Abstract
UN-Habitat identified the present COVID-19 pandemic as ‘city-centric’. In India, more than 50% of the total cases were documented in megacities and million-plus cities. The slums of cities are the most vulnerable due to its unhygienic environment and high population density that requires an urgent implementation of public healthcare measures. This study aims to examine habitat vulnerability in slum areas to COVID-19 in India using principal component analysis and Fuzzy AHP based technique to develop slum vulnerability index to COVID-19 (SVIcovid-19). Four slum vulnerability groups (i.e. principal components) were retained with eigen-values greater than 1 based on Kaiser criterion - poor slum household status; lack of social distance maintenance; high concentrations of slum population and towns and mobility of the households. This study also mapped composite SVIcovid-19 on the basis of PCA and Fuzzy AHP method at the state level for a better understanding of spatial variations. The result shows that slums located in the eastern and central parts of India (particularly Uttar Pradesh, Bihar, Jharkhand, Odisha, West Bengal) were more vulnerable to COVID-19 transmission due to lack of availability as well as accessibility to the basic services and amenities to slum dwellers. Thus, the findings of the study may not only help to understand the habitat vulnerability in slum areas to COVID-19 but it will also teach a lesson to implement effective policies for enhancing the quality of slum households (HHs) and to reduce the health risk from any infectious disease in future.
Keywords: COVID-19, Habitat vulnerability, Principal component analysis, Fuzzy AHP, Accessibility
1. Introduction
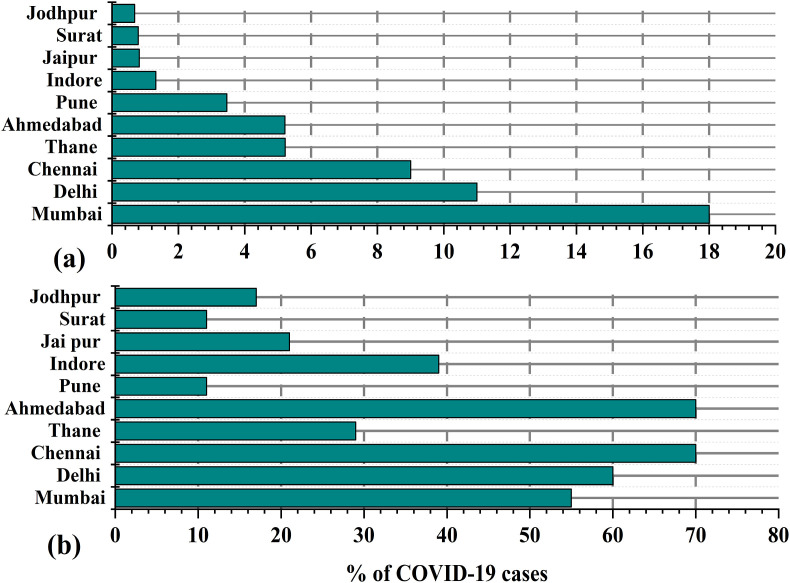
From the global scenario of the COVID-19 pandemic, it has been observed that the cities are more vulnerable to COVID-19 in terms of both confirmed cases and deaths. More than 95% of the total COVID-19 cases were recorded from more than 1430 cities across the world [1]. In India, the big cities such as Mumbai, Delhi, Kolkata, Ahmedabad, Indore, Pune, Jaipur, Thane, Hyderabad, Chennai and Agra are the worst hit by COVID-19 cases [2]. More than half of the total COVID-19 cases were recorded from these 10 cities in India [3]. This is surely a big challenge to public health because once it starts spreading in slum areas; it will be out of control. Therefore, the slum areas of the cities are likely to be more vulnerable to COVID-19 due to poor infrastructure, unavailability of medical equipment and high population density. For example, Asia's largest slum Dharavi in Mumbai recorded more than 1400 COVID-19 cases in May 2020 [4]. This clearly indicates how much vulnerable the slum areas are, to COVID-19 in India. It was mentioned earlier that cities across the world are more vulnerable to COVID-19. As of the date of 10th June, 3.5 million confirmed cases were recorded from New York with more than 30000 deaths (The New York Times, 2020). In Unite Nations, more than one-fourth of the total cases were recorded from London [5]. In India too, more than 50% of the total COVID-19 confirm cases were reported from ten large cities (Fig. 1 ). The households living in cities are more vulnerable due to poor living conditions and deprivation [6].
Fig. 1.
Scenario of COVID-19 status in India across 10 severely affected cities (a) % of COVID-19 cases to country and (b) % of COVID-19 cases to state (Source: Business insider, 2020).
With the rapid increase of population in cities of developing countries, the utmost importance is being provided to the availability as well as accessibility to basic services and amenities and provisions of infrastructure in cities. The provision of infrastructure is not only alleviating poverty but promote economic growth and environmental sustainability [7,8]. As an estimate, it was reported that the slum population will increase by about 2 billion by 2030 with the highest in developing countries [9]. As per the Census of India [10]; about 93 million population lives in slum areas. Indian slums are characterized by inadequate infrastructural facilities, poor housing conditions and poor neighborhood status [11]. Apart from these, in many research studies, it was well recognized that the accessibility to the basic services and amenities was limited to the slum households [8,12]. Thus from the previous research studies, it was cleared that the access to amenities like: water, sanitation facilities, housings, etc for the slum population is limited. Therefore, it is essential to examine how far the Indian slums are vulnerable to respiratory disease with special reference to COVID-19. According to the census of India [10]; Tamil Nadu has the maximum number of slum reporting towns (507) followed by Madhya Pradesh (307), Uttar Pradesh (293). Karnataka (206) and Maharashtra (189) respectively. More than 55% of the total slum reporting towns was located in these five states. The highest proportion of slum population lives in Maharashtra (18%) followed by Andhra Pradesh (15.6%), West Bengal (10%), Uttar Pradesh (9.5%), Tamil Nadu (8.92%) and Madhya Pradesh (8.75%) respectively. The current scenario of COVID-19 cases showed that maximum numbers of COVID-19 cases as well as deaths were recorded from these states. The major cities of these states became the major COVID-19 hotspot of the country. Thus a common research question that arises in this context is-how far the Indian slums are vulnerable to the COVID-19 transmission? How the living conditions of the slum dwellers may be vulnerable to COVID-19 transmission in the slum areas? To address these research questions, a SVIcovid-19 has been developed to understand the vulnerability of the slum population in India across states. The findings of the study have immense scope to understand how far the Indian slums are vulnerable to COVID-19. Apart from this, this study will surely assist planners and policy makers to implement strategies to cope with respiratory disease in the future. The top 10 COVID-19 affected cities in India are presented in Fig. 1. During the second wave of COVID-19, large cities such as Mumbai, Delhi, Pune, Thane became the major hotspot cities in India.
The word slum was firstly used in London to mean “room of low repute” and since then this word was widely applied in various kinds of literature [13]. As per the definition of UN-HABITAT [13]; slums were defined as the social, physical as well as spatial aspects of poverty. As per the revised definition of UN-HABITAT [14]; the slum was defined as “one or a group of individuals living under the same roof in an urban area, lacking in one or more of the following five amenities: 1) Durable housing (a permanent structure providing protection from extreme climatic conditions); 2) Sufficient living area (no more than three people sharing a room); 3) Access to improved water (water that is sufficient, affordable, and can be obtained without extreme effort); 4) Access to improved sanitation facilities (a private toilet, or a public one shared with a reasonable number of people), and 5) Secure tenure (de facto or de jure secure tenure status and protection against forced eviction)”. Thus, slums area is characterized by limited availability as well as accessibility to basic services and amenities such as water supply, sanitation, drainage system and electricity that largely affect the quality of life and well-being of the slum dwellers [[15], [16], [17], [18], [19]]. In India, slums were defined as” the areas having inadequate infrastructure, poor housing conditions, poor neighborhood condition and limited accessibility to WaSH (water, sanitation and hygiene) provision respectively [11,[15], [16], [17],20]. Thus, limited availability as well as accessibility to basic services and amenities is the main reason for vulnerability and slums were considered as one of the vulnerable habitat to transmission of COVID-19 [21,22]. According to UN-HABITAT [1]; “The impact of Covid-19 will be most devastating in poor and densely populated urban areas, especially for the one billion people living in informal settlements and slums worldwide”. Now the question is-why slums are vulnerable to COVID-19 transmission? Let's start with few examples, then it would be clear. Example 1: According to Ray [23]; more than 600 people collect water from a community tape in Kolkata (Kankulia Road slum and Panchanantala). Thus, only from a person, COVID-19 can transit others even spread to all slums areas. The slum people are dependent on community taps due to the lack of water facilities within the premises. Example 2: the slum people are socio-economically poor and not aware due to the lack of educational knowledge (illiteracy). Thus, it is very difficult for them to maintain guidelines (such as the usage of masks, washing hands with sanitizers, and frequent wash of hands with soaps) to curb COVID-19 transmission. Maintenance guidelines become more difficult as they are dependent on the informal sector and day-to-day earnings for their livelihood [24]. Example 3: According to Bag et al. [25]; about 70% of the slum dwellers were dependent on public toilet facilities across three megacities namely Kolkata Delhi and Mumbai. Thus, slum dwellers are highly exposed to COVID-19 transmission. Therefore, from the above evidence, it can be easily understood that slums in India are highly vulnerable to COVID-19 transmission.
Although the global cities are severely affected by this deadly disease but particularly the cities of the global south are more vulnerable due to high population density and limited access to affordable services [26]. Recently UN-Habitat [1]; published a report stating that the cities of global (add something) are the most vulnerable due to rapid urbanization as well as large concentrations of slum population. Recently, it was well documented that the areas (like slums) with high population are more vulnerable to COVID-19 transmission [6,[15], [16], [17],[27], [28], [29], [30]]. Even after a quick review of the previous works of literature, few research gaps were identified that inspired us to conduct this study over slum vulnerability in India. Firstly, most of the studies revealed that the cities were more vulnerable in India [6,31]. Secondly, the cities were the major COVID-19 hotspot across the world. But till now no studies were performed to examine the slum vulnerability in response to COVID-19 transmission. Apart from this, the second wave of COVID-19 has become dangerous in comparison to 2020. There are no beds in hospitals, people are dying without oxygen. In the second wave of COVID-19, the implementation of nationwide lockdown may be a great challenge to the government. Therefore, maintenance of social distancing, wearing masks are urgently required. Thus, slums may be the COVID-19 hotspots during the second wave of COVID-19 due to a high population density, lack of awareness and low accessibility to the basic services and amenties, respectively.
2. Materials and methods
2.1. Study area
This study focuses on the assessment of habitat vulnerability in slum areas across the states in India (Fig. 2 ). In India, the slums located in cities are vulnerable to multiple disasters such as floods, malaria, fires and the recent pandemic (COVID-19) respectively. The urban people residing in slum areas are socially, economically and physically most vulnerable than other people of the urban environment. According to the Census of India [10]; more than 80% of the total slum population was concentrated over nine states only. These states were- Tamilnadu, Madhya Pradesh, Uttar Pradesh, Karnataka, Andhra Pradesh, West Bengal, Maharastra, Rajasthan and Gujrat respectively.
Fig. 2.
Location map of the study area (State of India).
2.2. Data source
In this study, 12 variables have been selected which are directly or indirectly related to COVID-19 transmission in slum areas. The variables have been discussed under four broad heads i.e. (i) % of slum population concentrations and the number of slum reported towns (ii) maintenance of social distance (iii) households (HH) status and (iv) mobility of slum HHs (Table 1 ). State-wise data have been collected from primary Census abstract (2011) and house listing and housing's primary census abstract (2011). The data on COVID-19 to support the study were collected from various secondary sources such as newspapers (such as Times of India, Hindustan Times), https://www.covid19india.org/and Ministry of Family and Health Welfare, Government of India.
Table 1.
Indicators selected for construction t of SVIcovid-19.
| Dimensions | Variables | Descriptions | Relationship with COVID-19 |
|---|---|---|---|
| Slum population concentration and number of towns | % of Slum Population in Urban Population of state | % of slum population to the total urban population of the respective state | Positive |
| % of State Slum Population in Total Slum Population of India | % of slum population to the total urban population of the respective India | Positive | |
| Slum Reported Towns | Total number of slum reported towns as per as Census of India [10] | Positive | |
| Maintenance of social distance | No exclusive room | % of slum HHs having no separate living rooms | Positive |
| One room | % of slum HHs having only single dwelling room | Positive | |
| HHs status | Household Size (9+) | Total number of HHs members living in slums area | Positive |
| Rented | % of slum HHs residing on rent | Positive | |
| Illiteracy HHs | % of illiterate slum population living in slums areas | Positive | |
| Mobility of HHs | No Bathroom facility | % of slum HHs having no bathroom facility within premises | Positive |
| No drainage | % of HHs having no drainage facilities | Positive | |
| Location of Drinking Water (away from house) | % of HHs having no drinking water facilities within premises | Positive | |
| Availability of Latrine Facility (open) | % of HHs having open larine facilities | Positive |
2.3. Rationale of selection indicators
In this study, 12 indicators have been selected from four major domains namely- (i) % of slum population concentrations and the number of slum reported towns (ii) maintenance of social distance (iii) Households status and (iv)mobility of slum HHs, respectively. (i) Indicators related to slum population concentrations (%) and the number of slum reported towns: three indicators have been selected under this criteria-concentration of slum population to the total urban population of state and country (%). Slums are characterized by high population density and lack of availability as well as accessibility to basic services and amenities. Thus higher concentrations of slum population increase the risk of health hazards in urban areas [[32], [33], [34], [35]]. In recent studies, it was also well documented that the urban slums are more vulnerable to COVID-19 transmission [6,[15], [16], [17],27]. (ii) Indicators related to maintenance of social distance: Maintenance of social distance is considered as one of the key factors in controlling infectious diseases as well as COVID-19 transmission [[36], [37], [38], [39], [40]]. In slum areas, slum households has very limited access to exclusive rooms. In this case, it is very difficult to maintain the social distance that increases the risk of COVID-19 transmission. Even home quarantine for those slums HHs having no exclusive room or single room is not possible. Thus, these slums HHs are more vulnerable to COVID-19 transmission. (iii) Indicators related to slum HH status: The transmission of infectious diseases are largely determined by HHs characteristics (such as HHs size, housing conditions, illiteracy rate of slum HHs, rented HHs, etc). There are close linkages between respiratory diseases and slum household's status [33,35,41]. For example, to reduce the transmission of COVID-19 one must have to be very conscious regarding the severity of COVID-19. People must follow the guidelines suggested (such as the usage of masks, washing hands frequently, maintaining social distance). Thus, people ignore the proper guidelines related to the reduction of COVID-19 transmission due to a lack of proper health science knowledge and education [42,43]. (iv) Indicators related to the mobility of slum HHs: The most severely affected countries of the world imposed lockdown to reduce the rapid transmission of COVID-19 and the motto of lockdown was “stay home, stay safe”. But the slums HHs having no drinking water or bathroom facilities, is it possible to stay at home? How they would be safe? In many previous studies in India, it was well documented that there is a lack of availability, accessibility as well as inequality of these basic services and amenities in slum areas [44,45]. Thus, limited access to these services makes slum HHs more vulnerable to infectious diseases and most of the slum HHs are dependent on community toilets or water taps as well. The mobility of people increases the risk of COVID-19 transmission [[46], [47], [48], [49]]. The households having no drainage facilities are more vulnerable due to a poor living environment and therefore, are susceptible to a higher exposure to COVID-19 [43]. Thus, from the overall analysis, it was well recognized that the selected indicators used in this study are directly or indirectly linked with COVID-19 transmission in slum areas.
2.4. Methodology
In this study, a composite vulnerability approach has been adopted to map SVIcovid-19 across the states in India. Indicators related to COVID-19 vulnerability have been calculated for each state in India. By aggregating four domains, the cumulative COVID-19 slum vulnerability index has been developed to identify the states from highest to lowest vulnerability to COVID-19.
2.4.1. Normalization of the indicators
Normalization of indicators is important for multivariate statistical analysis due to the large and small range of variance [50]. The indicators selected to measure SVIcovid-19; different indicators with different measuring units have been used. Therefore, it is essential to make them unit-free [[15], [16], [17],51]. A similar kind of approach has been used for the human development index (HDI) and life expectancy [52,53]. The normalization of indicators has been performed using the following equation:
| (1) |
| (2) |
Where, is the observed value of indicator i; indicate the minimum and maximum value within the same array respectively. On the other hand, is the observed value of indicator i; indicate the minimum and maximum value within the same array respectively.
2.5. PCA based slum vulnerability index to COVID-19 (SVIcovid-19)
PCA was conducted to reduce the factor after extracting indicators and standardizing the value of selected indicators. COVID-19 vulnerability data from all the states have been normalized before statistical analysis. In this study, a composite COVID-19 vulnerability index in slum areas has been devised using PCA. PCA is a multivariate statistical technique and this technique is used to find out the principal factors or variable that explains this phenomena.
All the indicators are generally used to examine the vulnerability of any phenomena are not equally important i.e. there are few factors that trigger the vulnerability. In this context, we must consider the maximum number of factors and select the most effective ones. For this, PCA multivariate technique is used to obtain the most significant factors. For each state, the value of each indicator has been derived by a standardized value multiplied by corresponding factor loading. PCA techniques were widely used in previous studies for vulnerability assessment such as climatic vulnerability [50,[54], [55], [56], [57]]. For retention of principal components, several statistical tests are performed to find out the suitability of representative data in the case of PCA analysis. These are (i) Kaisar-Meyer-Olkin (KMO) test- KMO is basically used to measure sampling adequacy and the value of KMO ranges from 0 to 1. The KMO value > 0.50 is considered as suitable for PCA analysis. (ii) Bartlett's test – Bartlett's test is basically used to assess the significance level (‘p’ value < 0.5 is considered as significant). In this study, the PCA method was used for several potential advantages firstly, PCA can aggregate spatially explicit variables, more particularly incommensurable variables and reduces the trade of richness of information with communicability (Abson et a., 2012). Secondly, PCA plays a significant role to provide flexibility in reducing data through subjective choice PCs [58]. Thirdly and more importantly, PCA can be associated to original variables through factor loading of the principal components. In the case of habitat vulnerability mapping in slum areas, PCA scores related to multiple variables were conceptualized. The number of habitat vulnerability variables can be generated by accounting substantial proportion of variability within the original data. In this study, the spatial maps were developed for the variables as well as PCA and Fuzzy-AHP mappings. The spatial maps were developed using IDW techniques in the ArcGIS environment.
2.6. Fuzzy AHP based slum vulnerability index (SVI)
For the construction of a composite index, not all indicators are equally important. Therefore, the weight for each indicator must be provided for any modeling [31]. In this context, AHP is a very efficient method to calculate the weight for each indicator to solve complex decisions [59]. AHP method was widely used as multi-criteria decision making (MCDM) in different fields because of its feasibility and it highly assists the decision-making framework [60]. Thus, the AHP method is held to integrate the ‘domain-related knowledge’ in the model [60]. Thus, because of flexibility, the AHP method was widely used for vulnerability assessment such as urban vulnerability [6], climate change vulnerability [61], ecological health assessment [[15], [16], [17]] respectively. Apart from this, AHP was also used in health science such as ZIKA and dengue risk assessment [62,63]. These previous pieces of literature inspired us to implement the AHP method to assess slum vulnerability mapping. In this method, the input variables are provided weight on the basis of relative importance through pair-wise comparison based on which weights are computed [59,[64], [65], [66]]. In this study, for the construction of the slum vulnerability index, the weights for each variable have been calculated following Saaty [59]. The corresponding weights of variables have been computed by dividing the cell values and sum of column values of the pair-wise comparison matrix (Table 2, Table 3 ). For the validation of the weights, the consistency ratio (CR) has been calculated. The weights of the thematic layers have been normalized associated with maximum eigen values. The value of CR < 0.1 indicates the reliability of the analysis. The following equations have been used to calculate pair-wise comparison and CR, respectively.
| (3) |
Where
| (4) |
Table 2.
Relative weight for each variable of SVI generated through AHP method.
| Variables | Weight | |
|---|---|---|
| 1 | % of Slum Population in Urban Population | 0.116 |
| 2 | % of State Slum Population in Total Slum Population | 0.059 |
| 3 | Slum Reported Towns | 0.033 |
| 4 | No exclusive room | 0.083 |
| 5 | One room | 0.071 |
| 6 | Household Size (9+) | 0.099 |
| 7 | Rented | 0.041 |
| 8 | Illiteracy HHs | 0.136 |
| 9 | No Bathroom facility | 0.144 |
| 10 | No drainage | 0.062 |
| 11 | Location of Drinking Water (away from house) | 0.038 |
| 12 | Availability of Latrine Facility (open) | 0.077 |
Table 3.
The weight of the variables are based on the principal eigenvector of the decision matrix.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 4.00 | 3.00 | 0.50 | 1.00 | 3.00 | 3.00 | 2.00 | 0.33 | 2.00 | 2.00 | 1.00 |
| 2 | 0.25 | 1 | 2.00 | 0.33 | 0.33 | 1.00 | 2.00 | 0.50 | 0.50 | 1.00 | 2.00 | 2.00 |
| 3 | 0.33 | 0.50 | 1 | 0.50 | 0.33 | 0.50 | 0.50 | 0.33 | 0.50 | 0.50 | 0.50 | 0.50 |
| 4 | 2.00 | 3.00 | 2.00 | 1 | 2.00 | 0.33 | 3.00 | 0.33 | 0.33 | 1.00 | 2.00 | 0.50 |
| 5 | 1.00 | 3.00 | 3.00 | 0.50 | 1 | 0.50 | 2.00 | 0.50 | 0.50 | 0.50 | 1.00 | 2.00 |
| 6 | 0.33 | 1.00 | 2.00 | 3.00 | 2.00 | 1 | 3.00 | 0.50 | 0.33 | 2.00 | 2.00 | 3.00 |
| 7 | 0.33 | 0.50 | 2.00 | 0.33 | 0.50 | 0.33 | 1 | 0.50 | 0.33 | 0.50 | 2.00 | 0.33 |
| 8 | 0.50 | 2.00 | 3.00 | 3.00 | 2.00 | 2.00 | 2.00 | 1 | 3.00 | 2.00 | 3.00 | 2.00 |
| 9 | 3.00 | 2.00 | 2.00 | 3.00 | 2.00 | 3.00 | 3.00 | 0.33 | 1 | 3.00 | 3.00 | 2.00 |
| 10 | 0.50 | 1.00 | 2.00 | 1.00 | 2.00 | 0.50 | 2.00 | 0.50 | 0.33 | 1 | 2.00 | 0.33 |
| 11 | 0.50 | 0.50 | 2.00 | 0.50 | 1.00 | 0.50 | 0.50 | 0.33 | 0.33 | 0.50 | 1 | 0.50 |
| 12 | 1.00 | 0.50 | 2.00 | 2.00 | 0.50 | 0.33 | 3.00 | 0.50 | 0.50 | 3.00 | 2.00 | 1 |
Consistency ratio (CR) = 0.07.
The consistency ratio is applied using the following equation:
| (5) |
where RI denotes random index and CI refers to the consistency index. CI can be calculated using the following equation:
| (6) |
where, λ indicates the largest eigen value and it can be computed from the matrix and n is the total number of thematic layers, respectively.
3. Result and discussion
3.1. Availability and accessibility of basic services to the slum households
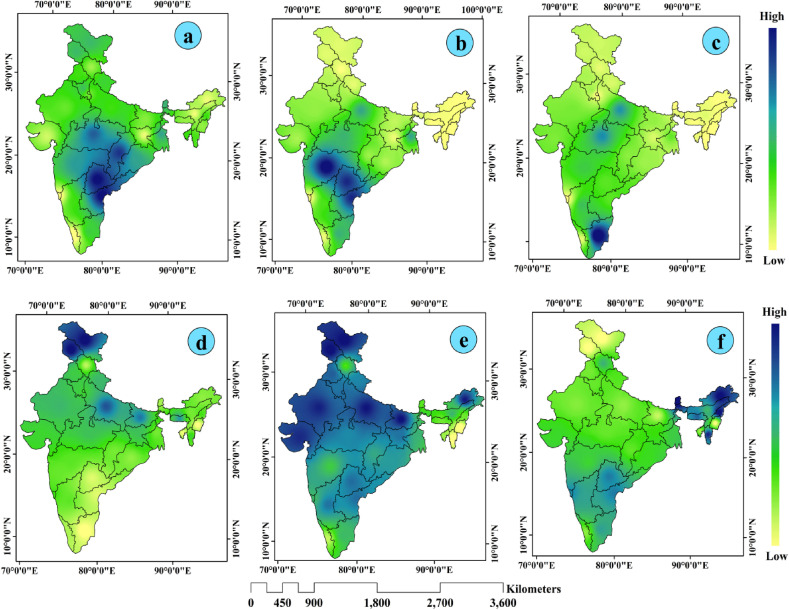
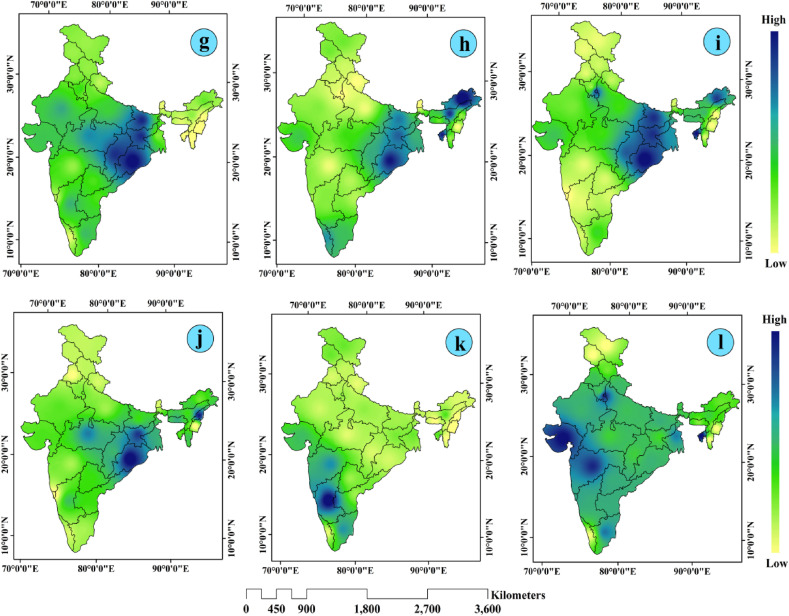
The slum population is more vulnerable as compared to the other communities of the city due to the lack or inadequacies of basic amenities and services. From the overall result of slum vulnerability, it was found that the central, western and some eastern states are more vulnerable to COVID-19 as compared to the other states of India. More particularly, the slum dwellers living in states like Maharashtra, Tamil Nadu, Karnataka, Madhya Pradesh, West Bengal, Uttar Pradesh, Bihar, Chhattisgarh were more vulnerable. More than 70% of the total states of the country fall under the category of very high vulnerability and high vulnerability categories. There were inadequacies of basic services and amenities that make them more vulnerable living in very high and high vulnerable states respectively. For example, in Gujrat and Maharashtra, more than 60% of the slum households had only one dwelling room. In this situation-is home quarantine is possible for any suspected COVID-19 person? In Odisha, about 50% of the slum households had no bathroom facility within premises followed by Bihar (43.25%) and Jharkhand (43.07%) respectively. In Maharashtra, more than 60% of the total slum households had no latrine facility followed by Odisha (51.85%) Chhattisgarh (51.33%), Jharkhand (47.31%) respectively. From the overall analysis, it was clear that there is a huge lack of basic services and amenities and inadequacies of equipment may increase the risk of COVID-19 infection and make them more vulnerable to COVID-19 (Fig. 4, Fig. 5). The result also showed that the slum dwellers living in COVID-19 hotspot states are likely to be exposed to this vulnerability due to the lack of adequate equipment. Fig. 3 showed the accessibility to basic services across four large megacities in slum areas. Table 4 shows the descriptive statistics of selected variables used in this study
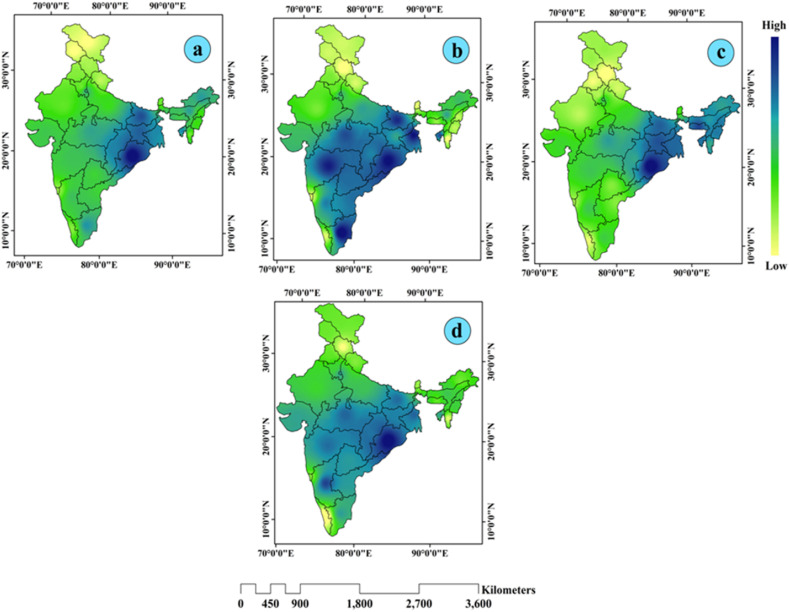
Fig. 4.
Indicators selected for the study (a) % of slum population in respect to state (b) % of slum population in respect to country (c) number of reported slum towns (d) households size (e) illiterate slum population and (f) slum rented households.
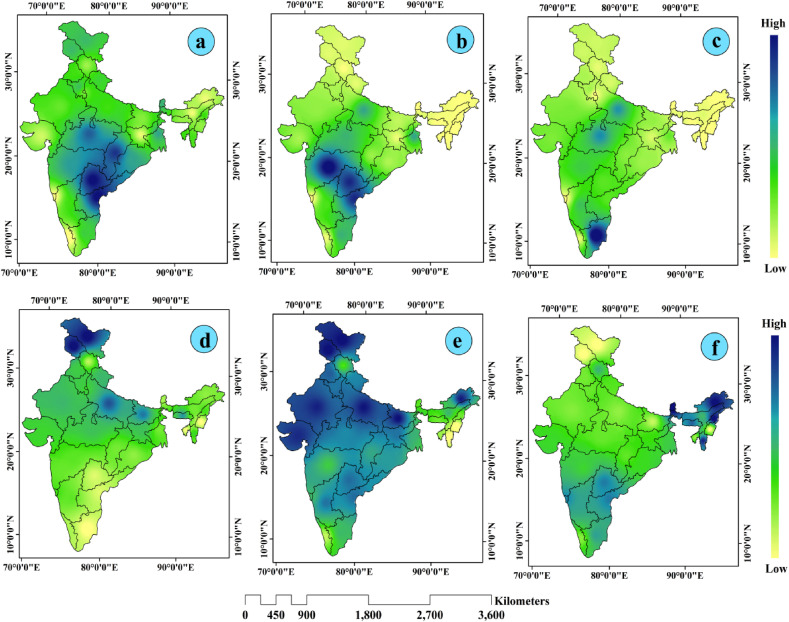
Fig. 5.
Indicators selected for the study (g) % of slum households having open toilet (h) % of slum households having no drainage (i) % of slum households having no bathroom (j) % of slum households having no water facility within premises (k) % of slum households having no exclusive rooms and (l) % of households having one dwelling room.
Fig. 3.
Accessibility to basic services (%) of slum population across four megacities (a) HHs by persons per room used for sleeping (b) HHs by type of toilet facility (c) HHs by location of water source and (d) HHs access to water and soap (Source: National Family Health Survey-4, 2015–2016).
Table 4.
Descriptive statistics of selected variables used in this study.
| Selected variables | N | Mean | Max | Min | SD | CV |
|---|---|---|---|---|---|---|
| % of Slum Population in Urban Population of state | 12 | 14.88 | 36.10 | 1.30 | 8.59 | 57.73 |
| % of State Slum Population in Total Slum Population of India | 3.62 | 18.09 | 0.02 | 4.93 | 136.32 | |
| Slum Reported Towns | 92 | 507 | 1 | 116.38 | 126.01 | |
| No exclusive room | 3.13 | 11.75 | 0.73 | 2.53 | 80.81 | |
| One room | 37.28 | 67.00 | 12.38 | 13.71 | 36.78 | |
| Household Size (9+) | 4.86 | 6.40 | 4.00 | 0.54 | 11.18 | |
| Rented | 27.85 | 63.78 | 2.91 | 15.96 | 57.33 | |
| Illiteracy HHs | 79.29 | 97.82 | 67.72 | 8.15 | 10.27 | |
| No Bathroom facility | 21.91 | 49.66 | 5.48 | 14.66 | 66.91 | |
| No drainage | 24.13 | 62.32 | 4.88 | 16.77 | 69.49 | |
| Location of Drinking Water (away from house) | 11.53 | 29.29 | 2.15 | 6.94 | 60.17 | |
| Availability of Latrine Facility (open) | 16.63 | 48.34 | 0.49 | 13.79 | 82.90 |
3.2. PCA based slum vulnerability index to COVID-19 (SVIcovid-19)
In this study, four principal components were retained from 12 selected indicators for slum vulnerability assessment to COVID-19 in India. Among all the principal components, the first component accounted for the highest percentage of variance (24.34%) followed by the second principal component (20.52%) respectively. The details of loading for each retained principal factor were presented in Table 5 . As per the result, it was recorded that the first principal component was highest loaded on household size, rented households, dilapidated households, illiteracy of households and availability of open latrine facility. The second principal component was given heaviest load on % of slum population (in respect to India), the number of slum reported towns, households having no drainage facility and households having no drinking water facility within premises. The third principal component had the heaviest load on % of slum population (in respect to state), households having only one room, % of slum population (in respect to state) and households having no latrine facility within premises. The last i.e. fourth principal component was heavily loaded on those indicators whatever loads were given on principal component first and third (household size and illiteracy of households-first PC; % of slum population (in respect to India, % of slum population (in respect to state and number of slum reported towns- Third PC respectively). In this analysis, four dimensions of slum vulnerability to COVID-19 were identified on the basis of loadings of twelve variables. These four aspects of slum vulnerability to COVID-19 were termed as “slum household status” (PC1), “social distance” (PC2), “slum population and towns” (PC3) and “mobility of households” (PC4) respectively. In this analysis, four components have been extracted from twelve variables. These four components explained more than 70% of the total cumulative variance in slum vulnerability to COVID-19 in India.
Table 5.
Total variance explained by 12 selected variables.
| Variables | Initial Eigen-values |
Extraction Sums of Squared Loadings |
||||
|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| % of Slum Population in Urban Population of state | 3.165 | 24.344 | 24.344 | 3.165 | 24.344 | 24.344 |
| % of State Slum Population in Total Slum Population of India | 2.668 | 20.522 | 44.866 | 2.668 | 20.522 | 44.866 |
| Slum Reported Towns | 1.941 | 14.931 | 59.797 | 1.941 | 14.931 | 59.797 |
| No exclusive room | 1.558 | 11.984 | 71.781 | 1.558 | 11.984 | 71.781 |
| One room | 0.913 | 7.021 | 78.802 | |||
| Household Size (9+) | 0.607 | 4.672 | 83.474 | |||
| Rented | 0.578 | 4.442 | 87.917 | |||
| Illiteracy HHs | 0.382 | 2.939 | 94.284 | |||
| No Bathroom facility | 0.306 | 2.354 | 96.637 | |||
| No drainage | 0.233 | 1.794 | 98.431 | |||
| Location of Drinking Water (away from house) | 0.152 | 1.166 | 99.597 | |||
| Availability of Latrine Facility (open) | 0.052 | 0.403 | 100.000 | |||
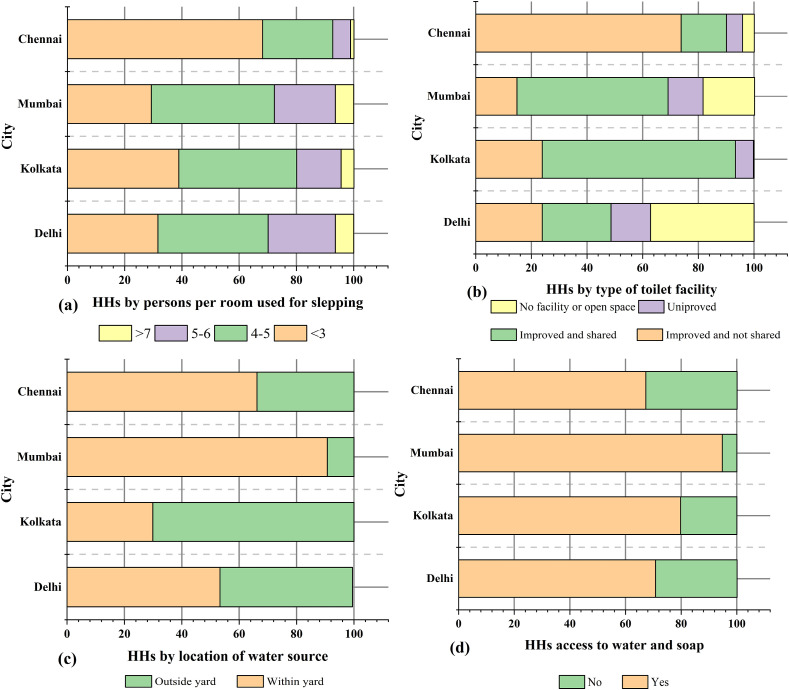
The result also showed that the percentage of variance decreases successively in each component. The number of principal components (4) having Eigen-value of more than 1.558 were determined in four rows in this study. A composite SVI score to COVID-19 for each state was developed (adding the score of each indicator). The SVI to COVID-19 value ranges from 0 to 1 where 0 indicates lower vulnerability and SVI value close to 1 refers to a relatively higher vulnerability. The states were also categorized into five vulnerable zones i.e. from highly vulnerable to very low vulnerability. The spatial mapping of major domains and composite PCA-based SVI were also developed (Fig. 8).
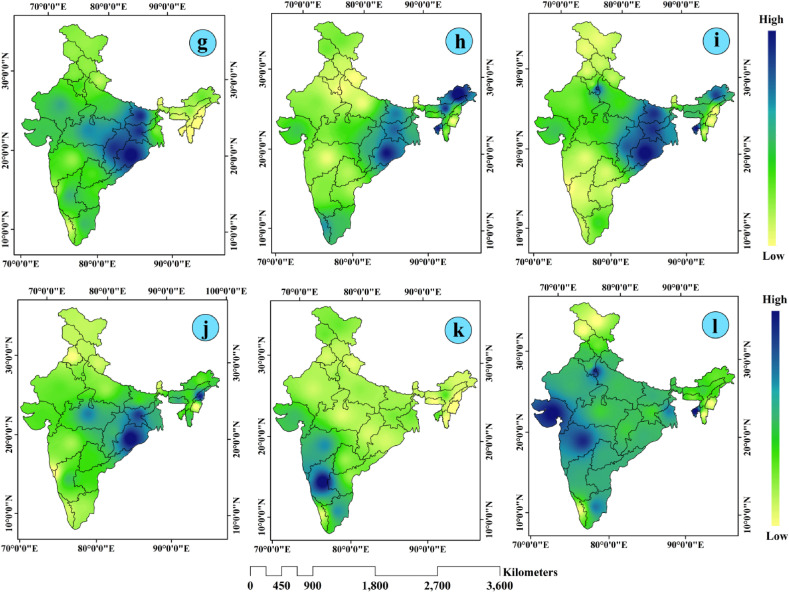
Fig. 8.
PCA based slum vulnerability mapping in India (a) PC1-vulnerablity due to poor slum households' status (b) PC2- vulnerability due to lack of social distance maintenance (c) PC3-vulnerability due to high concentrations of slum population and towns (d) PC4-vulnerability due to mobility of the households.
3.3. Fuzzy AHP based slum vulnerability index to COVID-19 (SVIcovid-19)
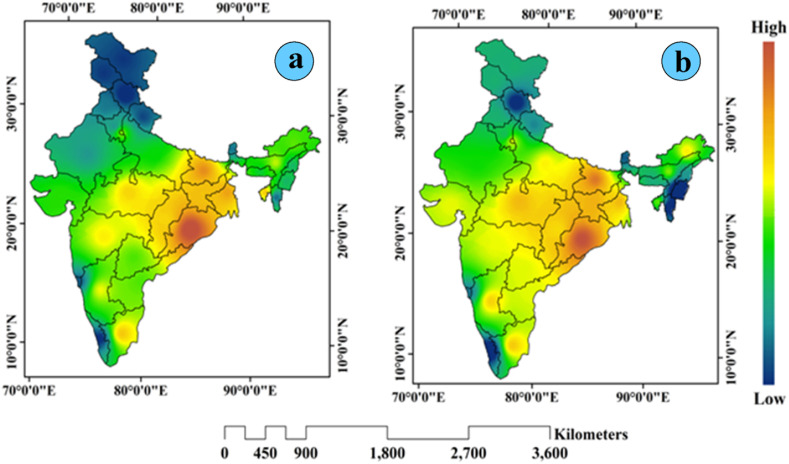
The availability as well as accessibility of the households to the basic services and amenities largely affects the transmission [[27], [28], [29]]. Recently the outbreak covid-19 has become significant global threats [[15], [16], [17]]. In India, large cities are mostly affected by this deadly disease due to high population density, unhygienic environment and the lack of accessibility to the services against COVID-19 transmission. Slums as an integral part of Indian cities are more vulnerable to COVID-19 due to a lack of accessibility to basic services. Therefore, assessment of vulnerability to slum areas is essential to understand the pattern of accessibility to the basic services and COVID-19 vulnerability in Indian slums. For the assessment of slum vulnerability using the Fuzzy AHP method, 12 variables related to COVID-19 transmission have been taken into consideration (Fig. 6 and Fig. 7 ). From the Fuzzy AHP based slum vulnerability index, it was found that eastern and central states were the more vulnerable to COVID-19 transmission. These states were more vulnerable to COVID-19 transmission due to lack of availability as well as accessibility to basic services and amenities. Particularly Odisha, Bihar, West Bengal and Jharkhand are more vulnerable to COVID-19 transmission due to poor household status. In these states, households have very limited access to basic services and amenities that are likely to be more vulnerable. From the PCA-based slum vulnerability index, it was observed that social distance maintenance (PC2) was highest in eastern, central as well as southern parts of India. As per the result of the study, it was observed that most of the households living in these states have no exclusive room and have only one room on sharing basis. In this situation, it is very difficult to maintain social distance even home quarantine is not possible for these households.
Fig. 6.
Fuzzy-AHP based spatial distribution of indicators (a) % of slum population in respect to state (b) % of slum population in respect to country (c) number of reported slum towns (d) households size (e) illiterate slum population and (f) slum rented households.
Fig. 7.
Fuzzy-AHP based spatial distribution of indicators (g) % of slum households having open toilet (h) % of slum households having no drainage (i) % of slum households having no bathroom (j) % of slum households having no water facility within premises (k) % of slum households having no exclusive rooms and (l) % of households having one dwelling room.
As per Fig. 8, it was obvious that there were regional differences in slum vulnerability to COVID-19 in India. Slum households living in eastern India are more vulnerable due to relatively poor household status. Particularly Odisha, Bihar, West Bengal and Jharkhand are more vulnerable to COVID-19 transmission due to poor household status. In these states, households have very limited access to basic services and amenities hence, they are more likely to be vulnerable. Vulnerability due to social distance maintenance (PC2) was highest in eastern, central as well as southern parts of India. As per the result of the study, it was observed that most of the households living in these states have no exclusive room and have only one room. In this situation, it is very difficult to maintain social distance even home quarantine is not possible for these households. Vulnerability due to high concentrations of slum population and slum towns (PC3) dominates in eastern as well as north-eastern parts of India. PC4 also shows that vulnerability due to lack of social distance maintenance also dominates in eastern, central as well as the southern part of India. From all the components, it was observed that the eastern and central parts of India were more vulnerable. A similar result also was recorded from the composite PCA-based slum vulnerability index (i.e. eastern and central India were more vulnerable than other regions) (Fig. 9 ). Table 6 represents the identification of states based on the level of vulnerability and weaknesses and strengths of indicators.
Fig. 9.
(a) Composite PCA based slum vulnerability index (b) Fuzzy AHP based slum vulnerability index (SVI).
Table 6.
Identification of states based on level of vulnerability and weaknesses and strengths of variables.
| Level of vulnerability | SVI score | Number of States | Weaknesses and strengths of variables |
|---|---|---|---|
| Highly vulnerable | >0.80 | Odisha, Bihar and West Bengal |
|
| Moderately vulnerable | 0.60–0.80 | Madhya Pradesh, Maharashtra, Tamil Nadu, Chhattisgarh, Jharkhand, Tripura |
|
| Vulnerable | 0.40–0.60 | Delhi, Uttar Pradesh, Gujrat, Karnataka, Andhra Pradesh, Assam, Meghalaya, Arunachal Pradesh |
|
| Low vulnerable | 0.20–0.40 | Haryana, Rajasthan, Sikkim, Mizoram, Manipur, Nagaland |
|
| Very low vulnerable | <0.20 | Himachal Pradesh, Punjab, Uttarakhand, Goa, Kerala, Jammu and Kashmir |
|
Recently in a number of studies, it was well recognized that the urban slums are more vulnerable to COVID-19 transmission due to high population density, poor living conditions and limited access to basic services [6,[15], [16], [17],[27], [28], [29], [30]]. More than 70% of the total confirmed COVID-19 cases were recorded from the states falling under the category of very high and high vulnerability zones. Maharashtra alone accounts for more than one-third of the total COVID-19 cases of the country. Mumbai has now become a significant COVID-19 hotspot city of the country [67]. In Mumbai, about 50% population lives in slum-like conditions [68] that makes the city more vulnerable. In Mumbai Dharavi (Asia's largest slum), Santosh Nagar and Bharat Nagar slums are the most vulnerable to COVID-19 due to very high density of population. In these slum areas, more than a million people reside within an area of 0.82 square miles [69]. Thus, maintenance of social distance and physical distance is very tough for authorities.
In Kolkata, more than 32% of the total urban population lives in slum areas (locally known as ‘Bustee’). Most of the slum population resides in the eastern (along the eastern metropolitan bypass), Western (dock area) and Northern (Cossipore) areas of the city. A study was performed by Ray [23] over the selected slum areas (Kankulia Road slum and Panchanantala) of Kolkata city and the result of the study showed that there was a lack of basic physical infrastructure in both the slum areas of the city. For example, there was only a community tap for the whole slum area from where 600 persons collect water (5/1000 households). Even large numbers of slum households are dependent on community toilets. If there is only a single positive COVID-19 person, it will surely bring a public health threat to other slums dwellers. From this scenario, one can easily understand that the slum population is under great threat and most vulnerable to COVID-19.
A study was performed by Bag et al. [25], on the assessment of living conditions of the slum population over Delhi, Kolkata and Mumbai. The result of their study showed that about 70% of slum dwellers were dependent on public sanitation facilities across three megacities. Is this situation not vulnerable to COVID-19 infection among slum dwellers? Of course, there is a high probability of spreading COVID-19 rapidly. In addition to this, a number of research studies were performed in different cities across the country and the result of those studies reported that most of the slum dwellers had very limited access to the basic services and amenities [[70], [71], [72], [73]]. After the outbreak of COVID-19 due to lockdown, slum dwellers lost their income sources and their capability to fight the pandemic gets destroyed.
As per the result of SVIcovid-19, it was observed that the states located in eastern and central India were more vulnerable as compared to other regions. Odisha was the most vulnerable state among all the states of India followed by Bihar, West Bengal, Madhya Pradesh, Maharashtra, Uttar Pradesh, Jharkhand, etc. respectively. These states are more vulnerable to COVID-19 in slum areas due to lack of availability, accessibility as well as inequalities of basic services and amenities and large concentrations of slum population.
Recently, in many pieces of literature, it was well documented that the slums are more vulnerable to infectious diseases [74,75]. In fact, for the slum population, the subsistence of livelihoods became more important than COVID-19 transmission. Most of the people living in slums are involved with informal activities and became economically vulnerable due to lockdown [76]. Slum households are highly relying on a robust social connection [77] for subsistence. Therefore, they cannot avoid the COVID-19 risk due to insecure economic activities during the lockdown. The access to basic services and amenities in slum areas is limited as compared to the other parts of the cities. In this circumstance, if one wants to follow the guidelines, it would be very difficult to maintain COVID-19 protocols due to space constraints, overcrowding lack of physical distancing maintenance and self-quarantine that may result in a rapid transmission of COVID-19. Thus, behavior of the people living in slum areas is largely influenced by poor economic conditions and lack of accessibility to basic services in comparison to other places as well as social groups of the city. Apart from India, in Bangladesh too, a study was performed by Ullah et al. [78] on Rohingya people and results of the study revealed that Rohingya camps were also vulnerable due to poor living conditions and it can be compared to slums as well.
3.4. Policy implications for slum vulnerability reduction to COVID-19
From the overall result of the study, it was well recognized that slums located in the eastern and central parts of India were more vulnerable to COVID-19. In most of the states located in eastern (such as Odisha, Bihar, West Bengal, Uttar Pradesh) and central (Madhya Pradesh, Chhattisgarh) part of India, there was a substantial lack of accessibility as well as availability to the basic services and amenities. In many previous studies, it was well recognized that there is a lack of better accessibility to the basic services in slum areas [6,27,51]. Thus, limited access to the basic services and amenities of the households may make them more vulnerable to COVID-19 transmission.
The findings of this study will not only help to understand the slum vulnerability to COVID-19 but, also provides an immense scope to implement policies and plantings to combat other infectious diseases in the future. In fact, urban slums in India are characterized by unhealthy and unhygienic environmental conditions and a lack of proper WASH (water, sanitation and hygiene) provision. Therefore, the policy makers and planners must focus on adequate access to the basic services for the betterment of their quality of life, to control the rapid spread of COVID-19 in highly dense areas as well as to combat any infectious disease in the future.
Indian government implemented a number of slum improvement and development schemes and policies such as the National Slum Development Program (NSDP), Basic Services to Urban Poor (BSUP), Housing for All etc. In all the schemes and programs, emphasis was given to provide basic services and amenities (such as water supply, latrine facilities, drainage, housings, etc.) to the slum dwellers.
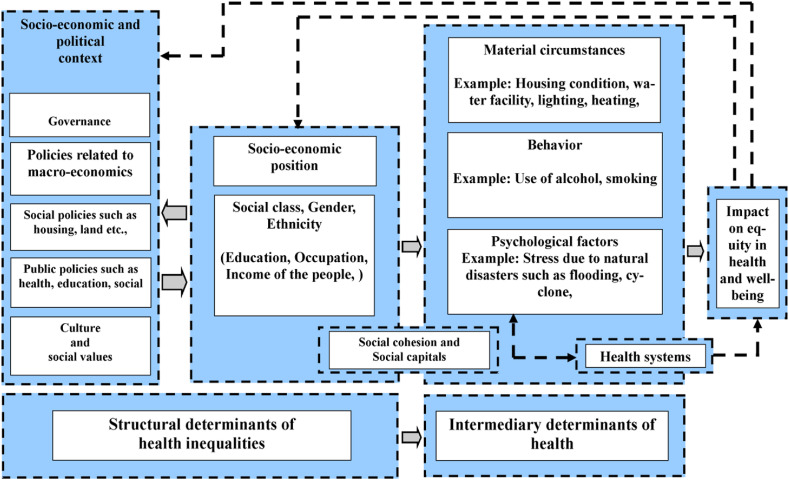
Fig. 10 represents the factors that largely determine the health of any communities. In this study, this frame was proposed for habitat vulnerability in slum areas to understand the factors affecting health as well as implementation of measures to reduce health vulnerability. A part from material services (such as access to housing, water facilities, and sanitations), slums areas are also vulnerable to any health diseases due to their behavior and psychological aspects of lives. For example, socio-economic positions of the slum dwellers such as lack of education, income largely determine the inequality from the people living in other parts of the city. Most of the time, slums dwellers are not aware about using of mask to reduce transmission of COVID-19 and cannot use hand sanitizer, masks, shops due to their poor economic conditions. Thus, social factors affecting health must be prioritized in slum areas.
Fig. 10.
Social determinants of health [79].
In this connection, the strategies of Asia's largest slum ‘Dharavi’ must be appreciated to combat COVID-19. Dharavi is located in Mumbai metro cities (Maharastra) with a geographical area of 2.1 km2 and population density over 277136 km2 respectively. Therefore, it is obvious that huge population density, health inequalities and socio-economic disparities may potentially convert the slum into one of the biggest hotspots of the country. The first confirm COVID-19 cases from Dharavi were reported on 1st April 2020 and after that, it started spearing very rapidly. At the end of April, a total of 491 new cases were reported in this slum. The local people, government and policymakers feared this as this area may become New York (USA) or Italy very soon. But a number of public health measures and proactive strategies were adopted by the local government to combat this deadly disease. Surprisingly, the growth rate of COVID-19 drooped from 12% (in April 2020) to 4.3% (in May 2020) and 1.02% (in June 2020) respectively [80]. During the first week of July 2020, only one case was recorded since the first week April 2020. Thus Dharavi became the model to the entire world. World Health Organization (WHO) also recognized the model called “chasing the virus” applied to reduce the transmission of COVID-19 and stated that “Dharavi should be seen as an example across the world”. WHO also acknowledged that the motto of the Dharavi model was “testing, tracing, isolating, and treating for breaking the chain of transmission”. Since the last three-four months, the COVID-19 cases and deaths were not so massive and everything is likely to be normal. During the second wave of COVID-19 (in February), the Dharavi model was again activated to curb COVID-19 transmission. As a result, COVID-19 cases significantly dropped and the Dharavi model’ of COVID-19 management as well as vaccination drive assisted successfully. Screening of the people at the door, aggressive and regular testing of the slum dwellers worked effectively to control COVID-19 transmission [81]. Thus, the Dharavi slum became the model in India and it was appreciated by World Health Organization (WHO). The Dharavi model has clearly shown how COVID-19 transmission can be curbed through proper management strategies and puts a unique example for other slum areas in cities. Particularly, the states having large proportions of slum population (such as Andhra Pradesh, West Bengal, Uttar Pradesh, Tamil Nadu and Madhya Pradesh) must follow the Dharavi model not only to fight with COVID-19, rather with other infectious diseases in the future.
From the result, it was well documented that the slums located in the central and eastern parts of India are more vulnerable in comparison to other states. Therefore, effective measures are needed to be implemented not only to curb COVID-19 transmission but, also to enhance the quality of life of slum dwellers by enlarging availability as well as accessibility to basic services and amenities. In India, the Central as well as State Government implemented several effective measures to curb the rapid spread of COVID-19 transmission in slum areas and successfully tackled the COVID-19 transmission. It can be stated that it is very difficult to implement ‘Dharavi model’ to control infectious diseases like COVID-19 rather it is better to ensure access to basic services of the slum residents and to make them conscious about health science. Thus, the transmission of infectious diseases like COVID-19 can also be (to some extent) controlled.
3.5. Limitations of the study and future research directions
The study has an immense potentiality to understand the impact of infectious diseases (like COVID- 19) on human health living in slums areas in Indian cities. Thus, this study reveals significant findings on how far slums are vulnerable to infectious diseases due to highly dense, unhygienic environments and where to implement effective public health measures for ensuring health well-being. In spite of this, this study has few drawbacks. Firstly, the habitat vulnerability in slum areas was assessed using data extracted from Census of India, 2011 and its linkages were presented using the recent COVID-19 scenario in India. Secondly, in this study, twelve variables closely related to COVID-19 (directly and indirectly) were considered to assess habitat vulnerability in slum areas. Thus, these variables may not sufficient for habitat vulnerability assessment. Thirdly, in this study, only slums were assessed for vulnerability assessment. The non-slum areas have not been taken into consideration for vulnerability assessment.
In spite of these limitations, this study will surely inspire the researchers and scientists to explore more research on the nexus between infectious diseases and habitat vulnerability particularly people living in highly dense unhygienic environments. Apart from slum areas, particularly cities in developing countries (like India) can be vulnerable due to high population density and limited accessibility as well as availability to basic services and amenities. Thus, from the limitations of the study, few suggestions can be proposed for further research in the future. Firstly, the researchers can utilize the recent data (from the next Census of India data) to examine the habitat vulnerability in slum areas. Secondly, more relevant as well as sufficient variables related to infectious diseases (COVID-19) can be incorporated to develop habitat vulnerability mapping in slum areas. Thirdly, some advance machine learning techniques can also be utilized to develop habitat vulnerability in slum areas.
4. Conclusion
The present paper mainly deals with the assessment of slum vulnerability to COVID-19 (SVI covid-19) across the states of India. Principal component analysis (PCA) and Fuzzy AHP based methods have been used to assess the SVIcovid-19 India. From the result, it was well documented that the slums located in the eastern and central Indian states were more vulnerable to COVID-19 due to limited access to basic services and a relatively higher concentration of slum population. The findings of this research study have immense scope to understand the relationship between living environment and respiratory disease (like COVID-19). Thus, it is an urgent task for policy-makers and city planners to integrate the urban slum improvement strategies for a better quality of life and to combat serious health disasters like COVID-19. Hence, in India, the second wave of COVID-19 spread more rapidly and a huge number of cases as well as deaths were reported from large cities. Therefore, slums due to high population density, unhygienic environment and limited access to the basic services and amenities may result in rapid transmission of COVID-19 and massive losses of lives. Therefore, it is important to understand the factors leading to the vulnerability of slum dwellers and to adopt necessary actions to curb the rapid transmission as well as deaths.
Thus, from the overall analysis, it was well documented that there was a substantial lack of availability as well as accessibility to basic services and amenities in slum areas. Thus, limited access to basic services increases the chances of infection due to lack of maintenance social distance, poor housing conditions, and limited infrastructural opportunities respectively.
-
(i)
As per the study, it was found that the states having a high concentration of slum population were highly affected by COVID-19 such as Maharashtra, Tamil Nadu, West Bengal, Karnataka, etc. As per the reports published by Business Insider [82]; more than 50% of the total COVID-19 cases were reported from large cities (such as Mumbai, Delhi, Pune, Thane etc.). In slum areas, there is significantly more scope of social mixing and limited scope for physical distancing due to high population density. As per the study of Chen et al. (2019), it was a high density of population that was linked with higher peaks of influenza in Delhi. The current pandemic (COVID-19) transmitted more rapidly in highly dense large cities due to high population density. Thus, slum areas are more vulnerable due to high population density and a poor living environment. Therefore, the government must adopt effective starategies in highly dense slum areas to reduce the transmission of such infectious diseases in the future.
-
(ii)
In slum areas, among most of the households, there was no inclusive room or having only one room. There were more than 60% HHs in Gujrat, about 60% HHs in Maharashtra and about 50% HHs in Tamil Nadu residing in slum areas with only one room. Among all the states, the highest % of slum HHs with no exclusive room was reported from Karnataka (11.75%) followed by Maharashtra (7.36%), Tamil Nadu (7.12%). The scenarios of COVID-19 showed that Ahmedabad, Mumbai, Chennai were some of the severely affected cities in India. Therefore, special focus needs to be given to slum areas to fight any health problems (like COVID-19).
-
(iii)
In slum areas, there is limited access to the basic infrastructural facilities (such as good conditions of house, drinking water facility within premises, and availability of toilets) [27,28]. Infections in a member of households increase the possibility of infecting other members in slum areas. The sizes of the HHs are highly responsible for a higher transmission of infectious diseases. Therefore, it is crucial to provide adequate basic infrastructural facilities for reducing the transmission of infectious diseases.
-
(iv)
During the second wave of COVID-19, it was found that the states located in eastern parts of India were highly affected such as West Bengal, Uttar Pradesh, Bihar, respectively. As per the result of the study, it was recorded that the slums located in the eastern states of the country were highly vulnerable to COVID-19. In these states, there was limited access to closed bathrooms, drainage facilities, water felicities respectively. Therefore, it is essential to provide basic infrastructural facilities to the slum HHs to tackle infectious diseases in the future for reducing the chances of a health risk.
Thus, from the overall analysis, we came to know that the slum habitats are vulnerable to COVID-19 due to limited access to basic services and amenities and it is very urgent to provide adequate basic infrastructural facilities for a better quality of slum HHs in the future. Mapping of slum vulnerability is not only important to understand the scenario of living conditions of the slum dwellers but also, can be very impactful to understand slum vulnerability with respect to other diseases (particularly infectious diseases like COVID-19) in the future. Thus, from the result, it was observed that the eastern and central states were more vulnerable to COVID-19 in comparison to other parts of India. From the study, we can conclude that although the central and eastern states were more vulnerable to COVID-19, effective measures can help in reducing the transmission of COVID-19. Infectious diseases like COVID-19 can be successfully tackled through appropriate measures like ‘Dharavi Model’ in Mumbai (Maharastra). Of course, slums are vulnerable to the infectious diseases COVID-19 due to high population density, unhygienic environment and lack of basic services but, their lives from any kind of health problems can be saved through proper scientific measures.
Funding
None.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.UN Habitat . 2020. 2020 UN HabitatUN-Habitat COVID-19 Response Plan [response Plan]. UN Habitat.https://unhabitat.org/sites/default/files/2020/04/final_un-habitat_covid-19_response_plan.pdf [Google Scholar]
- 2.Hindustan Times Hindustan times. https://www.hindustantimes.com/india-news/these-10-cities-are-worst-hit-by-covid-19-mumbai-delhi-ahmedabad-among-top-5/story-QR5ena9FBEoJsFZPRHAjWJ.html. 2020 Retrieved June 9 2020, From.
- 3.The Print The print. https://theprint.in/health/these-10-cities-have-over-half-of-indias-covid-19-cases-ahmedabad-indore-among-top-5/404998/ Retrieved June 9 2020.
- 4.The Times of India The times of India. https://timesofindia.indiatimes.com/city/mumbai/mumbai-dharavi-adds-1400-covid-19-cases-in-may/articleshow/76136859.cms. 2020 Retrieved June 9 2020, From.
- 5.Desai D. Urban densities and the Covid-19 pandemic: upending the sustainability myth of global megacities. ORF Occasional Paper. 2020;244(4):1–4. [Google Scholar]
- 6.Mishra S.V., Gayen A., Haque S.M. COVID-19 and urban vulnerability in India. Habitat Int. 2020;103:102230. doi: 10.1016/j.habitatint.2020.102230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parikh P., McRobie A. Engineering as a tool for improving human habitat. Int. J. Manag. Decis. Making. 2009;10(3–4):270–281. [Google Scholar]
- 8.Parikh P., Parikh H., McRobie A. The role of infrastructure in improving human settlements. Proceedings of the Institution of Civil Engineers-Urban Design and Planning. 2013;166(2):101–118. [Google Scholar]
- 9.Bhattacharya A., Romani M., Stern N. CCCEP, Grantham Research Institute on Climate Change and the Environment and G; 2012. Infrastructure for Development: Meeting the Challenge; p. 24. [Google Scholar]
- 10.Census of India 2011. https://censusindia.gov.in Accessed.
- 11.Gulyani S., Talukdar D. Slum real estate: the low-quality high-price puzzle in Nairobi's slum rental market and its implications for theory and practice. World Dev. 2008;36(10):1916–1937. [Google Scholar]
- 12.Butala N.M., VanRooyen M.J., Patel R.B. Improved health outcomes in urban slums through infrastructure upgrading. Soc. Sci. Med. 2010;71(5):935–940. doi: 10.1016/j.socscimed.2010.05.037. [DOI] [PubMed] [Google Scholar]
- 13.Habitat U.N. Earthscan; London: 2003. The Challenge of Slums: Global Report on Human Settlements 2003. [Google Scholar]
- 14.UN-Habitat U.N. 2006. State of the World's Cities 2006/7. The Millennium Development Goals and Urban Sustainability: 30 Years of Shaping the Habitat Agenda. [Google Scholar]
- 15.Das A., Das M., Ghosh S. Impact of nutritional status and anemia on COVID-19: is it a public health concern? Evidence from national family health survey-4 (2015–2016), India. Publ. Health. 2020;185:93. doi: 10.1016/j.puhe.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das A., Ghosh S., Das K., Dutta I., Basu T., Das M. Re:(In) visible impact of inadequate WaSH Provision on COVID-19 incidences can be not be ignored in large and megacities of India. Publ. Health. 2020;185:34. doi: 10.1016/j.puhe.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Das M., Das A., Mandal A. Research note: ecosystem Health (EH) assessment of a rapidly urbanizing metropolitan city region of eastern India–A study on Kolkata Metropolitan Area. Landsc. Urban Plann. 2020;204:103938. doi: 10.1016/j.landurbplan.2020.103938. [DOI] [Google Scholar]
- 18.Unicef . Esocialsciences; 2012. The State of the World's Children 2012: Children in an Urban World. [Google Scholar]
- 19.Hutton G., Haller L., Water S., World Health Organization . World Health Organization; 2004. Evaluation of the Costs and Benefits of Water and Sanitation Improvements at the Global Level. No. WHO/SDE/WSH/04.04) [Google Scholar]
- 20.Gupta I., Guin P. Health status and access to health services in Indian slums. Health. 2015;7(2):245. [Google Scholar]
- 21.Parth K. The economic cost of COVID-19: a potential pandemic impact on Indian economy. International Journal of Advanced Science and Technology. 2020:2182–2192. [Google Scholar]
- 22.Lee S.A., Jobe M.C., Mathis A.A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 2021;51(8):1403–1404. doi: 10.1017/S003329172000121X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ray B. Quality of life in selected slums of Kolkata: a step forward in the era of pseudo-urbanisation. Local Environ. 2016;22(3):365–387. [Google Scholar]
- 24.Agarwala R. Cambridge University Press; 2013. Informal Labor, Formal Politics, and Dignified Discontent in India. [Google Scholar]
- 25.Bag S., Seth S., Gupta A. Leeds University Business School Working Paper, (16-07); 2016. A Comparative Study of Living Conditions in Slums of Three Metro Cities in India. [Google Scholar]
- 26.Mitlin D. 2020. The Politics of Shelter: Understanding Outcomes in Three African Cities. [Google Scholar]
- 27.Parikh P., Karim Y.B., Paulose J., Factor-Litvak P., Nix E., Aisyah D.N.…Lakhanpaul M. COVID-19 and informal settlements–implications for water, sanitation and health in India and Indonesia. UCL Open Environment. 2020;1:1–5. doi: 10.14324/111.444/ucloe.000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Friesen J., Pelz P.F. COVID-19 and slums: a pandemic highlights gaps in knowledge about urban poverty. JMIR Public Health and Surveillance. 2020;6(3) doi: 10.2196/19578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hasan S.M., Das S., Hanifi S.M.A., Shafique S., Rashid S., Reidpath D.D. 2020. A Place-Based Analysis of COVID-19 Risk Factors in Bangladesh Urban Slums: A Secondary Analysis of World Bank Microdata. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nix E., Paulose J., Lakhanpaul M., Factor-Litvak P., Parikh P., Altamirano-Medina H., Manikam L. UCL Open. Environment Preprint; 2020. COVID-19 & informal settlements: is Stay Home safe? [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghosh S., Das A., Hembram T.K., Saha S., Pradhan B., Alamri A.M. Impact of COVID-19 induced lockdown on environmental quality in four indian megacities using landsat 8 OLI and TIRS-derived data and mamdani fuzzy logic modelling approach. Sustainability. 2020;12(13):5464. [Google Scholar]
- 32.Adiga A., Chu S., Eubank S., Kuhlman C.J., Lewis B., Marathe A., Wilson M.L. Disparities in spread and control of influenza in slums of Delhi: findings from an agent-based modelling study. BMJ open. 2018;8(1) doi: 10.1136/bmjopen-2017-017353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Góes L.G.B., Zerbinati R.M., Tateno A.F., de Souza A.V., Ebach F., Corman V.M.…Drexler J.F. Typical epidemiology of respiratory virus infections in a Brazilian slum. J. Med. Virol. 2020;92(8):1316–1321. doi: 10.1002/jmv.25636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neiderud C.J. How urbanization affects the epidemiology of emerging infectious diseases. Infect. Ecol. Epidemiol. 2015;5(1):27060. doi: 10.3402/iee.v5.27060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oppong J.R., Mayer J., Oren E. The global health threat of African urban slums: the example of urban tuberculosis. African Geographical Review. 2015;34(2):182–195. [Google Scholar]
- 36.Olivera-La Rosa A., Chuquichambi E.G., Ingram G.P. Keep your (social) distance: pathogen concerns and social perception in the time of COVID-19. Pers. Indiv. Differ. 2020;166:110200. doi: 10.1016/j.paid.2020.110200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Valenti V.E., de Lemos Menezes P., de Abreu A.C.G., Vieira G.N.A., Garner D.M. Social distancing measures may have reduced the estimated deaths related to Covid-19 in Brazil. Journal of Human Growth and Development. 2020;30(2):164–169. [Google Scholar]
- 38.Mohler G., Bertozzi A.L., Carter J., Short M.B., Sledge D., Tita G.E., Brantingham P.J. Impact of social distancing during COVID-19 pandemic on crime in Los Angeles and Indianapolis. J. Crim. Justice. 2020:101692. doi: 10.1016/j.jcrimjus.2020.101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carrion D., Colicino E., Pedretti N.F., Arfer K.B., Rush J., DeFelice N., Just A.C. medRxiv; 2020. Assessing Capacity to Social Distance and Neighborhood-Level Health Disparities during the COVID-19 Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable cities and society. 2020;62:102390. doi: 10.1016/j.scs.2020.102390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Checkley W., Pollard S.L., Siddharthan T., Babu G.R., Thakur M., Miele C.H., Van Schayck O.C. Managing threats to respiratory health in urban slums. The Lancet Respiratory Medicine. 2016;4(11):852–854. doi: 10.1016/S2213-2600(16)30245-4. [DOI] [PubMed] [Google Scholar]
- 42.van der Heijden J., Gray N., Stringer B., Rahman A., Akhter S., Kalon S., Biswas A. ‘Working to stay healthy’, health-seeking behaviour in Bangladesh's urban slums: a qualitative study. BMC Publ. Health. 2019;19(1):1–13. doi: 10.1186/s12889-019-6750-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Das A., Ghosh S., Das K., Basu T., Dutta I., Das M. Living environment matters: unravelling the spatial clustering of COVID-19 hotspots in Kolkata megacity, India. Sustainable Cities and Society. 2021;65:102577. doi: 10.1016/j.scs.2020.102577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saroj S.K., Goli S., Rana M.J., Choudhary B.K. Availability, accessibility, and inequalities of water, sanitation, and hygiene (WASH) services in Indian metro cities. Sustainable Cities and Society. 2020;54:101878. [Google Scholar]
- 45.Devkar G., Thillai Rajan A., Narayanan S., Elayaraja M.S. Provision of basic services in slums: a review of the evidence on top‐down and bottom‐up approaches. Dev. Pol. Rev. 2019;37(3):331–347. [Google Scholar]
- 46.Oztig L.I., Askin O.E. Human mobility and coronavirus disease 2019 (COVID-19): a negative binomial regression analysis. Publ. Health. 2020;185:364–367. doi: 10.1016/j.puhe.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jordan R.E., Adab P., Cheng K.K. 2020. Covid-19: Risk Factors for Severe Disease and Death. [DOI] [PubMed] [Google Scholar]
- 48.Kraemer M.U., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M., Brownstein J.S. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Badr H.S., Du H., Marshall M., Dong E., Squire M.M., Gardner L.M. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect. Dis. 2020;20(11):1247–1254. doi: 10.1016/S1473-3099(20)30553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Uddin M.N., Islam A.S., Bala S.K., Islam G.T., Adhikary S., Saha D., Akter R. Mapping of climate vulnerability of the coastal region of Bangladesh using principal component analysis. Appl. Geogr. 2019;102:47–57. [Google Scholar]
- 51.Das A., Das M., Barman H. Access to basic amenities and services to urban households in West Bengal: does its location and size of settlements matter? Geojournal. 2019:1–29. [Google Scholar]
- 52.Coulibaly J.Y., Mbow C., Sileshi G.W., Beedy T., Kundhlande G., Musau J. Mapping vulnerability to climate change in Malawi: spatial and social differentiation in the Shire River Basin. Am. J. Clim. Change. 2015;4(3):282. [Google Scholar]
- 53.Piya L., Maharjan K.L., Joshi N.P. Perceptions and realities of climate change among the Chepang communities in rural mid-hills of Nepal. Journal of Contemporary India Studies: Space and Society, Hiroshima University. 2012;2(5):35–50. [Google Scholar]
- 54.Žurovec O., Čadro S., Sitaula B.K. Quantitative assessment of vulnerability to climate change in rural municipalities of Bosnia and Herzegovina. Sustainability. 2017;9(7):1208. [Google Scholar]
- 55.Maiti S., Jha S.K., Garai S., Nag A., Bera A.K., Paul V., Deb S.M. An assessment of social vulnerability to climate change among the districts of Arunachal Pradesh, India. Ecol. Indicat. 2017;77:105–113. [Google Scholar]
- 56.Mavhura E., Manyena B., Collins A.E. An approach for measuring social vulnerability in context: the case of flood hazards in Muzarabani district, Zimbabwe. Geoforum. 2017;86:103–117. [Google Scholar]
- 57.Tran H.T., Campbell J.B., Tran T.D., Tran H.T. Monitoring drought vulnerability using multispectral indices observed from sequential remote sensing (Case Study: tuy Phong, Binh Thuan, Vietnam) GIScience Remote Sens. 2017;54(2):167–184. [Google Scholar]
- 58.Abson D.J., Dougill A.J., Stringer L.C. Using principal component analysis for information-rich socio-ecological vulnerability mapping in Southern Africa. Appl. Geogr. 2012;35(1–2):515–524. [Google Scholar]
- 59.Saaty T.L. A scaling method for priorities in hierarchical structures. J. Math. Psychol. 1977;15(3):234–281. [Google Scholar]
- 60.Gharizadeh Beiragh R., Alizadeh R., Shafiei Kaleibari S., Cavallaro F., Zolfani S.H., Bausys R., Mardani A. An integrated multi-criteria decision making model for sustainability performance assessment for insurance companies. Sustainability. 2020;12(3):789. [Google Scholar]
- 61.Giri M., Bista G., Singh P.K., Pandey R. Climate change vulnerability assessment of urban informal settlers in Nepal, a least developed country. J. Clean. Prod. 2021;307:127213. [Google Scholar]
- 62.Li X., Liu T., Lin L., Song T., Du X., Lin H., Zhang Y. Application of the analytic hierarchy approach to the risk assessment of Zika virus disease transmission in Guangdong Province, China. BMC Infect. Dis. 2017;17(1):1–9. doi: 10.1186/s12879-016-2170-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dom N.C., Ahmad A.H., Abd Latif Z., Ismail R. Application of geographical information system-based analytical hierarchy process as a tool for dengue risk assessment. Asian Pacific Journal of Tropical Disease. 2016;6(12):928–935. [Google Scholar]
- 64.Saaty T.L. McGraw Hill; New York, NY, USA: 1980. The Analytical Hierarchy Process; p. 350. [Google Scholar]
- 65.Sarkar S., Parihar S.M., Dutta A. Fuzzy risk assessment modelling of East Kolkata Wetland Area: a remote sensing and GIS based approach. Environ. Model. Software. 2016;75:105–118. [Google Scholar]
- 66.Saha S. Groundwater potential mapping using analytical hierarchical process: a study on Md. Bazar Block of Birbhum District, West Bengal. Spatial Information Research. 2017;25(4):615–626. [Google Scholar]
- 67.Porio E. Vulnerability, adaptation, and resilience to floods and climate change-related risks among marginal, riverine communities in Metro Manila. Asian J. Soc. Sci. 2011;39(4):425–445. [Google Scholar]
- 68.Shaikh M. 2020. With over 1,000 Cases, Mumbai Becomes India's Covid-19 Hotspot. India Today.https://www.indiatoday.in/india/story/with-over-1-000-cases-mumbai-becomes-india-scovid-19-hotspot-1665623-2020-04-10 Available at: [Google Scholar]
- 69.Bardhan R., Sarkar S., Jana A., Velaga N.R. Mumbai slums since independence: evaluating the policy outcomes. Habitat Int. 2015;50:1–11. [Google Scholar]
- 70.Sajjad H. Living standards and health problems of lesser fortunate slum dwellers: evidence from an Indian City. Int. J. Environ. Protect. Pol. 2014;2:54. [Google Scholar]
- 71.Kalkoti K. Rural sanitation—a Herculean task. Kurukshetra. 2013;61(3):3–7. [Google Scholar]
- 72.Phukan D.K. Levels of some basic amenities in the slums and their impacts on ecology: a case study of Jorhat City, Assam. Int. J. Sci. Res. 2014;3(1):71–74. [Google Scholar]
- 73.Goswami S., Manna S. Urban poor living in slums: a case study of Raipur city in India. Global Journal of Human Social Science Sociology & Culture. 2013;13(4):15–22. [Google Scholar]
- 74.Lilford R.J., Oyebode O., Satterthwaite D., Melendez-Torres G.J., Chen Y.F., Mberu B., Ezeh A. Improving the health and welfare of people who live in slums. Lancet. 2017;389:559–570. doi: 10.1016/S0140-6736(16)31848-7. 10068. [DOI] [PubMed] [Google Scholar]
- 75.Lopez O., Moloney A. Thompson Reuters Foundation; 2020. Coronavirus Chases the Slum Dwellers of Latin America; p. 18. [Google Scholar]
- 76.Mberu B.U., Ciera J.M., Elungata P., Ezeh A.C. Patterns and determinants of poverty transitions among poor urban households in Nairobi, Kenya. Afr. Dev. Rev. 2014;26(1):172–185. [Google Scholar]
- 77.Corburn J., Vlahov D., Mberu B., Riley L., Caiaffa W.T., Rashid S.F., Ayad H. Slum health: arresting COVID-19 and improving well-being in urban informal settlements. J. Urban Health. 2020;97(3):348–357. doi: 10.1007/s11524-020-00438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ullah A.A., Hossain M.A., Chattoraj D. Covid-19 and Rohingya refugee camps in Bangladesh. Intellect. Discourse. 2020;28(2):793–806. [Google Scholar]
- 79.Solar O., Irwin A. WHO Document Production Services; 2010. A Conceptual Framework for Action on the Social Determinants of Health. [Google Scholar]
- 80.Press Information Bureau, Government of India . 2020. COVID-19 Updates.https://pib.gov.in/PressReleseDetail.aspx?PRID=1633177 Available at. Accessed. [Google Scholar]
- 81.The Hindu 2021. https://www.thehindu.com/news/national/other-states/mumbais-dharavi-model-helps-tame-second-covid-19-wave-in-slum-town/article34664110.ece
- 82.Business Insider (2020), https://www.businessinsider.in/india/news/checkout-the-10-most-affected-cities-in-india-with-the-highest-number-of-coronavirus-cases/slidelist/76343170.cms. Assessed on 20 July, 2021.