Abstract
OBJECTIVE:
Transthoracic echocardiography (TTE) is important in the management of critically ill patients, yet it has not been incorporated into many residency programs’ curricula. Our objective is to determine if trainees undergoing a 60-minute training session on TTE have improved knowledge, ultrasound skills, and increases the utilization of TTE during their rotation in the intensive care unit (ICU). We will also compare the results of participants with prior TTE exposure to TTE-naïve trainees. Our hypothesis is that after the training, participants’ will have improved knowledge and ultrasound skills compared to before training. Our secondary hypotheses are that TTE-naïve trainees will have greater improvements in knowledge scores compared to those who have had prior TTE experience and trainees will increase their use of TTE in the ICU.
DESIGN:
Single-center, prospective trial.
SETTING:
Brigham and Women’s Hospital (academic hospital).
PARTICIPANTS:
Residents and fellows rotating through the ICU, at any level of postgraduate training.
RESULTS:
Forty-two trainees participated in the study. Statistically significant improvement after training was observed for all multiple choice questions (MCQ) and practical assessments (p < 0.001). When assessing the differences in score improvement between TTE-experienced versus TTE-naïve users, mean score improvements were notably higher for TTE-naïve participants (MCQ: 28.2 ± 11.6; echo clinical: 48.6 ± 23.4) compared to TTE-experienced users (MCQ: 18.6 ± 13.5, p = 0.01; echo clinical: 38.3 ± 30.2, p = 0.04).
CONCLUSIONS:
A short didactic presentation on TTE use may be useful in teaching ICU trainees basic TTE skills and encouraging the use of bedside TTE in the ICU.
Keywords: transthoracic echocardiography, education, intensive care unit
INTRODUCTION
Bedside transthoracic echocardiography (TTE) is an easy and noninvasive tool which is useful in evaluating intensive care unit (ICU) patients.1 It may be used to assess volume status and predict fluid responsiveness by measuring the inferior vena cava (IVC) diameter and respirophasic changes (caval index),1–3 determine the cause of hemodynamic failure, and distinguish between different shock states.4–6 Early echocardiography-guided therapy in shock is associated with improved survival, decreased rates of acute kidney injury, more days free of renal replacement therapy, less fluid administration, and increased inotrope use.7 TTE can be used to assist in making diagnoses and optimizing ICU patient management.8–12 However, TTE training is not universally incorporated in all residency or critical care training programs. TTE training is incorporated into all U.S. emergency medicine residency programs and is tested on their board examinations. It is unknown what percentage of surgical residency and critical care programs integrate bedside TTE education into their curriculum. Recent surveys demonstrated only 27.5% of anesthesiology residency programs had some form of ultrasound education,13 and only 46% anesthesiology critical care fellowships had a dedicated ultrasound curriculum.14 There is a need to incorporate ultrasound education into residency and ICU training programs. Previous studies have demonstrated that it is possible to teach personnel, who have no prior echocardiography experience, to perform and accurately interpret TTE cardiac views and fluid status.2,15 Ultrasound use in the ICU may be taught in a time-efficient manner through a concise curriculum.16
Although previous studies have examined TTE training and curricula in training programs, one of the most common barriers to implementing TTE education is time. Few studies have evaluated the impact of a brief training tutorial on TTE education. We have reviewed the literature and summarized studies comparing various course durations and assessment of trainee skills which can be found in Supplemental Table 1. Our goal was to assess the effect of a short didactic training session on trainees’ TTE skills and knowledge. We hypothesized that after basic TTE training, participants would improve their TTE knowledge and skills, as demonstrated by an increase in their scores on posttraining multiple choice questions (MCQs) and practical TTE examinations. Our secondary hypothesis was that trainees who never used TTE before (TTE-naïve group), would have a greater degree of improvement in knowledge and TTE skills after training, compared to trainees who had previous TTE experience. Furthermore, we believed that after the training, participants would utilize TTE more during their ICU rotation to guide patient management.
MATERIALS AND METHODS
This study was approved by the Brigham and Women’s Hospital Institutional Review Board (protocol # 2016P000171). The authors followed the appropriate EQUATOR guidelines.
This was a prospective, single-center, observational study redateg the effect of a 60-minute TTE didactic and hands-on session on TTE knowledge and skills of ICU trainees. We further compared the results of participants with no prior TTE education (n = 17), to those with prior TTE experience (n = 14). Consent was inferred when participants completed a pretraining survey. They were evaluated on their general TTE knowledge and clinical TTE examination performance on an ICU patient before and after a teaching session on TTE.
The target sample size for study participants was ≥20; this number was decided upon based on similar studies performed in the past.2,15,17–20 No a priori sample size calculation was performed. Inclusion criteria included ICU residents and fellows, at any level of training (i.e., postgraduate year-1 [PGY-1] and above), in any sub-specialty training program (i.e., surgery, emergency medicine, anesthesiology, pulmonary critical care, etc.). Medical students were excluded due to a short rotation course (i.e., 2-week ICU rotation) and difficulty scheduling posttraining test. Participants with previous echocardiography experience were included. Only trainees rotating through the thoracic, burn/trauma, and surgical ICUs were asked to participate in the study; participation was voluntary. Forty-two residents and fellows were enrolled in the study.
Participants completed a pretraining survey assessing their prior TTE experience and knowledge at the beginning of their ICU rotation. They also completed an 18-question multiple-choice test on TTE views, anatomy, and interpretation (Appendix A). Participants also performed a pretraining practical TTE examination (Appendix B) on an ICU patient who required a bedside ultrasound as part of routine care. The clinical TTE examination was only performed on those ICU patients who would have required a TTE on that day by an ICU team member regardless of the study; patients in whom a TTE evaluation was not clinically indicated were not considered for TTE examination by a trainee. Patient written consent was not required, and their consent to the TTE examination by a trainee was verbally obtained from the patient or their family. Patient information was not collected, nor were their images stored, to maintain anonymity. The practical TTE examination was graded by 1 of the 3 authors (C.M.K., M.T.H., M.S.E.), who were experienced sonographers who received TTE training, but were not certified.
Skills tested in the practical examination are shown in Appendix C. Participants had to show the subxiphoid IVC, parasternal long axis, and apical 4 chamber views; they had 2 minutes to demonstrate each view. This time restriction was chosen because it was previously used in a similar study.3 The instructors subjectively determined the adequacy and quality of the image window. Participants were not allowed to ask the instructor questions, and were not given guidance on how to obtain the specific views. The practical test score ranged from 0 to 35 points. After the pretraining practical examination, the instructors reviewed the examination with them and performed a 30-minute TTE tutorial. All participants performed the TTE examination using a Sonosite M-Turbo ultrasound machine with a P21, 1 to 5 mHz phased-array cardiac transducer (Sonosite Inc., Bothell, WA).
Additionally, all the participants were given a 30-minute PowerPoint lecture on TTE use and knowledge (including Focused Assessed Transthoracic Echocardiography [FATE] protocol views).21 The training was provided by one of the 3 authors. Participants were encouraged to use TTE at least once daily; this could have been done unsupervised or under the supervision of the ICU fellow or attending. At least 1 week after training, the trainees were asked to perform a post-training practical TTE examination on an ICU patient, a MCQ test, and a posttraining survey. The practical TTE and MCQ tests asked the same questions as the pretest but were arranged in a different order.
Statistical Analysis
Summary statistics on pretraining and posttraining survey responses are represented as N (%). Normality of the MCQ and practical TTE examination score outcomes were assessed graphically and by Kolmogorov-Smirnov tests.22 MCQ test and clinical TTE examination score outcomes are expressed as mean ± standard deviation, whereas the practical TTE examination time outcomes are expressed as median inter-quartile range. Paired t-tests and Wilcoxon signed rank tests were utilized as appropriate to compare participants’ test scores before and after the training intervention.22
Since participants with and without prior TTE experience were not expected to be equivalent on pretraining scores, a second analysis was performed using analysis of covariance. Differences in improvement scores were tested between participants with and without prior exposure to TTE, controlling for pretraining scores to adjust for differences in baseline. Differences in improvement scores for TTE exposure groups by pretraining scores were tested by including an interaction term in the model. Improvement scores were computed as post – pre for the MCQ and clinical TTE examination and pre – post for the practical TTE examination in order to represent improvement as positive values. Since the time-to outcomes (time to show IVC subxiphoid view, measure IVC diameter, show parasternal long axis view, and show apical 4 chamber) were not normally distributed, log-transformed values were calculated and tested for normality. However, since log-transformed values continued to be nonnormal, a rank-based analysis of covariance was utilized for these time-to outcomes.23 If participants were unable to complete a task during the practical examination, the maximum time allotted for the task (120 sec) was assigned to prevent bias due to non-ignorable missing data. The significance level was set to 0.05. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
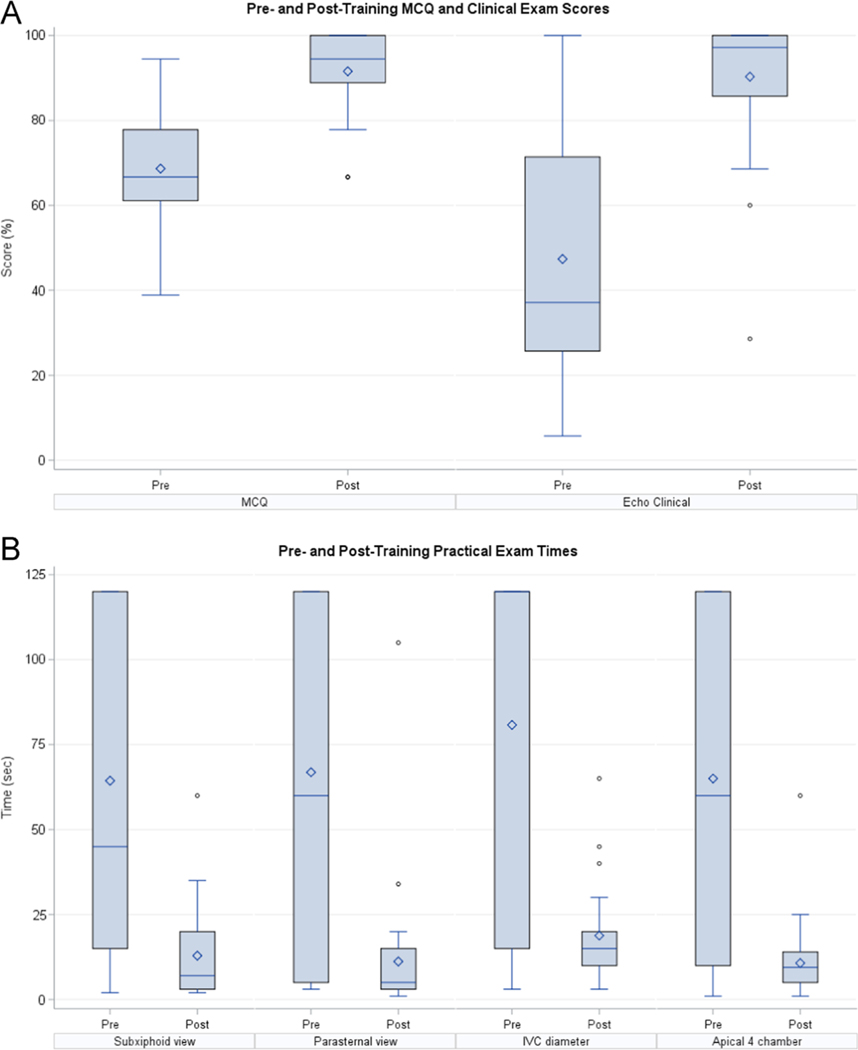
In total, 42 participants were enrolled in the study, of which, 31 participants (18 residents and 13 fellows) completed the study in its entirety. The median postgraduate training years of the participants was PGY-3. Table 1 summarizes the presurvey responses. The mean time between training and posttraining assessment was 3 weeks. Statistically significant improvement after training was observed for all MCQ and practical TTE assessments (p < 0.001) (Table 2). The mean improvement for the MCQ and the TTE practical were 22.9% and 42.9%, respectively (Fig. 1A and B). Time to show each TTE view improved by 30, 85, 56, and 55 seconds for time to show IVC subxiphoid view, measure IVC diameter, show parasternal long axis view, and show apical 4 chamber, respectively (Fig. 2A and B).
TABLE 1.
Pretraining Survey Responses
| Question | Number of Respondents N (%) |
|---|---|
| Training | |
| Resident | 18(58.1%) |
| Fellow | 13(41.9%) |
| Specialty | |
| Anesthesia | 19(61.3%) |
| Surgery | 7(22.6%) |
| EM | 2(6.5%) |
| Pulmonary | 2(6.5%) |
| OB/GYN | 1(2.3%) |
| Prior use of TTE to assess fluid status? | |
| Yes | 17(54.8%) |
| No | 14(45.2%) |
| What do you use to assess fluid status? | |
| Ultrasound | 17(22.1%) |
| CVP | 16(20.8%) |
| SVV | 22(28.6%) |
| PLR | 14(18.2%) |
| UOP | 3(3.9%) |
| Physical examination | 3(3.9%) |
| BUN/CR ratio | 2(2.6%) |
| Do you have a dedicated TTE curriculum in your residency training? | |
| Yes | 6(19.4%) |
| No | 25(80.7%) |
| What isyourPGYlevel? | |
| 1 | 2(6.5%) |
| 2 | 9(29.0%) |
| 3 | 5(16.1%) |
| 4 | 3(9.9%) |
| 5 | 9(29.0%) |
| 6 | 2(6.5%) |
| 12 | 1(3.2%) |
BUN/Cr, blood urea nitrogen/creatinine; CVP, central venous pressure; EM, emergency medicine; OB/GYN, obstetrics/gynecology; PLR, passive leg raise; SVV, stroke volume variation; UOP, urine output.
TABLE 2.
Pretraining and Posttraining Transthoracic Echocardiography (TTE) Practical and Multiple Choice Question (MCQ) Examination Results
| Test | Pretraining | Posttraining | Improvement | p Value |
|---|---|---|---|---|
| MCQ | 68.6 ± 14.4% | 91.6 ± 9.2% | 22.9 ± 13.4% | <0.001 |
| TTE examination | ||||
| Clinical | 47.4 ± 30.2% | 90.3 ± 15.9% | 42.9 ± 27.4% | <0.001 |
| Time to show IVC subxiphoid view | 45(15–120)sec | 7(3–20)sec | 30(2–110)sec | <0.001 |
| Time to measure IVC diameter* | 120 (15–120)sec | 15(10–20)sec | 85(5–105)sec | <0.001 |
| Time to show parasternal long axis view* | 60 (5–120)sec | 5(3–15)sec | 56(1–115)sec | <0.001 |
| Time to show apical 4 chamber* | 60 (10–120)sec | 9.5(5–14)sec | 55(2–110)sec | <0.001 |
Data presented as mean ± standard deviation (SD) for multiple choice question (MCQ) tests and median interquartile range (IQR) for practical transthoracic echocardiography (TTE) times.
N = 30 due to missing predata and postdata for 1 participant.
FIGURE 1.
(A) Pretraining and posttraining multiple choice question and clinical ultrasound exam scores. (B) Pretraining and posttraining practical ultrasound examination times to show views.
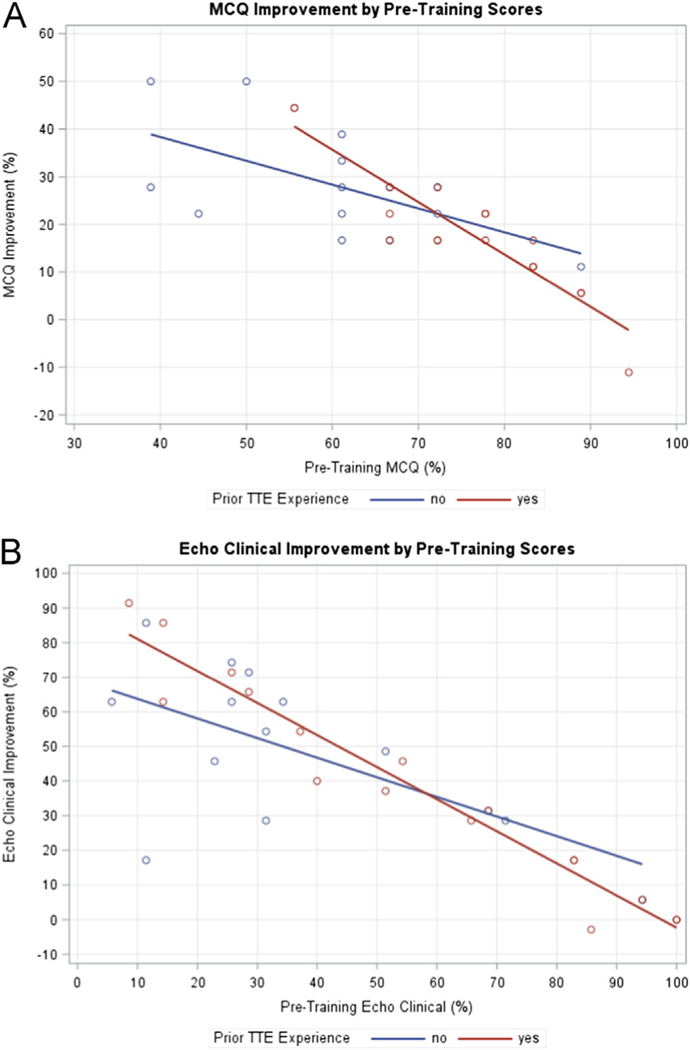
FIGURE 2.
(A) MCQ improvements by pretraining scores. (B) Echo clinical improvement by pretraining scores.
Further analysis was performed to assess the differences in improvement scores by participants’ prior TTE experience. In the presurvey, 17 participants reported prior TTE experience, whereas 14 did not. Mean improvement scores were notably higher for TTE-naïve participants (MCQ: 28.2 ± 11.6; echo clinical: 48.6 ± 23.4) compared to TTE-experienced participants (MCQ: 18.6 ± 13.5; echo clinical: 38.3 ± 30.2), and these differences were statistically significant after adjusting for differences in pretraining scores (MCQ: p = 0.01; echo clinical: p = 0.04). Compared to those without TTE experience, participants with TTE experience who scored poorly on their pretest demonstrated a greater mean improvement in their MCQ scores while those already starting out with a high pretraining MCQ score did not display as much improvement (interaction p = 0.02; Fig. 2A). A similar trend was observed for the clinical examination, but difference did not reach statistical significance (interaction p = 0.07; Fig. 2B).
For the TTE practical, mean improvements in the time to perform the required task was greater for the TTE-naïve group compared to the TTE-experienced group. However, after adjusting for differences in pretraining times, these differences were not statistically significant. No evidence of differences in mean improvement scores by TTE experience and pretraining times were noted for these outcomes (Table 3).
TABLE 3.
Pretraining and Posttraining Practical and Multiple Choice Question (MCQ) Examination Results by Prior Transthoracic Echocardiography (TTE) Experience
| No Prior TTE Experience | Prior TTE Experience | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Test | Pretraining | Posttraining | Improvement | Pretraining | Posttraining | Improvement | p Value |
| MCQ | 60.3 ± 13.8 | 88.5 ± 11.6 | 28.2 ± 11.6 | 75.5 ± 11.1 | 94.1 ± 5.7 | 18.6 ± 13.5 | 0.01* |
| TTE Examination | |||||||
| Clinical | 36.7 ± 25.7 | 85.3 ± 21.5 | 48.6 ± 23.4 | 56.1 ± 31.6 | 94.5 ± 7.8 | 38.3 ± 30.2 | 0.04* |
| Time to show IVC subxiphoid view | 85 (15–120) | 12.5 (5–20) | 55.5 (13–105) | 45 (6–120) | 5 (3–15) | 30 (1–110) | 0.14† |
| Time to measure IVC diameter | 120 (60-120) | 20 (10-30) | 90 (50-100) | 120 (15-120) | 15 (10-15) | 75 (0-105) | 0.58† |
| Time to show parasternal long axis view | 120 (60–120 | 10 (3–15) | 109 (45–116) | 10 (4–120) | 4 (3–5) | 7 (1–100) | 0.84† |
| Time to show apical 4 chamber | 75 (10–120) | 10(3–13) | 75 (7–107) | 60 (10–120) | 5 (5–14) | 50 (2–110) | 0.96† |
Data presented as mean ± standard deviation (SD) for multiple choice question (MCQ) tests and median interquartile range (IQR) for practical transthoracic echocardiography (TTE) times.
p values for the effect of prior TTE experience obtained by ANCOVA on improvement scores.
p values for the effect of prior TTE experience obtained by rank-based ANCOVA on improvement scores.
One outlier was noted for the TTE practical-time to show parasternal long axis view; this particular participant had a significantly longer time to show this view on their posttraining skills test compared to their pretraining time. The longer time was attributed to the body habitus and underlying pathology of the patient being examined on the posttraining test; obtaining views on this patient were challenging. Likely, the patient scanned for the pretest had a more ideal body habitus. A sensitivity analysis was conducted by re-running the models without the outlier. The change in time from pretraining to posttraining retained its significance (from Table 2) and the effect of the prior TTE experience on time improvement remained insignificant (from Table 3). Thus, we conclude that the outlier did not influence the models statistics.
All the participants reported an increase in TTE use after the training but before the last practical TTE examination; most (61%) reported that they used it 1 to 5 times after they received the training (Table 4). Twenty-two participants (71%) found the training to be very helpful, and 24 (77.4%) stated they were very likely to use TTE in the future. Results of the posttraining survey are reported in Table 5.
TABLE 4.
TTE Use Pretraining and Posttraining
| Question | Number of Respondents N (%) |
|---|---|
| Times used TTE for fluid assessment in past year(from pretraining survey) | |
| 0 | 13 (41.9%) |
| 1 to 5 | 7 (22.6%) |
| 6 to 10 | 4 (12.9%) |
| 11 to 19 | 2 (6.5%) |
| >20 | 5 (16.1%) |
| Times used TTE for fluid assessment after training (from posttraining survey) | |
| 0 | 0 |
| 1 to 5 | 19 (61.3%) |
| 6 to 10 | 8 (25.8%) |
| 11 to 19 | 2 (6.5%) |
| >20 | 2 (6.5%) |
TABLE 5.
Posttraining Survey Responses
| Question | Number of Respondents N (%) |
|---|---|
| Did performing TTE impact patient management? | |
| Yes | 28 (90.3%) |
| No | 2 (6.5%) |
| No response | 1 (3.2%) |
| Any barriers to performing TTE? | |
| Yes | 9 (29.0%) |
| No | 22 (71.0%) |
| No response | 0 |
| Any barriers to fluid management? | |
| Yes | 2 (6.5%) |
| No | 28 (90.3%) |
| No response | 1 (3.2%) |
| How helpful was the training*? | |
| 1 | 2 (6.5%) |
| 2 | 7 (22.6%) |
| 3 | 22 (71.0%) |
| After training, how likely are you to use TTE†? | |
| 1 | 0 |
| 2 | 7 (22.6%) |
| 3 | 24 (77.4%) |
| After training, what is your comfort level performing and | |
| interpreting TTE‡? | |
| 1 | 1 (3.2%) |
| 2 | 22 (71.0%) |
| 3 | 8 (25.8%) |
1—Not helpful, 2—Somewhat helpful, and 3—Very helpful.
0—Does not apply to my field, 1—Unlikely, 2—Somewhat likely, and 3—Very likely.
1—Poor, 2—Somewhat comfortable, and 3—Very comfortable.
DISCUSSION
This study demonstrates that a short ultrasound didactic session and tutorial may be helpful in teaching TTE to ICU trainees, as participants had a significant improvement on their MCQ and clinical TTE tests, and increased TTE use in the ICU. The training helped participants correctly identify structures and assess patient fluid status to guide fluid management using TTE. Furthermore, TTE-naïve participants had statistically significant greater improvements on their test scores as compared to TTE-experienced trainees. However, the improvement in the times to show each specific TTE view was similar for both groups. This suggests a short education session may be helpful in teaching TTE-naïve trainees basic TTE skills to a level where their skill set is comparable to a group with more TTE experience. This cannot, however, be interpreted as TTE skill proficiency.
Similarly, previous studies demonstrated that TTE imaging and interpretation are easy to teach to trainees with minimal training.24 Rebel et al. evaluated the TTE skills of 30 anesthesiology residents after they received education through a 15-minute video-based instruction session. They performed various TTE examinations in 6 different objective structured clinical examination stations. Although there was no structured training for abdominal ultrasound, over 67% of participants correctly identified and interpreted the IVC diameter respirophasic changes.24 Studies evaluating short training point-of-care ultrasound (PoCUS) curricula (ranging from 45 min to 3 h), found it improved image acquisition skills, interpretation of findings, and knowledge of trainees.2,25,26 One study demonstrated that a training course improved TTE skills and knowledge to the same degree regardless of professional training background and experience level with critical care ultrasound.27 Although the improvement in knowledge and TTE skills of trainees after short training sessions are promising, further studies are warranted to determine if shorter-length curricula are as effective as longer curricula programs, and if they result in long-term skill and knowledge retention and TTE proficiency. Furthermore, the effectiveness of the type of educational modality used in ultrasound training merits further investigation.
Although several medical societies recommend trainees should achieve competency in critical care ultrasound, there are numerous barriers to ultrasound education, including a deficient amount of time for training.14 Our results suggest that ultrasound education might be accomplished in a short amount of time, resulting in an improvement in trainee knowledge and echocardiography skills. Our subjective findings were that the course encouraged trainees to use ultrasound, improved their ability to correctly identify structures, and encouraged trainees to use ultrasound appropriately to assess fluid status to help guide fluid management. Considering the challenges of didactic instructors,’ model volunteers,’ and trainees’ busy schedules, a short training lecture and hands-on tutorial may be an effective method to teach ultrasonography to trainees. Our results do not suggest that our trainees were proficient in basic TTE after the short training course; future studies evaluating TTE proficiency are required. Furthermore, additional studies evaluating how ultrasound training impacts patient management and outcomes may also be beneficial.
Study advantages included using real ICU patients to perform the ultrasonography practical tests allowed participants to experience the challenges and non-idealized circumstances often encountered when performing bedside ultrasound in the ICU. The fact that we demonstrated an improvement in TTE examination scores in this setting, suggests that TTE may be effectively taught on nonideal, real-world patients. In clinical practice, participants will be examining these patients, and not standardized mannequins or healthy volunteers with ideal body habitus. Additionally, the time to posttest clinical evaluation ranged from 1 to 8 weeks posttraining, in contrast to other studies which performed posttest evaluation either immediately after training or <1 week after training.15,24,25,28,29 A comparison of studies is shown in Supplemental Table 1.
The limitations of this study included the use of non-standardized patients, the use of both spontaneously breathing and mechanically ventilated patients, variable follow-up times to posttraining assessments, nonstandardized teaching among the authors (although attempted by using one PowerPoint presentation), the authors performing the training and assessment of the participants were not officially certified in bedside TTE, small sample size and lack of a priori sample size calculation, and lack of eligible patients who required ultrasound. Thirty-one out of 42 participants rotating through the ICU who underwent TTE and fluid assessment training completed the study in its entirety. Reasons for not completing the study were most commonly that residents or fellows finished the ICU rotation without completing posttraining examinations or surveys. Due to scheduling conflicts, we could not complete all the residents′ posttraining examinations.
Furthermore, this single-group pre-post design is limited by the lack of a control group. We cannot conclude that the improvement in scores from pretraining did not improve due to the effect of taking the same test twice or the effect of normal maturation. Since different patients with varying body habitus were used between trainees and between pretraining and posttraining assessments, we cannot be sure that the times improved because of the training and not because the pretest conditions were more difficult than the posttest. Additionally, several ICU attendings may have provided additional TTE education and training after the training session, which could have contributed to some trainees’ improved performance. Participants who received prior TTE education may also confound the results. Finally, bias resulting from regression to the mean or the natural change that may occur due to time should not be overlooked.
CONCLUSIONS
This study demonstrated that a 60-minute TTE training session for ICU trainees resulted in improved knowledge and TTE skills. TTE-naïve trainees scored better on their post-tests after training compared to TTE-experienced trainees. Furthermore, the training encouraged trainees to use TTE more in the ICU. This time-efficient teaching modality may be beneficial to integrate TTE education into residency and critical care fellowship curricula, however, more studies are warranted.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank all the trainees who participated in this project, as well as the ICU nurses at Brigham and Women’s Hospital for their help and accommodation in performing the study.
This work was supported by Grants UL1TR001855 and UL1TR000130 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
COMPETENCIES: Practice-Based Learning and Improvement, Patient Care, Systems-Based Practice, Medical Knowledge, Interpersonal and Communication Skills, Professionalism
Main Affiliation Address: Brigham and Women’s Hospital, 75 Francis Street, Boston, MA 02115.
SUPPORTING INFORMATION
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.jsurg.2018.03.004.
REFERENCES
- 1.Singh S, Lighthall G. Update on the evaluation of intravascular fluid status in critically ill patients. PCCSU. 2013;25 Lesson 7. https://www.chestnet.org/Education/Products/e-Learning/Update-on-the-Evaluation-of-Intravascular-Fluid-Status-in-Critically-Ill-Patients. [Google Scholar]
- 2.Ramsigh D, Alexander B, Le K, Williams W, Canales C, Cannesson M. Comparison of the didactic lecture with the simulation/model approach for the teaching of a novel perioperative ultrasound curriculum to anesthesiology residents. J Clin Anesth. 2014;26: 443–454. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Z, Xu X, Ye S, Xu L. Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: systematic review and meta-analysis. Ultrasound Med Biol. 2014;40(5):845–853. [DOI] [PubMed] [Google Scholar]
- 4.Mclean AS. Echocardiography in shock management. Crit Care. 2016;20:275–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F. Haemodynamic instability in sepsis: bedside assessment by Doppler echocardiography. Am J Respir Crit Care Med. 2003;168:1270–1276. [DOI] [PubMed] [Google Scholar]
- 6.Charron C, Repesse X, Bodson L, Au SM, Vieillard-Baron A. Ten good reasons why everybody can and should perform cardiac ultrasound in the ICU. Anaesthesiol Intensive Ther. 2014;46(5):319–322. [DOI] [PubMed] [Google Scholar]
- 7.Kanji HD, McCallum J, Sirounis D, MacRedmond R, Moss R, Boyd JH. Limited echocardiography-guided therapy in subacute shock is associated with change in management and improved outcomes. J Crit Care. 2014;29:700–705. [DOI] [PubMed] [Google Scholar]
- 8.Shokoohi H, Boniface KS, Pourmand A, et al. Bedside ultrasound reduces diagnostic uncertainty and guides resuscitation in patients with undifferentiated hypotension. Crit Care Med. 2015;43:2562–2569. [DOI] [PubMed] [Google Scholar]
- 9.Bernier-Jean A, Albert M, Shiloh AL, Eisen LA, Williamson D, Beaulieu Y. The diagnostic and therapeutic impact of point-of-care ultrasonography in the intensive care unit. J Intensive Care Med. 2017;32(3):197–203. [DOI] [PubMed] [Google Scholar]
- 10.Oks M, Cleven KL, Cardenas-Garcia J, et al. The effect of point-of-care ultrasonography on imaging studies in the medical ICU a comparative study. Chest. 2014;146(6):1574–1577. [DOI] [PubMed] [Google Scholar]
- 11.Peris A, Tutino L, Zagli G, et al. The use of point-of-care bedside lung ultrasound significantly reduces the number of radiographs and computed tomography scans in critically ill patients. Anesth Analg. 2010;111: 687–692. [DOI] [PubMed] [Google Scholar]
- 12.Killu K, Coba V, Mendez M, et al. Model point-of-care ultrasound curriculum in an intensive care unit fellowship program and its impact on patient management. Crit Care Res Pract. 2014:1–6 [Article ID 934796], 10.1155/2014/934796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conlin F, Connelly NR, Raghunathan K, Friderici, Schwabauer A. Focused transthoracic cardiac ultrasound: a survey of training practices. J Cardiothorac Vasc Anesth. 2016;30(1):102–107. [DOI] [PubMed] [Google Scholar]
- 14.Mosier JM, Malo J, Stolz LA, et al. Critical care ultrasound training: a survey of US fellowship directors. J Crit Care. 2014;29:645–649. [DOI] [PubMed] [Google Scholar]
- 15.Edrich T, Seethala RR, Olenchock BA, et al. Providing initial transthoracic echocardiography training for anesthesiologists: simulator training is not inferior to live training. J Cardiothorac Vasc Anesth. 2014;28(1):49–53. [DOI] [PubMed] [Google Scholar]
- 16.Kanji HD, McCallum JL, Bhagirath KM, Neitzel AS. Curriculum development and evaluation of a hemodynamic critical care ultrasound: a systematic review of the literature. Crit Care Med. 2016;44:e742–e750. [DOI] [PubMed] [Google Scholar]
- 17.Tanzola RC, Walsh S, Hopman WM, Sydor D, Arellano R, Allard RV. Brief report: focused transthoracic echocardiography training in a cohort of Canadian anesthesiology residents: a pilot study. Can J Anesth. 2013;60:32–37. [DOI] [PubMed] [Google Scholar]
- 18.Dinh VA, Giri PC, Rathinavel I, et al. Impact of a 2-day critical care ultrasound course during fellowship training: a pilot study. Crit Care Res Pract. 2015:1–8 [Article ID 675041], 10.1155/2015/675041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hulett CS, Pathak V, Katz JN, Montgomery SP, Chang LH. Development and preliminary assessment of a critical care ultrasound course in an adult pulmonary and critical care fellowship program. Ann Am Thorac Soc. 2014;11(5):784–788. [DOI] [PubMed] [Google Scholar]
- 20.Solymos O, O’Kelly P, Walshe CM. Pilot study comparing simulation-based and didactic lecture-based critical care teaching for final-year medical students. BMC Anesthesiol. 2015;15:153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jensen MB, Sloth E, Larsen KM, Schmidt MB. Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. J Anaesthesiol. 2004;21:700–707. [DOI] [PubMed] [Google Scholar]
- 22.Dixon WJ, Massey FJ Jr.. Introduction to statistical analysis. 4th edNew York: McGraw-Hill Companies; 1983. 1–672. [Google Scholar]
- 23.Quade D. Rank analysis of covariance. J Am Stat Assoc. 1967;62(320):1187–1200. [Google Scholar]
- 24.Rebel A, Srour H, DiLorenzo A, et al. Ultrasound skill and application of knowledge assessment using an innovative OSCE competition-based simulation approach. J Educ Perioper Med. 2016;18(1):1–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Parks AR, Atkinson P, Verheul G, LeBlanc-Duchin D. Can medical learners achieve point-of-care ultrasound competency using a high-fidelity ultrasound simulator?: a pilot study Critical Care Ultrasound J. 2013;5: 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho AM, Critchley LAH, Leung JYC, et al. Introducing final-year medical students to pocket-sized ultrasound imaging: teaching transthoracic echocardiography on a 2-week anesthesia rotation. Teach Learn Med. 2015; 27(3):307–313. [DOI] [PubMed] [Google Scholar]
- 27.Diaz-Gomez JL, Perez-Protto S, Hargrave J, et al. Impact of a focused transthoracic echocardiography training course for rescue applications among anesthesiology and critical care medicine practitioners: a prospective study. J Cardiothorac Vasc Anesth. 2015;29(3):576–581. [DOI] [PubMed] [Google Scholar]
- 28.Neelankvil J, Howard-Quijano K, Hsieh TC, et al. Transthoracic echocardiography simulation is an efficient method to train anesthesiologists in basic transthoracic echocardiography skills. Anesth Analg. 2012;115(5):1042–1051. [DOI] [PubMed] [Google Scholar]
- 29.Parks AR, Verheul G, LeBlanc-Duchin D, Atkinson P. Effect of a point-of-care ultrasound protocol on the diagnostic performance of medical learners during simulated cardiorespiratory scenarios. CJEM. 2015;17(3):263–269. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.