Abstract
Children with autism spectrum disorder (ASD) are at elevated risk for psychiatric problems in response to the COVID‐19 pandemic. This risk is due to their high rates of pre‐pandemic psychiatric comorbidities and the pandemic's disruption to routines and access to necessary supports. Prior research has indicated that children with ASD may experience a worsening of specific psychiatric symptoms in response to COVID‐19, though this body of work is limited in scope. The present study expands this literature by examining specific types of psychiatric problems that emerged about 2 months after the onset of the pandemic, and risk factors predicting changes in these psychiatric symptoms. Parents of children with a confirmed ASD diagnosis (N = 257), who enrolled in a clinic registry at an outpatient specialty autism center, were included in this study. All data were gathered online via customized and standardized questionnaires. Results showed that 59% of children experienced either a worsening of their pre‐pandemic psychiatric diagnoses and/or the development of new psychiatric symptoms during the pandemic. Multivariable regression models indicated that risk factors for increased psychiatric problems included child understanding of COVID‐19, COVID‐19 illness in the family, low family income, and elevated parental depression and anxiety symptoms (all p < 0.05). Findings from this study emphasize the urgent need to provide effective and accessible psychiatric services for children with ASD and their families during and after the pandemic.
Lay summary
Children with ASD are at high risk for psychiatric problems during the COVID‐19 pandemic. We found that 59% of children in our clinical sample are experiencing increased psychiatric problems. The child's understanding of COVID‐19, COVID‐19 illness in the family, low family income, and depression and anxiety symptoms in the parent increase the risk for poor mental health during the pandemic. These findings indicate the importance of helping children with ASD access mental health treatment during COVID‐19.
Keywords: autism spectrum disorder, COVID‐19, children, psychiatric problems
INTRODUCTION
The impact of the COVID‐19 pandemic on the mental health of children with autism spectrum disorder (ASD) is of significant concern. This population is more likely than children without ASD to experience distress during the pandemic because they thrive on routines and external supports, which have been disrupted due to rigorous social distancing guidelines (Cassidy et al., 2020; White et al., 2021). Additionally, children with ASD have higher rates of psychiatric disorders compared to children without ASD, which are likely to exacerbate in the midst of pandemic‐related stressors (Joshi et al., 2010).
Research on psychiatric outcomes during the pandemic in children with ASD is beginning to emerge across the globe. Several survey studies indicate that, within the first few months of the pandemic, children with ASD are already experiencing higher levels of psychiatric symptoms such as anxiety, irritability, aggression, and sleep problems than before the pandemic (Amorim et al., 2020; Colizzi et al., 2020; Mutluer et al., 2020; Nonweiler et al., 2020). Pre‐existing behavior problems and parental anxiety have been identified as factors for these outcomes (Colizzi et al., 2020; Mutluer et al., 2020). A few qualitative studies have reported that COVID‐19 specific risk factors, including COVID‐19 impact on the family and the child's understanding of COVID‐19, may be risk factors for child psychiatric problems; however, quantitative data are needed to support narrative‐based findings (Asbury et al., 2020; O'Sullivan et al., 2021).
More data are urgently needed on psychiatric outcomes and their risk factors during COVID‐19 in children with ASD to inform policies and interventions. This study addresses the need by examining a broad range of psychiatric sequelae and risk factors during the pandemic including both child COVID‐19 understanding and COVID‐19 illness in the family. Based on prior research, we expect that pre‐existing psychiatric disorders will exacerbate during COVID‐19, and that parental mental health will predict psychiatric outcomes (Colizzi et al., 2020; Mutluer et al., 2020). We have no a priori hypothesis about other risk factors, as these have not been studied.
METHOD
Participants
This cross‐sectional online survey study was conducted from May 2020 to June 2020, 2 months after the World Health Organization declared the COVID‐19 pandemic. Participants were parents of children with ASD who were enrolled in a clinic research registry at the (BLINDED). Parents were invited to enroll in the registry at their child's initial appointment, thereby providing consent to be contacted for future research studies; 85% of parents enroll (BLINDED). The (BLINDED) approved the registry and this study.
For this study, children in the registry were retrospectively identified for inclusion based on the following criteria: (1) the child must have a diagnosis of ASD that was either established or confirmed by expert clinicians at (BLINDED), (2) the child must be between 2 and 16.9 years, (3) the parent must be English‐speaking. Parents of 3217 eligible children were sent an email that included an informational study video, a consent form, and instructions to complete the survey. Parents subsequently received two reminders to complete the survey; 257 (8%) responded. The survey took about 1.5 h to complete. Incentives were not provided.
Measures
The study authors developed a customized questionnaire for the primary caregiver that asked about parent demographic variables (race, education, household income, marital status, number of family members), the child's verbal ability, COVID‐19 impact on the family (loss of income, work in essential sectors, change in employment, COVID‐19 diagnosis in the family, COVID‐19 death in the family), and child psychiatric problems. Income groups were: low (<$35,000), middle ($35,000‐74,999), high ($75,000‐149,999), highest (≥$150,000) (See Supplement 1 for survey).
Parents of verbal children were asked four questions about their child's awareness of COVID‐19 as presented in Table 1: (a) child knows what COVID‐19 is, (b) parent talked about COVID‐19, (c) child asked about COVID‐19, (d) child aware of COVID‐19 in the family. A positive response to any of these questions indicated that the child was aware of COVID‐19. Parents of nonverbal children were asked only the questions that did not require a verbal response from the child (questions (a) and (b)). Since COVID‐19 awareness is dependent on the child's verbal ability, COVID‐19 awareness and verbal ability were combined to form a categorical variable called COVID‐19 understanding (Groups: Nonverbal, Verbal + No COVID‐19 awareness, Verbal + COVID‐19 awareness). The nonverbal group was considered the reference group because we could not be certain about their COVID‐19 awareness since no parent reported that their child knew about COVID‐19, and only 18% of parents talked to their child about COVID‐19.
TABLE 1.
Sample characteristics
| All children (N = 257) | No increased psychiatric problems (N = 106, 41%) | Increased psychiatric problems (N = 151, 59%) | |
|---|---|---|---|
| Parent demographic variables | |||
| Race | |||
| White | 140 (55.3) | 53 (52.0) | 87 (57.6) |
| Black | 75 (29.6) | 32 (31.4) | 43 (28.5) |
| Other a | 38 (15.0) | 17 (16.7) | 21 (13.9) |
| Education | |||
| High school degree/GED | 50 (19.8) | 20 (19.6) | 30 (19.9) |
| Trade school/Associate's | 48 (19.0) | 14 (13.7) | 34 (22.5) |
| College graduate | 62 (24.5) | 33 (32.4) | 29 (19.2) |
| Graduate degree | 93 (36.8) | 35 (34.3) | 58 (38.4) |
| Income*** | |||
| Less than 35,000 | 54 (22.1) | 12 (12.5) | 42 (28.4) |
| $35,000 ‐ $74,999 | 42 (17.2) | 26 (27.1) | 16 (10.8) |
| $75,000 ‐ $149,999 | 80 (32.8) | 36 (37.5) | 44 (29.7) |
| $150,000 or over | 68 (27.9) | 22 (22.9) | 46 (31.1) |
| Number of parents in the home | |||
| 1 | 57 (23.0) | 17 (17.2) | 40 (26.8) |
| 2 | 191(77.0) | 82 (82.8) | 109 (73.2) |
| Child characteristics | |||
| Child ageb | 9.12 (3.80) | 8.31 (3.88) | 9.69 (3.64) |
| Child sex | |||
| F | 50 (19.5) | 16 (15.1) | 34 (22.5) |
| M | 207 (80.5) | 90 (84.9) | 117 (77.5) |
| Child language level | |||
| Nonverbal, single words | 49 (19.2) | 24 (23.1) | 25 (16.6) |
| Verbal, short phrases | 38 (14.9) | 19 (18.3) | 19 (12.6) |
| Verbal, short sentences | 43 (16.9) | 17 (16.3) | 26 (17.2) |
| Verbal, fluent | 125 (49.0) | 44 (42.3) | 81 (53.6) |
| Child COVID‐19 awareness | |||
| Know what COVID‐19 is?* | |||
| No | 82 (38.7) | 39 (48.8) | 43 (32.6) |
| Yes | 130 (61.3) | 41 (51.2) | 89 (67.4) |
| Talked to child about COVID‐19?* | |||
| No | 70 (29.4) | 34 (38.2) | 36 (24.2) |
| Yes | 168 (70.6) | 55 (61.8) | 113 (75.8) |
| Child asked about COVID‐19?** | |||
| No | 120 (50.6) | 55 (61.8) | 65 (43.9) |
| Yes | 117 (49.4) | 34 (38.2) | 83 (56.1) |
| Child aware of family member with COVID‐19 who passed away?*** | |||
| No | 209 (92.5) | 83 (100) | 126 (88.1) |
| Yes | 17 (7.52) | 0 (0.00) | 17 (11.9) |
| Total number of children with COVID‐19 awareness | |||
| No | 67 (28.0) | 34 (37.8) | 33(22.1) |
| Yes | 172 (72.0) | 56 (62.2) | 116 (77.9) |
| Total number of children with COVID‐19 understanding* b | |||
| Nonverbal | 49 (20.4) | 24 (26.4) | 25 (16.8) |
| Verbal, no awareness | 28 (11.7) | 15 (16.5) | 13 (8.7) |
| Verbal, awareness | 163 (67.9) | 52 (57.1) | 111 (74.5) |
| COVID‐19 impact | |||
| Loss of income | |||
| No | 170 (69.1) | 68 (69.4) | 102 (68.9) |
| Yes | 76 (30.9) | 30 (30.6) | 46 (31.1) |
| Either parent or partner deemed essential worker and has work remained open? | |||
| No | 81 (32.5) | 30 (30.3) | 51 (34.0) |
| Yes | 168 (67.5) | 69 (69.7) | 99 (66.0) |
| COVID‐19 affected your employment status? | |||
| No | 179 (72.5) | 73 (73.7) | 106 (71.6) |
| Yes | 68 (27.5) | 26 (26.3) | 42 (28.4) |
| Anyone in family ever have a diagnosis of COVID‐19? | |||
| No | 225 (94.9) | 87 (97.8) | 138 (93.2) |
| Yes | 12 (5.1) | 2 (2.2) | 10 (6.8) |
| Anyone in the family or close to the family pass away from COVID‐19? | |||
| No | 236 (98.3) | 90 (100) | 146 (97.3) |
| Yes | 4 (1.67) | 0 (0.00) | 4 (2.67) |
| Parent mental health | |||
| Custom questionnaire*** | 9.54 (3.35) | 8.21 (2.69) | 10.3 (3.47) |
Other includes Asian, Hispanic/Spanish origin, and an unspecified other group.
COVID‐19 awareness corresponds to a yes to any one of the four COVID‐19 knowledge questions. COVID‐19 understanding is a composite variable that consists of COVID‐19 awareness plus verbal ability.
p ≤ 0.001; **p ≤ 0.01; *p ≤ 0.05.
The survey also asked parents three questions about their child's psychiatric status: (1) Has their child been diagnosed with any psychiatric conditions by a professional prior to the COVID‐19 pandemic (yes/no), (2) If yes, was there a change in the severity of the condition since COVID‐19 began (less severe, about the same, more severe, do not know), and (3) Has their child developed any new symptoms or behaviors since COVID‐19 began (yes/no)? If the child had a pre‐pandemic diagnosis, the parents were asked about all new symptoms except those pertaining to the pre‐pandemic diagnoses (e.g., those with a pre‐pandemic anxiety disorder were not asked about new onset anxiety). The outcome for this study, increased psychiatric problems during the pandemic, was therefore a composite variable reflecting either worsening of at least one pre‐pandemic psychiatric condition and/or the development of at least one new psychiatric symptom. A total of nine psychiatric conditions were assessed (see Figure 1).
FIGURE 1.
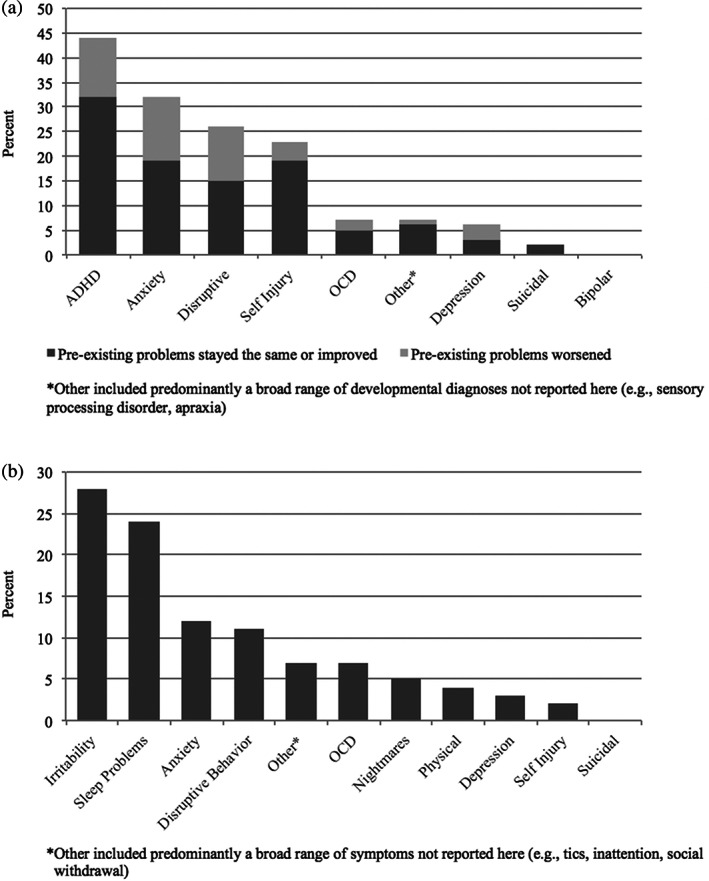
Changes in psychiatric symptoms 2 months into the COVID‐19 pandemic
Parents reported on their own level of anxiety and depression by completing a 5‐item custom questionnaire that asked about anxiety, depression, loneliness, hopefulness, and physical reactions in the past 7 days (Holingue et al., 2020).
Data analysis
Descriptive statistics were used to explore child psychiatric problems prior to and during the pandemic. Child, parent, and environmental variables were compared between children with and without increased psychiatric problems using t‐tests or chi‐square. Variables significantly associated with this outcome (p ≤ 0.05) and all COVID‐19 impact variables were included together in a multivariable logistic regression model to identify independent risk factors for increased psychiatric problems. Variables entered into the regression include age, income, COVID‐19 understanding, COVID‐19 diagnosis in the family, and parent mental health.
RESULTS
The sample consisted of 257 children and adolescents (M = 9.1 years, SD = 3.8 years, median = 8.9 years, range = 2–16.5 years, males = 80.5%, verbally fluent = 49%). Table 1 presents the sample characteristics according to children who did and did not experience increased psychiatric problems during the pandemic.
Overall, 64% of children had a prior psychiatric condition, of which 41% experienced a worsening of these problems. Over half (53%) of the sample developed new symptoms, of which 29% had no pre‐existing psychiatric problems. When combined, 59% experienced either a worsening of their pre‐pandemic psychiatric diagnoses and/or the development of new psychiatric symptoms (see Appendix S2 for more detailed data on pre‐ and post‐ psychiatric problems).
Figure 1a presents the percentage of children with pre‐existing psychiatric problems. The most common pre‐pandemic psychiatric problems were ADHD (44%), anxiety (32%), and disruptive behavior (26%). The most common pre‐existing psychiatric problems that exacerbated were depression (8 of 15 cases; 53%), disruptive behavior (28 of 65 cases; 44%), and anxiety disorder (33 of 80 cases; 42%).
Figure 1b presents the percentage of children with new psychiatric symptoms irrespective of pre‐existing psychiatric status. The most common new symptoms were irritability (28%), sleep problems (24%), anxiety (12%), and disruptive behavior (11%). These were also the most common new symptoms in children without pre‐existing psychiatric problems, i.e., irritability (26%), anxiety (22%), and sleep problems (19%).
Risk factors for increased psychiatric problems included: 1) COVID‐19 diagnosis in the family (OR = 5.06; 95% CI = 1.01, 25.25; p = 0.05), child COVID‐19 understanding (OR = 2.66; 95% CI = 1.06, 6.69; p = 0.04), and higher parental psychopathology symptoms (OR = 1.28; 95% CI = 1.15, 1.43; p < 0.001). Regarding income, the middle and high income groups were less likely to have increased psychiatric problems compared to the low income group (middle: OR = 0.24; 95% CI = 0.08, 0.72, p = 0.01; high: OR = 0.25, 95% CI = 0.09, 0.66, p = 0.01), however, this protective effect did not significantly extend to the highest income families (highest: OR = 0.5; 95% CI = 0.18, 1.39, p = 0.18).
DISCUSSION
We found that within 2 months of the onset of COVID‐19, almost 60% of children with ASD experienced increased psychiatric problems. About 45% of the sample had a worsening of their pre‐existing psychiatric disorder, and over 50% of children developed new symptoms. Among those who developed new psychiatric symptoms, nearly one‐third had no prior psychiatric problems. A broad range of psychiatric problems manifested in our sample. Although relatively infrequent, pre‐existing depression was most likely to exacerbate, followed by disruptive behavior and anxiety disorders. The most common new symptoms were irritability, sleep, and anxiety. These findings highlight the heavy toll and persistence of psychiatric morbidity in the ASD population during the pandemic.
Several correlates of increased psychiatric problems were identified including those uniquely pertaining to COVID‐19, that is, child COVID‐19 understanding and COVID‐19 in the family. In our study, verbal children with COVID‐19 understanding were at increased risk for psychiatric problems. These children likely absorbed large amounts of pandemic information through news, social media, and directly witnessing or hearing about a family member with COVID‐19. This influx can be difficult to understand and cope with, thereby triggering psychiatric problems (Depoux et al., 2020). With regards to nonverbal children, our study may not have adequately assessed COVID‐19 understanding in this subgroup with the two knowledge questions in the survey. Further research is necessary to develop approaches to best capture awareness and its association with psychopathology in children with ASD. It will also be important to consider other COVID‐19 related factors (e.g., disruptions in routines, social isolation, and hygiene regulations) when determining psychiatric risk.
Next, we found that low family income increased risk for psychiatric symptoms in children with ASD. This finding aligns with recent research highlighting significant socioeconomic health inequities in other populations (e.g., adults) during the pandemic (Ettman et al., 2020; Rudenstine et al., 2021). Parents of children with ASD with low income may be more vulnerable to employment loss, experience greater challenges finding care for their child, and struggle to access basic amenities. These findings indicate that policies and supports are needed to protect this vulnerable group to minimize their impact on child mental health.
Finally, we found that parental depression and anxiety symptoms positively correlated with child psychiatric problems. This finding is unsurprising given the overwhelming stress that parents of children with ASD may be experiencing during this time. Disruptions in routines, isolation, acute financial strain, and other stressors (Rivard et al., 2014) can affect both their own as well as their child's mental health. Conversely, increased psychiatric problems in children with ASD (e.g., disruptive behavior) could aggravate parent mental health (Falk et al., 2014; Manning et al., 2020).
Findings from this study highlight the need to expeditiously refer children with ASD for mental health treatment and maintain continuity of care, both during and possibly after the pandemic. Efforts to strengthen the access to and delivery of telehealth services for this population are needed, including parent management training to target disruptive behavior, cognitive behavioral therapy for anxiety and depression, and psychopharmacological monitoring of response and adverse events (Bearss et al., 2018; Hepburn et al., 2016). Our findings also emphasize a family‐centered treatment approach by asking about COVID‐19 illness in the family, referring parents for their own mental health treatment, and offering parents strategies to talk with their children about COVID‐19. Lastly, it is critical to connect low‐income families to mental health services and available community‐based supports to help them secure basic necessities.
This study has strengths and limitations. For strengths, expert clinicians established the child's ASD diagnosis, the analyses examined a broad range of psychiatric problems and risk factors, and the results yielded novel findings pertaining to COVID‐19 understanding in the child and COVID‐19 illness in the family. Limitations include the low response rate, which introduces selection biases and hinders generalization, and the use of a single informant and unstandardized survey, which could affect parent reporting of child psychiatric problems and COVID‐19 awareness. Another limitation is that our questionnaire did not assess whether worsening pre‐existing disorders or new symptoms reached a level of clinical significance or represented normative variations over time. We were also unable to examine interaction effects or characteristics of children whose psychiatric disorders improved, due to the small number of children with improvement in all of their pre‐existing psychiatric disorders and who developed no new symptoms. Finally, we could not determine if new symptoms represented an exacerbation of pre‐existing problems. Despite these limitations, our findings provide an important glimpse of the psychiatric vulnerabilities of children with ASD during the pandemic. Future studies during later stages of the pandemic and the reintegration to school and routines are needed to understand the trajectory of psychiatric problems and their risk factors in this population.
CONFLICT OF INTEREST
Dr. Vasa receives royalties for an edited book on childhood anxiety disorders published by Humana Press.
ETHICS STATEMENT
The Johns Hopkins Medicine Institutional Review Board approved this study.
Supporting information
Appendix S1. Supplement 1: COVID‐19 Mental Health Survey Questions
Appendix S2. Data on Pre‐ and Post‐ Pandemic Psychiatric Outcomes
ACKNOWLEDGMENTS
Dr. Amy Keefer is funded by the Organization for Autism Research Applied Research Award (2019A06). Dr. Roma A. Vasa is funded by the Organization for Autism Research Applied Research Award and the Kennedy Krieger Institute Goldstein Innovation Award. Dr. Luther G. Kalb is funded by the Eunice Kennedy Shriver National Institute on Child Health and Development (#U54 HD079123), the Capital Group, and the Organization for Autism Research Applied Research Award (2019A05). Dr. Calliope Holingue, Ms. Vini Singh and Mr. Yeon Jang have no funding sources to acknowledge.
Vasa, R. A. , Singh, V. , Holingue, C. , Kalb, L. G. , Jang, Y. , & Keefer, A. (2021). Psychiatric problems during the COVID‐19 pandemic in children with autism spectrum disorder. Autism Research, 14(10), 2113–2119. 10.1002/aur.2574
Funding information Capital Group, and the Organization for Autism Research Applied Research Award, Grant/Award Number: 2019A05; Eunice Kennedy Shriver National Institute on Child Health and Development, Grant/Award Number: #U54 HD079123; Organization for Autism Research Applied Research Award and the Kennedy Krieger Institute Goldstein Innovation Award; Organization for Autism Research Applied Research Award, Grant/Award Number: 2019A06
REFERENCES
- Amorim, R. , Catarino, S. , Miragaia, P. , Ferreras, C. , Viana, V. , & Guardiano, M. (2020). The impact of COVID‐19 on children with autism spectrum disorder. Impacto de la COVID‐19 en niños con trastorno del espectro autista. Revista de Neurologia, 71(8), 285–291. 10.33588/rn.7108.2020381 [DOI] [PubMed] [Google Scholar]
- Asbury, K. , Fox, L. , Deniz, E. , Code, A. , & Toseeb, U. (2020). How is COVID‐19 affecting the mental health of children with special educational needs and disabilities and their families? Journal of Autism and Developmental Disorders, 51(5), 1772–1780. 10.1007/s10803-020-04577-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearss, K. , Burrell, T. L. , Challa, S. A. , Postorino, V. , Gillespie, S. E. , Crooks, C. , & Scahill, L. (2018). Feasibility of parent training via telehealth for children with autism spectrum disorder and disruptive behavior: A demonstration pilot. Journal of Autism and Developmental Disorders, 48(4), 1020–1030. 10.1007/s10803-017-3363-2 [DOI] [PubMed] [Google Scholar]
- Cassidy, S. A. , Nicolaidis, C. , Davies, B. , Rosa, S. , Eisenman, D. , Morénike, G. O. , Kapp, S. , Kripke, C. , Rodgers, J. , & Waisman, T. C. (2020). An expert discussion on autism in the COVID‐19 pandemic. Autism in Adulthood, 2, 106–117. 10.1089/aut.2020.29013.sjc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi, M. , Sironi, E. , Antonini, F. , Ciceri, M. L. , Bovo, C. , & Zoccante, L. (2020). Psychosocial and behavioral impact of COVID‐19 in autism spectrum disorder: An online parent survey. Brain Sciences, 10(6), 341. 10.3390/brainsci10060341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depoux, A. , Martin, S. , Karafillakis, E. , Preet, R. , Wilder‐Smith, A. , & Larson, H. (2020). The pandemic of social media panic travels faster than the COVID‐19 outbreak. Journal of Travel Medicine, 27(3). 10.1093/jtm/taaa031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman, C. K. , Abdalla, S. M. , Cohen, G. H. , Sampson, L. , Vivier, P. M. , & Galea, S. (2020). Low assets and financial stressors associated with higher depression during COVID‐19 in a nationally representative sample of US adults. Journal of Epidemiology and Community Health, 75, 501–508. 10.1136/jech-2020-215213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk, N. H. , Norris, K. , & Quinn, M. G. (2014). The factors predicting stress, anxiety and depression in the parents of children with autism. Journal of Autism and Developmental Disorders, 44(12), 3185–3203. 10.1007/s10803-014-2189-4 [DOI] [PubMed] [Google Scholar]
- Hepburn, S. L. , Blakeley‐Smith, A. , Wolff, B. , & Reaven, J. A. (2016). Telehealth delivery of cognitive‐behavioral intervention to youth with autism spectrum disorder and anxiety: A pilot study. Autism, 20(2), 207–218. 10.1177/1362361315575164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holingue, C. , Badillo‐Goicoechea, E. , Riehm, K. E. , Veldhuis, C. B. , Thrul, J. , Johnson, R. M. , Fallin, M. D. , Kreuter, F. , Stuart, E. A. , & Kalb, L. G. (2020). Mental distress during the COVID‐19 pandemic among US adults without a pre‐existing mental health condition: Findings from American trend panel survey. Preventive Medicine, 139, 106231. 10.1016/j.ypmed.2020.106231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi, G. , Petty, C. , Wozniak, J. , Henin, A. , Fried, R. , Galdo, M. , Kotarski, M. , Walls, S. , & Biederman, J. (2010). The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: A large comparative study of a psychiatrically referred population. Journal of Autism and Developmental Disorders, 40(11), 1361–1370. 10.1007/s10803-010-0996-9 [DOI] [PubMed] [Google Scholar]
- Manning, J. , Billian, J. , Matson, J. , Allen, C. , & Soares, N. (2020). Perceptions of families of individuals with autism spectrum disorder during the COVID‐19 crisis. Journal of Autism and Developmental Disorders, 1–9. 10.1007/s10803-020-04760-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutluer, T. , Doenyas, C. , & Aslan Genc, H. (2020). Behavioral implications of the COVID‐19 process for autism spectrum disorder, and individuals' comprehension of and reactions to the pandemic conditions. Frontiers in Psychiatry, 11, 561882. 10.3389/fpsyt.2020.561882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonweiler, J. , Rattray, F. , Baulcomb, J. , Happé, F. , & Absoud, M. (2020). Prevalence and associated factors of emotional and behavioural difficulties during COVID‐19 pandemic in children with neurodevelopmental disorders. Children, 7(9), 128. 10.3390/children7090128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Sullivan, K. , Clark, S. , McGrane, A. , Rock, N. , Burke, L. , Boyle, N. , Joksimovic, N. , & Marshall, K. (2021). A qualitative study of child and adolescent mental health during the COVID‐19 pandemic in Ireland. International Journal of Environmental Research and Public Health, 18(3), 1062. 10.3390/ijerph18031062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivard, M. , Terroux, A. , Parent‐Boursier, C. , & Mercier, C. (2014). Determinants of stress in parents of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44(7), 1609–1620. 10.1007/s10803-013-2028-z [DOI] [PubMed] [Google Scholar]
- Rudenstine, S. , McNeal, K. , Schulder, T. , Ettman, C. K. , Hernandez, M. , Gvozdieva, K. , & Galea, S. (2021). Depression and anxiety during the COVID‐19 pandemic in an urban, low‐income public university sample. Journal of Traumatic Stress, 34(1), 12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, L. C. , Law, J. K. , Daniels, A. M. , Toroney, J. , Vernoia, B. , Xiao, S. , SPARK Consortium , Feliciano, P. , & Chung, W. K. (2021). Brief report: Impact of COVID‐19 on individuals with ASD and their caregivers: A perspective from the SPARK cohort. Journal of Autism and Developmental Disorders, 1–8. 10.1007/s10803-020-04816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supplement 1: COVID‐19 Mental Health Survey Questions
Appendix S2. Data on Pre‐ and Post‐ Pandemic Psychiatric Outcomes


