ABSTRACT
This research investigates the extent to which financial incentives (conditional cash transfers) would induce Americans to opt for vaccination against coronavirus disease of 2019. We performed a randomized survey experiment with a representative sample of 1000 American adults in December 2020. Respondents were asked whether they would opt for vaccination under one of three incentive conditions ($1000, $1500, or $2000 financial incentive) or a no-incentive condition. We find that—without coupled financial incentives—only 58 per cent of survey respondents would elect for vaccination. A coupled financial incentive yields an 8-percentage-point increase in vaccine uptake relative to this baseline. The size of the cash transfer does not dramatically affect uptake rates. However, incentive responses differ dramatically by demographic group. Republicans were less responsive to financial incentives than the general population. For Black and Latino Americans especially, very large financial incentives may be counter-productive.
I. INTRODUCTION
After the coronavirus disease of 2019 (COVID-19) vaccines were first authorized in the USA for emergency use in the winter of 2020–2021, there was more demand than supply. Yet by spring 2021, long before reaching herd immunity, supply began to exceed demand in some areas.1 Polls suggest that ~35 per cent of Americans may resist vaccination,2 and similar levels of hesitancy are seen in Ireland and the UK.3 Even among those prioritized to receive vaccines, such as healthcare workers, widespread hesitancy to accept the vaccine has been reported.4 Such hesitancy can be a constraint on achieving herd immunity, which for COVID-19 has been estimated to require 70 per cent or more of the population to be vaccinated.5 And the sooner the better—the delay in achieving herd immunity creates more opportunities for the virus to mutate into more resistant versions.
There are several possible explanations for vaccine hesitancy. Some persons have private information about their risk–benefit profiles (eg a medical contraindication) or hold erroneous beliefs about safety, efficacy, or background risk.6 Other causes include psychological biases, such as regret aversion, where people avoid vaccination to avoid the feeling of regret about their vaccination decision should they experience an adverse event.7 Regret aversion is the strongest when people make active choices for which they feel responsible, like taking the vaccine, rather than passive choices for which they feel other people or nature are responsible, like merely being exposed to the virus.8
Vaccine hesitancy can also vary with demographic attributes. For instance, black Americans have reasons to distrust the US healthcare and medical research systems, given a history of exclusion and exploitation.9 For different reasons, Republicans reportedly distrust public health experts.10 As of this article’s publication date, the available vaccines are not Food and Drug Administration (FDA) approved but rather authorized under Emergency Use Authorization (EUA). Research has found that, ‘concern about rushed development of the vaccine [is a] significant predictor[] of lower willingness to get a COVID-19 vaccine under EUA’.11 Some Americans may rationally adopt a ‘wait-and-learn’ approach.12
There are several policy mechanisms available to increase vaccine uptake. On one extreme, the Supreme Court has affirmed the constitutionality of a vaccine mandate in a classic case involving an adult who refused.13 In recent history, vaccination policy has primarily relied on state mandates for school-age children, with various exemptions and exemption procedures.14 Some healthcare employers have also mandated flu vaccinations for workers.15 In contrast to this emphasis on children and healthcare workers, the current pandemic requires broad vaccination of adults. Although governments arguably have legal power to mandate a COVID-19 vaccine, with or without religious or personal belief exemptions, such a move may be unethical or politically infeasible, especially prior to full FDA licensure of the vaccine products.16
To encourage vaccination uptake while respecting choice, policymakers and economists have proposed that governments should offer financial incentives—conditional cash transfers—with one prominent proposal recommending $1500 per person.17 Likewise, several businesses have reportedly begun to pay their employees to get vaccinated.18 In April 2021, one US state announced that they would begin giving $100 savings bonds to adults under the age of 35 who get vaccinated (including retroactive payments for those already vaccinated).19
This paper investigates the extent to which coupled financial incentives (conditional cash transfers) would induce Americans to opt for vaccination against COVID-19.
Economic theory and experience predict that financial incentives would increase vaccine uptake by lowering the effective price, thus increasing the quantity demanded (ie the Law of Demand).20 A similar economic logic in reverse justifies the use of taxes on alcohol and cigarettes to improve public health and the use of copays and deductibles to curb low-value healthcare consumption.21 These financial disincentives decrease the perceived personal benefits of a behavior on net, and thus discourage it. Prior work has found that incentives work in a range of health contexts, from home-based health monitoring for diabetics22 and warfarin adherence23 to physical activity24 and smoking cessation.25
Nevertheless, human behavior is not always as simple as implied by traditional economic models. Violations of these models have been long reported by researchers from psychology and behavioral economics. Indeed, leading behavioral scientists have recently suggested that paying financial incentives for COVID-19 vaccinations may not only be ineffectual, but could actually backfire by reducing overall vaccine uptake.26 As Volpp, Loewenstein, and Buttenheim (2021) argue, ‘considerable research shows that payments in some contexts can send the signal that an action is undesirable, unpleasant, or even dangerous and not worth taking based purely on personal benefit. Financial incentives are likely to discourage vaccination (particularly among those most concerned about adverse effects)’.27
Incentives could be ineffectual or backfire for multiple reasons. First, when people are motivated to get the vaccine for intrinsic motivations, like being a good citizen and contributing to the public good, an extrinsic motivation, like a cash payment, may ‘crowd-out’ the intrinsic motivations.28 The motive to be a good person may actually be stronger than the motive to earn a few bucks, and the two motives may not comfortably co-exist in a given context, like vaccination. Second, people may see the choice to accept a vaccine (putting a foreign body in their own bodies) as a ‘sacred value’ that is unaffected by monetary incentives.29 This concern relates to a broader problem of ‘commodification’, and whether everything can and should be priced.30
Third, and perhaps most importantly, a payment could signal that the vaccine is extra risky, a concern which has been observed when paying human subjects to participate in research studies.31 If high prices on products signal high quality to consumers, then a high payment being offered to consume a product (a negative price) may signal larger-than-expected risks.
Similar debates have played out in other public health contexts, such as the effect of paying for blood donations, where ethical theorists and lab data suggested that incentives may backfire and actually reduce donation rates.32 Nonetheless, when rigorous field studies were eventually completed, they consistently found that large positive effects of incentives on organ donation behavior.33 The perceived risks of vaccination (and of not vaccinating) may be quite different than for blood donation or other domains where incentives have been tested.
There is no empirical research that speaks directly to the question of whether incentives for a COVID-19 vaccine would be effective, but there has been research on the effects of incentives for other vaccines. A 2014 systematic review of four studies of financial incentives for parents to promote pediatric vaccinations concluded that there was insufficient evidence to determine effectiveness.34 On the other hand, a 2019 review of interventions to encourage Hepatitis B vaccination among substance users included three randomized controlled trials testing monetary rewards, and concluded that they were the most effective interventions.35 Likewise, in a randomized field trial of human papillomavirus (HPV) vaccines in England among 17–18 year old girls, researchers found that paying the USD $73 equivalent nearly doubled the rate of uptake (22 per cent versus 12 per cent).36 Several field experiments in developing countries have found substantial effects as well. For example, a tetanus vaccination campaign in Nigeria randomized women to receive either the equivalent of US $0.03, or $2, or $5.33 as conditional cash payments for vaccination. The higher payments caused dramatically higher uptake (55%, 76%, and 86%, respectively).37
II. METHODOLOGY
To assess the potential effectiveness of offering financial incentives for COVID-19 vaccination, we performed a randomized survey experiment in December 2020 with a sample of 1000 American adults (provided by Qualtrics, Provo, UT), stratified to be representative of US households in terms of age, gender, income, and education. Qualtrics uses an opt-in panel (thus not allowing calculation of a response rate) and selects respondents to fill quotas based on national demographics. As part of their proprietary methods, Qualtrics compensates respondents for their participation. We secure informed consent on the survey platform. The survey and the associated protocols were approved by the IRB at the University of Delaware.
We apply multivariate regression analysis to survey responses to shed light on three questions:
Would couple financial incentives (conditional cash transfers) induce Americans to opt for vaccination against COVID-19?
Does the size of the conditional cash transfer affect the level of uptake?
Do conditional cash transfers encourage uptake among the most hesitant demographic groups?
II.A. Survey Instrument
Survey respondents viewed, with equal probability, one of three incentive (ie treatment) conditions or a no-incentive (ie control) condition. In the no-incentive condition, we asked, ‘Suppose a vaccine, which has been shown to be 95 per cent effective at preventing COVID-19 infections, has been authorized for emergency use by the US Food and Drug Administration. If that vaccine was made available to you tomorrow at no cost, would you elect to receive the vaccine?’ In the incentive conditions, in between those two sentences, we added: ‘Further, suppose that the Federal Government is providing a one-time stimulus payment of [INCENTIVE] to persons who elect to receive the vaccine’, where the financial incentive amount was set to either $1000, $1500, or $2000. These values were chosen to bracket the $1500 value made in a prominent proposal.38 The between-subjects design insured that the respondents in the control condition were blinded to the purpose of the study, and thereby provide a baseline representing the status quo of no-incentive.
Respondents could answer ‘yes’, ‘no’, or ‘unsure’. Demographic information was collected alongside the experimental questions.
II.B. Statistical Analysis
Based on the responses to our experimental survey, we estimate a series of multi-variate regression models. For each of these regressions, our dependent variable Vaccinei is constructed as a binary outcome, where, for a given respondent i, the outcome is equal to one if the respondent chose to receive the vaccine, and equal to zero if the respondent declined or indicated they were unsure whether they would receive the vaccine.
1. Financial Incentives and Vaccine Uptake
To assess the extent to which coupled financial incentives (conditional cash transfers) induce Americans to opt for vaccination against COVID-19, we estimate the following model:
 |
(1) |
where variable Vaccine is as defined above. Our variable of interest (denoted  ) is a binary variable, which distinguishes between our treatment and control groups. The variable takes value one if the respondent viewed one of the financial incentive (ie treatment) conditions. The variable takes value zero if the respondent viewed the no-incentive (ie control) condition. The coefficient on INCENTIVE (
) is a binary variable, which distinguishes between our treatment and control groups. The variable takes value one if the respondent viewed one of the financial incentive (ie treatment) conditions. The variable takes value zero if the respondent viewed the no-incentive (ie control) condition. The coefficient on INCENTIVE ( ) measures the responsiveness of individuals to financial incentives to vaccination. Matrix
) measures the responsiveness of individuals to financial incentives to vaccination. Matrix  includes a series of indicator (dummy) variables to control for the demographic identity of the respondent, including age, stated gender, household income, education level, ethnicity, and preferred political party.
includes a series of indicator (dummy) variables to control for the demographic identity of the respondent, including age, stated gender, household income, education level, ethnicity, and preferred political party.
We assess the robustness of our model by re-estimating using a probit specification. We also estimate the average treatment effects (ATE) of financial incentives using two types of ‘matching’ models: nearest-neighbor matching39 and propensity score matching.40 As a further robustness check, the model in Equation (1) relies on an indicator specification of our dependent variable in which a ‘yes’ response is equal to one and a ‘no’ or ‘unsure’ response is coded as a zero. However, financial incentives could also push people into the ‘unsure’ category. To investigate this issue, we also consider a multinomial logit specification, where outcomes are defined alternatively as ‘no’, ‘unsure’, and ‘yes’.
Vaccine Uptake and the Size of Financial Incentives
It is possible, of course, that different sizes of conditional payments may induce higher (or lower) levels of uptake among respondents. This dose–response relationship is important to measure, given that a marginal change in the financial incentive can dramatically affect the cost of a mass incentive scheme. To assess the sensitivity of uptake response to different sizes of financial incentive, we re-estimate Equation (1) disaggregated variable  into three incentive sub-categories:
into three incentive sub-categories:  ,
,  , and
, and  . These sub-categories take value one for the specific incentive viewed by the respondent and are otherwise equal to zero. We formally test whether the size of the financial incentive affects vaccine uptake response by comparing model performance for an unconstrained model, in which incentive response is allowed to differ across incentive sub-categories, versus a model in which incentive responses are constrained to be identical across the incentive sub-categories.41
. These sub-categories take value one for the specific incentive viewed by the respondent and are otherwise equal to zero. We formally test whether the size of the financial incentive affects vaccine uptake response by comparing model performance for an unconstrained model, in which incentive response is allowed to differ across incentive sub-categories, versus a model in which incentive responses are constrained to be identical across the incentive sub-categories.41
Financial Incentives and Sensitive Demographic Groups
Finally, even if vaccine incentives are successful among the general population, certain demographic groups may be unresponsive or may respond differently to incentives than the population at large. Particularly sensitive in this respect are Black Americans, who have historically been more mistrustful of vaccination, and some segments of the Republican party, who have been reluctant to engage in government-mandated public health measures, including social distancing and mask-wearing. We compare the incentive response for these two sensitive demographic groups versus those for the broader population.
II.C. Summary Statistics
Full data, including demographics, are posted at the Open Science Framework at https://osf.io/n9qra/. Summary statistics are reported in Table 1. In the no-incentive condition, which can be interpreted as the base rate, 58 per cent of respondents said ‘yes’ they were willing to take the vaccine, 24 per cent said they were ‘unsure’, and 18 per cent said ‘no’. These rates are similar to those found in other national surveys.42 As in prior polls, we found that Democrats were the most likely to indicate willingness to take the vaccine, with a 20-percentage-point increase over the base rate. Women were 11 percentage points less likely and Black Americans were 10 percentage points less likely to take the vaccine overall, again reflecting known trends.
Table 1.
Summary statistics
| Variable | Portion of sample |
|---|---|
| Overall vaccine uptake | 0.64 |
| Incentive scenario | |
| No incentive | 0.24 |
| Incentive | 0.76 |
| $1000 Incentive | 0.25 |
| $1500 Incentive | 0.25 |
| $2000 Incentive | 0.26 |
| Age | |
| 18 to 29 | 0.39 |
| 30 to 49 | 0.23 |
| 50 to 64 | 0.17 |
| ≥65 | 0.21 |
| Gender | |
| Male | 0.50 |
| Female | 0.49 |
| Household income | |
| $0 to $29,000 | 0.28 |
| $30,000 to $59,000 | 0.22 |
| $60,000 to $149,999 | 0.40 |
| $150,000 or more | 0.10 |
| Education level | |
| Less than high school | 0.04 |
| High school/GED | 0.24 |
| Some college (no degree) | 0.24 |
| Associates degree | 0.11 |
| Bachelor’s degree | 0.23 |
| Graduate/professional degree | 0.14 |
| Ethnicity | |
| White | 0.78 |
| Black | 0.14 |
| Asian | 0.04 |
| Latino | 0.08 |
| Other | 0.05 |
| Political affiliation | |
| Republican | 0.29 |
| Democrat | 0.36 |
| Independent | 0.26 |
III. RESULTS
Table 2 reports our main results. Column (1) shows the impacts of financial incentives on vaccine uptake as estimated via ordinary least squares (OLS; ie Equation 1). Column (2) shows the results of Probit estimation, where reported coefficients are marginal effects. Columns (3) and (4), respectively, show the estimated average treatment effects (ATEs) obtained via nearest-neighbor matching43 and propensity score matching.44
Table 2.
Impacts of financial incentives on vaccine uptake
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Variables | OLS | Probit | NNMatch | PSMatch |
| Incentive | 0.0769** | 0.0788** | 0.0823** | 0.0709** |
| (0.0343) | (0.0327) | (0.0361) | (0.0341) | |
| Age | ||||
| 30 to 49 | −0.0827** | −0.0744* | ||
| (0.0403) | (0.0389) | |||
| 50 to 64 | −0.0764* | −0.0711* | ||
| (0.0463) | (0.0193) | |||
| ≥65 | 0.0168 | 0.0193 | ||
| (0.0425) | (0.0436) | |||
| Female | −0.1124*** | −0.1106*** | ||
| (0.0316) | (0.0301) | |||
| Household income | ||||
| $30,000 to $59,999 | −0.0505 | −0.0518 | ||
| (0.0445) | (0.0403) | |||
| $60,000 to $149,999 | 0.0451 | 0.0403 | ||
| (0.0414) | (0.0394) | |||
| $150,000 or more | 0.0813 | 0.0828 | ||
| (0.0585) | (0.0626) | |||
| Education level | ||||
| High school/GED | −0.0524 | −0.0508 | ||
| (0.0849) | (0.0776) | |||
| Some college (no degree) | −0.0089 | −0.0104 | ||
| (0.0861) | (0.0792) | |||
| Associate degree | −0.0099 | −0.0118 | ||
| (0.0917) | (0.0851) | |||
| Bachelor’s degree | 0.0508 | 0.0494 | ||
| (0.0865) | (0.0809) | |||
| Graduate/professional degree | 0.1393 | 0.1526* | ||
| (0.0890) | (0.0880) | |||
| Ethnicity | ||||
| Black | −0.1057** | −0.1041** | ||
| (0.0465) | (0.0427) | |||
| Asian | 0.1216* | 0.1236 | ||
| (0.0664) | (0.0773) | |||
| Latino | 0.0126 | 0.0091 | ||
| (0.0576) | (0.0552) | |||
| Other (non-White) | 0.1438** | 0.0091** | ||
| (0.0676) | (0.0750) | |||
| Political party | ||||
| Republican | 0.0442 | 0.0378 | ||
| (0.0634) | (0.0569) | |||
| Democrat | 0.2005*** | 0.1979*** | ||
| (0.0609) | (0.05515) | |||
| Independent | 0.0518 | 0.0448 | ||
| (0.0637) | (0.0570) | |||
| Observations | 1000 | 1000 | 1000 | 1000 |
Notes: Robust standard errors in parentheses; *** p < 0.01, ** p < 0.05, * p < 0.1.
Referring to our variable of interest in Table 2, we see that coupled incentives increase estimated vaccination rates by 7–8 percentage points. The magnitude of this response is consistent across Columns (1) through (4), and in each specification, the response is statistically significant at the 95 per cent level. Recall from Section 2.3 that average uptake among respondents in the no-incentive (ie control) group was 58 per cent. Thus, coupled incentives would bring US vaccination levels to more than 65 per cent—substantially closer to the rates that experts say are needed to reach herd immunity. Figure 1(a) reports the results of the multinomial estimation with respect to our outcomes of interest. The results depicted here are the marginal effects evaluated at the unconditional mean of the sample. As shown in Figure 1, offering any incentive yielded an 8-percentage-point increase (statistically significant at the 95% level) in vaccine uptake (‘yes’, compared to the base condition, when controlling for demographics. It also resulted in a 6-percentage-point decrease (statistically significant at the 95% level) in those responding ‘no’ and a smaller, nonsignificant decrease in those ‘unsure’. The softening of complete opposition may be important in coming months, as individuals gain more information about the safety of the vaccine and taking the vaccine becomes a social norm.
Figure 1.
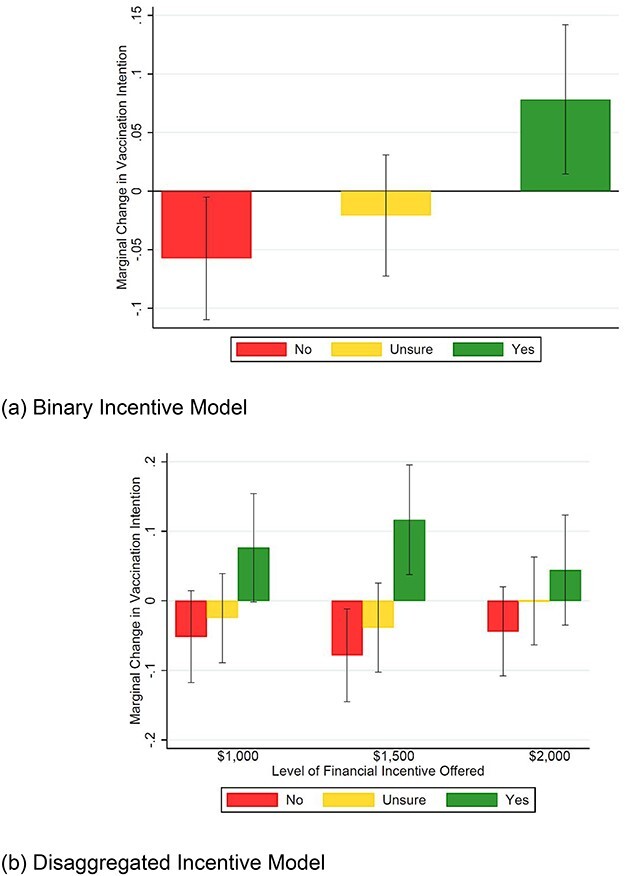
Multinomial logit model of vaccine uptake. Note: Figure reports the results of the multinomial estimation with respect to our outcomes of interest. Estimates are the marginal effects evaluated at the unconditional mean of the sample. Panel (a) of the Figure reports results for the model in which all incentive values are aggregated into a binary ‘incentive’ versus ‘no incentive’ condition. Panel (b) shows results for the model in which the different incentive values are disaggregated.
Does the size of the financial incentive matter in increasing uptake? Table 3 reports results of the analysis in which responses to financial incentives are dis-aggregated by payment size. Column (1) of the Table reports results of the specification in which all incentives are constrained to elicit an identical response. Column (2) reports estimates for the unconstrained model.
Table 3.
Vaccine uptake and the size of financial incentives
| (1) | (2) | ||
|---|---|---|---|
| Variables | Constrained | Unconstrained | |
| $1000 Incentive | 0.0769** | 0.0761* | |
| (0.0343) | (0.0411) | ||
| $1500 Incentive | 0.0769** | 0.1174*** | |
| (0.0343) | (0.0414) | ||
| $2000 Incentive | 0.0769** | 0.0399 | |
| (0.0343) | (0.0424) | ||
| Age | |||
| 30 to 49 | −0.0827** | −0.0804** | |
| (0.0403) | (0.0402) | ||
| 50 to 64 | −0.764* | −0.0763 | |
| (0.0463) | (0.0466) | ||
| ≥65 | 0.0168 | 0.0160 | |
| (0.0425) | (0.0424) | ||
| Female | −0.1124*** | −0.1141*** | |
| (0.0316) | (0.0317) | ||
| Household income | |||
| $30,000 to $59,999 | −0.0505 | −0.0564 | |
| (0.0445) | (0.0445) | ||
| $60,000 to $149,999 | 0.0451 | 0.0420 | |
| (0.0414) | (0.0414) | ||
| $150,000 or more | 0.0813 | 0.0819 | |
| (0.0585) | (0.0585) | ||
| Education level | |||
| High school/GED | −0.0524 | −0.0473 | |
| (0.0849) | (0.0850) | ||
| Some college (no degree) | −0.0089 | −0.0086 | |
| (0.0861) | (0.0858) | ||
| Associates degree | −0.0099 | −0.0065 | |
| (0.0917) | (0.0915) | ||
| Bachelor’s degree | 0.0508 | 0.0551 | |
| (0.0865) | (0.0864) | ||
| Graduate/professional degree | 0.1393 | 0.1422 | |
| (0.0890) | (0.0887) | ||
| Ethnicity | |||
| Black | −0.1057** | −0.1043** | |
| (0.0465) | (0.0462) | ||
| Asian | 0.1216* | 0.1291* | |
| (0.0664) | (0.0663) | ||
| Latino | 0.0126 | 0.0122 | |
| (0.0576) | (0.0573) | ||
| Other (non-White) | 0.1438** | 0.1523** | |
| (0.0676) | (0.0669) | ||
| Political party | |||
| Republican | 0.0442 | 0.0477 | |
| (0.0634) | (0.0638) | ||
| Democrat | 0.2005*** | 0.2015*** | |
| (0.0609) | (0.0611) | ||
| Independent | 0.0518 | 0.0538 | |
| (0.0637) | (0.0639) | ||
| AIC | 1294.134 | 1294.480 | |
| BIC | 1397.197 | 1407.359 | |
| Observations | 1000 | 1000 |
Notes: Robust standard errors in parentheses; *** p < 0.01, ** p < 0.05, * p < 0.1.
Note that, by design, incentive response estimates in Column (1) of Table 3 are identical to those reported in Column (1) of Table 2. Under this specification, each of the three incentive payment levels induce a 7.7-percentage-point increase in vaccine uptake (statistically significant at the 95% confidence level). In the unconstrained model in Column (2) of Table 3, the $1000 incentive generates a similar, 7.6-percentage-point increase in uptake (statistically significant at the 90% level). The point estimate for the $1500 incentive elicits an 11.7-percentage-point increase in uptake and is statistically significant at the 99 per cent confidence level. The estimated response to the $2000 incentive is positive (4.1 percentage points) but statistically insignificant at conventional levels. These patterns could be the result of low statistical power, or it could be that higher levels of payment reduce demand for the vaccine compared to the lower incentive amounts.
To determine whether the constrained model or the unconstrained model is preferable for the purposes of economic inference, we compare the AIC and BIC between the two models. As shown in Table 3, the constrained model—in which all incentive levels elicit an identical response—generates lower AIC and BIC scores than the unconstrained model, suggesting the constrained model is preferable. Moreover, using a post-estimation Wald test on the unconstrained model, we also fail to reject the hypothesis that the incentives elicit an identical response. In other words, we do not observe any meaningful difference in the effectiveness of incentives among the three payment levels. We caution that the results of this analysis hold only for the range of incentives we have tested here. Obviously, outcomes may diverge for dramatically higher or lower incentive levels.
Figure 1(b) above shows results for the multinomial logit model for which the different incentive values are disaggregated. These results are consistent with our indicator specification in Table 3. We fail to reject the hypothesis that the incentive response is identical across the different payments when we run the model disaggregating the three incentive conditions.
Figure 2 compares the incentive responses for various demographic groups, including race/ethnicity, income, and political identities. While it bears emphasis that our statistical power is limited within subgroups, The average responses differ dramatically by demographic group. For Black Americans, 53 per cent (±17%) of respondents in the no-incentive (control) indicated they would choose to receive the vaccine. At lower levels of financial incentive ($1000 and $1500), Black respondents appear highly responsive. The $1500 incentive increased vaccine uptake among Black respondents to 68 per cent (±16%). This is a substantially higher response than the sample average, and approaches the estimated threshold needed to achieve herd immunity. However, for the $2000 incentive, uptake among Black respondents falls dramatically to 39 per cent (±15%). This is 13.6 percentage points below vaccination rates among the control group. We see a similar trend for Latino respondents, and indeed every racial/ethnic group has a non-linear trend on the size of the incentive.
Figure 2.
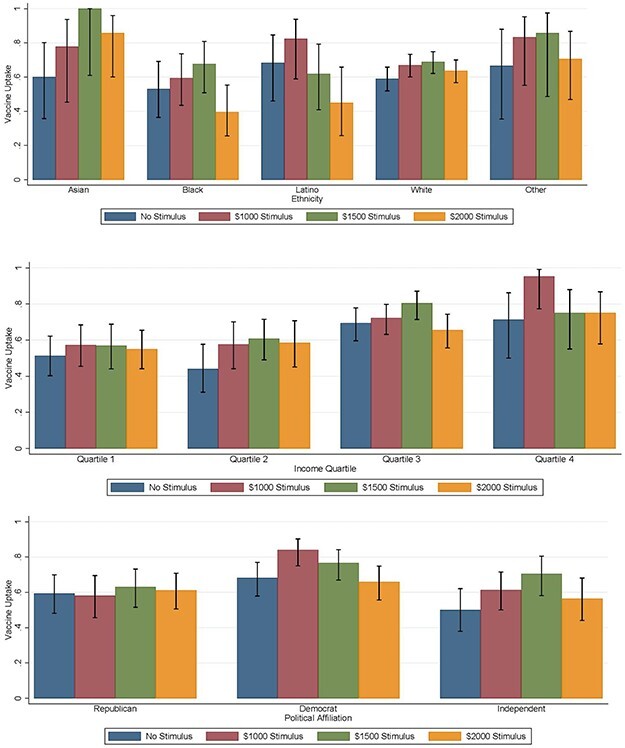
Financial incentives and demographic groups (with 95% CI). Note: Income quartiles are (1) < $30,000, (2) $30,000 to $59,999, (3) $60,000 to $149,999, and (4) $150,000 or more.
For income, we see generally lower incomes associated with lower vaccine uptake. The middle-income groups appear most responsive to the incentive. One might hypothesize that the lowest-income respondents would have the greatest response to the incentive, perhaps overriding their autonomous choices about whether to get the vaccine. That hypothesis is not supported by the patterns in the estimated effects by income group.
Republicans were less responsive to financial incentives than the general population. Referring to Figure 2, 59 per cent (±11%) of Republican respondents in the no-incentive group. Only 58 per cent (±12%) of those who viewed the $1000 incentive indicated they would elect for vaccination. Similarly, 63 per cent (±11%) and 61 per cent (±10%) of respondents, respectively, elected for vaccination under the $1500 and $2000 conditions. Interestingly, although independents showed the lowest vaccine uptake at baseline, they showed the most substantial response to the financial incentives. Democrats were both more receptive to the vaccine at baseline and were also responsive to the financial incentive. Again, across these groups, the $2000 incentive appears to be unhelpful compared to the more moderate sized incentives. We emphasize again that statistical power is limited for all these subgroup analyses.
IV. DISCUSSION AND CONCLUSION
Widespread hesitance toward COVID-19 vaccines has the potential to create a gap between the actual vaccination rate and the rate needed to achieve herd immunity. This research investigates the extent to which coupled financial incentives (conditional cash transfers) would help bridge this gap. We find that financial incentives between $1000 and $2000 to receive the vaccine yields an 8-percentage-point increase in uptake relative to baseline. The size of the cash transfer in this range does not dramatically affect uptake rates. However, incentive responses differ dramatically by demographic group. Republicans were less responsive to financial incentives than the general population. For Black and Latino Americans especially, very large financial incentives appear to be counter-productive.
We caution that, as an online survey experiment, our study has limitations. Our sample was constructed to be representative of the USA adult population on certain demographics, but excludes adults outside the USA. Even within the USA the sample may exclude some populations, such as those lacking internet access.
We measured self-reported vaccine intentions at one point in time, not actual behaviors in the future. We expect the overall willingness to take the vaccine to change over time, but the marginal effects of incentive may remain more constant.
Survey responses are subject to biases, including social desirability, but the anonymous between-subject design helps. And, it is not clear that such biases would interact with and confound our manipulations.
We tested a relatively large range of incentives, but further research could explore lower or higher payments, as well as explore framing effects and baseline effects.45 People may respond differently to receiving a conditional cash transfer (as in our experiment) or refundable tax credit for getting vaccinated versus a fine or civil penalty for not getting vaccinated, even if the economic impact is the same. Another frame is the mere compensation for the time and inconvenience of getting the vaccine (reducing hassle costs to net zero), which some employers are reportedly using.46
Although we examined demographic covariates, our sample was limited to explore subgroup effects. We also did not measure other attitudes or beliefs, which could moderate the observed outcomes. Our study cannot say whether the offer of payment changes beliefs about the vaccine’s safety or efficacy, for example.
Increasing vaccination rates through incentives faces implementation challenges. For example, policy designers will have to decide whether to pay those who have medical vaccine contraindications and whether to retroactively pay those who were vaccinated prior to the incentive being announced, two actions that may make the policy more politically popular but could reduce the marginal effectiveness of the incentive in changing behavior. Moreover, in the USA, the current mechanism to confirm vaccination, a paper card provided by the US Centers for Disease Control, is not robust against fraud. A digital passport would be valuable for many purposes beyond financial incentives, including conditional mandates (eg around workplaces and airline travel).47 In any initiative to increase vaccination rates, it is also important that all Americans have fair access to the vaccine. Thus incentives should track intended behaviors (vaccination) rather than structural inequities (such as disparate access to the vaccine).
We have not calculated the cost-effectiveness of vaccine incentives, and thus cannot say whether it would be a ‘prudent investment’, a point that some commentators have called into doubt.48 If the US government implemented the vaccine incentive as part of a broader stimulus plan, by simply making some payment that it would otherwise make (or a tax relief that it would otherwise provide) conditional on getting the vaccine, then the budgetary impact could be zero or actually negative (if some people still decline the vaccine-plus-incentive). Still, those who decline to be vaccinated could be helped in other ways, to minimize the welfare losses associated with the pandemic and to compensate for other pro-social behaviors.49
Our purpose is not to provide a full-throated ethical and policy defense, or even a comprehensive analysis, of incentives for COVID-19 vaccination. Yet, we can address some normative concerns that have been raised in the literature (and by reviewers).
Some have argued that financial incentives for vaccination would be ‘paternalistic’.50 Dworkin defines that term as ‘the interference of a state or an individual with another person, against their will, and defended or motivated by a claim that the person interfered with will be better off or protected from harm’.51 The concept seems inapposite for vaccine incentives for at least two reasons. First, an offer of money to persons is not an ‘interference … against their will’ – they are free to take it or leave it. Still, without waging into a semantic debate, one might call incentives a form of ‘asymmetric’ or ‘soft’ paternalism, depending on the giver’s motivation.52 Regardless of the label, incentives respect individual choices. Indeed, our data are inconsistent with the claim that incentives would ‘reinforce paternalism towards racial minorities and economically disadvantaged individuals’. In our data, approximately half of individuals indicated that they would exercise their will to decline the vaccine (Figure 2).
Further, the primary purpose of encouraging vaccination is not to promote the welfare of the individual recipient, like say a motorcycle helmet law. The goal is to provide a public good—population-level herd immunity.53 Putting the point differently, being unvaccinated is the textbook example of imposing a negative externality risk of infection on other persons.54 One could imagine tort law trying to internalize the costs of precaution by imposing liability, but in practice it would be infeasible for dead plaintiffs to sue, it would be hard to show specific causation, and many potential defendants are judgment-proof and uninsured for these liabilities. Thus, a prospective regulatory or incentives-based approach is more sensible.
More generally, one might worry that large payments would be irresistible (an ‘undue influence’ or ‘unjust inducement’) to those of limited means, making it nearly impossible for them to form autonomous choices about vaccination.55 This concern is also sometimes inaptly called ‘coercion’ by bioethicists.56 Our data do not support these concerns. If money functioned like a light attracting unthinking moths at night, then one might expect the largest money offers to induce the greatest response, and for the ultimate uptake to approach 100 per cent. Those expectations are not supported by our data. Instead, respondents appear to be capable of weighing other factors autonomously.
Moreover, this concern about money being irresistible would seem to be of greatest concern for those of lowest income, but we do not observe greater response to the incentive for this group (Figure 2). On the other hand, this lack of uptake suggests that, if implemented in the real world, the incentives may be disproportionately paid to higher-earning people who are more likely to opt for the vaccine, making the transfers regressive overall. Nonetheless, even lower-income respondents benefit from herd immunity. If they value being non-vaccinated more than the cash payment, but nonetheless enjoy the herd immunity results in their communities, then they may be best off overall. This same analysis may suggest that a vaccine mandate would be disproportionately coercive on lower-income people who have stronger preferences against vaccination.
Nonetheless, in a world of scarcity with a weak social safety net, people are often called upon to make difficult choices, using their bodies to perform dangerous jobs, for example. Desperation is arguably best addressed by building a stronger safety net, rather than canceling compensation for pro-social behaviors.
Ultimately, our data suggest that financial incentives should be on the table for policymakers. They can be used in conjunction with optimal distribution logistics to ensure that the vaccine reaches all the people who want it and optimal messaging to dispel misinformation and to maximize desire for the vaccine. Before incentives larger than $1500 are implemented, further research should explore whether there is in fact a non-linear dose–response effect, as suggested by our data. Other approaches should be explored for Republicans altogether. In sum, a well-tailored incentive may help boost vaccination uptake to levels needed to reach herd-immunity.
Footnotes
See eg Courtney Ann Jackson, COVID-19 Vaccine Demand Slowing in Mississippi, WLBT 2021, https://www.wlbt.com/2021/04/26/covid-vaccine-demand-slowing-mississippi/; Jeff Keeling, Bianca Marais, Vaccine Uptake plummets in Northeast Tennessee as Supply Far Outstrips Demand, WJHL, 2021, https://www.wjhl.com/local-coronavirus-coverage/vaccine-uptake-plummets-in-northeast-tennessee-as-supply-far-outstrips-demand/.
Gallup. US Readiness to Get COVID-19 Vaccine Steadies at 65%. Gallup.com, 2021.
Jamie Murphy, Frédérique Vallières, Richard P. Bentall, Mark Shevlin, Orla McBride, Todd K. Hartman, Ryan McKay, Kate Bennett, Liam Mason, Jilly Gibson-Miller, et al. Psychological Characteristics Associated with Covid-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. 12 Nat. Commun. 1–15 (2021).
Kin On Kwok, Kin-Kit Li, Wan In Wei, Arthur Tang, Samuel Yeung Shan Wong, and Shui Shan Lee. Influenza Vaccine Uptake, Covid-19 Vaccination Intention and Vaccine Hesitancy Among nurses: A survey. 114 Int. J. Nurs. Stud. 103854 (2021).
A. David Paltiel, Jason L. Schwartz, Amy Zheng, and Rochelle P. Walensky. Clinical Outcomes of a Covid-19 Vaccine: Implementation over Efficacy: Study Examines How Definitions and Thresholds of Vaccine Efficacy, Coupled with Different Levels of Implementation Effectiveness and Background Epidemic Severity, Translate into Outcomes. 40 Health Aff. 42–52 (2021).
Wändi Bruine de Bruin and Daniel Bennett. Relationships between Initial Covid-19 Risk Perceptions and Protective Health Behaviors: A National Survey. 59 Am. J. Prev. Med. 157–167 (2020).
Katrina F. Brown, J. Simon Kroll, Michael J. Hudson, Mary Ramsay, John Green, Charles A. Vincent, Graham Fraser, and Nick Sevdalis. Omission Bias and Vaccine Rejection by Parents of Healthy Children: Implications for the Influenza a/h1n1 Vaccination Programme. 28 Vaccine 4181–4185 (2010).
Id.
Gamble V.N. A Legacy of Distrust: African Americans and Medical Research. 9 Am. J. Prev. Med. (6 Suppl) 35–38 (1993, Nov–Dec). Fairchild A.L., Bayer R. Uses and Abuses of Tuskegee, 284 Science. 919–921 (1999 May 7). Shavers Vickie L., Lynch Charles F., Burmeister Leon F. Racial Differences in Factors that Influence the Willingness to Participate in Medical Research Studies. 12 Ann. Epidemiol. 248–256 (2002 May).
Frankovic K. COVID-19 Vaccine Rejectors Do Not Trust Healthcare Experts – But They Do Trust Trump | YouGov. https://today.yougov.com/ Web site. https://today.yougov.com/topics/politics/articles-reports/2021/03/30/who-vaccine-rejectors-dont-trust. Updated 2021 (accessed Apr. 13, 2021).
Guidry, Jeanine P.D., Linnea I. Laestadius, Emily K. Vraga, Carrie A. Miller, Paul B. Perrin, Candace W. Burton, Mark Ryan, Bernard F. Fuemmeler, and Kellie E. Carlyle. Willingness to Get the COVID-19 Vaccine With and Without Emergency Use Authorization, 49 Am. J. Infect. Control 137–142 (2021).
Daniel A. Salmon, et al., COVID-19 Vaccination Attitudes, Values and Intentions among United States Adults Prior to Emergency Use Authorization, 39 Vaccine 2698–2711 (2021).
Jacobson v. Massachusetts, 197 U.S. 11 (1905).
Neal D. Goldstein, Joanna S. Suder, and Jonathan Purtle. Trends and Characteristics of Proposed and Enacted State Legislation on Childhood Vaccination Exemption, 2011–2017, 109 Am. Public Health 102–107 (2019).
Samantha I. Pitts, et al., A Systematic Review of Mandatory Influenza Vaccination in Healthcare Personnel, 47 Am. J. Prev. Med. 330, 336 (2014), http://vaccinesafetyresource.elsevier.com/ sites/default/files/Flu-Pitts-Systematic.pdf (http://perma.cc/89RF-SGLQ) (accessed Jul. 15, 2021).
Dorit R. Reiss and Arthur L. Caplan. Considerations in Mandating a New Covid-19 Vaccine in the USA For Children and Adults, 7 J. Law Biosci. 1–9 (2020); Michelle M. Mello, Ross D. Silverman, and Saad B. Omer. Ensuring Uptake of Vaccines Against Sars-Cov-2, 384 N. Engl. J. Med. 1296–1299 (2020).
John Delaney. Pay Americans to Take a Coronavirus Vaccine. Washington Post, 2020, https://www.washingtonpost.com/opinions/2020/11/23/pay-americans-coronavirus-vaccine-john-delaney/. Robert Litan, Want Her Immunity? Pay People to Take the Vaccine, Brookings, Aug. 18, 2020 available at https://www.brookings.edu/opinions/want-herd-immunity-pay-people-to-take-the-vaccine/ (accessed Jul. 15, 2021). Julian Savulescu, Good Reasons to Vaccinate: Mandatory or Payment for Risk? 47 J. Med. Ethics, 78–85 (2021).
Claire Miller. Trader Joe’s, Dollar General, and Others Are Paying Workers to Get Vaccines. NPR, 2021.
Katie Lobosco and Kelsie Smith, West Virginia Giving People under 35 $100 Savings Bonds for Getting Vaccinated, CNN 2021, https://www.cnn.com/2021/04/26/politics/west-virginia-savings-bonds-vaccinated/index.htm.
Christopher T. Robertson, K. Aleks Schaefer, Daniel Scheitrum, Sergio Puig, and Keith Joiner. Indemnifying Precaution: Economic Insights for Regulation of a Highly Infectious Disease, 7 J. Law Biosci., lsaa032 (2020).
Alexandra Wright, Katherine E. Smith, and Mark Hellowell. Policy Lessons from Health Taxes: A Systematic Review of Empirical Studies, 17 BMC Public Health, 1–14 (2017); Christopher T. Robertson. Exposed: Why Our Health Insurance Is Incomplete and What Can Be Done About It (2019) Harvard University Press.
Sen, Aditi P., Taylor B. Sewell, E. Brooks Riley, Beth Stearman, Scarlett L. Bellamy, Michelle F. Hu, Yuanyuan Tao et al. Financial Incentives for Home-Based Health Monitoring: A Randomized Controlled Trial. 29 J. Gener. Internal. Med., 770–777 (2014).
Stephen Kimmel, et al. Randomized Trial of Lottery-Based Incentives to Improve Warfarin Adherence, 164 Am. Heart J., 268–274 (2012).
Mitesh Patel, et al. A Randomized, Controlled Trial of Lottery-Based Financial Incentives to Increase Physical Activity Among Overweight and Obese Adults, 32 Am. J. Health Promot, 1568–1575 (2018).
Volpp, Kevin G., Andrea B. Troxel, Mark V. Pauly, Henry A. Glick, Andrea Puig, David A. Asch, Robert Galvin et al. A Randomized, Controlled Trial of Financial Incentives for Smoking Cessation, 360 N. Engl. J. Med. 699–709 (2009).
Kevin G. Volpp, George Loewenstein, and Alison M. Buttenheim. Behaviorally Informed Strategies for a National Covid-19 Vaccine Promotion Program, 325 JAMA 125–126 (2021); Tappin, David, Linda Bauld, David Purves, Kathleen Boyd, Lesley Sinclair, Susan MacAskill, Jennifer McKell et al. Financial Incentives for Smoking Cessation in Pregnancy: Randomised Controlled Trial, 350 Bmj 1–12 (2015).
Id.
Kristen Underhill. When Extrinsic Incentives Displace Intrinsic Motivation: Designing Legal Carrots and Sticks to Confront the Challenge of Motivational Crowding-Out, 33 Yale J. Reg., 213 (2016).
Julio J. Elias, Nicola Lacetera, and Mario Macis. Sacred Values? The Effect of Information on Attitudes toward Payments for Human Organs. 105 Am. Econ. Rev., 361–65 (2015).
I Glenn Cohen. The Price of Everything, the Value of Nothing: Reframing the Commodification Debate. 117 Harvard Law Rev., 689 (2003).
Cynthia E. Cryder, Alex John London, Kevin G. Volpp, and George Loewenstein. Informative Inducement: Study Payment as a Signal of Risk. 70 Soc. Sci. Med., 455–464 (2010).
See generally, Pablo Rodriguez del Pozo, Paying Donors and the Ethics of Blood Supply, 20 J. Med. Ethics, 31–35 (1994).
Nicola Lacetera, Mario Macis, and Robert Slonim. Economic Rewards to Motivate Blood Donations. 340 Science 927–928 (2013).
Sarah Wigham, Laura Ternent, Andrew Bryant, Shannon Robalino, Falko F. Sniehotta, and Hean Adams. Parental Financial Incentives for Increasing Preschool Vaccination Uptake: Systematic Review, 134 Pediatrics, e1117–e1128 (2014).
Stacy Tressler and Ruchi Bhandari. Interventions to Increase Completion of Hepatitis B Vaccination in People Who Inject Drugs: A Systematic Review and Meta-Analysis. 6 In Open Forum of Infectious Diseases (Oxford University Press, US) (page ofz521, 2019).
Eleni Mantzari, Florian Vogt, and Theresa M. Marteau. Financial Incentives for Increasing Uptake of HPV Vaccinations: A Randomized Controlled Trial, 32 Health Psychol., 160 (2015).
Sato, R., and Fintan, B. Effect of Cash Incentives on Tetanus Toxoid Vaccination Among Rural Nigerian Women: A Randomized Controlled Trial. 16 Hum. Vaccines Immunother., 1181–1188 (2020).
See, supra, Delaney (2020) at note 9.
Alberto Abadie and Guido W. Imbens. Large Sample Properties of Matching Estimators for Average Treatment Effects, 74 Econometrica, 235–267 (2006); Alberto Abadie and Guido W. Imbens. Bias-Corrected Matching Estimators for Average Treatment Effects, 29 J. Bus. Econ. Stat., 1–11 (2011).
Alberto Abadie and Guido W, Imbens. Matching on the Estimated Propensity Score. 84 Econometrica, 781–807 (2016).
Comparison of the constrained and unconstrained models is based on the Akaike information criterion (AIC) and the Bayesian information criterion (BIC), where smaller levels of the information criteria indicate better model performance.
See, eg Gallup (2021) at note 2; Murphy et al. (2021) at note 3.
See, supra, note 25.
See, supra, note 26.
Ivo Vlaev, Dominic King, Ara Darzi, and Paul Dolan. Changing Health Behaviors Using Financial Incentives: A Review from Behavioral Economics, 19 BMC Pub Health, 1–9 (2019).
See, supra, Miller (2021) at note 10.
Alexandra L. Phelan. Covid-19 Immunity Passports and Vaccination Certificates: Scientific, Equitable, and Legal Challenges. 395 The Lancet, 1595–1598 (2020); Christopher T. Robertson. Vaccines and Airline Travel: a Federal Role to Protect the Public Health, 42 Am. J. Law Med., 543–571 (2016).
Emily A. Largent and Franklin G. Miller, Problems with Paying People to be Vaccinated against COVID-19, 325 JAMA 534–535 (2021); Ana Santos Rutschman and Timothy L. Wiemken, The Case Against Monetary Behavioral Incentives in the Context of COVID-19 Vaccination, 27 Harvard Public Health Rev, (2020), https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3830769.
See, supra, Robertson et al. (2020) at note 11.
Rutschman and Wiemken supra note 47.
Gerald Dworkin, Paternalism, in The Stanford Encyclopedia of Philosophy (Edward N. Zalta, ed., Fall 2020 Edition), https://plato.stanford.edu/archives/fall2020/entries/paternalism/.
See George Loewenstein, Troyen Brennan, and Kevin G. Volpp. Asymmetric paternalism to improve health behaviors. 298 Jama 2415–2417 (2007) (‘the guiding principle of asymmetric paternalism is that institutions and incentives should be structured and aligned in such a way to maximize the likelihood that individuals will engage in behaviors that are beneficial, making those who would otherwise engage in unhealthy behaviors better off without adverse consequences to other’).
Jonny Anomaly, Public Health and Public Goods. 4 Public Health Ethics, 251–259 (2011).
Joseph Stiglitz, Economics of The Public Sector, (p. 120, 1988)(“One of the methods by which the incidence of some diseases is reduced is through vaccination. Those who are vaccinated incur some cost (discomfort, time, money, and risk of getting the disease from a bad batch of the vaccine). They receive some private benefit through a reduced risk of getting the disease, but a major part of the benefit is public, the reduced incidence of the disease in the community from which all benefit. In many cases the private costs exceed the private benefits, but the social benefits—including a reduced incidence of the disease—far exceed the costs. Because of the free rider problem, governments frequently require that individuals become vaccinated.’)
See Scott D. Halpern, Jason H.T. Karlawish, David Casarett, Jesse A. Berlin, and David A. Asch. “Empirical Assessment of Whether Moderate Payments are Undue or Unjust Inducements for Participation in Clinical Trials, 164 Arch. Internal Med., 801–803 (2004).
Joseph Millum and Michael Garnett. How Payment for Research Participation Can Be Coercive, 19 Am. J. Bioethics, 21–31 (2019); Wertheimer A., Miller F.G. Payment for Research Participation: A Coercive Offer? 34 J. Med. Ethics 389–392 (2008). doi:10.1136/jme.2007.021857; Emily A. Largent and Holly Fernandez Lynch. Paying Research Participants: Regulatory Uncertainty, Conceptual Confusion, and a Path Forward. 17 Yale J. Health Policy, Law Ethics, 61 (2017).