Abstract
Objective Quality of life (QoL) outcomes following endoscopic endonasal transphenoidal surgery (EETS) across a variety of reconstructive methods improve by 2 to 6 months. An option for sellar reconstruction, in the absence of a significant intraoperative cerebrospinal fluid (CSF) leak, is a free mucosal graft (FMG) from the posterior septum. We analyze sinonasal QoL outcomes in patients undergoing EETS with FMG reconstruction.
Study Design This study was a retrospective review.
Setting This study was conducted at tertiary care academic center.
Participants This study group consisted of patients undergoing EETS for pituitary adenomas from 2013 to 2018.
Main Outcome Measures Tumor and surgical factors were included, along with postoperative complications. Patients completed Sinonasal Outcome Test-22 (SNOT-22) questionnaires. Pre- and postoperative scores were compared among the entire cohort using linear multilevel regression. A subcohort analysis was performed among patients who completed questionnaires during the preoperative visit and two postoperative visits (within 1 month and between 2 and 3 months, respectively); pre- and postoperative total and individual domain SNOT-22 scores were compared using paired t -tests.
Results A total of 243 patients underwent EETS with FMG reconstruction. Four patients (1.6%) developed a postoperative CSF leak requiring reoperation. Among the entire cohort, SNOT-22 scores increased at the first postoperative visit ( p < 0.01) but returned to baseline by the second, third, and fourth postoperative visits ( p = 0.27, p = 0.18, and p = 0.21). Among 48 patients who completed both preoperative and two postoperative questionnaires, scores increased within the first month ( p < 0.01) but returned to baseline at 2 to 3 months ( p = 0.67).
Conclusion Posterior septum FMG reconstruction of sellar defects is an effective option, demonstrating early recovery of baseline sinonasal QoL by 2 to 3 months.
Keywords: endoscopic endonasal transphenoidal surgery, sellar reconstruction, free mucosal graft, quality of life, sinonasal outcome test-22, sinonasal morbidity
Introduction
The endoscopic endonasal transphenoidal approach (EETS) is a minimally invasive, effective surgical treatment for benign and malignant tumors of the sella. Sellar defects created from this approach may be managed without formal reconstruction or with a variety of reconstructive materials including free mucosal grafts (FMG), nasoseptal flaps (NSF), dural substitutes, and fat grafts among others, depending on the size of the defect, presence and grade of an intraoperative cerebrospinal fluid (CSF) leak, and availability of the donor site. The EETS, however, can lead to sinonasal morbidity and reduced quality of life (QoL) following surgery. 1 Strategies to improve postoperative symptoms include nasal decongestants, saline sprays or irrigations, and endoscopic debridements in the outpatient setting. 1
The Sinonasal Outcome Test (SNOT)-22, a patient-reported 22-item questionnaire, has been validated to assess sinonasal QoL and outcomes following surgical intervention among patients with chronic rhinosinusitis. 2 The SNOT-22 may be further divided into five distinct domains, including three sinus-specific symptom domains (rhinologic, extra-rhinologic, and ear/facial symptoms) and two general health-related QoL domains (psychological and sleep dysfunction) to assess the specific factors responding to a given treatment modality. 3 While validated for patients with chronic rhinosinusitis, the SNOT-22 and its predecessor—SNOT-20—are also frequently used to assess QoL outcomes following EETS for sellar pathologies. 4 5 6 7
Prior studies have looked into the postoperative time period until QoL improvement following EETS across a variety of sellar reconstructive methods. Pledger et al showed that among 46 patients undergoing EETS for nonfunctioning pituitary tumors, patients experienced the worst nasal symptoms at 2 weeks postoperatively and improved to below baseline between 8 weeks and 1 year postoperatively. 5 The study, however, did not specify which reconstructive methods were performed. McCoul et al showed that among 81 patients undergoing EETS for functioning and nonfunctioning pituitary adenomas (PA), SNOT-22 scores peaked at 3 weeks postoperatively and improved to below baseline by 12 weeks to 1 year postoperatively. 4 All patients underwent multilayer reconstruction with rigid fixation, fat grafts, dural substitutes, fascia lata grafts, and/or NSF. Among 56 patients undergoing EETS for functioning and nonfunctioning pituitary tumors, of which the majority underwent a uninostril approach (98%), Davies et al demonstrated that General Nasal Patient Inventory scores peaked at 1 to 3 days postoperatively and improved to below baseline by 6 to 12 months. 1 This cohort of patients underwent a variety of reconstructive methods including dural substitutes, fat grafts, and/or NSF, depending on the presence and grade of a CSF leak. As each reconstructive method—or lack of reconstruction—has its own inherent morbidities that may negatively impact QoL, the heterogeneity of reconstructive methods in the above studies makes it difficult to ascertain which reconstructive option(s) may maximize QoL when a choice is available.
When considering reconstructive options, the use of a NSF may contribute to worse postoperative QoL outcomes, owing to donor site morbidity. 8 9 10 In an effort to improve sinonasal morbidity, FMG reconstruction is an alternative, equally effective reconstructive option for patients without significant intraoperative CSF leaks (including those without CSF leak or with a low-grade CSF leak)—in lieu of the NSF—with no significant difference in postoperative CSF leak rate between the two techniques. 11 A recent study by Scagnelli et al looked at QoL outcomes among 122 patients undergoing EETS for PAs with nasal cavity floor FMG reconstruction. 7 All patients also had an inlay synthetic collagen allograft placed. They found no significant differences in preoperative versus 1-month or 3-months postoperative SNOT-22 scores as well as only one (0.82%) postoperative CSF leak, suggesting minimal sinonasal morbidity and strong efficacy as a reconstructive option. In Scagnelli et al study, however, SNOT-22 scores were only available from 62 patients (preoperative), 63 patients (1-month postoperative), and 48 patients (3-month postoperative), suggesting that not all patients completed preoperative as well as 1-month postoperative and 3-month postoperative SNOT-22 questionnaires.
In our institution, we perform FMG reconstruction with or without inlay graft (including abdominal fat graft or dural substitute with or without rigid fixation) for patients with no or low-grade intraoperative CSF leaks. We harvest a FMG from the posterior septum, as opposed to the nasal cavity floor. A transient complication of a nasal cavity floor donor site includes postoperative numbness of the incisor teeth. 7 Since the posterior septum is routinely removed in EETS, the use of a posterior septum FMG would result in no additional donor site morbidity. The present study seeks to evaluate the efficacy of posterior septum FMG reconstruction among a large cohort of patients undergoing EETS for PAs. We propose that the posterior septum as an alternative harvest site for FMG reconstruction has similar efficacy rates in preventing postoperative CSF leaks and results in good QoL outcomes. Additionally, our study performs a subanalysis on only those patients who completed SNOT-22 questionnaires preoperatively, at the first postoperative visit (≤4 weeks after surgery), and at the second postoperative visit (8–12 weeks after surgery) to assess change in QoL over time and allow each case to serve as its own control.
Methods
Patient Population
Study approval was obtained through the institutional review board. A retrospective review was conducted of all patients undergoing EETS for PAs with FMG reconstruction between August 2013 and July 2018. Tumor and surgical factors including diagnosis, intraoperative CSF leak rate, postoperative CSF leak rate, and other postoperative complications were recorded.
Surgical Technique
All patients underwent EETS through a binostril four-hand technique, performed by one senior otolaryngologist (M.B.W.) and one senior neurosurgeon (M.B.). The procedure included lateralization of the inferior and middle turbinates, resection of the inferior one-third of the superior turbinates, and sphenoid sinusotomies bilaterally. A rescue flap was harvested using Bovie cautery on the right septum starting from the keel posteriorly and extending anteriorly along the septum halfway to the columella; the Cottle elevator was used to elevate the rescue flap off the underlying septal cartilage and bone and retract it inferiorly, preserving the vascular pedicle. The rescue flap was raised during the time of initial surgery in case a NSF would have been needed for revision surgery, such as for repair of postoperative CSF leak. The FMG was then harvested from the left posterior septum using Bovie cautery from the inferior sphenoid os to the middle turbinate anteriorly, inferiorly down to the septal floor, and then posteriorly along the septal floor to the choanae. The Cottle elevator was used to lift up the mucosal graft from the septum. Following harvest of the mucosal graft, a posterior septectomy was performed, followed by extensive drilling of the sphenoid sinuses to expose the sella and optico-carotid recesses bilaterally. Following tumor resection, the previously harvested FMG was placed as an overlay graft. In some cases with a low-grade CSF leak, an inlay graft of abdominal fat graft or dural substitute (DuraMatrix, Stryker, Kalamazoo, Michigan, United States) with or without rigid bone fixation was placed prior to the FMG overlay. Postoperatively, patients were instructed to use saline sprays four times daily starting on postoperative day 2. All patients underwent nasal endoscopies to assess healing of the FMG and outpatient debridements at the first postoperative visit and the second postoperative visit. The majority of our patients did not return for follow-up after the second postoperative visit. While we encouraged all patients to return as needed after two postoperative visits, we assume a reason why patients did not return was because they did not require additional debridements and were not experiencing significant sinonasal morbidity.
Questionnaire
Eligible patients were asked to complete a SNOT-22 questionnaire preoperatively and at postoperative visits. Generally, patients were encouraged to return for the first postoperative visit within the first month after surgery and for the second postoperative visit within 2 to 3 months after surgery. The SNOT-22 questionnaire is based on patient-reported answers to 22 questions, each graded on 0 to 5 scaling system. 2 Scores range from 0 to 110, with a higher score indicating greater QoL impairment. Individual domain scores for rhinologic symptoms, extra-rhinologic symptoms, ear/facial symptoms, psychological dysfunction, and sleep dysfunction were also recorded. 3
Statistical Analyses
In the primary analysis including the entire cohort of patients undergoing EETS for PAs with FMG reconstruction, a linear multilevel regression—with time nested in participant—was performed with SNOT-22 score as the outcome variable. Predictor variables included time of visit (preoperative visit, first postoperative visit, second postoperative visit, third postoperative visit, etc.), age (years), sex (male or female), history of diabetes (yes or no), history of chronic rhinosinusitis (yes or no), history of smoking (no history of smoking, prior smoker, or current smoker), and history of head and neck radiation (yes or no). Statistical significance was set at a two-sided p <0.05.
In our subanalysis, patients who did not complete at least a preoperative, first postoperative, and second postoperative visit questionnaire were excluded. Patients who had postoperative appointments outside of the time frame of within 1 month (for the first visit) or 2 to 3 months (for the second visit) were also excluded. These patients were excluded to control for variability in the time after surgery that patients presented for their postoperative visits. For example, patients who presented for their second postoperative visit at 2 versus 5 months may have reported different SNOT-22 scores. Preoperative and postoperative SNOT-22 scores were reported as a mean with standard deviation (SD). Mean preoperative SNOT-22 scores were compared with mean postoperative scores using the paired t -test on Stata16 (StataCorp, College Station, Texas). Statistical significance was set at a two-sided p <0.05. Paired t -tests were also performed comparing preoperative and postoperative scores for each SNOT-22 domain. Mean SNOT-22 scores were also compared between patients with nonfunctioning and functioning PAs using independent t -tests.
Results
In our study, 243 patients underwent EETS for PAs with posterior septum FMG reconstruction. A total of 187 patients (77%) had nonfunctioning PAs, while 56 patients (23%) had functioning PAs. Among those with functioning PAs, there were 22 cases with Cushing's disease, 20 cases with acromegaly, 13 cases with prolactinoma, and one case with a thyrotropin-secreting PA. Sellar reconstruction was performed with FMG overlay alone in 219 patients (90%), FMG overlay with abdominal fat graft inlay in 13 patients (5%), FMG overlay with abdominal fat graft and rigid bone fixation inlay in 10 patients (4%), and FMG overlay with dural substitute (DuraMatrix) and rigid bone fixation inlay in one patient (0.4%). Twenty-seven patients (11%) experienced a low-grade intraoperative CSF leak, while the remaining (89%) had no intraoperative CSF leak noted. Four patients (1.6%) developed a postoperative CSF leak and required reoperation for repair. Among these four patients, only one patient (25%) was noted to have an intraoperative CSF leak at the time of surgery. The postoperative CSF leak rate among patients who had a low-grade intraoperative CSF leak was 3.7%. The four patients with postoperative CSF leaks were reconstructed with an overlay NSF, overlay bilateral middle turbinate flaps, overlay NSF with inlay abdominal fat graft, or overlay NSF, respectively, without further postoperative CSF leak. Two patients (0.8%) experienced postoperative epistaxis requiring control of bleeding in the operating room.
Among our entire cohort of 243 patients, a linear multilevel regression analysis was performed with time nested in participant. Predictor variables were tested for significant association with SNOT-22 score as the outcome variable. The first postoperative visit scores were significantly different ( p < 0.01) from preoperative SNOT-22 scores. However, the second, third, and fourth postoperative visit scores were no longer significantly different ( p = 0.27, p = 0.18, and p = 0.21, respectively), compared with preoperative scores. Current smoker, as opposed to no prior history of smoking or prior smoker, was also significantly associated with higher SNOT-22 score ( p = 0.01) for all visits. However, after controlling for the history of smoking, the significant association between time of visit and SNOT-22 scores remained ( p < 0.01).
In our subanalysis, we excluded patients who did not complete a preoperative as well as two postoperative SNOT-22 questionnaires ( n = 137), leaving 106 patients (44%) available for further analysis. Among these 106 patients, the median time from the date of surgery to the first postoperative visit was 2 weeks (range = 1–5). The median time from the date of surgery to the second postoperative visit was 8 weeks (range = 2–34). Therefore, patients with a median time from the date of surgery to the first postoperative visit greater than 4 weeks ( n = 9; 8%) were excluded. In addition, patients with a median time from the date of surgery to the second postoperative visit less than 8 weeks ( n = 48; 45%) or greater than 12 weeks ( n = 10; 9%) were excluded. Nine patients had both a first postoperative visit greater than 4 weeks and a second postoperative visit either less than 8 weeks or greater than 12 weeks, so could not be excluded twice. After applying the above exclusion criteria, in total, 48 patients (20%) were eligible for our subanalysis. In this subcohort, the median time from the date of surgery to the first postoperative visit was 3 weeks (range = 1 to 4), and the median time from the date of surgery to the second postoperative visit was 9 weeks (range = 8–11). Nasal endoscopy performed at both postoperative visits showed good FMG take, with minimal or no crusting by the second postoperative visit. As seen in Fig. 1 and Table 1 , the mean preoperative SNOT-22 score was 15.7 ± 19.5 (SD); the mean first postoperative visit SNOT-22 score was 29.6 ± 20.7 ( p < 0.01, paired t -test); and the mean second postoperative visit SNOT-22 score was 16.8 ± 17.2 ( p = 0.67, paired t -test), suggesting worsened QoL outcomes within the first month postoperatively and improvement to baseline by 2 to 3 months postoperatively. Looking at individual SNOT-22 domains, there was significantly worsened QoL in all five domains within the first month. By the second to third month, patients recovered in all domains except for rhinologic symptoms ( p = 0.03, paired t -test). In this subcohort of 48 patients used for SNOT-22 questionnaire analyses, no patients experienced a postoperative CSF leak. One patient (2%) experienced postoperative epistaxis requiring reoperation.
Fig. 1.
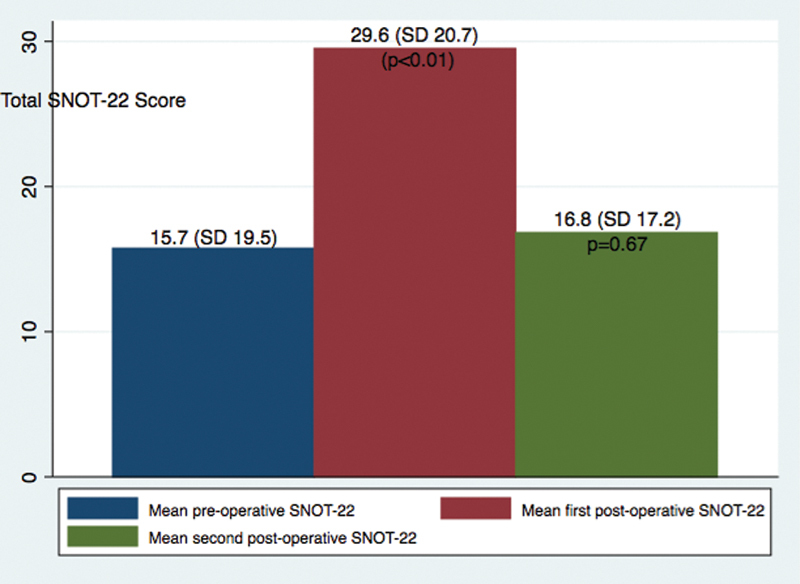
Mean preoperative and postoperative sinonasal outcome test-22 scores for patients who underwent endoscopic endonasal transphenoidal approach for pituitary adenomas with free mucosal graft reconstruction ( n = 48).
Table 1. Mean preoperative and postoperative sinonasal outcome test-22 scores for patients who underwent endoscopic endonasal transphenoidal approach for pituitary adenomas with free mucosal graft reconstruction, stratified by total score and domain scores ( n = 48) .
| Preoperative visit (mean ± SD) |
First postoperative visit, ≤4 weeks after surgery (mean ± SD) |
Second postoperative visit, between 8 and 12 weeks after surgery (mean ± SD) |
|
|---|---|---|---|
| Total SNOT-22 | 15.7 ± 19.5 | 29.6 ± 20.7 ( p < 0.01) | 16.8 ± 17.2 ( p = 0.67) |
| SNOT-22 domains | |||
| Rhinologic symptoms | 2.7 ± 4.7 | 9.4 ± 6.3 ( p < 0.01) | 4.4 ± 4.7 ( p = 0.03) |
| Extra-rhinologic symptoms | 1.0 ± 2.2 | 3.5 ± 3.4 ( p < 0.01) | 1.6 ± 2.3 ( p = 0.10) |
| Ear/Facial symptoms | 1.6 ± 2.7 | 4.7 ± 5.2 ( p < 0.01) | 3.4 ± 8.6 ( p = 0.10) |
| Psychological dysfunction | 6.5 ± 8.5 | 8.7 ± 7.4 ( p = 0.05) | 6.3 ± 7.6 ( p = 0.84) |
| Sleep dysfunction | 5.8 ± 6.6 | 8.9 ± 7.8 ( p = 0.01) | 5.7 ± 6.4 ( p = 0.96) |
Abbreviations: SD, standard deviation; SNOT-22, Sinonasal Outcome Test-22.
Comparing patients with nonfunctioning versus functioning PAs, there were no significant differences in preoperative SNOT-22 scores between the two cohorts ( p = 0.61, independent group t -test), first postoperative SNOT-22 scores ( p = 0.41, independent group t -test), or second-postoperative SNOT-22 scores ( p = 0.27, independent group t -test).
Discussion
Among our robust cohort of patients undergoing EETS for PAs, posterior septum FMG reconstruction was effective in preventing CSF leaks, while providing good sinonasal QoL by 2–3 months following surgery. Our study demonstrated intraoperative and postoperative CSF leak rates of 11 and 1.6%, respectively, with FMG alone among 243 patients. Of the patients with identified intraoperative CSF leaks ( n = 27; 11%), only one patient experienced a postoperative CSF leak (3.7%). Prior studies have shown that the rates of postoperative CSF leaks with the NSF are approximately 3%, indicating that the FMG alone is an effective alternative to NSF for the reconstruction of select sellar defects. 12 13 14 Among our four patients with postoperative CSF leaks requiring repair, since the majority of them ( n = 3; 75%) had no identifiable intraoperative CSF leak at the time of primary surgery, we assume that our true intraoperative CSF leak rate in this series may have been higher than 11%.
Looking at our entire cohort of 243 patients, linear multilevel regression analyses showed SNOT-22 score was significantly worse at the first postoperative visit ( p < 0.01), but normalized to baseline by the second, third, and fourth postoperative visits, suggesting improved and sustained postoperative QoL outcomes. Looking at only those patients who completed preoperative and two postoperative questionnaires (performed ≤ 4 weeks and between 8 and 12 weeks, respectively), SNOT-22 scores increased within 1 month postoperatively ( p < 0.01), but returned to baseline at 2 to 3 months postoperatively ( p = 0.67). Improvements in QoL were likely reflective of good graft healing, resolution of crusting in the sinonasal cavities, and institutionally standardized postoperative care regimens including saline irrigations and outpatient debridements.
Prior studies among patients undergoing EETS to pituitary tumors across a variety of reconstructive methods showed QoL improved to near or below baseline by 2 to 6 months postoperatively, similar to the findings in our study. 1 4 5 However, direct comparisons are difficult to make given the variety of reconstructive methods used in these studies. Similar to our study, Scagnelli et al showed that nasal cavity floor FMG reconstruction of sellar defects showed a low postoperative CSF leak rate and no difference in sinonasal morbidity by 3 months postoperatively. 7 A strength of our study compared with their study is that since each patient completed all three questionnaires, each patient acted as his or her own internal control, thereby controlling for subjective (personal preference) or objective factors (age, medical comorbidities, smoking history, or history of chronic rhinosinusitis) that may have influenced SNOT-22 scoring. As a posterior septectomy is routinely performed in our technique of EETS, we propose that the posterior septum harvest site results in no additional donor site morbidity, good graft survival with low rates of delayed CSF leaks, and comparable QoL outcomes.
In our subanalysis looking at individual SNOT-22 domains, all domains recovered to baseline by 2 to 3 months, except for rhinologic symptoms ( p = 0.03). The median date from date of surgery to the second postoperative visit was 9 weeks (range = 8–11), which may have been too soon to see complete resolution of rhinologic symptoms. Looking at patients who reported worse or similar rhinologic symptoms at the second postoperative visit compared with the first postoperative visit ( n = 7; 15%), only two patients returned for a third visit and only one patient returned for a fourth visit. Among these two patients, their rhinologic symptom scores eventually downtrended with each visit. All seven patients were noted to have some degree of crusting on postoperative nasal endoscopies, which may have been related to adherence to use of postoperative saline irrigations or higher susceptibility to poor wound healing. Since the majority of our patients did not return for follow-up after the second postoperative visit, we did not have enough SNOT-22 scores to assess long-term sinonasal symptoms. The literature, however, indicates that improvements in sinonasal QoL are seen up to 1 year postoperatively, suggesting longer follow-up may have seen additional improvements in the rhinologic symptoms domain. In a study among 51 patients who underwent an endonasal approach for a variety of skull base lesions, Pant et al showed that these patients experienced a statistically significant improvement in SNOT-22 scores from 1 to 3 months postoperatively to 6 to 12 months postoperatively. 9 In more than 75% of patients, the best postoperative SNOT-22 score was achieved by 6 to 12 months postoperatively. In other studies for patients undergoing EETS for pituitary tumors, improvements in QoL were achieved up to 1 year postoperatively. 1 4 5 In addition, it is possible that rhinologic symptom scores may be worse in the earlier postoperative period and trail total and other domain scores, with improvements seen more gradually in the postoperative period. A study by Pledger et al showed that while total SNOT-22 scores improved to below baseline by 4 weeks postoperatively, rhinologic symptom scores took a longer period of 8 weeks postoperatively to see improvement to below baseline, and rhinologic symptom scores continued to downtrend by 1 year postoperatively. 5 Another study by Chaudhry et al demonstrated that Rhinologic symptom scores worsened within 2 weeks after surgery compared with other domain scores, but trended toward improvement after 2 weeks. 15
A limitation of our study includes the questionnaire response rate for our subanalysis (20%). To provide a more robust statistical analyses, assessing for change over time and controlling for individual subjective and objective confounding factors, we decided to include only those patients who completed all three questionnaires instead of averaging the overall preoperative and postoperative SNOT-22 scores of the entire cohort of 243 patients. Our linear multilevel regression, however, which included all 243 patients, corroborates the data found in our subanalysis. In this model, we found that patients had significantly worse QoL scores at the first postoperative visit but experienced improvements to baseline by the second postoperative visit, which were sustained with time with further postoperative visits.
Another limitation includes the way we measured sinonasal QoL. QoL has been measured by various tools including the SNOT-22 questionnaire, Anterior Skull Base Questionnaire, and Rhinosinusitis Outcome Measure-31, among others 4 10 ; we utilized the SNOT-22 as it was a routinely used assessment tool in QoL outcomes following EETS for sellar pathologies in the literature. 4 5 6 7 Finally, measurements of QoL take into account the intrinsic nature of the disease, modality of treatment, surgical technique, postoperative care, and environmental or socioeconomic factors influencing postoperative recovery, all of which contribute to difficulty in capturing the overall QoL. To control for some of these factors, we limited our study to only patients with PA; we also performed additional analyses comparing SNOT-22 scores between patients with nonfunctioning and functioning PAs, as this may have been a confounding factor seen in other studies 1 16 and found no significant differences in preoperative or postoperative SNOT-22 scores. Only one team of surgeons performed all surgeries following a standardized EETS technique, and our postoperative care regimen was standardized in our institution. Additionally, by allowing for each person to act as his or her own historical control in our subanalysis, we hoped to control for environmental or socioeconomic factors in the recovery stage that may have influenced QoL outcomes.
Conclusion
Among patients undergoing EETS for PAs without significant intraoperative CSF leaks, posterior septum FMG reconstruction is an effective reconstructive tool in preventing postoperative CSF leaks, while providing early recovery to baseline sinonasal QoL by 2 to 3 months following surgery. Improvements in postoperative QoL are likely reflective of good graft healing, no additional donor site morbidity, and early resolution of crusting in the sinonasal cavities.
Footnotes
Conflict of Interest None declared.
References
- 1.Davies B M, Tirr E, Wang Y Y, Gnanalingham K K. Transient exacerbation of nasal symptoms following endoscopic transsphenoidal surgery for pituitary tumors: a prospective study. J Neurol Surg B Skull Base. 2017;78(03):266–272. doi: 10.1055/s-0036-1597814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hopkins C, Gillett S, Slack R, Lund V J, Browne J P. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol. 2009;34(05):447–454. doi: 10.1111/j.1749-4486.2009.01995.x. [DOI] [PubMed] [Google Scholar]
- 3.DeConde A S, Mace J C, Bodner T. SNOT-22 quality of life domains differentially predict treatment modality selection in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2014;4(12):972–979. doi: 10.1002/alr.21408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCoul E D, Bedrosian J C, Akselrod O, Anand V K, Schwartz T H. Preservation of multidimensional quality of life after endoscopic pituitary adenoma resection. J Neurosurg. 2015;123(03):813–820. doi: 10.3171/2014.11.JNS14559. [DOI] [PubMed] [Google Scholar]
- 5.Pledger C L, Elzoghby M A, Oldfield E H, Payne S C, Jane J A., Jr Prospective comparison of sinonasal outcomes after microscopic sublabial or endoscopic endonasal transsphenoidal surgery for nonfunctioning pituitary adenomas. J Neurosurg. 2016;125(02):323–333. doi: 10.3171/2015.6.JNS142695. [DOI] [PubMed] [Google Scholar]
- 6.Peris-Celda M, Chaskes M, Lee D D, Kenning T J, Pinheiro-Neto C D. Optimizing sellar reconstruction after pituitary surgery with free mucosal graft: results from the first 50 consecutive patients. World Neurosurg. 2017;101:180–185. doi: 10.1016/j.wneu.2017.01.102. [DOI] [PubMed] [Google Scholar]
- 7.Scagnelli R J, Patel V, Peris-Celda M, Kenning T J, Pinheiro-Neto C D. Implementation of free mucosal graft technique for sellar reconstruction after pituitary surgery: outcomes of 158 consecutive patients. World Neurosurg. 2019;122:e506–e511. doi: 10.1016/j.wneu.2018.10.090. [DOI] [PubMed] [Google Scholar]
- 8.Soudry E, Psaltis A J, Lee K H, Vaezafshar R, Nayak J V, Hwang P H. Complications associated with the pedicled nasoseptal flap for skull base reconstruction. Laryngoscope. 2015;125(01):80–85. doi: 10.1002/lary.24863. [DOI] [PubMed] [Google Scholar]
- 9.Pant H, Bhatki A M, Snyderman C H. Quality of life following endonasal skull base surgery. Skull Base. 2010;20(01):35–40. doi: 10.1055/s-0029-1242983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Georgalas C, Badloe R, van Furth W, Reinartz S, Fokkens W J. Quality of life in extended endonasal approaches for skull base tumours. Rhinology. 2012;50(03):255–261. doi: 10.4193/Rhino12.050. [DOI] [PubMed] [Google Scholar]
- 11.Kuan E C, Yoo F, Patel P B, Su B M, Bergsneider M, Wang M B. An algorithm for sellar reconstruction following the endoscopic endonasal approach: a review of 300 consecutive cases. J Neurol Surg B Skull Base. 2018;79(02):177–183. doi: 10.1055/s-0037-1606293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horridge M, Jesurasa A, Olubajo F, Mirza S, Sinha S. The use of the nasoseptal flap to reduce the rate of postoperative cerebrospinal fluid leaks following endoscopic trans-sphenoidal surgery for pituitary disease. Br J Neurosurg. 2013;27(06):739–741. doi: 10.3109/02688697.2013.795525. [DOI] [PubMed] [Google Scholar]
- 13.Thorp B D, Sreenath S B, Ebert C S, Zanation A M. Endoscopic skull base reconstruction: a review and clinical case series of 152 vascularized flaps used for surgical skull base defects in the setting of intraoperative cerebrospinal fluid leak. Neurosurg Focus. 2014;37(04):E4. doi: 10.3171/2014.7.FOCUS14350. [DOI] [PubMed] [Google Scholar]
- 14.Hadad G, Bassagasteguy L, Carrau R L. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116(10):1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhry S, Chaudhry S, Qureshi T, Batra P S. Evolution of sinonasal symptoms and mucosal healing after minimally invasive pituitary surgery. Am J Rhinol Allergy. 2017;31(02):117–121. doi: 10.2500/ajra.2017.31.4407. [DOI] [PubMed] [Google Scholar]
- 16.van Aken M O, Pereira A M, Biermasz N R. Quality of life in patients after long-term biochemical cure of Cushing's disease. J Clin Endocrinol Metab. 2005;90(06):3279–3286. doi: 10.1210/jc.2004-1375. [DOI] [PubMed] [Google Scholar]


