Abstract
Introduction
To investigate type 2 diabetes as a risk factor for COVID‐19 death following hospital admission in Kuwait.
Methods
A retrospective cohort study using data from a central hospital that cared for all hospitalized COVID‐19 patients in Kuwait. We investigated the association between type 2 diabetes, with COVID‐19 mortality using multiply imputed logistic regression and calculated the population attributable fraction.
Results
A total of 5333 patients were admitted with COVID‐19, of whom 244 died (4.6%). Diabetes prevalence was 24.8%, but 53.7% of those who died had diabetes. After adjusting for age, sex, ethnicity and other comorbidities, diabetes was associated with death (OR 1.70 [95% CI 1.23, 2.34]) and admission to the intensive care unit more than 3 days after initial admission (OR 1.78 [95% CI 1.17, 2.70]). Assuming causality, the population attributable fraction for type 2 diabetes in COVID‐19 death was 19.6% (95% CI 10.8, 35.6).
Conclusion
Type 2 diabetes is a strong risk factor for COVID‐19 death in the Middle East. Given the high prevalence of type 2 diabetes in the Middle East, as well as many Western countries, the public health implications are considerable.
Keywords: COVID‐19, death, diabetes
Type 2 diabetes is a strong risk factor for COVID‐19 death in the Middle East. Given the high prevalence of type 2 diabetes in the Middle East, as well as many western countries, the public health implications are considerable.
1. INTRODUCTION
The COVID‐19 pandemic 1 has led to efforts to identify people at greatest risk including older age groups, those with comorbidities such as type 2 diabetes and cardiovascular disease (CVD), poor oxygen saturation and elevated markers of inflammation. 2 , 3 , 4 The association of type 2 diabetes with poor outcomes is of particular interest, 5 since it is a risk factor that is potentially amenable to public health interventions.
Kuwait faces specific challenges in terms of health care, due to the high burden of obesity, poor lifestyle and type 2 diabetes. Specifically, prevalence of type 2 diabetes in older adults is around 25% and obesity 40%–50%. 6 , 7 Previous studies and a systematic review have shown that the issue of incidence and clinical management of type 2 diabetes in Kuwait and the Middle East in general is complicated by several lifestyle and cultural circumstances including low levels of habitual physical activity, peer and family pressure to consume a poor diet and poor medication adherence. 8 For instance, a hot climate, as well as lack of facilities and infrastructure to promote physical activity (such as pavements and walking routes), high traffic volume and cultural expectations surrounding PA behaviour among women are highly impactful. 9 This raises the question of whether diabetes is a particular risk factor for poor COVID‐19 outcomes in the Middle East, since the severity and prevalence of type 2 diabetes is distinct in this area of the world. One recent study specifically in people with type 2 diabetes in Kuwait suggests that diabetes patients with COVID‐19 have poor clinical prognosis. 10
We have previously reported demographic and clinical data on the first consecutive 1096 patient to be admitted to hospital with COVID‐19 in Kuwait, 11 and here, we expand to make use of this resource. Specifically, our objective was to investigate the importance of type 2 diabetes as a risk factors for COVID‐19 death in Kuwait, compared with the general population and report the population attributable fraction (PAF) for type 2 diabetes.
2. METHODS
2.1. Study population
This retrospective cohort study included a single cohort of adult and paediatric inpatients admitted to Jaber Al Ahmad Al Sabah hospital, the largest tertiary hospital with 1240 bed capacity, and has been named the dedicated COVID‐19 hospital by Ministry of Health for Kuwaiti residents and visitors with diagnosis of COVID‐19 based on a positive PCR testing. Mandatory health insurance is required for all expatriates in Kuwait and is enforced through residency requirements. The present cohort included those who were admitted between 24/02/20 and 15/07/20. In line with strengthening the reporting of observational studies in epidemiology (STROBE) guidance, as data were obtained through routinely collected available data, no post hoc power calculation has been performed. All patients with a positive RT‐PCR test were admitted to Jaber Al Ahamd Al Sabah hospital. All patients in this study had a confirmed diagnosis of COVID‐19 based on a positive result of RT‐PCR assay of nasal and/or nasal and pharyngeal swabs, in accordance with WHO interim guidance. The data are derived from in‐hospital databases used during routine care as previously described. 11 Ethical approval for use of the data was obtained by the standing committee for coordination of health and medical research in the ministry of health in Kuwait (IRB 2020/1400).
2.2. Outcome of interest
The primary outcome was death from COVID‐19, from the death certificate, which was matched to patients' hospital file numbers and study numbers using the Kuwaiti national Civil ID number, a unique number given to all residents. A secondary outcome was transfer to the intensive care unit (ICU) during COVID‐related hospitalization; this secondary outcome was only explored in patients who were not admitted to intensive care in the first 3 days following general admission.
2.3. Exposures of interest
Exposures of interest included age, sex, nationality and ethnicity, smoking status and clinical comorbidities, including type 2 diabetes. Vitals taken on admission included temperature, pulse, respiratory rate and oxygen saturation, systolic and diastolic blood pressure and body mass index. Laboratory biomarkers variables considered in the present study included routinely measured (as standard of care) platelet count, white blood cell count, estimated glomerular filtration rate (eGFR) and liver functions tests (gamma‐glutamyl transferase [GGT], alanine transaminase [ALT] and aspartate aminotransferase [AST]) as well as C‐reactive protein (CRP) and urea. Clinical vitals and biomarkers of interest were measured within seven days of admission.
2.4. Statistical analyses
Associations between exposures and outcomes of interest were first explored using a complete case analysis. All tests were performed in R using version 4.0.2. We then implemented and reported an analysis based on multiple imputations by chained equations (MICE) as part of the ‘mice’ R package. 12 The imputation methods were predictive mean matching for continuous variables and proportional odds models for ordered factor variables. The number of iterations for each permutation was 10, with 10 permutations performed. Convergence was checked using plots. Pooled confidence intervals were derived using Wald method with pooled estimates and SEs. We reported two models, the first including age, sex, ethnicity and baseline comorbidities. The second model also included clinical vitals and admission and biomarkers of interest. Logistic regression using the multiple imputation data sets was implemented, using model development as detailed above. Additionally, for the first, simpler, model for the mortality outcome, analyses were stratified by median age (43 years) and sex. PAFs were derived for comorbidities using model 1, as above, using the ‘AF’ R package. 13
3. RESULTS
Between 24/02/20 and 15/07/20, 5333 patients were admitted to hospital with confirmed COVID‐19. Nearly, two thirds of admission occurred between April and May 2020 (Figure 1). Patients admitted to hospital had mean age 44.2 (standard deviation [SD] 17.2) and were more often male sex (64.3%). Patient nationality was Kuwaiti in 55.8% of patients, and ethnicity was Arab in 67.1% and South Asian in 31.0%. Type 2 diabetes was diagnosed in 1317 patients (24.8%) and hypertension in 1417 (26.7%). Of the 5333 patients who were admitted, 244 died (4.6%). Type 2 diabetes prevalence in hospitalized patients was 24.8%, but 53.7% of those who died had type 2 diabetes (Figure 2). In addition, COVID‐19 death was more common in older patients (those who died were 15 years older than those who survived) in men and non‐Kuwaitis (Table 1).
FIGURE 1.
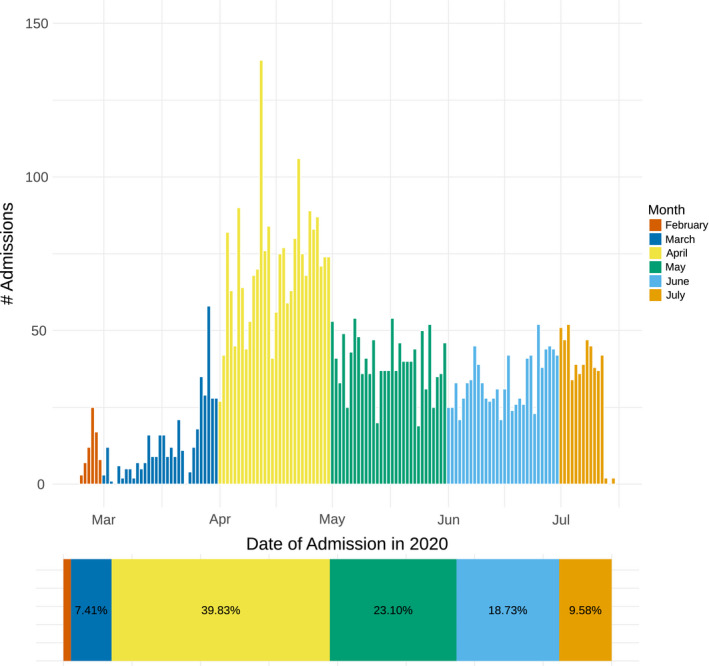
Temporal pattern of admission to Jaber Al Ahmad Al Sabah hospital for 5333 patients with PCR positive COVID‐19 between 24/02/20 and 15/07/20
FIGURE 2.
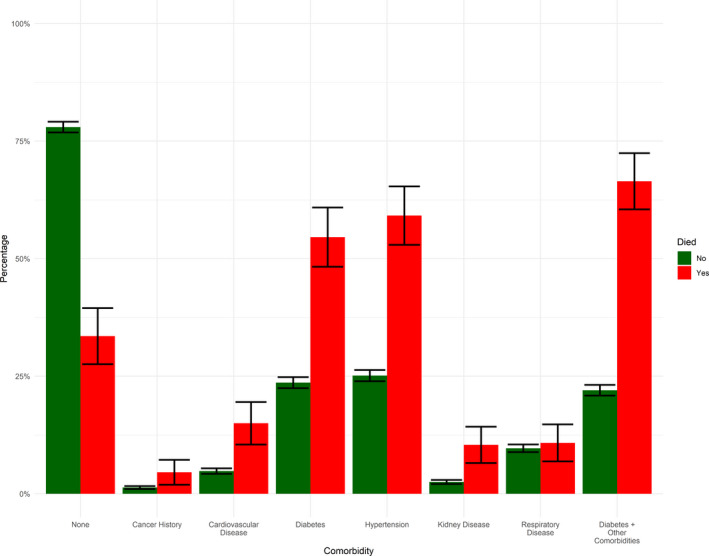
Proportion of patients with selected comorbidities, separately by COVID‐19 death status
TABLE 1.
Demographics and comorbidities by COVID‐19 death status
| Demographics |
Alive 5089 (95.4%) |
Died 244 (4.6%) |
|---|---|---|
| Male sex | 3243 (63.8%) | 187 (76.6%) |
| Age (years) | 43.5 (17.1) | 58.8 (13.4) |
| Nationality | ||
| Kuwaiti | 2851 (56.4%) | 107 (44.0%) |
| Other (40 Nationalities + ‘Other’) | 2205 (43.6%) | 136 (56.0%) |
| Missing | 33 | 1 |
| Ethnicity | ||
| African/Black | 27 (0.5%) | 1 (0.4%) |
| Arab | 3410 (67.5%) | 143 (58.6%) |
| Caucasian | 60 (1.2%) | 4 (1.6%) |
| East Asian | 6 (0.1%) | 1 (0.4%) |
| South Asian | 1547 (30.6%) | 95 (38.9%) |
| Missing | 39 | 0 |
| Type 2 diabetes | 1186 (23.4%) | 131 (54.6%) |
| Cardiovascular disease | 245 (4.8%) | 36 (15.0%) |
| Cancer history | 68 (1.3%) | 11 (4.6%) |
| Hypertension | 1275 (25.1%) | 142 (59.2%) |
| Kidney disease | 128 (2.5%) | 25 (10.4%) |
| Respiratory disease | 491 (9.7%) | 26 (10.8%) |
Of the 4860 patients at risk (excluding 473 patients who were admitted to ICU within 3 days of general admission), 133 (2.7%) progressed to ICU admission. Of those admitted to ICU, 51.9% had type 2 diabetes.
In multivariable models including simple demographics and comorbidities, age was strongly independently associated with death, as was male sex and South Asian ethnicity (Table 2). Comorbidities associated with death were type 2 diabetes, cancer, cardiovascular disease and renal disease; the association for type 2 diabetes was strong (OR 1.70). There was no interaction between ethnicity, or other comorbidities, and type 2 diabetes in the association with death. Stratifying separately by age and sex found stronger associations between type 2 diabetes and mortality in those aged ≤43 years (OR 2.70 vs 1.59; P‐for interaction = .0178) and females (OR 3.57 vs 1.40; P‐for interaction = .16) (Table 3). In the second adjustment model, type 2 diabetes was not associated with death after adjusting for additional clinical and laboratory variables (low oxygen saturation, high urea, high CRP, high neutrophil count, liver function tests (AST, ALT, GGT), eGFR and low platelet count) (OR 1.08; 95% CI 0.71–1.66). Risk associations were generally weaker for ICU admission, but type 2 diabetes remained a significant risk factor (Table 2).
TABLE 2.
Multivariable demographic and comorbid predictors of COVID‐19 death and ICU admission among COVID‐19 admissions in Kuwait
|
Death from COVID‐19 N = 5333, n deaths =244 |
ICU admission (after 3 days) N = 4860, n admissions =133 |
|
|---|---|---|
| Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Age (years) | 1.05 (1.04, 1.06) | 1.05 (1.04, 1.06) |
| Sex | ||
| Female (ref) | 1.00 | 1.00 |
| Male | 2.04 (1.46, 2.84) | 1.33 (0.91, 1.95) |
| Ethnicity | ||
| Arab (ref) | 1.00 | 1.00 |
| South Asian | 3.09 (2.21, 4.33) | 0.90 (0.55, 1.48) |
| Other | 1.93 (0.78, 4.76) | 0.86 (0.20, 3.63) |
| Type 2 diabetes | 1.70 (1.23, 2.34) | 1.78 (1.17, 2.70) |
| Cardiovascular disease | 1.23 (0.81,1.87) | 1.00 (0.55, 1.82) |
| Cancer history | 3.10 (1.52, 6.31) | 1.34 (0.46, 3.88) |
| Hypertension | 1.69 (1.20, 2.38) | 0.83 (0.53, 1.30) |
| Kidney disease | 2.37 (1.45, 3.89) | 1.17 (0.51, 2.66) |
| Respiratory disease | 1.39 (0.89, 2.18) | 2.03 (1.26, 3.25) |
TABLE 3.
Stratified analysis exploring risk factors for COVID‐19 death stratified by median age and sex
|
Death from COVID‐19 N = 5333, n deaths = 244 |
||||
|---|---|---|---|---|
|
Aged ≤43 years N = 2681, Deaths = 30 |
Aged >43 years N = 2650, Deaths = 214 |
Female N = 1901, Deaths = 57 |
Male N = 3430, Deaths =187 |
|
| Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Age (years) | 1.11 (1.03, 1.20) | 1.04 (1.02, 1.05) | 1.05 (1.02, 1.07) | 1.05 (1.04, 1.07) |
| Sex | ||||
| Female (ref) | 1.00 | 1.00 | – | – |
| Male | 1.27 (0.49, 3.24) | 2.15 (1.51, 3.07) | – | – |
| Ethnicity | ||||
| Arab (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| South Asian | 3.26 (1.31, 8.12) | 2.81 (1.94, 4.07) | 3.43 (1.50, 7.84) | 3.03 (2.09, 4.40) |
| Other | 6.77 (1.29, 35.62) | 1.27 (0.43, 3.71) | 3.72 (0.45, 30.63) | 1.70 (0.63, 4.56) |
| Type 2 diabetes | 2.70 (0.96, 7.60) | 1.59 (1.15, 2.21) | 3.57 (1.74, 7.31) | 1.40 (0.97, 2.02) |
| Cardiovascular disease | 1.71 (0.24, 12.48) | 1.24 (0.81, 1.89) | 2.09 (1.00, 4.34) | 1.00 (0.60, 1.66) |
| Cancer history | 33.58 (5.85, 192.67) | 2.26 (1.06, 4.81) | 1.60 (0.36, 7.10) | 4.11 (1.76, 9.60) |
| Hypertension | 1.99 (0.68, 5.84) | 1.54 (1.10, 2.17) | 0.78 (0.38, 1.60) | 2.06 (1.41, 3.01) |
| Kidney disease | 18.73 (4.95, 70.84) | 1.87 (1.10, 3.18) | 2.29 (0.93, 5.64) | 2.31 (1.28, 4.17) |
| Respiratory disease | 2.13 (0.57, 7.94) | 1.28 (0.79, 2.06) | 1.47 (0.74, 3.00) | 1.27 (0.69, 2.34) |
Estimating PAFs for death, point estimates were 19.6% (95% CI 10.8, 35.6) for type 2 diabetes, 2.7% (95% CI 1.0, 6.8) for cancer, 2.1% (95% CI 0.2, 22.2) for cardiovascular disease, 21.9% (95% CI 11.6, 41.3) for hypertension, 5.0% (95% CI 2.3, 10.8) for kidney disease and 2.4% (95% CI 0.4, 13.5) for respiratory disease.
4. DISCUSSION
Although Kuwait has a population with a high prevalence of type 2 diabetes and obesity, death rates from COVID‐19 were comparable to or lower than those reported in other parts of the world. 14 , 15 Despite this, type 2 diabetes appears to be an important risk factor for COVID‐19 death. Type 2 diabetes was associated with 70% increased odds of in‐hospital COVID‐19 death, and assuming causality, the PAF for COVID‐19 death caused by type 2 diabetes was 19.6%. Our data suggest that type 2 diabetes is an important, and potentially modifiable, driver of COVID‐19 deaths, and is of particular concern in countries with high prevalence of the condition.
The association between type 2 diabetes and COVID‐19 death observed in the current study (adjusted OR 1.70) is similar to that reported in a national study from England and Wales (adjusted OR 1.80). 16 This indicates that the condition increases risk by approximately the same proportion in both countries, and therefore, mechanisms linking the condition to increased COVID‐19 severity are probably similar. However, the burden of type 2 diabetes in Kuwait is considerable, and more than 50% of those who died of COVID‐19 in Kuwait had diabetes (in contrast to 31% in the study in England and Wales 16 ). This leads to a substantial COVID‐19 PAF associated with diabetes in Kuwait. The association of type 2 diabetes with poor outcomes was explained by poor respiratory function, elevated inflammatory markers, worse renal function and elevated liver enzymes at presentation. This suggests that type 2 diabetes leads to more severe multi‐organ disease at presentation, which then leads to worse outcomes.
Kuwait is in the process of undertaking public health initiatives to lower obesity and diabetes prevalence. 17 These results support the need for public health campaigns in countries with high type 2 diabetes burden to support weight loss initiatives. 2 , 18 , 19 Whilst we lack trial evidence to prove weight loss lowers risk of severe COVID‐19, weight loss can lead to remission of type 2 diabetes, 20 and there are many additional health benefits of weight loss.
Limitations of this study include some missingness due to use of real‐world data, although we were able to use multiple imputation. There is also likely to be a burden of undiagnosed type 2 diabetes within this population; our estimates may be underestimates. We acknowledge that admission ‘criteria’ for COVID‐19 are not standardised across times or healthcare practitioners, and therefore, there may be some biases in terms of hospital admission being representative of case severity across time. As these are observational data, caution must be used in making causal inferences.
In summary, these data emphasize the importance of type 2 diabetes as a risk factor for COVID‐19 death in an Arab country, and reiterate the public health importance of lessening diabetes rates in the Middle East. People with diabetes should be considered candidates for vaccine prioritization.
CONFLICT OF INTEREST
PW has received research grants from Roche Diagnostics, AstraZeneca and Boehringer Ingelheim outside the submitted work, and NS has received grant and personal fees from Boehringer Ingelheim and personal fees from Amgen, AstraZeneca, Eli Lilly, Merck Sharp & Dohme, Novartis, Novo Nordisk, Pfizer and Sanofi outside the submitted work; all authors declare no other relationships or activities that could appear to have influenced the submitted work.
AUTHOR CONTRIBUTIONS
EA‐O, YH, LA, NV, JAK, DA‐S, AAO, AH and FAM contributed to conception and data acquisition as well as interpretation of the data and critically revised the manuscript for important intellectual content. YH and NV cleaned the clinical data prior to statistical analysis. SVK, SRG, JMRG, CAC‐M and NS contributed to study design, analysis and interpretation of the data and critically revised the manuscript for important intellectual content. RB conducted statistical analyses and with PW contributed to conception and interpretation of the data and wrote the first draft. EA‐O is the guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.
ETHICAL APPROVAL
Ethical approval for use of the data was obtained by the standing committee for coordination of health and medical research in the ministry of health in Kuwait (IRB 2020/1400).
ACKNOWLEDGEMENTS
We would like to thank the IT department, Internal medicine, intensive care, director of the hospital and area director of Jaber Al Ahmad Al Sabah hospital, Kuwait. We would like to thank the Nursing Unit at the Dasman Diabetes Institute. The authors thank Liz Coyle (University of Glasgow) for her assistance in the preparation of this article.
Al‐Ozairi E, Brown R, Hamdan Y, et al. Risk of mortality among inpatients with COVID‐19 and type 2 diabetes: National data from Kuwait. Endocrinol Diab Metab. 2021;4:e287. 10.1002/edm2.287
Ebaa Al‐Ozairi and Rosemary Brown are joint first authors.
Funding information
The work in this study is supported by the British Heart Foundation Centre of Research Excellence Grant RE/18/6/34217. RB is supported by Medical Research Council Doctoral Training Programme studentship in Precision Medicine (MR/N013166/1). Work was supported by the Ministry of Health, Kuwait, the Kuwait Foundation for Advancement of Science (KFAS), and Dasman Diabetes Institute, Kuwait. SVK acknowledges funding from the NRS Senior Clinical Fellowship (SCAF/15/02), Medical Research Council (MC_UU_00022/2) and Scottish Government Chief Scientist Office (SPHSU17)
DATA AVAILABILITY STATEMENT
The raw data of the study can be provided upon request with maintenance of confidentiality, privacy and anonymity of the participants and abiding to ethical board regulations.
REFERENCES
- 1. World Health Organization . 2020. Coronavirus disease 2019 (COVID‐19) situation report‐76 s. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200405-sitrep-76-covid-19.pdf?sfvrsn=6ecf0977_4. Accessed Nov 19, 2020.
- 2. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Banerjee A, Pasea L, Harris S, et al. Estimating excess 1‐ year mortality from COVID‐19 according to underlying conditions and age in England: a rapid analysis using NHS health records in 3.8 million adults. Lancet. 2020;395:1715‐1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City Area. JAMA. 2020;323:2052‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dennis JM, Mateen BA, Sonabend R, et al. Type 2 diabetes and COVID‐19‐related mortality in the critical care setting: a national cohort study in England, March‐July 2020. Diabetes Care. 2021;44(1):50‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Channanath AM, Farran B, Behbehani K, Thanaraj TA. State of diabetes, hypertension, and comorbidity in Kuwait: showcasing the trends as seen in native versus expatriate populations. Diabetes Care. 2013;36(6):e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mokdad AH, El Bcheraoui C, Afshin A, et al. Burden of obesity in the Eastern Mediterranean Region: findings from the Global Burden of Disease 2015 study. Int J Public Health. 2018;63(Suppl 1):165‐176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. lsairafi ZK, Taylor KM, Smith FJ, Alattar AT. Patients' management of type 2 diabetes in Middle Eastern countries: review of studies. Patient Prefer Adherence. 2016;10:1051‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sharara E, Akik C, Ghattas H, et al. Physical inactivity, gender and culture in Arab countries: a systematic assessment of the literature. BMC Public Health. 2018;18:639‐739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alshukry A, Bu Abbas M, Ali Y, et al. Clinical characteristics and outcomes of COVID‐19 patients with diabetes mellitus in Kuwait. Heliyon. 2021;7(4):e06706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Almazeedi S, Al‐Youha S, Jamal MH, et al. Characteristics, risk factors and outcomes among the first consecutive 1096 patients diagnosed with COVID‐19 in Kuwait. EClinicalMedicine. 2020;24:100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Buuren S, Groothuis‐Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1‐67. [Google Scholar]
- 13. Dahlqwist E, Sjolander A. Package ‘AF’. https://cran.r‐project.org/web/packages/AF/AF.pdf. Accessed Mar 02, 2021.
- 14. Horwitz LI, Jones SA, Cerfolio RJ, et al. Trends in COVID‐19 risk‐adjusted mortality rates. J Hosp Med. 2021;16(2):90‐92. [DOI] [PubMed] [Google Scholar]
- 15. Dennis JM, McGovern AP, Vollmer SJ, Mateen BA. Improving survival of critical care patients with coronavirus disease 2019 in England: a national cohort study, March to June 2020. Crit Care Med. 2021;49(2):209‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID‐19‐related mortality in England: a whole‐population study. Lancet Diabetes Endocrinol. 2020;8(10):813‐822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Weiderpass E, Botteri E, Longenecker JC, et al. The prevalence of overweight and obesity in an adult Kuwaiti population in 2014. Front Endocrinol (Lausanne). 2019;10:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020;28(7):1195‐1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Collaborative TO, Williamson E, Walker AJ, et al. OpenSAFELY: factors associated with COVID‐19‐related hospital death in the linked electronic health records of 17 million adult NHS patients. Nature. 2020;584(7821):430‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lean MEJ, Leslie WS, Barnes AC, et al. Durability of a primary care‐led weight‐management intervention for remission of type 2 diabetes: 2‐year results of the DiRECT open‐label, cluster‐randomised trial. Lancet Diabetes Endocrinol. 2019;7(5):344‐355. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data of the study can be provided upon request with maintenance of confidentiality, privacy and anonymity of the participants and abiding to ethical board regulations.


