Abstract
Background
While COVID-19 vaccine uptake has been encouraging overall, some individuals are either hesitant towards, or refuse, the vaccine. Protection Motivation Theory (PMT) has been applied to influenza vaccine acceptance, but there is a lack of research applying PMT to COVID-19 vaccine acceptance. Additionally, prior research has suggested that coronavirus conspiracy beliefs and demographic factors may play a role in attitudes towards the vaccine. This study aimed to predict COVID-19 vaccination intention using PMT, coronavirus conspiracy beliefs, and demographic factors. Furthermore, vaccinated and unvaccinated individuals were compared in relation to their coronavirus conspiracy beliefs.
Methods
An online survey was administered to 382 (278 vaccinated, and 104 unvaccinated) individuals in the United Kingdom (77 males, 301 females, one non-binary/third gender, and three unstated). Respondents’ mean age was 43.78 (SD = 12.58).
Results
A hierarchical multiple linear regression was performed in three stages. Initially, four PMT constructs - severity, susceptibility, maladaptive response costs, and self-efficacy - emerged as significant predictors of COVID-19 vaccination intention. The final model accounted for 75% of the variance and retained two significant predictors from PMT - maladaptive response rewards and self-efficacy - alongside coronavirus conspiracy beliefs and age. An independent t-test established that unvaccinated individuals held greater coronavirus conspiracy beliefs than vaccinated ones.
Conclusions
Interventions and campaigns addressing COVID-19 vaccine acceptance should employ strategies increasing individuals’ perceived severity of COVID-19, perceived susceptibility, and perceived ability to get vaccinated, while decreasing perceived rewards of not getting vaccinated. Additionally, coronavirus conspiracy beliefs should be addressed, as these appear to play a role for some vaccine-hesitant individuals.
Keywords: COVID-19, Vaccination hesitancy, Conspiracy theories, Protection Motivation Theory
1. Introduction
Efforts to vaccinate the world population against COVID-19 are ongoing. At the end of May 2021, around 1.86 billion doses had been administered worldwide [1]. The COVID-19 vaccine programme has been rolled out rapidly across the United Kingdom [UK] [2]. While uptake has been encouraging [3], surveys have indicated that there are a significant number of people who are sceptical of the vaccine, and who would either be hesitant to receive it, or refuse it altogether [4], [5], [6]. In the UK, most of the people who have been hospitalised with COVID-19 are those who have not been fully vaccinated [7]. Therefore, to reduce hospitalisations and mortality rates, it is important that as many eligible individuals as possible are fully vaccinated against COVID-19.
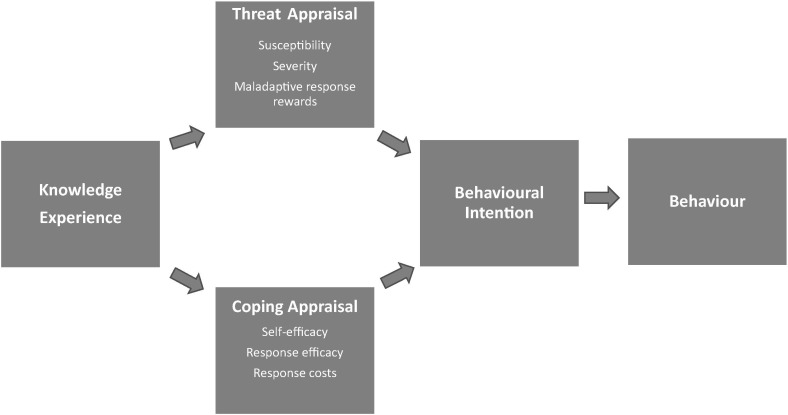
Behavioural research has identified three drivers of vaccine uptake, in addition to possessing the necessary knowledge: an enabling environment, social influences and motivation [8]. Protection Motivation Theory (PMT) [9] is a social cognition theory which attempts to explain motivation to respond to health threats such as COVID-19. According to PMT, the likelihood of engaging in a protective behaviour - such as being vaccinated - when faced with a threat is a product of the beliefs that individuals hold about engaging, or not engaging, in this protective behaviour as well as about the threat itself (see Fig. 1 ).
Fig. 1.
Protection Motivation Theory.
In PMT, intention most closely predicts behaviour. Intention itself is determined by both threat appraisal and coping appraisal. Threat appraisal is the result of one’s perceived vulnerability to the negative consequences of the threat (susceptibility), how serious one perceives these negative consequences to be (severity), and perceived benefits of engaging in behaviour that is maladaptive in relation to the threat (maladaptive response rewards). Coping appraisal is the product of confidence in one's perceived ability to successfully engage in the preventative behaviour (self-efficacy), beliefs about how effective the protective behaviour is at preventing the negative consequences of the threat (response efficacy), and any barriers affecting performance of the protective behaviour (response costs). PMT posits that, faced with a threat to their health, people are most likely to perform a protective behaviour when they believe that not acting poses a threat to themselves (high threat appraisal) and that engaging in the protective behaviour will reduce that threat (high coping appraisal).
PMT has been applied to seasonal influenza vaccine acceptability and uptake (e.g., [10], [11], [12], [13]), and to predict COVID-19 vaccination intention among Chinese university students [14]. However, no published studies examine the use of PMT to predict COVID-19 vaccination intention in the general UK population. COVID-19 is affecting not just the general population of the UK, but the global population. It is important that common theories of health behaviour and health behaviour change, such as PMT, be applied to COVID-19 vaccination intention in the general population, as this will allow for theory-based interventions to be designed to reach as many as possible, to increase vaccine uptake.
Conspiracy beliefs have been examined in relation to beliefs about COVID-19. These have shown to be prevalent in a significant minority and to be associated with less adherence to coronavirus government guidelines and lower willingness to take diagnostic or antibody tests or get vaccinated [4], [6]. The role of conspiracy beliefs in intention to receive a COVID-19 vaccination has not yet been explored extensively, nor alongside PMT in vaccination intention more broadly. As such beliefs are prevalent in a significant minority and may lower vaccine uptake [4], determining the extent of their influence on intention to get a COVID-19 vaccine is key to developing interventions for COVID-19 vaccine uptake.
In addition to psychological factors, demographic factors have been shown to be associated with COVID-19 vaccine hesitancy, namely age, gender [4], [15], [16], ethnicity [4], [5], [17], and education [15], [16]. Furthermore, religiosity has been shown to be negatively correlated with COVID-19 vaccination intention [18]. However, findings on the influence of demographic factors are mixed.
The current study aimed to predict COVID-19 vaccination intention in the UK population using PMT, coronavirus conspiracy beliefs, and demographic factors. We also sought to establish whether there were significant differences between those vaccinated for COVID-19 and unvaccinated individuals in relation to coronavirus conspiracy beliefs.
We hypothesised that COVID-19 vaccination intention would have significant positive relationships with
H1. perceived susceptibility to COVID-19
H2. perceived severity of contracting COVID-19
H3. perceived efficacy of the COVID-19 vaccine (response efficacy); and
H4. confidence in ability to obtain a COVID-19 vaccine (perceived self-efficacy).
We hypothesised that COVID-19 vaccination intention would have significant negative relationships with
H5. perceived response costs
H6. maladaptive response rewards; and
H7. coronavirus conspiracy beliefs.
H8. A significant difference in levels of coronavirus conspiracy beliefs was expected between individuals who had not been vaccinated for COVID-19 and those who had been vaccinated.
Additionally, the influence of demographic factors (ethnicity, age, gender, religiosity, and education) on intention to be vaccinated was also examined. Due to the inconsistent findings on the influence of these demographic variables, no hypotheses were generated for these; we nevertheless aimed to assess their influence on COVID-19 vaccination intention, if any.
2. Method
2.1. Design
The present study was correlational and used an online survey. The criterion variable was COVID-19 vaccination intention. Predictors were the PMT constructs (perceived severity of COVID-19, perceived susceptibility to COVID-19, perceived efficacy of the vaccine [response efficacy], confidence in one's ability to obtain a vaccination [self-efficacy], maladaptive response rewards and perceived response costs) and level of coronavirus conspiracy beliefs. Relevant demographic variables - ethnicity, age, gender, religiosity, and education - were also assessed.
2.2. Participants
Individuals eligible to participate in the study included anyone aged 18 or older and residing in the UK. Recruitment took place by disseminating the link to the online survey via social media, email, distributing flyers, and via an interview on a public radio station. Participants received no monetary or material rewards for their participation. Table 1 shows demographic characteristics of the respondents.
Table 1.
Demographic characteristics of respondents.
| Overall | ||
|---|---|---|
| N | 382 | |
|
278 | |
|
104 | |
| Age in years M (SD) | 43.78 (12.58) | |
| Age category | N (%) | |
| 18–29 | 59 (15.4) | |
| 30–39 | 81 (21.2) | |
| 40–49 | 114 (29.8) | |
| 50–59 | 84 (22) | |
| 60–69 | 39 (10.2) | |
| 70–79 | 4 (1) | |
| 80+ | 1 (0.3) | |
|
46.98 (12.01) | |
|
35.25 (9.85) | |
| Ethnicity (%) | White | 351 (91.9) |
| Non-White | 31 (8.1) | |
| Level of education (%) | No qualifications | 7 (1.8) |
| General Certificate of Secondary Education (equivalent to school leavers’ certificate) | 34 (8.9) | |
| Advanced level qualifications (equivalent to high school diploma) | 61 (16.0) | |
| Higher education (e.g., BA, BSc, or equivalent) | 141 (36.9) | |
| Postgraduate qualifications (e.g., MA, MSc, PhD, DPhil) | 139 (36.4) | |
| Religiosity M (SD) | Single item: ‘How important is religion in your life?’ (Five-point Likert scale; 1 = not important at all, 5 = extremely important) | 1.91 (1.25) |
A prospective power analysis conducted using the G*Power software, version 3.1.9.7 [19] established that for a power of 0.80 and with 12 predictors, a sample size of 127 would be needed to detect a medium effect size in a multiple linear regression analysis. A separate prospective power analysis for an independent t-test comparing vaccinated to unvaccinated individuals showed that for a power of 0.80, 128 respondents would be required to detect a medium effect size. A total of 382 individuals from nine regions in England, as well as in Scotland and Wales, completed the survey (77 males, 301 females, one non-binary/third gender, three preferred not to state their gender). The mean age was 43.78 (SD = 12.58). Of these, 278 respondents (72.8%) reported having had a COVID-19 vaccination, and 104 (27.2%) reported not having had one. The COVID-19 vaccination programme was being rolled out in the UK by age groups at the time this study was carried out, with older people being offered the vaccine before younger ones. At the time data collection ceased, all those aged 34 and older [20], as well as clinically extremely vulnerable individuals [21], frontline health and social care workers [22], [23], and individuals with underlying health conditions [24] were being offered the vaccine - a substantial proportion of the adult population. Still, the mean age of vaccinated individuals was higher (M = 46.98, SD = 12.01), than that of unvaccinated individuals (M = 35.25, SD = 9.85). An independent t-test established that this age difference was significant, t(223.70) = 9.73, p < .0001.
2.3. Measures
An adapted version of the PMT questionnaire [13] was used to measure the PMT constructs. Table 2 shows all PMT items by construct with associated internal consistency (Cronbach’s α). All subscales have previously been shown to have moderate to high internal consistency, ranging from α = 0.57 to α = 0.98 [13]. The original items were worded to assess PMT constructs in relation to the seasonal influenza vaccine. For the present study, these were adapted to assess these constructs in relation to the COVID-19 vaccine. On all subscales, participants indicated their agreement on a five-point Likert scale, ranging from 1 = strongly disagree, to 5 = strongly agree. Scores on each subscale were calculated as the mean of the items on each subscale. Items were reversed where necessary. Higher scores on each subscale indicated higher degrees of the particular construct.
Table 2.
Protection Motivation Theory items
| Construct and associated internal consistency | Items |
|---|---|
| Intention (α = 0.99) | I intend to have a COVID-19 vaccination. |
| I plan to have a COVID-19 vaccination. | |
| I expect to have a COVID-19 vaccination. | |
| Susceptibility (α = 0.78) | Without being vaccinated for COVID-19, I am vulnerable to contracting COVID-19. |
| Even if I don't get vaccinated for COVID-19, I don't think I'm likely to get COVID-19. | |
| If I don't get vaccinated for COVID-19 I am at risk of catching COVID-19. | |
| Severity (α = 0.74) | The negative impact of COVID-19 is very severe. |
| COVID-19 can be a life-threatening illness. | |
| COVID-19 is a serious illness for someone like me. | |
| Maladaptive response rewards (α = 0.57) | Not being vaccinated for COVID-19 would have some advantages for me. |
| If I am not vaccinated for COVID-19, then I will not have to worry about the safety of the vaccine. | |
| If I am not vaccinated for COVID-19, then I will not have to spend time and money getting vaccinated. | |
| Self-efficacy (α = 0.65) | I’d be able to be vaccinated for COVID-19 when it’s offered to me, if I wanted to. |
| Being vaccinated for COVID-19, once it's offered to me, would be difficult for me. | |
| Being vaccinated for COVID-19 is easy. | |
| Response efficacy (α = 0.75) | I’m sure that being vaccinated for COVID-19 would be effective in reducing my personal risk of contracting COVID-19. |
| Being vaccinated for COVID-19 would stop me from getting COVID-19. | |
| Being vaccinated for COVID-19 would guarantee that I will not get COVID-19. | |
| Response costs (α = 0.47) | Being vaccinated for COVID-19 would have some disadvantages for me. |
| Being vaccinated for COVID-19 is painful. | |
| The COVID-19 vaccine is expensive for me. |
Intention was assessed with three items in relation to COVID-19 vaccination intention. Susceptibility was measured with two items indicating in how far individuals perceived themselves as being vulnerable to the negative consequences of contracting COVID-19 and one item indicating lack of perceived susceptibility. Severity was a composite score calculated by averaging three items indicating that the negative impact of contracting COVID-19 is severe (α = 0.74). Higher perceived severity was indicated by higher scores. Maladaptive response rewards were measured with three items stating that there were perceived benefits to not getting a COVID-19 vaccination . Self-efficacy was assessed with two items indicating that individuals saw themselves as capable of getting a COVID-19 vaccination, and one item stating that it would be difficult for them to get a COVID-19 vaccination. Response efficacy was measured with three items indicating that receiving the COVID-19 vaccine would be effective in reducing vulnerability to and severity of the illness. Response costs were assessed with three items indicating that there were both financial and non-financial costs in relation to receiving a COVID-19 vaccination.
Conspiracy beliefs were assessed with the 7-item OCEANS Coronavirus Conspiracy Scale assessing general coronavirus conspiracy beliefs [6]. Items included statements on general beliefs about the coronavirus (e.g., “The virus is a hoax”) and participants indicated their agreement on a five-point Likert scale ranging from 1 = strongly disagree, to 5 = strongly agree. In the present study, internal consistency of the scale was high (α = 0.93).
Demographic variables were measured using multiple-choice items. Age was measured as a continuous variable; gender, ethnicity, and level of education were assessed using the UK census categories [25]. Religiosity was assessed with a single item (‘How important is religion in your life?’, measured using a five-point Likert scale ranging from 1 = not important at all to 5 = extremely important), in line with the Oxford Coronavirus Explanations, Attitudes, and Narratives Survey II [4].
2.4. Procedure
Ethics approval was granted by the institution of the last author. A website was set up to provide information on the study and a link to the survey on the online survey platform, Qualtrics. The website provided background information on the study and respondents were then invited to complete the anonymous online survey by clicking on the survey link. Respondents were presented with a consent form explaining the nature and aims of the study and were then asked to tick a box confirming that they had read and understood the information provided and that they would like to take part in the study. The survey took an average of five minutes to complete. Upon completion, respondents were presented with a screen thanking them for their time and providing a list of websites that could be accessed for more information on COVID-19 and vaccination. They were also encouraged to contact the National Health Service’s ‘NHS Direct’ website or their general practitioner if they had any coronavirus-related concerns.
2.5. Analysis
Version 26 of The Statistical Package for the Social Sciences [SPSS] [26] was used to analyse the data. A three-stage hierarchical multiple linear regression was performed on the survey data of respondents who had not had a COVID-19 vaccine (N = 104) to determine significant predictors of intention to receive a COVID-19 vaccination, as well as the relative contribution of each significant predictor and nature of its relationship to this outcome variable.
In line with previous research indicating the influence of PMT constructs on vaccination intention [13], these were entered at the first stage. Level of coronavirus conspiracy beliefs was entered at the second stage, and the demographic variables (age, gender, ethnicity – recoded into a dichotomous variable with two levels, White and non-White -, education, and religiosity) were entered at the third stage. Only respondents who reported not having had a COVID-19 vaccination were included in this analysis.
Additionally, an independent t-test was performed to compare individuals who had had a COVID-19 vaccine with those who had not had one in relation to their levels of coronavirus conspiracy beliefs.
3. Results
3.1. Descriptive statistics
To assess relationships between the PMT constructs, Pearson’s product-moment correlations were performed (see Table 2). As would be expected [13], nearly all constructs were significantly correlated with each other.
3.2. Inferential statistics
Due to the high levels of correlations between PMT constructs, tolerance and variance inflation factors (VIF) were examined for all predictors. None of the tolerance values were smaller than 0.1, and all VIF values were well below 10 [27]; thus, no multicollinearity was present. Results of the hierarchical multiple regression (see Table 3 ) showed that at stage 1, severity, susceptibility, maladaptive response rewards, and self-efficacy all contributed significantly to the regression model, with 68% of the variance in COVID-19 vaccination intention being accounted for. Adding conspiracy beliefs at stage 2 resulted in an additional 2% of the variance being explained, with the four predictors remaining significant, and conspiracy beliefs emerging as an additional and highly significant predictor of COVID-19 vaccination intention. Adding the demographic variables (age, gender, religiosity, level of education, and ethnicity) at stage 3 led to an additional 5% (75% in total) of the variance in COVID-19 vaccination intention being explained. Severity and susceptibility were no longer significant predictors, but maladaptive response rewards, self-efficacy, and conspiracy beliefs remained significant, and age emerged as an additional significant predictor of COVID-19 vaccination intention.
Table 3.
Correlations between variables measuring PMT constructs.
| Construct | M | SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
|
3.99 | 1.50 | ||||||
|
3.79 | 1.07 | 0.68** | |||||
|
3.89 | 0.91 | 0.58** | 0.65** | ||||
|
2.37 | 0.97 | -0.64** | -0.47** | -0.37** | |||
|
3.08 | 1.01 | 0.62** | 0.49** | 0.36** | -0.38** | ||
|
4.22 | 0.80 | 0.37** | 0.41** | 0.17 | -0.53** | 0.25* | |
|
2.15 | 0.76 | -0.60** | -0.60** | -0.37** | 0.64** | -0.41** | -0.59** |
*p < .05; **p < .01
The final model with all predictors showed that the lower the perceived rewards of not getting vaccinated for COVID-19, and the higher confidence in one's ability to obtain a vaccination, the higher the intention was to get vaccinated for COVID-19. Furthermore, the higher respondents’ level of conspiracy beliefs about COVID-19, and the older respondents were, the lower their intention to get vaccinated (see Table 4 ).
Table 4.
Results of hierarchical multiple linear regression predicting COVID-19 vaccination intention
| Predictor | β | 95% CI | t | R2 | R2 change | p |
|---|---|---|---|---|---|---|
| Stage 1 | 0.68 | 0.68 | ||||
| Intercept | [0.30, 4.58] | 2.01 | 0.047* | |||
| Severity | 0.17 | [0.02, 0.55] | 2.12 | 0.037* | ||
| Susceptibility | 0.23 | [0.06, 0.59] | 2.46 | 0.016* | ||
| Maladaptive response rewards | -0.31 | [-0.73, -0.22] | −3.72 | 0.000*** | ||
| Self-efficacy | 0.29 | [0.22, 0.64] | 4.13 | 0.000*** | ||
| Response efficacy | -0.05 | [-0.38, 0.20] | -0.61 | 0.544 | ||
| Response costs | -0.11 | [-0.57, 0.15] | −1.14 | 0.256 | ||
| Stage 2 | 0.70 | 0.02 | ||||
| Intercept | [0.66, 5.16] | 2.57 | 0.012** | |||
| Severity | 0.16 | [0.01, 0.52] | 2.04 | 0.045* | ||
| Susceptibility | 0.19 | [0.01, 0.52] | 2.03 | 0.045* | ||
| Maladaptive response rewards | -0.25 | [-0.64, -0.13] | −3.01 | 0.003** | ||
| Self-efficacy | 0.28 | [0.21, 0.61] | 4.07 | 0.000*** | ||
| Response efficacy | -0.05 | [-0.38, 0.19] | -0.67 | 0.506 | ||
| Response costs | -0.07 | [-0.49, 0.21] | -0.78 | 0.439 | ||
| Conspiracy beliefs | -0.20 | [-0.62, -0.09] | −2.64 | 0.010** | ||
| Stage 3 | 0.75 | 0.05 | ||||
| Intercept | [1.50, 7.74] | 2.95 | 0.004** | |||
| Severity | 0.11 | [-0.08, 0.43] | 1.36 | 0.177 | ||
| Susceptibility | 0.16 | [-0.02, 0.48] | 1.82 | 0.073 | ||
| Maladaptive response rewards | -0.20 | [-0.56, -0.07] | −2.55 | 0.013** | ||
| Self-efficacy | 0.18 | [0.05, 0.48] | 2.50 | 0.014** | ||
| Response efficacy | -0.08 | [-0.42, 0.14] | −1.02 | 0.312 | ||
| Response costs | -0.03 | [-0.40, 0.30] | -0.29 | 0.769 | ||
| Conspiracy beliefs | -0.35 | [-0.93, -0.31] | −3.98 | 0.000*** | ||
| Age | -0.24 | [-0.05, -0.01] | −3.23 | 0.002** | ||
| Gender | -0.01 | [-0.39, 0.35] | -0.12 | 0.904 | ||
| Religiosity | 0.10 | [-0.03, 0.27] | 1.54 | 0.127 | ||
| Level of education | 0.01 | [-0.16, 0.20] | 0.20 | 0.846 | ||
| Ethnicity | 0.08 | [-0.22, 1.13] | 1.34 | 0.183 | ||
*p < .05; **p < .01; ***p < .001.
Results of the t-test comparing COVID-19 vaccinated and unvaccinated individuals on their coronavirus conspiracy beliefs showed that unvaccinated individuals (M = 1.83, SD = 1.01) reported significantly higher levels of conspiracy beliefs than those who had been vaccinated (M = 1.58, SD = 0.78), t(138.73) = -2.25, p < 0.05.
4. Discussion
The present study aimed to establish the influence of PMT constructs, coronavirus conspiracy beliefs, and demographic factors, on individuals’ intention to get vaccinated for COVID-19. Furthermore, we aimed to compare those who had had the COVID-19 vaccine with those who had not been vaccinated in relation to their coronavirus conspiracy beliefs.
As expected [13], most of the PMT constructs correlated with each other. However, tolerance and VIF for all predictors were all acceptable [27] and did not show multicollinearity to be present. Therefore, these correlations were not of concern. We found that for the full regression model including all predictors, the lower respondents perceived rewards of not getting vaccinated for COVID-19 to be (maladaptive response rewards), and the higher their confidence in their ability to obtain a vaccination (self-efficacy), the higher their intention was to get vaccinated. Furthermore, the higher respondents’ coronavirus conspiracy beliefs were and the older they were, the lower their intention was to get vaccinated. Thus, in addition to two constructs from PMT – maladaptive response rewards and self-efficacy – coronavirus conspiracy beliefs and age both had independent effects on COVID-19 vaccination intention. Regression models with PMT constructs only, and with PMT constructs plus conspiracy beliefs, yielded additional significant PMT predictors in the form of perceived severity and perceived susceptibility: the higher perceived severity of COVID-19 and individuals’ perceived susceptibility to the disease, the higher their intention was to get vaccinated. These were non-significant in the full model, which suggests that demographic factors are of limited relevance to explaining COVID-19 vaccination intention; this has also been found in prior research on influenza vaccine intention [13]. Hence, four constructs from PMT predicted COVID-19 vaccination intention. Interventions and health promotion campaigns addressing vaccine uptake may need to aim for increasing individuals’ perceived severity of COVID-19, their perceived susceptibility to this illness, and their perceived ability to get the vaccine, while decreasing the perceived rewards of not getting vaccinated. However, it is important to note that emphasising disease severity may backfire, particularly with hesitant individuals; studies on childhood and influenza vaccine messaging have shown that messaging on disease risks is not necessarily effective for increasing intention to vaccinate (e.g., [28], [29]). Research is needed to establish if this is the case for the COVID-19 vaccine, and any health promotion campaign messaging on the severity of COVID-19 should be pre-tested in target audiences beforehand.
Our findings on PMT and COVID-19 vaccination intention are similar to previous research on influenza virus vaccination intention [10], [12], [13]. They contrast with those of a study revealing the influence of only one PMT construct - perceived severity - on coronavirus vaccination intention in Chinese students [14]. This difference may be due to cultural differences, with the present study being conducted in a Western setting and sampling the general UK population. Future research would benefit from cross-cultural comparisons of PMT in relation to COVID-19 vaccination intention.
Apart from coronavirus conspiracy beliefs being negatively related to vaccination intention, unvaccinated individuals had significantly higher levels of coronavirus conspiracy beliefs than vaccinated individuals. The findings on coronavirus conspiracy beliefs and their relationship to vaccination intention are in line with previous UK research [4], [6]. Unlike these previous studies, however, our study was conducted at a time when the COVID-19 vaccination programme was well underway. Therefore, in contrast to previous research, respondents in the present study did not have to indicate their beliefs in relation to a future scenario, as the COVID-19 vaccine was already available. This may have led to more accurate responses, as respondents did not have to imagine a hypothetical situation – no vaccines had been approved at the time these earlier studies were conducted - and allowed for a comparison of vaccinated to unvaccinated individuals in relation to their coronavirus conspiracy beliefs. The finding that unvaccinated individuals tended to have higher levels of such beliefs is potentially important for interventions and campaigns addressing COVID-19 vaccination uptake, as it indicates that more individuals in the unvaccinated population may hold coronavirus conspiracy beliefs. Furthermore, the role of social media in spreading misinformation about COVID-19 also needs to be considered. In other work, a negative relationship has been found between coronavirus conspiracy beliefs and COVID-19 health-protective behaviours, as well as a positive relationship between such conspiracy beliefs and using social media as a source of information about COVID-19 [30]. Campaigns addressing COVID-19 vaccine uptake should therefore consider using social media to address coronavirus conspiracy beliefs, perhaps using people who are not authority figures and therefore less likely to be perceived as being part of a conspiracy.
Among the assessed demographic factors, only age emerged as a significant predictor of COVID-19 vaccination intention. The younger respondents were, the higher their intention tended to be. This finding needs to be viewed in light of the fact that younger respondents were more likely to be unvaccinated than the older ones as many of them would not yet have been offered the vaccine. At the time data collection ceased, respondents aged 34 and older were eligible to be vaccinated. Respondents under 34 years of age would usually only have been offered the vaccine if they were part of one of the other priority groups, for example, being deemed clinically vulnerable, or being a frontline health or social care worker [31]. Findings of previous studies in relation to the role of age in COVID-19 vaccination intention are mixed [4], [6], [15], [16]. Once the vaccine has been offered across all adult age groups, it would be useful to explore the relationship of age to COVID-19 vaccination intention again, as a clearer picture may then emerge, with availability of the vaccine being, at least in principle, the same for individuals of all ages.
No significant relationship was found between ethnicity and COVID-19 vaccination intention, unlike previous research [4], [5], [17]. Black, Asian, and minority ethnic (BAME) individuals were not well-represented in the current study, making a comparison difficult and therefore a significant relationship between ethnicity and vaccination intention may not have been detected. The same is the case for religiosity, with the present study failing to detect a relationship with vaccination intention. It is advisable that further research be conducted in this area to ensure that larger numbers of such participants are recruited.
4.1. Strengths, limitations and future research
To our knowledge, the present study is the first to assess the influence of PMT, coronavirus conspiracy beliefs and demographic factors on COVID-19 vaccination intention. It offers important insights into potential directions for future research, and highlights issues to consider when devising interventions and campaigns addressing COVID-19 vaccine uptake.
Some limitations to the present study need to be acknowledged. While power was more than sufficient for the comparison of vaccinated to non-vaccinated respondents, the regression analysis was slightly underpowered to detect a medium effect size. That significant predictors still emerged suggests that the detected associations with COVID-19 vaccination intention are likely to be strong. This also means that further research with larger sample sizes would be beneficial.
The sample in the present study contained a bias towards more highly educated respondents. Although this could have conceivably affected the results, prior UK research has found no association between level of education and COVID-19 vaccination intention [4]. Nevertheless, it would be beneficial to establish whether the present findings hold up using a sample with a more even distribution of level of education. Larger numbers of BAME individuals, as well as religious individuals, should also be included in such research. Furthermore, a more even balance between males and females would be beneficial, as previous studies have found differences between genders in attitudes towards the COVID-19 vaccine [4], [15], [16].
While our findings make clear that four of the six PMT constructs as well as coronavirus conspiracy beliefs play a role in COVID-19 vaccination intention, we currently know little about the aetiology of these beliefs, or any other barriers towards vaccination which may be relevant in this context. Qualitative or mixed methods could be employed to examine these beliefs and their origins more closely. This would help devise interventions and campaigns targeting COVID-19 vaccine uptake, ensuring that their effectiveness is maximised.
5. Conclusions
The present study has shown that PMT and coronavirus conspiracy beliefs play an important role in individuals’ intention to receive the COVID-19 vaccine. With the possible exception of age, demographic factors do not appear to have any significant influence on this intention. Interventions and health promotion campaigns addressing vaccine uptake should consider employing techniques directed at increasing individuals’ perceived severity of COVID-19, their perceived susceptibility to this illness, and their perceived ability to get the vaccine, while decreasing the perceived rewards of not getting vaccinated. Furthermore, conspiracy beliefs should be addressed, as for some who are hesitant towards the vaccine, these may play an important role. No single intervention is likely to be effective [32], and it may take a combination of approaches, tailored to the needs of individuals, to achieve a reduction in COVID-19 vaccine hesitancy.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank Paul van Schaik for his useful advice on aspects of the data analysis. This work was supported by a grant from the National Institute for Health Research Clinical Research Network North East and North Cumbria, however all aspects of the work, including the interpretation of the data, the discussion of it and conclusions drawn were all carried out independently of CRN by JE and JL.
References
- 1.Bloomberg. Covid-19 Tracker; 2021.
- 2.NHS England. COVID-19 Vaccinations; 2021.
- 3.Public Health England. COVID-19 vaccine surveillance report: Week 20; 2021.
- 4.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020:1–15. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office for National Statistics. COVID-19 vaccine refusal, UK: February to March 2021; 2021.
- 6.Freeman D., Waite F., Rosebrock L., Petit A., Causier C., East A., et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol Med. 2020:1–13. doi: 10.1017/S0033291720001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahase E. Covid-19: Most people admitted to hospital after vaccination were infected before immunity could develop, research shows. BMJ. 2021:n1127. doi: 10.1136/bmj.n1127. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO technical advisory group on behavioural insights and sciences for health, meeting report, 15 October 2020; 2020.
- 9.Maddux J.E., Rogers R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. J Experim Soc Psychol. 1983;19:469–479. doi: 10.1016/0022-1031(83)90023-9. [DOI] [Google Scholar]
- 10.Crouse Quinn S., Jamison A.M., Freimuth V.S., An J., Hancock G.R. Determinants of influenza vaccination among high-risk Black and White adults. Vaccine. 2017;35:7154–7159. doi: 10.1016/j.vaccine.2017.10.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freimuth V.S., Jamison A., Hancock G., Musa D., Hilyard K., Quinn S.C. The Role of Risk Perception in Flu Vaccine Behavior among African-American and White Adults in the United States: The Role of Risk Perception in Flu Vaccine Behavior. Risk Anal. 2017;37:2150–2163. doi: 10.1111/risa.12790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinstein N.D., Kwitel A., McCaul K.D., Magnan R.E., Gerrard M., Gibbons F.X. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychol. 2007;26:146–151. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- 13.Ling M., Kothe E.J., Mullan B.A. Predicting intention to receive a seasonal influenza vaccination using Protection Motivation Theory. Soc Sci Med. 2019;233:87–92. doi: 10.1016/j.socscimed.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Wang P.-W., Ahorsu D.K., Lin C.-Y., Chen I.-H., Yen C.-F., Kuo Y.-J., et al. Motivation to Have COVID-19 Vaccination Explained Using an Extended Protection Motivation Theory among University Students in China: The Role of Information Sources. Vaccines. 2021;9:380. doi: 10.3390/vaccines9040380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazarus J.V., Wyka K., Rauh L., Rabin K., Ratzan S., Gostin L.O., et al. Hesitant or Not? The Association of Age, Gender, and Education with Potential Acceptance of a COVID-19 Vaccine: A Country-level Analysis. Journal of Health Communication. 2020;25:799–807. doi: 10.1080/10810730.2020.1868630. [DOI] [PubMed] [Google Scholar]
- 16.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet Regional Health - Europe. 2021;1 doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Troiano G., Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Faul F., Erdfelder E., Buchner A., Lang A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 20.NHS England. NHS invites people aged 34 and 35 for life-saving COVID-19 jab; 2021.
- 21.BBC News. Covid-19: Vaccine rollout extended to over-70s in England; 2021.
- 22.Bodell M. NHS organisations ordered to vaccinate staff ‘as quickly as possible’; 2021.
- 23.NHS England. Vaccinating frontline social care workers; 2021.
- 24.Sky News. COVID-19: Vaccine rollout begins for over-65s and clinically vulnerable people; 2021.
- 25.Office for National Statistics. Ethnic group, national identity and religion; 2021.
- 26.IBM Corp . IBM Corp.; NY: 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk. [Google Scholar]
- 27.Bowerman B.L., O’Connell R.T. 2nd ed. PWS-Kent Pub. Co; Boston: 1990. Linear statistical models: an applied approach. [Google Scholar]
- 28.Nyhan B., Reifler J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine. 2015;33:459–464. doi: 10.1016/j.vaccine.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 29.Nyhan B., Reifler J., Richey S., Freed G.L. Effective Messages in Vaccine Promotion: A Randomized Trial. Pediatrics. 2014;133:e835–e842. doi: 10.1542/peds.2013-2365. [DOI] [PubMed] [Google Scholar]
- 30.Allington D., Duffy B., Wessely S., Dhavan N., Rubin J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. 2021;51:1763–1769. doi: 10.1017/S003329172000224X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Health Service. Book or manage your coronavirus (COVID-19) vaccination; 2021.
- 32.Razai M.S., Chaudhry U.A.R., Doerholt K., Bauld L., Majeed A. Covid-19 vaccination hesitancy. BMJ. 2021:n1138. doi: 10.1136/bmj.n1138. [DOI] [PubMed] [Google Scholar]