Abstract
Background
The COVID-19 pandemic has affected the entire world, and the vaccine has emerged as a source of hope for return to normal life. Still, various countries have reported high vaccine hesitancy rates. It is important to know the vaccine hesitancy profile in Brazil to help design adequate communication strategies.
Methods
A voluntary, anonymous online survey was conducted from January 22 to 29, 2021, including resident Brazilian adults to assess factors related to vaccine hesitancy. Sociodemographic and epidemiological data were analyzed. A bivariate analysis was conducted with the independent variables, with vaccine hesitancy as the outcome variable, and a multivariate logistic model was used to calculated adjusted odds ratios.
Results
The sample included 173,178 respondents, and vaccine hesitancy was found in 10.5%. The principal factors associated with vaccine hesitancy were the following: assigning importance to the vaccinés efficacy (AOR = 16.39), fear of adverse reactions (AOR = 11.23), and assigning importance to the vaccinés country of origin (AOR = 3.72). Other risk factors were the following: male gender (AOR = 1.62), having children (AOR = 1.29), 9 years of schooling or less (AOR = 1.31), living in the Central-West region (AOR = 1.19), age ≥ 40 years (AOR = 1.17), and monthly income < U$788.68 (AOR = 1.13). The two vaccines available in Brazil, Covishield and CoronaVac, showed similar confidence, 80.13% and 76.36%, respectively, despite the higher rejection of the latter vaccinés Chinese origin.
Interpretation
This online survey confirms the low vaccine hesitancy rate among Brazilians and allowed the identification of a profile that can assist the elaboration of communication strategies to increase vaccine adherence.
Funding
National Institute of Women, Children and Adolescents Health Fernandes Figueira, FIOCRUZ, Rio de Janeiro, Brazil.
Keywords: Vaccine hesitancy, Brazil, Survey, Adverse reactions, COVID-19 vaccine, Efficacy
1. Introduction
Since 2020, the COVID-19 pandemic has caused more than 250 thousand deaths in Brazil [1]. The incidence and mortality rates are still high, with numerous cities facing an overload on their healthcare services, healthcare workerś exhaustion, and shortage of hospital beds and essential inputs [2]. The availability of vaccines for the prevention of COVID-19 in the world and the beginning of vaccination in Brazil in January have raised hope for control of the pandemic. However, despite the benefits of vaccination, vaccine hesitancy has been identified as the cause of resurgence of vaccine-preventable diseases such as measles [3]. Despite the severity of COVID-19, hesitancy with the COVID-19 vaccine has been observed in other countries [4], [5], [6], [7]. In Brazil, despite the alarming number of cases, the intense circulation of fake news in the social media raises concerns with vaccine confidence. Given the lack of effective curative treatments, safe and effective COVID-19 vaccines are critical for a significant reduction in the epidemic curve [5]. Although some studies estimate that immunization of 40–60% of the population is necessary to reach herd immunity [8], but as the pandemic enters its second year, the challenge of reaching a herd-immunity threshold was looking unlikely because of factors such as vaccine hesitancy, the emergence of new variants and the delayed arrival of vaccinations for children [9].
In this scenario, it is important to understand the profile of vaccine-hesitant Brazilians in relation to vaccination for the prevention of COVID-19. This evaluation can elucidate the underlying reasons for hesitancy and thus contribute to the elaboration of strategies to improve vaccination adherence for the prevention of COVID-19. This study was based on an online survey in the first week of vaccination in Brazil to assess vaccine hesitancy in the prevention of COVID-19. On the start date of the study on January 22, 2021 there were 56,552 new confirmed cases of COVID-19, 8,753,920 accumulated cases, 215,243 accumulated deaths, and at the end of the study on January 29, 2021, there were 59,826 new confirmed cases of COVID-19, 9,118,513 accumulated cases, and 222,666 accumulated deaths [10].
2. Methodology
This was a voluntary, anonymous online survey conducted from January 22 to 29, 2021, in Brazil, through a free platform (https://www.google.com/forms/about/) with the link made available on the social networks WhatsApp, Telegram, Facebook, Instagram, Twitter, and LinkedIn. All participants were encouraged to share the study form on their own social networks. The link to the form was also shared on the official webpage of the National Institute of Womeńs, Childreńs and Adolescents‘ Health Fernandes Figueira, FIOCRUZ (www.iff.fiocruz.br). The form consisted of 27 closed questions and 3 open questions, prepared after a literature review and discussion with the group of experts in the research team.
2.1. Inclusion and exclusion criteria and sample size
The sample consisted of all records of participants who stated they were 18 years or older, Brazilians, and residing in Brazil at the time of the survey. The sample excluded records with all the items completed identically, reflecting duplicate responses, and the forms with all the items left blank. Duplicate records were excluded through the SPSS, which compared the degree of similarity of responses from closed variable fields with two open fields that should present a higher level of heterogeneous responses.
To estimate the required sample size, an a priori power analysis was conducted. Based on the total population of Brazilians (n=≈213 million), with 50% prevalence of hesitancy, with 99,9% confidence levels, and a conservative 1% margin of error, a total of 36,474 participants were needed for the study (3,233 from North region, 9,860 from northeast region, 15,326 from Southeast, 5,198 from South region and 2,857 from Central West region.
2.2. Outcome
The studýs outcome is vaccine hesitancy according to the criteria of the SAGE Working Group on Vaccine Hesitancy, defining hesitancy as delay in acceptance or outright refusal of vaccines [11]. The current study thus defined vaccine-hesitant individuals as those who did not intend to be vaccinated, those who were unsure, and those who would only agree to be vaccinated depending on which vaccine was used.
2.3. Variables
The following independent variables were considered: 1) demographic: gender (male, female, other, or prefer not to answer), age bracket (18–39 years, 40–59 years, ≥ 60 years), children, state of residence, residence in the state capital, ethnicity (white versus non-white), schooling (primary, or the first 9 complete years, secondary, or university), and monthly income (family income was converted to U$ considering the average exchange rate in the month of January 2021, or BRL 5.363 = U$ 1.00, and stratified as zero income, ≤ U$197.17, U$197.18–788.67, U$788.68–985.85, U$985.86–1,971.70, and >U$1,972); 2) variables related to COVID-19: COVID-19 cases, deaths, or ICU admission of any family member for COVID-19, fear of catching COVID-19 (not afraid, somewhat afraid, more or less afraid, very afraid, and terrified), importance of COVID-19 vaccination (unimportant, somewhat important, do not know, important, very important); 3) variables related to the vaccine: importance of the efficacy and country of origin of the vaccine (American, Chinese, British, Indian, Russian); degree of vaccine confidence according to a Likert scale (I do not trust, I trust a little, I do not know, I trust enough, I trust very much) in the following vaccines: Covishield (AZD1222, Oxford-AstraZeneca/FIOCRUZ), CoronaVac (Sinovac Life Sciences, Beijing, China/Butantan Institute), Pfizer-BioNTech (BNT162b2, Pfizer, Inc; Philadelphia, Pennsylvania, USA), Moderna (mRNA-1273, ModernaTX, Inc; Cambridge, Massachusetts, USA), Sputnik V (Gam-COVID-Vac, Gamaleya National Research Centre for Epidemiology and Microbiology, Moscow, Russia), and Covaxin (BBV152, Bharat Biotech in collaboration with the Indian Council of Medical Research - National Institute of Virology).
2.4. Statistical analysis
Data were coded and analyzed in the SPSS software. All the variables were analyzed according to their absolute and relative frequencies. Bivariate analysis was performed with vaccine hesitancy as the outcome. This analysis used the chi-square test, and statistical significance of differences was set at p-value < 0.05. A multivariate logistic model was used to calculate adjusted odds ratios with the respective 95% confidence intervals for the set of statistically significant variables in the bivariate analysis.
3. Results
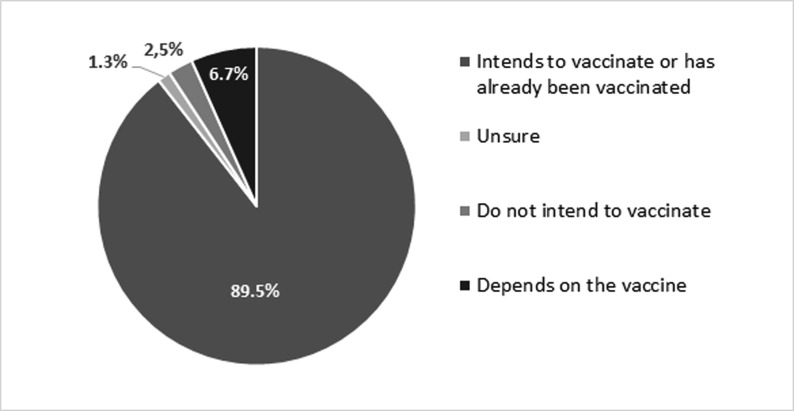
After exclusions (14,096), a total of 173,178 answers were included for analysis. The exclusions were: respondents that do not meet the inclusion criteria because were not Brazilians (1,019) or not residing in Brazil (4 5 1), blank forms (1,459) and duplicated records (11,167). The great majority of Brazilians who participated in the survey intended to be vaccinated (150,845) or had already been vaccinated against COVID-19 (4,083). Vaccine hesitancy was observed in 10.5% (18,250), and of these, 2.5% (4,401) did not intend to be vaccinated, 1.3% (2,274) were unsure, and 6.7% (11,575) would only agree to be vaccinated depending on the vaccine that was available, as shown in Fig. 1 .
Fig. 1.
Percentage of intention to vaccinate for COVID-19 among Brazilian adults in the study.
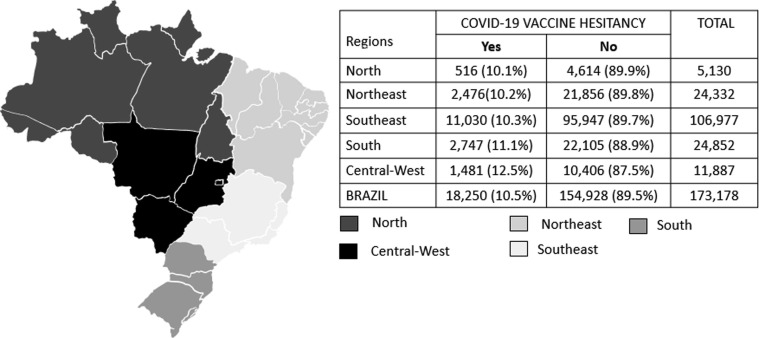
All 26 states of Brazil and the Federal District were represented in the study sample. The highest vaccine hesitancy rate was observed in the Central-West region, followed by the South, Southeast, Northeast, and North. Fig. 2 shows the number of respondents and intention to vaccinate according to major geographic region of the country. The majority lived in the state capitals, which showed lower vaccine hesitancy (10.1%) than those living in other areas of the states (11.4%).
Fig. 2.
Intention to vaccinate for COVID-19 according to major geographic regions of Brazil.
Vaccine hesitancy was assessed according to sociodemographic, COVID-19-related, and vaccine-related variables, as shown in Table 1 . Of the study population, 24,196 participants (14%) reported having had a positive COVID-19 diagnosis and 103,225 (59.6%) reported that a family member had died or been admitted to the ICU due to COVID-19, reflecting the impact of the disease on the study population. Having little or no fear of developing COVID-19 was a behavioral factor related to higher vaccine hesitancy. Vaccine hesitancy was also high in individuals who thought that the vaccine was unnecessary for individuals who had already had COVID-19. We identified 460 respondents who stated that they were against all traditionally used vaccines. In this group of individuals with outright anti-vax behavior, 86.7% showed vaccine hesitancy for the prevention of COVID-19. Among those who reported being in favor without restrictions of traditionally performed vaccines, 7.7% showed vaccine hesitancy for the prevention of COVID-19.
Table 1.
Vaccine hesitancy according to sociodemographic, COVID-19-related, and vaccine-related variables.
| Variables | COVID-19 vaccine hesitancy |
p-value | |
|---|---|---|---|
| Yes (18,250) | No (1,54,928) | ||
| Gender | |||
| Female | 10,249 (8.8%) | 106,037 (91.2%) | |
| Male | 7,887 (14%) | 48,261 (86%) | 0.000 |
| Other or missing | 114 (15.3%) | 630 (84.7%) | |
| Age bracket (years) | |||
| 18–39 | 4,429 (8.7%) | 46,452 (91.3%) | 0.000 |
| 40–59 | 8,573 (11%) | 69,505 (89%) | |
| 60–74 | 4,742 (11.8%) | 35,452 (88.2%) | |
| ≥75 | 506 (12.6%) | 3,519 (87.4%) | |
| Ethnicity | |||
| White | 13,138(10.7%) | 109,913 (89.3%) | 0.002 |
| Non-white | 5,052 (10.2%) | 44,651 (89.8%) | |
| Schooling | |||
| Primary or less | 471 (15.9%) | 2,498 (84.1%) | 0.000 |
| Incomplete secondary | 3,749 (13.2%) | 24,586 (86.8%) | |
| Complete secondary or more | 13,998 (9.9%) | 127,713 (90.1%) | |
| Family income (monthly) | |||
| None | 614 (16.1%) | 3,188 (83.9%) | 0.000 |
| ≤ $197.17 | 801 (12.5%) | 5,586 (87.5%) | |
| $197.18–$788.67 | 2,881 (10.8%) | 23,754 (89.2%) | |
| $788.68–$985.85 | 2,828 (9.9%) | 25,788 (90.1%) | |
| $985.86–1971.70 | 4,521 (9.7%) | 42,133 (90.3%) | |
| >$ 1972 | 6,217 (10.6%) | 52,643 (89.4%) | |
| Children | |||
| Yes | 13,198(11.9%) | 97,982 (88.1%) | 0.000 |
| No | 5,010 (8.1%) | 56,692 (91.9%) | |
| Residence in state capital | |||
| Yes | 10,732 (10%) | 96,409 (90%) | 0.000 |
| No | 7,452(11.4%) | 58,037 (88.6%) | |
| Have you had COVID? | |||
| Yes | 3,456 (14.3%) | 20,740 (85.7%) | 0.000 |
| No | 11,193 (9%) | 112,489 (91%) | |
| How important is the vaccine for someone who has already had COVID-19? | |||
| Not important | 2,434 (90.6%) | 253 (9.4%) | |
| Not very important | 2,801 (55.9%) | 2,211 (44.1%) | |
| I dońt know | 3,827 (39%) | 5,986 (61%) | 0.000 |
| Important | 3,961 (14.6%) | 23,172 (85.4%) | |
| Very important | 5,195 (4%) | 123,127 (96%) | |
| Has a family member died or been admitted to ICU for COVID-19? | |||
| Yes | 10,246 (9.9%) | 92,979 (90.1%) | |
| No | 7,947 (11.4%) | 61,581 (88.6%) | 0.000 |
| How afraid are you of COVID-19? | |||
| Ím not afraid | 3,754 (23.6%) | 12,185 (76.4%) | |
| A little afraid | 3,776 (26.9%) | 10,258 (73.1%) | 0.000 |
| More or less | 5,161 (13.9%) | 31,925 (86.1%) | |
| Very afraid | 4,597 (5.5%) | 78,631 (94.5%) | |
| Terrified | 926 (4.1%) | 21,742 (95.9%) | |
| Afraid of adverse reactions to the vaccine? | |||
| No | 1,440 (1.5%) | 91,593 (98.5%) | |
| A little | 5,664(10.3%) | 49,153 (89.7%) | 0.000 |
| Very | 10,334 (67.1%) | 5,076 (32.9%) | |
| Indifferent | 768 (7.9%) | 8,965 (92.1%) | |
| Importance of efficacy in decision to vaccinate | |||
| No | 4,758 (3.1%) | 147,672 (96.9%) | |
| Yes | 8,927 (66.6%) | 4,480 (33.4%) | |
| I dońt understand efficacy data | 1,246 (38.7%) | 1,976 (61.3%) | 0.000 |
| Indifferent | 3,083 (95.5%) | 144 (4.5%) | |
| Is the vaccinés country of origin important in the decision to vaccinate? | |||
| Yes | 9,106 (27.3%) | 24,227 (72.7%) | |
| No | 9,144(6.5%) | 130,701 (93.5%) | 0.000 |
3.1. Preference and rejection of vaccines
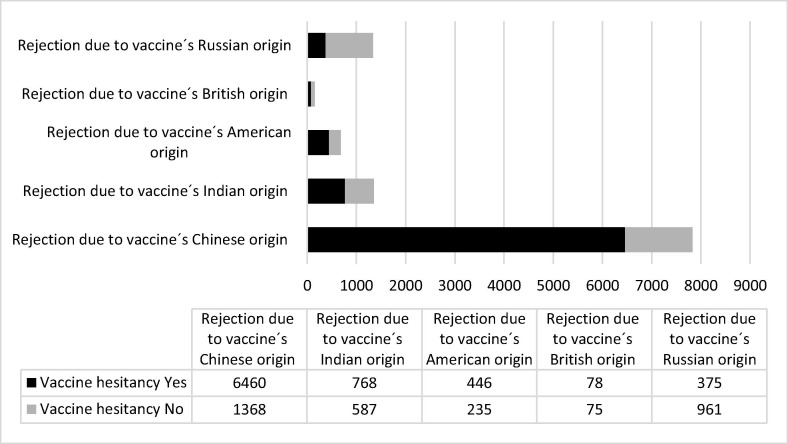
A total of 6.7% of participants stated that their decision to vaccinate depended on which vaccine was available, evidencing an issue of vaccine preference. The survey assessed whether vaccine preference was related to efficacy, country of origin, and/or fear of adverse reactions. Vaccine efficacy was reported as an important factor in the vaccination decision by 13,407 participants, showing vaccine hesitancy of 66.6% in this group. The vaccinés country of origin was reported as a factor in the vaccination decision by 33,333 participants, showing 27.3% vaccine hesitancy in this group.
Fig. 3 shows the rejection data according to the vaccine's country of origin. Although some vaccines are produced by pharmaceutical industries of different countries, the perception in Brazil of linkage between the brand and the country of vaccinés origin frequently assumes the brand of Coronavac to chinese origin, Sputinik to russian origin, Covishield to british origin, Pfizer to north american origin and Covaxin to indian origin. The highest degree of rejection related to country of origin was for the chinese vaccine, reported by 7,828 participants. Considering the total number of vaccine-hesitant individuals in this study, or 18,250 participants, 35.4% of these cited the chinese vaccine as one of the factors for not wanting to get vaccinated.
Fig. 3.
Degree of rejection of vaccine due to country of origin linked to the brand of the vaccine. More than one answer was allowed.
3.2. Multivariate logistic regression for prediction of vaccine hesitancy
Multivariate logistic regression analysis was performed to identify groups with higher and statistically significant odds ratios for predicting vaccine hesitancy (see Table 2 ). Assessment of the vaccinés efficacy in the decision to vaccinate showed by far the highest AOR (AOR = 16.39), followed by fear of adverse reactions (AOR = 11.230), importance of the vaccinés country of origin (AOR = 3.72), male gender (AOR = 1.62), having children (AOR = 1.29), 9 years of schooling or less (AOR = 1.31), residence in the Central-West region (AOR = 1.19), age over 40 years (AOR = 1.17), and monthly income less than U$788.68 (AOR = 1.13).
Table 2.
Multivariate logistic regression for predicton of vaccine hesitancy in study participants.
| Variables | β | Wald | p-value | AOR (95 %CI) |
|---|---|---|---|---|
| Gender (male vs. female and other) | 0.481 | 471.304 | 0.000 | 1.62 (1.55–1.69) |
| Age 40 years or older | 0.155 | 33.391 | 0.000 | 1.17 (1.11–1.23) |
| White ethnicity | 0.115 | 22.940 | 0.000 | 1.12 (1.07–1.17) |
| Schooling ≤ 9 years vs. other | 0.267 | 13.401 | 0.000 | 1.31 (1.13–1.50) |
| Monthly income < U$788.68 | 0.126 | 23.114 | 0.000 | 1.13 (1.08–1.20) |
| Children (yes) | 0.257 | 103.994 | 0.000 | 1.29 (1.23–1.36) |
| Residence in state capital | −0.58 | 6.955 | 0.000 | 0.94 (0.90–0.98) |
| Fear of catching COVID-19 | −1.56 | 2650.922 | 0.000 | 0.21 (0.20–0.22) |
| Family member died or admitted to ICU for COVID-19 | −1.71 | 63.543 | 0.000 | 0.84 (0.81–0.88) |
| Fear of adverse reactions | 2.42 | 7554.637 | 0.000 | 11.23 (10.63–11.85) |
| Residence in Central-West region | 0.173 | 18.710 | 0.000 | 1.19 (1.10–1.28) |
| Vaccinés country of origin affects decision | 0.22 | 3594.870 | 0.000 | 3.72 (3.56–3.88) |
| Vaccinés efficacy affects decision | 2.80 | 12368.47 | 0.000 | 16.39 (15.60–17.21) |
| Constant | −3.75 | 5987.47 | 0.000 | 0.24 |
Factors associated with lower vaccine hesitancy were residence in the state capital (AOR = 0.94), having a family member that died or was admitted to intensive care for COVID-19 (AOR = 0.84), and fear of catching COVID-19 (AOR = 0.21).
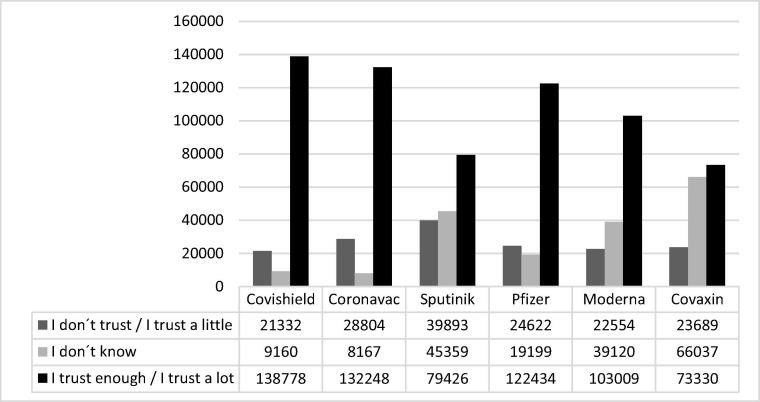
3.3. Vaccine confidence
Fig. 4 shows trust in the vaccines. The vaccines with the highest confidence were Covishield (80.13%), CoronaVac (76.36%), Pfizer/BioNTech (70.6%), Moderna (59.58%), Sputnik (45.86%), and Covaxin (42.34%).
Fig. 4.
Confidence according to specific vaccines.
4. Discussion
With 173,178 participants, this study assess the intention to vaccinate for COVID-19 in resident Brazilians. The study covers all regions of the country in the context of the recent emergency approval of vaccines to contain the COVID-19 pandemic. The study showed that despite the political context, antivax movements, and proliferation of controversial opinions in the social media, Brazilians reported an extremely high rate of intention to vaccinate (89.5%). Even among vaccine-hesitant individuals (10.5% of the sample), only 2.5% did not intend to vaccinate at all, while 8% were unsure or were only willing to vaccinate with a specific vaccine, demonstrating even greater potential for adherence to awareness-raising campaigns, which have still not been conducted in the country. Higher levels of vaccine hesitancy have been observed in other countries, specially in the beginning of pandemic. A survey on intention to vaccinate in June in the United States found that only 52% of the study population was very willing to be vaccinated [12]. A telephone survey in Hong Kong in July and August 2020 during the third wave of the COVID-19 epidemic assessed the intention to vaccinate in 1,200 individuals and found a rate of only 42.2% [13]. A study in the United Kingdom also assessed intention to vaccinate for prevention of COVID-19 when a vaccine became available in 32,361 adults and showed that 64% intended to vaccinate, 23% were unsure, and 14% did not intend to vaccinate [14]. A study in China surveyed 3,541 persons and found intention to vaccinate for the prevention of COVID-19 in 28.7% of respondents [15]. However, as vaccines to prevent covid-19 became available some change in the hesitancy profile was observed. In United States of America, a national survey that recruited 443,680 respondents from January to March 2021 showed an overall 13% COVID-19 vaccine hesitancy what is consistent with a significant drop in hesitancy [16]. But some countries still have high rates of hesitancy as show by a study that assessed the attitudes towards COVID-19 vaccines among the general public in Jordan, Kuwait and other Arab countries and found a rate of acceptance of 29,4% [17]. Similarly, a phone-based survey in february 2021 in four couties of Kenya showed that COVID-19 vaccine hesitancy was high: 36,5% [18].
The high correlation between fear of COVID-19 and vaccine adherence was expected. However, an important finding was the identification of people who had little or no fear of the disease (n = 29,973; 17.3% of respondents), despite the high number of COVID-19 deaths in Brazil. This group may represent a portion of the population that has difficulty accepting or understanding data on the pandemic, behaving as science denialists [19]. It is important to address this issue, since vaccine hesitancy in this group was high, at 26%.
More than two-thirds of the participants in the study were women (67.1%), which has also been seen other studies [12], [13], [14], [15]. However, vaccine hesitancy was higher in men, unlike findings in other studies [4], [12], [14]. This is relevant in the context of COVID-19, since men show higher risk of severe clinical evolution, indicating that campaigns should also focus on this more vaccine-hesitant gender [20]. Some authors have suggested that this involves a sociocultural issue, where men are more likely to disguise fear and reject preventive practices, explaining this higher vaccine hesitancy rate in men [21], [22].
The vaccine hesitancy rate was inversely related to schooling and income, corroborating other studies [12], [14].
Among respondents that stated being against all the vaccines already in use for other diseases, that is, with an antivax profile, 13.3% were willing to take the COVID-19 vaccine. This may indicate a possible turning point caused by the impact of COVID-19 on everyonés lives, leading to a rethinking of radical antivax positions. However, definitive conclusions cannot be established, since the survey only identified a small group of persons with an antivax profile (0.26% of respondents), possibly reflecting limited interest by this group in answering questionnaires on this topic.
Even with these low vaccine hesitancy rates when compared to other countries, the identification of fear of adverse reactions (11.23 time higher in the vaccine hesitancy group) can help orient awareness-raising campaigns on the vaccineś safety, further increasing vaccination adherence. Our data also showed that parents present higher vaccine hesitancy (11.9%), which has been reported in other studies [12], [14]. Fear of an adverse reaction to the vaccine that would prevent them from caring for their children has been suggested as a possible cause of this hesitancy. Even among participants who stated being in favor of the traditionally used vaccines, 7.7% showed vaccine hesitancy for the prevention of COVID-19, which may also reflect concern over this vaccinés safety.
Considering that 13,407 participants viewed the vaccinés efficacy as an important factor in the decision to vaccinate, but that more than double this number (33,333) cited the vaccinés country of origin as an important factor, the population may not consider only technical issues in their vaccine preference. Vaccine confidence (or lack thereof) does not depend exclusively on knowledge or disinformation, but on an ecosystem of culture, politics, personal experiences, beliefs, and life histories [23]. A previous study had already shown that Americans preferred vaccines produced in the United States and rejected those produced in the United Kingdom, Russia, and especially China [6]. Rejection of the Chinese origin of the vaccine among Brazilians in the current survey may have originated from fake news, portraying China as the intentional source of the virus with the subsequent objective of selling the vaccine, as well as political disputes between opposing groups in Brazil. However, alongside the Covishield vaccine, the Chinese CoronaVac vaccine is also positively rated in Brazil. The two vaccines were considered the most reliable, ahead of the Pfizer and Moderna vaccines, whose efficacy has been rated higher in clinical trials. The trust in and respect for these vaccines can probably be explained by the fact that these are the vaccines currently supplied to the Brazilian population and the ones produced in partnerships with nationally renowned research institutes, namely FIOCRUZ and the Butantan Institute.
Among the studýs limitations, although the survey was answered by persons from all regions of Brazil, the Southeast accounted for 61.8% of the respondents, which may have created a selection bias. Another important limitation was the lower proportion of respondents with low schooling and income, since these strata presented higher vaccine hesitancy. Given that 46.6% of the Brazilian population 25 years or older has nine years of schooling or less, the true vaccine hesitancy rate may be higher than measured in this study [15].
According to this study, Brazilians have high intention to vaccinate to prevent COVID-19, evidencing that access to the vaccine is a bigger problem than vaccine hesitancy in Brazil. In this context, wealthy countries, which represent a small proportion of the world population, have already purchased more than 53% of the available vaccines, and vaccine developers have shown no intention to share the technology, thus drastically curtailing vaccination coverage in poor countries in 2021 [24]. As already discussed, the lack of access to vaccines in low- and middle-income countries, with 75% of the world́s population, seriously challenges global responsibility and equity [25]. There are currently two vaccines available in Brazil, CoronaVac (Sinovac) and Covishield (AstraZeneca/Oxford's AZD1222), with low numbers of doses in relation to the Brazilian population, leading to slow immunization, even in the priority groups. The global context notwithstanding, it is not possible to exempt local leaders and government from their responsibility in this short supply of vaccine doses [26]. It is essential to guarantee access to the vaccine and fight vaccine hesitancy, which is comparatively less in Brazil than in other countries, although in absolute terms it is quite relevant because of Braziĺs large population. This study is of particular importance because it was carried out in the first week of the availability of the vaccine for the prevention of covid-19 in the national territory. Some factors have been identified as important in influencing the vaccine hesitancy and can now be tracked over time It is important to focus special attention on population strata with low schooling and income, besides dealing with sociocultural issues related to males, since these groups concentrate higher vaccine hesitancy rates and require adequate communication strategies.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.MonitoraCovid-19 [Internet]. [citado 12 de outubro de 2020]. Disponível em: https://bigdata-covid19.icict.fiocruz.br/.
- 2.Sabino E.C., Buss L.F., Carvalho M.P.S., Prete C.A., Crispim M.A.E., Fraiji N.A., et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet 6 de fevereiro de. 2021;397(10273):452–455. doi: 10.1016/S0140-6736(21)00183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown AL, Sperandio M, Turssi CP, Leite RMA, Berton VF, Succi RM, et al. Vaccine confidence and hesitancy in Brazil. Cadernos de Saúde Pública [Internet]. 2018 [citado 2 de fevereiro de 2021];34(9). Disponível em: http://www.scielo.br/scielo.php?script=sci_abstract&pid=S0102-311X2018000905014&lng=en&nrm=iso&tlng=en. [DOI] [PubMed]
- 4.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol [Internet]. 1o de agosto de 2020 [citado 24 de janeiro de 2021];35(8):775–9. Disponível em: https://doi.org/10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed]
- 5.Dubé E., MacDonald N.E. How can a global pandemic affect vaccine hesitancy? Expert Rev Vaccines outubro de. 2020;19(10):899–901. doi: 10.1080/14760584.2020.1825944. [DOI] [PubMed] [Google Scholar]
- 6.Motta M. Can a COVID-19 vaccine live up to Americans’ expectations? A conjoint analysis of how vaccine characteristics influence vaccination intentions. Soc Sci Med. 2020:113642. doi: 10.1016/j.socscimed.2020.113642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K., et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):29. doi: 10.1038/s41467-020-20226-9. 4 de janeiro de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwok KO, Lai F, Wei WI, Wong SYS, Tang JWT. Herd immunity – estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect [Internet]. junho de 2020 [citado 15 de janeiro de 2021];80(6):e32–3. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151357/. [DOI] [PMC free article] [PubMed]
- 9.Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature março de. 2021;591(7851):520–522. doi: 10.1038/d41586-021-00728-2. [DOI] [PubMed] [Google Scholar]
- 10.Covid-19 Casos e Óbitos [Internet]. [citado 1o de setembro de 2021]. Disponível em: https://qsprod.saude.gov.br/extensions/covid-19_html/covid-19_html.html.
- 11.MacDonald N.E. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. 14 de agosto de. [DOI] [PubMed] [Google Scholar]
- 12.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health. 2021 doi: 10.1007/s10900-020-00958-x. 3 de janeiro de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong M.C.S., Wong E.L.Y., Huang J., Cheung A.W.L., Law K., Chong M.K.C., et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine. 2021 doi: 10.1016/j.vaccine.2020.12.083. 6 de janeiro de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet Regional Health - Europe [Internet]. 26 de dezembro de 2020 [citado 30 de janeiro de 2021];0(0). Disponível em: https://www.thelancet.com/journals/lanepe/article/PIIS2666-7762(20)30012-0/abstract. [DOI] [PMC free article] [PubMed]
- 15.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl Trop Dis [Internet]. 17 de dezembro de 2020 [citado 30 de janeiro de 2021];14(12). Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7775119/. [DOI] [PMC free article] [PubMed]
- 16.Liu R., Li G.M. Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM Popul Health setembro de. 2021;15 doi: 10.1016/j.ssmph.2021.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sallam M., Dababseh D., Eid H., Al-Mahzoum K., Al-Haidar A., Taim D., et al. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines (Basel) 2021;9(1) doi: 10.3390/vaccines9010042. 12 de janeiro de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orangi S., Pinchoff J., Mwanga D., Abuya T., Hamaluba M., Warimwe G., et al. Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya. Vaccines (Basel) 2021;9(8):936. doi: 10.3390/vaccines9080936. 23 de agosto de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller B.L. Science Denial and COVID Conspiracy Theories: Potential Neurological Mechanisms and Possible Responses. JAMA. 2020;324(22):2255–2256. doi: 10.1001/jama.2020.21332. 8 de dezembro de. [DOI] [PubMed] [Google Scholar]
- 20.Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nature Communications [Internet]. 9 de dezembro de 2020 [citado 30 de janeiro de 2021];11(1):6317. Disponível em: https://www.nature.com/articles/s41467-020-19741-6. [DOI] [PMC free article] [PubMed]
- 21.Griffith DM, Sharma G, Holliday CS, Enyia OK, Valliere M, Semlow AR, et al. Men and COVID-19: A Biopsychosocial Approach to Understanding Sex Differences in Mortality and Recommendations for Practice and Policy Interventions. Prev Chronic Dis [Internet]. 16 de julho de 2020 [citado 30 de janeiro de 2021];17. Disponível em: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7380297/. [DOI] [PMC free article] [PubMed]
- 22.Medrado B, Lyra J, Nascimento M, Beiras A, Corrêa ÁC de P, Alvarenga EC, et al. Homens e masculinidades e o novo coronavírus: compartilhando questões de gênero na primeira fase da pandemia. Ciência & Saúde Coletiva [Internet]. janeiro de 2021 [citado 3 de fevereiro de 2021];26(1):179–83. Disponível em: http://www.scielo.br/scielo.php?script=sci_abstract&pid=S1413-81232021000100179&lng=en&nrm=iso&tlng=pt. [DOI] [PubMed]
- 23.Rapid Review: Vaccine Hesitancy and Building Confidence in COVID-19 Vaccination | GOARN [Internet]. [citado 6 de março de 2021]. Disponível em: https://extranet.who.int/goarn/rapid-review-vaccine-hesitancy-and-building-confidence-covid-19-vaccination.
- 24.Dyer O. Covid-19: Many poor countries will see almost no vaccine next year, aid groups warn. BMJ [Internet]. 11 de dezembro de 2020 [citado 11 de fevereiro de 2021];371:m4809. Disponível em: https://www.bmj.com/content/371/bmj.m4809. [DOI] [PubMed]
- 25.The people’s vaccine: How a covid-19 vaccine will be a test of global accountability and equity [Internet]. The BMJ. 2020 [citado 11 de fevereiro de 2021]. Disponível em: https://blogs.bmj.com/bmj/2020/12/15/the-peoples-vaccine-how-a-covid-19-vaccine-will-be-a-test-of-global-accountability-and-equity/.
- 26.Abbasi K. Covid-19: Social murder, they wrote-elected, unaccountable, and unrepentant. BMJ. 2021;372:n314. doi: 10.1136/bmj.n314. In this issue. [DOI] [PubMed] [Google Scholar]