Abstract
Pulmonary arterial hypertension (PAH) is a fatal disease of the cardiopulmonary system that lacks curative treatments. The main pathological event in PAH is elevated vascular resistance in the pulmonary circulation, caused by abnormal vasoconstriction and vascular remodelling. Ion channels are key determinants of vascular smooth muscle tone and homeostasis, and four PAH channelopathies (KCNK3, ABCC8, KCNA5, TRPC6) have been identified so far. However, the contribution of ion channels in other forms of PAH, which account for the majority of PAH patients, has been less well characterised. Here we reason that a variety of triggers of PAH (e.g. BMPR2 mutations, hypoxia, anorectic drugs) that impact channel function may contribute to the onset of the disease. We review the molecular mechanisms by which these ‘extrinsic’ factors converge on ion channels and provoke their dysregulation to promote the development of PAH. Ion channels of the pulmonary vasculature are therefore promising therapeutic targets because of the modulation they provide to both vasomotor tone and proliferation of arterial smooth muscle cells.
Keywords: ion channels, patch clamp, potassium channels, pulmonary hypertension, vascular smooth muscle
Introduction
Pulmonary arterial hypertension (PAH) is a progressive disease of the cardiopulmonary system with life-limiting consequences. PAH is defined by a mean pulmonary artery pressure above 25 mmHg at rest, and end-expiratory pulmonary artery wedge pressure of less than 15 mmHg. Disease factors include: (i) genetic origins (i.e. mutations in genes crucial for pulmonary vascular function); (ii) other pathologies including congenital heart disease, portal hypertension, HIV or COPD; (iii) drugs or toxins, or (iv) unknown factors (i.e. PAH of idiopathic origins) [1]. In all cases, a complex pathological cascade leads to narrowing and remodelling of arteries and/or increased vascular reactivity ultimately leading to increased vascular resistance and elevated pulmonary blood pressure which may precipitate in right heart failure and death [1]. The development of PAH-specific therapies significantly improved patients’ outcome and quality of life [2]. However, poor prognosis (57% five-year survival rate), resistance to current drugs, and lack of curative treatment means there is an unmet need for new and innovative targets in PAH pharmacotherapy [2].
Ion channels have an important homeostatic function whereby they regulate the resting membrane potential and cytoplasmic [Ca2+] of pulmonary arterial smooth muscle cells (PASMC), which is a key determinant of vasoconstriction and vascular cell proliferation [3,4]. Therefore, the dual involvement of ion channels in the control of arterial tone and remodelling makes them potential key mediators in the pathogenic cascade of PAH, which can be therapeutically targeted. Supporting this view is the notion that mutations in ion channel genes may lead to hereditary forms of PAH [4,5]. Ion channel dysregulation may also be secondary to alterations in the cellular environment that take place during PAH, and thus contribute to worsening of the condition [6,7]. We therefore suggest that dysregulation of ion channels could be a convergence point in PAH pathogenesis, independent of the pathological trigger.
Here we examine the pathophysiological roles of ion channels in PAH, and how their dysfunction, either directly caused by genetic alterations in ion channel genes (‘intrinsic’ dysregulation) or secondary to altered cellular microenvironment (‘extrinsic’ factors), can lead to PAH. Since a range of recent reviews has covered the pathophysiology of PAH channelopathies [4,5], we primarily focus this review on the extrinsic factors (e.g. hypoxia, endothelial dysfunction, drugs, HIV) that contribute to dysfunction of plasmalemmal channels in PASMCs during PAH.
Overview of channelopathies in PAH
A range of de novo and heritable mutations in PASMC ion channels have been implicated in familiar forms of PAH, these include mutations in the KCNK3, ABCC8, KCNA5 and TRPC6 genes. [4]
The TWIK-related acid-sensitive K+ (TASK) channels belong to the superfamily of Two-Pore Domain K+ (K2P) channels [8]. The TASK1 (KCNK3) channel is responsible for the background IKN leak current that contributes to the resting membrane potential, vasomotor tone as well as proliferation of PASMCs [7,9]. So far, 12 loss-of-function missense mutations were identified in KCNK3, which was the first channelopathy discovered in PAH [5]. The lack of ‘protective’ heterodimerisation with TASK3 appears to underlie the lung-specific phenotype of KCNK3 mutations [10]. Several in vivo studies confirmed that TASK1 loss-of-function precedes haemodynamic changes and is sufficient to cause PAH [7,9].
ATP-sensitive K+ (KATP) channels promote hyperpolarisation and vasodilation in vascular smooth muscle cells [11]. Recently, 23 loss-of-function mutations in ABCC8 (encoding the regulatory SUR1 subunit) were found in PAH patients [5,12]. These heterozygous mutations appear to impair channel trafficking and/or affect ATP sensitivity [13]. Several paradoxes surround this second PAH channelopathy, such as the lack of congenital hyperinsulinism, or the observation that patients with Cantú syndrome, with gain-of-function mutations in Kir6.1 and SUR2 subunits, also exhibit pulmonary hypertension [14]. The role of KATP in the pulmonary circulation therefore remains to be clarified.
In the pulmonary vasculature voltage-gated K+ (Kv) channels also regulate the resting membrane potential, Ca2+ influx and vasoconstriction as well as cellular apoptosis, migration and proliferation [3,15]. Strong lines of evidence support a causal role for Kv1.5 dysfunction in PAH [16]. Sequencing of idiopathic PAH (IPAH) patients identified a number of mutations in the promoter and coding regions of KCNA5 believed to affect its transcription, trafficking, and interaction with its β subunits [17,18]. A new variant has also been found in Pulmonary Hypertension of the Newborn (PPHN) [19]
Transient Receptor Potential Canonical (TRPC) channels are a subfamily of non-selective cation channels, which represent a major alternative route of Ca2+ entry outside voltage-gated Ca2+ channels, by functioning as both store-operated (SOC) and receptor-operated (ROC) channels [20]. Pharmacological blockade and knock-out experiments found a strong correlation between TRPC6 expression, capacitative Ca2+ entry, resting cytoplasmic [Ca2+], vascular tone and proliferation of rat PASMCs [21]. In PAH, increased TRPC6 expression promotes vasoconstriction and neomuscularisation of pulmonary arteries [22]. A genotypic analysis found that the 254(C → G) single nucleotide polymorphism (SNP) was 2.85 times more common in IPAH patients [23]. It is of interest that another mutation in TRPC6 (F443I) was recently found to associate with PPHN [19].
Extrinsic dysregulation of ion channels in PAH
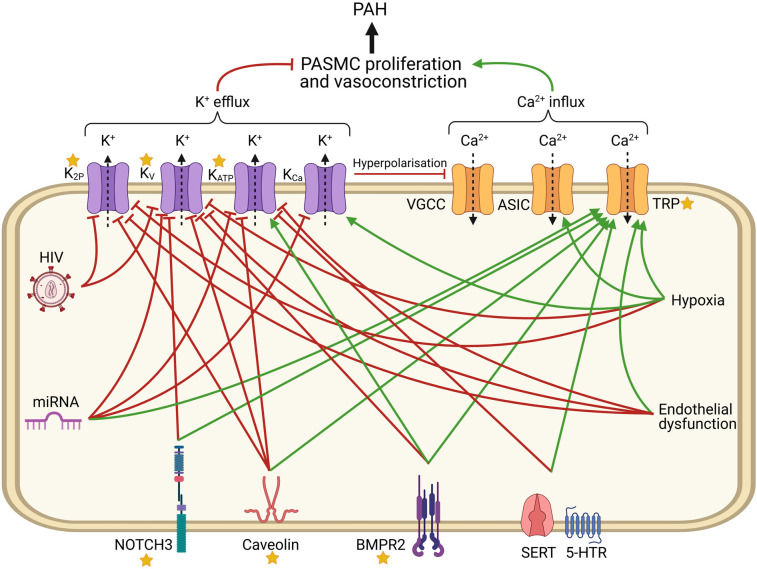
Individuals with mutations in ion channels represent a minority of PAH patients, whereas dysregulation of ion channels is also observed in patients with other forms of PAH [6,7,24]. PAH can be induced by a wide variety of triggers, giving rise to different classifications (Table 1) [1]. In this section, the involvement of ion channels in the various forms of PAH is examined (Figure 1).
Table 1. Clinical classification of PAH.
| 1. Pulmonary arterial hypertension (PAH) |
| 1.1 Idiopathic PAH (IPAH) |
| 1.2 Heritable/familial PAH (HPAH) |
| 1.2.1 BMPR2 mutations |
| 1.2.2 Other mutations (e.g. KCNK3, CAV1) |
| 1.3 Drug-induced PAH (DPAH) (e.g. fenfluramine) |
| 1.4 PAH Associated with comorbidities (APAH) |
| 1.4.1 Connective tissue disease (e.g. systemic sclerosis) |
| 1.4.2 Human immunodeficiency virus (HIV) infection |
| 1.4.3 Portal hypertension |
| 1.4.4 Congenital heart disease |
| 1.4.5 Schistosomiasis |
| 1′. Pulmonary veno-occlusive disease and/or pulmonary capillary haemangiomatosis |
| 1″. Persistent pulmonary hypertension of the newborn (PPHN) |
Figure 1. Dysregulation of PASMC ion channels during PAH.
Red lines represent inhibitory influences vs activation for green arrows. Stars represent proteins with mutations associated with PAH.
Germline mutations
BMPR2
Signalling events involving the transforming growth factor-β (TGFβ) family, in particular bone morphogenetic proteins (BMP), are an important regulator of PASMC homeostasis. More than 806 loss-of-function variants in bone morphogenetic protein receptor type II (BMPR2) have been identified, which account for 75% and 25% of heritable PAH (HPAH) and IPAH cases, respectively [24,25].
Several lines of evidence link BMP signalling to regulation of K+ channels in PASMC. Indeed, BMP2 up-regulates the expression of α subunits through Mothers Against Decapentaplegic Homologues (SMADs), while decreasing the expression of inhibitory β and γ subunits in human PASMC [26]. In a murine model of PAH, BMPR2 loss-of-function reduced Kv1.5 expression, and resulted in increased voltage-gated Ca2+ entry and vasoconstriction [27]. Additive effects between BMPR2 and KCNA5 mutations may underlie the earlier age of onset and higher disease severity in digenic patients, suggesting that mutational load and the presence of ‘second hits’ is important in PAH progression [28]. BMPR2 deletion was also shown to down-regulate TASK1 and promote vasoconstriction in rat PASMC, although in this case modulation appears to be transcription-independent, but instead due to altered channel trafficking [25]. ABCC8 mRNA expression was also up-regulated in lung biopsies obtained from BMPR2 patients [29].
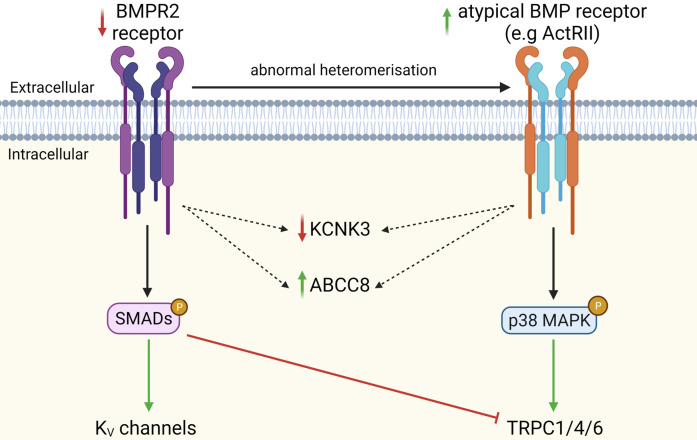
BMPR2 mutations also promote the formation of atypical heteromeric BMP receptors, shifting BMP signalling towards non-canonical MAPK-dependent pathways in murine PASMCs [30,31]. This shift is important, as BMP2 was shown to inhibit the expression of TRPC1/4/6 channels and proliferation of proximal rat PASMCs, whereas BMP4 up-regulated TRPC1/4/6 expression and distal PASMCs proliferation via non-canonical cascade PASMCs [32,33]. Overall, BMPR2 haploinsufficiency favours the formation of different BMP receptor complexes, suppressing the canonical, pro-apoptotic BMP2/SMAD signalling in proximal PASMCs, and potentiating the non-canonical, pro-proliferative BMP4/p38 axis in distal human PASMCs (Figure 2) [34,35].
Figure 2. Consequences of shift from canonical BMPR2 to non-canonical BMP signalling on ion channel function in PASMCs.
Continuous arrows denote inhibition/down-regulation (red) or activation/up-regulation (green). Dotted arrows represent undefined links. ‘P’ denotes phosphorylated, activated mediator. MAPK, mitogen-activated protein kinase; ActRII, activin type 2 receptor.
Caveolin
The scaffolding protein caveolin is a structural component of caveolae, which are specialised dynamic lipid rafts important for microdomain functional coupling [36]. For instance, in the pulmonary vasculature, the caveolin ‘signalplex’ regulates arterial vasoconstriction by interacting with Ca2+ regulatory molecules [36]. Several mutations that decrease caveolin-1 (CAV1) expression were found in PAH, and CAV1 knock-out in animal models leads to pulmonary hypertension [37,38]. Contrary to the loss of expression in pulmonary endothelium, CAV1 expression is up-regulated in rat PASMCs and promotes proliferation [39]. Caveolin-1 directly influences the kinetics, assembly and regulation of several vascular channels via its scaffolding domain. For instance, binding of caveolins to Kir6.1, Kv1.5 and TASK1 reduced their functional activity in heterologous expression systems [40–42]. Caveolin-1 is also a positive regulator of TRPC assembly and SOCE in mice pulmonary vascular cells [43]. Increased caveolin expression in PASMCs of two rat models of PAH (chronic hypoxia and monocrotaline) was found to enhance agonist-induced SOCE/ROCE and vasoconstriction in pulmonary arteries [44].
NOTCH3
The transmembrane NOTCH3 receptor controls the differentiation of PASMCs from proliferative to contractile phenotype [45]. Three genetic variants in NOTCH3 were linked to PAH [19,46]. Clinical studies found a causative role for the overexpression of NOTCH3 in the abnormal proliferation of PASMCs in PAH [47,48]. NOTCH3 enhanced Ca2+ entry in human PASMCs by (i) up-regulating TRPC6-dependent SOCE and (ii) inhibiting Kv1.2/Kv1.5 activity, which in turn promotes voltage-gated Ca2+ entry [45,49]. The resulting increased Ca2+ mobilisation leads to PAH by preferentially promoting vascular remodelling [47]. The fact that some of these effects were transcription-independent hints that non-canonical signalling of NOTCH3 may be involved in this pathological process [45,49]. Indeed, the two NOTCH3 missense mutations were shown to boost proliferative signalling of NOTCH3, despite actually decreasing its downstream transcriptional activity [46]. The NOTCH intracellular domain (NICD) has also been proposed to directly influence ion channel activity [45,49].
Epigenetics
MicroRNAs (miRNAs) are small non-coding RNAs that regulate gene expression by binding and silencing the translation of target mRNAs. Several studies have shown a correlation between dysregulation of miRNAs, altered ionic currents and dysfunction of rat and human pulmonary artery in vivo. For example, the Kv1.2, Kv1.5, Kv7.5, BKCaβ1 and TASK1 channels are under direct negative control of miR-1, miR-23b-3p, miR-29b, miR-138, miR-190, miR-206 and miR-222, whose up-regulation in PAH (e.g. 4-fold for miR-1) decreased channel expression in human and rodent PASMCs, and promoted membrane depolarisation and arterial wall hypertrophy [50–52]. In addition, down-regulation of miR-135a-5p increased TRPC1 expression and promoted PASMC proliferation [53]. miRNAs are promising diagnostic markers of PAH, as well as potential therapeutic targets to correct ion channel dysfunction in PAH.
Comorbidities and PAH
HIV
PAH is one of the most severe complications of HIV infection and a major cause of mortality in HIV-PAH patients, leading to a lower survival rate compared with other PAH patients [54]. HIV infection increases the incidence of PAH by 2500-fold in human subjects [54], and can trigger PAH in some laboratory animals (rats and macaques, but not mice) [55–57]. Two studies showed that HIV transgenes down-regulated the IKN and IKV currents (decreased Kv1.5, Kv7.1 and Kv7.4 expression) in rodent pulmonary arteries, possibly contributing to membrane depolarisation [55,57]. The Vpu protein of HIV-1 shares a high homology with the N-terminal of TASK1 channel, and it promotes abnormal oligomerisation of Vpu and TASK1 subunits, which leads to their degradation in heterologous expression systems [58]. The connection between HIV and PAH remains to be determined, one question being why only a small proportion (8.3%) of HIV patients have PAH.
Hypoxia
Hypoxia is a known trigger of pulmonary hypertension and ion channels are essential mediators of the hypoxic pulmonary vasoconstriction (HPV) [59]. The inhibition of Kv1.5 and Kv2.1 channels in the small resistance pulmonary arteries is a major contributor of HPV [15,60], but the underlying regulatory mechanisms remain controversial [61,62]. Although redox signalling is a key component of HPV, the extent of changes in the level of reactive oxygen species (ROS) during hypoxia are not fully defined, and both a decrease and an increase in ROS were shown to inhibit Kv channel opening [61]. The molecular mechanisms of oxygen sensing in PASMCs are also not fully defined. Mitochondria, which produce ROS in proportion to PO2 levels, are likely involved in the PASMC response to hypoxia [62]. Cytoplasmic NADPH oxidases, which also produce ROS, reportedly lead to inhibition of Kv1.5 channel activity and modulation of channel trafficking via oxidation of C-terminal cysteine residues [63]. Also the TASK1 channel mediates an O2-sensitive current in carotid body cells [64]. Conversely, hypoxia down-regulated both TASK1 expression (via the RELMβ-STAT3-NFAT pathway) and activity (via the kinase Src), which promote human PASMC proliferation and vasoconstriction [65,66].
Hypoxia led to activation of store-operated Ca2+ entry (SOCE) and elevation of cytoplasmic [Ca2+] in rodent PASMCs [67]. Mice in which the Trpc1 and Trpc6 genes were deleted (knockouts) had impaired hypoxic response and loss of hypoxic vasoconstriction [22]. The rise in ROS up-regulates both the expression and assembly of SOCE channels to promote Ca2+ mobilisation in hypoxic PASMCs [68,69]. There is evidence indicating that hypoxia directly modulates TRPC6 via the second messenger diacylglycerol and the enzyme AMP-activated protein kinase. Calcium Release-Activated Calcium (ORAI) channels are involved in the control of proliferation of rat PASMCs, but their role in PAH requires further investigation [21].
The mechanisms of chronic hypoxia, more relevant to the context of PAH, may differ from those of HPV. Hypoxia-inducible factors (HIFs) are key transcription factors that contribute to remodelling of pulmonary artery during chronic hypoxia [70]. Selective down-regulation of the expression of Kv α subunits (Kv1.1, Kv1.5, Kv2.1, Kv4.3, Kv9.3) in PASMC via HIF1α occurs during chronic hypoxia; this signalling pathway is abnormally potentiated by ROS during PAH [71,72]. In contrast, hypoxia increased the expression of Ca2+-activated K+ (BKCa) channels in rat PASMCs, which may explain the BKCa up-regulation seen in pulmonary arteries of PAH patients [73]. The underlying mechanism involves altered expression of the auxiliary β1 subunit via HIF1α, which enhances BKCa channel sensitivity to voltage and Ca2+, hence promoting PASMC relaxation and thus constituting an endogenous protective mechanism [74].
Chronic hypoxia also selectively up-regulates a range of non-selective cation channels in PASMCs including TRPC1 and TRPC6, via the HIF1α and Notch signalling pathways, and the osmo-mechanosensitive cation channels, TRPV1/4 [75–77]. The family of acid-sensitive ion channels (ASIC) can also participate in SOCE in pulmonary vascular cells [67]. ASIC1-dependent Ca2+ entry during hypoxia is independent of changes in gene expression [67], but it depends on inactivation of the inhibitory effect of H2O2 on ASIC1 channel, as well as stimulation of forward trafficking via the protein RhoA [67,78]. The increase in cytoplasmic [Ca2+] in PASMCs observed in hypoxia led to activation of transcription factor NFAT which down-regulates Kv1.5 expression and mitochondrial homeostasis, potentially hardwiring ionic dysfunction in a pathological feedback loop [79].
5-HT Signalling and anorectic drugs
Appetite-suppressants that potentiate serotonin signalling (e.g. fenfluramine, benfluorex) were taken off market after causing a drug-induced PAH epidemic in the 1960–70s [80]. The causal role of up-regulated 5-HT signalling in PASMCs of PAH patients and animal models further reinforced this ‘serotonin hypothesis’ of PAH [81]. The serotonin transporter (SERT) is strongly implicated in the pathogenesis of PAH [82], and some studies have linked a gain-of-function polymorphism in SERT to an increased risk of PAH [83].
5-HT is both a potent vasoconstrictor and PASMC mitogen, known to up-regulate TRPC1, TRPC6, TRPV4 currents in rat PASMCs [84,85]. Anorectic drugs constrict pulmonary arteries by inhibiting Kv1.5 currents, although the underlying molecular mechanisms are not fully understood and may include direct KV channel inhibition, activation of 5-HT2 receptors or internalisation by SERT [86]. The pathways downstream of the 5-HT receptor and transporter seem to converge on second messengers like ROS [87] and kinases [86], which are known modulators of ion channel activity. For instance, 5-HT triggers the endocytosis of Kv1.5 channels in PASMC through a 5-HT2AR/tyrosine kinase/caveolin pathway [88].
Endothelial dysfunction
The endothelium produces several vasoactive mediators that play an important role in PASMC homeostasis. A shift towards vasoconstrictive and mitogenic endothelial signals is one of the first events in PAH. It is still unclear whether endothelial dysfunction is a cause or consequence of PAH; however a monocrotaline-induced animal model of PAH presents pulmonary endothelium dysfunction, which is targeted by current PAH therapies (e.g. endothelin receptor antagonists, prostacyclin analogues) [89]. Endothelial dysfunction is accompanied by up-regulation of endothelin-1 and down-regulation of NO and PGI2 signalling [89]. These factors modulate vascular ion channels through cyclic nucleotides and protein kinases [90]. Endothelin-1 promotes depolarisation in rodent and human PASMCs and vasoconstriction by inhibiting IKV, IKATP and up-regulating ICaCl, IBKCa and TRPC currents through the PLC/PKC pathway [90]. Endothelin-1 also inhibits TASK1 in PASMC, which could involve both gating inhibition in TASK1 as well as its phosphorylation-dependent internalisation [91,92]. The NO/cGMP/PKG pathway promotes vasorelaxation by activating IKv, IKCa, IKN, IKATP, and inhibiting ISOCE [90,93]. Likewise, the PGI2/ cAMP/PKA axis activates IKv, IKCa, IKN, IKATP and inhibits TRPC channels [90,94].
Summary and implications for therapy
Ion channels are key determinants of the tone and the remodelling of the pulmonary artery. Over 50 genetic variants in four ion channels (KCNK3, ABCC8, KCNA5 and TRPC6) have been found in PAH patients [4]. In this review, we show that ion channel dysfunction occurs in virtually in all forms of PAH (Figure 1).
A better characterisation of the regulation of ion channels in PAMSCs could provide new information about why so many different triggers (e.g. anorectic drugs, HIV, hypoxia) can all lead to PAH. Integrative ‘omic’ approaches hold hope for establishing a deep genotype-phenotype correlation of the disease. Identifying new pathways that regulate PASMCs ion channels will be important to draw an accurate picture of their pathological relevance in the various forms of PAH (e.g. the recently proposed link between TASK1 and vitamin D deficiency) [95]. Also, the molecular mechanisms that dysregulate the Kv7 channel [96], the mechanosensitive Piezo1 channel [97] and the Ca2+-activated Cl− channel TMEM16A [98] in PAH remain poorly understood.
Multiple studies showed that activators of K+ channels [7,99] and inhibitors of both Cl- channels [98] and TRPC channels [100] can prevent and/or reverse PAH in animal models. Optimising the selectivity, potency and lung-specific delivery of these compounds will therefore be paramount to the development of new PAH therapies. Recent advances in the determination of structures for these channel types may also expedite drug discovery efforts towards this goal
Perspectives
Highlight the importance of the field: Pulmonary arterial hypertension is a multifactorial and severe disease with no curative treatments. Vasoconstriction and arterial remodelling both contributes to elevated resistance to blood flow and increased blood pressure.
A summary of the current thinking: Ion channels are involved in the control of both arterial tone and proliferation of pulmonary artery smooth muscle cells. Dysfunction of ion channels plays a causative role in PAH, and may link the different pathological triggers of PAH to the onset of the disease.
A comment on future directions: Ion channels are currently under-explored targets for PAH. Understanding the regulation and pathophysiological role of ion channels in PAH will provide new avenues for therapeutic intervention.
Acknowledgements
This work was supported by funding from the British Heart Foundation (PG/19/8/34168), the Biotechnology and Biological Sciences Research Council (BB/T007664/1 and BB/T002018/1) and the Wellcome Trust. T.J.-T. is a student on the OXION PhD Programme in Ion Channels and Disease. Figures were created with Biorender.
Abbreviations
- BMP
bone morphogenetic proteins
- BMPR2
bone morphogenetic protein receptor type II
- CAV1
caveolin-1
- HIF
hypoxia-inducible factor
- HPAH
heritable pulmonary arterial hypertension
- HPV
hypoxic pulmonary vasoconstriction
- IPAH
idiopathic pulmonary arterial hypertension
- KATP
ATP-sensitive K+
- PAH
Pulmonary arterial hypertension
- PASMC
pulmonary arterial smooth muscle cells
- PPHN
Pulmonary Hypertension of the Newborn
- ROS
reactive oxygen species
- SERT
serotonin transporter
- SOCE
store-operated Ca2+ entry
- TASK1
TWIK-Related Acid Sensitive K+ Channel 1
- TRPC
Transient Receptor Potential Canonical
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Open Access Statement
Open access for this article was enabled by the participation of University of Oxford in an all-inclusive Read & Publish pilot with Portland Press and the Biochemical Society under a transformative agreement with JISC.
Author contributions
All authors were involved in writing and editing the manuscript. T.J.-T. produced the figures.
References
- 1.Galiè, N., Humbert, M., Vachiery, J.L., Gibbs, S., Lang, I., Torbicki, A.et al. (2015) 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Respir. J. 46, 903–975 10.1183/13993003.01032-2015 [DOI] [PubMed] [Google Scholar]
- 2.Lau, E.M.T., Giannoulatou, E., Celermajer, D.S. and Humbert, M. (2017) Epidemiology and treatment of pulmonary arterial hypertension. Nat. Rev. Cardiol. 14, 603–614 10.1038/nrcardio.2017.84 [DOI] [PubMed] [Google Scholar]
- 3.Kuhr, F.K., Smith, K.A., Song, M.Y., Levitan, I. and Yuan, J.X.J. (2012) New mechanisms of pulmonary arterial hypertension: role of Ca2+ signaling. Am. J. Physiol. Heart Circ. Physiol. 302, 1546–1562 10.1152/ajpheart.00944.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambert, M., Capuano, V., Olschewski, A., Sabourin, J., Nagaraj, C., Girerd, B.et al. (2018) Ion channels in pulmonary hypertension: a therapeutic interest? Int. J. Mol. Sci. 19, 3162 10.3390/ijms19103162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Ribeuz, H., Capuano, V., Girerd, B., Humbert, M., Montani, D. and Antigny, F. (2020) Implication of potassium channels in the pathophysiology of pulmonary arterial hypertension. Biomolecules 10, 1261 10.3390/biom10091261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu, X.R., Zhang, M.F., Yang, N., Liu, Q., Wang, R.X., Cao, Y.N.et al. (2012) Enhanced store-operated Ca2+ entry and TRPC channel expression in pulmonary arteries of monocrotaline-induced pulmonary hypertensive rats. Am. J. Physiol. Cell Physiol. 302, 77–87 10.1152/ajpcell.00247.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antigny, F., Hautefort, A., Meloche, J., Belacel-Ouari, M., Manoury, B., Rucker-Martin, C.et al. (2016) Potassium channel subfamily K member 3 (KCNK3) contributes to the development of pulmonary arterial hypertension. Circulation 133, 1371–1385 10.1161/CIRCULATIONAHA.115.020951 [DOI] [PubMed] [Google Scholar]
- 8.Bayliss, D.A., Czirják, G., Enyedi, P., Goldstein, S.A.N., Lesage, F., Minor, Jr, D.L.et al. (2019) Two P domain potassium channels (version 2019.4) in the IUPHAR/BPS Guide to Pharmacology Database. IUPHAR/BPS Guid. to Pharmacol. CITE
- 9.Lambert, M., Capuano, V., Boet, A., Tesson, L., Bertero, T., Nakhleh, M.K.et al. (2019) Characterization of Kcnk3 -mutated rat, a novel model of pulmonary hypertension. Circ. Res. 125, 678–695 10.1161/CIRCRESAHA.119.314793 [DOI] [PubMed] [Google Scholar]
- 10.Bohnen, M.S., Roman-Campos, D., Terrenoire, C., Jnani, J., Sampson, K.J., Chung, W.K.et al. (2017) The impact of heterozygous KCNK3 mutations associated with pulmonary arterial hypertension on channel function and pharmacological recovery. J. Am. Heart Assoc. 6, e006465 10.1161/JAHA.117.006465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Foster, M.N. and Coetzee, W.A. (2015) KATP channels in the cardiovascular system. Physiol. Rev. 96, 177–252 10.1152/physrev.00003.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lago-Docampo, M., Tenorio, J., Hernández-González, I., Pérez-Olivares, C., Escribano-Subías, P., Pousada, G.et al. (2020) Characterization of rare ABCC8 variants identified in spanish pulmonary arterial hypertension patients. Sci. Rep. 10, 15135 10.1038/s41598-020-72089-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ashcroft, F.M. (2005) ATP-sensitive potassium channelopathies: focus on insulin secretion. J. Clin. Invest. 115, 2047–2058 10.1172/JCI25495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McClenaghan, C., Woo, K.V. and Nichols, C.G. (2019) Pulmonary hypertension and ATP-sensitive potassium channels: paradigms and paradoxes. Hypertension 74, 14–22 10.1161/HYPERTENSIONAHA.119.12992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonnet, S. and Archer, S.L. (2007) Potassium channel diversity in the pulmonary arteries and pulmonary veins: implications for regulation of the pulmonary vasculature in health and during pulmonary hypertension. Pharmacol. Ther. 115, 56–69 10.1016/j.pharmthera.2007.03.014 [DOI] [PubMed] [Google Scholar]
- 16.Pozeg, Z.I., Michelakis, E.D., McMurtry, S., Thébaud, B., Wu, X.C., Dyck, J.R.B.et al. (2003) In vivo gene transfer of the O2-sensitive potassium channel Kv1.5 reduces pulmonary hypertension and restores hypoxic pulmonary vasoconstriction in chronically hypoxic rats. Circulation 107, 2037–2044 10.1161/01.CIR.0000062688.76508.B3 [DOI] [PubMed] [Google Scholar]
- 17.Pousada, G., Baloira, A., Vilariño, C., Cifrian, J.M. and Valverde, D. (2014) Novel mutations in BMPR2, ACVRL1 and KCNA5 genes and hemodynamic parameters in patients with pulmonary arterial hypertension. PLoS ONE 9, e100261 10.1371/journal.pone.0100261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Remillard C, V., Tigno, D.D., Platoshyn, O., Burg, E.D., Brevnova, E.E., Conger, D.et al. (2007) Function of Kv1.5 channels and genetic variations of KCNA5 in patients with idiopathic pulmonary arterial hypertension. Am. J. Physiol. Cell Physiol. 292, 1837–1853 10.1152/ajpcell.00405.2006 [DOI] [PubMed] [Google Scholar]
- 19.Liu, X., Mei, M., Chen, X., Lu, Y., Dong, X., Hu, L.et al. (2019) Identification of genetic factors underlying persistent pulmonary hypertension of newborns in a cohort of Chinese neonates. Respir. Res. 20, 174 10.1186/s12931-019-1148-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Earley, S. and Brayden, J.E. (2015) Transient receptor potential channels in the vasculature. Physiol. Rev. 95, 645–690 10.1152/physrev.00026.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernandez, R.A., Wan, J., Song, S., Smith, K.A., Gu, Y., Tauseef, M.et al. (2015) Upregulated expression of STIM2, TRPC6, and orai2 contributes to the transition of pulmonary arterial smooth muscle cells from a contractile to proliferative phenotype. Am. J. Physiol. Cell Physiol. 308, C581–C593 10.1152/ajpcell.00202.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malczyk, M., Erb, A., Veith, C., Ghofrani, H.A., Schermuly, R.T., Gudermann, T.et al. (2017) The role of transient receptor potential channel 6 channels in the pulmonary vasculature. Front. Immunol. 8, 1–11 10.3389/fimmu.2017.00707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu, Y., Keller, S.H., Remillard C, V., Safrina, O., Nicholson, A., Zhang, S.L.et al. (2009) A functional single-nucleotide polymorphism in the TRPC6 gene promoter associated with idiopathic pulmonary arterial hypertension. Circulation. 119, 2313–2322 10.1161/CIRCULATIONAHA.108.782458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Southgate, L., Machado, R.D., Gräf, S. and Morrell, N.W. (2020) Molecular genetic framework underlying pulmonary arterial hypertension. Nat. Rev. Cardiol. 17, 85–95 10.1038/s41569-019-0242-x [DOI] [PubMed] [Google Scholar]
- 25.Hautefort, A., Mendes-Ferreira, P., Sabourin, J., Manaud, G., Bertero, T., Rucker-Martin, C.et al. (2019) Bmpr2 mutant rats develop pulmonary and cardiac characteristics of pulmonary arterial hypertension. Circulation 139, 932–948 10.1161/CIRCULATIONAHA.118.033744 [DOI] [PubMed] [Google Scholar]
- 26.Fantozzi, I., Platoshyn, O., Wong, A.H., Zhang, S., Remillard C, V., Furtado, M.R.et al. (2006) Bone morphogenetic protein-2 upregulates expression and function of voltage-gated K+ channels in human pulmonary artery smooth muscle cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 291, L993–L1004 10.1152/ajplung.00191.2005 [DOI] [PubMed] [Google Scholar]
- 27.Young, K.A., Ivester, C., West, J., Carr, M. and Rodman, D.M. (2006) BMP signaling controls PASMC KV channel expression in vitro and in vivo. Am. J. Physiol. Lung Cell. Mol. Physiol. 290, L841–L848 10.1152/ajplung.00158.2005 [DOI] [PubMed] [Google Scholar]
- 28.Pousada, G., Baloira, A. and Valverde, D. (2016) Complex inheritance in pulmonary arterial hypertension patients with several mutations. Sci. Rep. 6, 33570 10.1038/srep33570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bohnen, M.S., Ma, L., Zhu, N., Qi, H., McClenaghan, C., Gonzaga-Jauregui, C.et al. (2018) Loss-of-function ABCC8 mutations in pulmonary arterial hypertension. Circ. Genomic Precis. Med. 11, e002087 10.1161/CIRCGEN.118.002087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu, P.B., Beppu, H., Kawai, N., Li, E. and Blocht, K.D. (2005) Bone morphogenetic protein (BMP) type II receptor deletion reveals BMP ligand-specific gain of signaling in pulmonary artery smooth muscle cells. J. Biol. Chem. 280, 24443–24450 10.1074/jbc.M502825200 [DOI] [PubMed] [Google Scholar]
- 31.Derynck, R. and Zhang, Y.E. (2003) Smad-dependent and Smad-independent pathways in TGF-b family signalling. Nature 425, 577–584 10.1038/nature02006 [DOI] [PubMed] [Google Scholar]
- 32.Zhang, Y., Lu, W., Yang, K., Xu, L., Lai, N., Tian, L.et al. (2013) Bone morphogenetic protein 2 decreases TRPC expression, store-operated Ca2+ entry, and basal [Ca2+]i in rat distal pulmonary arterial smooth muscle cells. Am. J. Physiol. Cell Physiol. 304, 833–843 10.1152/ajpcell.00036.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang, Y., Wang, Y., Yang, K., Tian, L., Fu, X., Wang, Y.et al. (2014) BMP4 increases the expression of TRPC and basal [Ca2+]i via the p38MAPK and ERK1/2 pathways independent of BMPRII in PASMCs. PLoS ONE 9, e112695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang, X., Long, L., Southwood, M., Rudarakanchana, N., Upton, P.D., Jeffery, T.K.et al. (2005) Dysfunctional Smad signaling contributes to abnormal smooth muscle cell proliferation in familial pulmonary arterial hypertension. Circ. Res. 96, 1053–1063 10.1161/01.RES.0000166926.54293.68 [DOI] [PubMed] [Google Scholar]
- 35.Dewachter, L., Adnot, S., Guignabert, C., Tu, L., Marcos, E., Fadel, E.et al. (2009) Bone morphogenetic protein signalling in heritable versus idiopathic pulmonary hypertension. Eur. Respir. J. 34, 1100–1110 10.1183/09031936.00183008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schach, C., Firth, A.L., Xu, M., Remillard C, V., Patel, H.H., Insel, P.A.et al. (2008) REGULATION OF PULMONARY VASOCONSTRICTION BY AGONISTS AND CAVEOLAE. Exp. Lung Res. 34, 195–208 10.1080/01902140801925471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Austin, E.D., Ma, L., LeDuc, C., Rosenzweig, E.B., Borczuk, A., Phillips, J.A.et al. (2012) Whole exome sequencing to identify a novel gene (Caveolin-1) associated with human pulmonary arterial hypertension. Circ. Cardiovasc. Genet. 5, 336–343 10.1161/CIRCGENETICS.111.961888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maniatis, N.A., Shinin, V., Schraufnagel, D.E., Okada, S., Vogel, S.M., Malik, A.B.et al. (2008) Increased pulmonary vascular resistance and defective pulmonary artery filling in caveolin-1-/- mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 294, 865–873 10.1152/ajplung.00079.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang, J., Wolk, J.H., Gewitz, M.H. and Mathew, R. (2012) Caveolin-1 expression during the progression of pulmonary hypertension. Exp. Biol. Med. 237, 956–965 10.1258/ebm.2012.011382 [DOI] [PubMed] [Google Scholar]
- 40.Liu, J., Qu, C., Li, H., Zhang, Y., Sun, J., Yang, S.et al. (2016) Expression of KCNA5 protein in human mammary epithelial cell line associated with caveolin-1. J. Membr. Biol. 249, 449–457 10.1007/s00232-016-9885-2 [DOI] [PubMed] [Google Scholar]
- 41.Davies, L.M., Purves, G.I., Barrett-Jolley, R. and Dart, C. (2010) Interaction with caveolin-1 modulates vascular ATP-sensitive potassium (KATP) channel activity. J. Physiol. 588, 3255–3266 10.1113/jphysiol.2010.194779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kang, C., Hernandez, V.A. and Hu, K. (2017) Functional interaction of the two-pore domain potassium channel TASK-1 and caveolin-3. Biochim. Biophys. Acta Mol. Cell Res. 1864, 1537–1544 10.1016/j.bbamcr.2017.06.016 [DOI] [PubMed] [Google Scholar]
- 43.Murata, T., Lin, M.I., Stan R, V., Bauer, P.M., Yu, J. and Sessa, W.C. (2007) Genetic evidence supporting caveolae microdomain regulation of calcium entry in endothelial cells. J. Biol. Chem. 282, 16631–16643 10.1074/jbc.M607948200 [DOI] [PubMed] [Google Scholar]
- 44.Jiao, H.X., Mu, Y.P., Gui, L.X., Yan, F.R., Lin, D.C., Sham, J.S.K.et al. (2016) Increase in caveolae and caveolin-1 expression modulates agonist-induced contraction and store- and receptor-operated Ca2+ entry in pulmonary arteries of pulmonary hypertensive rats. Vascul. Pharmacol. 84, 55–66 10.1016/j.vph.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 45.Morris, H.E., Neves, K.B., Montezano, A.C., MacLean, M.R. and Touyz, R.M. (2019) Notch3 signalling and vascular remodelling in pulmonary arterial hypertension. Clin. Sci. 133, 2481–2498 10.1042/CS20190835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chida, A., Shintani, M., Matsushita, Y., Sato, H., Eitoku, T., Nakayama, T.et al. (2014) Mutations of notch3 in childhood pulmonary arterial hypertension. Mol. Genet. Genomic Med. 2, 229–239 10.1002/mgg3.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li, X., Zhang, X., Leathers, R., Makino, A., Huang, C., Parsa, P.et al. (2009) Notch3 signaling promotes the development of pulmonary arterial hypertension. Nat. Med. 15, 1289–1297 10.1038/nm.2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yao, J., Fang, X., Zhang, C., Yang, Y., Wang, D., Chen, Q.et al. (2021) Astragaloside IV attenuates hypoxia-induced pulmonary vascular remodeling via the Notch signaling pathway. Mol. Med. Rep. 23, 89 10.3892/mmr.2020.11726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Song, S., Babicheva, A., Zhao, T., Ayon, R.J., Rodriguez, M., Rahimi, S.et al. (2020) Notch enhances Ca2+ entry by activating calcium-sensing receptors and inhibiting voltage-gated K+ channels. Am. J. Physiol. Cell Physiol. 318, C954–C968 10.1152/ajpcell.00487.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lv, Y., Fu, L., Zhang, Z., Gu, W., Luo, X., Zhong, Y.et al. (2019) Increased expression of microRNA-206 inhibits potassium voltage-gated channel subfamily a member 5 in pulmonary arterial smooth muscle cells and is related to exaggerated pulmonary artery hypertension following intrauterine growth retardation in rats. J. Am. Heart Assoc. 8, e010456 10.1161/JAHA.118.010456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Babicheva, A., Ayon, R.J., Zhao, T., Ek Vitorin, J.F., Pohl, N.M., Yamamura, A.et al. (2020) MicroRNA-mediated downregulation of K+ channels in pulmonary arterial hypertension. Am. J. Physiol. Lung Cell. Mol. Physiol. 318, L10–L26 10.1152/ajplung.00010.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Le Ribeuz, H., Courboulin, A., Ghigna, M., Lambert, M., Hautefort, A., Humbert, M.et al. (2020) In vivo miR-138-5p inhibition alleviates monocrotaline-induced pulmonary hypertension and normalizes pulmonary KCNK3 and SLC45A3 expression. Respir. Res. 21, 186 10.1186/s12931-020-01444-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu, H.M., Jia, Y., Zhang, Y.X., Yan, J., Liao, N., Li, X.H.et al. (2019) Dysregulation of miR-135a-5p promotes the development of rat pulmonary arterial hypertension in vivo and in vitro. Acta Pharmacol. Sin. 40, 477–485 10.1038/s41401-018-0076-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Correale, M., Palmiotti, G.A., Lo Storto, M.M., Montrone, D., Foschino Barbaro, M.P., Di Biase, M.et al. (2015) HIV-associated pulmonary arterial hypertension: from bedside to the future. Eur. J. Clin. Invest. 45, 515–528 10.1111/eci.12427 [DOI] [PubMed] [Google Scholar]
- 55.Lund, A.K., Lucero, J.A., Herbert, L., Liu, Y. and Naik, J.S. (2011) Human immunodeficiency virus transgenic rats exhibit pulmonary hypertension. Am. J. Physiol. Lung Cell. Mol. Physiol. 301, L315–L326 10.1152/ajplung.00045.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tarantelli, R.A., Schweitzer, F., Simon, M.A., Vanderpool, R.R., Christman, I., Rayens, E.et al. (2018) Longitudinal evaluation of pulmonary arterial hypertension in a rhesus macaque (Macaca mulatta) model of HIV infection. Comp. Med. 68, 461–473 10.30802/AALAS-CM-18-000012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mondejar-Parreño, G., Morales-Cano, D., Barreira, B., Callejo, M., Ruiz-Cabello, X.J., Moreno, L.et al. (2018) HIV transgene expression impairs K+ channel function in the pulmonary vasculature. Am. J. Physiol. Lung Cell. Mol. Physiol. 315, L711–L723 10.1152/ajplung.00045.2018 [DOI] [PubMed] [Google Scholar]
- 58.Hsu, K., Seharaseyon, J., Dong, P., Bour, S. and Marbán, E. (2004) Mutual functional destruction of HIV-1 Vpu and host TASK-1 channel. Mol. Cell. 14, 259–267 10.1016/S1097-2765(04)00183-2 [DOI] [PubMed] [Google Scholar]
- 59.Veit, F., Pak, O., Brandes, R.P. and Weissmann, N. (2015) Hypoxia-dependent reactive oxygen species signaling in the pulmonary circulation: focus on ion channels. Antioxidants Redox Signal. 22, 537–552 10.1089/ars.2014.6234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Firth, A.L., Platoshyn, O., Brevnova, E.E., Burg, E.D., Powell, F., Haddad, G.H.et al. (2009) Hypoxia selectively inhibits KCNA5 channels in pulmonary artery smooth muscle cells. Ann. N. Y. Acad. Sci. 1177, 101–111 10.1111/j.1749-6632.2009.05040.x [DOI] [PubMed] [Google Scholar]
- 61.Smith, K.A. and Schumacker, P.T. (2019) Sensors and signals: the role of reactive oxygen species in hypoxic pulmonary vasoconstriction. J. Physiol. 597, 1033–1043 10.1113/JP275852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dunham-Snary, K.J., Hong, Z.G., Xiong, P.Y., Del Paggio, J.C., Herr, J.E., Johri, A.M.et al. (2016) A mitochondrial redox oxygen sensor in the pulmonary vasculature and ductus arteriosus. Pflugers Arch. Eur. J. Physiol. 468, 43–58 10.1007/s00424-015-1736-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mittal, M., Gu, X.Q., Pak, O., Pamenter, M.E., Haag, D., Fuchs, D.B.et al. (2012) Hypoxia induces K v channel current inhibition by increased NADPH oxidase-derived reactive oxygen species. Free Radic. Biol. Med. 52, 1033–1042 10.1016/j.freeradbiomed.2011.12.004 [DOI] [PubMed] [Google Scholar]
- 64.Buckler, K.J. (2015) TASK channels in arterial chemoreceptors and their role in oxygen and acid sensing. Pflugers Arch. Eur. J. Physiol. 467, 1013–1025 10.1007/s00424-015-1689-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nagaraj, C., Tang, B., Bálint, Z., Wygrecka, M., Hrzenjak, A., Kwapiszewska, G.et al. (2013) Src tyrosine kinase is crucial for potassium channel function in human pulmonary arteries. Eur. Respir. J. 41, 85–95 10.1183/09031936.00211811 [DOI] [PubMed] [Google Scholar]
- 66.Han, L., Song, N., Hu, X., Zhu, A., Wei, X., Liu, J.et al. (2020) Inhibition of RELM-β prevents hypoxia-induced overproliferation of human pulmonary artery smooth muscle cells by reversing PLC-mediated KCNK3 decline. Life Sci. 246, 117419 10.1016/j.lfs.2020.117419 [DOI] [PubMed] [Google Scholar]
- 67.Reyes R, V., Castillo-Galán, S., Hernandez, I., Herrera, E.A., Ebensperger, G. and Llanos, A.J. (2018) Revisiting the role of TRP, orai, and ASIC channels in the pulmonary arterial response to hypoxia. Front. Physiol. 9, 486 10.3389/fphys.2018.00486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Malczyk, M., Veith, C., Schermuly, R.T., Gudermann, T., Dietrich, A., Sommer, N.et al. (2016) NADPH oxidases—do they play a role in TRPC regulation under hypoxia? Pflugers Arch. Eur. J. Physiol. 468, 23–41 10.1007/s00424-015-1731-3 [DOI] [PubMed] [Google Scholar]
- 69.Chen, T.X., Xu, X.Y., Zhao, Z., Zhao, F.Y., Gao, Y.M., Yan, X.H.et al. (2017) Hydrogen peroxide is a critical regulator of the hypoxia-induced alterations of store-operated Ca2+entry into rat pulmonary arterial smooth muscle cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 312, L477–L487 10.1152/ajplung.00138.2016 [DOI] [PubMed] [Google Scholar]
- 70.Veith, C., Schermuly, R.T., Brandes, R.P. and Weissmann, N. (2016) Molecular mechanisms of hypoxia-inducible factor-induced pulmonary arterial smooth muscle cell alterations in pulmonary hypertension. J. Physiol. 594, 1167–1177 10.1113/JP270689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang, J., Weigand, L., Wang, W., Sylvester, J.T. and Shimoda, L.A. (2005) Chronic hypoxia inhibits Kv channel gene expression in rat distal pulmonary artery. Am. J. Physiol. Lung Cell. Mol. Physiol. 288, 1049–1058 10.1152/ajplung.00379.2004 [DOI] [PubMed] [Google Scholar]
- 72.Bonnet, S., Michelakis, E.D., Porter, C.J., Andrade-Navarro, M.A., Thébaud, B., Bonnet, S.et al. (2006) An abnormal mitochondrial-hypoxia inducible factor-1α-Kv channel pathway disrupts oxygen sensing and triggers pulmonary arterial hypertension in fawn hooded rats: similarities to human pulmonary arterial hypertension. Circulation 113, 2630–2641 10.1161/CIRCULATIONAHA.105.609008 [DOI] [PubMed] [Google Scholar]
- 73.Nagaraj, C., Tang, B., Nagy, B., Papp, R., Jain, P., Marsh, L.et al. (2016) Docosahexaenoic acid causes rapid pulmonary arterial relaxation via KCa channel-mediated hyperpolarisation in pulmonary hypertension. Eur. Respir. J. 48, 1127–1136 10.1183/13993003.01814-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Barnes, E.A., Lee, L., Barnes, S.L., Brenner, R., Alvira, C.M. and Cornfield, D.N. (2018) ß1-Subunit of the calcium-sensitive potassium channel modulates the pulmonary vascular smooth muscle cell response to hypoxia. Am. J. Physiol. Lung Cell. Mol. Physiol. 315, L265–L275 10.1152/ajplung.00060.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smith, K.A., Voiriot, G., Tang, H., Fraidenburg, D.R., Song, S., Yamamura, H.et al. (2015) Notch activation of Ca2+ signaling in the development of hypoxic pulmonary vasoconstriction and pulmonary hypertension. Am. J. Respir. Cell Mol. Biol. 53, 355–367 10.1165/rcmb.2014-0235OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang, X.Y., Mo, D., Tian, W., Liu, X.X., Zhou, Y.G., Sun, Y.et al. (2019) Inhibition of RhoA/ROCK signaling pathway ameliorates hypoxic pulmonary hypertension via HIF-1α-dependent functional TRPC channels. Toxicol. Appl. Pharmacol. 369, 60–72 10.1016/j.taap.2019.02.017 [DOI] [PubMed] [Google Scholar]
- 77.Parpaite, T., Cardouat, G., Mauroux, M., Gillibert-Duplantier, J., Robillard, P., Quignard, J.F.et al. (2016) Effect of hypoxia on TRPV1 and TRPV4 channels in rat pulmonary arterial smooth muscle cells. Pflugers Arch. Eur. J. Physiol. 468, 111–130 10.1007/s00424-015-1704-6 [DOI] [PubMed] [Google Scholar]
- 78.Plomaritas, D.R., Herbert, L.M., Yellowhair, T.R., Resta, T.C., Bosc, L.V.G., Walker, B.R.et al. (2014) Chronic hypoxia limits H2O2-induced inhibition of ASIC1-dependent store-operated calcium entry in pulmonary arterial smooth muscle. Am. J. Physiol. Lung Cell. Mol. Physiol. 307, L419–L430 10.1152/ajplung.00095.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bonnet, S., Rochefort, G., Sutendra, G., Archer, S.L., Haromy, A., Webster, L.et al. (2007) The nuclear factor of activated T cells in pulmonary arterial hypertension can be therapeutically targeted. Proc. Natl Acad. Sci. U.S.A. 104, 11418–11423 10.1073/pnas.0610467104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Orcholski, M.E., Yuan, K., Rajasingh, C., Tsai, H., Shamskhou, E.A., Dhillon, N.K.et al. (2018) Drug-induced pulmonary arterial hypertension: a primer for clinicians and scientists. Am. J. Physiol. Lung Cell. Mol. Physiol. 314, L967–L983 10.1152/ajplung.00553.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.MacLean, M.R.M. (2018) The serotonin hypothesis in pulmonary hypertension revisited: targets for novel therapies (2017 Grover conference series). Pulm. Circ. 8, 2045894018759125 10.1177/2045894018759125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Guignabert, C., Izikki, M., Tu, L.I., Li, Z., Zadigue, P., Barlier-Mur, A.M.et al. (2006) Transgenic mice overexpressing the 5-hydroxytryptamine transporter gene in smooth muscle develop pulmonary hypertension. Circ. Res. 98, 1323–1330 10.1161/01.RES.0000222546.45372.a0 [DOI] [PubMed] [Google Scholar]
- 83.Jiao, Y.R., Wang, W., Lei, P.C., Jia, H.P., Dong, J., Gou, Y.Q.et al. (2019) 5-HTT, BMPR2, EDN1, ENG, KCNA5 gene polymorphisms and susceptibility to pulmonary arterial hypertension: a meta-analysis. Gene 680, 34–42 10.1016/j.gene.2018.09.020 [DOI] [PubMed] [Google Scholar]
- 84.Ducret, T., Guibert, C., Marthan, R. and Savineau, J.P. (2008) Serotonin-induced activation of TRPV4-like current in rat intrapulmonary arterial smooth muscle cells. Cell Calcium 43, 315–323 10.1016/j.ceca.2007.05.018 [DOI] [PubMed] [Google Scholar]
- 85.Han, J., Tian, H., Liu, Y. and Fan, F. (2019) Sarpogrelate attenuates pulmonary arterial hypertension via calcium/calcineurin axis. Front. Biosci. 24, 607–615 10.2741/4739 [DOI] [PubMed] [Google Scholar]
- 86.Sung, D.J., Noh, H.J., Kim, J.G., Park, S.W., Kim, B., Cho, H.et al. (2013) Serotonin contracts the rat mesenteric artery by inhibiting 4-aminopyridine-sensitive Kv channels via the 5-HT2A receptor and Src tyrosine kinase. Exp. Mol. Med. 45, e67 10.1038/emm.2013.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Genet, N., Billaud, M., Rossignol, R., Dubois, M., Gillibert-Duplantier, J., Isakson, B.E.et al. (2017) Signaling pathways linked to serotonin-induced superoxide anion production: a physiological role for mitochondria in pulmonary arteries. Front. Physiol. 8, 76 10.3389/fphys.2017.00076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cogolludo, A., Moreno, L., Lodi, F., Frazziano, G., Cobeño, L., Tamargo, J.et al. (2006) Serotonin inhibits voltage-gated K+ currents in pulmonary artery smooth muscle cells: role of 5-HT2A receptors, caveolin-1, and KV1.5 channel internalization. Circ. Res. 98, 931–938 10.1161/01.RES.0000216858.04599.e1 [DOI] [PubMed] [Google Scholar]
- 89.Kurakula, K., Smolders, V.F.E.D., Tura-Ceide, O., Wouter Jukema, J., Quax, P.H.A. and Goumans, M.J. (2021) Endothelial dysfunction in pulmonary hypertension: cause or consequence? Biomedicines 9, 57 10.3390/biomedicines9010057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Manoury, B., Idres, S., Leblais, V. and Fischmeister, R. (2020) Ion channels as effectors of cyclic nucleotide pathways: functional relevance for arterial tone regulation. Pharmacol. Ther. 209, 107499 10.1016/j.pharmthera.2020.107499 [DOI] [PubMed] [Google Scholar]
- 91.Inoue, M., Matsuoka, H., Harada, K., Mugishima, G. and Kameyama, M. (2020) TASK channels: channelopathies, trafficking, and receptor-mediated inhibition. Pflugers Arch. Eur. J. Physiol. 472, 911–922 10.1007/s00424-020-02403-3 [DOI] [PubMed] [Google Scholar]
- 92.Seyler, C., Duthil-Straub, E., Zitron, E., Gierten, J., Scholz, E.P., Fink, R.H.A.et al. (2012) TASK1 (K 2P3.1) K+ channel inhibition by endothelin-1 is mediated through Rho kinase-dependent phosphorylation. Br. J. Pharmacol. 165, 1467–1475 10.1111/j.1476-5381.2011.01626.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cunningham, K.P., Holden, R.G., Escribano-Subias, P.M., Cogolludo, A., Veale, E.L. and Mathie, A. (2019) Characterization and regulation of wild-type and mutant TASK-1 two pore domain potassium channels indicated in pulmonary arterial hypertension. J. Physiol. 597, 1087–1101 10.1113/JP277275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Olschewski, A., Li, Y., Tang, B., Hanze, J., Eul, B., Bohle, R.M.et al. (2006) Impact of TASK-1 in human pulmonary artery smooth muscle cells. Circ. Res. 98, 1072–1080 10.1161/01.RES.0000219677.12988.e9 [DOI] [PubMed] [Google Scholar]
- 95.Callejo, M., Mondejar-Parreño, G., Morales-Cano, D., Barreira, B., Esquivel-Ruiz, S., Olivencia, M.A.et al. (2020) Vitamin D deficiency downregulates TASK-1 channels and induces pulmonary vascular dysfunction. Am. J. Physiol. Lung Cell. Mol. Physiol. 319, L627–L640 10.1152/ajplung.00475.2019 [DOI] [PubMed] [Google Scholar]
- 96.Mondéjar-Parreño, G., Barreira, B., Callejo, M., Morales-Cano, D., Barrese, V., Esquivel-Ruiz, S.et al. (2020) Uncovered contribution of Kv7 channels to pulmonary vascular tone in pulmonary arterial hypertension. Hypertension 76, 1134–1146 10.1161/HYPERTENSIONAHA.120.15221 [DOI] [PubMed] [Google Scholar]
- 97.Liao, J., Lu, W., Chen, Y., Duan, X., Zhang, C., Luo, X.et al. (2021) Upregulation of Piezo1 (Piezo type mechanosensitive ion channel component 1) enhances the intracellular free calcium in pulmonary arterial smooth muscle cells from idiopathic pulmonary arterial hypertension patients. Hypertension 77, 1974–1989 10.1161/HYPERTENSIONAHA.120.16629 [DOI] [PubMed] [Google Scholar]
- 98.Papp, R., Nagaraj, C., Zabini, D., Nagy, B.M., Lengyel, M., Skofic Maurer, D.et al. (2019) Targeting TMEM16A to reverse vasoconstriction and remodelling in idiopathic pulmonary arterial hypertension. Eur. Respir. J. 53, 1800965 10.1183/13993003.00965-2018 [DOI] [PubMed] [Google Scholar]
- 99.Ferraz, A.P., Seara, F.A.C., Baptista, E.F., Barenco, T.S., Sottani, T.B.B., Souza, N.S.C.et al. (2021) BKCa channel activation attenuates the pathophysiological progression of monocrotaline-induced pulmonary arterial hypertension in Wistar rats. Cardiovasc. Drugs Ther. 35, 719–732 10.1007/s10557-020-07115-5 [DOI] [PubMed] [Google Scholar]
- 100.Chen, Y., Lu, W., Yang, K., Duan, X., Li, M., Chen, X.et al. (2020) Tetramethylpyrazine: a promising drug for the treatment of pulmonary hypertension. Br. J. Pharmacol. 177, 2743–2764 10.1111/bph.15000 [DOI] [PMC free article] [PubMed] [Google Scholar]