Abstract
Acute interstitial nephritis can result due to exposure to any medication, toxins, infections or malignancy. In the midst of this Coronavirus (COVID‐19) pandemic, there has been a race for finding remedies to prevent the spread of and control the complications due to Severe Acute Respiratory Syndrome Coronavirus 2. Certain Indian medicinal herb concoctions like kabasura kudineer and nilavembu kudineer are being widely publicized to boost immunity and reduce the risk of developing COVID‐19. Little knowledge exists about the adverse effects of these herbal remedies. We report two patients who presented to us with vague complaints following the ingestion of kabasura kudineer and we diagnosed them with acute tubulointerstitial nephritis (ATIN). The temporal relationship of ingestion of these remedies to the development of ATIN calls for vigilance and caution with regular monitoring of renal functions especially in those with chronic kidney disease.
Keywords: acute kidney injury (AKI), COVID‐19, herbal medications
SUMMARY AT A GLANCE
Summary At A Glance: Certain herbal medicines are being prescribed to boost immunity and reduce the risk of developing COVID‐19 in India. Little is known about the adverse effects of these herbal remedies. This study reports the nephrotoxicity of the Kabasura Kudineer formulation which calls for attention to potentially serious adverse effects of some alternative medicine.
1. INTRODUCTION
The COVID‐19 pandemic, which first reported in Wuhan, China, has now more than 10 million people infected worldwide. Various therapeutic strategies are being researched, and trials are being done to find the prevention and cure for this deadly virus. Traditional Indian systems of medications which include Siddha have also offered a variety of herbs to improve immunity to prevent the development of COVID‐19. Official Siddha formulations kabasura kudineer chooranam is believed to be a potent formulation with anti‐viral and immuno‐modulatory properties. 1 , 2 We report two patients who developed acute kidney injury (AKI) following the consumption of this formulation.
2. CASE HISTORY
2.1. Patient K
Mr K, a 51‐year‐old male who had an aortic valve replacement in 2013 presented with loss of appetite and easy fatigability of 1‐week duration. He reported no history of diabetes or hypertension. His medications included warfarin and nebivolol. He had no fever, rash, joint pains, cough, or hemoptysis. He had not consumed any known nephrotoxic agents like antibiotics, non‐steroidal anti‐inflammatory drugs or proton pump inhibitors (PPI). On further questioning, he said that he was taking 'kabasura kudineer' 60 ml once a day a week prior to the start of his symptoms. His baseline serum creatinine (SCr) done 2 months prior was 1.1 mg/dl. At presentation, he was euvolemic and had a blood pressure of 120/70 mmHg. His urinalysis showed no proteinuria but sediment revealed 3–5 WBC/HPF, 10–15 RBC/HPF and many granular casts. Mid‐stream urine culture was sterile. Serum creatinine at presentation was 2.8 mg/dl and international normalized ratio was 2.4. Ultrasound showed normal sized kidneys with no hydronephrosis. After stopping warfarin and the herbal drink for 5 days, a kidney biopsy was performed as serum creatinine was still 2.8 mg/dl. Renal biopsy revealed acute tubulointerstitial nephritis (ATIN) in the background of mild arteriosclerosis, immunofluorescence (IF) was negative (Figure 1A). He was started on 0.5 mg/kg/day of prednisone. SCr after 2 weeks is 1.3 mg/dl and steroids were tapered by 5 mg every 5 days. Three months later his SCr remains at 1.2 mg/dl.
FIGURE 1.
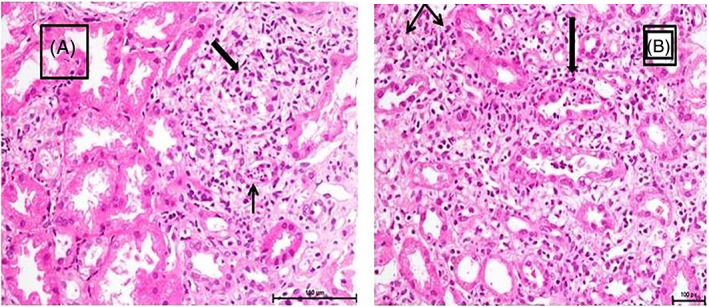
(A) Interstitial inflammation with tubular injury and WBC cast (H&E). (B) Tubular injury with neutrophilc tubulitis and WBC cast; interstitial edema and inflammation (H&E)
2.2. Patient D
Mr D, a 63‐year‐old male with no known co‐morbidities presented with nausea of 1‐week duration. He was on no medications except for kabasura kudineer around 30–40 ml twice a day for 2 days prior to the symptoms. He had not consumed any known nephrotoxic agents like antibiotics, NSAID or PPI. At presentation he was anaemic, euvolemic and had a blood pressure of 140/70 mmHg. He was afebrile with no rash or joint swelling. He did not have any baseline blood tests done prior to this episode. SCr was 3.8 mg/dl, haemoglobin 7.2 g/dl and urinalysis showed many WBC and WBC casts. Mid‐stream urine culture was negative and ultrasound showed normal sized kidneys. Renal biopsy was performed which showed ATIN on a background of early IgA staining on IF (Figure 1B). He was started on 0.5 mg/kg/day of prednisone after confirming a normal gastroscopy. The serum SCr decreased to 2.8 mg/dl a week later. He was tapered off the steroids over 6 weeks and his serum creatinine after 2 months is 1.1 mg/dl.
The details of the both the patients are illustrated in Table 1.
TABLE 1.
Clinical characteristics of the patients
| Name | Mr. K | Mr. D |
| Age | 51 years | 63 years |
| Gender | Male | Male |
| Base line serum creatinine [SCr (mg/dl)] | 1.21 mg/dl in January 2020 | Not available |
| Diabetes mellitus | No | No |
| Systemic hypertension | No | No |
| Others | S/P. Aortic valve replacement (January/2013) | None |
| Medications | Warfarin and metoprolol | None |
| Urine routine | Albumin‐nil, sugar‐nil, pus cells 3–5, epithelial cells 1–2, RBC 10–15, granular cast present | Albumin‐nil, sugar‐nil, Pus cells >50, epithelial cells 2–3, RBC 3–5, WBC cast and granular cast present |
| Haemoglobin (g/dl) | 12.9 | 7.2 |
| Total leucocyte count (cells/mm3) | 18 300 | 8900 |
| Platelet (Lak/mm3) | 3.00 | 3.18 |
| Urea (mg/dl) | 29 | 74 |
| SCr at presentation (mg/dl) | 3.56 | 3.25 |
| Sodium (mmol/L) | 138 | 124 |
| Potassium (mmol/L) | 3.47 | 2.89 |
| Bicarbonate (mmol/L) | 29 | 30 |
| Calcium (mg/dl) | 8.6 | 8.4 |
| Phosphorous (mg/dl) | 3.2 | 4.4 |
| T. protein (g/dl) | 10.3 | 6.5 |
| Albumin (g/dl) | 4.7 | 3.4 |
| TSH (mIU/L) | 3.22 | 1.95 |
| HbA1c (%) | 5.6 (23 December 2019) | 6.3 |
|
Oro pharyngeal Swab for RT‐PCR COVID |
Negative | Negative |
| Kidney biopsy Findings |
Acute tubulointerstitial nephritis Mild to moderate Arteriosclerosis Interstitial fibrosis and tubular atrophy 10%–15% |
Acute tubulointerstitial nephritis IgA nephropathy Interstitial fibrosis and tubular atrophy 5%–10% |
| Immunofluorescence | Negative for IgA, IgG, C3, Kappa and Lambda | IgA (2+), C3 (Trace), Lambda (2+) and Kappa (Trace) |
| Treatment given | Prednisone 0.5 mg/kg bodyweight/day tapered over 8 weeks | Prednisone 0.5 mg/kg bodyweight/day tapered over 6 weeks |
| SCr (mg/dl) after 2 weeks of treatment with steroids | 1.49 | 2.23 |
| SCr (mg/dl) on further follow up | 1.2 mg/dl after 3 months | 1.1 mg/dl after 2 months |
| Side effects of treatment | Hyperglycemia needing medications | Hyperglycemia needing medications |
3. DISCUSSION
Acute kidney injury with ATIN can occur due to numerous prescribed and over‐the‐counter medications and health drinks. It is estimated that one in three cases of ATIN can be due to endogenous and exogenous toxins. Establishing the causality of health food & health drink toxins inducing kidney disease is a challenge and requires a detailed history, time course, assessment of competing risk factors, and mechanism of injury and biological plausibility of the toxins.
Kidney toxicity of the agent and underlying patient characteristics such as increasing age, alter the metabolism and pathway of excretion of various agents administered and enhance the risk of the development of ATIN. 3 The National Kidney Foundation has cautioned against the use of herbal supplements and drugs without adequate monitoring as vulnerable populations like those with chronic kidney disease (CKD) can suffer significant damage. 4 , 5 The kidneys which are involved in the elimination of xenobiotics, environmental agent and metals through glomerular filtration, tubular secretion and metabolism is highly vulnerable to the toxicity of these agents. 6
Siddha system of medicine, one of the oldest systems of medicine, has been promoting 'kabasura kudineer', as a formulation for immunity building affecting tumour necrosis factor signalling pathways. 7 It contains 16 constituents (Zingiber officinale, Piper longum, Syzygium aromaticum, Cirucirukancori ver, Tragia involucrata, Anacyclus pyrethrum, Solanum anguivi, Terminalia chebula, Justicia adhatoda, Coleus aromaticus, Saussurea costus, Tinospora cordifolia, Clerodendron serratum, Andrographis paniculata, Cissampelos pareira, Cyperus rotundus and neer [water]). It has been recommended to mix 8 g of the powder in four glasses of water and boil to reduce it to a glass and to be taken two to three times a day. Active phytoconstituents of this polyherbal decoction is supposed to have high affinity to the spike protein of the COVID‐19 virus and hence prevents its binding to the ACE2 receptor on the host cell. 7 , 8 Among the constituents, Syzygium aromaticum, 9 Solanum anguivi, 10 Andrographis paniculata 11 and Cyperus rotundus 12 have been known to produce various degrees of nephrotoxicity according to case reports and series.
To the best of our knowledge, ATIN due to 'kabasura kudineer' has not yet been reported. We referred to the criteria by Naranjo et al. 13 to report an adverse drug event. A score of 6 was derived using these criteria, rating this adverse reaction as “probable”. Nephrotoxicity was attributed to this drug on the basis of the criteria of Naranjo et al., clinical onset of AKI, absence of any other nephrotoxic drugs being administered, and histopathological findings on the renal biopsy. 13 In our two patients, the temporal relationship to kidney injury with no previous known nephrotoxic agents establishes a cause and effect relationship. The ATIN seems to be dose independent as both the patients took different amounts of the drug and the time period to the development of AKI has also been variable. Interestingly both had gastrointestinal symptoms after taking the formulation. It is worthwhile to think both these patients had some baseline CKD (as evidenced on biopsy) which makes them more vulnerable to AKI. Patient D had mesangial IgA deposits in the kidney which may be mean he had pre‐existing IgA nephropathy (IgAN) or it was an incidental IgA deposition. However, the kidney biopsy findings in patient D were not suggestive of IgAN. Both patients improved after stopping the formulation and with the addition of a short course of low dose steroids.
A multi‐pronged approach for prevention includes increased awareness for both providers and patients of the potential nephrotoxicity of herbal formulations. A high index of suspicion of potential toxicity is necessary for early recognition and management.
Parthasarathy R, Mathew M, Koshy P, Babu M, Abraham G. Traditional medicines prescribed for prevention of COVID‐19: Use with caution. Nephrology. 2021;26(12):961‐964. 10.1111/nep.13947
REFERENCES
- 1. Kiran G, Karthik L, Devi MSS, et al. In silico computational screening of kabasura kudineer—official siddha formulation and JACOM against SARS‐CoV‐2 spike protein. J Ayurveda Integr Med. 2020:S0975‐9476(20)30024‐3. 10.1016/j.jaim.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Heron M. Deaths: Leading Causes for 2017. Vol 68. Hyattsville, MD: US Department of Health and HUMAN Services/Centers for Disease Control and Prevention/National Center for Health Statistics/National Vital Statistics System; 2019. No. 6. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_06-508.pdf. [PubMed] [Google Scholar]
- 3. National Kidney Foundation website—Kidney Disease—A to Z Health Guide—Use of Herbal Supplements in Chronic Kidney Disease. http://www.kidney.org/ATOZ/.
- 4. Singh N, Ganguli A, Prakash A. Drug‐induced kidney disease. J Assoc Phys India. 2003;51:970‐979. [PubMed] [Google Scholar]
- 5. Charen E, Harbord N. Toxicity of herbs, vitamins, and supplements. Adv Chronic Kidney Dis. 2020;27(1):67‐71. [DOI] [PubMed] [Google Scholar]
- 6. Saravanan J, Devasia N, Gopalasatheeskumar K, Sanish Devan V, ThangaKokila K, Sanjay M. Anti‐inflammatory, antipyretic and antibacterial study of kabasura kudineer choornam. Int J Curr Adv Res. 2018;7(2):9992e7. [Google Scholar]
- 7. Thillaivanan S, Parthiban P, Kanakavalli K, Sathiyarajeshwaran P. A review on “kapasura kudineer”—a siddha formulary prediction for swine flu. Int J Pharm Sci Drug Res. 2015;7(5):376‐383. [Google Scholar]
- 8. Vellingiri B, Jayaramayya K, Iyer M, et al. COVID‐19: a promising cure for the global panic. Sci Total Environ. 2020;725:138277. 10.1016/j.scitotenv.2020.138277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lane BW, Ellenhorn MJ, Hulbert TV, McCarron M. Clove oil ingestion in an infant. Hum Exp Toxicol. 1991;10(4):291‐294. [DOI] [PubMed] [Google Scholar]
- 10. Oh SS, Choi MW, Choi MR, et al. Acute interstitial nephritis induced by Solanum nigrum . Kidney Res Clin Pract. 2016;35(4):252‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang W‐X, Zhang Z‐M, Zhang Z‐Q, Wang Y, Zhou W. Andrographolide induced acute kidney injury: analysis of 26 cases reported in Chinese literature. Nephrology (Carlton, Vic.). 2014;19(1):21‐26. 10.1111/nep.12172 [DOI] [PubMed] [Google Scholar]
- 12. Yang S, Oh A, Ha T‐S. Two pediatric patients with herbal medicine‐induced nephrotic syndrome. Child Kidney Dis. 2015;19(2):171‐175. 10.3339/chikd.2015.19.2.171 [DOI] [Google Scholar]
- 13. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239‐245. 10.1038/clpt.1981.154 [DOI] [PubMed] [Google Scholar]


