Abstract
Supracondylar humeral fractures are widely considered the most common elbow fracture in children. Gartland classification plays a fundamental role in decision-making regarding management and prognosis. Recent literature recommends conservative management for non or minimally displaced fractures, whereas there seems to be a trend towards surgical treatment for all displaced fractures. The preferred treatment for displaced Gartland II and Gartland III fractures is closed reduction and percutaneous fixation with lateral pins. In particular patterns medial pin is recommended for obtain a stable construct. Neurovascular complications are mostly associated with Type III fractures and sometimes surgical exploration with fracture reduction is needed. Correct diagnosis and proper management protocol is mandatory for avoid early and late complications such as neurovascular impairment and malunion.
Keywords: supracondylar fractures, pediatric elbow, precutaneous fixation, Gartland classification
Introduction
Supracondylar humerus fractures in children are the most common fractures of the elbow, with an annual incidence estimated at 177.3 per 100000 and a male predominance accounting for 16% of all pediatric fractures (1). The more common presentation, accounting 90% of all cases, is at 5-7 years of age, and non-dominant arm is more frequently involved (2).
Clinical presentation of these fractures is for the 97-99% of cases in extension (3,4) due to the most frequent mechanism of injury represented by a fall onto the outstretched hand with the elbow in full extension.
The high risk of immediate complications potentially limb threatening due to the involvement of neurovascular structures requires a close vigilance and proper protocol management.
The potential complications associated with these fractures are cubitus varus deformity, prolonged loss of mobility and social consequence for the child and the family.
Presentation
The classical presentation is a fall on outstretched hand and consequent pain and swelling over the elbow. The characteristics of the pain are fundamental to ascertain whether are due to the fracture or related to muscle and tissue ischemia that has a late onset.
Urgent assessment should be done when there are absence of radial pulse, ischemia of hand (pale and cool extremities), severe swelling, skin puckering, open fracture and neurological injury (5). In case of neurological involvement, careful evaluation and documentation are suggested, in particular when it became apparent, the degree of involvement and progression of symptoms.
Radiological assessment
Antero-Posterior (AP) and a lateral view of the elbow should be performed in case of pain and tenderness after a trauma. Often the pain limits flexion and extension manoeuvres of the articulation leading to difficulties in the interpretation of the images.
The position of the ossification centers is checked, considering that they appear in a predictable order: capitellum at 1 year of age, radial head and medial epicondyle at 4-5 years of age, trochlea and olecranon at 8-9 years of age and lateral condyle appear at 10 years od age (6).
Assess the Baumann’s angle on AP view: the angle between the humeral shaft line and the parallel line to the lateral condylar phisis should be approximately 75° (7). In case of doubts, related to individual variation of Baumann’s angle, radiographs of the contralateral elbow should be used for comparison. Other parameters to evaluate are the alignment of anterior humeral line that should intersect the middle 1/3 of the capitellum, anterior and posterior fat pad sign as indicators of elbow effusion (8,9). A positive fat pad sign is suggestive of fracture even in case of absence of radiological fracture lines.
Classification
Extension type supracondylar fractures are more common than flexion type injuries, and are subdivided by Gartland (10) on the basis of displacement extent.
Type I are undisplaced fractures: often in these cases the fracture line is not easily visible and the fat pad sign could help for obtain a proper diagnosis.
In Gartland type II fractures the posterior cortical is intact but there is an angulation and the humeral line is positioned anterior to the middle of capitellum.
Type III fractures are completely displaced, the direction is often posteromedial, without continuity between the two fragments (Figure 1).
Figure 1.
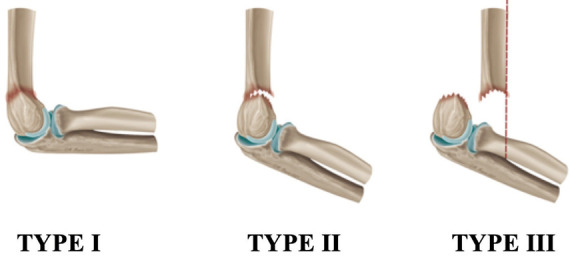
Gartland classification of supracondylar humeral fractures in children.
Gartland classification is successively modified by Wilkins et al (11), that introduce A and B subtipe for type II fractures. Type IIA are only extended, while Type IIB have some component of rotational displacement or translation. Leitch and colleagues expanded the classification with another type: Type IV fracture are multidirectionally unstable in both flexion and extension, because of complete loss of both anterior and pesterior periosteal hinges (12).
In this review we subdivided the treatment section on the basis of original Gartland classification, because thus probably helps the reader to better understand the decision making process.
Treatment
A patient with supracondylar elbow fracture requires emergent surgical attention in case of pale and pulseless hand. Closed fractures without neurovascular damage could be treated on an urgent basis with conservative or close/open surgery methods depending on the fracture pattern. Each decision should be taken by the orthopaedic surgeon considering Gartland classification (13,14).
Type I fracture
These fractures are by definition stable fractures with minimal risk of further displacement or angulation. Anterior humeral line is intact and the fracture displacement is less than 2 mm. The treatment is not surgical, in a long arm cast with the elbow in 60-90° of flexion for approximately 3 weeks (15). These injuries simply require immobilization for comfort and protection; long-term outcome is usually excellent (16,17). A pitfall in the treatment of Gartland type I fracture lies in not recognizing medial impaction that could result in a varus deformity, which will not correct with growth (18). A type I fracture with medial compression should be reduced with external manoeuvres under general anaesthesia preventing the cubitus varus.
In case of varus at the fracture site more than 10°, compared to contralateral limb, close reduction and percutaneous pinning should be strongly considered (2). Larger diameter pins should be adopted in order to obtain better stability and maintain reduction and alignment of the fracture.
Type II fracture
In a Gartland type II fracture the anterior humeral line is interrupted and the posterior cortex in hinged. In case of no rotational deformity, coronal malalignment or significant extension of distal fragment (type IIA according to Wilkins (19)) this injury may potentially be treated nonoperatively (20-22) with close reduction and casting. Circumferential casting and extreme manoeuvres of flexion should be avoided to prevent vascular and neurological compromises (9, 23). Surgeons should advise the parents about the possibility of loss of reduction and need for later surgical intervention.
If more than 90° of flexion is needed to maintain reduction, stabilization of the fracture with percutaneous pinning should be performed, in order to minimize risk of complications due to the position. Skaggs et al reported a large series with extremely low rates of complication and secondary operations after closed reduction and percutaneous pinning comparing to close reduction without pinning (24).
Type III fracture
Completely displaced supracondylar fractures, with or without rotational deformity, are classified as Gartland type III fractures and treated surgically in most centers. Close or even open reduction should be necessary and choice of treatment most often depends on the experience of the surgeon and the characteristics of the fracture (25). Most common and recommended treatments are reduction and pin fixation (9,25-27). Traumatic and idiopathic nerve injuries are quite common in this type of fractures. In a study nerve injury rate is reported up to 18% (only 3% preoperative) (28) that highlight the importance of a thorough preoperative and postoperative clinical examination of the patient. Nevertheless all patients sustained a nerve impairment in that series fully recovered at long-term follow up.
Also vascular injury rates are reported up to 20% in several studies conducted on patients with displaced Gartland type III supracondylar fractures (29,30). Reduction of the fracture in the operating room often improves the vascular condition and for this reason angiography prior to reduction is not recommended, in order to avoid any delay of the procedure.
Compartment syndrome is rare but should be considered in high-energy trauma (31), other risk factors are Gartland type III fractures, preoperative median nerve palsy, floating elbow, delayed treatment in a patient with vascular compromise, long arm casting in hyperflexion.
Techniques
Reduction manoeuvers
General anaesthesia and fluoroscopy assistance are mandatory to obtain an anatomic reduction freeing the proximal fragment from soft-tissue entrapment.
Surgeons should apply traction in line with the humerus in slight flexion, avoiding full extension to prevent tethering of neurovascular structures over the proximal fragment. In case of suspect that the proximal fragment has pierced through the brachialis muscle a gradual traction in slightly flexed elbow should be given for a minute, or in alternative a proximal to distal “milking” manoeuvre as described in literature (32).
The reduction manoeuvre should begin hyper flexing the elbow while pushing the olecranon in anterior direction. In case of internal rotation of distal fragment is necessary to press harder on the medial side during the reduction, and pronate the forearm. The opposite applies for an external rotation of distal fragment.
In case of vascular impairment if the status doesn’t improve after gross manoeuvre of reduction, open reduction must be performed.
Close reduction and percutaneous pinning
Close reduction and percutaneous pinning with K-wire remain the classic treatment options for all displaced supracondylar fracture or in case that manipulations fail to maintain the reduction.
Typically the child is positioned supine and the limb suspended over the side of the table. This position allows free access of the C-arm direct under the arm, parallel to the operating table. Fracture reduction is performed applying a longitudinal traction to the forearm, with previous described manoeuvres. Once obtained fracture reduction is confirmed fluoroscopically. Sagittal alignment may be checked by rotation of the C-arm to prevent loss of reduction. The Jones (transcondylar) view is useful to assess coronal alignment with the elbow flexed, internal and external rotations of the arm allow assessing the alignment of medial and lateral columns of the elbow. If reduction is satisfactory percutaneous pinning is performed. It’s controversial if whether a medial entry pin should be used or whether two lateral pins are sufficient. A standard technique of supracondylar fracture pinning is described by Mubarak and Davids (33). Two smooth 0.062 inch K-wire are placed through the capitellar side of the fracture, divergent or parallel, engaging the far cortex and preferably avoid crossing through the center of the olecranon fossa. After that the elbow is extended and the carrying angle is determined, assessing the stability of the fracture. A third lateral pin can be placed, but in case of medial comminution or varus instability a medial pin can be placed to augment the construct (Fig. 2,3). Extension of the elbow relaxes any tension on the ulnar nerve and allows the positioning of the medial pin in a safer manner. The pin should run in a slight posterior to anterior direction, because the medial epicondyle is a posteromedial structure. To protect the nerve, the surgeon’s thumb should be placed over the cubital tunnel and K-wire can the placed medially. Also this pin should engage the opposite far cortex. In case of acceptable reduction the pins are carefully bent and cut leaving approximately 2 cm to prevent migration and facilitate pin removal at 3 or 4 weeks postoperative. A long arm cast is then performed to protect the reduction.
Figure 2.
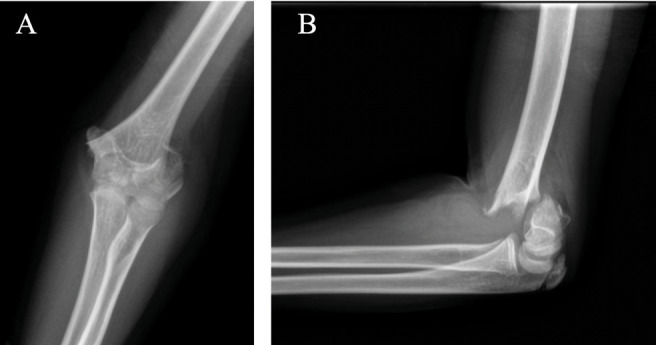
Gartland type III supracondylar humeral fracture (A: Anteroposterior view, B: Lateral view).
Figure 3.
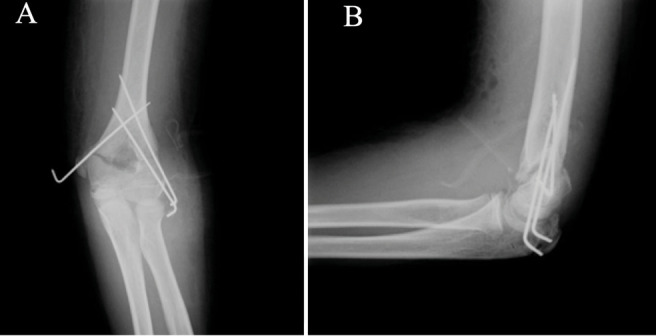
Post-operative x-rays of cross-pinning fixation (A: Anteroposterior view, B: Lateral view).
Both biomechanical and clinical comparisons between all-lateral and cross-pin constructs have been performed comparing the stability of the reduction, reoperation rate and iatrogenic ulnar nerve injury. Kocher et al in randomized prospective study reported a statistically significant decrease in risk of loss of reduction using the cross-pin technique (4%) compared with all-lateral technique (21%) (34).
Edmonds et al reported three different fracture pattern that necessitate a medial pin for the stability of the fixation: high supracondylar fracture without adequate cross sectional area for >2 lateral pins, fracture patterns that traverse near the olecranon fossa with comminution of the medial cortex and fractures with initial cubitus varus and medial instability that require a medial pin to act as a structural support for the medial cortex (35).
Comparing all-lateral fixation construct with cross-pinning fixation construct, results indicated that the risk of iatrogenic nerve injury with the first technique was 0.53% against 6% obtained with cross pinning fixation (35) with a relative risk of 1.44 (less common in lateral pinning) (36). Recent study (35) conducted on 381 supracondylar fractures reported an incidence of iatrogenic injury of 1% obtained with elbow in extension and manual protection of the ulnar nerve. The extension is the key because this manoeuvre will relax the nerve (37) and the position obtained allows for better palpation and identification of the medial epicondyle during pinning (33).
Open reduction and internal fixation
Failure to achieve adequate reduction is the most common cause of a poor outcome after supracondylar humeral fracture (Fig. 4,5,6) and open reduction is considered preferable to repeated attempts at closed reduction or accepting suboptimal alignment. Other indications are intrarticolar comminution, open fractures that require irrigation and debridement, vascular compromise or neurologic loss after reduction that require exploration and possible repair of neurovascular structures.
Figure 4.
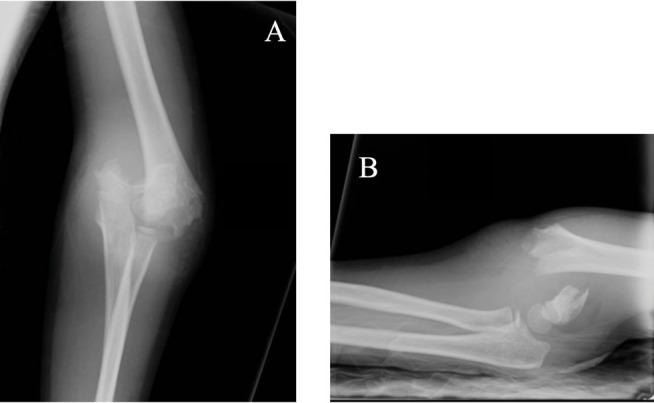
Gartland type III supracondylar humeral fracture (A: Anteroposterior view, B: Lateral view).
Figure 5.
Clinical result after reduction and stabilization with lateral pins.
Figure 6.
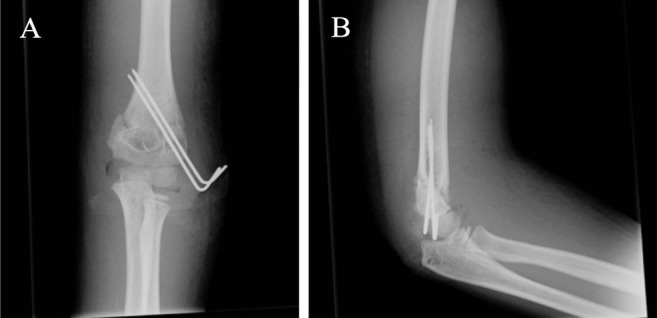
Lateral pin fixation: post-operative x-rays (A: Anteroposterior view, B: Lateral view).
Also soft tissue interposition require an open reduction, in particular Fleuriau-Chateau et al report buttonholing of the brachialis muscle by the distal end of proximal fragment as the most common finding in open procedures (38) (Fig. 7,8).
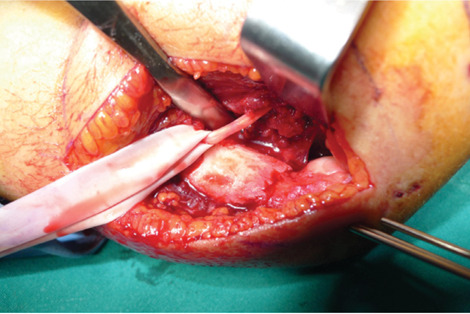
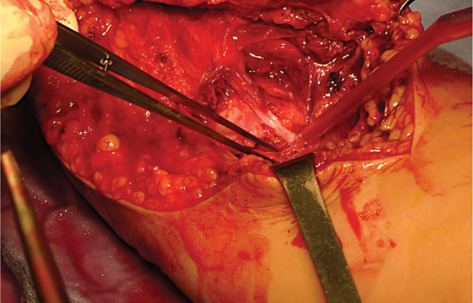
Figure 7.
Brachialis interposition at the fracture level that require open reduction.
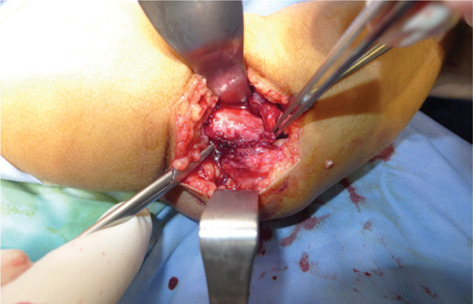
Figure 8.
Clinical result after reduction and stabilization with lateral pins.
Surgical approaches are choosed on the basis of the fracture type and neurovascular deficit. An anterior approach through a transverse incision in the antecubital fossa provides access to the common soft tissue impediments to reduction and the best exposure of the neurovascular structures (Fig. 9,10). Lateral approach is performed in case of symptoms that suggest radial nerve exploration. Lateral incision is made over the lateral condyle of the distal humerus and allows exposing the lateral side of the fracture. After reduction manoeuvres the pins are left protruding from the skin.
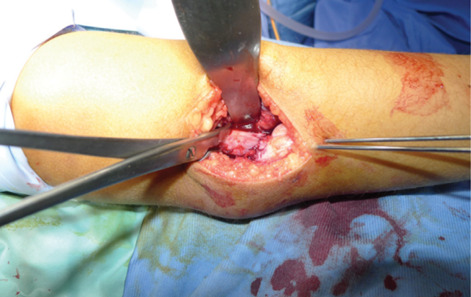
Figure 9.
Radial artery and nerve entrapment at the fracture site.
Figure 10.
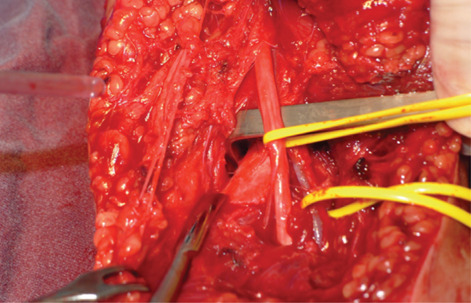
Radial artery and nerve after after estraction from the fracture.
In literature results after open reduction with pin fixation and closed reduction with percutaneous pin fixation are comparable (39), despite the fact that the fractures in the open reduction group were more severe and unable to be reduced by closed means (40).
Complications
Vascular deficit
Brachial artery injury is most commonly associated with Type II and III supracondylar fractures, in particular in case of postero-laterally displaced fractures (41,42). Radial pulseless is reported in 6 to 20 percent of all supracondylar fractures (15,43). Emergency exploration is mandatory in patients without significant improvement in pulse after orthopaedic care, expecially if there is intractable pain, persistence or increasing pain despite of fracture site reduction and stabilization (41-47).
Type III supracondylar fracture associated with vascular and neurological deficits should be treated with early exploration, because these characteristics are strongly predictive of nerve and vessel entrapment at the fracture site (46) (Fig. 9).
Isolated vascular deficit could be managed by closed reduction and could be observed for return of vascularity and if needed secondary exploration (2).
Compartment syndrome is a rare complication of supracondylar fracture of the humerus in children.
Vascular injury and primary swelling from the injury can lead to the development of compartment syndrome within 12 to 24 hours (48). The traditional signs of ischemia (pain, paresthesia, paralysis, pallor and pulselessness) are less rialable in predicting the presence of impending compartment syndrome in children. An increase of analgesic requirement has been shown to be the most sensitive indicator of impending compartment syndrome, preceding change in vascular status by more than 7 hours. Others characteristics are anxiety, agitation and progressive deterioration of neurological status. In these cases tissue pressure measurements should be obtained ad in case of high values a fasciotomy should be performed. In case of delayed treatment the ischemia may progress to infarction and subsequent development of Volkmann’s ischemic contracture: flexion of the elbow, pronation of the forearm, flexion at the wrist and metacarpal-phalangeal joint extension.
Neurologic deficit
The incidence of neurologic injury after extension type supracondylar humeral fractures is about 12% (49). The most common nerve involved is the anterior interosseus (median nerve), followed by injury to the radial nerve. Most often associated nerve injuries are neuroapraxias that usually resolve within two to three months (6,29,50,51).
Early nerve exploration is indicated if nerve function deteriorates after close reduction and pinning of the fracture because of the likelihood of nerve entrapment in the fracture site or iatrogenic injury.
Extraction of the nerve from the fracture or from constricting structures and removal of any compromising hardware should be performed ad soon as possible.
Malunion
Cubitus varus (also called “gunstock” deformity) is a common angular deformity after supracondylar fractures. Modern surgical techniques have reduced the incidence from 58% to approximately 3% in children treated properly (4).
This malunion occurs as a result of malreduction or loss of reduction of the fracture and recognition is often delayed until the elbow can be fully extended.
Other authors report higher risk of cubitus varus after anatomic reduction of type III fractures due to the initial compression of the medial column (52).
Cubitus varus is not only a cosmetic problem, it is associated with tardy ulnar nerve palsy (53), tardy Postero-Lateral Rotatory Instability (PLRI) (54) and secondary distal humeral fractures (55).
To avoid such complications humeral osteotomy is the indicated surgical procedure.
Conclusions
Supracondylar fracture of the humerus is a common problem in pediatric population and surgeons have to deal with such fractures sometime burdened by severe complications.
Conservative management is recommended for Gartland type I fractures and nondisplaced type II fractures. Closed reduction and percutaneous pinning (with two or three lateral pins) are the preferred treatment options for most displaced supracondylar fractures. Medial pin positioning is mandatory in particular fracture patterns and operative techniques are described to avoid nerve injuries. Usage of appropriate criteria is wise in managing these fractures; prognosis in case of complications or possible complication should be explained.
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997;5:19–26. doi: 10.5435/00124635-199701000-00003. doi: 10.5435/00124635-199701000-00003. [DOI] [PubMed] [Google Scholar]
- Kumar V, Singh A. Fracture supracondylar humerus: a review. J Clin Diagn Res. 2016;10(12):RE01–RE06. doi: 10.7860/JCDR/2016/21647.8942. doi: 10.7860/JCDR/2016/21647.8942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. J Pediatr Orthop B. 2001;10:63–67. PMID: 1126981. [PubMed] [Google Scholar]
- Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998;18:38–42. PMID 9449099. [PubMed] [Google Scholar]
- Villarin LA, Belk KE, Freid R. Emergency department evaluation and treatment of elbow and forearm injuries. Emerg Med Clin North Am. 1999;17(4):843–58. doi: 10.1016/s0733-8627(05)70100-0. PMID: 10584105 DOI: 10.1016/s0733-8627(05)70100-0. [DOI] [PubMed] [Google Scholar]
- Kasser JR, Beaty JH. Supracondylar fractures of the distal humerus. In: Beaty JH, Kasser JR, editors. Rockwood and Wilkins’ Fractures in Children. 5th. Philadelphia: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- Worlock P. Supracondylar fractures of the humerus. Assessment of cubitus varus by the Baumann angle. J Bone Joint Surg Br. 1986;68(5):755–7. doi: 10.1302/0301-620X.68B5.3782238. doi: 10.1302/0301-620X.68B5.3782238. [DOI] [PubMed] [Google Scholar]
- Skaggs DL. Elbow fractures in children: diagnosis and management. J Am Acad Orthop Surg. 1997;5(6):303–12. doi: 10.5435/00124635-199711000-00002. doi: 10.5435/00124635-199711000-00002. PMID: 10797226. [DOI] [PubMed] [Google Scholar]
- Azbug JM, Herman MJ. Management of supracondylar humerus fractures in children: Current concepts. J Am Acad Ortho Surg. 2012;20(2):69–77. doi: 10.5435/JAAOS-20-02-069. doi: 10.5435/JAAOS-20-02-069. PMID: 22302444. [DOI] [PubMed] [Google Scholar]
- Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109(2):145–54. PMID 13675986. [PubMed] [Google Scholar]
- Heal J, Bould M, Livingstone J. Reproducibility of the Gartland classification for supracondylar humeral fractures in children. J of Orthop Surg. 2007;15:12–14. doi: 10.1177/230949900701500104. doi: 10.1177/230949900701500104. PMID: 17429110. [DOI] [PubMed] [Google Scholar]
- Leicht KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-4 fracture. J Bone Joint Surg Am. 2006;88(5):980–5. doi: 10.2106/JBJS.D.02956. PMID: 16651572 DOI: 10.2106/JBJS.D.02956. [DOI] [PubMed] [Google Scholar]
- Gartland JJ. Supracondylar fractures of the humerus. Med Trial Tech Q. 1963;10:37–46. PMID:14101044. [PubMed] [Google Scholar]
- Barton KL, Kaminsky CK, Green DW, Shean CJ, Kautz SM, Skaggs DL. Reliability of a modified Gartland classification of supracondylar humerus fractures. J Pediatr Orthop. 2001;21:27–30. doi: 10.1097/00004694-200101000-00007. doi: 10.1097/00004694-200101000-00007. PMID: 11176349. [DOI] [PubMed] [Google Scholar]
- Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1121–1132. doi: 10.2106/JBJS.G.01354. doi: 10.2106/JBJS.G.01354. PMID: 18451407. [DOI] [PubMed] [Google Scholar]
- Cuomo AV, Howard A, Hsueh S, Boutis K. Gartland type I supracondylar humerus fractures in children: is splint immobilization enough? Pediatr Emerg Care. 2012;28:1150–1153. doi: 10.1097/PEC.0b013e3182716fea. PMID: 23114238. [DOI] [PubMed] [Google Scholar]
- Price CT, Flynn JM. Management of fractures. In: Morrissy RT, Weinstein SL, editors. Lovell and Winter’s pediatric orthopaedics. Philadelphia, PA: Lippincott,Williams & Wilkins; 2006. pp. 1430–1463. [Google Scholar]
- De Boeck H, De Smet P, Penders W, De Rydt D. Supracondylar elbow fracture with impaction of the medial condyle in children. J Pediatr Orthop. 1995 Jul-Aug;15(4):444–8. doi: 10.1097/01241398-199507000-00006. PMID: 7560031. doi: 10.1097/01241398-199507000-00006. [DOI] [PubMed] [Google Scholar]
- Wilkins KE. Supracondylar fractures: what’s new. J Pediatr Orthop B. 1997 Apr;6(2):110–6. doi: 10.1097/01202412-199704000-00006. doi: 10.1097/01202412-199704000-00006. PMID: 9165439. [DOI] [PubMed] [Google Scholar]
- Hadlow AT, Devane P, Nicol RO. A selective treatment approach to supracondylar fracture of the humerus in children. J Pediatr Orthop. 1996 Jan-Feb;16(1):104–106. doi: 10.1097/00004694-199601000-00021. doi: 10.1097/00004694-199601000-00021. PMID: 8747365. [DOI] [PubMed] [Google Scholar]
- Spencer HT, Dorey FJ, Zionts LE, Dichter DH, Wong MA, Moazzaz P, Silva M. Type II supracondylar humerus fractures: can some be treated nonoperatively? J Pediatr Orthop. 2012;32:675–681. doi: 10.1097/BPO.0b013e318269c459. PMID: 22955530 DOI: 10.1097/BPO.0b013e318269c459. [DOI] [PubMed] [Google Scholar]
- Parikh SN, Wall EJ, Foad S, et al. Displaced type II extension supracondylar humerus fractures: do they all need pinning? J Pediatr Orthop. 2004;24:380–384. doi: 10.1097/00004694-200407000-00007. doi: 10.1097/00004694-200407000-00007. PMID: 15205619. [DOI] [PubMed] [Google Scholar]
- Ponce BA, Hedequist DJ, Zurakowski D, Atkinson CC, Waters PM. Complications and timing of follow-up after closed reduction and percutaneous pinning of supracondylar humerus fractures: follow-up after closed reduction and percutaneous pinning of supracondylar humerus fractures. J Pediatr Orthop. 2004;24(6):610–14. doi: 10.1097/00004694-200411000-00002. PMID: 15502556 DOI: 10.1097/00004694-200411000-00002. [DOI] [PubMed] [Google Scholar]
- Skaggs DL, Sankar WN, Albrektson J, Vaishnav S, Choi PD, Kay RM. How safe is the operative treatment of Gartland Type 2 supracondylar humerus fractures in children? J Pediatr Orthop. 2008;28(2):139–41. doi: 10.1097/BPO.0b013e3181653ac8. PMID: 18388704 DOI:10.1097/BPO.0b013e3181653ac8. [DOI] [PubMed] [Google Scholar]
- Lee S, Park MS, Chung CY, Kwon DG, Sung KH, Kim TW, Choi IH, Cho TJ, Yoo WJ, Lee KM. Consensus and different perspectives on treatment of supracondylar fractures of the humerus in children. Clin Orthop Surg. 2012;4:91–97. doi: 10.4055/cios.2012.4.1.91. doi: 10.4055/cios.2012.4.1.91. PMID: 22379561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence-based guideline. J Pediatr Orthop. 2012;32(Suppl 2):S143–S152. doi: 10.1097/BPO.0b013e318255b17b. PMID: 22890454 DOI: 10.1097/BPO.0b013e318255b17b. [DOI] [PubMed] [Google Scholar]
- Howard A, Mulpuri K, Abel MF, Abel MF, Braun S, Bueche M, Epps H, Hosalkar H, Mehlman CT, Scherl S, Goldberg M, Turkelson CM, Wies JL, Boyer K. The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg. 2012;20:320–327. doi: 10.5435/JAAOS-20-05-320. doi: 10.5435/JAAOS-20-05-320. PMID: 22553104. [DOI] [PubMed] [Google Scholar]
- Khademolhosseini M, Abd Rashid AH, Ibrahim S. Nerve injuries in supracondylar fractures of the humerus in children: is nerve exploration indicated? J Pediatr Orthop B. 2013;22:123–126. doi: 10.1097/BPB.0b013e32835b2e14. doi: 10.1097/BPB.0b013e32835b2e14. PMID: 23222035. [DOI] [PubMed] [Google Scholar]
- Campbell CC, Waters PM, Emans JB, Kasser JR, Millis MB. Neurovascular injury and displacement in type III supracondylar humerus fractures. J Pediatr Orthop. 1995;15:47–52. doi: 10.1097/01241398-199501000-00011. doi: 10.1097/01241398-199501000-00011. PMID: 7883927. [DOI] [PubMed] [Google Scholar]
- Lyons ST, Quinn M, Stanitski CL. Neurovascular injuries in type III humeral supracondylar fractures in children. Clin Orthop Relat Res. 2000;376:62–67. doi: 10.1097/00003086-200007000-00010. PMID: 10906859 DOI: 10.1097/00003086-200007000-00010. [DOI] [PubMed] [Google Scholar]
- Diesselhorst MM, Deck JW, Davey JP. Compartment syndrome of the upper arm after closed reduction and percutaneous pinning of a supracondylar humerus fracture. J Pediatr Orthop. 2014;34(2):e1–4. doi: 10.1097/BPO.0b013e3182933c69. PMID: 23774207 DOI: 10.1097/BPO.0b013e3182933c69. [DOI] [PubMed] [Google Scholar]
- Archibeck MJ, Scott SM, Peters CL. Brachialis muscle entrapment in displaced supracondylar humerus fractures: a technique of closed reduction and report of initial results. J Pediatr Orthop. 1997;17(3):298–302. PMID: 9150015. [PubMed] [Google Scholar]
- Mubarak SJ, Davids JR. Closed reduction and percutaneous pinning of supracondylar fractures of the distal humerus in the child. In: Morrey BF, editor. Master Techniques in Orthopedic Surgery, The Elbow. New York: Raven Press, Ltd; 1994. pp. 37–51. [Google Scholar]
- Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, Hedequist D, Karlin L, Kim YJ, Murray MM, Millis MB, Emans JB, Dichtel L, Matheney T, Lee BM. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Am. 2007;89:706–712. doi: 10.2106/JBJS.F.00379. doi: 10.2106/JBJS.F.00379. PMID: 17403790. [DOI] [PubMed] [Google Scholar]
- Edmonds EW, Roocroft JH, Mubarak SJ. Treatment of displaced pediatric supracondylar humerus fracture patterns requiring medial fixation: a reliable and safer cross-pinning technique. J Pediatr Orthop. 2012 Jun;32(4):346–51. doi: 10.1097/BPO.0b013e318255e3b1. doi: 10.1097/BPO.0b013e318255e3b1. PMID: 22584833. ANZ J Surg. [DOI] [PubMed] [Google Scholar]
- Kwok SM, Clayworth C, Nara N. Lateral versus cross pinning in paediatric supracondylar humerus fractures: a meta-analysis of randomized control trials. ANZ J Surg. 2021 Apr 1 doi: 10.1111/ans.16743. doi: 10.1111/ans.16743. [DOI] [PubMed] [Google Scholar]
- Zaltz I, Waters PM, Kasser JR. Ulnar nerve instability in children. J Pediatr Orthop. 1996;16:567–569. doi: 10.1097/00004694-199609000-00003. PMID: 8865037 DOI: 10.1097/00004694-199609000-00003. [DOI] [PubMed] [Google Scholar]
- Fleuriau-Chateau P, McIntyre W, Letts M. An analysis of open reduction of irreducible supracondylar fractures of the humerus in children. Can J Surg. 1998;41(2):112–8. PMID: 9575993 PMCID: PMC3949823. [PMC free article] [PubMed] [Google Scholar]
- Duffy S, Flannery O, Gelfer Y, Monsell F. Overview of the contemporary management of supracondylar humeral fractures in children. Eur J Orthop Surg Traumatol. 2021 doi: 10.1007/s00590-021-02932-2. doi: 10.1007/s00590-021-02932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer KE, Devito DP, Green NE. Comparison of closed reduction and percutaneous pinning versus open reduction and percutaneous pinning in displaced supracondylar fractures of the humerus in children. J Orthop Trauma. 1992;6(4):407–12. doi: 10.1097/00005131-199212000-00002. doi: 10.1097/00005131-199212000-00002.PMID: 1494091. [DOI] [PubMed] [Google Scholar]
- Skaggs D, Pershad J. Pediatric elbow trauma. Paediatr Emerg Care. 1997;13(6):425–34. doi: 10.1097/00006565-199712000-00021. PMID: 9435010 DOI: 10.1097/00006565-199712000-00021. [DOI] [PubMed] [Google Scholar]
- Griffin KJ, Walsh SR, Markar S, Tang TY, Boyle JR, Hayes PD. The pink pulseless hand: a review of the literature regarding management of vascular complications of supracondylar humeral fractures in children. Eur J Vasc Endovasc Surg. 2008;36(6):697–702. doi: 10.1016/j.ejvs.2008.08.013. PMID: 18851922 DOI: 10.1016/j.ejvs.2008.08.013. [DOI] [PubMed] [Google Scholar]
- Garg S, Weller A, Larson AN, Fletcher ND, Kwon M, Schiller J, Schiller J, Browne R, Copley L, Ho C. Clinical characteristics of severe supracondylar humerus fractures in children. J Pediatr Orthop. 2014;34(1):34–39. doi: 10.1097/BPO.0b013e31829c0046. doi: 10.1097/BPO.0b013e31829c0046. PMID: 23812149. [DOI] [PubMed] [Google Scholar]
- Lins RE, Simovitch RW, Waters PM. Pediatric elbow trauma. Orthop Clin North Am. 1999;30:119. doi: 10.1016/s0030-5898(05)70066-3. PMID: 9882730 DOI: 10.1016/s0030-5898(05)70066-3. [DOI] [PubMed] [Google Scholar]
- Valentini MB, Farsetti P, Martinelli O, Laurito A, Ippolito E. The value of ultrasonic diagnosis in the management of vascular complications of supracondylar fractures of the humerus in children. Bone Joint J. 2013;95(5):694–98. doi: 10.1302/0301-620X.95B5.31042. PMID: 23632684 DOI: 10.1302/0301-620X.95B5.31042. [DOI] [PubMed] [Google Scholar]
- Mangat KS, Martin AG, Bache CE. The ‘pulseless pink’ hand after supracondylar fracture of the humerus in children: the predictive value of nerve palsy. J Bone Joint Surg Br. 2009;91:1521–25. doi: 10.1302/0301-620X.91B11.22486. PMID: 19880900 DOI: 10.1302/0301-620X.91B11.22486. [DOI] [PubMed] [Google Scholar]
- Blakey CM, Biant LC, Birch R. Ischaemia and the pink, pulseless hand complicating supracondylar fractures of the humerus in childhood: long-term follow up. J Bone Joint Surg Br. 2009;91:1487. doi: 10.1302/0301-620X.91B11.22170. PMID: 19880895 DOI: 10.1302/0301-620X.91B11.22170. [DOI] [PubMed] [Google Scholar]
- Wu J, Perron AD, Miller MD, Powell SM, Brady WJ. Orthopaedic pitfalls in the ED: pediatric supracondylar humerus fractures. Am J Emerg Med. 2002;20(6):544–50. doi: 10.1053/ajem.2002.34850. PMID: 12369030 DOI: 10.1053/ajem.2002.34850. [DOI] [PubMed] [Google Scholar]
- Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop. 2010;30(3):253–63. doi: 10.1097/BPO.0b013e3181d213a6. PMID: 20357592 DOI: 10.1097/BPO.0b013e3181d213a6. [DOI] [PubMed] [Google Scholar]
- Lyons ST, Quinn M, Stanitski CL. Neurovascular injuries in type III humeral supracondylar fractures in children. Clin Orthop Relat Res. 2000;376:62–67. doi: 10.1097/00003086-200007000-00010. PMID: 10906859 DOI: 10.1097/00003086-200007000-00010. [DOI] [PubMed] [Google Scholar]
- Barrett KK, Skaggs DL, Sawyer JR, Andras L, Moisan A, Goodbody C, Flynn JM. Supracondylar humeral fractures with isolated anterior interosseous nerve injuries: is urgent treatment necessary? J Bone Joint Surg Am. 2014;96(21):1793–97. doi: 10.2106/JBJS.N.00136. PMID: 25378506 DOI: 10.2106/JBJS.N.00136. [DOI] [PubMed] [Google Scholar]
- Eren A, Guven M, Erol B, Akman B, Ozkan K. Correlation between posteromedial or posterolateral displacement and cubitusvarus deformity in supracondylar humerus fractures in children. J Child Orthop. 2008;2(2):85–89. doi: 10.1007/s11832-008-0088-y. PMID: 19308586 PMCID: PMC2656790 DOI: 10.1007/s11832-008-0088-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abe M, Ishizu T, Shirai H, Okamoto M, Onomura T. Tardy ulnar nerve palsy caused by cubitus varus deformity. J Hand Surg Am. 1995;20:5–9. doi: 10.1016/S0363-5023(05)80047-4. PMID: 7722265 DOI: 10.1016/S0363-5023(05)80047-4. [DOI] [PubMed] [Google Scholar]
- O’Driscoll SW, Spinner RJ, McKee MD, Kibler WB, Hastings H, Morrey BF, Kato H, Takayama S, Imatani J, Toh S, Graham HK. Tardy posterolateral rotatory instability of the elbow due to cubitusvarus. J Bone Joint Surg Am. 2001;83:1358–69. doi: 10.2106/00004623-200109000-00011. PMID: 11568199 DOI: 10.2106/00004623-200109000-00011. [DOI] [PubMed] [Google Scholar]
- Takahara M, Sasaki I, Kimura T, Kato H, Minami A, Ogino T. Second fracture of the distal humerus after varusmalunion of a supracondylar fracture in children. J Bone Joint Surg Br. 1998;80:791–97. doi: 10.1302/0301-620x.80b5.8831. PMID: 9768888 DOI: 10.1302/0301-620x.80b5.8831. [DOI] [PubMed] [Google Scholar]


