Summary
The outbreak of the novel coronavirus disease 2019 (COVID‐19) changed lifestyles worldwide and subsequently induced individuals’ sleep problems. Sleep problems have been demonstrated by scattered evidence among the current literature on COVID‐19; however, little is known regarding the synthesised prevalence of sleep problems (i.e. insomnia symptoms and poor sleep quality) for males and females separately. The present systematic review and meta‐analysis aimed to answer the important question regarding prevalence of sleep problems during the COVID‐19 outbreak period between genders. Using the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guideline and Newcastle–Ottawa Scale checklist, relevant studies with satisfactory methodological quality searched for in five academic databases (Scopus, PubMed Central, ProQuest, Web of Science , and EMBASE) were included and analysed. The protocol of the project was registered in the International Prospective Register of Systematic Reviews (PROSPERO; identification code CRD42020181644). A total of 54 papers (N = 67,722) in the female subgroup and 45 papers (N = 45,718) in the male subgroup were pooled in the meta‐analysis. The corrected pooled estimated prevalence of sleep problems was 24% (95% confidence interval [CI] 19%–29%) for female participants and 27% (95% CI 24%–30%) for male participants. Although in both gender subgroups, patients with COVID‐19, health professionals and general population showed the highest prevalence of sleep problems, it did not reach statistical significance. Based on multivariable meta‐regression, both gender groups had higher prevalence of sleep problems during the lockdown period. Therefore, healthcare providers should pay attention to the sleep problems and take appropriate preventive action.
Keywords: COVID‐19, gender, insomnia, prevalence, sleep
1. INTRODUCTION
The outbreak of the novel coronavirus disease 2019 (COVID‐19) changed most people’s lifestyles globally. Indeed, many countries and governments used different policies (e.g. city lockdown, boarder control, online teaching, and special distancing) to slow down the COVID‐19 infection rate (Chen et al., 2020; Chen, Chen et al., 2021); as COVID‐19 was found to have an extraordinary transmission rate and cause an alarming number of deaths (Ahorsu, Lin, Imani et al., 2020; Mamun et al., 2021). With the high prevalence and level of mortality (WHO, 2020), COVID‐19 has impacted peoples psychological health. Indeed, numerous studies have found that COVID‐19 together with the reactions toward controlling COVID‐19 infection are associated with different aspects of psychological health, including depression, anxiety, stress, and sleep problems (Ahorsu, Lin, & Pakpour, 2020; Chang et al., 2020; Lin, Broström et al., 2020, Lin, Imani et al., 2020).
Among the psychological health aspects, sleep is one of the major concerns for healthcare providers (Pakpour et al., 2020) for the following reasons. First, sleep is an essential component for individuals having effective cognitive and emotional processing, and a good night’s sleep is proposed to be vital for all people (Garbarino et al., 2016; Kopasz et al., 2010; Tarokh et al., 2016; Yaffe et al., 2014). Second, ample evidence has shown that sleep is a key factor for individuals maintaining satisfactory and good health, including physical functioning, mental functioning, social functioning, spiritual functioning, and overall quality of life (Garbarino et al., 2016; Gradisar et al., 2008; Shochat et al., 2014). Third, an association between good sleep and health behaviours have been proposed (Lin, Strong et al., 2018, Lin, Lin et al., 2018). However, individuals living in the modern world have different obstacles for achieving good sleep (Strong et al., 2018), given that the technology today contributes to sleep disturbance (Alimoradi et al., 2019). Moreover, recent research shows that problematic social media use, a behaviour found to have increased during the COVID‐19 outbreak (Hashemi et al., 2020; Lin, Broström et al., 2020), is associated with poor sleep (Wong et al., 2020). In short, there is a need to investigate in‐depth the sleep problems occurring during the COVID‐19 outbreak period.
The available literature on COVID‐19 shows the findings of sleep problems. Zhang, Zhang et al. (2020) studied sleep problems amongst healthcare workers and found different prevalence rates of insomnia between non‐medical healthcare workers (e.g. volunteers in the hospital, medical students, and community workers; prevalence of 38.4%) and medical healthcare workers (e.g. medical doctors and nurses; prevalence of 30.5%). Wang, Song et al. (2020) also examined sleep problems in four populations and found different prevalence rates as well. The prevalence of sleep problems among medical staff was 66.1%, in non‐medical staff was 47.8%, in frontline healthcare providers was 68.1%, and in non‐frontline healthcare providers was 64.5%. Although the information on sleep problems during the COVID‐19 outbreak period has been studied and reported, healthcare providers need synthesised information regarding sleep problems across gender. However, to the best of the present authors’ knowledge, no empirical studies have focussed on the sleep problems between genders during the COVID‐19 pandemic, although the studies have controlled for gender in their statistical analyses.
Gender is an important issue for sleep because different treatments may be designed or used for different genders. More specifically, prior evidence has shown that males and females have different processes in brain functions (Xin et al., 2019). Therefore, males and females may not always share the same values on everything. For example, prior research indicates that males as compared with females appreciate physical activity more (Ou et al., 2017). Additionally, males and females report different levels of psychological health (including quality of life) from children and older people (Lin et al., 2016; Su et al., 2013). Therefore, it is important for healthcare providers to understand sleep problems separately for males and females during the COVID‐19 outbreak period.
To answer the important question regarding prevalence of sleep problems during the COVID‐19 outbreak period across gender, the present study was designed and conducted as a systematic review and meta‐analysis. With the robust methods used in the present review, information on sleep problems across gender were synthesised and should assist healthcare providers in understanding the impacts of the COVID‐19 outbreak on sleep.
2. METHODS
This systematic review is reported based on the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guideline (Moher et al., 2010), a systematic literature search was done in five academic databases, relevant studies were abstracted, and their methodological quality was assessed using the Newcastle–Ottawa Scale (NOS) checklist. Findings were synthesised using a meta‐analysis approach. Results of the present paper are part of the findings from a larger project, the protocol of this project was registered in the International Prospective Register of Systematic Reviews (PROSPERO; identification code CRD42020181644) (Alimoradi & Pakpour, 2020).
2.1. Search strategy
Five academic databases including Scopus, PubMed Central, ProQuest, Web of Science (WoS), and the Excerpta Medica dataBASE (EMBASE) were searched systematically. The search terms were extracted from published reviews and primary studies besides PubMed Medical Subject Headings (MeSH). Specifically, the Patient‐problem, Exposure, Comparison, and Outcome (PECO) framework was used to determine search terms. In this regard, the “patient‐problem” was any human population, the “exposure” was COVID‐19 pandemic with a variety of factors contributing to sleep problems (including stress, reduced light exposure, extended working hours, and changed lifestyle), the “comparison” was none given that all the populations were impacted by exposure to the COVID‐19 pandemic, and the “outcome” was sleep. The main search terms were sleep and COVID‐19. The Boolean search method (AND/OR/NOT) was used to develop the search query. Search syntax was customised based on the advanced search attributes of each database. The search strategy is provided as Additional File 1. Additionally, reference lists of included studies were searched to increase the likelihood of retrieving relevant empirical studies.
2.2. Inclusion criteria
Observational studies, including case‐control and cross‐sectional studies, were included if relevant data relationships were reported. English, peer‐reviewed papers published between December 2019 and February 2021 were included. However, the papers were further screened to ensure that the data collection period was during the COVID‐19 pandemic or COVID‐19 endemic in mainland China. No limitation was imposed regarding participants characteristics. Sleep problems as primary outcomes should have been assessed using valid and reliable scales. Specifically, sleep problems defined in the present review are insomnia symptoms (assessed using Insomnia Severity Index [ISI] and Athens Insomnia Scale [AIS]) and poor sleep quality (assessed using Pittsburgh Sleep Quality Index [PSQI]).
2.2.1. Primary outcome
Gender‐specific estimation of sleep problems prevalence during the COVID‐19 pandemic was the primary outcome.
2.2.2. Secondary outcomes
Assessing the heterogeneity and its possible sources.
Influencing variables (e.g. age and marital status) in gender‐specific sleep problems prevalence during the COVID‐19 pandemic.
2.3. Study screening and selection
In the first step, the title and abstract of all retrieved papers were screened based on the inclusion criteria. The full texts of potentially relevant studies were further examined based on the aforementioned criteria. In this process, relevant studies were selected.
2.4. Quality assessment
The NOS was used to evaluate the methodological quality of the studies in observational studies. Three characteristics of selection, comparability, and outcome are examined with the NOS checklist. The checklist has three versions for evaluating cross‐sectional studies (seven items), case‐control (eight items), and cohort (eight items). Despite a slight difference in number and content of items, each item is rated with a star, except the comparability that can have two stars, thus resulting in a maximum score of 9. Studies with <5 points are classified as having a high risk of bias (Luchini et al., 2017). No studies were excluded based on the quality. But subgroup analysis was conducted to assess the impact of quality on pooled effect size.
2.5. Data extraction
A pre‐designed form was prepared to extract data from included studies. Data including first author’s name, collection date, study design, country, number of participants, gender, mean age, scale used to assess sleep problems, numerical results regarding the frequency of sleep problems. In the process of data extraction, two Excel sheets were initially designed, with one summarising the features of the included studies (e.g. author name and publication year) and the other evaluating methodological quality. The required data from the articles were later entered into another Excel datasheet for coding and preparing for analysis using STATA statistical software.
It should be noted that study selection, quality assessment, and data extraction were processes performed independently by two reviewers. In whole processes (i.e. study selection, quality assessment, and data extraction) disagreements were resolved through discussion by two independent reviewers. A third party was not required to resolve disagreements between the two independent reviewers because there were only minor disagreements, and both reviewers easily reached a consensus.
2.6. Data synthesis
A quantitative synthesis using STATA software version 14 was conducted. Meta‐analysis was run using a random effect model, as it was proposed that included studies were taken from different populations both within‐ and between‐study variances should be accounted for (Hox & Leeuw, 2003). The Q Cochrane statistic was used to assess heterogeneity. Also, the severity of heterogeneity was estimated using the I 2 index. Heterogeneity is interpreted as mild when I 2 is <25% and is considered moderate when I 2 is 25%–50%, and severe heterogeneity is diagnosed when I 2 is 50%–75%. An I 2 >75% is considered to have very severe heterogeneity (Huedo‐Medina et al., 2006).
Prevalence of sleep problems was the selected key measure for the present study. This pooled estimate of this key measure with 95% confidence interval (CI) is reported. Subgroup analysis or meta‐regression was done to find possible sources of heterogeneity and influencing variables on gender‐specific sleep problems prevalence. Funnel plot and the Begg's test were used to assess publication bias (Rothstein et al., 2005). Potential publication bias was corrected with the “fill‐and‐trim” method (Duval & Tweedie, 2000). The “Jackknife” method was used for sensitivity analysis (Hedges & Olkin, 2014).
3. RESULTS
3.1. Study screening and selection process
The initial search of the five databases resulted in 7,263 studies: Scopus (n = 2,518), WoS (n = 474), PubMed (n = 338), EMBASE (n = 1,426), and ProQuest (n = 2,507). After removing duplicate papers, a further 5,647 papers were screened based on title and abstract. Finally, 555 papers appeared to be potentially eligible and their full texts were reviewed. In this process, 54 studies in the female subgroup and 45 studies in the male subgroup met the eligibility criteria and were pooled in the meta‐analysis. Figure 1 shows the search process based on the PRISMA flowchart.
FIGURE 1.
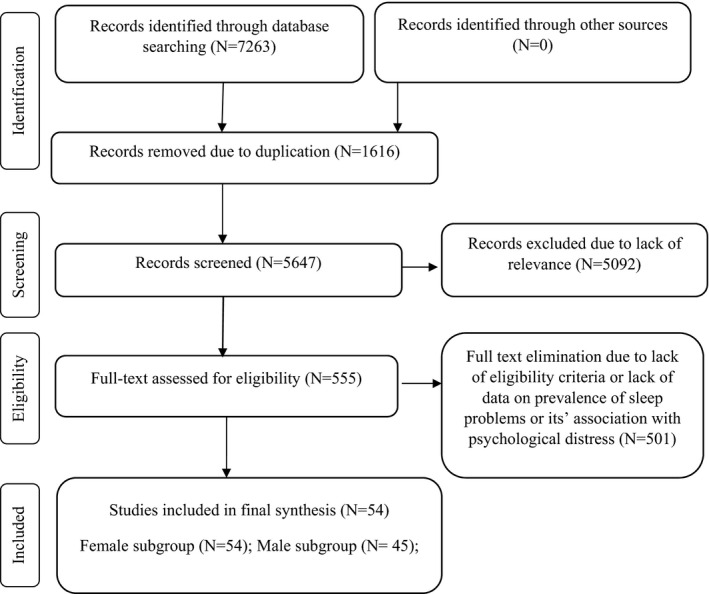
Search process based on the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flowchart
4. MALE SUBGROUP
4.1. Study description
A total of 45 papers with 45,718 participants from 13 countries (China [38,545 participants], Italy [2717], Austria [475], Turkey [480], Bangladesh [223], Pakistan [406], Greece [40], India [340], Belgium, [81] Egypt [133], Saudi Arabia [295], UK [45], and Iran [1,314]) were included. Four papers gathered data during the lockdown period. The smallest sample size was 12, and the largest was 27,149. The individual country with the most eligible studies was China (N = 23). The mean age of participants varied from 15.5 to 70 years and ~65.9% were married. Most studies involved the general population (24 studies), with others involving health professionals (14), and patients with COVID‐19 (seven). Most of the studies were cross‐sectional (43 studies). The two remaining studies had a longitudinal design and collected data during the COVID‐19 pandemic and baseline data were extracted. The ISI and PSQI were used to assess sleep problems (in 25 and 14 studies, respectively). Considering NOS >5 as high quality, 71% of the included studies (32 papers) were categorised as high‐quality. Table 1 provides the summary characteristics of the included studies.
TABLE 1.
Summarised characteristics of included studies
| ID | Authors | Year | Country | Collection date | Lockdown period | Design | Participant group | Sample size, n | Sex, % female | % Married | Age, years mean/range | NOS | Sleep problem scale |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | Zhang (Zhang, Yang et al., 2020) | 2020 | China | January 29–February 3, 2020 | no | cross‐sectional | medical staff | 1,563 | 82.73 | 63.92 | 18–>60 | 5 | ISI |
| 5 | Huang (Huang & Zhao, 2020) | 2020 | China | February 3–10, 2020 | no | cross‐sectional | volunteer population | 603 | 69 | 36.5 | 5 | PSQI | |
| 28 | Fu (Fu et al., 2020) | 2020 | China | February 18–28, 2020 | no | cross‐sectional | Wuhan residents | 1,242 | 69.73 | 33.7 | >18 | 5 | AIS |
| 30 | Zhang (Zhang, Zhang et al., 2020) | 2020 | China | February 19–March 20, 2020 | no | longitudinal surveys | college students | 66 | 62.12 | 20.70 | 5 | PSQI | |
| 32 | Li (Zhou, Shi et al., 2020) | 2020 | China | April 25–May 9, 2020 | no | cross‐sectional | workers with income losses | 398 | 49.5 | 49.5 | 18–>40 | 9 | ISI |
| 34 | Wang (Wang, Xie et al., 2020) | 2020 | China | January 30–February 7, 2020 | no | cross‐sectional | medical workers | 123 | 90 | 30.08 | 33.75 | 6 | PSQI |
| 35 | Hu (Giardino et al., 2020) | 2020 | China | March 7–24, 2020 | no | cross‐sectional | COVID−19 inpatients | 85 | 49.4 | 85.9 | 48.8 | 6 | ISI |
| 36 | Yang (Xiao et al., 2020) | 2020 | China | March 5–14, 2020 | no | cross‐sectional | general population | 2,410 | 49.2 | 76.55 | 36.3 | 5 | PSQI |
| 45 | Gualano (Gualano et al., 2020) | 2020 | Italy | April 19 and May 3, 2020 | yes | cross‐sectional | general population | 1,515 | 65.6 | 61.1 | 42 | 5 | ISI |
| 57 | Pieh (Pieh et al., 2020) | 2020 | Austria | April 15–30, 2020 | yes | cross‐sectional | general population | 1,005 | 52.7 | 18–>65 | 6 | ISI | |
| 65 | Zhuo (Zhuo et al., 2020) | 2020 | China | March 2020 | no | cross‐sectional | medical staff | 26 | 46.15 | 41.92 | 5 | ISI | |
| 69 | Wang (Ren et al., 2020) | 2020 | China | February 2 and 3, 2020 | no | cross‐sectional | medical staff | 1,045 | 85.8 | 7 | ISI | ||
| 70 | Shi (Shi et al., 2020) | 2020 | China | February 28–March 11, 2020 | no | cross‐sectional | general population | 56,932 | 52.1 | 77.2 | 35.97 | 7 | ISI |
| 11 | Lai (Lai, Ma et al., 2020) | 2020 | China | January 29–February 3, 2020 | no | cross‐sectional | healthcare workers | 1,257 | 76.7 | 66.7 | 18–>40 | 6 | ISI |
| 46 | Zhou (Zhou, Yang et al., 2020) | 2020 | China | March 24–3 April, 2020 | no | cross‐sectional | healthcare workers | 1,931 | 95.4 | 63.4 | 35.08 | 5 | PSQI |
| 56 | Zhang (Zhang, Xu et al., 2020) | 2020 | China | January 25 and March 15 | no | retrospective cohort | Covid‐19 patients | 136 | 42.2 | 95.6 | 63 | 6 | PSQI |
| 554 | Wasim (Wasim et al., 2020) | 2020 | Pakistan | May 20–June 3, 2020 | no | cross‐sectional | tertiary care hospital dealing with corona patients | 356 | 52.00 | 51.40 | 20–>50 | 6 | ISI |
| 537 | Sharma (Sharma et al., 2020) | 2020 | India | 0 | no | cross‐sectional | obstetrics staff | 184 | 58.70 | 54.35 | 20–>50 | 5 | ISI |
| 535 | Tiete (Tiete et al., 2020) | 2021 | Belgium | April 17–May 25, 2020 | no | cross‐sectional | healthcare professionals | 647 | 78.40 | 80.50 | 20–>50 | 8 | ISI |
| 511 | Franceschini (Franceschini et al., 2020) | 2020 | Italy | March 10–May 4, 2020 | yes | cross‐sectional | general population | 6,439 | 73.10 | 65.10 | 33.90 | 6 | Medical Outcomes Study–Sleep Scale (MOS‐SS) |
| 447 | Bhat (Bhat et al., 2020) | 2020 | Kashmir | April 4–10, 2020 | no | cross‐sectional | general population | 264 | 27.70 | <18–>60 | 8 | PSQI | |
| 420 | Liu (Liu et al., 2020) | 2021 | China | February 1–10, 2020 | no | cross‐sectional | general population | 2,858 | 53.60 | 60.20 | <18–>50 | 6 | PSQI |
| 410 | Alamrawy (Alamrawy et al., 2021) | 2021 | Egypt | July 2–23, 2020 | no | cross‐sectional | young adults of both genders aged between 14 and 24 years | 447 | 70.20 | 20.72 | 8 | ISI | |
| 397 | Akıncı (Akıncı & Başar, 2021) | 2021 | Turkey | April and May, 2020 | no | cross‐sectional | patients hospitalised with COVID‐19 | 189 | 41 | 82.50 | 46.27 | 6 | PSQI |
| 394 | Barua (Barua et al., 2020) | 2021 | Bangladesh | April 1–May 30, 2020 | no | cross‐sectional | healthcare professionals | 370 | 39.70 | 66.80 | 30.50 | 8 | SCI‐02 |
| 389 | Fidanci (Fidanci et al., 2020) | 2020 | Turkey | May 2020 | no | cross‐sectional | healthcare professionals | 153 | 67.30 | 33.40 | 5 | PSQI | |
| 376 | Gu (Peng et al., 2020) | 2020 | China | February 15–22, 2020 | no | cross‐sectional | patients with COVID‐19 | 461 | 64.90 | 95.90 | 18–>50 | 5 | ISI |
| 348 | Almater (Almater et al., 2020) | 2020 | Saudi Arabia | March 28–April 4, 2020 | no | cross‐sectional | ophthalmologists | 107 | 43.90 | 32.90 | 8 | ISI | |
| 12 | Khoury (Khoury et al., 2021) | 2021 | Canada | June 3 and July 31, 2020 | no | cross‐sectional | pregnant individuals | 303 | 100.00 | 100.00 | 32.13 | 7 | ISI |
| 17 | Wang (Wang, Zhao et al., 2020) | 2021 | China | January 28–March 31, 2020 | no | cross‐sectional | general population | 5,676 | 71.40 | 68.90 | 6 | ISI | |
| 25 | Zreik (Zreik et al., 2021) | 2021 | Israel | 20–30 April, 2020 | yes | cross‐sectional | general population | 264 | 100 | 100 | 33.97 | 5 | ISI |
| 47 | Xie (Xie et al., 2021) | 2020 | China | 0 | no | cross‐sectional | pregnant individuals | 689 | 100 | 100 | 29.03 | 6 | PSQI |
| 48 | Zhang (Zhang et al., 2021) | 2021 | China | January–February, 2020 | no | cross‐sectional | pregnant individuals | 456 | 100 | 100 | 6 | PSQI | |
| 57 | Massicotte (Massicotte et al., 2021) | 2021 | Canada | April 28 and May 29, 2020 | no | cross‐sectional | breast cancer patients | 36 | 100 | 66.7 | 53.6 | 5 | ISI |
| 67 | Chen (Chen, Wang et al., 2021) | 2021 | China | March 14–21, 2020 | no | cross‐sectional | breast cancer patients | 834 | 100 | 86 | 5 | ISI | |
| 81 | Yadav (Yadav et al., 2021) | 2021 | India | June–August, 2020 | no | cross‐sectional | COVID‐19 patients | 100 | 27 | 42.9 | 5 | ISI | |
| 92 | Bacaro (Bacaro et al., 2020) | 2020 | Italy | April 1– May 4, 2020 | yes | cross‐sectional | general population | 1,989 | 76.17 | 38.4 | 7 | ISI | |
| 106 | Zhou (Zhou, Shi et al., 2020) | 2020 | China | February 28–March 12, 2020 | no | cross‐sectional | general population of pregnant and non‐pregnant women | 859 | 100 | 93.25 | 33.25 | 9 | ISI |
| 120 | Fazeli (Fazeli et al., 2020) | 2020 | Iran | May 2–August 26, 2020 | no | cross‐sectional | adolescents | 1,512 | 43.6 | 15.51 | 9 | ISI | |
| 130 | Şahin (Şahin et al., 2020) | 2020 | Turkey | April 23 and May 23, 2020 | no | cross‐sectional | healthcare workers | 939 | 66 | 65.7 | 18–>40 | 9 | ISI |
| 137 | Lai (Lai, Lee et al., 2020) | 2020 | UK | April 28–May 12, 2020 | no | cross‐sectional | international university students | 124 | 63.7 | 9 | ISI | ||
| 138 | Wang (Wang, Chen et al., 2020) | 2020 | China | February 21–March 7, 2020 | no | cross‐sectional | college students | 3,092 | 66.4 | 9 | SRSS | ||
| 159 | Wang (Wang, Zhu et al., 2020) | 2020 | China | March 2020 | no | cross‐sectional | COVID‐19 inpatients | 484 | 50.2 | 91.7 | 52.5 | 9 | ISI |
| 164 | Xia (Xia et al., 2020) | 2020 | China | April 20–30, 2020 | no | case‐ control | patients with Parkinson disease | 288 | 51.85 | 60.50 | 9 | PSQI | |
| 174 | Alnofaiey (Alnofaiey et al., 2020) | 2020 | Saudi Arabia | May–August, 2020 | no | cross‐sectional | healthcare workers | 340 | 49.1 | 20–60 | 9 | PSQI | |
| 190 | Juanjuan (Juanjuan et al., 2020) | 2020 | China | February 16–19, 2020 | no | cross‐sectional | patients with breast cancer | 658 | 100 | 88.9 | 9 | ISI | |
| 201 | Wang (Wang, Gong et al., 2020) | 2020 | China | February 4–18, 2020 | no | cross‐sectional | general population | 6,437 | 56.13 | 38.99 | 9 | PSQI | |
| 277 | Parlapani (Parlapani et al., 2020) | 2020 | Greece | 0 | no | cross‐sectional | general population | 103 | 61.17 | 69.85 | 9 | AIS | |
| 239 | Lin (Chang et al., 2020) | 2020 | Iran | February 15–30, 2020 | no | cross‐sectional | general population | 1,078 | 58.3 | 26.24 | 9 | ISI | |
| 375 | Ahorsu (Ahorsu, Lin, & Pakpour, 2020) | 2020 | Iran | April 1–30, 2020 | no | cross‐sectional | general population | 413 | 38 | 87.9 | 57.72 | 9 | ISI |
Abbreviations: AIS, Athens Insomnia Scale; COVID‐19, coronavirus disease 2019; ISI, Insomnia Severity Index; NOS, Newcastle–Ottawa Scale; PSQI, Pittsburgh Sleep Quality Index; SCI‐02, Sleep Condition Indicator two‐item short‐form; SRSS, Self‐Rating Scale of Sleep.
4.2. Estimation of sleep problem prevalence
The pooled estimated prevalence of sleep problems was 31% (95% CI 28%–35%; I 2: 97.58%, tau2: 0.01). Figure 2 provides a Forest plot of the pooled prevalence of sleep problems in this group.
FIGURE 2.
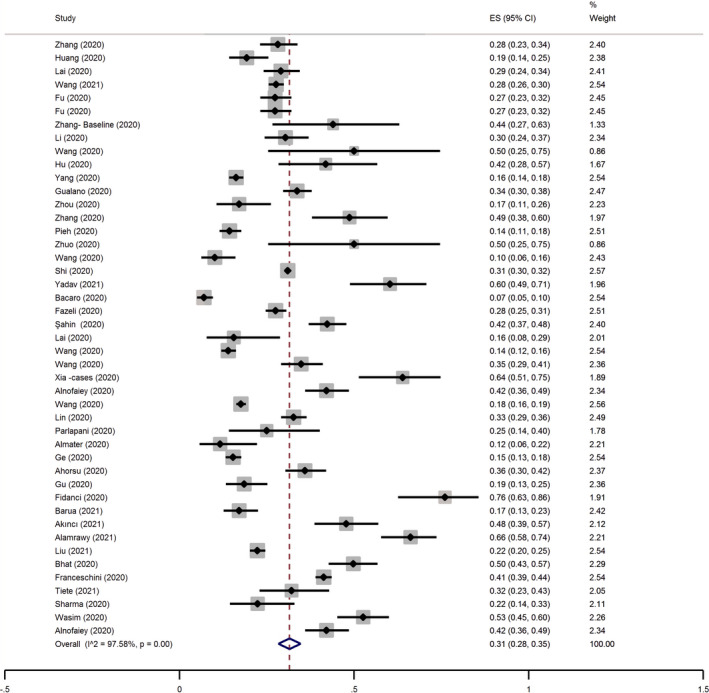
Forest plot for the pooled prevalence of sleep problems in the male group. CI, confidence interval; ES, effect size
Subgroup analysis (Table 2) showed that the prevalence of sleep problems was higher in longitudinal versus cross‐sectional studies (48% versus 31%). Although prevalence of sleep problems appeared to be different among male healthcare professionals (34%), the general population (29%) and patients with COVID‐19 (39%), these differences were not statistically significant considering overlap in the 95% CI of pooled prevalence among these groups (26%–43% for healthcare professionals, 24%–33% for general population, and 27%–50% for patients with COVID‐19). Based on multivariable meta‐regression (Table 4), being in lockdown period, quality of studies, and measure used to assess sleep problems were significant predictors of sleep problems prevalence among male participants. These variables together explained 100% of the variance.
TABLE 2.
Results of subgroup analysis for estimated pooled prevalence
| Variable | Female participants (N = 54 studies) | Male participants (N = 45 studies) | ||||
|---|---|---|---|---|---|---|
| No. studies | Pooled prevalence, % (95% CI) | I 2, % | No. studies | Pooled prevalence, % (95% CI) | I 2, % | |
| Lockdown period | ||||||
| Yes | 5 | 37 (13–62) | 99.83 | 4 | 24 (6–42) | 99.4 |
| No | 49 | 41 (36–45) | 99.24 | 41 | 32 (29–35) | 96.7 |
| Study quality | ||||||
| Low quality | 16 | 38 (31–45) | 98.27 | 13 | 32 (25–38) | 93.95 |
| High quality | 38 | 41 (36–47) | 99.56 | 32 | 31 (28–35) | 97.96 |
| Study design | ||||||
| Cross sectional | 52 | 40 (35–45) | 99.45 | 45 | 31 (28–34) | 97.6 |
| Longitudinal | 2 | 55 (46–65) | ‐ | 2 | 48 (38–57) | ‐ |
| Participants’ group | ||||||
| Health professionals | 15 | 41 (31–51) | 99.02 | 15 | 34 (26–43) | 94.8 |
| General patients | 32 | 38 (32–44) | 99.58 | 25 | 29 (24–33) | 98.4 |
| COVID‐19 patients | 7 | 51 (42–60) | 84.68 | 7 | 39 (27–50) | 91.3 |
| Measure of Sleep | ||||||
| ISI | 31 | 41 (36‐47) | 99.33 | 14 | 30 (26–34) | 96.7 |
| PSQI | 17 | 41 (33–50) | 99.08 | 27 | 38 (31–44) | 97.2 |
| Other | 6 | 34 (13–55) | 99.76 | 6 | 25 (14–37) | 98.4 |
| Overall estimated prevalence | 54 | 41 (37–46) | 99.41 | 45 | 31 (25–38) | 97.48 |
Abbreviations: COVID‐19, coronavirus disease 2019; ISI, Insomnia Severity Index; PSQI, Pittsburgh Sleep Quality Index.
TABLE 4.
Results of multivariable meta‐regression for estimated pooled prevalence
| Variable | Female participants | Male participants | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p | Coefficient | SE | p | |
| Country | 0.007 | 0.004 | 0.14 | −0.002 | 0.001 | 0.32 |
| Design | −0.07 | 0.13 | 0.59 | −0.02 | 0.04 | 0.57 |
| Lockdown period (yes versus no) | 0.41 | 0.16 | 0.03 | 0.19 | 0.04 | 0.02 |
| Study quality (low versus high quality) | 0.34 | 0.12 | 0.02 | 0.23 | 0.03 | 0.004 |
| Participants group | −0.03 | 0.07 | 0.73 | 0.007 | 0.01 | 0.64 |
| Age | 0.009 | 0.006 | 0.15 | 0.007 | 0.002 | 0.06 |
| % married of participants | 0.002 | 0.003 | 0.52 | −0.003 | 0.002 | 0.20 |
| Measure of sleep | −0.16 | 0.09 | 0.09 | −0.11 | 0.03 | 0.04 |
| Number of included studies in multivariable regression | 18 | 12 | ||||
| Between‐study variance (tau2) | 0.03 | 0.004 | ||||
| % residual variation due to heterogeneity (I 2 residual) | 98.98 | 0 | ||||
| Proportion of between‐study variance explained (Adjusted R 2) | 34.18 | 100 | ||||
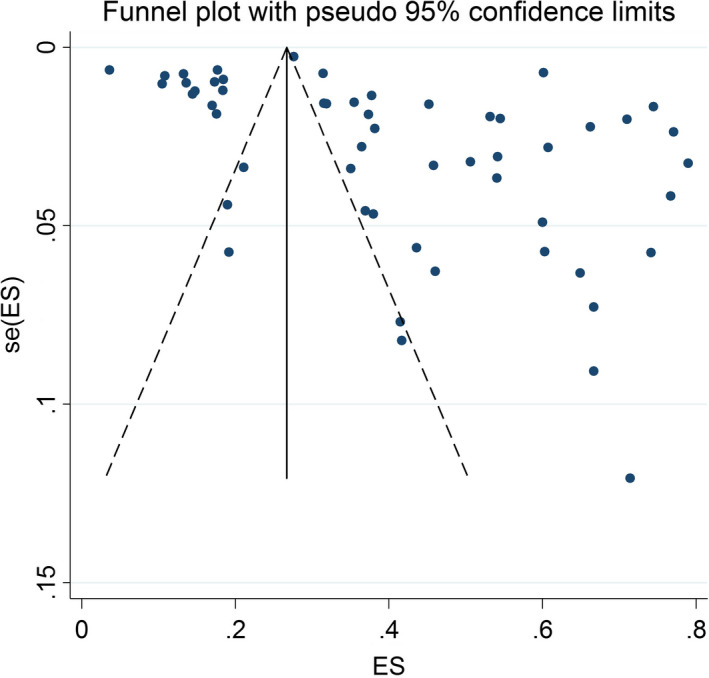
Begg’s test (p = 0.006) and funnel plot (Figure 3) consider probability of publication bias. Meta trim was used to correct publication bias. Based on the trim method, eight studies were imputed, and the corrected prevalence of sleep problems was 27% (95% CI 24%–30%). The corrected funnel plot is provided in Figure 4. Also, sensitivity analysis showed that pooled effect size was not affected by the effect of a single study.
FIGURE 3.
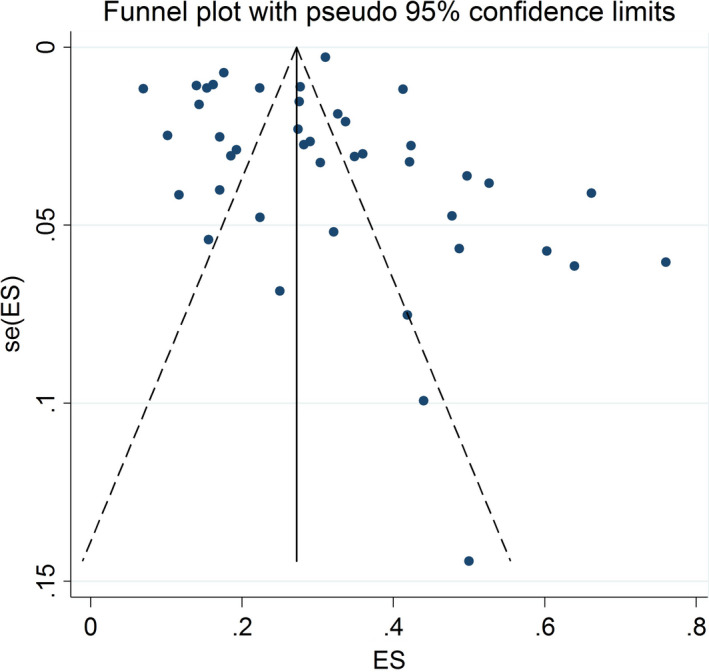
Funnel plot assessing the publication bias among the included studies in the male subgroup. ES, effect size
FIGURE 4.
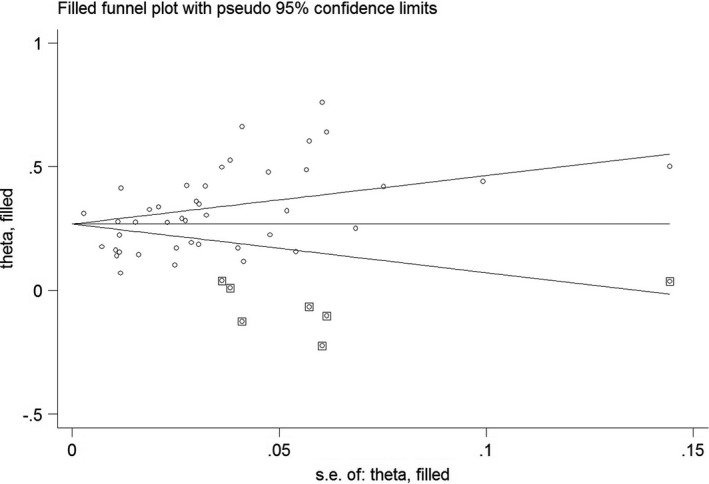
Corrected funnel plot based on the fill‐and‐trim method in the male subgroup
5. FEMALE SUBGROUP
5.1. Study description
A total of 54 papers with 67,722 participants from 15 countries (China [54,801 participants], Italy [7,222], Austria [530], Turkey [801], Bangladesh [147], Pakistan [907], Greece [63], India [12,266], Belgium [507], Egypt [314], Saudi Arabia [274], UK [79], Canada [339], Israel [264], and Iran [12,266]) were included. Five papers gathered data during the lockdown period. The individual country with the most eligible studies was China (N = 29). The smallest sample size was 14, and the highest was 29,530. The mean age of participants varied from 15.4 to 70 years and ~72.1% were married. Most studies involved the general population (32 studies), with others involving health professionals (15), and patients with COVID‐19 (seven). Most of the studies were cross‐sectional (52 studies). The two remaining studies had a longitudinal design and collected data during the COVID‐19 pandemic and baseline data were extracted. The ISI and PSQI were used to assess sleep problems (in 31 and 17 studies, respectively). Considering NOS >5 as high quality, 70% of the included studies (38 papers) were categorised as high‐quality. Table 1 provides the summary characteristics of the included studies.
5.2. Estimation of sleep problem prevalence
The pooled estimated prevalence of sleep problems was 41% (95% CI 36%–45%; I 2: 99.43%, tau2: 0.03). Figure 5 provides a Forest plot regarding the pooled prevalence of sleep problems in this group.
FIGURE 5.
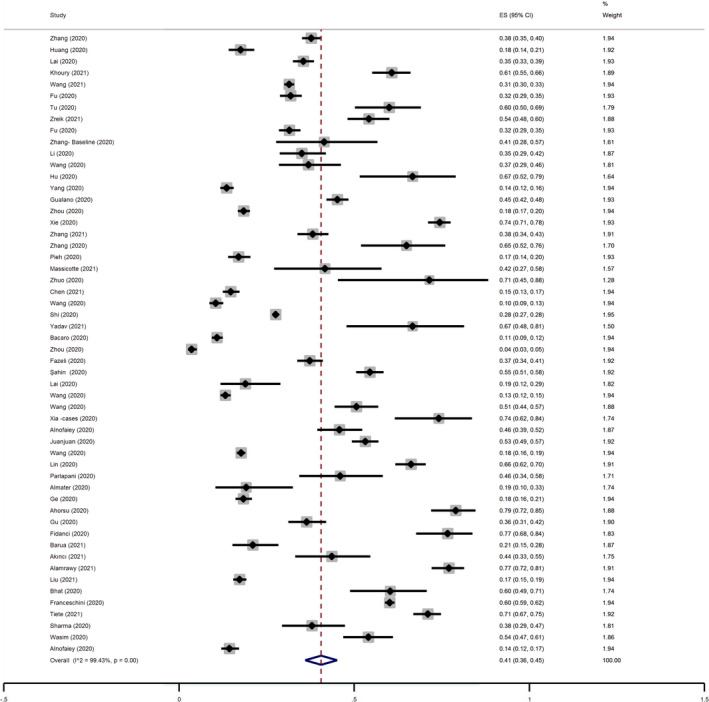
Forest plot for the pooled prevalence of sleep problems in the female group. CI, confidence interval; ES, effect size
Subgroup analysis (Table 2) showed that the prevalence of sleep problems was higher in longitudinal versus cross sectional studies (55% versus 41%). Although prevalence of sleep problems appeared to be different among female patients with COVID‐19 (51%), healthcare professionals (41%), and the general population (38%), these differences were not significantly different considering the overlap in 95% CI of pooled prevalence among these groups (31%–51% for healthcare professionals, 32%–44% for general population, and 42%–60% for patients with COVID‐19). Based on univariate meta‐regression (Table 3), country and percentage of married participants were other significant predictors of sleep problems prevalence among women. In multivariable meta‐regression (Table 4) being in lockdown and study quality were significant predictors of sleep problems prevalence among female participants, which explained 34.18% of the variance.
TABLE 3.
Results of meta‐ regression for gender‐specific estimated pooled prevalence
| Univariable | Female | Male | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | No. studies | Coeff. | SE | p | I 2 res., % | Adj. R 2, % | Tau2 | No. studies | Coeff. | SE | p | I 2 res., % | Adj. R 2, % | Tau2 |
| Country | 54 | 0.01 | 0.003 | 0.02 | 99.35 | 9.26 | 0.04 | 45 | 0.002 | 0.002 | 0.35 | 97.59 | 0.51 | 0.02 |
| Age | 30 | 0.004 | 0.003 | 0.29 | 99.59 | 0.44 | 0.05 | 24 | 0.001 | 0.003 | 0.62 | 97.75 | −3.32 | 0.03 |
| % of married participants | 34 | 0.0003 | 0.002 | 0.05 | 99.53 | 8.51 | 0.03 | 25 | 0.001 | 0.001 | 0.43 | 95.87 | −0.88 | 0.01 |
Abbreviation: Coeff., coefficient.
As indicated above, the Begg’s test (p = 0.08) and funnel plot (Figure 6) consider probability of publication bias. Meta trim was used to correct publication bias. Based on the trim method, 22 studies were imputed, and the corrected prevalence of sleep problems was 24% (95% CI 19%–29%). The corrected funnel plot is provided in Figure 7. Also, sensitivity analysis showed that the pooled effect size was not affected by the effect of a single study.
FIGURE 6.
Funnel plot assessing the publication bias among included studies in the female subgroup. ES, effect size
FIGURE 7.
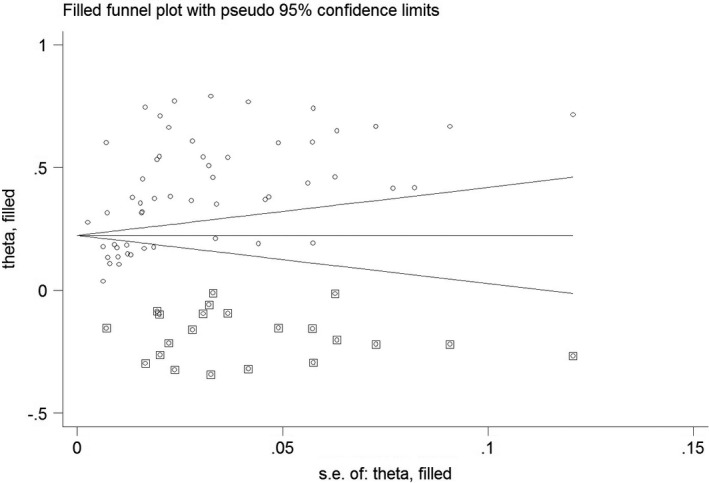
Corrected funnel plot based on the fill‐and‐trim method in the male subgroup
6. DISCUSSION
The present systematic review and meta‐analysis aimed to provide timely information for healthcare providers to understand how the COVID‐19 pandemic and the related government actions impacted on sleep problems worldwide. More specifically, the present study estimated the prevalence of sleep problems separately for males and females using amalgamated data from 54 recently published studies in the female subgroup and 45 recently published studies in the male subgroup. With the use of the PRISMA guideline and rigorous meta‐analysis methods, robust and valid information on the prevalence of sleep problems between males and females worldwide are provided in the present study. We should note that the estimate of sleep problems was calculated based on the reports emanating from 15 countries for the female subgroup and 13 countries for the male subgroup with nearly 115,000 participants, and therefore, expanded information originating from other regions would be valuable to assess for the consistency and applicability of the present findings. As a corollary to these considerations, we uncovered sex differences in the prevalence of reported sleep problems with women exhibiting greater prevalence. Moreover, subgroup analysis and meta‐regression showed a lower rate of prevalence for sleep problems regardless of gender in regions where the lockdown was implemented than in regions where control measures without lockdown were put in place. Additionally, COVID‐19‐infected patients had higher prevalence rates of sleep problems than did health professionals and the general population. It is possible that such effects of COVID‐19 reflect central nervous system involvement by the virus or unspecific consequences of the disease stress induced by the infection (Cénat et al., 2020). Notwithstanding, female health professionals appear to be more likely to experience sleep problems compared to their counterparts in the general population, but such differences did not emerge in men.
As indicated, most of the data retrieved for the present systematic review and meta‐analysis originated from cross‐sectional designed studies. Notwithstanding, we surmise that the fear and stress associated with COVID‐19 may be one of the major reasons contributing to the high prevalence of sleep problems. More specifically, social media and news channels have continuously routinely reported on daily deaths and on the number of cumulative infected cases of COVID‐19 both at the national and global scales, and such intensive media exposure is likely to generate the anxiety and stress that facilitate the emergence of sleep problems (Lin, Broström et al., 2020, Lin, Imani et al., 2020). Indeed, higher levels of psychological distress and signs of mental disorders have been reported during this pandemic among different populations worldwide (Mamun et al., 2021; Rodríguez‐Rey et al., 2020; Wang, Pan et al., 2020) and significant sleep difficulties have been identified in the context of major public health threats (e.g. Ebola) (Cates et al., 2018; Lehmann et al., 2015).
The reasons for the higher prevalence of sleep problems in females are unclear, but possibly may reside in the underlying brain structural differences across sexes (Xin et al., 2019). Therefore, exposure to the same circumstances may yield different perceptions and lead to divergent emotional processing. Indeed, prior evidence found that self‐reported outcomes on subjective health (e.g. quality of life) differ between males and females (Lin et al., 2016; Su et al., 2013). Additionally, women are more likely to report psychological problems in response to taxing situational settings (Wang et al., 2017). Finally, issues such as insomnia exhibit clear gender dimorphic features (Kocevska et al., 2020; Silva‐Costa et al., 2020; Sivertsen et al., 2021).
The sleep problems among healthcare professionals found in the present systematic review and meta‐analysis could be attributed to the interactions between the COVID‐19 pandemic and the specific attributes of the jobs. From the perspective of the COVID‐19 pandemic, health professionals, especially those who had to be in direct contact with patients with COVID‐19 and those who were at high risk of being exposed to the COVID‐19 virus, had higher levels of worry and psychological distress. The higher levels of worry and psychological distress are likely to subsequently foster the development of their sleep problems (Fidanci, derinöz Güleryüz, & Fidanci, 2020). From the perspective of the job itself, health professionals, especially those who work in a large hospital, have irregular work schedules when compared to individuals who work in other occupations (Caruso, 2014; Ferri et al., 2016; Jahrami et al., 2019; Koinis et al., 2015; Kumar et al., 2018; Mohanty et al., 2019). Such irregular work schedules are harmful for a good night’s sleep. Therefore, the interaction between the COVID‐19 pandemic and job type may increase the workload for healthcare professionals and exacerbate their sleep issues.
There are some strengths and limitations of the present study that deserve mention. First, the timely and comprehensive search of the literature ensures that the information and estimates reported reflect the available state of knowledge. Moreover, inclusion of different cohorts such as those represented by patients with COVID‐19, healthcare professionals, and the general populations provide a wider perspective on the effects of the pandemic on sleep. Second, the present systematic review and meta‐analysis utilised robust and rigorous methodology to ensure the quality of the analysed studies and synthesised estimations. More specifically, the literature search was systematically conducted in several major databases, including Scopus, PubMed Central, ProQuest, ISI WoS, and EMBASE. All the review processes were conducted using the international standard, i.e. PRISMA guidelines (Moher et al., 2010), and the NOS checklist was used to ascertain the quality of each study. Third, the cumulative sample size was relatively large (>100,000) and encompassed 15 countries (China, Italy, Austria, Turkey, Bangladesh, Pakistan, Greek, India, Belgium, Egypt, Saudi Arabia, UK Canada, Israel, and Iran), likely adding generalisability to the findings of the present study. However, we should also point out that a cross‐sectional design was the most used design among the included papers, and thus the causal relationship between the COVID‐19 outbreak and sleep problems is tentative at best. More specifically, it is unclear whether the prevalence of sleep problems was significantly changed between before and during the COVID‐19 outbreak. Furthermore, sleep problems estimates were derived from different survey instruments, which obviously differ in their psychometric properties and may also differentially capture heterogeneous aspects of sleep problems. More specifically, some people may be for example identified as having sleep problems using the ISI, but not with the PSQI. Therefore, the biases in estimating prevalence of sleep problems cannot be overcome. Third, the measures used to identify sleep problems were all based on self‐reporting. Therefore, commonly encountered biases (e.g. recall bias and social desirability bias) cannot not be excluded. Fourth, the actual figures of COVID‐19 regarding suspected cases, confirmed cases, and deaths are widely different across countries; therefore, the impact of such figures on sleep problems may not be the same. Furthermore, different countries applied different policies for COVID‐19 outbreak control (Chang et al., 2020; Chen, Chen et al., 2021, Chen, Wang et al., 2021; Chen et al., 2020; Lin, Broström et al., 2020, Lin, Imani 2020; Mamun et al., 2021; Pramukti et al., 2020) and such measures could affect the prevalence rates of sleep problems.
In summary, a relatively high prevalence of sleep problems emerged during the COVID‐19 pandemic and imposed increased effects on women. The sleep problems found in the present systematic review and meta‐analysis concur with the evidence of well‐established adverse impacts of long‐term lockdown on mental health (Ahorsu, Lin, & Pakpour, 2020; Chang et al., 2020; Lin, Broström et al., 2020, Lin, Imani et al., 2020). Considering the present findings, specific measures aimed at mitigating the effect of the COVID‐19 pandemic on sleep should be developed and tried in a gender‐specific fashion.
AUTHOR CONTRIBUTIONS
Each author made a substantial contribution to project design, data collection or data analysis. Additionally, all authors contributed to the preparation of this manuscript.
CONFLICT OF INTEREST
All authors have no conflicts to declare.
FUNDING INFORMATION
The open access was funded by Jönköping University.
Supporting information
Supplementary Material
ACKNOWLEDGEMENT
C‐YL was supported in part by a research grant from the Ministry of Science and Technology, Taiwan (MOST109‐2327‐B‐006‐005).
Alimoradi, Z. , Gozal, D. , Tsang, H. W. H. , Lin, C.‐Y. , Broström, A. , Ohayon, M. M. , & Pakpour, A. H. (2022). Gender‐specific estimates of sleep problems during the COVID‐19 pandemic: Systematic review and meta‐analysis. Journal of Sleep Research, 31, e13432. 10.1111/jsr.13432
Contributor Information
Chung‐Ying Lin, Email: cylin36933@gmail.com.
Amir H. Pakpour, Email: Pakpour_Amir@yahoo.com.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- Ahorsu, D. K. , Lin, C.‐Y. , Imani, V. , Saffari, M. , Griffiths, M. D. , & Pakpour, A. H. (2020). The fear of COVID‐19 scale: Development and initial validation. International Journal of Mental Health and Addiction, [Epub ahead of print]. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu, D. K. , Lin, C.‐Y. , & Pakpour, A. H. (2020). The association between health status and insomnia, mental health, and preventive behaviors: The mediating role of fear of COVID‐19. Gerontology and Geriatric Medicine, 6, 2333721420966081. 10.1177/2333721420966081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akıncı, T. , & Başar, H. M. (2021). Relationship between sleep quality and the psychological status of patients hospitalised with COVID‐19. Sleep Medicine, 80, 167–170. 10.1016/j.sleep.2021.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alamrawy, R. G. , Fadl, N. , & Khaled, A. (2021). Psychiatric morbidity and dietary habits during COVID‐19 pandemic: A cross‐sectional study among Egyptian Youth (14–24 years). Middle East Current Psychiatry, 28(1), 1–10. 10.1186/s43045-021-00085-w [DOI] [Google Scholar]
- Alimoradi, Z. , Lin, C.‐Y. , Broström, A. , Bülow, P. H. , Bajalan, Z. , Griffiths, M. D. , Ohayon, M. M. , & Pakpour, A. H. (2019). Internet addiction and sleep problems: A systematic review and meta‐analysis. Sleep Medicine Reviews, 47, 51–61. 10.1016/j.smrv.2019.06.004 [DOI] [PubMed] [Google Scholar]
- Alimoradi, Z. , & Pakpour, A. H. (2020). Sleep and Covid‐19 related psychological distress. Retrieved 2020, 04, 28, from https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=181644 [Google Scholar]
- Almater, A. I. , Tobaigy, M. F. , Younis, A. S. , Alaqeel, M. K. , & Abouammoh, M. A. (2020). Effect of 2019 coronavirus pandemic on ophthalmologists practicing in Saudi Arabia: A psychological health assessment. Middle East African Journal of Ophthalmology, 27(2), 79. 10.4103/meajo.MEAJO_220_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alnofaiey, Y. H. , Alshehri, H. A. , Alosaimi, M. M. , Alswat, S. H. , Alswat, R. H. , Alhulayfi, R. M. , Alghamdi, M. A. , & Alsubaie, R. M. (2020). Sleep disturbances among physicians during COVID‐19 pandemic. BMC Research Notes, 13(1), 1–7. 10.1186/s13104-020-05341-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacaro, V. , Chiabudini, M. , Buonanno, C. , De Bartolo, P. , Riemann, D. , Mancini, F. , & Baglioni, C. (2020). Insomnia in the Italian population during Covid‐19 outbreak: A snapshot on one major risk factor for depression and anxiety. Frontiers in Psychiatry, 11, 579107. 10.3389/fpsyt.2020.579107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barua, L. , Zaman, M. S. , Omi, F. R. , & Faruque, M. (2020). Psychological burden of the COVID‐19 pandemic and its associated factors among frontline doctors of Bangladesh: A cross‐sectional study. F1000Research, 9, 1304. 10.12688/f1000research.27189.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat, B. A. , Mir, R. A. , Hussain, A. , & Shah, I. R. (2020). Depressive and anxiety symptoms, quality of sleep, and coping during the 2019 coronavirus disease pandemic in general population in Kashmir. Middle East Current Psychiatry, 27(1), 1–10. 10.1186/s43045-020-00069-2 [DOI] [Google Scholar]
- Caruso, C. C. (2014). Negative impacts of shiftwork and long work hours. Rehabilitation Nursing, 39(1), 16–25. 10.1002/rnj.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates, D. S. , Gomes, P. G. , & Krasilovsky, A. M. (2018). Behavioral Health Support for Patients, Families, and Healthcare Workers. In: Hewlett A., & Murthy K. A. (eds) Bioemergency Planning (pp. 195–214). Springer. [Google Scholar]
- Cénat, J. M. , Blais‐Rochette, C. , Kokou‐Kpolou, C. K. , Noorishad, P.‐G. , Mukunzi, J. N. , McIntee, S.‐E. , Dalexis, R. D. , Goulet, M.‐A. , & Labelle, P. (2020). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID‐19 pandemic: A systematic review and meta‐analysis. Psychiatry Research, 295, 113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, K.‐C. , Strong, C. , Pakpour, A. H. , Griffiths, M. D. , & Lin, C.‐Y. (2020). Factors related to preventive COVID‐19 infection behaviors among people with mental illness. Journal of the Formosan Medical Association, 119(12), 1772–1780. 10.1016/j.jfma.2020.07.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, C.‐Y. , Chen, I.‐H. , O’Brien, K. S. , Latner, J. D. , & Lin, C.‐Y. (2021). Psychological distress and internet‐related behaviors between schoolchildren with and without overweight during the COVID‐19 outbreak. International Journal of Obesity, 45, 677–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, I.‐H. , Chen, C.‐Y. , Pakpour, A. H. , Griffiths, M. D. , & Lin, C.‐Y. (2020). Internet‐related behaviors and psychological distress among schoolchildren during COVID‐19 school suspension. Journal of the American Academy of Child and Adolescent Psychiatry, 59(10), 1099. 10.1016/j.jaac.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, X. , Wang, L. , Liu, L. , Jiang, M. , Wang, W. , Zhou, X. , & Shao, J. (2021). Factors associated with psychological distress among patients with breast cancer during the COVID‐19 pandemic: A cross‐sectional study in Wuhan, China. Supportive Care in Cancer, 29, 4773–4782. 10.1007/s00520-021-05994-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval, S. , & Tweedie, R. (2000). Trim and fill: A simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics, 56(2), 455–463. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- Fazeli, S. , Zeidi, I. M. , Lin, C.‐Y. , Namdar, P. , Griffiths, M. D. , Ahorsu, D. K. , & Pakpour, A. H. (2020). Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID‐19 outbreak. Addictive Behaviors Reports, 12, 100307. 10.1016/j.abrep.2020.100307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferri, P. , Guadi, M. , Marcheselli, L. , Balduzzi, S. , Magnani, D. , & Di Lorenzo, R. (2016). The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Management and Healthcare Policy, 9, 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidanci, İ. , derinöz Güleryüz, O. , & Fidanci, İ. (2020). An analysis on sleep quality of the healthcare professionals during the covid‐19 pandemic. Acta Medica, 36, 3797. [Google Scholar]
- Franceschini, C. , Musetti, A. , Zenesini, C. , Palagini, L. , Scarpelli, S. , Quattropani, M. C. , Lenzo, V. , Freda, M. F. , Lemmo, D. , Vegni, E. , Borghi, L. , Saita, E. , Cattivelli, R. , De Gennaro, L. , Plazzi, G. , Riemann, D. , & Castelnuovo, G. (2020). Poor sleep quality and its consequences on mental health during the COVID‐19 lockdown in Italy. Frontiers in Psychology, 11, 3072. 10.3389/fpsyg.2020.574475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu, W. , Wang, C. , Zou, L. , Guo, Y. , Lu, Z. , Yan, S. , & Mao, J. (2020). Psychological health, sleep quality, and coping styles to stress facing the COVID‐19 in Wuhan, China. Translational Psychiatry, 10(1), 1–9. 10.1038/s41398-020-00913-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbarino, S. , Lanteri, P. , Durando, P. , Magnavita, N. , & Sannita, W. G. (2016). Co‐morbidity, mortality, quality of life and the healthcare/welfare/social costs of disordered sleep: A rapid review. International Journal of Environmental Research and Public Health, 13(8), 831. 10.3390/ijerph13080831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giardino, D. L. , Huck‐Iriart, C. , Riddick, M. , & Garay, A. (2020). The endless quarantine: The impact of the COVID‐19 outbreak on healthcare workers after three months of mandatory social isolation in Argentina. Sleep Medicine, 76, 16–25. 10.1016/j.sleep.2020.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradisar, M. , Terrill, G. , Johnston, A. , & Douglas, P. (2008). Adolescent sleep and working memory performance. Sleep and Biological Rhythms, 6(3), 146–154. 10.1111/j.1479-8425.2008.00353.x [DOI] [Google Scholar]
- Gualano, M. R. , Lo Moro, G. , Voglino, G. , Bert, F. , & Siliquini, R. (2020). Effects of Covid‐19 lockdown on mental health and sleep disturbances in Italy. International Journal of Environmental Research and Public Health, 17(13), 4779. 10.3390/ijerph17134779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashemi, S. G. S. , Hosseinnezhad, S. , Dini, S. , Griffiths, M. D. , Lin, C.‐Y. , & Pakpour, A. H. (2020). The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID‐19 among Iranian online population. Heliyon, 6(10), e05135. 10.1016/j.heliyon.2020.e05135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges, L. V. , & Olkin, I. (2014). Statistical methods for meta‐analysis. Academic Press. [Google Scholar]
- Hox, J. J. , & Leeuw, E. D. D. (2003). Multilevel models for meta‐analysis. In: Reise S. P., & Duan N. (Eds.), Multilevel modeling: Methodological advances, issues, and applications (pp. 90–111). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: A web‐based cross‐sectional survey. Psychiatry Research, 288, 112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huedo‐Medina, T. B. , Sánchez‐Meca, J. , Marín‐Martínez, F. , & Botella, J. (2006). Assessing heterogeneity in meta‐analysis: Q statistic or I² index? Psychological Methods, 11(2), 193. 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- Jahrami, H. , Dewald‐Kaufmann, J. , Faris, M.‐A.‐I. , AlAnsari, A. M. , Taha, M. , & AlAnsari, N. (2019). Prevalence of sleep problems among medical students: A systematic review and meta‐analysis. Journal of Public Health, 28, 605–622. 10.1007/s10389-019-01064-6 [DOI] [Google Scholar]
- Juanjuan, L. , Santa‐Maria, C. A. , Hongfang, F. , Lingcheng, W. , Pengcheng, Z. , Yuanbing, X. , Yuyan, T. , Zhongchun, L. , Bo, D. , Meng, L. , Qingfeng, Y. , Feng, Y. , Yi, T. , Shengrong, S. , Xingrui, L. , & Chuang, C. (2020). Patient‐reported outcomes of patients with breast cancer during the COVID‐19 outbreak in the epicenter of China: A cross‐sectional survey study. Clinical Breast Cancer, 20(5), e651–e662. 10.1016/j.clbc.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury, J. E. , Atkinson, L. , Bennett, T. , Jack, S. M. , & Gonzalez, A. (2021) COVID‐19 and mental health during pregnancy: The importance of cognitive appraisal and social support. Journal of Affective Disorders, 282, 1161–1169. 10.1016/j.jad.2021.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocevska, D. , Lysen, T. S. , Dotinga, A. , Koopman‐Verhoeff, M. E. , Luijk, M. P. , Antypa, N. , Biermasz, N. R. , Blokstra, A. , Brug, J. , Burk, W. J. , Comijs, H. C. , Corpeleijn, E. , Dashti, H. S. , de Bruin, E. J. , de Graaf, R. , Derks, I. P. M. , Dewald‐Kaufmann, J. F. , Elders, P. J. M. , Gemke, R. J. B. J. , … Tiemeier, H. (2020). Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: A systematic review and meta‐analysis. Nature Human Behaviour, 5(1), 113–122. 10.1038/s41562-020-00965-x [DOI] [PubMed] [Google Scholar]
- Koinis, A. , Giannou, V. , Drantaki, V. , Angelaina, S. , Stratou, E. , & Saridi, M. (2015). The impact of healthcare workers job environment on their mental‐emotional health. Coping strategies: The case of a local general hospital. Health Psychology Research, 3(1), 1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopasz, M. , Loessl, B. , Hornyak, M. , Riemann, D. , Nissen, C. , Piosczyk, H. , & Voderholzer, U. (2010). Sleep and memory in healthy children and adolescents–A critical review. Sleep Medicine Reviews, 14(3), 167–177. 10.1016/j.smrv.2009.10.006 [DOI] [PubMed] [Google Scholar]
- Kumar, A. , Bhat, P. S. , & Ryali, S. (2018). Study of quality of life among health workers and psychosocial factors influencing it. Industrial Psychiatry Journal, 27(1), 96. 10.4103/ipj.ipj_41_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, A.‐Y.‐K. , Lee, L. , Wang, M.‐P. , Feng, Y. , Lai, T.‐T.‐K. , Ho, L.‐M. , Lam, V.‐S.‐F. , & Ip, M.‐S.‐M. , & Lam, T.‐H. (2020). Mental health impacts of the COVID‐19 pandemic on international university students, related stressors, and coping strategies. Frontiers in Psychiatry, 11, 584240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. , Cai, Z. , Hu, J. , Wei, N. , Wu, J. , Du, H. , Chen, T. , Li, R. , Tan, H. , Kang, L. , Yao, L. , Huang, M. , Wang, H. , Wang, G. , Liu, Z. , & Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann, M. , Bruenahl, C. A. , Löwe, B. , Addo, M. M. , Schmiedel, S. , Lohse, A. W. , & Schramm, C. (2015). Ebola and psychological stress of health care professionals. Emerging Infectious Diseases, 21(5), 913. 10.3201/eid2105.141988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C.‐Y. , Broström, A. , Griffiths, M. D. , & Pakpour, A. H. (2020). Investigating mediated effects of fear of COVID‐19 and COVID‐19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interventions, 21, 100345. 10.1016/j.invent.2020.100345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. Y. , Imani, V. , Majd, N. R. , Ghasemi, Z. , Griffiths, M. D. , Hamilton, K. , Hagger, M. S. , & Pakpour, A. H. (2020). Using an integrated social cognition model to predict COVID‐19 preventive behaviours. British Journal of Health Psychology, 25(4), 981–1005. 10.1111/bjhp.12465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C.‐Y. , Li, Y.‐P. , Lin, S.‐I. , & Chen, C.‐H. (2016). Measurement equivalence across gender and education in the WHOQOL‐BREF for community‐dwelling elderly Taiwanese. International Psychogeriatrics, 28(8), 1375. 10.1017/S1041610216000594 [DOI] [PubMed] [Google Scholar]
- Lin, C.‐Y. , Strong, C. , Scott, A. J. , Broström, A. , Pakpour, A. H. , & Webb, T. L. (2018). A cluster randomized controlled trial of a theory‐based sleep hygiene intervention for adolescents. Sleep, 41(11), zsy170. [DOI] [PubMed] [Google Scholar]
- Lin, P.‐H. , Lin, C.‐Y. , Wang, P.‐Y. , & Yang, S.‐Y. (2018). Association between sleeping duration and health‐related behaviors in college student. Social Health and Behavior, 1(1), 31. [Google Scholar]
- Liu, C. , Liu, D. , Huang, N. , Fu, M. , Ahmed, J. F. , Zhang, Y. , Wang, X. , Wang, Y. , Shahid, M. , & Guo, J. (2020). The combined impact of gender and age on post‐traumatic stress symptoms, depression, and insomnia during COVID‐19 outbreak in China. Frontiers Public Health, 8, 620023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchini, C. , Stubbs, B. , Solmi, M. , & Veronese, N. (2017). Assessing the quality of studies in meta‐analyses: Advantages and limitations of the Newcastle Ottawa Scale. World Journal of Meta‐Analysis, 5(4), 80–84. 10.13105/wjma.v5.i4.80 [DOI] [Google Scholar]
- Mamun, M. A. , Sakib, N. , Gozal, D. , Bhuiyan, A. I. , Hossain, S. , Bodrud‐Doza, M. , Al Mamun, F. , Hosen, I. , Safiq, M. B. , Abdullah, A. H. , Sarker, M. A. , Rayhan, I. , Sikder, M. T. , Muhit, M. , Lin, C.‐Y. , Griffiths, M. D. , & Pakpour, A. H. (2021). The COVID‐19 pandemic and serious psychological consequences in Bangladesh: A population‐based nationwide study. Journal of Affective Disorders, 279, 462–472. 10.1016/j.jad.2020.10.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massicotte, V. , Ivers, H. , & Savard, J. (2021). COVID‐19 pandemic stressors and psychological symptoms in breast cancer patients. Current Oncology, 28(1), 294–300. 10.3390/curroncol28010034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohanty, A. , Kabi, A. , & Mohanty, A. P. (2019). Health problems in healthcare workers: A review. Journal of Family Medicine and Primary Care, 8(8), 2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Ou, H.‐T. , Su, C.‐T. , Luh, W.‐M. , & Lin, C.‐Y. (2017). Knowing is half the battle: The association between leisure‐time physical activity and quality of life among four groups with different self‐perceived health status in Taiwan. Applied Research in Quality of Life, 12(4), 799–812. 10.1007/s11482-016-9488-1 [DOI] [Google Scholar]
- Pakpour, A. H. , Griffiths, M. D. , Ohayon, M. M. , Broström, A. , & Lin, C.‐Y. (2020). A good sleep: The role of factors in psychosocial health. Frontiers in Neuroscience, 14, 520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parlapani, E. , Holeva, V. , Nikopoulou, V. A. , Sereslis, K. , Athanasiadou, M. , Godosidis, A. , Stephanou, T. , & Diakogiannis, I. (2020). Intolerance of uncertainty and loneliness in older adults during the COVID‐19 pandemic. Frontiers in Psychiatry, 11, 842. 10.3389/fpsyt.2020.00842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng, M. , Mo, B. , Liu, Y. , Xu, M. , Song, X. , Liu, L. , Fang, Y. , Guo, T. , Ye, J. , Yu, Z. , Deng, Q. , & Zhang, X. (2020). Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID‐19 outbreak. Journal of Affective Disorders, 275, 119–124. 10.1016/j.jad.2020.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh, C. , Budimir, S. , & Probst, T. (2020). The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID‐19) lockdown in Austria. Journal of Psychosomatic Research, 136, 110186. 10.1016/j.jpsychores.2020.110186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pramukti, I. , Strong, C. , Sitthimongkol, Y. , Setiawan, A. , Pandin, M. G. R. , Yen, C.‐F. , Lin, C.‐Y. , Griffiths, M. D. , & Ko, N.‐Y. (2020). Anxiety and suicidal thoughts during the COVID‐19 pandemic: Cross‐country comparative study among Indonesian, Taiwanese, and Thai university students. Journal of Medical Internet Research, 22(12), e24487. 10.2196/24487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren, Y. , Qian, W. , Li, Z. , Liu, Z. , Zhou, Y. , Wang, R. , Qi, L. , Yang, J. , Song, X. , Zeng, L. , & Zhang, X. (2020). Public mental health under the long‐term influence of COVID‐19 in China: Geographical and temporal distribution. Journal of Affective Disorders, 277, 893–900. 10.1016/j.jad.2020.08.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez‐Rey, R. , Garrido‐Hernansaiz, H. , & Collado, S. (2020). Psychological impact and associated factors during the initial stage of the coronavirus (COVID‐19) pandemic among the general population in Spain. Frontiers in Psychology, 11, 1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein, H. R. , Sutton, A. J. , & Borenstein, M. (2005). Publication bias in meta‐analysis. In: Rothstein H. R., Sutton A. J., & Borenstein M. (Eds.), Publication Bias in Meta‐Analysis: Prevention, Assessment and Adjustments (pp. 1‐7). : John Wiley & Sons, Ltd. [Google Scholar]
- Şahin, M. K. , Aker, S. , Şahin, G. , & Karabekiroğlu, A. (2020). Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID‐19 pandemic in Turkey. Journal of Community Health, 45(6), 1168–1177. 10.1007/s10900-020-00921-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, R. , Seth, S. , Solanki, H. K. , Mishra, N. , Srivastava, A. , & Jakhar, K. (2020). COVID‐19 and obstetrical care: Coping with new stress. Cureus, 12(12), e12116. 10.7759/cureus.12116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, L. , Lu, Z.‐A. , Que, J.‐Y. , Huang, X.‐L. , Liu, L. , Ran, M.‐S. , Gong, Y.‐M. , Yuan, K. , Yan, W. , Sun, Y.‐K. , Shi, J. , Bao, Y.‐P. , & Lu, L. (2020). Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Network Open, 3(7), e2014053. 10.1001/jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shochat, T. , Cohen‐Zion, M. , & Tzischinsky, O. (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. [DOI] [PubMed] [Google Scholar]
- Silva‐Costa, A. , Rotenberg, L. , Nobre, A. A. , Chor, D. , Aquino, E. M. , Melo, E. C. , Barreto, S. M. , Schmidt, M. I. , & Griep, R. H. (2020). Sex differences in the association between self‐reported sleep duration, insomnia symptoms and cardiometabolic risk factors: Cross‐sectional findings from Brazilian longitudinal study of adult health. Archives of Public Health, 78, 1–13. 10.1186/s13690-020-00429-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen, B. , Pallesen, S. , Friborg, O. , Nilsen, K. B. , Bakke, Ø. K. , Goll, J. B. , & Hopstock, L. A. (2021). Sleep patterns and insomnia in a large population‐based study of middle‐aged and older adults: The Tromsø study 2015–2016. Journal of Sleep Research, 30(1), e13095. 10.1111/jsr.13095 [DOI] [PubMed] [Google Scholar]
- Strong, C. , Lin, C. Y. , Jalilolghadr, S. , Updegraff, J. A. , Broström, A. , & Pakpour, A. H. (2018). Sleep hygiene behaviours in Iranian adolescents: An application of the theory of planned behavior. Journal of Sleep Research, 27(1), 23–31. 10.1111/jsr.12566 [DOI] [PubMed] [Google Scholar]
- Su, C.‐T. , Wang, J.‐D. , & Lin, C.‐Y. (2013). Child‐rated versus parent‐rated quality of life of community‐based obese children across gender and grade. Health and Quality of Life Outcomes, 11(1), 1–9. 10.1186/1477-7525-11-206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarokh, L. , Saletin, J. M. , & Carskadon, M. A. (2016). Sleep in adolescence: Physiology, cognition and mental health. Neuroscience and Biobehavioral Reviews, 70, 182. 10.1016/j.neubiorev.2016.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiete, J. , Guatteri, M. , Lachaux, A. , Matossian, A. , Hougardy, J.‐M. , Loas, G. , & Rotsaert, M. (2020). Mental health outcomes in healthcare workers in COVID‐19 and non‐COVID‐19 care units: A cross‐sectional survey in Belgium. Frontiers in Psychology, 11, 3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Gong, Y. , Chen, Z. , Wu, J. , Feng, J. , Yan, S. , Lv, C. , Lu, Z. , Mu, K. , & Yin, X. (2020). Sleep disturbances among Chinese residents during the Coronavirus Disease 2019 outbreak and associated factors. Sleep Medicine, 74, 199–203. 10.1016/j.sleep.2020.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, M. , Zhao, Q. , Hu, C. , Wang, Y. , Cao, J. , Huang, S. , Li, J. , Huang, Y. , Liang, Q. , Guo, Z. , Wang, L. , Ma, L. , Zhang, S. , Wang, H. , Zhu, C. , Luo, W. , Guo, C. , Chen, C. , Chen, Y. , … Yang, Y. (2020). Prevalence of psychological disorders in the COVID‐19 epidemic in China: A real world cross‐sectional study. Journal of Affective Disorders, 281, 312–320. 10.1016/j.jad.2020.11.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, S. , Ungvari, G. S. , Forester, B. P. , Chiu, H. F. , Wu, Y. , Kou, C. , Fu, Y. , Qi, Y. , Liu, Y. , Tao, Y. , Yu, Y. , Li, B. , & Xiang, Y.‐T. (2017). Gender differences in general mental health, smoking, drinking and chronic diseases in older adults in Jilin province, China. Psychiatry Research, 251, 58–62. 10.1016/j.psychres.2017.02.007 [DOI] [PubMed] [Google Scholar]
- Wang, S. , Xie, L. , Xu, Y. , Yu, S. , Yao, B. , & Xiang, D. (2020). Sleep disturbances among medical workers during the outbreak of COVID‐2019. Occupational Medicine, 70(5), 364–369. 10.1093/occmed/kqaa074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, W. , Song, W. , Xia, Z. , He, Y. , Tang, L. , Hou, J. , & Lei, S. (2020). Sleep disturbance and psychological profiles of medical staff and non‐medical staff during the early outbreak of COVID‐19 in Hubei Province, China. Frontiers in Psychiatry, 11, 733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X. , Chen, H. , Liu, L. , Liu, Y. , Zhang, N. , Sun, Z. , Lou, Q. , Ge, W. , Hu, B. , & Li, M. (2020). Anxiety and sleep problems of college students during the outbreak of COVID‐19. Frontiers in Psychiatry, 11, 588693. 10.3389/fpsyt.2020.588693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Zhu, L.‐Y. , Ma, Y.‐F. , Bo, H.‐X. , Deng, H.‐B. , Cao, J. , Wang, Y. , Wang, X.‐J. , Xu, Y. , Lu, Q.‐D. , Wang, H. , & Wu, X.‐J. (2020). Association of insomnia disorder with sociodemographic factors and poor mental health in COVID‐19 inpatients in China. Sleep Medicine, 75, 282–286. 10.1016/j.sleep.2020.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasim, T. , e Raana, G. , Bushra, N. , & Riaz, A. (2020). Effect of COVID‐19 pandemic on mental wellbeing of healthcare workers in tertiary care hospital. Annals of King Edward Medical University, 26(Special Issue), 140–144. [Google Scholar]
- WHO (2020). WHO Coronavirus Disease (COVID‐19) Dashboard. Retrieved 2020/10/19, from https://covid19.who.int/?gclid=Cj0KCQjw8rT8BRCbARIsALWiOvQVKIr7Qv‐_c3pE0T0De1netsJ4NqqqnydNM0DQstHyOl‐9s_T‐sZ4aAs2CEALw_wcB [Google Scholar]
- Wong, H. Y. , Mo, H. Y. , Potenza, M. N. , Chan, M. N. M. , Lau, W. M. , Chui, T. K. , Pakpour, A. H. , & Lin, C.‐Y. (2020). Relationships between severity of internet gaming disorder, severity of problematic social media use, sleep quality and psychological distress. International Journal of Environmental Research and Public Health, 17(6), 1879. 10.3390/ijerph17061879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia, Y. , Kou, L. , Zhang, G. , Han, C. , Hu, J. , Wan, F. , Yin, S. , Sun, Y. , Wu, J. , Li, Y. , Zhang, Z. , Huang, J. , Xiong, N. , & Wang, T. (2020). Investigation on sleep and mental health of patients with Parkinson's disease during the Coronavirus disease 2019 pandemic. Sleep Medicine, 75, 428–433. 10.1016/j.sleep.2020.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. , & Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID‐19) in January and February 2020 in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 26, e923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, M. , Wang, X. , Zhang, J. , & Wang, Y. (2021) Alteration in the psychologic status and family environment of pregnant women before and during the Covid‐19 pandemic. International Journal of Gynecology & Obstetrics, 153(1), 71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin, J. , Zhang, Y. , Tang, Y. , & Yang, Y. (2019). Brain differences between men and women: Evidence from deep learning. Frontiers in Neuroscience, 13, 185. 10.3389/fnins.2019.00185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav, R. , Yadav, P. , Kumar, S. S. , & Kumar, R. (2021). Assessment of depression, anxiety, and sleep disturbance in COVID‐19 patients at tertiary care centre of North India. Journal of Neurosciences in Rural Practice, 12, 316‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe, K. , Falvey, C. M. , & Hoang, T. (2014). Connections between sleep and cognition in older adults. The Lancet Neurology, 13(10), 1017–1028. 10.1016/S1474-4422(14)70172-3 [DOI] [PubMed] [Google Scholar]
- Zhang, C. , Yang, L. , Liu, S. , Ma, S. , Wang, Y. , Cai, Z. , Du, H. , Li, R. , Kang, L. , Meilei, S. , Zhang, J. , Liu, Z. , & Zhang, B. (2020). Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry, 11, 306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, J. , Xu, D. , Xie, B. , Zhang, Y. , Huang, H. , Liu, H. , Chen, H. , Sun, Y. , Shang, Y. , Hashimoto, K. , & Yuan, S. (2020). Poor‐sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID‐19: A retrospective cohort study. Brain, Behavior, and Immunity, 88, 50–58. 10.1016/j.bbi.2020.05.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X. , Liu, J. , Han, N. , & Yin, J. (2021). Social media use, unhealthy lifestyles, and the risk of miscarriage among pregnant women during the COVID‐19 pandemic: Prospective observational study. JMIR Public Health and Surveillance, 7(1), e25241. 10.2196/25241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Zhang, H. , Ma, X. , & Di, Q. (2020). Mental health problems during the COVID‐19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. International Journal of Environmental Research and Public Health, 17(10), 3722. 10.3390/ijerph17103722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, Y. , Shi, H. , Liu, Z. , Peng, S. , Wang, R. , Qi, L. , Li, Z. , Yang, J. , Ren, Y. , Song, X. , Zeng, L. , Qian, W. , & Zhang, X. (2020). The prevalence of psychiatric symptoms of pregnant and non‐pregnant women during the COVID‐19 epidemic. Translational Psychiatry, 10(1), 1–7. 10.1038/s41398-020-01006-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, Y. , Yang, Y. , Shi, T. , Song, Y. , Zhou, Y. , Zhang, Z. , Guo, Y. , Li, X. , Liu, Y. , Xu, G. , Cheung, T. , Xiang, Y.‐T. , & Tang, Y. (2020). Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID‐19 outbreak. Frontiers in Psychiatry, 11, 520. 10.3389/fpsyt.2020.00520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuo, K. , Gao, C. , Wang, X. , Zhang, C. , & Wang, Z. (2020). Stress and sleep: A survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID‐19 pandemic. General Psychiatry, 33(3), e100260. 10.1136/gpsych-2020-100260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zreik, G. , Asraf, K. , Haimov, I. , & Tikotzky, L. (2021). Maternal perceptions of sleep problems among children and mothers during the coronavirus disease 2019 (COVID‐19) pandemic in Israel. Journal of Sleep Research, 30(1), e13201. 10.1111/jsr.13201 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


