected with COVID‐19 has increased and the need to mitigate the virus has become paramount, health care leaders have shifted from a shared governance model to a command‐and‐control hierarchy (Rosser et al., 2020). This command‐and‐control hierarchy, in response to enhanced prevention and control policies set forth by various state and federal agencies, has led to decreased patient autonomy and self‐determination as well as increased HCP psychosocial distress (de Campos & Daniels, 2021; Jeffrey, 2020).
The COVID‐19 pandemic has created surges in health care demand that require HCPs to prioritize the health and safety of the community rather than that of individual patients (Berlinger et al., 2020). This shift from patient‐centred practice to public focused care, coupled with necessary changes in leadership style, may lead to decreased professional quality of life (QOL) and moral distress in HCPs who are acclimating to a new work environment (Lam et al., 2018; de Campos & Daniels, 2021; Rosser et al., 2020). Although HCPs typically receive some education and training in disaster management, there is little to no training about applying public health approaches in the acute care or outpatient setting (Lam et al., 2018).
Rapidly changing or unclear treatment guidelines, lack of access to PPE and repeated exposure to trauma typical in a public health emergency may decrease HCP compassion satisfaction and increase compassion fatigue and burnout (Buselli et al., 2020; Liu et al., 2020; Pappa et al., 2020; Stamm, 2010). In addition to decreased professional QOL, HCPs caring for patients during the COVID‐19 pandemic may experience moral distress when they are unable to maintain standards of care for their patients due to fear of contracting and spreading the virus and ethical concerns about the provision of care (Daubman et al., 2020; Morley et al., 2020; Sun et al., 2020; Xiang et al., 2020). Unclear role expectations and lack of communication from leadership may lead to decreased professional QOL and increased moral distress for HCPs as they attempt to uphold their standards of care in a pandemic environment (Epstein et al., 2019; Jeffrey, 2020).
Decreased professional QOL and increased moral distress may lead HCPs away from the bedside at a time when their experience is needed the most. Existing literature about COVID‐19 focuses on diagnosis and treatment among patients; however, there is lack of research regarding changing standards of care as well as the influence of leadership during the COVID‐19 pandemic on HCP's professional QOL and moral distress. Thus, the aim of this study is to understand the impact of professional stressors on HCPs professional QOL and moral distress as they cared for patients during the COVID‐19 pandemic.
2. METHODS
A convergent mixed‐methods design (see Figure 1) was conducted to concurrently collect both qualitative and quantitative data (Creswell & Poth, 2018). A mixed‐methods design served to yield a better understanding of how professional stressors influence personal and professional QOL as well as moral distress in HCPs caring for patients during the COVID‐19 pandemic (Creswell & Poth, 2018). Qualitative and quantitative data were analysed independently, with results interpreted together. This study was approved by the University of Delaware Institutional Review Board, and informed consent was obtained from all participants.
FIGURE 1.
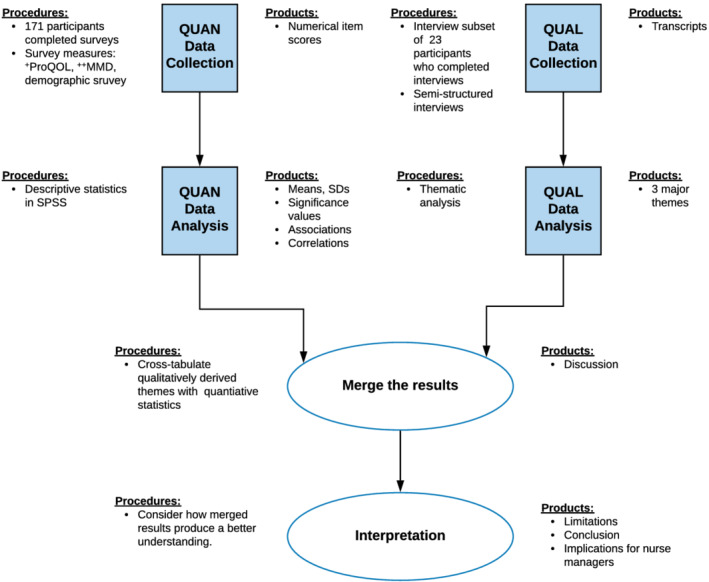
Convergent parallel analysis of quantitative and qualitative data. +ProQOL = Professional Quality of Life; ++MMD‐HP = Measure of Moral Distress
2.1. Sample size and recruitment
Participants were recruited to complete an online survey via convenience and snowball sampling and an information systems‐supported recruiting process (e‐recruiting). Due to restrictions in place during COVID‐19, this study was conducted virtually via Research Electronic Data Capture (REDCap) and Zoom. Researchers shared Institutional Review Board (IRB)‐approved recruitment materials on social media platforms (including Facebook and Twitter) and with contacts at hospitals nationwide. Eligible participants met the following inclusion criteria: (1) HCPs caring for patients in the inpatient or outpatient setting during the coronavirus pandemic, (2) able to read and write English and (3) have internet access. Interested HCPs meeting the eligibility criteria completed an electronic informed consent via REDCap (Harris et al., 2009). Of the 182 consented participants, 171 completed the online surveys.
To gain a deeper understanding of HCPs experiences while caring for patients during the COVID‐19 pandemic, interested participants were recruited to participate in a Zoom interview. In addition to the above inclusion criteria, potential interview participants were required to provide direct, hands‐on care to patients presumed to be positive or diagnosed with COVID‐19 for at least 50% of their workday and able to hear. Participants who met the interview eligibility requirements completed an additional electronic informed consent.
2.2. Data collection
Study enrolment and quantitative data collection took place as the initial surge of COVID‐19 cases was just beginning in the United States, between May 2020 and June 2020. A REDCap database was used to screen potential participants for eligibility, obtain electronic informed consent, collect demographic data and provide links to the electronic survey. Participants completed the quantitative database that consisted of a demographic and COVID‐19 practice survey, Professional Quality of Life Scale (ProQOL; Stamm, 2010) and Measure of Moral Distress‐Healthcare Professionals (MMD‐HP; Epstein et al., 2019) taking approximately 25–30 min to complete. The COVID‐19 practice survey included questions related to professional role, practice setting, hospital size, self‐isolation practices and PPE availability and usage.
Semi‐structured interviews were conducted in July 2020 using an interview guide with open‐ended questions (Table 1) and lasted approximately 60 min. Interviews were conducted in a private office by the first author (M.N.) via Zoom. Participants were able to speak freely beyond the interview questions, and data collection ceased after data saturation was reached.
TABLE 1.
Semi‐structured interview questions
| 1. How has daily life changed for you since the start of the pandemic? |
| 2. How would you describe your current state of health? |
| 3. How is your family doing right now? |
| 4. What was your job normally like before COVID‐19? |
| 5. Walk me through how you felt when you heard you would be caring for COVID + patients. |
| 6. How do you typically cope and handle stress? |
| 7. How have you been coping with stress related to caring for COVID + patients (i.e., dealing with traumatic events, risk of contamination, operating in draining environments and people's attitudes towards you when returning home)? Please give examples. |
| 8. Tell me about any concerns for your personal safety. |
| 9. What was your experience with PPE? |
| 10. Tell me about the type of support that is/was available to you at your worksite. |
| 11. What information, education or training did you and your health care colleagues receive prior to working with COVID‐19 patients? |
| 12. How have changes in policies and procedures related to COVID‐19 influenced your ability to provide patient care? |
| 13. How has the COVID‐19 pandemic influenced changes or improvements to the delivery of patient care at your hospital? |
| 14. How has your organisation made things easier for you during this time? |
| 15. How has COVID‐19 influenced your relationship with your patients? |
| 16. Has your experience caring for COVID‐19 patients led you to consider leaving nursing? |
| 17. How has the media coverage surrounding the pandemic influenced you? |
| 18. How has caring for COVID‐19 patients influenced your home life? |
| 19. What has been the most challenging thing about this time? |
| 20. What do you think it will be like as states/businesses start to resume pre‐COVID activities? |
| 21. What positive things have or will come out of this pandemic? |
Abbreviation: PPE, personal protective equipment.
2.2.1. Quantitative data: Instruments
The ProQOL was used to measure professional QOL in HCPs. This 30‐item self‐report instrument measures compassion fatigue (CF), a combined measure of burnout and secondary trauma, and compassion satisfaction (Stamm, 2010). The instrument is a 5‐point Likert scale ranging from 1 to 5 (never to very often) with subscale score ranges from 10 to 50 (Stamm, 2010). This scale is widely used to measure the negative and positive effects of helping others who experience suffering and trauma and has been used by researchers around the world (Ahmad et al., 2015; Berger et al., 2015; Dang et al., 2015). The ProQOL has been tested extensively with Cronbach's alpha of .88 for compassion satisfaction, .75 for burnout and .81 for secondary traumatic stress (Alkema et al., 2008; Amin et al., 2015; Beaumont et al., 2016).
The MMD‐HP was used to measure moral distress in HCPs. The MMD‐HP is a 27‐item self‐report instrument designed to measure the current level of moral distress as a function of how frequent a situation occurs and how distressing it is in clinical practice (Epstein et al., 2019). The instrument has a 5‐point scale ranging from 0–4 for frequency (never to very frequently) and level of distress (none to very distressing) with a total score ranging from 0 to 432 (Epstein et al., 2019). The MMD‐HP has been widely used to measure the most currently understood causes of moral distress and has been used in a variety of settings around the world (Astbury et al., 2017; Burston et al., 2017; Fujii et al., 2021). The MMD‐HP is a reliable instrument with Cronbach's alphas ranging from .77 to .95, depending on the sampled professional group (Hamric & Blackhall, 2007; Sauerland et al., 2014; Whitehead et al., 2015).
2.2.2. Qualitative data: Interviews
The primary author (M.N.) conducted the interviews using semi‐structured, open‐ended questions that were vetted by HCPs caring for patients presumed positive or diagnosed with COVID‐19 during the pandemic (see Table 1). Interviews were conducted in a private office and recorded via Zoom video conferencing technology. In order to foster a deeper exploration of the participant's experience, the interviewer used two or three probes per question to ensure understanding. Interviews continued until saturation was reached and were transcribed verbatim using an automatic transcription service and verified by two authors (M.N. & J.S.).
2.3. Data analysis
Using a convergent parallel design (see Figure 1), researchers concurrently collected quantitative and qualitative data independent of each other. Data were analysed separately using the analytic procedures described below. Data interpretation included evaluating results of both data sets for convergence or divergence from each other yielding a better understanding of the study's overall purpose.
Quantitative data analyses were conducted using SPSS Version 26. Data were cleaned with response sample scores divided into three categories by creating new variables for the 25th, 50th, and 75th percentile cut‐points for each subscale (CS, STS and BO) of the ProQOL (Stamm, 2010) and MMD‐HP (Hamric & Blackhall, 2007) indicating low, average and high levels. Descriptive statistics was used to describe the participants' demographic personal and workplace characteristics, professional QOL and moral distress. Using a significance level of .05, non‐parametric statistics (Mann–Whitney U and Kendall's Tau‐b) were used to examine the associations between nominal and ordinal variables of the ProQOL three subscales and MMD‐HP. Each scale of the ProQOL and the total composite scores of the MMD‐HP were normally distributed, and associations were analysed using Pearson's r.
The qualitative data were analysed using a thematic approach to identify emergent ideas prior to beginning the coding process (Creswell & Poth, 2018). The researchers simultaneously analysed and collected data allowing the processes to influence each other (Sandelowski, 2000). Interviews were independently reviewed by the first and second author (M.N. and J.S.) to identify emergent concepts in order to establish initial categories as well as to create a digital audit trail that served as the foundation of the validation strategy (Creswell & Poth, 2018). Once the initial interpretation of the data was complete (M.N. and J.S.), an inductive coding system was applied to identify themes that emerged in the data (Creswell & Poth, 2018). To achieve consensus, researchers resolved disagreements by iteratively recoding, rereading and reanalysing transcripts (Creswell & Poth, 2018). Final themes were evaluated to ensure that interpretations and findings were clearly derived from the data (Lincoln & Guba, 1985). The consolidated criteria for reporting research (COREQ) checklist was used to ensure quality reporting in the study (Tong et al., 2007).
3. RESULTS
3.1. Participant characteristics
Demographic, COVID‐19 practice‐related information, ProQOL and MMD‐HP data were collected from 171 HCPs from across the U.S. caring for patients during the COVID‐19 pandemic from May 2020–June 2020 (Table 2). The majority of the participants were female (92%, n = 157), married (77%, n = 131), bedside nurses (71%, n = 118), who were employed in an acute care facility (78%, n = 133). Participants averaged 11–20 years in practice (25%, n = 43), working 25–48 h a week (73%, n = 115) and 69% (n = 118) were nurses (Table 2). Most participants had obtained a bachelor's degree (44%, n = 75) or beyond (32%, n = 55). In our sample, 18% of HCPs were required to move from one practice area to another (e.g., cardiac intensive care unit to COVID‐19 unit). Additionally, 22% of HCPs considered leaving their current position due to moral distress.
TABLE 2.
Socio‐demographic and workplace characteristics of participating health care providers who cared for patients during the COVID‐19 pandemic (n = 171)
| Sample characteristic | N (%) |
|---|---|
| Age | |
| 18–25 | 11 (6.4%) |
| 26–30 | 29 (17%) |
| 31–40 | 61 (36%) |
| 41–50 | 46 (27%) |
| 51–60 | 19 (11%) |
| 61–70 | 5 (3%) |
| Children | |
| None | 76 (44%) |
| One | 29 (17%) |
| Two | 35 (21%) |
| Three or more | 31 (18%) |
| Regions of the United States | |
| Northeast | 37 (28%) |
| South | 78 (46%) |
| Midwest | 28 (16%) |
| West | 28 (16%) |
| Professional role | |
| Bedside nurse | 118 (71%) |
| Other nursing role | 17 (9%) |
| Patient care/laboratory/imaging technician | 8 (5%) |
| Physical therapy/occupational therapist | 10 (6%) |
| Physician | 3 (3%) |
| Other | 10 (6%) |
| Place of employment | |
| Hospital: less than 100 beds | 11 (8%) |
| Hospital: 101–499 beds | 70 (53%) |
| Hospital: more than 500 beds | 52 (39%) |
| Years in practice | |
| Less than 2 years | 26 (15%) |
| 3–5 years | 28 (16%) |
| 6–10 years | 39 (23%) |
| 11–20 years | 43 (25%) |
| 21+ years | 30 (18%) |
Note: Items may not add up to 171 as participants may have chosen not to answer specific questions.
3.2. Quantitative
3.2.1. Professional Quality of Life
Among the 171 participants, 150 (88%) completed the ProQOL scale (see Table 3).
TABLE 3.
Moral Distress‐Healthcare Professional and Professional Quality of Life of participating health care providers who cared for patients during the COVID‐19 pandemic (n = 171)
| Measurement | Mean (SD) | Range |
|---|---|---|
| Measure of Moral Distress‐Healthcare Professionals | 119.96 + 73.03 |
(0–432) |
| Professional Quality of Life subscales | ||
| Compassion satisfaction | 28.17 + 6.8 | (7–50) |
| Burnout | 24.89 + 6.03 | (3–38) |
| Secondary traumatic stress | 15.49 + 6.84 | (11–43) |
Perception of support from administrators was significantly associated with all three ProQOL scales. If participants felt supported by executive leadership, compassion satisfaction increased (r = .448, p. = 001), whereas burnout (r = −.464, p = .001) and secondary traumatic stress decreased (r = −.309, p = .001). The mean rank of compassion satisfaction (U = 1742.0, p = .018) and burnout (U = 2830.50, p = .012) were significantly lower in HCPs who worked at the bedside prior to COVID‐19 (70.63 and 62.11, respectively) than those who did not work at the bedside prior to COVID‐19 (88.02 and 80.71, respectively) (see Table 4). Mean rank of compassion satisfaction was significantly higher in HCPs who changed their practice setting (91.42) than those who did not change practice setting (72.32), U = 1960.5, p = .031(see Table 4). Conversely, the mean rank of burnout was significantly lower in HCPs who changed their practice setting (58.90) than those who did not change practice setting (78.82), U = 1147.5, p = .025 (see Table 5). Mean rank of secondary traumatic stress was significantly higher in HCPs who worked overtime (82.87) than those who did not work overtime (66.61), U = 3393.5, p = .015 (see Table 4).
TABLE 4.
Significant associations between independent variables and Professional Quality of Life subscales and the Measure of Moral Distress among health care providers caring for patients during the COVID‐19 pandemic
| Mean rank | U value | p value | |
|---|---|---|---|
| Professional quality of life: Compassion satisfaction | |||
| Did you work as a bedside nurse before and during COVID‐19? | 1742.0 | .018* | |
| Yes group (n = 108) | 70.63 | ||
| No group (n = 42) | 88.02 | ||
| During COVID‐19, did your practice area change? | 1960.5 | .031* | |
| Yes group (n = 25) | 91.42 | ||
| No group (n = 125) | 72.32 | ||
| During COVID‐19, did you have new PPE each shift? | 3649.0 | .001** | |
| Yes group (n = 85) | 85.93 | ||
| No group (n = 68) | 61.86 | ||
| Professional quality of life: burnout | |||
| Did you work as a bedside nurse before and during COVID‐19? | 2830.5 | .012* | |
| Yes group (n = 108) | 62.11 | ||
| No group (n = 42) | 80.71 | ||
| During COVID‐19, did your practice area change? | 1147.5 | .025* | |
| Yes group (n = 25) | 58.90 | ||
| No group (n = 125) | 78.82 | ||
| During COVID‐19, did you have new PPE each shift? | 1855.0 | .001** | |
| Yes group (N = 85) | 64.82 | ||
| No group (N = 68) | 89.46 | ||
| Professional Quality of Life: Secondary traumatic stress | |||
| During COVID‐19, did you work overtime? | 3393.5 | .015* | |
| Yes group (N = 82) | 82.87 | ||
| No group (N = 68) | 66.61 | ||
| During COVID‐19, did you have new PPE each shift? | 2246.5 | .037* | |
| Yes group (N = 85) | 69.43 | ||
| No group (N = 65) | 83.44 | ||
| Measure of Moral Distress‐Healthcare Provider | |||
| During COVID‐19, did you work in an acute care setting? | 1477.0 | .003* | |
| Yes group (N = 94) | 63.21 | ||
| No group (N = 23) | 41.78 | ||
| During COVID‐19, did you have new PPE each shift? | 1309.0 | .018* | |
| Yes group (N = 62) | 52.61 | ||
| No group (N = 55) | 66.20 | ||
Note: Mann–Whitney U was statistical analyses.
Abbreviation: PPE, personal protective equipment.
p ≤ .05.
p ≤ .001.
TABLE 5.
Correlations between MMD‐HP and ProQOL subscales among health care providers caring for patients during the pandemic (n = 117)
| Variable | MMD‐HP | Compassion satisfaction | Burnout | Secondary traumatic stress |
|---|---|---|---|---|
| MMD‐HP | 1 | −.462** | .557** | .334** |
| Compassion satisfaction a | −.462** | 1 | −.493** | −.289** |
| Burnout a | .557** | −.493** | 1 | .632** |
| Secondary traumatic stress a | .334** | −.289** | .632** | 1 |
Abbreviation: MMD‐HP, Measure of Moral Distress; ProQOL, Professional Quality of Life.
ProQOL Scale.
Correlation is significant at the .01 level (two‐tailed).
The mean rank of compassion satisfaction (U = 3649.0, p = .001), burnout (U = 1855.0, p = .001) and secondary traumatic stress (U = 2246.5, p = .037) was significant between those with and without access to new PPE every shift (see Table 4). For HCPs with access to new PPE every shift, compassion satisfaction was significantly higher (85.93), and burnout (64.82) and secondary traumatic stress (69.43) were significantly lower compared with those without access to new PPE 61.86, 89.46, and 83.44, respectively (see Table 4). No relationship was found between the subscales of the ProQOL and years in number of children, region of the United States, education, relationship status and size of practice measured by number of beds. Of the ProQOL subscales, significant correlations were found at a p value of .001. Secondary traumatic stress was positively correlated with burnout (r = .632), and there was a negative correlation between burnout and compassion satisfaction (r = −.493) (see Table 5).
3.2.2. Measure of Moral Distress‐Healthcare Professionals
Among the participants, 68% (n = 117) completed the MMD‐HP with a mean score of 119.96 ± 73.03 (Table 3). In scoring the MMD‐HP, those with a score ≥168.4 are at increased risk of choosing to leave their current health care position due to moral distress (Epstein et al., 2019). Twenty five percent of our sample met this criteria. Mean rank of moral distress was significantly higher among HCP working in an acute care setting (63.21) compared with those not in an acute care setting (41.78), U = 1477.0, p = .003 (see Table 4). Mean rank of moral distress was significantly lower among HCP who had access to new PPE each shift (52.61) compared with HCP without access to new PPE each shift (66.20), U = 1309.0, p = .018. There was an inverse relationship between organisational support and moral distress (−.420, p = .001). There was a significant relationship between each ProQOL subscale and the MMD‐HP, yet no strong correlations greater than r ≥ .7 for any subscale (see Table 5). There are, however, statistically significant correlations at the p value of .001. There was a positive relationship between MMD‐HP and burnout (r = .557) and an inverse relationship between MMD‐HP and compassion satisfaction (r = −.462 (see Table 5).
3.3. Qualitative
Semi‐structured interviews were conducted with 23 participants in July 2020. Most HCPs were nurses (78%; n = 18) and had been in practice less than 10 years (61%; n = 14). The majority of HCPs had obtained a bachelor's degree (39%; n = 9) or beyond (30%; n = 7).
A thematic analysis of the qualitative data for the 23 interviewed HCPs resulted in three major themes highlighting the factors influencing professional QOL and moral distress as experienced by HCPs caring for patients during the COVID‐19 pandemic. Themes were as follows: (1) balancing fear and moral obligation; (2) coping with leadership challenges and system breakdowns; and (3) focusing on teamwork and building resilience.
3.3.1. Theme 1: Balancing fear and moral obligation
Balancing their own personal distress while maintaining their commitment to their profession and their patients was a struggle for HCPs. M.D., a respiratory therapist, said, ‘there is going to be a whole generation of healthcare workers that are going to be deeply scarred for the rest of their lives.’ Despite concerns about personal health issues and/or fears of contracting the virus, HCPs placed increased pressure on themselves to come to work and care for patients. F. Y., a nurse, wondered,
Am I going to get it? How am I going to be sure that I am focused? Did I don and doff properly? Did I treat someone without enough PPE? And what if I get it wrong and bring it home to my family?
Although their own personal safety was a concern, HCPs indicated that they felt obligated to report to work to support their team. H.B., a nurse, said, ‘[she] kept working because that's what I signed up for.’ G.R., a patient care technician, felt ‘called’ to travel to New York City at the height of the pandemic to help, stating ‘I saw it as a privileged time to be either like an EMT or paramedic or someone that works in emergency because here's an actual emergency and you get to be part of it, you know?’ L.G., a nurse, reported that her mother passed away from COVID‐19 and said,
On Saturday she died … I went back in on Sunday morning. It's busy. All the things I would normally do to give myself comfort on losing a mom I cannot do. So I went to work and people were like, why are you here? I'm like, what are my choices? … And staying busy was not a bad thing that day.
Navigating patient and family concerns in the setting of conflicting media coverage was particularly challenging, related to the sense that trust in HCPs was often undermined by reports stating that the virus is a ‘hoax’ and that ‘it will disappear on election day.’ S.H., a nurse, stated, ‘it's frustrating for me to encounter patients who are influenced more by the media than by what their doctors and nurses are telling them.’
3.3.2. Theme 2: Working in the midst of leadership challenges and system breakdowns
The realities of caring for patients during a pandemic left many HCPs feeling unprepared. H.F., a nurse, stated, ‘I just remember looking around and being like, Oh my God, like, what is this? And from there on out, it just kind of got worse.’ T.D., a nurse, indicated that executive leadership seemed disconnected from front line caregivers, stating, ‘[They] aren't doing the work. So why [were they] making changes [in patient care protocols] without discussing it with staff?’ In contrast, participants reported receiving a lot of support from their front line/unit managers on a more consistent basis. F.P., a nurse, stated that her direct supervisor had ‘been going full throttle to make sure we have enough PPE … because all of the PPE is locked up in the administration office.’
Frequently changing information made providers feel less secure in their relationship with the hospital. G. P, a nurse, stated, ‘Frustration … what do they want? Like, can we just get one concise answer? What do you want us to do? Because no one knows and we don't know how vital these changes are.’ Constant use of PPE and changes in how it was allocated increased patient care burden and personal distress. This left providers feeling unprotected in roles in which executive leaders were not routinely practicing. D.W., a physician, said,
I really did not like non‐clinical upper management coming down and trying to tell us, Oh, you should not be wearing all that. You're scaring the patient. Well then why do not you go in there? Care for the patient yourself without any PPE. But wait, you do not want to do that.
Several participants reported that the depiction of HCPs as ‘heroes’ was particularly distressing to those working at the bedside during the pandemic and compounded feelings of distress. G.F., a nurse, said ‘the whole hero thing feels disingenuous. I don't like it. It seems like self‐aggrandizing too, to wear a shirt that says ‘healthcare hero’ on it.’ Nurses indicated that they felt they were being regarded as heroes as a way to improve public relations for the hospital yet were not being supported by executive leadership. H.J., a nurse, said,
They're taking away our staff the whole time telling us ‘you are heroes’ but we are not going to actually support you in any real or meaningful way … When really what I want is for you to give me more PPE and more staff like that would be beneficial to me.
3.3.3. Theme 3: Focusing on teamwork and building resilience
The majority of HCPs reported experiencing improved inter‐ and intradisciplinary collaboration, and some felt a newfound sense of respect for other members of the care team. T.D., a respiratory technician, stated, ‘I will say with nursing‐physician relationships … it [working side‐by‐side during the pandemic] solidified our bond. I mean, we already had very good working relationships with the departments because we [respiratory therapists] were the link [in patient care].’ Participants reported feeling more included among their team and felt that communication about patients and potential treatment plans was improved. T.F., a nurse, said, ‘it's nice to encounter the humanizing aspect of this pandemic … instead of just a coworker or, you know, another healthcare worker, you see another side of that person.’ Nurses in particular spoke of the increased teamwork. N.G., a nurse, stated,
It's been amazing like the docs and the nurses and like all of the ancillary, you know, all the therapies, we have all kind of pulled together. Right? Cause this is a little, this has been a battle we have kind of been in together just trying to figure it out … I feel like we are a better team than we were before COVID started.
Nurses were intermediaries for physicians, patient care technicians and other ancillary personnel who were instructed or opted to stay out of patient rooms, leaving nurses to accommodate their roles while comforting patients who were scared and upset by this lack of contact. S.H., a nurse, stated,
They told us ‘we want you to minimize the number of times you go into a patient's room and the number of people that go into that patient's room’. So for our techs who usually go in and do their blood sugars, their vital signs and, turn the patients, they are not doing that.
In order to ensure that patients received the care they needed and that colleagues remained safe, HCPs reported taking on new roles or expanding their usual job duties. T.D., a respiratory therapist, said,
Initially everybody was told that you might have to adjust and take on different roles. I had to learn to operate x‐ray machines at one point. Either putting the plates behind the patient and prop them up against the window, into the X rays through the window, or x‐ray tech would roll the machine and tell us what buttons to push, how to position the plates, and shoot the x‐ray.
4. DISCUSSION
Constantly evolving information, changes in the delivery of care and inconsistent support from executive leaders influenced HCP professional QOL and moral distress during the COVID‐19 pandemic. Nurses and other HCPs indicated that while immediate supervisors and managers actively assisted in patient care and worked to keep them informed, executive leadership was consistently ‘out of touch’ with the realities of bedside care leading to decreased professional QOL and increased moral distress. This belief was likely enhanced due to necessary shifts from patient‐centred to community‐centred care during this wide‐scale public health crisis, which left HCPs feeling uninformed and unprepared to care for patients (Morley et al., 2020). Communication challenges and a perceived lack of control in decision‐making led to increased levels of frustration among HCPs at the bedside. Given the conversion from a shared decision making model to a command and control hierarchy, this is not entirely unexpected as moral distress occurs when HCPs do not feel ‘heard’ by leadership (Epstein et al., 2019; Morley et al., 2020).
A sense of obligation to report to work in order to care for patients and support their coworkers led HCPs in relationships to experience increased levels of distress related to balancing concerns about contracting and spreading COVID‐19 to family and friends. Competing priorities such as those described align with research that describes increased moral distress and decreased professional QOL among HCPs as they care for patients during pandemics (Daubman et al., 2020; Liu et al., 2020). Those who reported working longer hours and/or overtime experienced increased secondary traumatic stress likely related to increased exposure to the virus and separation from loved ones. Access to clean PPE each shift was associated with increased compassion satisfaction as well as decreased burnout, secondary traumatic stress and moral distress. Frequent donning and doffing of PPE negatively impacted HCPs ability to care for and connect with their patients. This is consistent with research conducted by Morley and colleagues (Morley et al., 2020), which found that the availability and use of PPE influenced moral distress, indicating that frontline HCPs should drive the allocation and use of resources, including PPE. Executive leadership can promote autonomy and respect for HCPs on the frontlines by relying on the principles of shared governance, ensuring that HCPs at all levels have the opportunity to have a voice in decision‐making processes (McDowell et al., 2010).
Despite preparation for mass casualty incidents using drills and simulations, HCPs reported feeling unprepared for the realities of patient care during this pandemic. While HCPs were driven by the sense that they were ‘all in this together,’ many were required to assume duties outside their regular area of practice in order to support each other in the clinical setting. In an attempt to meet the needs of many patients at one time, many intensive care and step‐down units were converted to ‘COVID units’ in order to provide specialized care for those diagnosed with the virus. While HCPs who experienced a change in practice area indicated that they received no specific training when they moved to a new unit after the start of the COVID‐19 pandemic, they did report increased levels of compassion satisfaction and decreased burnout. This may be due to change in leadership and staffing dynamics in the new unit or enhanced sense of job satisfaction related to caring specifically for COVID‐19 patients.
Additionally, conflicting data and media coverage of the developing pandemic negatively impacted providers as they increasingly felt that the public, as well as their patients, no longer viewed them as a credible source of health care information. Nursing has been consistently ranked as the most honest and ethical profession for nearly 20 years (Gallup Organization, 2019), and these new findings raise concerns about how HCPs might be perceived in similar situations in the future. Those employed in acute care settings experienced increased moral distress compared with colleagues in other settings likely related to constantly changing information about patient management and the acuity of patients with COVID‐19 in the acute care settings. Participants in this study indicated that they received limited mental health support during the COVID‐19 pandemic. This supports previous research conducted by Liu et al. (2020), suggesting that hospital leadership can reduce anxiety by providing adequate psychological support and counselling services to HCPs working at the bedside during large scale public health crises. Previous research indicates that decreased professional QOL and increased moral distress may lead experienced HCPs away from the bedside during the pandemic when their expertise is most needed; therefore, it is imperative that managers partner with executive leaders to identify and respond to concerns about QOL and moral distress among frontline providers expediently (Morley et al., 2020; Pavlish et al., 2016).
4.1. Limitations
Despite our attempt to enrol a multidisciplinary sample of HCPs, our participants were primarily nurses. Therefore, additional research is recommended to fully explore the experience of other HCPs. As the COVID‐19 pandemic continues to evolve, availability of information and resources has changed. Data were collected early in the pandemic, prior to the availability of a vaccine, when most U.S. states were experiencing their first cases of COVID‐19 and abiding by government‐mandated shutdowns and social distancing.
5. CONCLUSION
The U.S. health care system and HCPs have been significantly challenged by the unprecedented nature of the COVID‐19 pandemic. This study used a mixed‐methods approach to explore the influence of professional experiences on HCPs as they cared for patients during the COVID‐19 pandemic on their professional QOL and moral distress. Findings from this study indicate that HCPs reported feeling unprepared for the realities of caregiving during the pandemic. Lack of perceived support from executive leadership and concerns about the availability of clean PPE each shift negatively influenced professional QOL and moral distress. Decreased professional QOL and increased moral distress were also associated with HCPs who were married or cohabitating. Additionally, working overtime/longer hours or moving from a familiar practice setting to a COVID‐19 unit was also associated with decreased professional QOL and increased moral distress. As the pandemic continues to evolve, executive leaders should consider how lessons learned from shared governance can be applied in order to establish consistent support systems for HCPs on the front lines that reduce the likelihood of moral distress.
5.1. Implications for nursing leadership
Concerns about limited PPE, practicing in unfamiliar practice areas without advanced preparation or training and feeling like they were not being ‘heard’ by leadership negatively influenced QOL and moral distress among HCPs who cared for patients during the pandemic. The need to prioritize the health and safety of the community rather than that of individual patients left HCPs feeling unprepared for the ‘realities’ of caring for patients during a pandemic. Executive leadership should rely on lessons learned from shared governance to ensure that frontline HCPs have a voice in workflow decisions as well as the allocation of materials during large‐scale public health crises. Clear lines of communication regarding the availability of PPE and how it might be distributed as well as additional training for HCPs who may be required to move to a different care setting should be provided. Disaster training clarifying the role of team members, including executive leadership, should be provided to all staff in all practice settings. Additional education will ensure that team members understand their role, as well as the role of leadership, in the prevention and mitigation of public health disasters.
Fear of contracting and transmitting COVID‐19 and separation from loved ones negatively impacted HCPs. Executive leaders must also work to support unit‐based leadership as they endeavour to support those working on the frontlines. Partnership between nurse managers and executive leaders is key in devising recognizable support for frontline HCPs and their QOL and moral distress. Executive leadership can take a proactive role in understanding the drivers of professional QOL and moral distress and looking for signs of distress among staff. Approaching lessons learned from this pandemic using continuous quality improvement strategies may help leaders who have limited experience in supporting staff during pandemics and/or identifying moral distress among their team.
AUTHOR CONTRIBUTIONS
M.N. and J.S. co‐designed the study, collected and analysed the data and wrote/reviewed/edited the manuscript. L.D. co‐designed the study, drafted the conclusion section and reviewed/edited the manuscript. K.E. analysed the data and contributed to the results section.
CONFLICT OF INTEREST
Michelle Ness, Jennifer Saylor, Leigh DiFusco and Kristen Evans declare that they have no conflict of interest.
ETHICS STATEMENT
This study was approved by the University of Delaware Institutional Review Board (#1601049‐2). All procedures performed this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in this study.
ACKNOWLEDGEMENT
The authors would like to thank the health care providers that elected to participate in this study. Their willingness to share their stories is greatly appreciated.
Ness MM, Saylor J, DiFusco LA, Evans K. Leadership, professional quality of life and moral distress during COVID‐19: A mixed‐methods approach. J Nurs Manag. 2021;29:2412-2422. 10.1111/jonm.13421
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Ahmad, S. , Arshad, T. , & Kausar, R. (2015). Psychological correlates of distress in rescue 1122 workers in Pakistan. International Journal of Emergency Mental Health and Human Resilience, 17(2), 486–494. [Google Scholar]
- Alkema, K. , Linton, J. , & Davies, R. (2008). A study of the relationship between self‐care, compassion satisfaction, compassion fatigue, and burnout among hospice professionals. Journal of Social Work in End‐of‐Life & Palliative Care, 4(2), 101–119. [DOI] [PubMed] [Google Scholar]
- Amin, A. , Vankar, J. , Nimbalkar, S. , & Phatak, A. (2015). Perceived stress and professional quality of life in neonatal intensive care unit nurses in Gujarat, India. Indian Journal of Pediatrics, 82(11), 1001–1005. [DOI] [PubMed] [Google Scholar]
- Astbury, J. , Gallagher, C. , Astbury, J. L. , & Gallagher, C. T. (2017). Development and validation of a questionnaire to measure moral distress in community pharmacists. International Journal of Clinical Pharmacy, 39(1), 156–164. 10.1007/s11096-016-0413-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont, E. , Durkin, M. , Hollins Martin, C. J. , & Carson, J. (2016). Compassion for others, self‐compassion, quality of life and mental well‐being measures and their association with compassion fatigue and burnout in student midwives: A quantitative survey. Midwifery, 34, 239–244. 10.1016/j.midw.2015.11.002 [DOI] [PubMed] [Google Scholar]
- Berger, J. , Polivka, B. , Smoot, E. A. , & Owens, H. (2015). Compassion fatigue in pediatric nurses. Journal of Pediatric Nursing, 30(6) e11–7. 10.1016/j.pedn.2015.02.005 [DOI] [PubMed] [Google Scholar]
- Berlinger, N. , Wynia, M. , Powell T., Hester, D. M. , Miliken, A. , Fabi, R. , … Jenks, N. P. (2020). Ethical framework for health care institutions & guidelines for institutional ethics services responding to the coronavirus pandemic. https://wcc.on24.com/webcast/present?e=2233370%26k=B7392A3A3F099A073A390723187C0089
- Burston, A. , Eley, R. , Parker, D. , & Tuckett, A. (2017). Validation of an instrument to measure moral distress within the Australian residential and community care environments. International Journal of Older People Nursing, 12(2). 10.1111/opn.12144 [DOI] [PubMed] [Google Scholar]
- Buselli, R. , Corsi, M. , Baldanzi, S. , Chiumiento, M. , del Lupo, E. , Dell'Oste, V. , Bertelloni, C. , Massimetti, G. , Dell'Osso, L. , Cristaudo, A. , & Carmassi, C. (2020). Professional quality of life and mental health outcomes among health care workers exposed to Sars‐Cov‐2 (Covid‐19). International Journal of Environmental Research and Public Health, 17, 6180. 10.3390/ijerph17176180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell, J. , & Poth, C. (2018). Qualitative inquiry & research design (4th ed.). Sage. [Google Scholar]
- Dang, W. , Cheng, W. , Ma, H. , Liu, J. , Wu, B. , Ma, N. , … Yu, X. (2015). Reliability and validity of professional quality of life scale among government staff in earthquake‐stricken areas in China. Chinese Journal of Industrial Hygiene and Occupational Diseases, 33(6), 440–443. [PubMed] [Google Scholar]
- Daubman, B. , Black, L. , & Goodman, A. (2020). Recognizing moral distress in the COVID‐19 pandemic: Lessons from global disaster response. Journal of Hospital Medicine, 15(11), 696–698. [DOI] [PubMed] [Google Scholar]
- de Campos, A. P. , & Daniels, S. (2021). Ethical implications of COVID‐19: Palliative care, public health, and long‐term care facilities. Journal of Hospice & Palliative Nursing, 23(2), 120–127. 10.1097/NJH.0000000000000735 [DOI] [PubMed] [Google Scholar]
- Dudzinski, D. , Hoisington, B. , & Brown, C. (2021). Ethics lessons from Seattle's early experience with COVID‐19. American Journal of Bioethics, 20(7), 67–74. 10.1080/15265161.2020.1764137 [DOI] [PubMed] [Google Scholar]
- Epstein, E. , Whitehead, P. , Prompahakul, C. , Thacker, L. , & Hamric, A. (2019). Enhancing understanding of moral distress: The measure of moral distress for health care professionals. AJOB Empirical Bioethics. 10.1080/23294515.2019.1586008 [DOI] [PubMed] [Google Scholar]
- Fernandez, P. R. , Lord, H. , Halcomb, P. E. , Moxham, P. L. , Middleton, D. R. , Alananzeh, D. I. , & Ellwood, L. (2020). Implications for COVID‐19: A systematic review of nurses' experiences of working in acute care hospital settings during a respiratory pandemic. International Journal of Nursing Studies, 111, 103637. Advance online publication. 10.1016/j.ijnurstu.2020.103637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujii, T. , Katayama, S. , Miyazaki, K. , Nashiki, H. , Niitsu, T. , Takei, T. , Utsunomiya, A. , Dodek, P. , Hamric, A. , & Nakayama, T. (2021). Translation and validation of the Japanese version of the measure of moral distress for healthcare professionals. Health & Quality of Life Outcomes, 19(1), 1–11. 10.1186/s12955-021-01765-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallup Organization . (2019). The Gallup poll briefing. Gallup Organization. [Google Scholar]
- Hamric, A. , & Blackhall, L. (2007). Nurse‐physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Critical Care Medicine., 35(2), 422–429. 10.1097/01.CCM.0000254722.50608.2D [DOI] [PubMed] [Google Scholar]
- Harris, P. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffrey, D. (2020). Relational ethical approaches to the COVID‐19 pandemic. Journal of Medical Ethics, 46(8), 495–498. 10.1136/medethics-2020-106264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam, S. K. K. , Kwong, E. W. Y. , Hung, M. S. Y. , & Chien, W. T. (2020). Emergency nurses' perceptions regarding the risk appraisal of the threat of the emerging infectious disease situation in emergency departments. International Journal of Qualitative Studies on Health and Well‐Being, 15(1), e1718468. 10.1080/17482631.2020.1718468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam, S. K. K. , Kwong, E. W. Y. , Hung, M. S. Y. , Pang, S. M. C. , & Chiang, V. C. L. (2018). Nurses’ preparedness for infectious disease outbreaks: A literature review and narrative synthesis of qualitative evidence. Journal of Clinical Nursing, 27(7–8), e1244–e1255. 10.1111/jocn.14210 [DOI] [PubMed] [Google Scholar]
- Li, Y. , Chen, K. , Collignon, S. , & Ivanov, D. (2021). Ripple effect in the supply chain network: Forward and backward disruption propagation, network health and firm vulnerability. European Journal of Operational Research, 291(3), 11101131. 10.1016/j.ejor.2020.09/053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln, Y. , & Guba, E. (1985). Naturalistic Inquiry (Vol. 9) (pp. 438–439). Sage. 10.1016/0147-1767(85)90062-8 [DOI] [Google Scholar]
- Liu, C. , Yang, Y. , Zhang, X. , Xu, X. , Dou, Q. , Zhang, W. , & Cheng, A. (2020). The prevalence and influencing factors in anxiety in medical workers fighting COVID‐19 in China: A cross‐sectional survey. Epidemiology & Infection, 148, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell, J. B. , Williams, R. L. , Kautz, D. D. , Madden, P. , Heilig, A. , & Thompson, A. (2010). Shared governance: 10 years later. Nursing Management, 41(7), 32–37. 10.1097/01.NUMA.0000384033.17552.03 [DOI] [PubMed] [Google Scholar]
- Morley, G. , Sese, D. , Rajendram, P. , & Horsburgh, C. (2020). Addressing caregiver moral distress during the COVID‐19 pandemic. Cleveland Clinic Journal of Medicine. 10.3949/ccjm.87a.ccc047 [DOI] [PubMed] [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlish, C. , Brown‐Saltzman, K. , So, L. , & Wong, J. (2016). SUPPORT: An evidence‐based model for leaders addressing moral distress. Journal of Nursing Administration, 46(6), 313–320. 10.1097/nna.0000000000000351 [DOI] [PubMed] [Google Scholar]
- Rosser, E. , Westcott, L. , Ali, P. A. , Bosanquet, J. , Castro‐Sanchez, E. , Dewing, J. , McCormack, B. , Merrell, J. , & Witham, G. (2020). The need for visible nursing leadership during COVID‐19. Journal of Nursing Scholarship : An Official Publication of Sigma Theta Tau International Honor Society of Nursing. 10.1111/jnu.12587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski, M. (2000). Whatever happened to qualitative description? Research in Nursing & Health, 23, 334–340. DOI. [DOI] [PubMed] [Google Scholar]
- Sauerland, J. , Marotta, K. , Peinemann, M. A. , Berndt, A. , & Robichaux, C. (2014). Assessing and addressing moral distress and ethical climate, part 1. Dimensions of Critical Care Nursing, 33(4), 234–245. 10.1097/DCC.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Sheehan, J. , Lyons, B. , & Holt, F. (2020). The use of Lean Methodology to reduce personal protective equipment wastage in children undergoing congenital cardiac surgery during the COVID‐19 pandemic. Pediatric Anesthesia, 31(2), 213–220. https://doi.org/10/1111/pan14102 [DOI] [PubMed] [Google Scholar]
- Stamm, B. H. (2010). The ProQOL Concise Manual (2nd ed.). http://www.proQOL.org/ProQOL_Test_Manuals.html [Google Scholar]
- Sun, N. , Wei, L. , Shi, S. , Jiao, D. , Song, R. , Ma, L. , Wang, H. , Wang, C. , Wang, Z. , You, Y. , Liu, S. , & Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID‐19 patients. American Journal of Infection Control, 48, 592–598. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. [DOI] [PubMed] [Google Scholar]
- Ulrich, C. , Rushton, C. , & Grady, C. (2020). Nurses confronting the coronavirus: Challenges met and lessons learned to date. Nursing Outlook, 68(6), 838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead, P. B. , Herbertson, R. K. , Hamric, A. B. , Epstein, E. G. , & Fisher, J. M. (2015). Moral distress among healthcare professionals: Report of an institution‐wide survey. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 47(2), 117–125. 10.1111/jnu.12115 [DOI] [PubMed] [Google Scholar]
- Xiang, Y. , Yang, Y. , Li, W. , Zhang, L. , Zhang, Q. , & Ng, C. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet, 7(3), 228–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


