Abstract
Aims
This study examines the role of servant leadership through the mechanism of psychological safety in curbing nurses' burnout during the COVID‐19 pandemic.
Background
During the COVID‐19 pandemic, studies have shown an increased level of stress and burnout among health care workers, especially nurses. This study responds to the call for research to explore the mechanisms of servant leadership in predicting nurses' burnout by employing the perspective of conservation of resources theory.
Methods
Through a cross‐sectional quantitative research design, data were collected in three waves from 443 nurses working in Pakistan's five public sector hospitals. Data were analysed by employing the partial least squares path modelling (PLS‐PM) technique.
Results
Servant leadership (β = −0.318; 95% CI = 0.225, 0.416) and psychological safety (β = −0.342; CI = 0.143, 0.350) have an inverse relationship with nurses' burnout and explain 63.1% variance.
Conclusions
Servant leadership significantly reduces nurses' burnout, and psychological safety mediates this relationship.
Implications for Nursing Management
Human resource management policies in health care must emphasize training nursing leaders in servant leadership behaviour.
Keywords: conservation of resources theory, COVID‐19, nurses' burnout, psychological safety, servant leadership
1. INTRODUCTION
With over 172 million confirmed cases and 3.7 million deaths worldwide (World Health Organization, 2021), the severity of the COVID‐19 pandemic as a public health challenge has caused fear and physio‐psychological stress among health care workers. Amnesty International has collated the data of deaths in more than 70 countries and reported that as of March 2021, at least 17,000 health workers have died from COVID‐19. Health care workers, especially nurses involved in COVID‐19 treatments, are highly susceptible to adverse psychological outcomes. The suffering and death of patients bring traumatic experiences. Besides being the front‐line fighters, nurses are at a high risk of exposure to the disease (Domínguez‐Salas et al., 2021). Such negative emotions at the workplace may lead to nurses' burnout (Liu & Aungsuroch, 2019). Burnout at the workplace is defined as “the employees' negative response to chronic work stressors” (Vullinghs et al., 2018). Burnout is associated with emotional dysfunction, cognitive impairment, physical morbidity, fatigue, and sleep impairment (Schaufeli et al., 2009). Likewise, it is also linked to socio‐economic ramifications such as job dissatisfaction, increased turnover, reduced productivity at work (García‐Sierra et al., 2016), and withdrawal from the job in the shape of absenteeism or even intention to leave the nursing profession (Theodosius et al., 2021). A report published by the World Health Organization (2020) highlighted that to reach Sustainable Development Goal number three (health and well‐being), the world will need an additional nine million nurses and midwives by the year 2030. The significant shortages of nurses are in South East Asia and Africa. In the context of Pakistan, there was severe shortage of nurses, 1.3 million, even before the COVID‐19 pandemic. Thus, the factors that can subside burnout among nurses during COVID‐19 are an exciting avenue to be explored.
Literature has identified several predictors of burnout, that is, inadequate social support, organizational politics, bullying at the workplace, employer unfairness, and leadership (Hildenbrand et al., 2018). Leadership and burnout have been studied for transformational, ethical, authentic, and transactional leadership styles (Arnold et al., 2017; Hildenbrand et al., 2018; Laschinger et al., 2013; Lee et al., 2019). However, servant leadership has been given less attention in terms of its impact on work‐related burnout. Greenleaf (1977) coined the term servant leadership as an approach to leadership that emphasizes developing followers to their fullest potential in self‐motivation, task effectiveness, and community service. Despite receiving acceptable criticism regarding a distinctive theory (Bradley, 1999), servant leadership has gathered a reasonable share in research publications (Eva et al., 2019). Servant leadership is all about philosophy and practices that improve individuals' lives and focus more on creating better organizations and a caring world (Martin, 2018). In addition, servant leaders are concerned about emotional healing, altruism, and creating a better relationship with their followers. It is posited that these humanistic characteristics of servant leaders would be negatively associated with nurses' burnout during the COVID‐19 pandemic.
First, this study contributes by responding to suggestions of scholars to explore the intervening variables that serve as a mechanism in predicting the relationship between servant leadership and employees' outcomes (Faraz et al., 2019). The mechanism through which servant leadership influences nurses' burnout needs further research as the matter is yet not sufficiently clear. Chughtai (2016) found that servant leadership enhances the employees' psychological safety, which mediates feedback and voice behaviours. Second, responding to the call for research (Eva et al., 2019), this study investigates the relationship between servant leadership and nurses' burnout during the COVID‐19 pandemic in the backdrop of the conservation of resources (COR) theory. Third, it responds to the call by Edmondson (2014) for further research on antecedents and outcomes of psychological safety and is the first study to explore the mediating role of psychological safety between servant leadership and nurses' burnout relationship.
2. THEORY AND HYPOTHESES
2.1. Servant leadership and nurses burnout
Leaders are responsible for employees' work‐related well‐being by balancing their job resources and demands. A nurse servant leader seeks to determine the needs of their staff and frequently asks how they can support the team to resolve problems and promote their personal growth (Best, 2020). Servant leaders can effectively deal with job burnout among nurses because such leaders mainly focus on followers' well‐being (Coetzer et al., 2017). This support and positive association of leaders towards employees compels them to accomplish a meaningful outcome (Faraz et al., 2021) beneficial not only for the individuals but also for the organizations and the community (Coetzer et al., 2017).
Health care organizations strive to meet increased workload during the COVID‐19 pandemic, which has led to increased job burnout of the nurses. Job burnout, a stress reaction, is identified with three dimensions: emotional exhaustion, cynicism, and professional efficacy (Maslach et al., 1996; Xie et al., 2020). Emotional exhaustion is the result of resource depletion, and an individual feels the loss of control over what happens in his/her life. This emotional exhaustion leads to demotivation among employees (Maslach et al., 1996). Cynicism distrusts others' motives, while professional efficacy is a lack of interest in one's work (Leiter, 1997). The impact of job burnout is linked to both positive and negative outcomes. Scholars argued that burnout is associated with positive job performance, health, and negative behaviours such as absenteeism, job dissatisfaction, and higher turnover (Hunsaker, 2019).
Conservation of resources (COR) theory holds the tenet that individuals endeavour to acquire, protect, and foster those resources they centrally value. It comprehends and predicts work‐related stress, that is, burnout within specific work settings and cultures. COR posits that the occurrence of stress among individuals is subject to three conditions: (a) when an individual's essential resources are threatened with loss, (b) when critical resources are lost, and (c) when an individual fails to obtain the critical resources following significant effort (Hobfoll et al., 2018). Therefore, to overcome this threat of loss of resources or the loss of existing resources, individuals in response acquire and conserve resources for survival. These valuable resources for survival include social bonding, energy, and personal strength (Usman et al., 2020). To ensure survival and respond to stress, individuals employ relationships as critical resources.
Divya and Suganthi (2018) concluded that servant leaders reduce employee burnout. This study argues that servant leadership is a critical organizational resource that reduces nurses' burnout. Servant leaders emphasize more one‐to‐one communication with subordinates. By instilling motivation and self‐efficacy, servant leaders try to bring out the best in their followers, encouraging them to transform into servant leaders (Babakus et al., 2010). In this process, they act as role models for followers by supporting risk‐taking and pro‐active behaviour, encouraging them to speak about their concerns and intentions for others' well‐being. So, the servant leaders serve the nurses by acting as an organizational resource, which increases their motivation and eagerness to learn and grow. Thus, nurses supervised by servant leaders positively perceive the leaders as an essential resource during the time of crisis like COVID‐19. Therefore, grounded on the COR theory and on empirical evidence, we propose the following:
Hypothesis 1
Servant leadership is negatively related to nurses' burnout.
2.2. Mediating role of psychological safety
Psychological safety is an individual's perception concerning the consequences of risk‐taking, others' well‐being, and admitting mistakes (Erkutlu & Chafra, 2019). It refers to a situation where employees believe that they will not be punished for raising their voices and ideas, reporting mistakes, and sharing opinions (Edmondson & Lei, 2014). Leaders can play a critical role in employees' psychological safety (Dirik & Seren Intepeler, 2017) by dealing with the challenges of emotional exhaustion, cynicism, and professional efficacy. There is a call for the scholarship to examine the role of servant leadership in relation to psychological safety and burnout (Eva et al., 2018). Servant leaders facilitate nurses by creating a safe working environment where employees' mistakes are tolerated. A servant leader is characterized by empathy, healing, awareness, persuasion, stewardship, and commitment to subordinates' growth (Sherman, 2019). Such leaders focus on encouragement by empowering and lifting those who work for them (Karatepe et al., 2019): always look after staff's needs and work for the self‐development of subordinates (Lee et al., 2020). So, a servant leader naturally safeguards the psychological safety of the nurses. Such leaders follow the open communication approach. Leaders' accessibility to employees sends signals that it is safe to approach them. This high‐quality interpersonal relationship between a leader and his/her subordinate facilitates the introduction of psychological safety (Erkutlu & Chafra, 2019).
Leaders' support, trust, and open communication develop an atmosphere of psychological safety (Zhao, Ahmed, & Faraz, 2020), which helps nurses be less prone to work‐related stress, emotional exhaustion, cognitive impairment, and interpersonal risk effects at the workplace (Erkutlu & Chafra, 2019). Following COR theory, we argue that servant leaders show empathy, availability, and concern for their followers. These characteristics of servant leaders are perceived as a resource by the nurses and thus develop a sense of psychological safety (Iqbal et al., 2020). Nurses with a higher level of psychological resources, including psychological safety, will be motivated to invest those resources in coping with the workplace's challenges like burnout. Based on the above discussion, we posit that psychological safety acts as a mediator between a servant leadership and nurses' burnout (Figure 1). Therefore, the following are hypothesized:
Hypothesis 2a
Servant leadership is positively related to nurses' psychological safety.
Hypothesis 2b
Psychological safety is negatively related to nurses' burnout.
Hypothesis 2
Psychological safety mediates the relationship between servant leadership and nurses' burnout.
FIGURE 1.
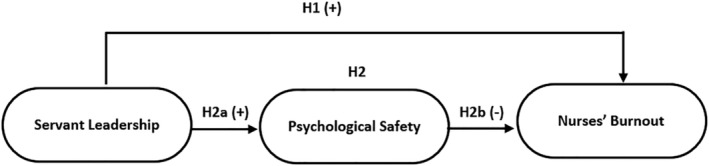
Theoretical model
3. METHODOLOGY
3.1. Sample and procedure
This study's population comprised nurses working in five sizeable public sector hospitals of Pakistan dealing with the COVID‐19 patients. Criteria for selecting hospitals include (i) employing at least 500 nurses, (ii) one from the four provincial capitals, and one from the capital city of Pakistan. The authors approached the HR department of the selected hospitals, explained the purpose of the study, ensured the participants' privacy, and sought approval for data collection. After getting approval from the HR department for data collection, a written request was made to provide the list of nurses' names and email addresses. The final consolidated list containing 3579 nurses from five hospitals was sorted alphabetically for every hospital. By employing systematic random sampling, every fourth nurse was shortlisted as a potential respondent. Researchers designed three separate survey forms to capture independent, mediator, and dependent variables on Google docs. The questionnaires were administered online separately at three time periods during February to March 2021 with a temporal separation of 10 days to overcome likely common method bias (Podsakoff et al., 2012). At the first time point, the questionnaire was administered to 895 nurses, wherein they were requested to provide demographic data and rate the servant leadership of their supervisors/head nurses. At the end of the first survey, 631 usable responses were received. After 10 days, at the second time point, questions about psychological safety were asked from those 631 nurses who participated in the initial survey. The second survey resulted in 512 responses complete in all aspects. At the third time point, 512 nurses who had participated in the first two surveys were requested to fill questions about burnout. Finally, we received 443 responses complete in all respects for all variables. The questionnaires were designed to do not accept missing values, so there were no missing values in the final data. The summarized demographics of the respondents are presented in Table 1.
TABLE 1.
Demographics of the participants
| Gender | Male | Female | |
|---|---|---|---|
| 26 (06%) | 417 (94%) | ||
| Age (in years) | 18–30 | 31–45 | Above 45 |
| 186 (42%) | 173 (39%) | 84 (19%) | |
| Experience (in years) | 01–10 | 11–20 | Above 20 |
| 155 (35%) | 195 (44%) | 93 (21%) | |
| Education | College/diploma | Bachelors | Masters and above |
| 75 (17%) | 266 (60%) | 102 (23%) |
3.2. Measures
A 7‐point Likert scale (1 = strongly disagree, 7 = strongly agree) was employed to solicit the participants' responses. The nurses' servant leadership was evaluated by the nurses' on a seven‐item measure of the global servant leadership (Liden et al., 2015). A typical item includes “My leader/head nurse emphasizes the importance of giving back to the community.” Since the development of the 7‐item measure of global servant leadership (SL‐7), researchers have widely used this scale, and it has established validity and reliability. Psychological safety was evaluated with a three‐item scale adapted by Detert and Burris (2007) from the original measure of psychological safety by Edmondson (1999). A sample item includes the following: “In this hospital, it is safe for me to make suggestions.” Burnout was assessed with 16 items from the Maslach Burnout Inventory‐General Survey (Maslach et al., 1996), commonly used with total score of the three dimensions, namely, exhaustion, cynicism, and professional efficacy. A sample item is “I feel emotionally drained from my work.”
4. ANALYSIS AND FINDINGS
Analysis of this study was performed by introducing the partial least squares path modelling (PLS‐PM) technique with the Smart‐PLS 3.3.3 software. The study in hand preferred the PLS‐PM method because of multiple reasons. First, it facilitates the analysis of multifaceted models comprising several constructs, indicators, and relationships (Ringle et al., 2018). Second, due to its dominance over other techniques while analysing mediation; third, it is particularly appropriate for prediction‐oriented studies (Zhao, Ahmed, Iqbal, et al., 2020), for instance, nurses' burnout. Fourth, it is equipped with the latest statistical tools, including confidence intervals for hypothesis testing, effect size to know the relative contribution of predictor constructs, graphs for moderation analysis, and heterotrait–monotrait (HTMT) ratio for discriminant validity. Lastly, comparatively, it offers better statistical power. PLS‐PM comprises a two‐stage approach for analysis (Hair et al., 2020), and for these reasons, its use has increased over the years in management research (Zhao, Ahmed, & Faraz, 2020; Zhao, Ahmed, Iqbal, et al., 2020) in recent years.
4.1. Confirmatory composite analysis (CCA)
Recently scholars have advanced confirmatory composite analysis (CCA) as a systematic methodological procedure for evaluating PLS‐PM measurement models (Hair et al., 2020). All other constructs have been treated as reflective lower‐order except burnout which is treated as higher‐order reflective‐reflective. The subsequent steps perform the CCA:
In the first step of CCA, the evaluation of the items' loadings was calculated. Under a two‐tailed test, an item is treated as signification if it has a loadings value above 0.708 and a t statistic above ±1.96 (Hair et al., 2020). Table 2 presents these statistics.
TABLE 2.
Confirmatory composite analysis (CCA)
| Constructs | Items code | Loading | t value | CI | |
|---|---|---|---|---|---|
| 5% | 95% | ||||
| CCA of the lower order reflective constructs | |||||
|
Servant leadership [α = 0.85, CR = 0.932, AVE = 0.663, VIF = 1.72] |
SL1 | 0.81 | 24.28 | 0.66 | 0.93 |
| SL2 | 0.83 | 22.28 | 0.69 | 0.87 | |
| SL3 | 0.82 | 25.15 | 0.62 | 0.76 | |
| SL4 | 0.81 | 16.05 | 0.55 | 0.79 | |
| SL5 | 0.79 | 18.01 | 0.41 | 0.60 | |
| SL6 | 0.81 | 19.95 | 0.56 | 0.71 | |
| SL7 | 0.83 | 22.18 | 0.44 | 0.85 | |
|
Exhaustion [α = 0.81, CR = 0.879, AVE = 0.592, VIF = 1.46] |
EX1 | 0.74 | 16.76 | 0.35 | 0.65 |
| EX2 | 0.79 | 17.57 | 0.48 | 0.70 | |
| EX3 | 0.75 | 18.88 | 0.19 | 0.53 | |
| EX4 | 0.71 | 12.26 | 0.42 | 0.67 | |
| EX5 | 0.85 | 26.69 | 0.50 | 0.82 | |
|
Cynicism [α = 0.80, CR = 0.875, AVE = 0.585, VIF = 1.86] |
CY1 | 0.73 | 12.25 | 0.29 | 0.53 |
| CY2 | 0.75 | 19.24 | 0.51 | 0.78 | |
| CY3 | 0.82 | 28.08 | 0.18 | 0.43 | |
| CY4 | 0.73 | 16.11 | 0.20 | 0.41 | |
| CY5 | 0.79 | 22.46 | 0.31 | 0.71 | |
|
Professional efficacy [α = 0.79, CR = 0.89, AVE = 0.581, VIF = 1.93] |
EF1 | 0.80 | 23.65 | 0.16 | 0.38 |
| EF2 | 0.76 | 14.70 | 0.16 | 0.64 | |
| EF3 | 0.74 | 13.53 | 0.33 | 0.75 | |
| EF4 | 0.72 | 18.58 | 0.27 | 0.81 | |
| EF5 | 0.81 | 21.40 | 0.41 | 0.73 | |
| EF6 | 0.74 | 17.79 | 0.39 | 0.88 | |
|
Psychological safety [α = 0.79, CR = 0.845, AVE = 0.646, VIF = 1.45] |
PS1 | 0.83 | 24.52 | 0.57 | 0.79 |
| PS2 | 0.80 | 25.70 | 0.35 | 0.65 | |
| PS3 | 0.78 | 21.36 | 0.44 | 0.73 | |
| CCA of the higher order reflective‐reflective construct | |||||
|---|---|---|---|---|---|
|
Nurses' burnout [α = 0.76, CR = 0.827, AVE = 0.614, VIF = 1.49] |
EX | 0.82 | 23.58 | 0.25 | 0.49 |
| CY | 0.76 | 15.40 | 0.41 | 0.69 | |
| EF | 0.77 | 17.79 | 0.19 | 0.64 | |
Note: t values and CI values were obtained by 5000 Bootstrap runs at two‐tailed significant at 5%.
Abbreviations: α, Cronbach's alpha; AVE, average variance extracted; CY, cynicism; CI, confidence interval; CR, composite reliability; EF, professional efficacy; Ex, exhaustion; VIF, variance inflation factor.
In the next step of CCA, reliability at the construct level was evaluated through the commonly used Cronbach's alpha (α) and composite reliability (CR) statistics. These statistics' standard range is between 0.70 to 0.95. Table 2 enlisted reliability metrics of the constructs. The third step of CCA ensured the convergent validity of the constructs. The average variance extracted (AVE) (Hair et al., 2019) was employed in this study. The AVE value above 0.50 is considered to explain more than 50% variance of the items constituting that construct. Table 2 enlists convergent validity statistics through the AVE metric.
The last step of CCA is to ensure the distinctiveness of the constructs. The latest guidelines have recommended the heterotrait–monotrait (HTMT) ratio of correlations. The standard values for HTMT should be below 0.90 (Hair et al., 2019). Table 3 confirms the distinctness of the constructs through the HTMT approach.
TABLE 3.
Mean, standard deviations, and discriminant validity through HTMT approach
| Mean | SD | NB | PS | SL | |
|---|---|---|---|---|---|
| Nurses' burnout | 4.73 | 0.87 | |||
| Psychological safety | 4.58 | 0.92 | 0.754 | ||
| Servant leadership | 4.64 | 1.07 | 0.598 | 0.584 |
Abbreviations: HTMT, heterotrait–monotrait; NB, nurses burnout; PS, psychological safety; SD, standard deviation; SL, servant leadership.
4.2. Structural model assessment (SMA)
Structural model assessment (SMA) was done by following the latest developments and guidelines on PLS‐PM, which includes the performance of the following steps:
In the first step of SMA, multicollinearity's potential issue was assessed through variance inflation factor (VIF) statistic. The latest guidelines suggest that its values should be less than three (Hair et al., 2020). Table 2 contained VIF values that are within the allowed limits.
The next step in SMA deals with the assessment of the direct and indirect hypothesized paths. The path coefficient (β) is one of the metrics for this purpose for which values were obtained through the bootstrapping procedure in the PLS algorithm. The guidelines for using and reporting SMA results suggested reporting percentile bootstrap confidence intervals (Hair et al., 2019). The values of confidence intervals must not contain the zero value for the structural path's statistical significance. Table 4 presents these metrics' values, which shows that the direct and indirect hypotheses have been supported.
TABLE 4.
Structural model assessment
| Structural paths | Path coefficient | t value | 95 percentile CI | Decision | |
|---|---|---|---|---|---|
| Control variables | |||||
| Gender → NB | 0.063 | 1.042 | [−0.019, 0.108] | n.s. | |
| Age → NB | −0.090 | 1.152 | [−0.022, 0.115] | n.s. | |
| Education → NB | 0.180 | 2.114 | [0.141, 0.238] | Significant | |
| Tenure → NB | −0.197 | 2.301 | [−0.214, −0.053] | Significant | |
| Direct hypotheses | |||||
| H1: SL → NB | −0.318 | 5.457 | [0.225, 0.416] | Supported | |
| H2‐a: SL → PS | 0.325 | 6.092 | [0.103, 0.338] | Supported | |
| H2‐b: PS → NB | −0.342 | 6.450 | [0.143, 0.350] | Supported | |
| Indirect hypothesis (mediation) | |||||
| H2: SL → PS → NB | 0.132 | 03.041 | [0.078, 0.229] | Supported | |
| Quality indicators | |||||
| R 2 Nurses' Burnout = 0.631 | Q 2 Nurses' Burnout = 0.349 | ||||
| R 2 Psychological Safety = 0.290 | Q 2 Psychological Safety = 0.152 | ||||
Note: p < 0.01; t values and CI values were obtained by 5000 Bootstrap runs at two‐tailed significant at 5%.
Abbreviations: CI, confidence interval; NB, nurses burnout; n.s., not significant; PS, psychological safety; Q2, predictive quality and strength; R 2, variance explained in predicted variable; SL, servant leadership.
In SMA, the third step deals with the assessment of in‐sample prediction wherein the coefficient of determination (R 2) and predictive relevance (Q 2) must be reported. The values of R 2 describe the percentage of variance in dependent variables(s) explained by the independent variable(s). Its values, 0.19, 0.33, and 0.67, are treated as small, moderate, and substantial, respectively (Chin, 1998). Figure 2 shows that structural model results with R 2 values for psychological safety (0.290) and nurses' burnout (0.631) are moderate.
FIGURE 2.
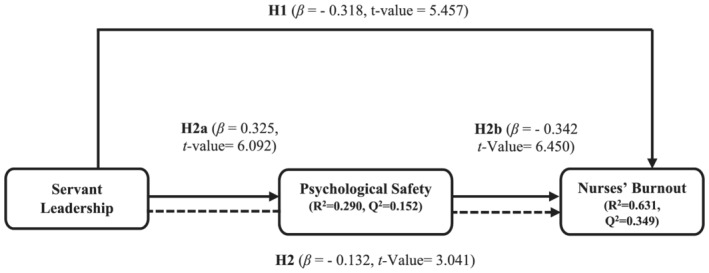
Structural model results
The predictive relevance (Q2) was employed to know the predictive accuracy of a structural model. The blindfolding procedure of PLS‐PM generated values for Q 2. The Q 2 values for psychological safety (0.152) and nurses' burnout (0.349) are well above the cut‐off zero value.
5. DISCUSSION
This study aimed to explore how servant leadership reduces nurses' burnout via the mediating mechanism of psychological safety. The findings lent credence to the direct effect of servant leadership on nurses' burnout and are consistent with the available handful of empirical studies on employee well‐being. According to COR (Hobfoll, 2018), employees strive to protect their resources. The types of job resources servant leaders provide to decrease burnout are organizational resources (organizational support), positional resources (job clarity), and social resources (supervisor support). Support refers to participating in decision‐making as well as personal growth and development opportunities. Servant leaders are sincerely concerned about the empowerment and independence of their subordinates. Such leaders believe in the emotional healing of subordinates and always behave ethically. The explanation of this finding could be twofold. First, it could mean that servant leaders provide the necessary job resources to buffer the adverse effects of high job demands that would typically cause burnout (Bakker et al., 2008). It could also mean that servant leaders provide the needed job resources to help employees recover from burnout. In other words, employees working under servant leaders might be less prone to burnout because they will receive the necessary job resources either to cope with high job demands or to recover from burnout. We operationalized nurses' burnout as having feelings of emotional exhaustion, cynicism, and personal inefficacy. The characteristics of the servant leadership model advanced by Liden et al. (2008) are highly relevant to the dimensions of burnout. Empowerment, emotional healing, and ethical behaviour reduce employees' feelings of emotionally about emotional exhaustion.
The psychological safety is supported by our findings as a mediator between the relationship of servant leadership and burnout. A psychologically safe working environment nurtured by servant leadership is one of the critical preconditions for reducing nurses' burnout. Precisely, psychological safety embodies employees' perceptions about their working environment instead of a specific task. When perceived safe, lower the risks of failure, rejection, and stress ultimately reduce burnout. Only one study has previously examined servant leadership's influence on employees' psychological safety (Chughtai, 2016). Therefore, this study adds a much‐needed contribution to the literature on servant leadership and burnout.
5.1. Implications for nursing management
Our findings offered several implications for nursing management. It offers a roadmap of how servant leadership reduces the potential burnout of nurses. In the face of epidemics, natural disasters and emergencies, the nursing leadership must ensure mental well‐being and psychological safety of the workforce for two main reasons. One, to avoid employee turnover and retain the existing workforce by reducing burnout from demanding job requirements; two, to avoid adverse events and outcomes at the hospitals during patient care.
There is need to train leaders in servant leadership behaviour to develop empathy so that they can monitor employees' mental well‐being by reducing emotional exhaustion through their support. When leaders are rude with their subordinates at the workplace may feel insecure and face psychological pressure, which leads to job burnout. This attitude from subordinates in an organization may prompt them to doubt their professional efficacy in handling the pressure. Even worse, subordinates could become cynical and deliberately harm the organization as they are not concerned about their jobs. Leaders must be proactive in their relationship with subordinates, and they must lead them with empathy to have a cordial relationship within the organization (Salvarani et al., 2019).
With a higher level of interpersonal acceptance accompanied by the element of empathy, servant leaders become able to cognitively adopt the psychological perspectives of others and experience feelings of warmth, compassion, and forgiveness when confronted with offenses, arguments, and mistakes. Head nurses with servant leadership approach build a close relationship with the nurses, listen to their opinions, involve them in decision making, encourage them to take risks for the betterment, and thus play a key role in cherishing employees' feelings of psychological safety.
According to Liden et al. (2008), servant leaders give liberty and provide emotional strength to their subordinates to recognize their full potential. The fulfilment of hospitals' job requirements, especially during emergency services, needs more emotional healing due to work‐related pressure. This study reconfirms the notion that head nurses with servant leadership style improves subordinates' job behaviour, which leads them to perform better.
6. LIMITATIONS AND FUTURE RESEARCH
This study, like any other research, has some limitations. At first, the cross‐sectional data collection design of this study confines its ability to offer causal inferences. For future studies, it is suggested to design a longitudinal investigation on this study's model with the methodology used by Ahmed et al. (2021) for their longitudinal study on psychological safety and psychological distress among nurses. Second, we collected data from a single source, likely leading to social acquiescence and desirability. It is recommended to collect multisource data, for example, supervisors, peers, and patients, to avoid biases in future studies. Lastly, this study included psychological safety as a mediator. Future studies may include organizational, team, and individual level constructs as mediators, for example, organizational support, leader‐identification, and psychological empowerment and moderating role of factors such as trust in leader, political skills of nursing staff, and perceptions of politics at work.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
ETHICS AND INFORMED CONSENT
The researchers met the hospital administration to explain the academic nature of the study and obtained approval to proceed with this study. The questionnaire included a clear statement assuring participants of complete anonymity, confidentiality, explained they had the right to withdraw anytime during the study, and that proceeding to fill in the questionnaire shall deem their informed consent. The study was not invasive did not involve any intervention or manipulation of the human subjects and participants were not vulnerable to any physical or psychological harm.
ACKNOWLEDGEMENTS
The authors acknowledge help of Dr. Muhammad Saood Akhtar for helping us revise this manuscript.
This research was partially supported by Independent Innovation Research Foundation (grant number 2020IVA079), Wuhan University of Technology, Wuhan, Hubei, China.
Ma Y, Faraz NA, Ahmed F, et al. Curbing nurses' burnout during COVID‐19: The roles of servant leadership and psychological safety. J Nurs Manag. 2021;29:2383-2391. 10.1111/jonm.13414
Ying Ma and Naveed Ahmad Faraz should be considered joint first authors.
Funding information Wuhan University of Technology, Grant/Award Number: 2020IVA079
Contributor Information
Dr. Naveed Ahmad Faraz, Email: naveedahmad@whut.edu.cn.
Dr. Fawad Ahmed, Email: fawadahmed1@live.com.
DATA AVAILABILITY STATEMENT
Author elects to not share data.
REFERENCES
- Ahmed, F. , Zhao, F. Q. , Faraz, N. A. , & Qin, Y. J. (2021). How inclusive leadership paves way for psychological well‐being of employees during trauma and crisis: A three‐wave longitudinal mediation study. Journal of Advanced Nursing, 77(2), 819–831. 10.1111/jan.14637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold, K. A. , Connelly, C. E. , Gellatly, I. R. , Walsh, M. M. , & Withey, M. J. (2017). Using a pattern‐oriented approach to study leaders: Implications for burnout and perceived role demand. Journal of Organizational Behavior, 38(7), 1038–1056. 10.1002/job.2182 [DOI] [Google Scholar]
- Babakus, E. , Yavas, U. , & Ashill, N. J. (2010). Service worker burnout and turnover intentions: Roles of person‐job fit, servant leadership, and customer orientation. Services Marketing Quarterly, 32(1), 17–31. 10.1080/15332969.2011.533091 [DOI] [Google Scholar]
- Bakker, A. B. , Schaufeli, W. B. , Leiter, M. P. , & Taris, T. W. (2008). Work engagement: An emerging concept in occupational health psychology. Work & Stress, 22(3), 187–200. 10.1080/02678370802393649 [DOI] [PubMed] [Google Scholar]
- Best, C. (2020). Is there a place for servant leadership in nursing? Practice Nursing, 31(3), 128–132. 10.12968/pnur.2020.31.3.128 [DOI] [Google Scholar]
- Bradley, Y. (1999). Servant Leadersip: A critique of Robert Greenleaf's concept of leadersip. Journal of Christian Education, 2, 43–54. 10.1177/002196579904200207 [DOI] [Google Scholar]
- Chin, W. W. (1998). The partial least squares approach to structural equation modeling. Modern Methods for Business Research, 295(2), 295–336. [Google Scholar]
- Chughtai, A. A. (2016). Servant leadership and follower outcomes: Mediating effects of organizational identification and psychological safety. The Journal of Psychology, 150(7), 866–880. 10.1080/00223980.2016.1170657 [DOI] [PubMed] [Google Scholar]
- Coetzer, M. F. , Bussin, M. H. , & Geldenhuys, M. (2017). Servant leadership and work‐related well‐being in a construction company. SA Journal of Industrial Psychology, 43(1), 1–10. 10.4102/sajip.v43i0.1478 [DOI] [Google Scholar]
- Detert, J. R. , & Burris, E. R. (2007). Leadership behavior and employee voice: Is the door really open? Academy of Management Journal, 50(4), 869–884. 10.5465/amj.2007.26279183 [DOI] [Google Scholar]
- Dirik, H. F. , & Seren Intepeler, S. (2017). The influence of authentic leadership on safety climate in nursing. Journal of Nursing Management, 25(5), 392–401. 10.1111/jonm.12480 [DOI] [PubMed] [Google Scholar]
- Divya, S. , & Suganthi, L. (2018). Influence of transformational‐servant leadership styles and justice perceptions on employee burnout: A moderated mediation model. International Journal of Business Innovation and Research, 15(1), 119–135. 10.1504/IJBIR.2018.088475 [DOI] [Google Scholar]
- Domínguez‐Salas, S. , Gómez‐Salgado, J. , Guillén‐Gestoso, C. , Romero‐Martín, M. , Ortega‐Moreno, M. , & Ruiz‐Frutos, C. (2021). Healthcare workers' protection and psychological safety during the COVID‐19 pandemic in Spain. Journal of Nursing Management, 10.1111/jonm.13331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmondson, A. (1999). Psychological safety and learning behavior in work teams. Administrative Science Quarterly, 44(2), 350–383. 10.2307/2666999 [DOI] [Google Scholar]
- Edmondson, A. (2014). Building a psychologically safe workplace: TEDx Talk. TedX. https://www.youtube.com/watch?v=LhoLuui9gX8
- Edmondson, A. C. , & Lei, Z. (2014). Psychological safety: The history, renaissance, and future of an interpersonal construct. Annual Review of Organizational Psychology and Organizational Behavior, 1(1), 23–43. 10.1146/annurev-orgpsych-031413-091305 [DOI] [Google Scholar]
- Erkutlu, H. , & Chafra, J. (2019). Leader psychopathy and organizational deviance: The mediating role of psychological safety and the moderating role of moral disengagement. International Journal of Workplace Health Management, 12(4), 197–213. 10.1108/IJWHM-12-2018-0154 [DOI] [Google Scholar]
- Eva, N. , Robin, M. , Sendjaya, S. , van Dierendonck, D. , & Liden, R. C. (2019). Servant leadership: A systematic review and call for future research. The Leadership Quarterly, 30(1), 111–132. 10.1016/j.leaqua.2018.07.004 [DOI] [Google Scholar]
- Eva, N. , Sendjaya, S. , Prajogo, D. , Cavanagh, A. , & Robin, M. (2018). Creating strategic fit: Aligning servant leadership with organizational structure and strategy. Personnel Review, 47(1), 166–186. 10.1108/PR-03-2016-0064 [DOI] [Google Scholar]
- Faraz, N. A. , Ahmed, F. , Ying, M. , & Mehmood, S. A. (2021). The interplay of green servant leadership, self‐efficacy, and intrinsic motivation in predicting employees' pro‐environmental behavior. Corporate Social Responsibility and Environmental Management. 10.1002/csr.2115 [DOI] [Google Scholar]
- Faraz, N. A. , Mughal, M. F. , Ahmed, F. , Raza, A. , & Iqbal, M. K. (2019). The impact of servant leadership on employees' innovative work behaviour‐mediating role of psychological empowerment. International Journal of Management Sciences and Business Research Administration, 5(11). [Google Scholar]
- García‐Sierra, R. , Fernández‐Castro, J. , & Martínez‐Zaragoza, F. (2016). Relationship between job demand and burnout in nurses: Does it depend on work engagement? Journal of Nursing Management, 24(6), 780–788. 10.1111/jonm.12382 [DOI] [PubMed] [Google Scholar]
- Greenleaf, R. K. (1977). Servant leadership: A journey into the nature of legitimate power and greatness (pp. 1–37). Paulist Press. [Google Scholar]
- Hair, J. F. Jr. , Howard, M. C. , & Nitzl, C. (2020). Assessing measurement model quality in PLS‐SEM using confirmatory composite analysis. Journal of Business Research, 109, 101–110. 10.1016/j.jbusres.2019.11.069 [DOI] [Google Scholar]
- Hair, J. F. , Risher, J. J. , Sarstedt, M. , & Ringle, C. M. (2019). When to use and how to report the results of PLS‐SEM. European Business Review, 31(1), 2–24. 10.1108/EBR-11-2018-0203 [DOI] [Google Scholar]
- Hildenbrand, K. , Sacramento, C. A. , & Binnewies, C. (2018). Transformational leadership and burnout: The role of thriving and followers' openness to experience. Journal of Occupational Health Psychology, 23(1), 31–43. 10.1037/ocp0000051 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. , Halbesleben, J. , Neveu, J.‐P. , & Westman, M. (2018). Conservation of resources in the organizational context: The reality of resources and their consequences. Annual Review of Organizational Psychology and Organizational Behavior, 5, 103–128. 10.1146/annurev-orgpsych-032117-104640 [DOI] [Google Scholar]
- Hunsaker, W. (2019). Spiritual leadership and job burnout: Mediating effects of employee well‐being and life satisfaction. Management Science Letters, 9(8), 1257–1268. [Google Scholar]
- Iqbal, A. , Latif, K. F. , & Ahmad, M. S. (2020). Servant leadership and employee innovative behaviour: Exploring psychological pathways. Leadership & Organization Development Journal, 41(6), 813–827. [Google Scholar]
- Karatepe, O. M. , Ozturk, A. , & Kim, T. T. (2019). Servant leadership, organisational trust, and bank employee outcomes. The Service Industries Journal, 39(2), 86–108. [Google Scholar]
- Laschinger, H. K. S. , Wong, C. A. , & Grau, A. L. (2013). Authentic leadership, empowerment and burnout: A comparison in new graduates and experienced nurses. Journal of Nursing Management, 21(3), 541–552. 10.1111/j.1365-2834.2012.01375.x [DOI] [PubMed] [Google Scholar]
- Lee, A. , Lyubovnikova, J. , Tian, A. W. , & Knight, C. (2020). Servant leadership: A meta‐analytic examination of incremental contribution, moderation, and mediation. Journal of Occupational and Organizational Psychology, 93(1), 1–44. 10.1111/joop.12265 [DOI] [Google Scholar]
- Lee, H. F. , Chiang, H. Y. , & Kuo, H. T. (2019). Relationship between authentic leadership and nurses' intent to leave: The mediating role of work environment and burnout. Journal of Nursing Management, 27(1), 52–65. 10.1111/jonm.12648 [DOI] [PubMed] [Google Scholar]
- Leiter, M. P. (1997). The truth about burnout: How organizations cause personal stress and what to do about it. Wiley. [Google Scholar]
- Liden, R. C. , Wayne, S. J. , Meuser, J. D. , Hu, J. , Wu, J. , & Liao, C. (2015). Servant leadership: Validation of a short form of the SL‐28. The Leadership Quarterly, 26(2), 254–269. 10.1016/j.leaqua.2014.12.002 [DOI] [Google Scholar]
- Liden, R. C. , Wayne, S. J. , Zhao, H. , & Henderson, D. (2008). Servant leadership: Development of a multidimensional measure and multi‐level assessment. The Leadership Quarterly, 19(2), 161–177. 10.1016/j.leaqua.2008.01.006 [DOI] [Google Scholar]
- Liu, Y. , & Aungsuroch, Y. (2019). Work stress, perceived social support, self‐efficacy and burnout among Chinese registered nurses. Journal of Nursing Management, 27(7), 1445–1453. 10.1111/jonm.12828 [DOI] [PubMed] [Google Scholar]
- Martin, A. G. (2018). Serving those who serve: An examination of the relationship between servant leadership and employee burnout in healthcare. Our Lady of the Lake University. [Google Scholar]
- Maslach, C. , Jackson, S. , Leiter, M. , Schaufeli, W. , & Schwab, R. (1996). Maslach Burnout Inventory–General Survey. MBI Manual, 19–26.
- Podsakoff, P. M. , MacKenzie, S. B. , & Podsakoff, N. P. (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. 10.1146/annurev-psych-120710-100452 [DOI] [PubMed] [Google Scholar]
- Ringle, C. M. , Sarstedt, M. , Mitchell, R. , & Gudergan, S. P. (2018). Partial least squares structural equation modeling in HRM research. The International Journal of Human Resource Management, 31(12), 1617–1643. [Google Scholar]
- Salvarani, V. , Rampoldi, G. , Ardenghi, S. , Bani, M. , Blasi, P. , Ausili, D. , Di Mauro, S. , & Strepparava, M. G. (2019). Protecting emergency room nurses from burnout: The role of dispositional mindfulness, emotion regulation and empathy. Journal of Nursing Management, 27(4), 765–774. 10.1111/jonm.12771 [DOI] [PubMed] [Google Scholar]
- Schaufeli, W. B. , Leiter, M. P. , & Maslach, C. (2009). Burnout: 35 years of research and practice. Career Development International, 14, 204–220. 10.1108/13620430910966406 [DOI] [Google Scholar]
- Sherman, R. O. (2019). The case for servant leadership. Elsevier. 10.1016/j.mnl.2018.12.001 [DOI] [Google Scholar]
- Theodosius, C. , Koulouglioti, C. , Kersten, P. , & Rosten, C. (2021). Collegial surface acting emotional labour, burnout and intention to leave in novice and pre‐retirement nurses in the United Kingdom: A cross‐sectional study. Nursing Open, 8(1), 463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usman, M. , Ali, M. , Yousaf, Z. , Anwar, F. , Waqas, M. , & Khan, M. A. S. (2020). The relationship between laissez‐faire leadership and burnout: Mediation through work alienation and the moderating role of political skill. Canadian Journal of Administrative Sciences/Revue Canadienne des Sciences de l'Administration, 37(4), 423–434. [Google Scholar]
- Vullinghs, J. T. , De Hoogh, A. H. , Den Hartog, D. N. , & Boon, C. (2018). Ethical and passive leadership and their joint relationships with burnout via role clarity and role overload. Journal of Business Ethics, 165(4), 719–733. [Google Scholar]
- World Health Organization (2020). Nursing and midwifery. https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery [Google Scholar]
- World Health Organization (2021). WHO Coronavirus (COVID‐19) dashboard. https://covid19.who.int/ [Google Scholar]
- Xie, C. , Li, X. , Zeng, Y. , & Hu, X. (2020). Mindfulness, emotional intelligence and occupational burnout in intensive care nurses: A mediating effect model. Journal of Nursing Management, 29(3), 535–542. [DOI] [PubMed] [Google Scholar]
- Zhao, F. , Ahmed, F. , & Faraz, N. A. (2020). Caring for the caregiver during COVID‐19 outbreak: Does inclusive leadership improve psychological safety and curb psychological distress? A cross‐sectional study. International Journal of Nursing Studies, 110, 103725. 10.1016/j.ijnurstu.2020.103725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, F. , Ahmed, F. , Iqbal, M. K. , Mughal, M. F. , Qin, Y. J. , Faraz, N. A. , & Hunt, V. J. (2020). Shaping behaviors through institutional support in British higher educational institutions: Focusing on employees for sustainable technological change. Frontiers in Psychology, 11(3382). 10.3389/fpsyg.2020.584857 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Author elects to not share data.


