Abstract
Background
Although much of the attention surrounding the opioid epidemic has focused on rural and suburban Whites and prescription opioids, heroin overdoses among urban Blacks are on the rise. While some argue that legalization of cannabis will combat the epidemic, there are concerns it ignores the shift in the epidemic and could increase vulnerability to opioid misuse. The goal of this study is to examine the association between cannabis use from adolescence to young adulthood with opioid misuse in a primarily urban Black cohort.
Methods
Data are from a study of 580 youth (85% Black, 67% low SES) residing in Baltimore City followed from ages 626. Cannabis trajectories were identified between ages 14–26 using group-based trajectory modeling. Logistic regressions were conducted to examine the impact of trajectories on opioid misuse in young adulthood adjusting for individual, neighborhood and peer factors. Opioid misuse was defined as using heroin or narcotics or painkillers without a prescription between ages 1926.
Results
Four cannabis trajectories were identified: Low/Non-Users (59.7%) Adolescent Onset Limited (19.5%), Young Adult Onset (10.8%), and Adolescent Onset Chronic (10.0%). Adolescent Onset Chronic cannabis users had the highest rate of opioid misuse (44.8%) followed by Adolescent Onset Limited (18.8%), Young Adult Onset (14.8%) and Low/Non-Users (8.3%). Prevalences were significantly higher for Adolescent Onset group relative to Low/Non-Users even after adjustment for neighborhood factors.
Conclusions
Adolescent onset cannabis use is associated with opioid misuse in young adulthood among urban Blacks even after adjustment for neighborhood factors associated with opioid misuse.
Keywords: Blacks, cannabis, longitudinal patterns, opioids, urban
1. Introduction
The opioid epidemic remains a public health emergency with an estimated 130 Americans dying each day from an opioid overdose (Hedegaard et al., 2018). Much of the national attention surrounding the epidemic has focused on White suburban and rural users and the over-prescription of painkillers. However, recent data suggest a shift in the epidemic with heroin more often reported as the first opioid of use rather than prescription opioids (Cicero et al., 2017, 2018). This shift may be due to the success of prescription opioid supply chain reduction efforts (Dart et al., 2015) as well as the increased availability of heroin; a cheaper alternative with a comparable high (Cicero et al., 2014; Compton et al., 2016).
With the majority of opioid overdoses occurring among Whites, less attention has been given to the impact of the epidemic on the Black community. However, there have been substantial increases in opioid overdoses among Blacks from 3.5 per 100,000 in 2000 to 14.0 per 100,000 in 2018 (CDC, 2020). In fact, opioid mortality rates have been increasing more rapidly over the past five years for Blacks compared to Whites (James & Jordan, 2018) with the sharpest increase in opioid overdoses occurring among Blacks living in urban areas (Lippold et al., 2019). Blacks may be at an increased risk for opioid overdoses as heroin and injection drug use has been on the rise in many urban centers in the US where Blacks disproportionately reside (Brighthaupt et al., 2019). In fact, heroin overdoses more than quadrupled for Blacks from 0.9 per 100,000 in 2000 to 4.9 per 100,00 in 2018 (CDC, 2020; SAMHSA, 2020). It is suspected that some of the increase in opioid overdoses in the Black community may be attributable to the more potent fentanyl-laced heroin entering the illict drug supply in urban areas (Katz & Goodnough, 2017; Spencer et al., 2019; SAMHSA, 2020).
Despite alarming increases in overdoses in the Black community and the national framing of the epidemic as a public health problem, Blacks are more likely to be arrested as a result of their opioid use, while Whites are more often refered to treatment (Human Rights Watch, 2009). Hence, the public health focus remains on prescription opioids and physician prescribing practices. In fact, some states are attempting to modify existing medical cannabis laws to allow patients to substitute their prescription opioids with medical cannabis to treat chronic pain as a means to attenuate the epidemic, despite conflicting evidence of the impact of these laws (Bachhuber et al., 2014; Bradford et al., 2018; Chihuri & Li 2019; Flexon et al., 2019; Nugent et al., 2017; Shover et al., 2019; Wen et al., 2015; Wen & Hockenberry, 2018). Not only does this approach ignore the role heroin is playing in the epidemic, it ignores the fact that Blacks are less likely to be prescribed opioids than Whites (Green et al., 2003; Meghani et al., 2012).
Efforts to legalize medical cannabis also ignore preliminary data suggesting cannabis use may increase vulnerability to opioid misuse. This could place individuals no necessarily prescribed opioids, like Blacks, at increased risk for opioid misuse. Pharmacologic evidence suggests that exposure to cannabis increases opioid intake and impacts the rewarding properties of opiates (Chen et al., 1990; Corchero et al., 1997; Ellgren et al., 2007; Hurd et al., 2014; Ledent et al., 1999; Manzanares et al., 1998, 1999; Tanda et al., 1997). Animal studies have demonstrated a cross-sensitization for a wide range of delta-9-tetrahydrocannabinol (THC) doses and opioids (Cadoni et al., 2001; 2008; Gorriti et al., 1999; Lamarque et al., 2001). Finally, clinical studies suggest cannabis use may lead to behavioral disinhibition, which can increase the risk of using opioids (Fergusson et al., 2003; Lopez-Quintero et al., 2011; Lynskey et al, 1998). Longitudinal epidemiologic data examining the cannabis-opioid causal pathway, however, are limited. In a twin study, use of cannabis before the age of 17 was significantly associated with opioid misuse and dependence in adulthood (Lynskey et al., 2003). A study using data from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) found that cannabis use before the age of 18 was associated with prescription opioid misuse between ages 18–25 (Fiellin et al., 2013) while another study, also using NESARC data, found that cannabis use at baseline was associated with prescription opioid misuse and disorder at follow-up (Olfson et al., 2018). These few studies examining the association between cannabis and opioids were limited to examining cannabis use at one point in time and were conducted in primarily White samples.
In the present study, we seek to identify trajectories of cannabis use from ages 14–26 in a sample of primarily low-income, urban-dwelling Blacks and examine their impact on opioid misuse in young adulthood (ages 19–26). We focus on trajectories because there is likely a great deal of heterogeneity in longitudinal patterns of cannabis use that may reflect different etiologic pathways and different susceptibilities to opioid misuse (Ellickson et al., 2004; Kelly & Vuolo, 2018; Lee et al., 2018; Scalco & Colder, 2017). Because individuals are embedded within social contexts, an examination of socioecological factors is necessary to understand etiological pathways associated with cannabis use over time. Therefore, we examine whether neighborhood violence, neighborhood disorder, deviant peer affiliation, and early use of other drugs are predictive of cannabis trajectories in addition to individual level socio-demographics. These factors are particularly salient in impoverished urban neighborhoods where residents may be unable to monitor activities in their neighborhoods and, as a result, drug use (both licit and illicit) may flourish promoting ease of availability as well as reinforcement of positive drug-using norms (Sampson et al., 1997). These neighborhoods also often lack the social capital to provide positive experiences for youth which can result in the formation of deviant peer groups where values conducive to drug use can arise and spread (Dishion et al., 1999; Patterson et al., 1992). In addition, early use of alcohol and tobacco may provide a surrogate both for availability of drugs and exposure to positive drug -taking norms, as well as a possible ‘common liability’ to use other drugs and may, thus, be important to consider in relation to cannabis use trajectories, as well as opioid misuse (Degenhardt et al., 2009; Palmer et al., 2009). The purpose of this study is to provide longitudinal evidence as to whether cannabis use increases vulnerability to opioid misuse after adjusting for socioecological risk factors particularly salient in low-income, Black communities to better understand potential unintended consequences of cannabis legalization in these vulnerable communities.
2. Method
2.1. Sample
Data were derived from a randomized prevention trial conducted by the Baltimore Prevention Research Center at the JHU Bloomberg School of Public Health. A total of 798 children and families entering 1st grade in nine Baltimore City public elementary schools in 1993 were recruited to participate in two school-based, preventive interventions targeting early learning and aggressive and disruptive behavior. Students were randomly assigned to one of two intervention or control classrooms (9 schools, 3 classrooms per school). Interventions were provided during the 1st grade year. The sample of 798 children was predominantly Black (85%) and 46% were male. The mean age at entrance into first grade was 6.2 years (SD=0.37). About 2/3 of children were receiving free or reduced price meals; a proxy for low socioeconomic status. Annual structured interviews were conducted through age 26 in 2013 using an audio-computer assisted interview to increase accurate reporting of sensitive behavior. The sample for this analysis included 580 youth with an assessment in 8th grade and at least one young adult (ages 19–26) assessment. This sample in 1st grade was 87% Black, 54% male, and 71% were receiving free or reduced-price meals.
2.2. Measures
Frequency of Substance Use
Frequency of cannabis, opioid, alcohol and tobacco use in the past year was assessed annually with questions adapted from the Monitoring the Future (MTF) study (Johnston et al., 2000). Participants reported on the frequency of use in the past year on a 0–7 Likert scale: (0=none, 1=once, 2=twice, 3=3–4 times, 4=5–9 times, 5=10–19 times, 6=20–39 times, 7=40 or more times). Data on opioid misuse were collected beginning at age 19. Opioid misuse included heroin and the misuse of prescription narcotics (e.g., morphine, oxycodone, hydrocodone, hydromorphone, etc.). Participants who reported misusing any of these substances in the past year at any of the assessments between ages 19 and 26 were coded as positive for opioid misuse. Data on cannabis, alcohol and tobacco use were collected annually beginning at age 14. Past year frequency of use of cannabis from ages 14–26 was used for trajectory modeling. Early use of alcohol and tobacco was included as a covariate and defined as using the substance before age 15.
Neighborhood Disorder
Perceptions of neighborhood disorder were assessed in 8th grade using 10 items from the Neighborhood Environment Scale (Elliott et al., 1985). This scale contains true- false items that assess neighborhood safety, violent crime, and drug use and sales. Items are rated on a 4-point Likert scale (1=not at all true to 4=very true) and summed to create a total score.
Neighborhood Violence
Exposure to violence in the community was measured in 8th grade using the Children’s Report of Exposure to Violence (Cooley-Quille et al., 1995). This is a self-report measure of exposure to violence that is directly witnessed, as well as victimization. The events include being beaten up, robbed or mugged, stabbed or shot, witnessing someone else experience one of these events or witnessing a murder in the community. Youth who experienced any exposure to violence were compared to all others using a binary indicator.
Deviant Peer Affiliation
We used a subset of items from Capaldi and Patterson’s youth self-report scale to measure deviant peer affiliation in sixth, seventh and eighth grades (Capaldi & Patterson, 1989). Youth were asked in multiple choice format to indicate how many of their friends (1 = none to 5 = all of them) have engaged in antisocial behavior, such as hitting or threatening someone, stealing, and damaging others’ property and how many of their friends have used marijuana. This scale was the sum of seven items with higher scores indicating more deviant peer affiliation.
Sociodemograyhics
The school district provided information on students’ sex and ethnicity. School records and parent reports indicating each student’s free and reduced-price meal status were collapsed into a dichotomous variable of free or reduced price meals versus self-paid meals at any time during high school as an individual indicator of student socioeconomic status. Intervention status was coded 1 for youth in a 1st grade intervention classroom and 0 otherwise.
2.3. Analysis
Group-based trajectory modeling was used to identify patterns of past-year cannabis use frequency from age 14 to 26 (Nagin & Tremblay, 1999). Models used zero-inflated Poisson distribution to account for the large number of youth that did not use cannabis. Linear and quadratic terms for each trajectory group were included and compared. One to five group models were considered. The best model was selected based on a combination of the Bayesian information criteria (BIC), entropy, group interpretability, and having reasonably large groups (at least 10% of the sample). Trajectory models were constructed using PROC TRAJ in SAS version 9.4. Maximum likelihood estimation was used to estimate model parameters. Participants were assigned to the cannabis trajectory group with the highest probability of membership. Bivariate associations between trajectory group membership and measures of individual, peer and neighborhood characteristics were tested using chi-squared tests for categorical outcomes and F- tests for continuous measures. Bivariate associations between cannabis trajectory membership and opioid misuse in young adulthood were tested using chi-squared tests. We examined the relationship between cannabis trajectories and opioid misuse overall, as well as prescription opioid misuse and heroin separately. A logistic regression model was then fitted to estimate the strength of the association in specific cannabis use trajectory groups before and after adjustment for socioecological factors and other substance use behaviors.
3. Results
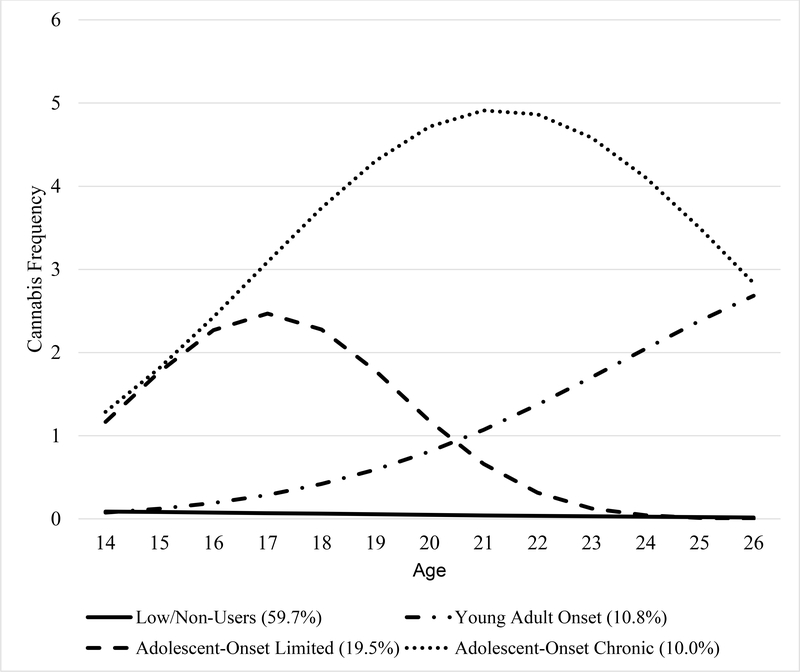
For modeling cannabis trajectories from age 14 to 26, the BIC increased with the addition of each trajectory group, but the rate of improvement declined and reached an elbow at four groups (Table 1). Entropy measures indicated the classification accuracy was adequate for all models. The four-group cannabis trajectory model is presented in Figure 1. The most common trajectory was a group with little to no cannabis use between the ages of 14 and 26 (Low/Non-Users; 59.7%). The largest cannabis user group was a group that was using cannabis by age 14 with increasing frequency until age 18 followed by declines in use (Adolescent Onset Limited; 19.5%). A second group was also using cannabis by age 14, but their frequency of use increased into adulthood (Adolescent Onset Chronic; 10.0%). The third group of cannabis users did not begin using cannabis until after the age of 18 (Young Adult Onset; 10.8%).
Table 1.
Fit indices for cannabis trajectory group solutions.
| Number of Trajectory Groups | BIC | Entropy | Minimum Class Size (%) |
|---|---|---|---|
| 1 | −10780.2 | 1.00 | 100.0 |
| 2 | −7538.1 | 0.99 | 29.1 |
| 3 | −6791.6 | 0.98 | 17.2 |
| 4 | −6359.0 | 0.98 | 10.0 |
| 5 | −6279.9 | 0.96 | 9.8 |
| 6 | −6147.8 | 0.95 | 5.4 |
Figure 1.
Cannabis Trajectories Ages 14–26
As shown in Table 2, after assigning youth to their most likely cannabis trajectory group, youth in the Young Adult Onset, Adolescent Onset Limited, and Adolescent Onset Chronic trajectory groups were more likely to be male, exposed to violence in their neighborhood and to be early drinkers compared to those in the Low/Non-User group. Both Adolescent Onset Limited and Adolescent Onset Chronic trajectory groups were more likely to affiliate with deviant peers, live in disordered neighborhoods and initiate tobacco use early compared to Low/Non-User and Young Adult Onset groups.
Table 2.
Individual, peer and neighborhood factors by cannabis trajectory group
| Characteristic | Overall N=580 |
Low/Non-Users N=349 |
Young Adult Onset N=61 |
Adolescent Onset Limited N=112 |
Adolescent Onset Chronic N=58 |
|
|---|---|---|---|---|---|---|
| Binary indictors | N (%) | N (%) | N (%) | N (%) | N (%) | p-value |
| Male Sex | 314 (54.1) | 171 (49.0) | 38 (62.3) | 66 (58.9) | 39 (67.2) | 0.016 |
| Black Race | 505 (87.1) | 304 (87.1) | 56 (91.8) | 100 (89.3) | 45 (77.6) | 0.096 |
| Free/Reduced Price Lunch | 369 (70.0) | 214 (66.5) | 39 (73.6) | 73 (73.7) | 43 (81.1) | 0.110 |
| Intervention Group | 378 (65.2) | 234 (67.1) | 41 (67.2) | 65 (58.0) | 38 (65.5) | 0.366 |
| Violence Exposure | 334 (57.6) | 167 (47.8) | 43 (70.5) | 86 (76.8) | 38 (65.5) | <0.001 |
| Early Alcohol Use | 385 (66.4) | 196 (56.2) | 45 (73.8) | 95 (84.8) | 49 (84.5) | <0.001 |
| Early Tobacco Use | 195 (33.6) | 77 (22.1) | 19 (31.2) | 68 (60.7) | 31 (53.4) | <0.001 |
| Scales | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-value |
| Deviant Peer Affiliation | 1.56 (0.64) | 1.58 (0.56) | 1.58 (0.72) | 1.74 (0.68) | 1.72 (0.81) | 0.0004 |
| Neighborhood Disorder | 1.73 (0.64) | 1.66 (0.60) | 1.70 (0.70) | 1.81 (0.62) | 1.97 (0.73) | 0.0032 |
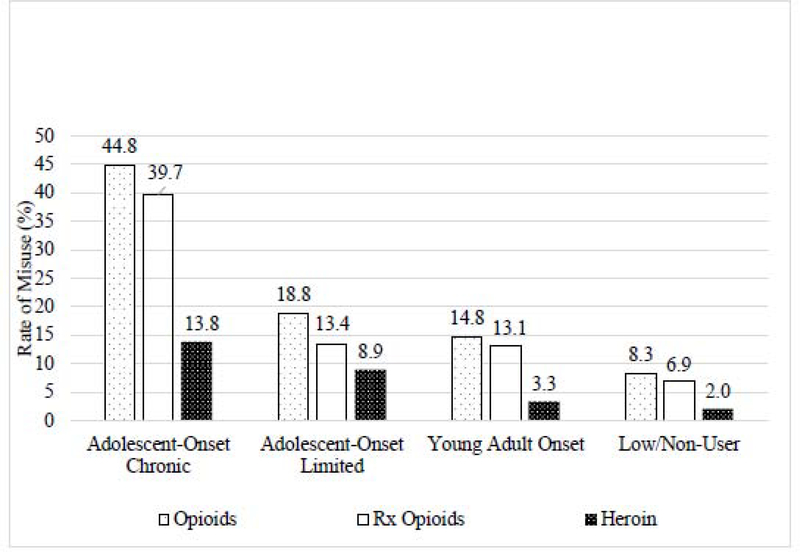
As shown in Figure 2, Adolescent Onset Chronic cannabis users had the highest rates of opioid misuse (44.8%), prescription opioid misuse (39.7%) and heroin use (13.8%) followed by Adolescent Onset Limited (18.8%, 13.4%, 8.9%), Young Adult Onset (14.8%, 13.1%, 3.3%) and Low/Non-Users (8.3%, 6.9%, 2.0%). Overall, 14.7% of our sample misused opioids in young adulthood. Specifically, 12.1% misused prescription opioids and 4.7% used heroin. Only 20% of opioid users reported using opioids more than five times in the past year between ages 19 and 21, increasing to 33–47% between ages 22 and 26.
Figure 2.
Rates of Opioid Misuse Between Ages 19–26 by Cannabis Trajectory Group
In unadjusted logistic regression models presented in Table 3, Adolescent Onset Limited and Adolescent Onset Chronic cannabis use trajectories were significantly associated with opioid misuse overall and prescription opioid misuse and heroin use specifically in young adulthood. The effect sizes were highest for the Adolescent Onset Chronic cannabis use trajectory group compared to Low/Non-Users (OR=9.0, 95%CI=4.7, 17.0; OR=8.9, 95%CI=4.6, 17.4; OR=7.8, 9’%CI=2.7, 22.5, respectively) with effect sizes for the Adolescent Onset Limited (OR =2.5, 95% CI=1.4, 4.7; OR=2.1, 95% CI=1.1, 4.1; OR=4.8, 95% CI=1.8, 12.9) trajectory group much smaller. The Young Adult Onset trajectory was not associated with opioid misuse in unadjusted models. Blacks had a significantly reduced risk of opioid misuse (OR=0.4, 95%CI=0.2, 0.8), prescription opioid misuse (OR=0.4, 95%CI=0.2, 0.8) and heroin use (OR=0.4, 95%CI=0.2, 1.0). Males (OR=1.8; 95%CI=1.1, 2.9), early drinkers (OR=1.9; 95%CI=1.1, 3.3) and early tobacco users (OR=1.8; 95%CI=1.2, 2.9) were significantly more likely to report opioid misuse and, in particular, heroin use (OR=5.2, 95%CI=1.8, 15.2 for males OR=3.0, 95%CI=1.0, 8.9 for early drinkers and OR=2.6, 95%CI=1.2, 5.6 for early tobacco users). Affiliating with deviant peers was significantly associated with an increased risk of heroin use (OR=1.7; 95%CI=1.0, 2.7).
Table 3.
Associations Between Cannabis Trajectory Groups, Socioecological Factors and Opioid Misuse in Young Adulthood (age 19–26)
| Cannabis Trajectory | Opioids | Prescription Opioids | Heroin | |||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Non-Users | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Young Adult Onset | 1.9 (0.8, 4.3) | 1.8 (0.8, 4.1) | 2.0 (0.9, 4.8) | 2.0 (0.8, 4.9) | 1.7 (0.3, 8.2) | 1.4 (0.3, 7.2) |
| Adolescent Onset Limited | 2.5 (1.4, 4.7) | 2.2 (1.2, 4.4) | 2.1 (1.1, 4.1) | 2.1 (1.0, 4.4) | 4.8 (1.8, 12.9) | 3.4 (1.2, 10.0) |
| Adolescent Onset Chronic | 9.0 (4.7, 17.0) | 7.2 (3.6, 14.4) | 8.9 (4.6, 17.4) | 8.1 (3.9, 16.8) | 7.8 (2.7, 22.5) | 4.7 (1.5, 14.8) |
| Male Sex | 1.8 (1.1, 2.9) | 1.5 (0.9, 2.6) | 1.3 (0.8, 2.2) | 1.1 (0.6, 1.9) | 5.2 (1.8, 15.2) | 4.6 (1.5, 13.9) |
| Black Race | 0.4 (0.2, 0.8) | 0.5 (0.2, 0.9) | 0.4 (0.2, 0.8) | 0.5 (0.2, 0.9) | 0.4 (0.2, 1.0) | 0.4 (0.2, 1.2) |
| Free/Reduced Price Lunch | 1.1 (0.7, 1.9) | 1.0 (0.6, 1.8) | 1.2 (0.7, 2.1) | 1.1 (0.6, 2.0) | 0.8 (0.4, 1.8) | 0.8 (0.3, 1.8) |
| Intervention Group | 1.0 (0.6, 1.6) | 1.0 (0.6, 1.7) | 1.0 (0.6, 1.6) | 1.0 (0.6, 1.7) | 0.9 (0.4, 2.0) | 0.9 (0.4, 2.1) |
| Violence Exposure | 1.3 (0.8, 2.0) | 1.0 (0.6, 1.7) | 1.2 (0.7, 2.0) | 1.1 (0.6, 1.9) | 1.5 (0.7, 3.4) | 0.8 (0.3, 2.2) |
| Early Alcohol Use | 1.9 (1.1, 3.3) | 1.4 (0.7, 2.6) | 1.7 (0.9, 3.0) | 1.3 (0.6, 2.5) | 3.0 (1.0, 8.9) | 2.0 (0.6, 6.8) |
| Early Tobacco Use | 1.8 (1.2, 2.9) | 1.1 (0.6, 2.0) | 1.5 (0.9, 2.4) | 0.9 (0.5, 1.6) | 2.6 (1.2, 5.6) | 1.2 (0.5, 3.2) |
| Deviant Peer Affiliation | 1.1 (0.8, 1.6) | 0.9 (0.6, 1.3) | 1.0 (0.7, 1.5) | 0.8 (0.5, 1.3) | 1.7 (1.0, 2.7) | 1.3 (0.8, 2.2) |
| Neighborhood Disorder | 1.3 (0.9, 1.8) | 1.1 (0.7, 1.6) | 1.3 (0.9, 1.9) | 1.1 (0.7, 1.7) | 1.4 (0.8, 2.5) | 1.1 (0.6, 2.0) |
In fully adjusted models, the associations between Adolescent Onset Limited and Adolescent Onset Chronic trajectories and opioid misuse including prescription opioids and heroin remained significant. However, the magnitude of the association between the Adolescent Onset Limited (aOR=3.4, 95%CI=1.2, 10.0) and Adolescent Onset Chronic (aOR=4.7 95%CI=1.5, 14.8) trajectories and heroin use were diminished, while the magnitude of the association for prescription opioid misuse changed very little (aOR=2.1; 95%CI=1.1, 4.4 and aOR=8.1, 95%CI=3.9, 16.8). Blacks retained a significantly reduced risk for opioid misuse, specifically prescription opioid misuse (aOR=0.5, 95%CI=0.2, 0.9) and male gender remained significant for heroin use (aOR=4.6, 95%CI=1.5, 13.9). Affiliation with deviant peers, and early use of other substances did not retain statistical significance in fully adjusted models.
4. Discussion
In this sample of primarily low-income, urban Blacks, we identified four trajectories of cannabis use reflecting variation in timing of onset and patterns of use, consistent with other studies in urban samples (Brook, 2011; Finlay et al., 2012; Juon et al., 2011; Reboussin et al., 2018). Male gender, early onset drinking and exposure to neighborhood violence were predictive of cannabis using trajectories regardless of timing of onset relative to the non-using trajectory. In contrast, affiliation with deviant peers and living in more disordered neighborhoods distinguished Adolescent Onset (both Chronic and Limited) from Young Adult Onset cannabis trajectories. Involvement with deviant peers and living in disordered neighborhoods during adolescence may result in increased availability and exposure to positive drug-taking norms placing individuals at risk for early cannabis use (Dishion et al., 1999; Patterson et al., 1992; Sampson et al., 1997). Black youth are particularly vulnerable to these neighborhood level risk factors for early cannabis use as they disproportionately reside in socially-disadvantaged neighborhoods characterized by poverty, crime, violence. and physical disorder (Garbarino, 1995; Wallace and Muroff, 2002). We also found an association between early tobacco use and Adolescent Onset cannabis trajectories. This is consistent with studies showing that co-use of cannabis and tobacco is common (Agrawal et al., 2012; Lemyre et al., 2019; Schauer et al., 2015). Further, most users of cigarillos also report past month blunt use, i.e. smoking cannabis in a cigarillo wrapper (Antognoli et al., 2018). Therefore, early tobacco use, possibly in the form of cigarillos, which are disproportionately used by Blacks (Cohn et al., 2016), may result in an earlier transition to cannabis use due to the use of a common vehicle for administering tobacco and cannabis.
Prevalence of opioid misuse overall in this sample was almost three times current rates in the general population aged 18–25 (14.7% vs 5.6%) (SAMSHA, 2019). Opioid misuse was primarily misuse of prescription opioids not heroin, although the prevalence of heroin use was almost ten times that in the general population aged 18–25 (4.7% vs 0.5%). Prevalence of prescription opioid misuse and heroin use were also higher in our sample than for Blacks in the general population aged 18–25 (4.6% and 0.1%, respectively). Higher rates of heroin use in this sample is not surprising given that heroin has been endemic in Baltimore City since the 1960s (Agar & Reisinger, 2002; Schwartz et al., 2015). The higher prevalence of prescription opioid misuse is somewhat surprising given evidence of physicians’ under-prescribing of opioids to Blacks (Burgess et al., 2008). However, recent data find that almost two-thirds of Black prescription opioid misusers get opioids from sources other than a physician (SAMHSA, 2020). Baltimore City in particular has seen increases in morbidity and mortality due to prescription drug misuse since 2000 consistent with national trends (Wejnert, 2016). Male gender, affiliation with deviant peers, early drinking and early tobacco use were associated with increased risk of heroin but not prescription opioid misuse and may be reflective of increased access to heroin, alcohol, and tobacco in deviant peer groups during adolescence in low-income, urban neighborhoods.
Ever after adjustment for other risk factors, Adolescent Onset Chronic cannabis use conferred an eight-fold increased risk of prescription opioid misuse and an almost five-fold increased risk of heroin use compared to Low/Non-Use. Cannabis use that begins early but declines in young adulthood (Adolescent Onset Limited) was still associated with an increased risk of prescription opioid misuse and heroin use although the effect was much smaller (two to three times the risk, respectively). Findings for Young Adult Onset cannabis users were not statistically significant. These results are consistent with other prospective epidemiologic studies in primarily White samples demonstrating that early cannabis use is a risk factor for opioid misuse (Lynskey et al., 2003; Fiellen et al. 2013). These findings demonstrate that even after adjustment for other risk factors that are particularly salient among Blacks living in urban neighborhoods, adolescent cannabis use, whether it continues into young adulthood or declines, further increases their vulnerability for opioid misuse.
It is possible that some of the association between cannabis use initiated in adolescence with opioid misuse in young adulthood may be driven by shared morphology and neurobiological systems (Wiese & Wilson-Poe, 2018). For example, there is evidence that receptors within the endocannabinoid and opioidergic systems are found in many of the same neurobiological regions underlying reward and reinforcement, suggesting overlapping expression (Wiese & Wilson-Poe, 2018). These two systems are integrally connected such that in the nucleus accumbens, increased cannabinoid administration increases endogenous opioid levels (Caillé & Parsons, 2006; Valverde et al., 2001).
At the behavioral level, cannabis use in adolescence may increase exposure to drug-using peers or access to illicit mg markets, particularly for Blacks living in urban areas, that may confer an increased risk for using other substances such as opioids (Fergusson et al., 2003; Lopez-Quintero et al., 2011; Lynskey et al., 2003; Reboussin et al., 2016; Wilcox et al., 2002). While the associations between adolescent onset cannabis use and opioid misuse remained significant after adjustment for factors associated with both cannabis use and opioid misuse, including early use of other substances and affiliation with deviant peers, there was a notable attenuation in the magnitude of the effects for heroin use suggesting that some of the impact of early cannabis use in urban Black samples may be mediated by affiliation with deviant peers and early use of other substances, while the impact on prescription opioid misuse may be more independent of these environmental factors and potentially driven by brain cross-sensitization. These findings are consistent with family studies demonstrating the shared environment plays little role in the nonmedical use of analgesics with heritability playing a moderate role (Gillespie et al., 2019; Kendler et al., 2003).
Limitations of the study should be noted. First, we relied on self-report to measure drug use, which is subject to bias. Biological assays of drug use would have strengthened this study. Second, this study did not assess opioid use until age 19, so that we are unable to account for prior opioid use or draw conclusions about its’ incidence. We also did not collect data on the source of prescription opioids (e.g. street markets, overprescribing or illegal prescribing), which would have been helpful in understanding mechanisms. These data were also collected prior to the introduction of fentanyl into the illicit drug market, which may explain the higher rates of prescription opioid misuse relative to heroin misuse in this sample. Third, this study was limited to Baltimore City. Although national probability studies have provided critical information on drug use in the U.S. population as a whole, they are less informative in understanding prevalence in subgroups; particularly socioeconomically disadvantaged, ethnic minority populations living in large urban areas Our ability to accurately reflect minority drug use in the context of the urban neighborhoods and illuminate within group differences makes this a unique contribution to the literature. Lastly, our study followed up participants through young adulthood and future research is needed to investigate whether cannabis use during adolescence similarly confer risk for opioid misuse later into adulthood.
Implications
Our findings highlight that the magnitude of the risk of opioid misuse in young adulthood seems dependent upon the course of cannabis use, with the greatest risk conferred by cannabis use that begins in adolescence and escalates into young adulthood. Early, school-based prevention programs that address cannabis use among primarily low-income, urban Blacks are warranted to help prevent opioid misuse in young adulthood in this vulnerable population. Mechanistically, our results are in line with pharmacologic findings suggesting a cross-sensitization between cannabis and opioids. However, some of the association between cannabis and heroin use was explained by neighborhood factors suggesting the environment plays a larger role in the risk for heroin use than it does for prescription opioid misuse in this sample. Therefore, prevention programs that also target the neighborhood context are especially important for preventing heroin use among Blacks. As shown in Reboussin et al (2019), prosocial neighborhood activities (e.g. youth playing outside, adults interacting in a positive manner) have the potential to modify the negative effects of living in physically disordered, urban environments and should also be considered when developing interventions. While cannabis legalization may provide alternative pain treatment for primarily White adult patients who would normally be prescribed opioids, it ignores the impact of legalization on low-income, urban Blacks who are less often prescribed opioids. Legalization instead has the potential to increase adolescent cannabis use through greater availability and exposure to cannabis placing youth at increased risk for later opioid misuse, both prescription opioids and heroin Therefore, it is important that policymakers and clinicians consider and closely monitor the potential unintended consequences of cannabis legalization on these vulnerable populations.
Highlights.
Four cannabis trajectories were identified reflecting differences in timing of onset and progression
Adolescent onset cannabis trajectory groups were most likely to affiliate with deviant peers, live in disordered neighborhoods and initiate tobacco use early
The adolescent onset chronic trajectory group had the highest rates of opioid misuse even after adjustment for individual, peer and neighborhood factors
Acknowledgments
Funding: This grant was supported by the National Institute of Drug Abuse of the National Institutes of Health under Award Numbers R01DA044184S1 and R01DA032550. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The study sponsor did not have any role in study design; data collection, analysis, or interpretation; writing the report; or the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agar M, & Reisinger HS (2002). A heroin epidemic at the intersection of histories: the 1960s epidemic among African Americans in Baltimore. Med Antrhopol, 21(2), 115–56. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Budney AJ, Lynskey MT (2012). The co-occurring use and misuse of cannabis and tobacco: a review. Addiction, 107(7), 1221–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antognoli E, Koopman GS, Trapl E, Cavallo D, Lim R. Lavanty B, Flocke S. (2018). The social context of adolescent co-use of cigarillos and marijuana in blunts. Subst Use Misuse, 53(4), 654–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, & Barry CL. (2014). Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern Med, 174(10), 1668–1673. doi: 10.1001/jamainternmed.2014.4005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, Abraham A, & Bagwell Adams G (2018). Association Between US State Medical Cannabis Laws and Opioid Prescribing in the Medicare Part D Population. JAMA Intern Med. 178(5), 667–672. doi: 10.1001/jamainternmed.2018.0266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brighthaupt S-C, Schneider K. e, Johnson JK, Jones AA, & Johnson RM. (2019). Trends in Adolescent Heroin and Injection Drug Use in Nine Urban Centers in the U.S., 1999–2017. The Journal of Adolescent Health, 65(2), 210–215. https://doiorg/10.1016/j.jadohealth.2019.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS (2011) Developmental Trajectories of Marijuana Use From Adolescence to Adulthood: Personal Predictors. Archives of Pediatrics & Adolescent Medicine, 165(1), 55. doi: 10.1001/archpediatrics.2010.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Crowley-Matoka M, Phelan S, Dovidio JF, Kerns R, Roth C, Saha S, van Ryn M (2008). Patient race and physicians’ decisions to prescribe opioids for chronic low back pain. Soc Sci Med, 67(11), 1852–60. [DOI] [PubMed] [Google Scholar]
- Cadoni C, Pisanu A, Solinas M, Acquas E, & Di Chiara G (2001). Behavioural sensitization after repeated exposure to Delta 9-tetrahydrocannabinol and cross-sensitization with morphine. Psychopharmacology (Berl), 158(3), 259–266. doi: 10.1007/s002130100875 [DOI] [PubMed] [Google Scholar]
- Cadoni C, Valentini V, & Di Chiara G (2008). Behavioral sensitization to delta 9- tetrahydrocannabinol and cross-sensitization with morphine: Differential changes inaccumbal shell and core dopamine transmission. J Neurochem, 106(4), 1586–1593. doi: 10.1111/j.1471-4159.2008.05503.x [DOI] [PubMed] [Google Scholar]
- Caillé S, & Parsons LH (2006). Cannabinoid modulation of opiate reinforcement through the ventral striatopallidal pathway. Neuropsychopharmacology, 31(4), 804–813. doi: 10.1038/sj.npp.1300848 [DOI] [PubMed] [Google Scholar]
- Capaldi DM, & Patterson GR (1989). Psychometric properties of fourteen latent constructs from the Oregon Youth Study. New York: Springer-Verlag. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2020). Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics; 2020. Available at http://wonder.cdc.gov. [Google Scholar]
- Chen JP, Paredes W, Li J, Smith D, Lowinson J, & Gardner EL (1990). Delta 9- tetrahydrocannabinol produces naloxone-blockable enhancement of presynaptic basal dopamine efflux in nucleus accumbens of conscious, freely-moving rats as measured by intracerebral microdialysis. Psychopharmacology, 102 (2) 156–162. doi: 10.1007/bf02245916 [DOI] [PubMed] [Google Scholar]
- Chihuri S, & Li G (2019). State marijuana laws and opioid overdose mortality. Inj Epidemiol, 6, 38. doi: 10.1186/s40621-019-0213-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Kasper ZA, & Ellis MS (2018). Increased use of heroin as an initiating opioid of abuse: Further considerations and policy implications. Addiction, 87, 267–71. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, & Kasper ZA (2017). Increased use of heroin as an initiating opioid of abuse. Addict Behav, 74, 63–66. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, & Kurtz SP (2014). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry, 71(7), 821–26. [DOI] [PubMed] [Google Scholar]
- Cohn AM, Johnson AL, Rath JM, & Villanti AC. (2016). Patterns of the co-use of alcohol, marijuana and emerging tobacco products in a national sample of young adults. Am J Addict, 25(8), 634–40. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, & Baldwin GT (2016). Relationship between nonmedical prescription opioid use and heroin use. NEJM, 374, 154–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooley-Quille MR, Turner SM, & Beidel DC. (1995). Emotional impact of children’s exposure to community violence: a preliminary study. Journal of the American Academy of Child and Adolescent Psychiatry, 34(10), 1362–1368. doi: 10.1097/00004583-199510000-00022 [DOI] [PubMed] [Google Scholar]
- Corchero J, Fuentes JA, & Manzanares J (1997). delta 9-Tetrahydrocannabinol increases proopiomelanocortin gene expression in the arcuate nucleus of the rat hypothalamus. Eur J Pharmacy, 323 (2–3), 193–195. doi: 10.1016/s0014-2999(97)00144-1 [DOI] [PubMed] [Google Scholar]
- Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, & Green JL(2015). Trends in opioid analgesic abuse and mortality in the United States. NEJM, 372, 241–48. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Chiu WT, Conway K, Dierker L, Glantz M, Kalaydjian A, … Kessler RC. (2009). Does the ‘gateway’ matter? Associations between the order of drug use initiation and the development of drug dependence in the National Comorbidity Study Replication. Psychol Med, 39(1), 157–167. doi: 10.1017/s0033291708003425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, McCord J, & Poulin F (1999). When interventions harm. Peer groups and problem behavior. The American Psychologist, 54(9), 755–764. [DOI] [PubMed] [Google Scholar]
- Ellgren M, Spano SM, & Hurd YL (2007). Adolescent cannabis exposure alters opiate intake and opioid limbic neuronal populations in adult rats. Neuropsychopharmacology, 32(3), 607–615. doi: 10.1038/sj.npp.1301127 [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Martino SC, & Collins RL (2004). Marijuana use from adolescence to young adulthood: multiple developmental trajectories and their associated outcomes. Health Psychol, 23(3), 299–307. doi: 10.1037/0278-6133.23.3.299 [DOI] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, & Ageton SS (1985). Explaining delinquency and drug use: Sage Publications. [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT, & Madden PA (2003). Early reactions to cannabis predict later dependence. Arch Gen Psychiatry, 60(10), 1033–1039. doi: 10.1001/archpsyc.60.10.1033 [DOI] [PubMed] [Google Scholar]
- Fiellin LE, Tetrault JM, Becker WC, Fiellin DA, & Hoff RA (2013). Previous use of alcohol, cigarettes, and marijuana and subsequent abuse of prescription opioids in young adults. J Adolesc Health, 52(2), 158–163. doi: 10.1016/j.jadohealth.2012.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay AK, White HR, Mun EY, Cronley CC, & Lee C (2012). Racial differences in trajectories of heavy drinking and regular marijuana use from ages 13 to 24 among African- American and White males. Drug Alcohol Depend, 121(1–2), 118–123. doi: 10.1016/j.drugalcdep.2011.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flexon JL, Stolzenberg L, & D’Alessio SJ (2019). The effect of cannabis laws on opioid use. Int J Drug Policy, 74, 152–159. doi: 10.1016/j.drugpo.2019.09.013 [DOI] [PubMed] [Google Scholar]
- Garbarino J (1995). Raising children in a socially toxic environment. Jossey-Bass; San Francisco. [Google Scholar]
- Gillespie NA, Bates TC, Hickie IB, Medland SE, Verhulst B, Kirkpatrick RM, … Benotsch EG. (2019). Genetic and environmental risk factors in the non-medical use of over-the-counter or prescribed analgesics, and their relationship to major classes of licit and illicit substance use and misuse in a population-based sample of young adult twins. Addiction. doi: 10.1111/add.14750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorriti MA, Rodriguez de Fonseca F, Navarro M, & Palomo T (1999). Chronic (−)-delta9- tetrahydrocannabinol treatment induces sensitization to the psychomotor effects of amphetamine in rats. Eur J Pharmacol, 365(2–3), 133–142. doi: 10.1016/s0014-2999(98)00851-6 [DOI] [PubMed] [Google Scholar]
- Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Kalauokalani DA, Lasch KE, Myers C, Tait RC, Todd KH, & Vallerand AH (2003). The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med, 4(3), 277–94. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Minino AM, Warner M (2018). Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief, No. 329. Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Human Rights Watch (2009). Decades of Disparity: Drug Arrests and Race in the United States, March 2009, available at https://www.hrw.org/publications?keyword=+drug+arrests&date%5Bvalue%5D%5Bvear%5D=2009 (last visited April 8, 2020).
- Hurd Y, L Michaelides M, Miller ML, & Jutras-Aswad D. (2014). Trajectory of adolescent cannabis use on addiction vulnerability. Neuropharmacology, 76 Pt B(0 0), 416–424. doi: 10.1016/j.neuropharm.2013.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James K and Jordan A, 2018. The opioid crisis in Black communities. J. Law Med. Ethics 46, 404–421. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, & Bachman JG (2000). Monitoring the Future National Survey Results on Drug Use, 1975–1999. Volume I: Secondary School Students. [Google Scholar]
- Juon H-S, Fothergill KE, Green KM, Doherty EE, & Ensminger ME (2011). Antecedents and consequences of marijuana use trajectories over the life course in an African American population. Drug and Alcohol Dependence, 118(2–3), 216–223. doi: 10.1016/j.drugalcdep.2011.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J, & Goodnough A (2017). The opioid crisis is getting worse, particularly for Black Americans. The New York Times. Retrieved from https://www.nytimes.com/interactive/2017/12/22/upshot/opioid-deaths-are-spreading-rapidly-into-black-america.html
- Kelly BC, & Vuolo M (2018). Trajectories of marijuana use and the transition to adulthood. Soc Sci Res, 73, 175–188. doi: 10.1016/j.ssresearch.2018.03.006 [DOI] [PubMed] [Google Scholar]
- Kendler KS, Jacobson KC, Prescott CA, & Neale MC (2003). Specificity genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. The American. Journal of Psychiatry, 160(4), 687–695. doi: 10.1176/appi.ajp.160.4.687 [DOI] [PubMed] [Google Scholar]
- Lamarque S, Taghzouti K, & Simon H (2001). Chronic treatment with Delta(9)- tetrahydrocannabinol enhances the locomotor response to amphetamine and heroin. Implications for vulnerability to drug addiction. Neuropharmacology, 41(1), 118–129. doi: 10.1016/s0028-3908(01)00039-9 [DOI] [PubMed] [Google Scholar]
- Ledent C, Valverde O, Cossu G, Petitet F, Aubert JF, Beslot F, Bohme GA, Imperato A, Pedrazzini T, Roques BP, Vassart G, Fratta W & Parmentier M. (1999). Unresponsiveness to cannabinoids and reduced addictive effect of opiates in CB1 receptor knockout mice. Science, 283(5400), 401–404. doi: 10.1126/science.283.5400.401 [DOI] [PubMed] [Google Scholar]
- Lee JY, Brook JS, Finch SJ, & Brook DW (2018). Trajectories of cannabis use beginning in adolescence associated with symptoms of posttraumatic stress disorder in the midthirties. Subst Abus, 39(1), 39–45. doi: 10.1080/08897077.2017.1363121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemyre A, Poliakova N, Belanger RE (2019). The relationship between tobacco and cannabis use: a review. Subst Use Misuse, 54(1), 130–45. [DOI] [PubMed] [Google Scholar]
- Lippold KM, Jones CM, O’Malley Olsen E, Giroir BP (2019). Racial/ethnic and age group differences in opioid and synthetic opioid-involved overdose deaths among adults aged >= 18 years in metropolitan areas - United States, 2015–2017. MMWR Morb Motral Wkly Rep, 68(43):967–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Quintero C, Pérez de los Cobos J, Hasin DS, Okuda M, Wang S, Grant BF, & Blanco C. (2011). Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug and Alcohol Dependence, 115(1–2), 120–130 doi: 10.1016/j.drugalcdep.2010.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynskey MT, fergusson DM, & Horwood LJ. (1998). The origins of the correlations between tobacco, alcohol, and cannabis use during adolescence. J Child Psychol Psychiatry, 39(7), 995–1005. [PubMed] [Google Scholar]
- Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, Statham DJ, & Martin NG. (2003). Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA, 289(4), 427–433. doi: 10.1001/jama.289.4.427 [DOI] [PubMed] [Google Scholar]
- Manzanares J, Corchero J, Romero J, Fernandez-Ruiz JJ, Ramos JA, & Fuentes JA (1998). Chronic administration of cannabinoids regulates proenkephalin mRNA levels in selected regions of the rat brain. Brain Res Mol Brain Res, 55(1), 126–132. doi: 10.1016/s0169-328x(97)00371-9 [DOI] [PubMed] [Google Scholar]
- Manzanares J, Corchero J, Romero J, Fernandez-Ruiz JJ, Ramos JA, & Fuentes JA (1999). Pharmacological and biochemical interactions between opioids and cannabinoids. Trends Pharmacol Sci, 20(7), 287–294. doi: 10.1016/s0165-6147(99)01339-5 [DOI] [PubMed] [Google Scholar]
- Meghani SH, Byun E, & Gallahger RM (2012). Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med, 13(2), 150–74. [DOI] [PubMed] [Google Scholar]
- Nagin D, & Tremblay RE (1999). Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Dev, 70(5), 1181–1196. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) (2019). Health, United States, 2018 Hyattsville, Maryland. [PubMed]
- Nugent SM, Morasco BJ, O’Neil ME, Freeman M, Low A, Kondo K, Elven C, Zakher B, Motu’apuaka M, Paynter R, & Kansagara D (2017). The Effects Cannabis Among Adults With Chronic Pain and an Overview of General Harms: A Systematic Review. Ann Intern Med, 167(5), 319–331. doi: 10.7326/m17-0155 [DOI] [PubMed] [Google Scholar]
- Olfson M, Wall MM, Liu SM, & Blanco C (2018). Cannabis Use and Risk. of Prescription Opioid Use Disorder in the United States. Am J Psychiatry, 175(1), 47–53. doi: 10.1176/appi.ajp.2017.17040413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer RHC, Young SE, Hopfer CJ, Corley RP, Stallings MC, Crowley TJ, & Hewitt JK (2009). Developmental epidemiology of drug use and abuse in adolescence and young adulthood: Evidence of generalized risk Drug and Alcohol Dependence, 102(1–3), 78–87. doi: 10.1016/j.drugalcdep.2009.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Reid JB, & Dishion TJ (1992) Anitsocial boys (Vol. 4): Castalia Publishing Company. [Google Scholar]
- Reboussin BA, Ialongo NS, Green KM, Furr-Holden DM, Johnson RM, & Milam AJ. (2018). The Impact of the Urban Neighborhood Environment on Marijuana Trajectories During Emerging Adulthood. Prev Sci. doi: 10.1007/s11121-018-0915-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reboussin BA, Milam AJ, Green KM, Ialongo NS, & Furr-Holden CDM (2016). Clustering of Black Adolescent Marijuana Use in Low-Income, Urban Neighborhoods. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 93(1), 109–116. doi: 10.1007/s11524-015-0014-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush S. w., & Earls F (1997). Neighborhoods and violent crime: a multilevel study of collective efficacy. Science (New York, N.Y.), 277(5328), 918–924. [DOI] [PubMed] [Google Scholar]
- Scalco MD, & Colder CR. (2017). Trajectories of marijuana use from late childhood to late adolescence: Can Temperament x Experience interactions discriminate different trajectories of marijuana use? Dev Psychopathol, 29(3), 775–790. doi: 10.1017/s0954579416000468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer GL, Berg C, Kegler MC, Donovan DM, & Windler M. (2015). Assessing the overlap between tobacco and marijuana: trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addictive Behaviors, 49, 26–32. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, Gryczynski J, Mitchell SG, O’Grady KE, Jaffe JH (2015). Heroin use, HIV-risk, and criminal behavior in Baltimore: findings from clinical research. J Addict Dis, 34, 151–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiels MS, Freedman ND, Thomas D, & Berrington de Gonzalez A (2018). Trends in U.S. drug overdose deaths in non-Hispanic Black, Hispanic, and non-Hispanic White Persons, 2000–2015. Annals of Internal Medicine, 168,6,453–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover CL, Davis CS, Gordon SC, & Humphreys K (2019). Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proc Natl Acad Sci U S A, 116(26), 12624–12626. doi: 10.1073/pnas.1903434116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer M, Warner M, Bastian BA, Trinidad JP, Hedegaard H. (2019). Drug overdose deaths involving fentanyl, 2011–2016. National Vital Statistics Reports, 68(3), 1–19. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19–5068, NSDUH Series H-54) Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2020). “2018 National Survey on Drug Use and Health: African Americans.” Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/. [Google Scholar]
- Substance Abuse and Mental Health Services Administration: The Opioid Crisis and the Black/African American Population: An Urgent Issue. Publication No. PEP20–05-02–001. Office of Behavioral Health Equity. Substance Abuse and Mental Health Services Administration, 2020. [Google Scholar]
- Tanda G, Pontieri FE, Frau R, & Di Chiara G (1997). Contribution of blockade of the noradrenaline carrier to the increase of extracellular dopamine in the rat prefrontal cortex by amphetamine and cocaine. Eur J Neurosci, 9(10), 2077–2085. doi: 10.1111/j.1460-9568.1997.tb01375.x [DOI] [PubMed] [Google Scholar]
- Valverde O, Noble F, Beslot F, Daugé V, Fournié-Zaluski MC, & Roques BP (2001). Delta9-tetrahydrocannabinol releases and facilitates the effects of endogenous enkephalins: reduction in morphine withdrawal syndrome without change in rewarding effect. Eur J Neurosci, 13(9), 1816–1824 doi: 10.1046/j.0953-816x.2001.01558.x [DOI] [PubMed] [Google Scholar]
- Wallace JM, & Muroff JR (2002). Preventing substance abuse among African-American children and youth: race differences in risk factor exposure and vulnerability. Journal of Primary Prevention, 22, 235–261. [Google Scholar]
- Wejnert C (2016). Vital signs: trends in HIV diagnoses, risk behaviors, and prevention among persons who inject drugs—United States. MMWR Morbidity and Mortality Weekly Report, 2016, 65. [DOI] [PubMed] [Google Scholar]
- Wen H, & Hockenberry JM (2018). Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA Intern Med, 178(5), 673–679. doi: 10.1001/jamainternmed.2018.1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, & Cummings JR (2015). The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. Journal of Health economics 42, 64–80. doi: 10.1016/j.jhealeco.2015.03.007 [DOI] [PubMed] [Google Scholar]
- Wiese B, & Wilson-Poe AR (2018). Emerging Evidence for Cannabis’ Role in Opioid Use Disorder. Cannabis Cannabinoid Res, 3(1), 179–189. doi: 10.1089/can.2018.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Wagner FA, & Anthony JC (2002). Exposure opportunity as a mechanism linking youth marijuana use to hallucinogen use. Drug and Alcohol Dependence, 66(2), 127–135. doi: 10.1016/s0376-8716(01)00191-0 [DOI] [PubMed] [Google Scholar]
- Wilson N, Kariisa M, Seth P, Smith IV H, & Davis NL (2020). Drug and opioid-involved overdose deaths − United States, 2017–2018. MMWR Morb Mortal Wkly Rep; 69:290–297. doi: 10.15585/mmwr.mm6911a4externalicon [DOI] [PMC free article] [PubMed] [Google Scholar]