Abstract
Pneumomediastinum is a relatively rare and usually a self-limiting condition in infants. However, it can lead to tension pneumomediastinum or pneumothorax, which may rapidly become life-threatening. Therefore, its timely and accurate detection is important and close follow-up to resolution is needed. Ultrasound can be used as a real-time problem solver to accurately diagnose pneumomediastinum in an infant and should be encouraged as a radiation-free adjunct imaging modality when radiography cannot provide a definite diagnosis. We present a case of a 13-month-old preterm girl with bronchopulmonary dysplasia and acute respiratory infection who presented with sudden respiratory failure due to spontaneous pneumomediastinum. Pneumomediastinum was eventually diagnosed with ultrasound, after chest radiography performed during the on-call hours was misinterpreted because not all typical radiographic signs of pneumomediastinum were present.
Keywords: Infant, pneumomediastinum, respiratory failure, thoracic radiography, ultrasonography
Introduction
Pneumomediastinum or mediastinal emphysema is defined as the presence of extraluminal air in the mediastinum.1 The underlying pathophysiological mechanism of pneumomediastinum is alveolar rupture with subsequent leakage of air into the pulmonary interstitium, and eventually through the hilum into the mediastinum. The term spontaneous pneumomediastinum is used for cases that do not occur after chest trauma, thoracic procedures or mechanical ventilation.2,3 It is a relatively rare condition in infants, mostly associated with an underlying lung disease.4 Its incidence ranges from one in 800 to one in 42,000 patients presenting at hospital emergency units.1
We present a case of an infant with acute respiratory failure in whom spontaneous pneumomediastinum was initially missed by chest radiography (CXR) and later diagnosed correctly by ultrasound (US). The literature reports of using US to diagnose pneumomediastinum in infants are currently sparse, and this case presentation may help clinicians to incorporate this readily available, portable, dependable and non-invasive imaging modality into more routine clinical use for this indication.
Case report
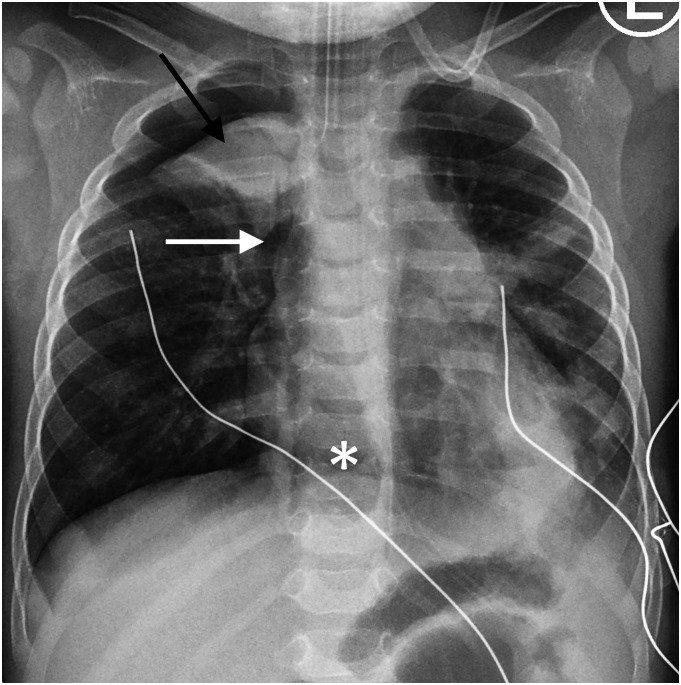
A 13-month-old preterm girl (corrected age of 10 months) with bronchopulmonary dysplasia was admitted to our paediatric hospital because of an acute respiratory infection. During the night, her respiratory condition suddenly deteriorated. The patient required intubation and mechanical ventilation. Based on the CXR obtained, intensive care neonatologist and radiology resident on-call both interpreted it as viral bronchiolitis with confluent atelectasis of the right upper lobe (Fig. 1).
Fig. 1.
Anteroposterior supine chest radiograph in a 13-month-old preterm girl with a history of bronchopulmonary dysplasia, treated at a paediatric hospital because of acute viral respiratory infection, who presented with sudden respiratory failure. Black arrow points to the dense opacity in the right upper lung zone which was misdiagnosed as confluent atelectasis accompanying viral bronchiolitis. The lucent linear band along the right side of the heart (white arrow) and the lucent area in the lower mediastinum (asterisk) are possible CXR findings of pneumomediastinum; however, they were not correctly diagnosed on CXR. Interposition of air between the diaphragm and the heart, linear bands of air parallel to the left side of the heart or extension of air along the great vessels into the neck, which are among the more typical signs of pneumomediastinum, were not present on this CXR. Of note, mild left lower lobe atelectasis is also seen. CXR: chest radiography.
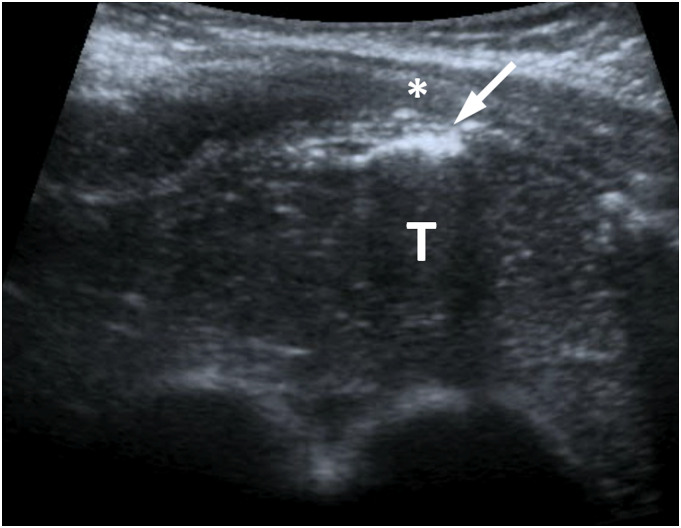
The next morning, the CXR was re-evaluated by a paediatric radiologist who suspected pneumomediastinum and US was proposed for further evaluation. US showed that the presumed confluent atelectasis in the right upper lung zone was, in fact, the thymus. Additionally, small air bubbles located anterior to the thymus were detected within the mediastinum confirming the diagnosis of pneumomediastinum (Fig. 2, Supplementary Video 1). US showed no evidence for lung atelectasis or pneumothorax (Supplementary Video 2). Consequently, the child’s respiratory support was changed to high frequency oscillatory ventilation. Pneumomediastinum fortunately spontaneously resolved over the next 3 days. The patient’s subsequent clinical course was favourable and the patient was discharged from the hospital 2 weeks after admission. Bocavirus was isolated as the cause of the patient’s underlying viral bronchiolitis.
Fig. 2.
Transverse ultrasound image of the upper mediastinum shows the linear hyperechoic line (arrow) with posterior reverberation which is consistent with air (i.e. pneumomediastinum) located between the anterior chest wall (asterisk) and the thymus (T).
Discussion
Spontaneous pneumomediastinum is a relatively rare condition in infants and it is mostly associated with an underlying lung disease.4 The diagnosis of pneumomediastinum is usually made based on CXR. The typical radiographic appearance is the classic ‘spinnaker sail’ sign, also known as the ‘angel wing’ sign, caused by the elevation of one or both thymic lobes superiorly and laterally by air located within the mediastinum. Other CXR features of pneumomediastinum are interposition of air between the diaphragm and the heart, linear bands of air parallel to the left side of the heart and sometimes extension of air along the great vessels into the neck, although the latter CXR finding is rarely present in infants due to the persistence of sternopericardial ligament.1–5 Assessment of pneumomediastinum by CXR can sometimes be challenging because the typical CXR findings are not always present,5 as in our case (Fig. 1). Furthermore, the diagnosis can be especially difficult during the on-call hours when general radiologists and radiology residents, who are less experienced in paediatric radiology specifics, are sometimes the only staff available for evaluation.
The CXR appearance of pneumomediastinum can sometimes resemble the appearance of a medial pneumothorax, pneumonia or viral bronchiolitis with confluent atelectasis, as seen in our case. Nowadays, US is readily available in many neonatal intensive care units and the working staff is often well versed in the use of US for various indications. Although the reports in the literature are currently sparse, it is known that US can allow recognition of abnormal air in the mediastinum. This applies particularly in neonates and infants, due to the unique anatomy of the paediatric chest at that age.3,5,6 The neonates and infants have a relatively large thymus and, not yet ossified, cartilaginous bony structures which lead to available acoustic window for the US visualization of mediastinal structures. Consequently, pneumomediastinum can be detected with US as small amounts of air located between the thymus and the anterior chest wall in the midline of the upper thorax, as seen in our patient (Fig. 2, Supplementary Video 1). Besides being a dependable imaging modality for diagnosing pneumomediastinum, other benefits of US include its portability, relatively low-cost and lack of harmful ionizing radiation associated with other imaging modalities, including CXR.3 Traditionally, chest computerized tomography (CT) has been considered the most precise radiological imaging modality to utilize in equivocal cases of pneumomediastinum on CXR because CT can accurately confirm the diagnosis even with the presence of a minimal amount of air.4 However, potentially harmful radiation, the need for sedation, availability and the relatively high cost are known disadvantages of CT in infants.
Timely and accurate detection of pneumomediastinum is important and close follow-up to resolution is needed. Although it is usually a self-limiting condition, it can potentially progress to tension pneumomediastinum, a life-threatening condition. The underlying pathophysiology of tension pneumomediastinum is due to the trapping of air in the mediastinum with a resulting increase in pressure causing compression of the great vessels which lead to decreased venous return and eventual cardiovascular compromise.7 Another possible life-threatening complication is tension pneumothorax, which can be caused by the rupture of the mediastinal pleura due to stretching.1 To lessen the risk of complications from pneumomediastinum, mechanical ventilation technique can be adjusted once the diagnosis is made in an infant. Novel ways of ventilation, such as high frequency oscillatory ventilation and asynchronous independent lung ventilation, may improve ventilation in some affected patients.8
In conclusion, spontaneous pneumomediastinum in an infant is a relatively rare and usually benign self-limiting condition, mostly associated with an underlying lung disease. However, missed pneumomediastinum can rapidly become tension pneumomediastinum or pneumothorax, a life-threatening condition. Pneumomediastinum is usually diagnosed by the classic chest radiographic ‘spinnaker sail’ sign. Ultrasound can be used as a real-time problem solver to accurately diagnose pneumomediastinum in an infant and should be encouraged as a radiation-free adjunct imaging modality when CXR cannot provide a definite diagnosis.
Supplementary Material
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplementary material: Supplementary material for this article is available online.
ORCID iDs
Polona Klavzar https://orcid.org/0000-0001-6974-2115
Domen Plut https://orcid.org/0000-0001-6850-1715
References
- 1.Chalumeau M, Le Clainche L, Sayeg N, et al. Spontaneous pneumomediastinum in children. Pediatr Pulmonol 2001;31:67–75. [DOI] [PubMed] [Google Scholar]
- 2.Hauri-Hohl A, Baenziger O, Frey B. Pneumomediastinum in the neonatal and paediatric intensive care unit. Eur J Pediatr 2008;167:415–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung AY, Yang I, Go HS, et al. Imaging neonatal spontaneous pneumomediastinum using ultrasound. J Med Ultrason 2014;41:45–49. [Google Scholar]
- 4.Jariwala PS, Kalaniti K, Wonko N, et al. The value of different radiological modalities in assessment of spontaneous pneumomediastinum: case review and diagnostic perspective. AJP Rep 2019;9:e72–e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Megremis S, Stefanaki S, Tsekoura T, et al. Spontaneous pneumomediastinum in a child: sonographic detection in a case with minimal findings on chest radiography. J Ultrasound Med 2008;27:303–306. [DOI] [PubMed] [Google Scholar]
- 6.Testa A, Candelli M, Pignataro G, et al. Sonographic detection of spontaneous pneumomediastinum. J Ultrasound Med 2008;27:1507–1509. [DOI] [PubMed] [Google Scholar]
- 7.Clancy DJ, Lane AS, Flynn PW, et al. Tension pneumomediastinum: a literal form of chest tightness. J Intensive Care Soc 2017;18:52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mousa S, Edriss H. Pneumomediastinum secondary to invasive and non-invasive mechanical ventilation. Southwest Respir Crit Care Chron 2019;7:36–42. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.