Abstract
Purpose
To evaluate the effect of ultrasound-guided quadratus lumborum block (QLB) preemptive analgesia on recovery in colon cancer patients undergoing open radical surgery and provide reference for its clinical application.
Methods
From July 2019 to June 2020, according to the anesthesia method, 56 patients who received open radical colon surgery were divided into two groups: Group Q (n=27), which received QLB combined general anesthesia, and Group C (n=29), which received general anesthesia only. Both groups were given self-controlled intravenous analgesia pump after surgery. The primary outcome is a series of parameters representing postoperative recovery. The secondary outcome was VAS scores and opioid consumption.
Results
The first time of getting up, flatus, taking semi-liquid diet and the postoperative hospital stay in Group Q were significantly reduced (P<0.01). The rest and active VAS scores were significantly lower in Group Q (P<0.01). The opioids consumption was significantly decreased in Group Q (P<0.05).
Conclusion
The application of ultrasound-guided QLB preemptive analgesia in open radical colon cancer surgery can significantly enhance the postoperative analgesia effect, reduce opioid consumption, and accelerate the postoperative recovery of the patients.
Clinical Trial Registration Number
The Chinese Clinical Trial Registry (ChiCTR-2000034824).
Keywords: colon cancer, open radical surgery, quadratus lumborum block, ultrasound guidance, preemptive analgesia, postoperative recovery
Introduction
Colon cancer is one of the most common malignant tumors in digestive tract, the morbidity and mortality are increasing year by year, and so far surgery remains the mainstream curative treatment for colon cancer.1–3 Postoperative pain can delay the wound healing, the first ambulation and the recovery of intestinal tract, leading to the patient’s body in a stress status, which results in the damage of immune function, thus promoting the recurrence and metastasis of tumor after surgery, and delaying the overall postoperative recovery speed.4–12 It has been demonstrated that scientific and reasonable pain management is helpful to reduce complications and accelerate the recovery of patients.13 For a long time, opioids have played a major role in postoperative analgesia, but heavy use of these drugs will cause adverse reactions such as nausea, vomiting and enteroparalysis, which is not conducive to rapid recovery after surgery. At present, preemptive analgesia has been defined as a clinical anesthesia technique and/or multi-drug combination analgesic treatment, which anticipates that pain can be modified by analgesic nerve blocks prior to tissue trauma with its resultant release of nociceptive stimuli and prevent central sensitization.14,15 In recent years, with the development of ultrasound visualization technology, regional block technique has become a hot spot in the field of anesthesia. Quadratus lumborum block (QLB) provides a local block through the local anesthetic in the paravertebral space. QLB decreases the dose of opioids, reduces adverse reactions and accelerates the recovery of patients.16,17 However, it is still unclear if QLB has effects on recovery in post-operation patients. Here, in this retrospective study, through evaluating the impact of QLB preemptive analgesia on postoperative analgesia and recovery speed of colon cancer patients receiving open radical surgery, we aim to verify the safety and effectiveness of QLB preemptive analgesia, and provide reference for its clinical application.
Materials and Methods
General Data
This study is a clinical retrospective cohort study, which was registered at the Chinese Clinical Trial Registry (ChiCTR-2000034824), was approved by the Research Ethics Committee of the second Hospital of Shandong University (No: KYLL-2020LW-043), and was conducted in accordance with the Declaration of Helsinki. The written informed consent was waived, due to no damage to patients or conflicts of interest. The confidentiality of patient data was guaranteed according to the requirements of the Ethics Committee. A total of 56 colon cancer patients who underwent open radical surgery in the second hospital of Shandong University between July 2019 and June 2020 were included in the study. The data extracted from clinical electronic medical record system, and then according to the anesthesia method the patients were divided into two groups: QLB group (Group Q, n=27) and control group (Group C, n=29). Inclusion criteria: 30–65 years old; ASA class II–III; The diagnosis of colon cancer by pathological examination was consistent with the surgical indications; The same surgical technique applied to all patients (The surgery was performed through a paramedian incision in the lower abdomen, the length of the incision site was about 13 cm, the length of the removed bowel was 15 cm or so, and the lymph nodes around the bowel and the root of mesentery were cleaned.); Total intravenous anesthesia or combined QLB3 (anterior QLB) was applied to all operations; All surgeries and anesthesia management were carried out by the same team; patients signed the informed consent for 48-hour postoperative analgesia, and sufentanil was used for emergency analgesia when PCIA was insufficient. Exclusion criteria: preoperative cognitive dysfunction; severe cardiopulmonary dysfunction; severe liver or kidney dysfunction (CHILD grade less than 10 and the creatinine at 451–707 mol/L respectively.); hematological system disease, coagulation abnormality or anticoagulation treatment; distant organ metastasis; recent take of analgesics; past history of abdominal surgery; preoperative chemoradiotherapy; emergent operations for complete obstruction or bleeding; regional block contraindications or complications; failure to complete data collection and follow-up.
Anesthetic Methods
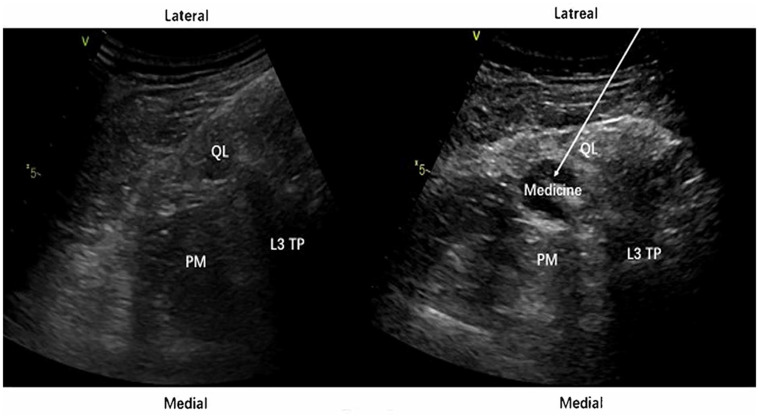
Patients were regularly fasted for 6 to 8 hours before surgery. After entering the operating theatre, the patients inhaled oxygen through nose and non-invasive blood pressure was measured. ECG and pulse oxygen saturation were monitored, and were given heat preservation. Before induction of general anesthesia, the QLB3 approach18 was used to perform bilateral ultrasound-guided quadratus lumborum block in Group Q: the patient was placed in the lateral position, and a low-frequency probe was placed between the iliac crest and costal margin to scan laterally. After identifying the external abdominal obliques, internal abdominal obliques, and transverse abdominal muscles, the probe was slid to the rear, and the goal is to find the third lumbar transverse process, psoas muscles, quadratus lumborum and erector spinae muscles. By using the short-axis in-plane technology, the 22 G needle tip was delivered to the place between the quadratus lumborum and psoas major muscles. If no blood is drawn back, an injection of 1 mL of normal saline was made to confirm the injection plan by visualizing the dissection between the two muscles. Once confirmed, a 0.3% ropivacaine solution (0.4 mL/kg) was injected between the fascias of the two muscles on each side (Figure 1). After injection, the psoas muscle was suppressed by the local anesthetic, which can initially prove that the injection was successful. After 10–20 min, the pain of blocked area was evaluated via pinprick test. If the local blocks were satisfying, the general anesthesia would be performed. Both groups of patients were given endotracheal intubation anesthesia with propofol, sufentanil, remifentanil and cisatracurium, and PCIA was performed immediately after the surgery. The formula was: sufentanil 2 μg/kg diluted to 100 mL with normal saline, initial load was 5 mL, background dose was 2 mL/h, locking time 15 min, additional amount was 0.5 mL.
Figure 1.
The ultrasound view of the QLB3. Medicine: drug solution. The arrow denotes the puncture path of the needle. Compared with left picture, the psoas muscle in right picture is pressed down by the drug solution.
Abbreviations: QL, quadratus lumborum; PM, psoas major muscle; L3 TP, the third lumbar transverse process.
Observation Index
(1) Gender, age, weight, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, preoperative albumin level, preoperative hemoglobin level, the duration of anesthesia and surgery, intraoperative blood loss, intraoperative fluid replacement, lesion site, type of colectomy, removal time of drainage, and intraoperative urine volume were observed.
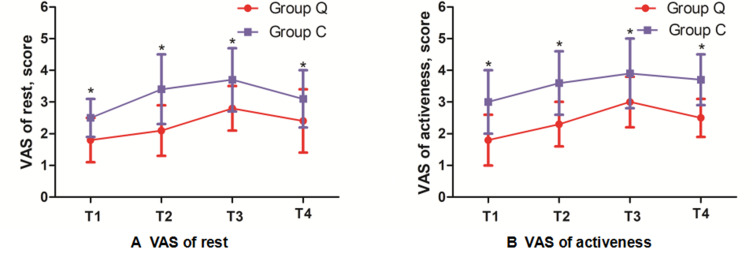
(2) The visual analog scores (VAS) (0–10 points) of rest pain (such as bed resting pain) and active pain (such as cough pain and the pain caused by body turnover) were observed at 0 h (T1), 12 h (T2), 24 h (T3) and 48 h (T4) after surgery.
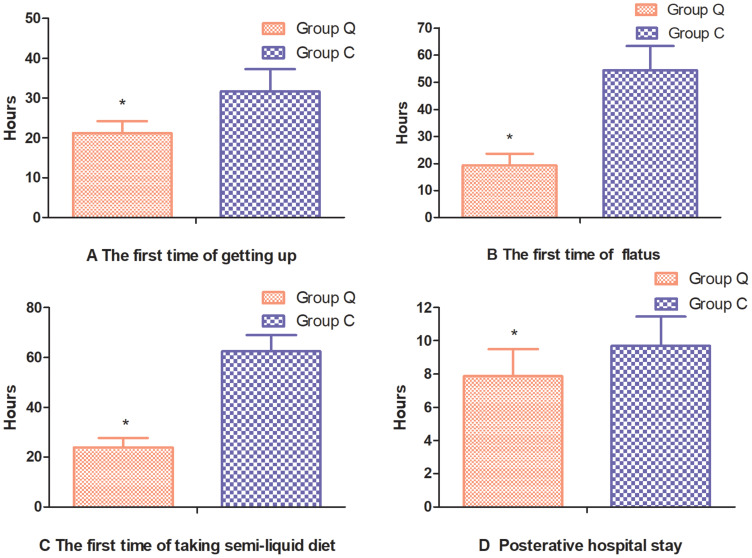
(3) The recovery of the two groups was observed, including the first time of getting up, the first time of flatus, the first time to intake semi-liquid diet, and postoperative hospital stay.
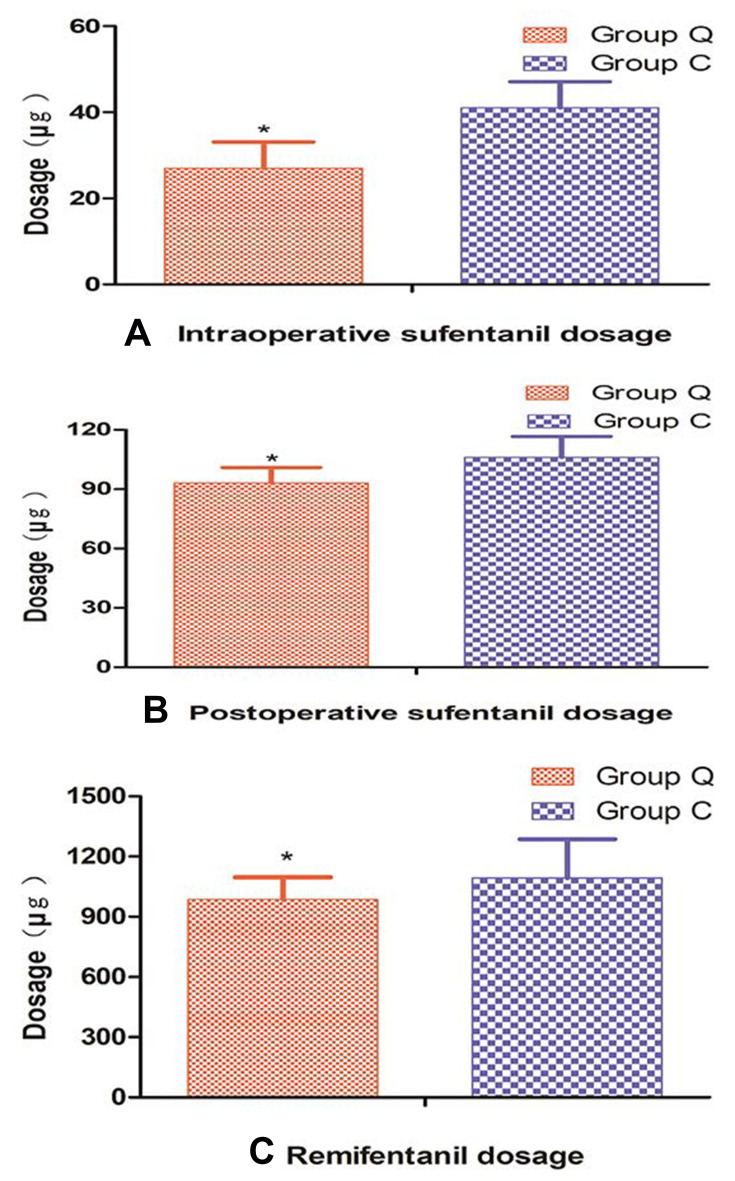
(4) Opioid analgesics used during and 48 h after the operation were observed, including remifentanil dosage, intraoperative sufentanil dosage, and postoperative sufentanil dosage.
(5) The incidence of adverse reactions, such as drowsiness, nausea, vomiting, itching, urinary retention, respiratory depression (RR<10 bpm lasting for more than 10 min), bradycardia (HR<50 bpm) and hypotension (BP<30% of the baseline value) within 48 h postoperatively were observed.
Statistical Analysis
The sample size was calculated by PASS 11.0 (NCSS-PASS 11, USA). According to the preliminary experiment results, the principal parameter-postoperative VAS (rest pain) at 24 h was 2.6±0.9 in Group Q and 3.5±1.1 in Group C. The power of the endpoint is calculated based on a two sample t-test with a significance level of 5%, and the β power is 0.20. The sample size of each group is calculated 18 cases by the software and considering a 20% dropout rate; then, 46 patients (23 patients per group) should be sufficient in the present trial; hence, the sample size (n=56) meets the requirements and the results are credible. IBM SPSS Statistics for Windows, version 23.0 (IBM Corp, Armonk, NY, USA) was used for data analyses. Normality was tested using the Kolmogorov–Smirnov test. A repeated-measures analysis of variance was applied for comparisons between the two groups at different time points. Intragroup comparisons were performed using the Student’s t-test or Mann–Whitney U-test. Qualitative variables were compared using the chi-square (χ2) test or Fisher’s exact test. P<0.05 were considered statistically significant. Data are expressed as mean ± standard deviation (SD) or the number (proportion) as appropriate.
Results
Eventually, 27 patients in Group Q and 29 patients in Group C who met the criteria were enrolled. Patients demographics for the two groups were comparable. There were no statistically significant differences between the two groups in gender, age, weight, BMI, ASA classification, preoperative albumin level, preoperative hemoglobin level, the duration of anesthesia and surgery, intraoperative blood loss, intraoperative fluid replacement, lesion site, type of colectomy, removal time of drainage, and intraoperative urine volume (P>0.05, Table 1). The VAS scores of rest pain and active pain in Group Q were significantly lower compared with that of Group C at all time points (P<0.01, Figure 2). Regarding postoperative recovery, the first time of getting up, the first time of flatus, the first time to intake semi-liquid diet, and postoperative hospital stay in Group Q were significantly reduced compared with those in Group C (P<0.01, Figure 3). The dosage of remifentanil, intraoperative sufentanil and postoperative sufentanil in Group Q were significantly less than Group C, respectively (P<0.05, Figure 4). There were no statistical differences in adverse reactions separately in both the groups (P>0.05, Table 2).
Table 1.
Comparison of Demographic Data and Characteristics in the Two Groups
| Indicators | Group Q (n=27) | Group C (n=29) | P |
|---|---|---|---|
| Gender (male/female, case) | 17/10 | 21/8 | 0.45 |
| Age (years) | 51.6 ± 5.9 | 52.2 ± 3.5 | 0.64 |
| Weight (kg) | 63.5 ± 8.2 | 64.2 ± 8.6 | 0.52 |
| BMI (kg/m2) | 21.7 ± 0.9 | 21.3 ± 1.5 | 0.18 |
| ASA grade (II/III, case) | 10/17 | 10/19 | 0.84 |
| Preoperative albumin level (g/L) | 40.2 ± 6.2 | 38.3 ± 6.1 | 0.25 |
| Preoperative hemoglobin level (g/L) | 123.2 ± 18.9 | 125.2 ± 20.6 | 0.70 |
| Lesion site (AC/DC/SC, case) | 3/9/15 | 1/12/16 | 0.55 |
| Type of colectomy (left/right/sigmoid, case) | 3/9/15 | 1/12/16 | 0.55 |
| Anesthesia time (min) | 184.5 ± 18.0 | 187.5 ± 19.4 | 0.56 |
| Surgery time (min) | 167.0 ± 13.5 | 173.5 ± 23.4 | 0.21 |
| Intraoperative blood loss (mL) | 189.6 ± 36.4 | 202.4 ± 46.3 | 0.26 |
| Intraoperative fluid replacement (mL) | 1775.9 ±303.2 | 1878.6 ± 384.5 | 0.27 |
| Urine volume (mL) | 410.7 ± 36.3 | 396.6 ± 27.3 | 0.11 |
| Removal time of drainage (day) | 5.7±1.5 | 6.5±1.7 | 0.09 |
Notes: Data are presented as the mean ± SD or number; Continuous data were compared by Student’s t-test or repeated-measures analysis of variance; categorical data were compared by Fisher’s exact test; ranked data were compared by Mann–Whitney U-test.
Abbreviations: BMI, Body mass index; ASA, American Society of Anesthesiologists; AC, ascending colon; DC, descending colon; SC, sigmoid colon; SD, standard deviation.
Figure 2.
Comparison of postoperative pain scores in the two groups. The VAS scores of rest pain (A) and active pain (B) in the both groups at 0 h (T1), 12 h (T2), 24 h (T3) and 48 h (T4) after surgery. Data represent the mean ± SD, compared with Group C, *P<0.01. Data were compared by Mann–Whitney U-test.
Abbreviation: VAS, visual analog scores.
Figure 3.
Comparison of postoperative recovery in the two groups. The first time of getting up (A), The first time of flatus (B), The first time of intake semi-liquid diet (C), Postoperative hospital stay (D). Data represent the mean ± SD, compared with Group C, *P<0.01. Continuous data were compared by Student’s t-test.
Figure 4.
Comparison of analgesic drugs dosage in the two groups. Intraoperative sufentanil dosage (A), Postoperative sufentanil dosage (B), Remifentanil dosage (C). Data represent the mean ± SD, compared with Group C, *P<0.05. Continuous data were compared by Student’s t-test.
Table 2.
Comparison of Adverse Reactions After Operation (Case)
| Indicators | Group Q (n=27) | Group C (n=29) | P |
|---|---|---|---|
| Drowsiness | 1(3.7%) | 2(6.9%) | 0.09 |
| Nausea | 2(7.4%) | 5(17.2%) | 0.42 |
| Vomiting | 1(3.7%) | 3(10.3%) | 0.61 |
| Itching | 1(3.7%) | 2(6.9%) | 1.00 |
| Urinary retention | 0(0%) | 3(10.3%) | 0.24 |
| Respiratory depression | 0(0%) | 1(3.4%) | 1.00 |
| Bradycardia | 0(0%) | 1(3.4%) | 1.00 |
| Hypotension | 0 | 0 | — |
Notes: Data are expressed as number (percentage); Categorical data were compared by Fisher’s exact test.
Discussion
The most important finding of the study was that the application of ultrasound-guided QLB preemptive analgesia in open radical colon cancer surgery can significantly accelerate the postoperative recovery of the patients, enhance the postoperative analgesia effect, and reduce opioid consumption. Open surgery is still the most typical operation in intestine malignancies, despite the development of laparoscopic operations. We appreciate the merits of laparoscopic operations, such as fast recovery and reduced tissue damage. However, laparoscopic surgery could not completely substitute open surgery in several circumstances, including vast tumor invasions and emergency operations.1,19–23 In fact, due to various reasons, surgeons mainly perform open surgery in our hospital. However, due to the factors such as surgical injury, organ stretch ischemia, inflammatory exudate stimulation in abdominal cavity and large incision in the abdominal wall, patients can feel moderate-to-severe pain after surgery.4,24 The postoperative pain of the surgery mainly includes abdominal incision pain, visceral pain and inflammatory pain. Thus, it is necessary to use a variety of analgesic measures or drugs to treat the pain caused by various reasons, so as to achieve good analgesic effect. In recent years, preemptive analgesia has gradually developed into a preventive analgesic measure, which intervenes before the harmful stimulation acting on the body. It can weaken or suppress the surgical stress, inhibit the central or peripheral nerve sensitivity, and reduce or eliminate the pain caused by the harmful stimulation, so as to achieve effective analgesia, reduce the dosage of analgesic drugs and reduce adverse reactions.25,26 Opioids are the main drugs for preemptive analgesia with definite effect, but they have many adverse reactions, which may delay the postoperative recovery of patients.27,28 As a new truncal nerve block technique, ultrasound-guided QLB is accurate, safe and effective which is very widely used in clinical practice. Hansen et al16 revealed ultrasound-guided QLB for elective cesarean section significantly reduces postoperative opioid consumption and prolongs time to the first opioid request. Kwak et al29 reported that preoperative unilateral QLB successfully decreased postoperative pain and opioid consumption after laparoscopic nephrectomy. In a randomized controlled trial, Öksü et al30 showed that QLB provided longer and more effective postoperative analgesia compared with the transversus abdominis plane block in pediatric patients undergoing unilateral inguinal hernia repair or orchiopexy. Several studies have shown that the nerve block used for preemptive analgesia can produce better analgesic effect, and it has the advantages of stable hemodynamics, reduced opioid dosage and less adverse reactions.31,32 The mechanism of QLB is that the drug is injected into the space between the quadratus lumborum and its surrounding fascia to block the innervation of the anterior abdominal wall, and the block range can reach T7-L4 segment. The drug diffuses into the paravertebral space through the thoracolumbar fascia, and blocks part of the sympathetic nerve, thus blocking part of the visceral pain. The distribution of the blood vessels on the plane of quadratus lumborum is less, and the absorption of the drug through the blood vessels is less and slow. Therefore, QLB yields prolonged analgesic effect that can reach up to 48 h.33–36 Several studies have shown that QLB3 provided more effective and longer lasting postoperative analgesia and lower opioid consumption compared to QLB1 or QLB2.37,38 So, we preferred to choose QLB3 in our hospital.
Results showed that the VAS scores of rest pain and active pain within 48 h postoperatively in Group Q were significantly lower than those in Group C (P<0.01), which is very similar to that of Deng et al39 that the QLB is a more effective postoperative analgesia in patients undergoing laparoscopic colorectal surgery, and which is consistent with the results of Kukreja et al31 indicating that QLB preemptive analgesia complies with the concept of multimodal analgesia: using analgesic drugs that have different mechanisms can create an additive or synergistic effect, thereby enhancing the analgesic efficacy.40,41 QLB preemptive analgesia can block part of visceral pain by blocking part of the sympathetic nerve, reduce incision pain by blocking nerve fiber impulse conduction, and inhibit the release of inflammatory factors by reducing or preventing stress response, so as to reduce inflammatory pain.42
Postoperative recovery speed is closely associated with the extent of surgical trauma, postoperative analgesia, early postoperative ambulation, and postoperative intestinal function recovery.43,44 Our results showed that these parameters in Group Q were significantly improved compared with those in Group C (P<0.01). Our findings are very similar to those of Wang et al,45 who reported that QLB significantly reduced perioperative opioid requirement, alleviated postoperative analgesia, shortened the time to first ambulation and flatus, and accelerated postoperative recovery of the patients undergoing laparoscopic colorectal surgery. In a randomized controlled trial, Zhu et al46 study reported that QLB could improve recovery and postoperative cognitive function in elderly patients undergoing laparoscopic radical gastrectomy after surgery. The sustained pain control provides several benefits. For example, it reduces the usage of opioid drug, which subsequently prohibits intestinal peristalsis and facilitates early ambulation. On the other hand, it accelerates the fast recovery and early discharge.25,47,48
The dosage of remifentanil, intraoperative sufentanil and postoperative sufentanil in Group Q were significantly less than Group C, respectively (P<0.05), indicating that QLB preemptive analgesia can significantly reduce postoperative pain, which is consistent with the results of Kadam et al.49 In a systematic review and meta-analysis, Korgvee et al50 revealed that QLB could reduce postoperative opioid consumption and prolonged the time to the first rescue opioid analgesic after abdominal and hip surgery. Surgical factors, residual anesthetics and postoperative analgesics may cause adverse reactions such as drowsiness, nausea, and vomiting.51 The results also showed that there were no significant differences in adverse reactions in both groups (P> 0.05). All these indicated that the QLB and the dosage of opioids were safe.
Our study had some limitations: (1) The current study is a retrospective trial, while a prospective randomized control trial might be more convincing. (2) Since several approaches were developed for QLB, it might be necessary and interesting to compare among different approaches. (3) The remifentanil can induce tolerance and hyperalgesia, which has not been taken into account, so that, this probably affects the postoperative pain score and opioid consumption. (4) Since our conclusion was based on a single-center study, a multi-center study with increased cases might further confirm the validity of our results.
In this study, we use multimodal analgesia together with QLB to preemptive analgesia. It happens that such a method is consistent with the recent concept of the ERAS, which is popular worldwide. Although ERAS has not been widely utilized in our hospital, we strive to optimize the use of perioperative analgesia, which plays an important role in the multidisciplinary integration of ERAS.
Conclusions
The present study demonstrated that the application of ultrasound-guided QLB preemptive analgesia in open radical colon cancer surgery can significantly enhance the postoperative analgesic effect and reduce opioid consumption. Furthermore, it can accelerate the postoperative recovery of the patients.
Acknowledgments
The authors thank all the research assistants and patients for their time and efforts in this retrospective study.
Data Sharing Statement
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Niemeläinen S, Huhtala H, Ehrlich A, Kössi J, Jämsen E, Hyöty M. Long-term survival following elective colon cancer surgery in the aged. A population-based cohort study. Colorectal Dis. 2020;22(11):1585–1596. doi: 10.1111/codi.15242 [DOI] [PubMed] [Google Scholar]
- 2.Cao W, Chen HD, Yu YW, Ni L, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J. 2021;134(7):783–791. doi: 10.1097/CM9.0000000000001474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anania G, Arezzo A, Davies RJ, et al. A global systematic review and meta-analysis on laparoscopic vs open right hemicolectomy with complete mesocolic excision. Int J Colorectal Dis. 2021;36(8):1609–1620. doi: 10.1007/s00384-021-03891-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feldheiser A, Aziz O, Baldini G, et al. Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016;60(3):289–334. doi: 10.1111/aas.12651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eisenach JC. Can a blood test of immune responsiveness predict speed of recovery from pain and dysfunction after surgery. Anesthesiology. 2015;123(6):1221–1223. doi: 10.1097/ALN.0000000000000888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang WK, Tai YH, Lin SP, Wu HL, Tsou MY, Chang KY. An investigation of the relationships between postoperative pain trajectories and outcomes after surgery for colorectal cancer. J Chin Med Assoc. 2019;82(11):865–871. doi: 10.1097/JCMA.0000000000000166 [DOI] [PubMed] [Google Scholar]
- 7.Fan X, Wang D, Chen X, Wang R. Effects of anesthesia on postoperative recurrence and metastasis of malignant tumors. Cancer Manag Res. 2020;12:7619–7633. doi: 10.2147/CMAR.S265529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubowitz J, Hiller J, Riedel B. Anesthetic technique and cancer surgery outcomes. Curr Opin Anaesthesiol. 2021;34(3):317–325. doi: 10.1097/ACO.0000000000001002 [DOI] [PubMed] [Google Scholar]
- 9.Heaney A, Buggy DJ. Can anaesthetic and analgesic techniques affect cancer recurrence or metastasis? Br J Anaesth. 2012;109(Suppl 1):i17–i28. doi: 10.1093/bja/aes421 [DOI] [PubMed] [Google Scholar]
- 10.Missair A, Cata JP, Votta-Velis G, et al. Impact of perioperative pain management on cancer recurrence: an ASRA/ESRA special article. Reg Anesth Pain Med. 2019;44(1):13–28. doi: 10.1136/rapm-2018-000001 [DOI] [PubMed] [Google Scholar]
- 11.Page GG, Blakely WP, Ben-Eliyahu S. Evidence that postoperative pain is a mediator of the tumor-promoting effects of surgery in rats. Pain. 2001;90(1–2):191–199. doi: 10.1016/s0304-3959(00)00403-6 [DOI] [PubMed] [Google Scholar]
- 12.Forget P, Aguirre JA, Bencic I, et al. How anesthetic, analgesic and other non-surgical techniques during cancer surgery might affect postoperative oncologic outcomes: a summary of current state of evidence. Cancers. 2019;11:5. doi: 10.3390/cancers11050592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rice D, Rodriguez-Restrepo A, Cata J, et al. Matched pairs comparison of an enhanced recovery pathway versus conventional management on opioid exposure and pain control in patients undergoing lung surgery. Ann Surg. 2020. doi: 10.1097/SLA.0000000000003587 [DOI] [PubMed] [Google Scholar]
- 14.Radwan RW, Gardner A, Jayamanne H, Stephenson BM. Benefits of pre-emptive analgesia by local infiltration at day-case general anaesthetic open inguinal hernioplasty. Ann RColl Surg Engl. 2018;100(6):450–453. doi: 10.1308/rcsann.2018.0059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahiskalioglu A, Yayik AM, Demir U, et al. Preemptive analgesic efficacy of the ultrasound-guided bilateral superficial serratus plane block on postoperative pain in breast reduction surgery: a prospective randomized controlled study. Aesthetic Plast Surg. 2020;44(1):37–44. doi: 10.1007/s00266-019-01542-y [DOI] [PubMed] [Google Scholar]
- 16.Hansen CK, Dam M, Steingrimsdottir GE, et al. Ultrasound-guided transmuscular quadratus lumborum block for elective cesarean section significantly reduces postoperative opioid consumption and prolongs time to first opioid request: a double-blind randomized trial. Reg Anesth Pain Med. 2019;44(9):896–900. doi: 10.1136/rapm-2019-100540 [DOI] [PubMed] [Google Scholar]
- 17.Li X, Xu ZZ, Li YT, Lin ZM, Liu ZY, Wang DX. Analgesic efficacy of two approaches of ultrasound-guided quadratus lumborum block for laparoscopic renal surgery: a randomised controlled trial. Eur J Anaesthesiol. 2021;38(3):265–274. doi: 10.1097/EJA.0000000000001433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed A, Fawzy M, Nasr MAR, et al. Ultrasound-guided quadratus lumborum block for postoperative pain control in patients undergoing unilateral inguinal hernia repair, a comparative study between two approaches. BMC Anesthesiol. 2019;19(1):184. doi: 10.1186/s12871-019-0862-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Petrucciani N, Memeo R, Genova P, et al. Impact of conversion from laparoscopy to open surgery in patients with right colon cancer. Am Surg. 2019;85(2):177–182. doi: 10.1177/000313481908500225 [DOI] [PubMed] [Google Scholar]
- 20.Wu B, Wang W, Hao G, Song G. Effect of cancer characteristics and oncological outcomes associated with laparoscopic colorectal resection converted to open surgery: a meta-analysis. Medicine. 2018;97(50):e13317. doi: 10.1097/MD.0000000000013317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhama AR, Charlton ME, Schmitt M, Cromwell JW, Byrn JC. Factors associated with conversion from laparoscopic to open colectomy using the National Surgical Quality Improvement Program (NSQIP) database. Colorectal Dis. 2015;17(3):257–264. doi: 10.1111/codi.12800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheetz KH, Norton EC, Birkmeyer JD, Dimick JB. Provider experience and the comparative safety of laparoscopic and open colectomy. Health Serv Res. 2017;52(1):56–73. doi: 10.1111/1475-6773.12482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bailey MB, Davenport DL, Vargas HD, Evers BM, McKenzie SP. Longer operative time: deterioration of clinical outcomes of laparoscopic colectomy versus open colectomy. Dis Colon Rectum. 2014;57(5):616–622. doi: 10.1097/DCR.0000000000000114 [DOI] [PubMed] [Google Scholar]
- 24.Benz S, Barlag H, Gerken M, Fürst A, Klinkhammer-Schalke M. Laparoscopic surgery in patients with colon cancer: a population-based analysis. Surg Endosc. 2017;31(6):2586–2595. doi: 10.1007/s00464-016-5266-2 [DOI] [PubMed] [Google Scholar]
- 25.Saad FS, El Baradie SY, Aliem MA, et al. Ultrasound-guided serratus anterior plane block versus thoracic paravertebral block for perioperative analgesia in thoracotomy. Saudi J Anaesth. 2018;12(4):565–570. doi: 10.4103/sja.SJA_153_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu L, Yi J, Wasson MN. Techniques for preemptive analgesia in gynecologic surgery. J Minim Invasive Gynecol. 2019;26(2):197. doi: 10.1016/j.jmig.2018.09.768 [DOI] [PubMed] [Google Scholar]
- 27.Arsoy D, Gardner MJ, Amanatullah DF, et al. Continuous femoral nerve catheters decrease opioid-related side effects and increase home disposition rates among geriatric hip fracture patients. J Orthop Trauma. 2017;31(6):e186–e189. doi: 10.1097/BOT.0000000000000854 [DOI] [PubMed] [Google Scholar]
- 28.Mujukian A, Truong A, Tran H, Shane R, Fleshner P, Zaghiyan K. A standardized multimodal analgesia protocol reduces perioperative opioid use in minimally invasive colorectal surgery. J Gastrointest Surg. 2020;24(10):2286–2294. doi: 10.1007/s11605-019-04385-9 [DOI] [PubMed] [Google Scholar]
- 29.Kwak KH, Baek SI, Kim JK, Kim TH, Yeo J. Analgesic effect of ultrasound-guided preoperative unilateral lateral quadratus lumborum block for laparoscopic nephrectomy: a randomized, double-blinded, controlled trial. J Pain Res. 2020;13:1647–1654. doi: 10.2147/JPR.S257466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Öksüz G, Bilal B, Gürkan Y, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. 2017;42(5):674–679. doi: 10.1097/AAP.0000000000000645 [DOI] [PubMed] [Google Scholar]
- 31.Kukreja P, MacBeth L, Sturdivant A, et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty: a randomized, controlled study. Reg Anesth Pain Med. 2019;44:1075–1079. doi: 10.1136/rapm-2019-100804 [DOI] [PubMed] [Google Scholar]
- 32.Aslan M, Hergünsel GO. Effect of quadratus lumborum block on postoperative analgesic requirements in pediatric patients: a randomized controlled double blinded study. Minerva Anestesiol. 2019;86:150–156. doi: 10.23736/S0375-9393.19.13361-5 [DOI] [PubMed] [Google Scholar]
- 33.Akerman M, Pejčić N, Veličković I. A review of the quadratus lumborum block and ERAS. Front Med. 2018;26(5):44. doi: 10.3389/fmed.2018.00044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumar A, Sadeghi N, Wahal C, Gadsden J, Grant SA. Quadratus lumborum spares paravertebral space in fresh cadaver injection. Anesth Analg. 2017;125(2):708–709. doi: 10.1213/ANE.0000000000002245 [DOI] [PubMed] [Google Scholar]
- 35.Putzu M, Gambaretti E, Rizzo F, Latronico N. Postoperative analgesia for laparotomic surgery provided by bilateral single-shot quadratus lumborum block. Minerva Anestesiol. 2018;84(10):1231–1232. doi: 10.23736/S0375-9393.18.12777-5 [DOI] [PubMed] [Google Scholar]
- 36.Murouchi T, Iwasaki S, Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med. 2016;41(2):146–150. doi: 10.1097/AAP.0000000000000349 [DOI] [PubMed] [Google Scholar]
- 37.Carline L, McLeod GA, Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016;117(3):387–394. doi: 10.1093/bja/aew224 [DOI] [PubMed] [Google Scholar]
- 38.Yayik AM, Cesur S, Ozturk F, Ahiskalioglu A, Celik EC. Continuous quadratus lumborum type 3 block provides effective postoperative analgesia for hip surgery: case report. Rev Bras Anestesiol. 2019;69(2):208–210. doi: 10.1016/j.bjan.2018.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deng W, Long X, Li M, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain management after laparoscopic colorectal surgery: a randomized controlled trial. Medicine. 2019;98(52):e18448. doi: 10.1097/MD.0000000000018448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simpson JC, Bao X, Agarwala A. Pain management in enhanced recovery after surgery (ERAS) protocols. Clin Colon Rectal Surg. 2019;32(2):121–128. doi: 10.1055/s-0038-1676477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Backer JT, Jordan MR, Leahy DT, et al. Preemptive analgesia decreases pain following anorectal surgery: a prospective, randomized, double-blinded, placebo-controlled trial. Dis Colon Rectum. 2018;61(7):824–829. doi: 10.1097/DCR.0000000000001069 [DOI] [PubMed] [Google Scholar]
- 42.Boulianne M, Paquet P, Veilleux R, et al. Effects of quadratus lumborum block regional anesthesia on postoperative pain after colorectal resection: a randomized controlled trial. Surg Endosc. 2020;34:4157–4165. doi: 10.1007/s00464-019-07184-0 [DOI] [PubMed] [Google Scholar]
- 43.Michelet D, Andreu-Gallien J, Skhiri A, Bonnard A, Nivoche Y, Dahmani S. Factors affecting recovery of postoperative bowel function after pediatric laparoscopic surgery. J Anaesthesiol Clin Pharmacol. 2016;32(3):369–375. doi: 10.4103/0970-9185.168196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cavallaro P, Bordeianou L. Implementation of an ERAS pathway in colorectal surgery. Clin Colon Rectal Surg. 2019;32(2):102–108. doi: 10.1055/s-0038-1676474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang D, He Y, Chen X, Lin Y, Liu Y, Yu Z. Ultrasound guided lateral quadratus lumborum block enhanced recovery in patients undergoing laparoscopic colorectal surgery. Adv Med Sci. 2021;66(1):41–45. doi: 10.1016/j.advms.2020.12.002 [DOI] [PubMed] [Google Scholar]
- 46.Zhu M, Qi Y, He H, Zhang S, Mei Y. Effect of quadratus lumborum block on postoperative cognitive function in elderly patients undergoing laparoscopic radical gastrectomy: a randomized controlled trial. BMC Geriatr. 2021;21(1):238. doi: 10.1186/s12877-021-02179-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang ZD, Gu HY, Zhu J, et al. The application of enhanced recovery after surgery for upper gastrointestinal surgery: meta-analysis. BMC Surg. 2020;20(1):3. doi: 10.1186/s12893-019-0669-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jain S, Kalra S, Sharma B, Sahai C, Sood J. Evaluation of ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing intraperitoneal onlay mesh repair. Anesth Essays Res. 2019;13(1):126–131. doi: 10.4103/aer.AER_176_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kadam VR. Ultrasound⁃guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J Anaesth Clin Pharmacol. 2013;29(4):550–552. doi: 10.4103/0970-9185.119148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Korgvee A, Junttila E, Koskinen H, Huhtala H, Kalliomaki ML. Ultrasound-guided quadratus lumborum block for postoperative analgesia: a systematic review and meta-analysis. Eur J Anaesthesiol. 2021;38(2):115–129. doi: 10.1097/EJA.0000000000001368 [DOI] [PubMed] [Google Scholar]
- 51.Ge DJ, Qi B, Tang G, Li JY. Intraoperative dexmedetomidine promotes postoperative analgesia and recovery in patients after abdominal hysterectomy: a double-blind, randomized clinical trial. Sci Rep. 2016;6:21514. doi: 10.1038/srep21514 [DOI] [PMC free article] [PubMed] [Google Scholar]