Abstract
In spring 2020, the COVID-19 pandemic was declared. The threat the pandemic poses as well as associated lockdown measures created challenging times for many. This study aimed to investigate the individual and social factors associated with low mental health, particularly perceived threat and lockdown measures, and factors associated with psychological well-being, particularly sense of control. An online survey was completed by participants (N = 8,229) recruited from 79 countries. In line with pre-registered hypotheses, participants showed elevated levels of anxiety and depression worldwide. This poor mental health was predicted by perceived threat. The effect of threat on depression was further moderated by social isolation, but there was no effect of sense of control. Sense of control was low overall, and was predicted negatively by maladaptive coping, but positively by adaptive coping and the perception that the government is dealing with the outbreak. Social isolation increased with quarantine duration, but was mitigated by frequent communication with close ones. Engaging in individual actions to avoid contracting the virus was associated with higher anxiety, except when done professionally. We suggest that early lockdown of the pandemic may have had detrimental psychological effects, which may be alleviated by individual actions such as maintaining frequent social contact and adaptive coping, and by governmental actions which demonstrate support in a public health crisis. Citizens and governments can work together to adapt better to restrictive but necessary measures during the current and future pandemics.
Keywords: COVID-19, Mental health, Quarantine, Sense of control, Social isolation, Government action
Lay Summary
The COVID-19 pandemic is a difficult time for many; not only are people isolated at home, they may also experience the threat that COVID-19 will have a severe impact on their lives. We ran an online survey with 8,229 individuals from 79 countries in April 2020. After establishing levels of psychological well-being, we investigated which factors contribute to better psychological well-being, and which to worse. We found that levels of anxiety and depression were markedly elevated worldwide. The more people thought that COVID-19 was going to have severe effects on their lives, the more anxious and depressed they felt. This effect was even stronger when the individuals felt socially isolated, which was increased when people had been in quarantine for a long time, but reduced when people frequently communicated with their close ones. People felt more in control of their lives when they engaged in positive coping behaviors, such as reframing their situation positively, but not negative coping behaviors, such as substance use. People also felt in control when their government was dealing with the crisis well. We conclude that there are several ways in which psychological well-being can be supported, in the current pandemic but also potential future pandemics.
Adaptive coping strategies and keeping in touch with close ones may help increase low psychological wellbeing resulting from concern about COVID-19 and social isolation during lockdown.
Implications.
Practice: Measures to support social connection between individuals in isolation, and to provide assistance and guidance with adaptive coping and the avoidance of maladaptive coping will likely be most instrumental in contributing to psychological well-being in the pandemic.
Policy: In order to support psychological well-being during the current but also potential future pandemics, policymakers should ensure that governments demonstrate support in a public health crisis by showing capability, benevolence, and integrity in dealing with the crisis, such as through communicating clearly, reinforcing a sense of togetherness, and providing resources.
Research: Future research can identify what factors can contribute to a sufficiently increased sense of control (associated with psychological well-being) in catastrophic times such as COVID-19 pandemic where many people struggle to find a sense of control through the usual channels.
Introduction
On March 11, 2020, the COVID-19 outbreak was declared a pandemic by the World Health Organisation (WHO). Billions of people were suddenly faced with the threat of catching the virus and the threat of financial and job uncertainty, and potential social isolation as a result of lockdown measures. How might this combination of threat and lockdown measures impact mental health and what factors might contribute to alleviate their negative impact during the pandemic? To address this question, we asked participants (N = 8,236) worldwide who had been living in social isolation (range 0–110 days, M = 23.0, SD = 9.5 days), to answer a pre-registered online survey (from March 28 until April 24, 2020) which included measures of perceived personal threat, anxiety, and depression. Pre-registered analyses sought to assess how various factors, particularly exacerbating (e.g., threat) and mitigating factors (e.g., social contact), may be associated with mental health outcomes. In addition, we investigated what may be associated with a sense of personal control during the pandemic, a factor which we predicted would be associated with better psychological well-being.
Threat, Lockdown, and Mental Health Model
The pandemic brings with it high levels of uncertainty: No one can accurately predict how the pandemic will progress. Thus, the level of perceived threat includes a projection of one’s fears concerning the likelihood of becoming ill or dying (for oneself or one’s family), or of losing one’s job, among other threatening possibilities. For example, levels of perceived threat may be based on number of diagnoses in one’s community, one’s perceived risk of contracting the virus, and one’s personal financial situation, given that the pandemic has substantially increased unemployment (e.g., in the USA, the unemployment rate went from a range of 3.5–3.7% to 4.4% in March, and then shot to 14.7% in April and 13.3% in May [1]).
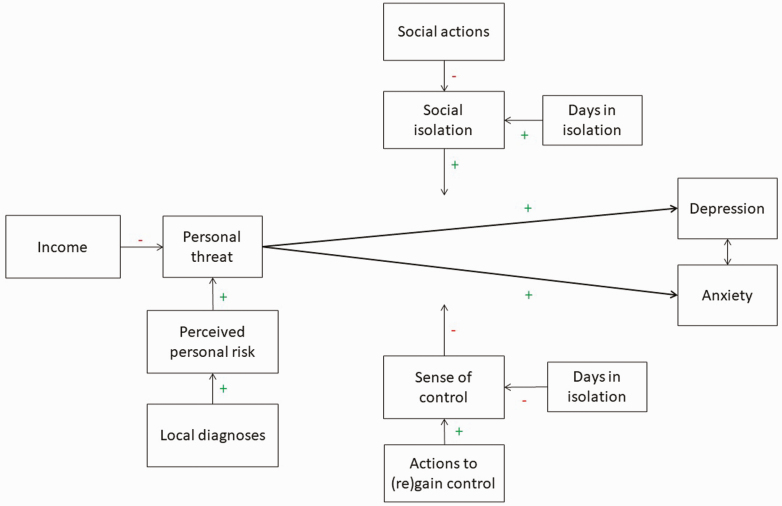
However, perceived threat does not necessarily dictate psychological ill health. Individuals may engage with various behaviors in order to help them deal with the negative aspects of lockdown; here, we suggest that these mitigating factors will moderate the effect of perceived threat on psychological well-being. Such behaviors include staying in contact with close others, taking actions to avoid contracting the virus (e.g., washing one’s hands), and engaging in adaptive coping mechanisms (e.g., reframing the situation in a positive light). Together, these behaviors can give a sense of control and togetherness, and manifest resilience in the face of a threat, thus avoiding anxiety and depression—see Fig. 1 for the Threat, Lockdown, and Mental Health Model, and Table 1 at the end of the introduction for an overview of the pre-registered hypotheses. We also considered external factors that might contribute to people’s mental health during lockdown. For example, the number of days spent in isolation potentially affects stress levels, though not necessarily in a linear fashion. In the early days of lockdown, a “novelty effect” of lockdown may be expected, reflecting initial low levels of stress, which after this initial adjustment phase may be followed by a spike of the negative effects of lockdown. This in turn may decrease in time due to habituation.
Fig 1 |.
The Threat, Lockdown, and Mental Health Model; explaining the effect of personal threat and lockdown consequences (social isolation and reduced sense of control) on depression and anxiety, and factors that may mitigate or exacerbate the effect.
Table 1 |.
Overview of pre-registered hypotheses and models
| Model | Hypotheses |
|---|---|
| Threat, Lockdown, and Mental Health Model | Personal threat will be predicted by the perceived risk of contracting the virus, which in turn is predicted by contagion rates in one’s environment. Finances will further negatively impact threat. |
| Levels of social connectedness are predicted by the social actions one takes; levels of sense of control are predicted by actions to regain control (at the individual or governmental level). | |
| Days in isolation will have a quadratic effect on social connectedness and perceived sense of control: initially, levels will be high as isolation does not yet take grip, and later on they will be low as individuals will have adapted to isolation. | |
| Antecedents of Control Model | A perceived sense of control is predicted by (a) frequency of behaviors taken to avoid contracting the virus, (b) communicating with close others, and (c) other types of coping behavior. |
| In addition, sense of control is predicted by how often an individual consults information sources, and this relationship is moderated by the level of trust in these sources. | |
| A perceived sense of control is further predicted by the extent to which governments take actions to deal with the COVID-19 pandemic, and this relationship is moderated by the level of trust in the government. |
Antecedents of Control Model
The state of emergency issued by many countries, which severely restricted freedom of movement, has led to an inevitable decrease in direct control over one’s environment. Therefore, we hypothesized that sense of control would be particularly affected, and that people would engage in actions to regain this control. There are two main processes for achieving control: primary or personal control, which is the ability to influence the environment in response to personal needs, and secondary or compensatory control, which is the ability to adapt the self in response to the environment [2, 3]. Having a sense of control over one’s environment is considered a fundamental motivation [4], and a perceived lack of control is directly associated with poor mental health outcomes [5].
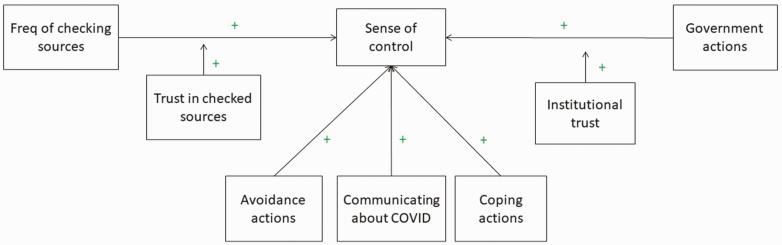
Although the level of direct control over a pandemic is, for most of us, negligible, we hypothesize that there are various behaviors which will impact one’s sense of control, through both primary and secondary pathways: individuals can take actions on their own to try reducing the risk of contracting the virus (e.g., avoiding physical contact with others) and to gather information about the disease (through checking news sources or through communicating with others), but they can also gain a sense of control without attempting to change the current situation, such as by trusting the government to take effective action in order to control the pandemic [6]; see Fig. 2 for the Antecedents of Control Model, and Table 1 for the hypotheses).
Fig 2 |.
Antecedents of Control Model; explaining how a sense of control may be achieved through primary and secondary control mechanisms during the COVID-19 pandemic.
METHODS
Pre-registration
We pre-registered our models and analyses at the Open Science Framework (https://doi.org/10.17605/OSF.IO/TSJNB) while data collection was ongoing but prior to examining the data and running analyses.
Ethics
University ethics approval was obtained prior to data collection. All participants read the participant information page and signed an online consent form.
Procedure
Data was collected via an online survey hosted by Qualtrics. The survey was online from March 28 to April 24, 2020, and was advertised on social media, including international COVID-19 groups on Facebook and Reddit. In a snowballing method, the survey link was also e-mailed through the social networks of the authors.
Participants
We collected data from 8,236 participants. Of these, seven individuals were excluded on the basis of pre-registered criteria (Supplementary Materials, SM.2). The resulting data set contained responses from 8,229 participants, of whom 3245 male (39.4%), 4888 female (59.4%), and 91 other/non-binary (1.1%). Age ranged from 18 to 88 years old (M = 38.3, SD = 13.5). In descending order of total number of responses, we obtained responses from the following countries: USA (n = 2167), UK (n = 1082), Italy (n = 1029), Brazil (n = 884), Australia (n = 489), the Netherlands (n = 489), Portugal (n = 367), Germany (n = 282), France (n = 237), Finland (n = 219), Croatia (n = 209), and New Zealand (n = 194), with remaining responses divided among 67 countries with fewer than 100 responses each (total participants n = 377). See Supplementary Materials, SM.3 for an overview of the descriptive statistics (gender, age, education levels, days in isolation) and situation (e.g., mandatory self-isolation, key worker) of the participants from the top 12 countries.
Measures
See Supplementary Materials, SM2.3 for example items of the scales. Scoring options were kept similar across scales as much as possible. Standard quantity options were: “Not at all” (0), “A little” (1), “A moderate amount” (2), “A lot” (3), to “A great deal” (4). Standard frequency options were: “Never” (0), “Rarely” (1), “Occasionally” (2), “Sometimes, more than occasionally” (3), “Often” (4), “All the time” (5)1. For income, government action, and institutional trust, an option “I’d rather not say” was also provided, which was excluded from the analyses. For frequency of communication about COVID-19, the option “We do not communicate/NA” was excluded from the analyses.
Demographics
Demographics included: Country of residence; age (in years); gender (female, male, or other/non-binary); level of education in nine tiers, from “No schooling completed, or less than 1 year” (1) to “Doctorate degree (PhD, EdD, etc.)” (9); household income from “Far below average” (−2) to “Far above average” (2); essential worker job (medical profession; delivery or post personnel, supermarket or shop personnel, garbage or recycling collection; driver in public transport; nursery/childcare/education employee; construction worked; police or armed forces; other; none of the above).
Diagnoses
Participants were asked to indicate whether there had been diagnoses of COVID-19 in any of their environment(s). Options were: no, or global: in my country, in my state/province/county, in my city, and local: in my workplace, school, or children’s nursery, my acquaintances, my close friends, my family, my household, and I’m infected. Answers (yes = 1, no = 0) were summed in global and local scores.
Days of self-isolation
Participants were asked how many days they had been in in self-isolation (voluntary or mandatory).
Anxiety and depression
The Hospital Anxiety and Depression Scale [7] was used to measure symptoms of anxiety and depression, with 7 items each. Example of items for anxiety are: “I get a sort of frightened feeling as if something awful is about to happen.”; examples for depression are: “I feel as if I am slowed down.” The score per item is 0–3, total 0–21. We summed the scores to compare to Zigmond and Snaith’s [7] criteria levels: a score of 7 or less reflected “non-cases,” scores of 8–10 were “doubtful cases” and scores of 11 or more were “definite cases.” In addition, scores of 11–14 were considered “moderate,” and 15–21 “severe” [8]. We also computed averages for anxiety (α = .861) and depression (α = .778), as sum scores are not robust to missing values in structural equation models.
Threat
We measured threat by asking participants how severe they thought the effects of COVID-19 would be on their personal lives (personal threat) and on global society (global threat). Options for answers were: “Not at all” (0), “A little” (1), “Somewhat” (2), “Considerably” (3), “Very” (4), and “Extremely” (5). We used personal threat as a single-item measure, meaning we cannot compute reliability.
Perceived risk
We asked participants to rate, for themselves and their family/close friends, the risk of becoming infected, of experiencing a severe version of the infection, and of dying from the infection. These questions were answered on a scale from “Very low” (−2), “Low” (−1), “Neither low nor high” (0), “High” (1), to “Very high” (2). These scores were averaged (α = .787).
Sense of control
We used two items to measure sense of control: “Currently, do you feel that you are the actor in, or the director of, your life?” and “Is the amount of control you experience in life right now lower or higher than you would want, or is it just right?.” Both questions were measured on a sliding scale from −10 to 10 to create an average score (α = .664).
Social isolation
Four items of the Social Connectedness Scale [9] measured social isolation. Example: “I catch myself losing all sense of connectedness with society.” These scores were averaged (α = .885).
Social actions
Social actions were measured by the frequency with which participants were in contact with their family, friends, and colleagues/fellow students, either through the exchange of messages, calls, or video chats. Options were: “not once/NA” (0), “few times a month” (1), “weekly” (2), “few times a week” (3), “once a day” (4), to “few times a day” (5). These scores were averaged (α = .824).
Avoidance actions
Avoidance actions were measured by COVID-19 safety precautions, adapted from a concurrent Stanford survey [10]. Participants were asked: “In the past week, how much have you made it a priority to…” followed by each of 12 actions, including “Wash your hands for at least 20 s,” “Stay home,” and “Wear a mask of any kind.” Options were: “Not at all” (0), “A little bit” (1), “Some” (2), “A lot” (3), to “As much as possible” (4). Scores were averaged (α = .757).
PPE availability for essential workers
Key workers in the sample were asked whether they had access to sufficient personal protective equipment (PPE), on a slider from “Not sufficient; nothing” (−10) to “Sufficient; plenty” (10).
Information actions
Participants were asked how often they consulted, and how much they trusted, nine different sources for information about COVID-19, including: the World Health Organization (WHO), national health services, government website(s), newspaper website(s), Facebook, Twitter, Instagram, websites with maps or tables with COVID-19 cases counts, and websites following Google searches about COVID-19. The response options were: “Never” (0), “Rarely” (1), “Occasionally” (2), “Sometimes, more than occasionally” (3), “Often” (4), “All the time” (5) for frequency; and “Not at all” (0), “A little” (1), “A moderate amount” (2), “A lot” (3), to “A great deal” (4) for quantity of trust.
Frequency of communication about COVID-19
Participants were asked how often they spoke about COVID-19 with family, friends, and colleagues/fellow students by exchanging messages, calling, and video chatting. The response options were “Never” (0), “Rarely” (1), “Occasionally” (2), “Sometimes, more than occasionally” (3), “Often” (4), “All the time” (5), and scores were averaged (α = .824).
Coping actions
The Brief COPE scale [11] was used, which consists of 28 items reflecting adaptive (e.g., using emotional support; α = .785) and maladaptive coping (e.g., substance use; α = .714).
Government actions
We included six government actions that help in making quarantine experiences tolerable [12], including: Telling people what is happening and why; Explaining how long it will continue; Providing meaningful activities for people to do while in quarantine; Providing clear communication; Ensuring basic supplies (such as food, water, and medical supplies) are available; Reinforcing a sense of togetherness. Participants were asked to indicate how much they think the government of the country they reside in has accomplished these actions. The response options were: “Not at all” (0), “A little” (1), “A moderate amount” (2), “A lot” (3), to “A great deal” (4). These scores were averaged (α = .906).
Institutional trust
Institutional trust was measured through three factors: capability, integrity, and benevolence [6], measured by two items each. Participants were asked “To what degree do you perceive that..” followed by the items, including “the government is capable of stopping the COVID-19 outbreak?” (capability, α = .783); “…the actions of the government in regard to COVID-19 outbreak are driven by sound values and principles?” (benevolence, α = .885); “…the government tries to counteract COVID-19 outbreak?” (integrity, α = .885). Together, these items constituted institutional trust (α = .913). The response options were: “Not at all” (0), “A little” (1), “A moderate amount” (2), “A lot” (3), to “A great deal” (4). For USA respondents, questions were also asked about state capability (α = .811), state benevolence (α = .921), and state integrity (α = .924), together forming state institutional trust (α = .933).
Perceived knowledge
Participants were asked how informed they felt with regards to four aspects of COVID-19: The risk of contracting COVID-19, symptoms of COVID-19, how COVID-19 spreads, how to prevent COVID-19 from spreading. Participants were also asked how informed they felt about the treatment of COVID-19, but this option was removed as it was considered too medically niche. Participants were asked to include in their judgment how much they felt they knew, and how much they trusted that information. The response options were: “Not at all” (0), “A little” (1), “A moderate amount” (2), “A lot” (3), to “A great deal” (4). These scores were averaged (α = 880).
Actual knowledge
To examine how informed the participants were, four facts were gleaned from the WHO’s WhatsApp list of common COVID-19 myths, and participants were asked to indicate if they thought them to be true or false, or to indicate that they did not know. The answer to all fact statements was “False”: Only people of a certain age can get COVID-19; Pets can transmit COVID-19; Vaccines against pneumonia provide protection against COVID-19. (We also had a fact statement “Taking antibiotics is effective against COVID-19,” but this was removed when it was pointed out that antibiotics do help with the recovery of pneumatic infection following COVID-19). The sum of all “false” (i.e., correct) answers was used as an indicator of actual knowledge.
One of the main hypotheses of this study was that having information in times of threat would increase psychological well-being. Having information was measured through either actual or perceived knowledge (i.e., being or feeling informed). Upon closer inspection, it appeared that the actual knowledge variable has too little variance to meaningful test in this sample. None of the participants got all four myths wrong: correctly judging each of the 4 myths (n = 6924, 84.3%), 3 myths (n = 1212, 14.8%), 2 myths (n = 71, 0.9%), 1 myth (n = 8, 0.1%), 0 myths (n = 0). As such, this variable has been excluded from the analyses.
Analyses
All analyses were conducted in R [R Team, [13]], using the lme4 package for linear regressions [14], lavaan for structural equation modelling [15], ggplot2 for plotting figures [16], and tidySEM for plotting SEM graphs [17]. This project follows the Workflow for Open Reproducible Code in Science [18]. Regression analyses allow countries (of residence) to have random intercepts, and conditional R2 and ICC which take these effects into account [19] have been reported. All analysis scripts are publicly available on our project on Open Science Framework (https://doi.org/10.17605/OSF.IO/TSJNB).
Power analyses
Using the semPower package in R [20], we conducted a post-hoc power analysis for the Threat, Lockdown, and Mental Health Model, and found that a sample size of N = 8229 is associated with a power larger than > 99.99 % (more precisely, 1 - 9.812621e-116) to reject a wrong model (with df = 27) with an amount of misspecification corresponding to RMSEA = .06 on alpha = .05. Using G*Power [21], post-hoc power analyses for our main two regressions, predicting sense of control and reduced anxiety, confirmed sufficient power (>.99) for the effect sizes f2 = .24 and .64 for the regressions, respectively (f2 calculated from regression R2 with the formula R2/(1-R2)), given N = 8229, an alpha-level of .05, and 9 predictors.
Translations
The survey was translated from English into Italian, French, Dutch, German, Portuguese, Brazilian Portuguese, and Spanish by native speakers (an author or a colleague familiar with surveys), and checked by another native speaker. See our project on Open Science (https://doi.org/10.17605/OSF.IO/TSJNB) for all full versions of the survey.
RESULTS
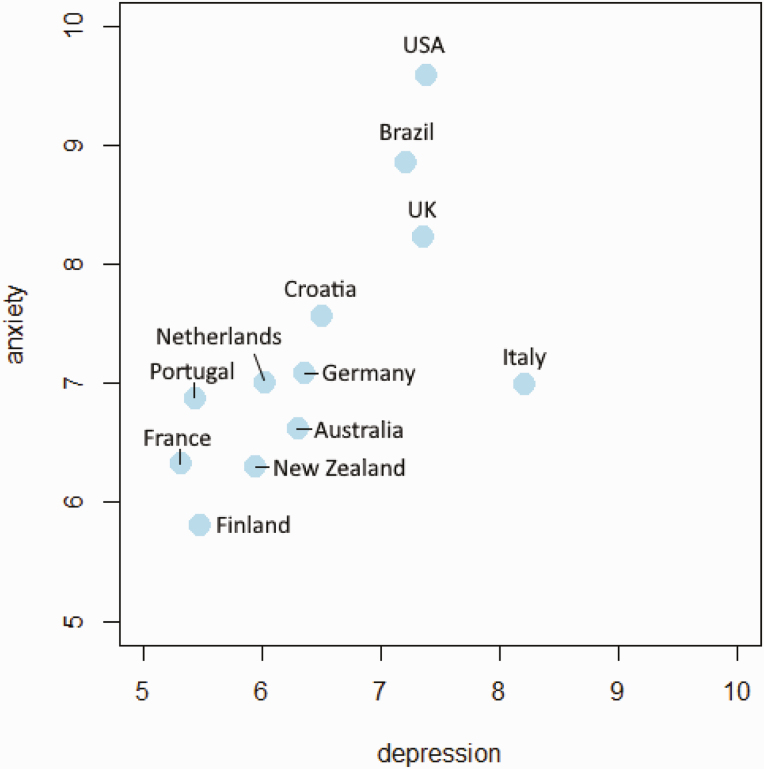
First, we examined levels of anxiety (M = 7.96, SD = 4.49) and depression (M = 6.97, SD = 4.01) for the 12 main countries, see Fig. 3 (see also Supplementary Materials, Fig. SM4.2 and Supplementary Materials, SM.5 for comparisons). See Supplementary Materials for an overview of descriptive statistics of the participants (Supplementary Materials, SM.3) and model variables (Supplementary Materials, SM.3).
Fig 3 |.
Scatterplot of average anxiety symptoms by depression symptoms per country (averages of sums of symptom scores).
Threat, Lockdown, and Mental Health Model
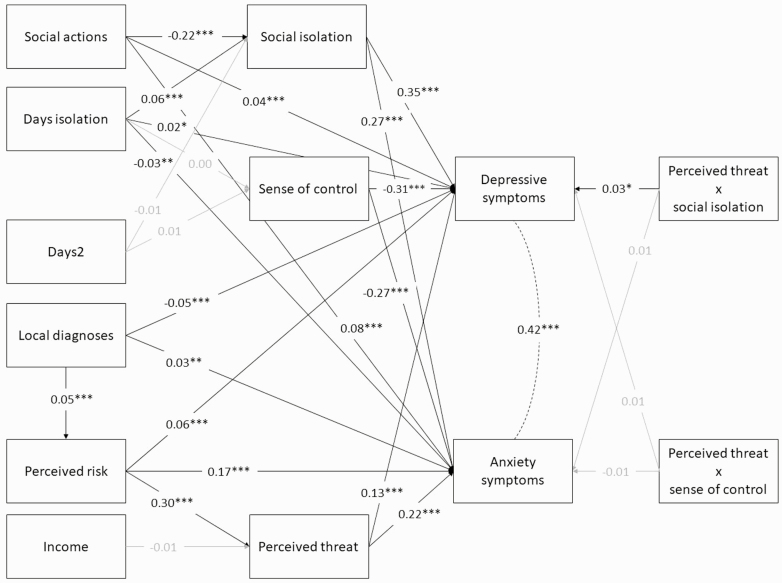
We pre-registered a basic model including anxiety, depression, perceived threat, social isolation and sense of control, which was significant (Supplementary Materials, SM.6). Our second pre-registered model (see Fig. 1) added a number of important variables to this basic model. We considered RMSEA ≤ 0.08, combined with CFI > 0.90 and SRMR ≤ 0.08, to be indicative of an acceptable model fit [22]. Using these criteria, we were able to accept this model (RMSEA (0.06), CFI (0.94), and SRMR (0.04)1, see Fig. 4 and Supplementary Materials, Table SM7.1).
Fig 4 |.
Threat, Lockdown, and Mental Health Model results. Standardized coefficients are shown; (residual) variances omitted for clarity, non-significant paths printed in gray, and the dotted line reflects correlation. “Days2” is included to test the quadratic function of days in isolation on social isolation and sense of control. *p < .05, **p < .01, ***p < .001.
Most of our pre-registered predictions were confirmed: Social isolation positively predicted depression, a reduced perception of control predicted anxiety, and perceived personal threat positively predicted both anxiety and depression. The interaction of social isolation by personal threat was significant. Social isolation also significantly predicted anxiety, and a reduced sense of control predicted depression. In addition, as expected, the more local diagnosed infections, the higher the perceived risk of contracting COVID-19. Perceived risk in turn predicted a higher perceived threat of COVID-19. Contrary to expectation, though, income level did not predict perceived personal threat, and the quadratic function of days in isolation did not significantly predict sense of control (nor the linear function), though the linear effect did predict social isolation (see Supplementary Materials, SM.8 for scatterplots).
Antecedents of Control Model
Our next pre-registered analysis examined the predictors for sense of control (see Fig. 2). Fit indices RMSEA (0.06), CFI (0.54), and SRMR (0.05) of this model were examined, and it was found that these indicated an unacceptable model fit, given our criteria (see above), and we thus rejected the model. See Supplementary Materials, SM.9 for the figure and table of the unexpected model results. One explanation may be that the hypothesized latent variable did not bear out and reduced the power of the analysis. We therefore ran an exploratory regression analysis predicting sense of control by the main hypothesized mechanisms of control without the hypothesized latent variable, see Fig. 5 (and Supplementary Materials, Table SM10.1 for a full regression table).
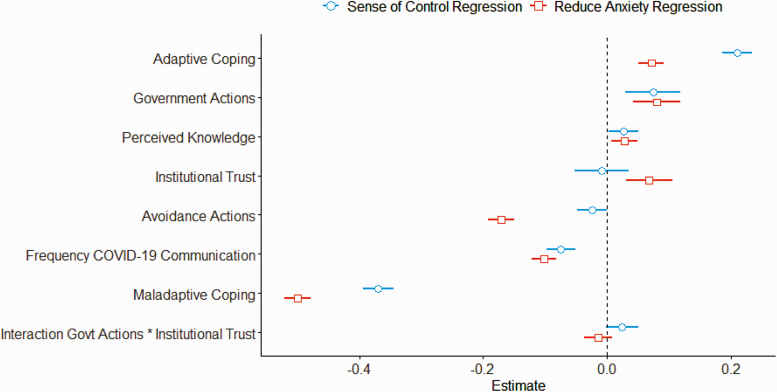
Fig 5 |.
Plot of regression coefficients for regressions predicting sense of control (blue circles) and reduced anxiety (orange squares) with 95% confidence intervals. Predictor variables are ordered by magnitude from the sense of control regression, with the exception of the interaction variable (placed last). Estimates are standardized.
Next we investigated whether anxiety could be predicted from the same factors. While we found that a lower sense of control predicted anxiety, the level of sense of control had no influence on the effect of personal threat over anxiety. Therefore, we investigated whether the factors influencing control would affect anxiety; see Fig. 5 (and Supplementary Materials, Table SM10.2 for a full regression table).
The analyses showed a good fit in predicting sense of control (cond. R2 = .203) and anxiety (cond. R2 =.384). While sense of control was predicted first and foremost by coping—maladaptive coping (negatively) and adaptive coping (positively)—it was also predicted by frequency of communication about COVID-19 (negatively) and government actions and perceived knowledge (positively). We also found that avoidance actions, institutional trust, and their interaction did not significantly predict sense of control. Anxiety, on the other hand, was predicted by all factors, except for the interaction between government actions and institutional trust.
Primary control
We were surprised by the lack of efficacy of primary control mechanisms: avoidance actions did not predict sense of control; unexpectedly they predicted an increase rather than a decrease in anxiety. We therefore ran additional regressions predicting control and anxiety with all of avoidance behaviors individually. As the conditional R2 of the control regression was only 0.025, we will only discuss the anxiety regression (cond. R2 = .086, see Supplementary Materials, Table SM11.1). We found that wearing a N-95 or higher (health grade) mask was the only predictor of lower levels of anxiety, while wearing a mask of any kind significantly predicted higher levels of anxiety. In addition, washing one’s hands for at least 20 s, cleaning and disinfecting one’s home, using antibacterial products, and avoiding food prepared by someone you do not know were also all predictive of higher levels of anxiety. The same regression was run for participants who indicated that they are essential workers (n = 942; Supplementary Materials, Table SM11.2) and it showed a similar pattern, except that the use of antibacterial products in this group was overall not predictive of anxiety. Indeed, essential keyworkers engaged in more actions to avoid contracting the virus (M = 2.57, SD = 0.65) than participants who were not essential workers virus (M = 2.51, SD = 0.61, F(1,8133) = 10.09, p = .001, η p2 = .001), and also had higher levels of anxiety (M = 8.28, SD = 4.56, compared to M = 7.92, SD = 4.48, F(1,8219) = 5.23, p = 0.2, η p2 = .001)2. Essential workers were also asked whether they felt they had sufficient PPE (see Supplementary Materials, Fig. SM11.1 for overall frequencies and Supplementary Materials, Fig. SM11.2 for access to PPE per country) and access to sufficient PPE was significantly correlated with lower levels of anxiety symptoms (r = −.17, p < .001) and depressive symptoms (r = −.12, p < .001).
Secondary control
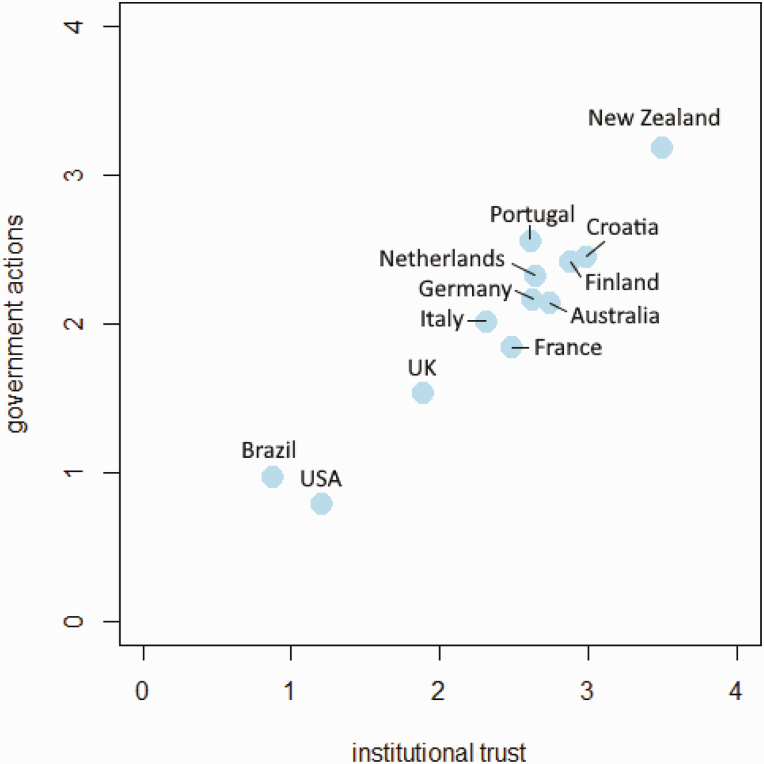
Government actions were found to be predictive of both sense of control and reduced anxiety, whereas institutional trust was only associated with reduced anxiety. See Fig. 6 for averages of government actions and institutional trust per country (and Supplementary Materials, SM.12 for further breakdowns, including of USA federal and state governments). Additional exploratory regressions (see Supplementary Materials, SM.13) indicated that positive government actions both contributed to a greater sense of control (cond. R2 = .062,), and predicted lower levels of anxiety (cond. R2 = .101).
Fig 6 |.
Scatterplot of government actions averages and institutional trust averages per country.
Discussion
The global crisis around COVID-19 stands out because of the combination of two main factors: it involves (a) a practically constant threat and (b) global lockdowns. We hypothesized in a pre-registration that many perceive that COVID-19 will have severe effects on their lives, and that this would be negatively associated with their psychological well-being. Moreover, we hypothesized that lockdown measures would be associated with depression symptoms in people who are socially disconnected and anxiety symptoms in those experiencing a sense of loss of personal control. Finally, we hypothesized that a range of behaviors, such as communicating with others, or governmental actions, would be associated with positive mental health outcomes.
Data from over 8,000 participants worldwide showed that overall rates of anxiety (M = 7.96) and depression (M = 6.97) were at quasi-clinical levels [8]. While the Hospital Anxiety and Depression Scale is typically used with patients, some studies have used the scale in the general population [23]. This study showed averages ranging from 3.9 (57 years and over) to 5.1 (18–65 years old), suggesting that though we were not able to obtain a pre-pandemic baseline, there is a marked elevation in anxiety and depressive symptoms, in line with other recent findings [24, 25]. The USA, the UK, and Brazil had especially elevated levels of anxiety and depression compared to other countries, with Italy additionally scoring highest on depression, at clinical levels of mild symptoms [8]. This is an alarming finding.
Our main pre-registered hypotheses were confirmed: Perceived personal threat (i.e., thinking that COVID-19 will have severe effects on one’s life) predicted anxiety and depression symptoms in our model. The effect of personal threat on depressive symptoms was stronger when one felt socially isolated. A low sense of control predicted anxiety symptoms, but did not further increase the effect of personal threat on anxiety symptoms. The level of local COVID-19 diagnoses increased the perceived risk of contracting the virus, and this significantly increased perceived personal threat, in line with recent COVID-19 research on risk and resilience [26]. Both perceived risk and threat predicted levels of anxiety. Days of lockdown were, as expected, a significant predictor of social isolation, but not of reduced control. We did not find evidence for a hypothesized U-curve for either factor, where initial low levels of stress would increase but then reduce due to habituation.
The COVID-19 pandemic has involved lockdown, social distancing, and quarantine for people across the globe. This has led, among other things, to a severe reduction in social connectedness between people. Social connectedness is of pivotal importance to psychological well-being: feelings of loneliness and social isolation have been associated with higher mortality [27], depression [28], and other negative mental and physical health outcomes [29]. The current results show that engaging in frequent communication with close ones (family, friends, colleagues/fellow students) through a variety of sources (messages, calls, and video chats) was generally associated with reduced feelings of social isolation.
Secondary control mechanisms (e.g., coping, government actions) significantly contributed to a higher sense of control, but primary control mechanisms (e.g., actions to avoid contracting COVID-19) did not. When a threat is deemed controllable individuals will adapt their behaviors to address the threat [30]. However, when threat cannot be controlled, defensive reactions may set in, leading to feelings of helplessness [31], which is often associated with depression [32]. In support of the idea that participants in our sample felt there was little they could do to regain control, we found that sense of control predicted both depressive and anxiety symptoms.
We further investigated the puzzling association between avoidance behaviors and increased anxiety, and found that of the listed avoidance behaviors, only wearing high-grade medical masks (e.g., N-95) was associated with lower levels of anxiety. Other common and ostensibly sensible actions, such as washing your hands for at least 20 s, were associated with higher levels of anxiety. These results may reflect that individuals who are particularly anxious engage in these activities more often. In line with that idea, the results showed that essential workers with high levels of anxiety engaged in those activities more often too. Moreover, for this group, wearing masks of any kind was associated with higher levels of anxiety, whereas wearing a high health-grade mask (N-95) was associated with lower levels of anxiety. Having access to sufficient PPE was also associated with lower levels of anxiety and depressive symptoms. Thus, while professional actions to reduce the chance of contracting the virus reduce anxiety, other avoidance actions are likely performed more often (at home) by individuals with high levels of anxiety.
As expected, adaptive coping mechanisms such as acceptance and humor were associated with higher levels of sense of control and lower levels of anxiety, whereas maladaptive coping mechanisms such as denial and substance use were associated with higher levels of anxiety, in line with previous findings [33]. Interestingly, frequency of COVID-19 communication—hypothesized to reflect the seeking out of information about COVID-19—was associated with lower levels of sense of control. It may be that low levels of sense of control and high levels of anxiety feed the need to talk more frequently about COVID-19.
A recent review [12] listed what governments can do to alleviate suffering due to quarantine, and in our survey we found that the perception that the government had undertaken many of these actions was associated with higher levels of sense of control and lower levels of anxiety. Institutional trust—the belief in the government’s capability, benevolence, and integrity to deal with the COVID-19 outbreak—independently predicted lower levels of anxiety. Trust in the government is extremely important; during the Ebola outbreak, trust in the Liberian government was correlated with taking precautions and compliance with government-instituted control policies [34] and the use of health services during the outbreak [35]. Therefore, it is paramount that the leaders of national governments and officials of national health institutions put forward factual and reliable information.
There are some limitations to this research, such as the use of a cross-sectional survey, which means that causal inferences cannot be made, and that we did not assess levels of pre-existing anxiety and depression. We made this decision on the basis of debates about the quality of, and biases in, the retrospective recall of emotional states [36]. It should be noted that the participants in our sample were, on average, relatively highly educated and predominantly—though not exclusively—from Western countries. This might limit the generalizability of our findings. Due to the employed study design and samples, we were not able to directly compare countries. However, we hypothesized that people’s psychological responses to the pandemic would be generally uniform given the universal themes of lack of social contact and feelings of threat due to the pandemic. Another limitation was that we could not use our measurement of actual COVID-19 knowledge due to too little variance. Luckily, this reflects that four common myths about COVID-19 were not believed widely in the current large sample. Moreover, recent research has shown that individuals’ perceived knowledge about COVID-19 infection was more predictive of emotional well-being than actual knowledge [24].
Conclusions
Disasters, whether natural or human-made, are becoming more common occurrences [37, 38], with such traumatic events being experienced by people almost every day [39]. Often those who experience and survive these disasters show a variety of psychological problems, including generalized anxiety disorder and major depression disorder [40]. These psychological issues are often exacerbated—if not caused—by additional problems, such as loss of income and disruption of social networks and daily activities [41]. It is therefore paramount that factors that might mitigate these issues are identified. The results of our study indicate that some individual and social actions, such as maintaining frequent social contact and governments taking positive actions to manage a public health crisis, are associated with psychological well-being during lockdown. This means that citizens and governments could together engage in helpful actions to adapt better to restrictive measures during the current and future pandemics.
Supplementary Material
Acknowledgments
We thank the following external translators for their work: Lotte Pummerer (German), Francesca Mellano (French), Ingrid Ruesink (French, Dutch), Everton Maraldi (Brazilian Portuguese), and Lluis Oviedo (Spanish). We received no funding for this work.
Footnotes
To ensure measurement invariance, we estimated configural and metric invariance models for all scales across countries with >100 respondents. Although most chi-square difference tests were significant, these are overpowered with a large sample size. According to BIC, the metrically invariant models actually had superior fit to the configurally invariant models for all most scales except institutional trust. This means that the scales measure the same construct across countries (although mean levels might vary).
Essential workers were also found to have lower levels of social isolation (M = 1.02, SD = 1.02, compared to M = 1.23, SD = 1.08, F(1,8212) = 30.12, p < .001, η p2 = .004), despite being in less contact with friends, family, and colleagues (M = 2.21, SD = 0.99) than participants who were not essential workers (M = 2.29, SD = 1.00, F(1,8167) = 5.35, p = .02, η p2 = .001). They did communicate about COVID-19 more (M = 3.35, SD = 0.99) than participants who were not essential workers (M = 3.10, SD = 1.01, F(1,6503) = 45.29, p < .001, η p2 = .007), with no further significant differences between the groups in the main variables, including depression symptoms (F’s < 2.04, p’s < .15).
Funding
This study was performed without funding.
Compliance With Ethical Standards
Conflict of Interest: All listed authors declare that they have no conflicts of interest.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
Transparency Statements
Study Registration: Study registration involves declaring the study design, variables, and treatment conditions in an independent, institutional repository(e.g., http://clinicaltrials.gov, http://openscienceframework.org, http://socialscienceregistry.org/). A study is considered pre-registered if it is registered in a repository prior to the study began. Consider the following examples:
The study was pre-registered at Open Science Framework, https://osf.io/tsjnb/
Analytic Plan Pre-registration: Pre-registration of an analytic plan involves specification of the planned sequence of analyses or the statistical model that will be reported. Reporting the planned outcome variables alone does not qualify as analytic plan pre-registration. Consider the following examples:
The analysis plan was registered prior to beginning data collection at Open Science Framework, https://osf.io/tsjnb/
Data Availability: Indicate whether the data underlying the presented analyses will be made available in a third-party archive/repository. If data are available in an archive, indicate if this is fully available to the public or has protected access (available for limited audience, with clearly defined requirements and steps to obtain data). If data are not in a public archive, describe any steps needed to access the data. Consider the following examples:
De-identified data from this study are available in a public archive: https://osf.io/tsjnb/
Analytic Code Availability: Analytic code refers to the programming code used to conduct the analyses in the statistical software. Consider the following examples:
Analytic code used to conduct the analyses presented in this study are available in a public archive: https://osf.io/tsjnb/
Materials Availability: Materials include any stimuli used in this study, intervention protocols, and survey instruments and items. Consider the following examples:
All materials used to conduct the a study are available in a public archive: https://osf.io/tsjnb/
References
- 1.Statistica. Monthly unemployment rate in the United States from May 2019 to May 2020. 2020. Available at https://www.statista.com/statistics/273909/seasonally-adjusted-monthly-unemployment-rate-in-the-us/. Accessibility verified January 21, 2021.
- 2.Rothbaum F, Weisz JR, Snyder SS. Changing the world and changing the self: a two-process model of perceived control. J Pers Soc Psychol. 1982;42(1):5–37. [Google Scholar]
- 3.Kay AC, Gaucher D, Napier JL, Callan MJ, Laurin K. God and the government: testing a compensatory control mechanism for the support of external systems. J Pers Soc Psychol. 2008;95(1):18–35. [DOI] [PubMed] [Google Scholar]
- 4.Heckhausen J, Schulz R. A life-span theory of control. Psychol Rev. 1995;102(2):284–304. [DOI] [PubMed] [Google Scholar]
- 5.Skinner EA. A guide to constructs of control. J Pers Soc Psychol. 1996;71(3):549–570. [DOI] [PubMed] [Google Scholar]
- 6.Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Acad Manag Rev. 1995;20(3):709–734. [Google Scholar]
- 7.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 8.Stern AF. The hospital anxiety and depression scale. Occup Med (Lond). 2014;64(5):393–394. [DOI] [PubMed] [Google Scholar]
- 9.Lee RM, Robbins SB. Measuring belongingness: the social connectedness and the social assurance scales. J Counsel Psychol.1995;42(2):232–241. [Google Scholar]
- 10.Zion S, Heathcote LC, Horii R, Leibowitz K, Louis K, Crum A. The role of mindsets in the context of the COVID-19 viral outbreak.2020. Retrieved March 17. 2020. Open Science Framework (OSF) project. Available at https://osf.io/4cus5/
- 11.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. [DOI] [PubMed] [Google Scholar]
- 12.Brooks SK, Webster RK, Smith LE, et al. . The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. [Google Scholar]
- 14.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2014;67(1):1–48. [Google Scholar]
- 15.Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Soft. 2012;48(2):1–36. [Google Scholar]
- 16.Wickham H.ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag; 2016. [Google Scholar]
- 17.Van Lissa CJ. tidySEM: tidy structural equation modeling. Available at https://cjvanlissa.github.io/tidySEM
- 18.Van Lissa CJ, Brandmaier AM, Brinkman L, Lamprecht A, Peikert A,. Struiksma ME, Vreede BMI. WORCS: A workflow for open reproducible code in science. Data Science. 2021; 4(1): 29– 49. [Google Scholar]
- 19.Nakagawa S., Johnson PC, Schielzeth H. The coefficient of determination R 2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface. 2017;14(134):20170213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moshagen M, Erdfelder E. A new strategy for testing structural equation models. Struct Equ Modeling. 2016;23(1):54–60. [Google Scholar]
- 21.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. [DOI] [PubMed] [Google Scholar]
- 22.Kline RB.Principles and Practice of Structural Equation Modeling. London: Guilford Publications; 2011. [Google Scholar]
- 23.Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–370. [DOI] [PubMed] [Google Scholar]
- 24.Yang H, Ma J. How an epidemic outbreak impacts happiness: factors that worsen (vs. protect) emotional well-being during the coronavirus pandemic. Psychiatry Res. 2020;289:113045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L., ... Stocks TV. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. 2020. Available at 10.31234/osf.io/hb6nq. Accessibility verified April 20, 2021. [DOI] [Google Scholar]
- 26.Dryhurst S, Schneider CR, Kerr J, Freeman AL, Recchia G, Van Der Bles AM, ... van der Linden S. Risk perceptions of COVID-19 around the world. J Risk Res. 2020; 23:1–13. [Google Scholar]
- 27.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. [DOI] [PubMed] [Google Scholar]
- 28.Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav. 2000;27(5):591–615. [DOI] [PubMed] [Google Scholar]
- 31.Alloy LB, Abramson LY. Learned helplessness, depression, and the illusion of control. J Pers Soc Psychol. 1982;42(6):1114–1126. [DOI] [PubMed] [Google Scholar]
- 32.Maier SF, Seligman ME. Learned helplessness at fifty: insights from neuroscience. Psychol Rev. 2016;123(4):349–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahmoud JS, Staten R, Hall LA, Lennie TA. The relationship among young adult college students’ depression, anxiety, stress, demographics, life satisfaction, and coping styles. Issues Ment Health Nurs. 2012;33(3):149–156. [DOI] [PubMed] [Google Scholar]
- 34.Blair RA, Morse BS, Tsai LL. Public health and public trust: survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc Sci Med. 2017;172:89–97. [DOI] [PubMed] [Google Scholar]
- 35.Morse B, Grépin KA, Blair RA, Tsai L. Patterns of demand for non-Ebola health services during and after the Ebola outbreak: panel survey evidence from Monrovia, Liberia. BMJ Glob Health. 2016;1(1):e000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levine LJ, Safer MA. Sources of bias in memory for emotions. Curr Dir Psychol Sci. 2002;11(5):169–173. [Google Scholar]
- 37.Warsini S, West C, Ed Tt GD, Res Meth GC, Mills J, Usher K. The psychosocial impact of natural disasters among adult survivors: an integrative review. Issues Ment Health Nurs. 2014;35(6):420–436. [DOI] [PubMed] [Google Scholar]
- 38.Beck U, Lash S, Wynne B.. Risk Society: Towards a New Modernity, Vol. 17. New York, NY: Sage; 1992. [Google Scholar]
- 39.Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65(3):240–260. [DOI] [PubMed] [Google Scholar]
- 40.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207–239. [DOI] [PubMed] [Google Scholar]
- 41.Nikapota A. After the tsunami: a story from Sri Lanka. Int Rev Psychiatry. 2006;18(3):275–279. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.