Abstract
Background
The COVID‐19 pandemic has had a profound effect on the presentation and management of trauma at the Royal Melbourne Hospital, a level 1 adult major trauma service and a designated COVID‐19 hospital. This study compares the changes in epidemiology and trauma patient access to emergency imaging and surgery during the pandemic response.
Methods
The population of interest was all trauma patients captured in the hospital's trauma registry from 16 March 2016 to 10 September 2020. Regression modelling assessed changes in mechanism and severity of the injury, and mortality during two lockdowns compared with the proceeding 4 years. Cases were matched with hospital administrative databases to assess mean time from admission to emergency computed tomography (CT) scan, operating theatre, length of stay (LOS) and immediate surgery (OPSTAT).
Results
Throughout 2020, the hospital treated 525 COVID‐19 patients. Compared with previous years, there was up to 34% reduction in major trauma and a 28% reduction in minor trauma admissions during the pandemic (p < 0.05). Intensive care unit admissions were almost half of predicted. Some of the largest reductions were seen in motor vehicle crashes (49%) and falls (28%) (p < 0.05). Time to CT, surgery and immediate surgery (OPSTAT) showed no change and having a suspected COVID‐19 diagnosis did not prolong any of these times except for the LOS. Mortality was similar to previous years.
Conclusion
The COVID‐19 pandemic has had widespread societal changes, resulting in a substantial decrease in trauma presentations. Despite COVID's immense impact on the hospital's trauma service, the quality of care was not impaired.
Keywords: COVID‐19, emergency medicine, epidemiology, health services, public health
The COVID‐19 pandemic has had widespread societal changes, resulting in a substantial decrease in trauma presentations. Despite COVID's immense impact on the Royal Melbourne Hospital's level 1 trauma service, the quality of care was not compromised.

Introduction
On 11 March 2020, the World Health Organization declared the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2, the causative virus for COVID‐19) outbreak a pandemic and global health emergency. As of May 2021, Australia ranks 121 of 215 countries on the Worldometer's list for the number of COVID‐19 cases and 102 for the number of COVID‐19 deaths. 1 Nevertheless, Melbourne has experienced one of the world's longest and strictest lockdowns. 2 , 3 Residents have endured more than 5 months under some form of stay‐at‐home restrictions: 52 days from 16 March 2020, when cases ranged from 30 to 50 a day during the first wave, then another 111 days from 8 July 2020, when cases increased to 500–700 a day, during a more prolonged second wave.
During the first wave, there was a decrease in trauma cases presenting to the Royal Melbourne Hospital (RMH), a level 1 adult major trauma service. An analysis of expected numbers showed a 24% reduction in trauma emergency presentations and a 42% reduction in trauma hospital admissions. 4 Similar reductions have been reported worldwide, where there have been considerably higher COVID‐19 cases compared with Australia. 5 Nevertheless, the RMH needed to adapt to meet patients' needs and keep both patients and healthcare workers safe.
While overall trauma cases presenting to the hospital decreased during the pandemic, it is unknown what type of cases they were and if the trends continued during the larger second wave of COVID‐19. Due to statewide restrictions in travel and social activities, we hypothesised that motor vehicle and sport‐related accidents decreased, along with assaults from unknown persons. In contrast, because of financial and employment stresses during this time, we hypothesised an increase in family violence cases. Cases that often occur in the elderly, such as hip fractures, were thought unlikely to change. Therefore, the aims of this study were to (1) explore the number and type of trauma cases presenting to the RMH during the COVID‐19 pandemic; and (2) investigate the impact of the pandemic on the quality of care of trauma patients.
Methods
The RMH is a 600‐bed metropolitan, quaternary hospital and a level 1 adult major trauma service. It provides care to more than 4000 trauma patients annually and is one of the two designated adult major trauma services responsible for providing care to the state of Victoria (with a population of 6.5 million and an average growth rate of 2% per annum). 6 The hospital is committed to maintaining a state of readiness, including 24/7 access to an operating room, the intensive care unit (ICU) and the full complement of trauma service resources. In response to rising positive COVID‐19 cases, the hospital set up a screening clinic and became a dedicated centre for COVID‐19.
Using a trauma registry maintained by the hospital, we obtained data for all trauma patients who presented to the emergency department (ED) from 16 March 2016 to 10 September 2020, with an abbreviated injury scale (AIS) score of ≥1 to any body region and a length of stay (LOS) ≥24 h. Additional outcomes from the administrative database that the hospital uses to store patient data were linked with the trauma registry patients. As per the Victoria State Trauma System guidelines, patients were defined as ‘Major Trauma’ if they met any of the following criteria: death (excludes dead on arrival); Injury Severity Score >12; admitted to ICU for >24 h with >0 h of mechanical ventilation; required urgent surgery for an injury to the head, chest, abdomen, pelvis or spine injury in <48 h; or had partial or full‐thickness burns (total body surface area 20%–29%). ‘Minor Trauma’ patients were those with a principal diagnosis of injury, AIS score of ≥1 to any body region and LOS ≥24 h. Some trauma patients were school age because their size was closer to that of an adult or they did not meet the paediatric trauma definition of <16 years of age. Regardless of their theatre status, patients with multiple severe injuries were assumed to have COVID‐19 until testing proved otherwise, and those with major or minor injuries who reported any symptoms (fever, dry cough, sore throat or shortness of breath) or were unable to answer screening questions were assumed to have COVID‐19. Patients were also suspected to have COVID‐19 if they were close contacts of a confirmed case of COVID‐19, returned from overseas in the last 14 days, or were a healthcare worker or aged care worker. Initially, test results were received within 24 h and reduced to 1–2 h when rapid COVID testing with GeneXpert became systematically available in July 2020. The patient's hospital record documented if they were suspected of COVID‐19, and so in the analysis, we tested whether their suspected diagnosis impacted their time to first computed tomography (CT) scan, operation or overall LOS compared with 2016–2019.
Patients in 2020 who were identified as not being at risk of COVID‐19 were also analysed separately and compared with 2016–2019. For quality‐of‐service indicators, we used the time to first CT scan and first trauma operation, regardless of type or categorised urgency to assess the entire service delivery, not just the critical patients. For time‐critical trauma patients, we measured time to trauma OPSTAT (defined as immediate surgery for life‐saving in the exsanguinating patient).
We separated the findings into three periods: (1) 16 March to 11 May to represent the first wave of COVID‐19 (57 days), (2) 12 May to 7 July to signify the transition period when daily COVID‐19 cases dropped to single digits (57 days) and (3) 8 July to 10 September to capture the second wave of COVID‐19 cases (61 days). March 16 corresponds to the onset of the first lockdown in Victoria when stage 3 restrictions were used, which involved the closure of schools, childcare remained open, face masks were mandatory, gatherings of up to two people only were allowed and individuals could only leave their house for essential reasons. On 12 May, restrictions were eased, initially allowing gatherings of up to 10 people and then 20 people, and children returned to school. Case numbers then began to rise, and the second lockdown began on 8 July with stage 4 restrictions, which introduced over and above stage 3, an evening curfew, closure of childcare and travel no more than 5 km from home. On 10 September, the pandemic curve had passed its peak and flattened out to low numbers. The similar duration for all three periods allowed us to compare the findings across the two waves and the transition period.
The study was approved as a Quality Assurance Project (QA2020087) by the Melbourne Health Office for Research Ethics & Governance and Human Research Ethics Committee.
Statistical analysis
A generalised linear model (Poisson for count variables and Gaussian for continuous variables) was developed using data from 2016 to 2019 and used to predict numbers for 2020. We tested the null hypothesis that there was no difference in the number of cases between pre‐pandemic (2016 to 2019) and pandemic (2020) periods. Separate regression models were fitted to the number of (1) trauma presentations (major and minor), (2) ICU admissions, (3) mechanism of injury, (4) intent, (5) location of injury, (6) mean LOS and four quality‐of‐care indicators: (1) mean time to CT (time from admission to first CT scan for all trauma patients), (2) mean time to operation (time from admission to any first surgery), (3) mortality of major trauma patients and (4) mean time from admission to trauma OPSTAT (which was analysed using independent t‐test because of the small numbers). To find the difference between expected and observed cases, we subtracted one from the other and the difference was considered statistically significant (p < 0.05) if the 95% confidence intervals did not include zero. Nonparametric Mann–Whitney U‐tests were also used to compare the quality‐of‐care outcomes for patients in 2020 at‐risk versus not at risk of COVID‐19.
Poisson regression models showed the goodness of fit for most outcomes, and for those it did not (25%), no other approach (negative binomial regression or Gaussian) improved the model. Overdispersion was not detected in any analysis as indicated by the Pearson chi‐square dispersion statistic. Neither the Poisson nor Gaussian regression models showed any autocorrelation as indicated by the Durbin–Watson statistic. As an exploratory study, we did not correct for multiple‐hypothesis testing. All analyses were conducted using Stata version 16 (StataCorp., TX, USA).
Results
Overview of 2020
From 1 January to 10 September 2020, there were 20 271 positive SARS‐CoV‐2 (COVID‐19) notifications in Victoria, Australia, of which 525 were admitted to the RMH. Reports for COVID‐19 first peaked in early April (first wave) and reached a higher second peak in early August (second wave). Figure 1 shows there was a concomitant decrease in trauma presentations (minor and major) during both waves.
Fig. 1.
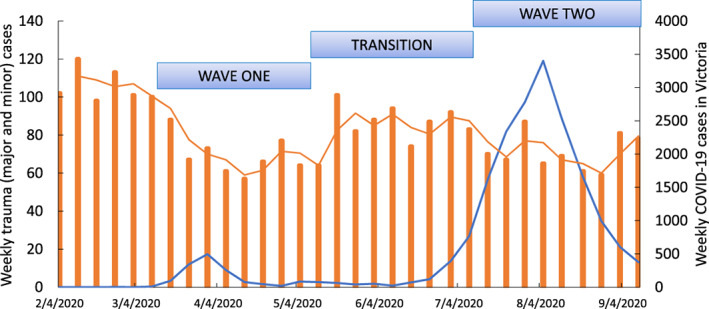
Weekly number of positive COVID‐19 cases in Victoria (blue line) and the corresponding weekly trauma presentations (major and minor) (orange bars and orange trend line) at the Royal Melbourne Hospital from 4 February to 14 September 2020.  , Weekly trauma cases;
, Weekly trauma cases;  , weekly COVID‐19 cases.
, weekly COVID‐19 cases.
Case numbers in 2020 compared with the last 4 years
From 2016 to 2019, there was a gradual increase in trauma presentations, both major and minor cases (Fig. 2). From 16 March to 11 May 2020, when the first wave of COVID‐19 cases peaked, there was a marked reduction in total trauma presentations (30% reduction), major trauma cases (34% reduction) and minor trauma cases (28% reduction) (all p < 0.05) (Fig. 3). There was a significant reduction in trauma cases secondary to falls (28% reduction) and motor vehicle crashes (49% reduction) and incidents occurring during sport and leisure activities (93% reduction) (all p < 0.05) (Table 1). The number of ICU admissions from trauma was also lower during the first wave (47% reduction, p < 0.05).
Fig. 2.
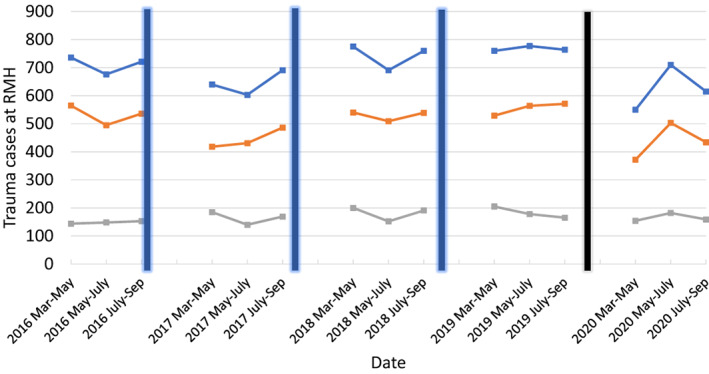
Total number of trauma (minor and major) cases presenting to the Royal Melbourne Hospital during our three periods of interest: March to May (wave 1), May to July (transition) and July to September (wave 2), from 2016 to 2020. The blue vertical line indicates the time in between our periods of interest, and the black vertical line indicates the beginning of the first wave of COVID‐19 in Victoria and the onset of lockdown (16 March 2020).  , Total trauma;
, Total trauma;  , minor cases;
, minor cases;  , major cases.
, major cases.
Fig. 3.
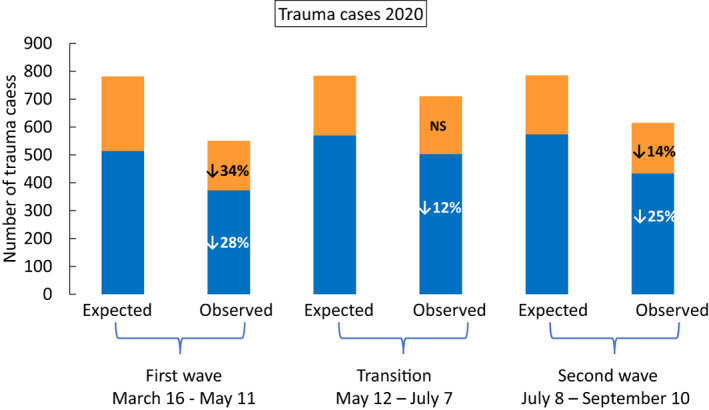
Minor (blue,  ) and major (orange,
) and major (orange,  ) trauma cases presenting to the Royal Melbourne Hospital during our three periods of interest: March to May (wave 1), May to July (transition) and July to September (wave 2). The number of expected (modelled from case numbers in 2016–2019) and observed cases in 2020 are shown, with the percent deviation from what was expected indicated in text in the observed columns.
) trauma cases presenting to the Royal Melbourne Hospital during our three periods of interest: March to May (wave 1), May to July (transition) and July to September (wave 2). The number of expected (modelled from case numbers in 2016–2019) and observed cases in 2020 are shown, with the percent deviation from what was expected indicated in text in the observed columns.
Table 1.
Characteristics of people presenting with trauma‐related injuries at the emergency department of the Royal Melbourne Hospital from 16 March to 10 September 2020
| 16 March to 11 May, first wave (57 days) | 12 May to 7 July, transition period (57 days) | 8 July to 10 September, second wave (61 days) | ||||
|---|---|---|---|---|---|---|
| 2020 | Difference between predicted and observed | 2020 | Difference between predicted and observed | 2020 | Difference between predicted and observed | |
| Mechanism of injury, N | ||||||
| Animal‐related | 27 | 9 (−2 to 20) | 21 | 4 (−6 to 14) | 23 | −6 (−16 to 4) |
| Fall | 228 | −87 (−118 to −56) † | 296 | 2 (−36 to 40) | 288 | −55 (−88 to −22) † |
| Firearm | 4 | 3 (−1 to 7) | 2 | −3 (−6 to −0.1) † | 4 | 3 (−1 to 7) |
| Burn, electricity, machinery | 59 | −11 (−27 to 5) | 71 | −26 (−44 to −8) † | 66 | 10 (−5 to 25) |
| Motor vehicle | 111 | −106 (−128 to −84) † | 171 | −28 (−52 to −4) † | 128 | −85 (−110 to −60) † |
| Cyclist/pedestrian | 63 | −8 (−28 to 12) | 68 | −15 (−30 to 0) | 37 | −25 (−37 to −14) † |
| Struck | 54 | −23 (−40 to 6) | 76 | 3 (−14 to 20) | 56 | −19 (−36 to −2) † |
| Other | 4 | −10 (−14 to 6) | 5 | −11 (−15 to −7) † | 12 | 2 (−5 to 9) |
| Intent, N | ||||||
| Accident | 480 | −223 (−266 to −180) † | 608 | −93 (−154 to −41) † | 525 | −186 (−230 to −142) † |
| Maltreatment/neglect/assault (family, ex/partner) | 3 | −2 (−5 to 2) | 4 | −2 (−6 to 2) | 6 | 0 (−5 to 5) |
| Sexual/assault by other/unknown | 39 | −51 (−65 to −38) † | 63 | −17 (−31 to −3) † | 38 | −57 (−68 to 47) † |
| Intentional self‐harm | 17 | 3 (−5 to 11) | 25 | −5 (−15 to 5) | 34 | 18 (7 to 29) |
| Other | 4 | −4 (−7 to 0) | 6 | −7 (−12 to −3) † | 8 | −1 (−6 to 4) |
| Place, N | ||||||
| Leisure/sport | 2 | −29 (−32 to −26) † | 6 | −21 (−26 to −16) † | 6 | −31 (−36 to −27) † |
| Farm/school | 10 | 4 (−2 to 10) | 16 | 6 (−2 to 14) | 10 | 6 (−1 to 13) |
| Home | 168 | 8 (−17 to 33) | 236 | 86 (49 to 123) † | 208 | 34 (3 to 65) † |
| Work | 31 | 1 (−9 to 11) | 32 | −14 (−25 to −3) † | 27 | −9 (−18 to 0) |
| Road | 180 | −95 (−124 to −66) † | 226 | −47 (−72 to −22) † | 162 | −112 (−138 to −86) † |
| Other | 159 | −122 (−148 to −96) † | 194 | −79 (−108 to −50) † | 202 | −62 (−91 to −33) † |
| Hip fracture ‡ , N | 22 | −8 (−1 to 17) | 25 | −8 (−19 to 3) | 22 | −6 (−15 to 3) |
| ICU admission, N | 68 | −60 (−76 to −42) † | 81 | 13 (−7 to 33) | 77 | 6 (−9 to 21) |
Mean differences and 95% confidence interval between observed versus predicted numbers are provided for 16 March to 11 May 2020 (first wave), 12 May to 7 July 2020 (transition period), and 8 July to 10 September 2020 (second wave).
Significant difference as indicated by the 95% confidence intervals.
Hip fractures include neck of femur and intertrochanteric region and were included in major trauma numbers.
ICU, intensive care unit.
During the transition period (12 May to 7 July 2020), compared with previous years, trauma presentations reduced slightly (10% reduction), due to fewer minor cases (12% reduction) (both p < 0.05); major cases were unchanged (Fig. 3). Trauma cases due to motor vehicle crashes and sport and leisure activities continued to be lower than expected (14% and 78% reduction, respectively, p < 0.05) (Table 1). There was a decrease in firearm injuries (60% reduction); injuries from burns, electricity and machinery (27% reduction); and the number of accidents in the workplace (30% reduction) (all p < 0.05). In contrast, accidents occurring at the home increased (57% increase, p < 0.05). ICU admissions did not change from what was expected.
During the large second wave of COVID‐19 (8 July to 10 September 2020), compared with previous years, trauma presentations were again reduced (22% reduction) mostly due to a reduction in minor cases (25% reduction), less so from major cases (14% reduction) (all p < 0.05) (Fig. 3). There was a significant reduction in cases from motor vehicle crashes (40% reduction), pedestrian and cycling accidents (40% reduction), falls (16% reduction), as well as those occurring during sport and leisure activities (84% reduction) (all p < 0.05) (Table 1). Similar to wave 1, trauma events in the home increased (20% increase, p < 0.05).
For all three periods, hip fractures, accidents at school or a farm and animal‐related injuries did not change from what was expected.
Assaults
Cases of family and interpersonal violence due to either maltreatment/neglect/or assault by a family member/current/ex‐partner were not different to expected numbers during the first wave, the transition period or the second wave (Table 1). The number of sexual assaults/or assaults by an unknown person was lower during the first wave (57% reduction), the transition period (22% reduction) and the second wave (60% reduction) (all p < 0.05). Intentional self‐harm was not different compared with the number expected for all three time periods.
Quality of care
The COVID‐19 outbreak did not appear to negatively affect the quality‐of‐care indicators (Table 2). During the first wave, the mean time from admission to the first CT scan for patients not at risk of COVID‐19 was reduced compared with what was expected (305 vs. 486 min expected, p < 0.05), and no different for patients not at risk of COVID‐19 (619 vs. 497 min expected, NS). The mean time from admission to an operation was not different from what was expected for patients at risk of COVID‐19 (1695 vs. 2160 min expected, NS) but reduced for those not at risk of COVID‐19 (1808 vs. 2187 min expected, p < 0.05).
Table 2.
Length of stay and quality of care indicators for all admitted trauma patients who were and were not suspected of a positive COVID‐19 diagnosis.
| March 16 to May 11First wave (57 days) | May 12 to July 7 Transition period (57 days) | July 8 to September 6Second wave (61 days) | ||||
|---|---|---|---|---|---|---|
| 2020 | Difference between predicted and observed (95% CI) | 2020 | Difference between predicted and observed (95% CI) | 2020 | Difference between predicted and observed (95% CI) | |
| Length of stay, days | ||||||
| Risk of COVID patients, mean (SD) | 6.3 (7.8) | 0.4 (‐2.1 to 2.8) | 8.4 (12.4)* | 3.2 (0.2 to 6.2)‡ | 7.2 (7.4)** | 1.5 (0.1 to 2.8)‡ |
| Median (IQR) | 4.0 (4.2) | 5.4 (7.9)* | 5.0 (6.7)** | |||
| No risk of COVID patients, mean (SD) | 4.9 (6.0) | –1.0 (–1.6 to –0.5)‡ | 5.2 (4.9) | 0.2 (–0.4 to 0.8) | 6.6 (5.0) | –0.8 (–1.4 to –0.2)‡ |
| Median (IQR) | 2.8 (1.9) | 3.0 (1.2) | 2.7 (1.5) | |||
| Time from admission to CT scan, min | ||||||
| Risk of COVID patients, mean (SD) | 619 (1651) | 122 (–417 to 661) | 240 (497)* | –78 (–202 to 46) | 279 (739) | –108 (–246 to 31) |
| Median (IQR) | 70 (91) | 84 (114)* | 104 (127) | |||
| No risk of COVID patients, mean (SD) | 305 (1014) | –181 (–282 to –80)‡ | 337 (1204) | 19 (–86 to 124) | 295 (992) | –91 (–190 to 9) |
| Median (IQR) | 90 (49) | 102 (37) | 102 (54) | |||
| Mean time from admission to operation, min | ||||||
| Risk of COVID patients, mean (SD) | 1695 (1772) | –465 (–1394 to 463) | 2209 (2558) | 169 (–1011 to 1349) | 2162 (2897) | –4.2 (–744 to 735) |
| Median (IQR) | 857 (2290) | 1452 (1642) | 1141 (1310) | |||
| No risk of COVID patients, mean (SD) | 1808 (2215) | –379 (–644 to –155)‡ | 1907 (2787) | –135 (–454 to 185) | 1480 (1472) | –685 (–878 to –492)‡ |
| Median (IQR) | 1193 (641) | 1278 (836) | 1120 (503) | |||
| Time from admission to OPSTAT, min | ||||||
| All patients, mean (SD) | 31 (20) | –37 (–14 to 88) | 61 (26) | –1 (–54 to 52) | 64 (13) | –16 (–67 to 33) |
| Median (IQR) | 32 (40) | 57 (51) | 64 (19) | |||
| Mortality of major trauma patients, % | 11.0 | 3.2 (–3.8 to 10.1) | 8.7 | 2.9 (–0.5 to 6.3) | 10.7 | 0.8 (–4.0 to 4.6) |
Note: ‡Significant difference as indicated by the 95% confidence intervals. Any difference noted between what the overall expected number should be for at risk of COVID and not at risk of COVID‐19 patients is the result of separate regression models creating predictions for a different sample size, all other parameters are the same. Mann‐Whitney U test between 2020 patients at risk of COVID vs. not at risk: *p < 0.05, **p < 0.01. Supplementary tables present numbers from all years
During the transition period, the mean time to a CT scan and the first operation was as expected for all patients, but time to CT scan was shorter for patients at risk of COVID‐19 when directly compared with not at‐risk patients during the same period (240 vs. 337 min, p < 0.05). When the second wave began, the mean time to first CT scan was unaffected for at‐risk (279 vs. 387 min expected, NS) and not at‐risk COVID‐19 patients (295 vs. 386 min expected, NS). However, the mean time to first trauma operation was reduced for patients not at risk of COVID‐19 (1480 vs. 2165 min expected, p < 0.05), and not different to what was expected for patients at risk of COVID‐19 (2162 vs. 2166 min expected, NS). The mean time from admission to the operating theatre for immediate life‐saving surgery (OPSTAT) was unaffected during all phases in 2020.
The mean LOS for trauma patients not at risk of COVID‐19 was reduced during wave 1 (4.9 vs. 5.9 days expected) and wave 2 (6.3 vs. 5.9 days expected) (both p < 0.05) and no difference was observed during the transition period. Conversely, patients at risk of COVID‐19 had a longer mean LOS during the transition period (8.4 vs. 5.2 days expected) and wave 2 (7.2 vs. 5.7 days expected) (both p < 0.05). Their LOS was also significantly longer than patients not at risk of COVID‐19 during both periods (p < 0.05 to <0.01). Mortality rates of major trauma patients were as expected for all three time periods (Table 2).
Discussion
Restrictions imposed by the state government during the first and second waves of COVID‐19 are likely to explain the observed 22%–30% decrease in the number of trauma cases presenting to a quaternary, level 1 major trauma hospital. Individuals were recommended to avoid unnecessary movements and to stay at home as much as possible. Non‐essential businesses were closed, and construction sites had fewer workers. We found that the number of trauma cases due to motor vehicle crashes, sport‐related injuries, falls and interpersonal violence were all lower than expected based on trends from 2015 to 2019. Numbers continued to be lower in the transition period, albeit to a lesser extent, most likely because people were advised to continue working from home if possible and sporting activities were slow to commence. In contrast, hip fractures that often occur in the elderly did not appear to be impacted by the restrictions and support findings reported in Europe. 7 , 8
There was no change in family violence cases, despite reports of a 6.7% increase in domestic abuse callouts from the Victorian police. 9 This increase has been reported internationally and attributed to the social isolation measures that have restricted people to living in volatile situations of family violence to their homes. 10 The apparent absence of these victims to our hospital may be due to a combination of a fear of contracting COVID‐19 since the RMH was known as a dedicated COVID‐19 hospital 11 and the minority of family violence victims reaching minor or major trauma criteria, and of those who do, may not reveal the true causality of their injury for fear of personal safety. This should by no means be considered a comprehensive assessment of the impact of the pandemic on family violence.
Quality‐of‐care indicators for the treatment of trauma patients, including the mean duration from admission to CT scan and to the first operation, were not compromised and at times reduced for patients at risk and not at risk of COVID‐19 compared with what was expected. This was surprising given the additional requirements for suspected COVID patients to ensure staff safety. For example, time‐critical trauma interventions such as intubation and intercostal catheter insertion were deemed high‐risk aerosol‐generating procedures, resulting in less staff being present to reduce potential exposure, plus increased personal protective equipment (PPE) requirements for attending staff. 12 Nevertheless, this is likely to have been counteracted by the increased availability of operating theatres and CT scanners because of a 25%–50% reduction in elective surgery and fewer trauma patients being admitted to the hospital. 13 , 14 And, all seriously injured trauma patients were assumed to have COVID‐19 and triaged to the RED zone which contained the usual CT scanner, thus this may explain why time to CT was not compromised. 12 The mean time to immediate life‐saving surgery (OPSTAT) was no longer than in previous years, although low numbers require interpretive caution. The mortality rate of major trauma patients was also not different from what was expected (5%–14%), further supporting our claim that quality of care was not compromised during a lockdown.
When COVID‐19 case number began to rise, the median LOS was reduced for patients not at risk of COVID‐19. This could have been because fewer admitted patients meant more available resources, efforts to discharge patients in anticipation of COVID‐19 patients arriving or patients requesting to be discharged due to fear of contracting COVID‐19 in hospital. Conversely, patients at risk of COVID‐19 had significantly longer median LOS during the transition period and wave 2, possibly because clinical teams less familiar with trauma care were treating these patients on the wards; discharge planning became more complex as access to rehabilitation, psychiatric and nursing home bed was reduced due to COVID‐19 restrictions; and delays in being discharged until patients were cleared of COVID‐19. However, even the introduction of rapid genetic testing in July 2020 when test results arrived after 1–2 h compared with 24 h did not make a big impact on the LOS because of other possible setbacks.
The number of patients needing ICU beds was lower than expected during the first wave but no different during the second wave even though the total number of patients treated was similar. Upon examination, our findings during the first wave may be due to an exceptionally high number of ICU admissions from March to May 2017 (Table S1), which artefactually increased the expected numbers during the first wave in 2020. Nevertheless, during the larger second wave, when the hospital was treating critically ill COVID‐19 patients, trauma patients continued to have access to ICU beds and ethically difficult decisions were not needed about which patients should be prioritised to receive scarce resources. 15
Colleagues at the RMH described the impact of COVID‐19 on the day‐to‐day running of the hospital and found it was during the second wave when the service was overwhelmed by redeployed staff; 262 healthcare workers contracted COVID‐19 and 680 staff were furloughed. 16 Workforce shortages meant that staff were taking on extra shifts and working in unfamiliar roles. Trauma patients were admitted based on suspected COVID status, rather than their injury status, meaning they were often cared for by nurses and allied health less familiar with caring for an injured patient. The ED was split into two with patients triaged primarily on suspected COVID‐19 status into a ‘RED’ (Respiratory ED), where all suspected COVID‐19 patients or those unable to be excluded were treated or a NED (Normal ED). All trauma resuscitation areas plus the CT scanner remained in the COVID‐19 hot zone. While this was necessary for workforce protection, it resulted in further dilution of staff and was less flexible in the event of trauma patient under‐triage. Nevertheless, our metrics for quality of care were not compromised.
This study is limited by the fact that it is a single‐centre study; therefore, we cannot know whether the decrease in trauma cases was partly due to patients being triaged to another hospital, or not being transferred from a rural hospital. The Victoria State Trauma System has two adult major trauma services, the RMH and The Alfred Hospital, and many other level 1, 2, 3 and 4 centres throughout Victoria. Although consideration was given to changing ambulance and prehospital retrieval protocols, this was not enacted, and the RMH was never placed on trauma bypass. To fully address this limitation, data linkage studies are needed to see if patients went elsewhere or if numbers were down across the state. Another limitation of this study is that our analysis included several subgroups of trauma with small numbers in each subgroup and we did not adjust for multiple comparisons. Therefore, our findings should be considered hypothesis‐generating. A strength of this study is that it includes a second wave of COVID‐19, allowing us to test and re‐test the relationship between lockdown and changes to healthcare utilisation. Including data from 2016 to 2019 allowed us to factor in fluctuations over time and increase the likelihood that changes observed in 2020 were due to restrictions or changes in behaviour. Nevertheless, we cannot discount the notion that smaller numbers may in part be due to fewer people inhabiting the neighbouring suburbs because flight restrictions limited international students, residents stuck overseas and tourists from entering the country.
The global COVID‐19 pandemic has had an immense impact on the daily functioning of hospitals. Our hospital observed a significant reduction in the presentation of trauma patients, both minor and major trauma victims. Although the demands on clinical staff increased due to workforce shortages and working with PPE, the quality of care was not compromised. As anticipated, motor vehicle and sport‐related incidents decreased, hip fractures did not change, but other mechanisms predicted to decrease such as interpersonal and family violence did not. Although the Royal Melbourne trauma service did not see an increase in family violence admissions, this is by no means a comprehensive assessment, and the well‐being of victims should remain a priority in case of future COVID‐19 surges or other pandemics. Major trauma services need to adapt their models of care without compromising patient safety, balancing the needs of the trauma patient while ensuring the physical and mental health of their staff. For the general population, the significant reduction in motor vehicle crashes and assaults during lockdown suggests there may be long‐term advantages for dispersing or limiting the number of patrons in public places and allowing employees to work from home.
Author contributions
Timothy Fazio: Conceptualization; data curation; resources; writing – review and editing. Kellie Gumm: Data curation; writing – original draft; writing – review and editing. Steven Tong: Conceptualization; formal analysis; writing – review and editing. Leanne Saxon: Formal analysis; methodology; project administration; writing – original draft. David Read: Conceptualization; formal analysis; methodology; project administration; resources; writing – review and editing.
Conflict of interest
None declared.
Supporting information
Table S1. Characteristics of patients presenting with trauma‐related injuries from 16 March 2016 to 11 May 2020.
Table S2. Characteristics of patients presenting with trauma‐related injuries from 12 May 2016 to 7 July 2020.
Table S3. Characteristics of patients presenting with trauma‐related injuries from 8 July 2016 to 10 September 2020.
L. Saxon PhD; T. N. Fazio MBBS, MIS, FRACP, FAIDH; K. Gumm CNC; S. Y. C. Tong MBBS, PhD, FRACP; D. J. Read MBBS, FRACS.
The abstract of this paper was presented at the College of Surgeons, Annual Scientific Congress, 2021
Data availability statement
Data are available upon reasonable request. The study includes deidentified patient data from the Royal Melbourne Hospital, Australia.
References
- 1. Worldometer. COVID‐19 Coronavirus Pandemic. [cited 2021 May 18]. Available from: https://www.worldometers.info/coronavirus/#countries2021
- 2. Wikipedia . COVID‐19 lockdowns. 2021. [cited 2021 Apr 18]. Available from: https://en.wikipedia.org/wiki/COVID-19_lockdowns
- 3. Butt C. Scanning the second waves: how Victoria's COVID‐19 response compares. The Age. October 25, 2020. Melbourne, Australia: Nine Entertainment. [Google Scholar]
- 4. McNamara E, Saxon L, Bond K, Campbell BCV, Douglass J, Dutch MJ, et al. The threat of COVID‐19 impacting on a quaternary healthcare service: a retrospective cohort study of administrative data. BMJ Open. 2021;11:e045975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kamine TH, Rembisz A, Barron RJ, Baldwin C, Kromer M. Decrease in trauma admissions with COVID‐19 pandemic. West J Emerg Med. 2020;21(4):819–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Population Australia Population of Victoria. 2021 [cited 2021 Apr 18]. Available from: http://www.population.net.au/population-of-victoria2021
- 7. Nunez JH, Sallent A, Lakhani K, Guerra‐Farfan E, Vidal N, Ekhtiari S, et al. Impact of the COVID‐19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51(7):1414–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Park C, Sugand K, Nathwani D, Bhattacharya R, Sarraf KM. Impact of the COVID‐19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the "golden month". Acta Orthop. 2020;91(5):556–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pfitzner N, Fitz‐Gibbon K & True J Responding to the ‘shadow pandemic’: practitioner views on the nature of and responses to violence against women in Victoria, Australia during the COVID‐19 restrictions. Monash University: Monash Gender and Family Violence Prevention Centre, Monash University, Melbourne, Australia. 2020.
- 10. Kofman YB, Garfin DR. Home is not always a haven: the domestic violence crises amid the COVID‐19 pandemic. Psychol Trauma. 2020;12:S199–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fielding S. In quarantine with an abuser: surge in domestic violence reports linked to coronavirus. The Guardian. 2020. [cited 2020 Apr 3]. Available from: https://www.theguardian.com/us‐news/2020/apr/03/coronavirus‐quarantine‐abuse‐domestic‐violence
- 12. Read DJ. Perspective. Don't forget trauma patient: lessons from a major trauma and major COVID centre. ANZ J Surg. 2021;91:1055–6. [DOI] [PubMed] [Google Scholar]
- 13. Davey M. Covid‐19 Victoria: hospitals advised to reduce elective surgery as doctors warn of overcrowding [Newspaper]. The Guardian. 2020. [cited 2020 Jul 9]. Available from: https://www.theguardian.com/australia-news/2020/jul/09/covid-19-victoria-hospitals-advised-to-reduce-elective-surgery-as-doctors-warn-of-overcrowding
- 14. Hume M. Elective surgery restrictions reimposed on Melbourne hospitals. Insight News. [updated 2020 Jul 16; cited 2020 Jul 16]. Available from: https://www.insightnews.com.au/elective-surgery-restrictions-reimposed-on-melbourne-hospitals/
- 15. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of Covid‐19. N Engl J Med. 2020;382(21):2049–55. [DOI] [PubMed] [Google Scholar]
- 16. Buising KL, Williamson D, Cowie BC, MacLachlan J, Orr E, MacIsaac C, et al. A hospital‐wide response to multiple outbreaks of COVID‐19 in health care workers: lessons learned from the field. Med J Aust. 2021;214(3):101–4.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of patients presenting with trauma‐related injuries from 16 March 2016 to 11 May 2020.
Table S2. Characteristics of patients presenting with trauma‐related injuries from 12 May 2016 to 7 July 2020.
Table S3. Characteristics of patients presenting with trauma‐related injuries from 8 July 2016 to 10 September 2020.
Data Availability Statement
Data are available upon reasonable request. The study includes deidentified patient data from the Royal Melbourne Hospital, Australia.


