Abstract
Inflammation acts like a double-edged sword and can be harmful if not appropriately controlled. COVID-19 is created through a novel species of coronavirus SARS-CoV-2 (2019-nCoV). Elevated levels of inflammatory factors such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), etc. lead to Acute Respiratory Distress Syndrome (ARDS) and severe complications of infection in the lungs of coronavirus-infected patients. Astaxanthin is a natural and potent carotenoid with powerful antioxidant activity as well as an anti-inflammatory agent that supports good health. The effects of astaxanthin on the regulation of cyclooxygenase-2 (COX-2) pathways and the reduction and suppression of cytokines and other inflammatory agents such as IL-6 and TNF-α have already been identified. Therefore, these unique features can make this natural compound an excellent option to minimize inflammation and its consequences.
Keywords: COVID-19, Interleukin-6, Tumor necrosis factor-alpha, Respiratory distress syndrome, Astaxanthin, Anti-inflammatory agent
INTRODUCTION
The new pandemic SARS-CoV-2 virus (Severe Acute Respiratory Syndrome Coronavirus 2), began in late 2019 in Wuhan, China, as a COVID-19 has spread around the globe (1). Infection with the new coronavirus SARS-CoV-2 is initially associated with nonspecific and general symptoms such as nausea, fatigue, and body aches, fever, and dry cough. Patients may suffer symptoms of nausea and diarrhea shortly before the fever. A small number of patients may also have headaches or vomiting of blood and may even be relatively asymptomatic. In severe cases, the sufferer shows severe symptoms, which include pneumonia and shortness of breath. In cases where the patient’s condition is deteriorating, respiratory distress, infectious shock, and failure are present in other body organs (2). A lot of pro-inflammatory cytokines and chemokines such as IL-6, IL1B, IFNγ, IP10, and MCP1 IL2, IL7, IL10, GCSF, MIP1A, and TNF-α have been observed in patients infected with SARS-CoV-2 (3, 4). The main factor in the development of cytokine release syndrome (CRS) is IL-6. The uncontrolled increase in IL-6 causes an over-immune response and a cytokine storm in the body (5). Chemical signals (cytokines) cause inflammation, and if the immune system is unable to balance, over-inflammation and, consequently, the immune system overreaction can exacerbate the disease. Laboratory studies confirm that the angiotensin-converting enzyme 2 (ACE2) expressed at the cellular level acts as a gateway for 2-CoV-SARS to enter the cell (6). But in addition to the respiratory system, other organs in which the ACE2 is expressed, such as endothelial vascular cells of the heart, brain stem, kidneys, liver, intestines, and testicles, etc., are also prone to infection and damage caused by coronavirus (7).
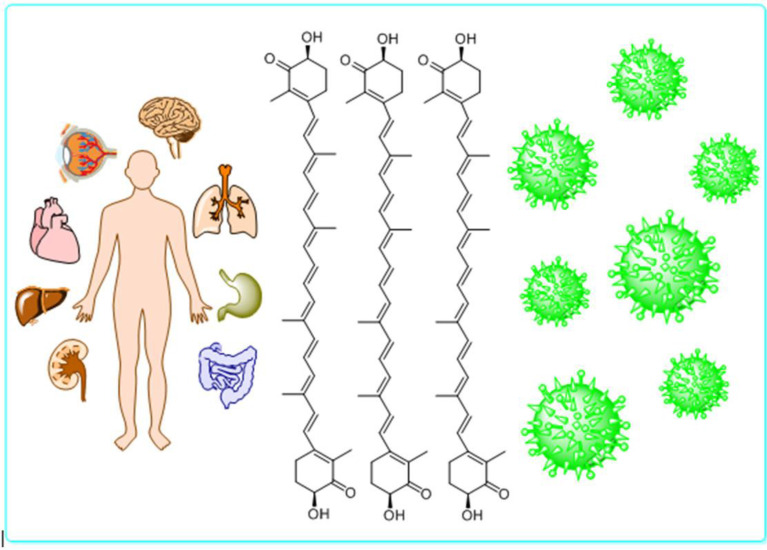
Astaxanthin is an antioxidant and anti-inflammatory compound extraordinary. This bright orange compound has a significant impact on human health, including strengthening the immune system and preventing cardiovascular disease, various cancers, diabetes, liver disease, stomach, obesity problems, and the aging process of cells (8). Astaxanthin balances and boosts the immune system and ameliorates the body’s ability to fight inflammation (9). In some studies, anti-inflammatory therapies have been used to control acute respiratory syndrome (10). Astaxanthin prevents cytokine storms by inhibiting nuclear factor-kB (NF-κB) signaling cascade as well as inflammatory cytokines. It thus has the potential to prevent acute respiratory syndrome due to coronavirus infection (11–13). To reduce and also counteract the severe effects of the virus and the resulting disease, it is necessary to use methods and treatments that reduce anti-inflammatory agents and cytokines. The immune system needs to be strengthened to prevent chronic inflammation and severe complications from respiratory SARS-CoV-2. Using natural astaxanthin, an extremely potent and highly effective antioxidant, can be a great option with high potential to protect the immune system and other organs. The purpose of this paper is to review the properties of astaxanthin as a powerful natural anti-inflammatory that has the ability to protect, strengthen and balance the immune system. Therefore, it may have a beneficial and positive effect on reducing the complications of the SARS-CoV-2 disease and acts as a barrier against coronavirus (Fig. 1).
Fig. 1.
Astaxanthin as a barrier against Coronavirus
Coronavirus pathogenesis and human immune system.
Human coronaviruses, as important pathogens, have always caused infections of varying severity in the respiratory tract and intestines and have been associated with a variety of complications. High-pathogenic coronaviruses SARS-CoV (SARS), MERS-CoV (MERS) and more recently SARS-CoV-2 can cause severe respiratory illness by infecting the lower respiratory tract (14). The new coronavirus uses spike glycoprotein (S) to bind to ACE2 cell surface receptors and enter the cell, as well as SARS-CoV, while MERS-CoV utilizes dipeptidyl peptidase 4 (DPP4) for the binding process (2, 6, 15). The crucial role of this binding in tissue proliferation as well as in the multidrug infection of the SARS-CoV-2 is related to the pervasive expression of ACE2 in cells, such as alveolar type II (ATII) cells, the upper esophagus, epithelial cells, the vascular endothelial cells of the heart, kidney, liver, testis and absorptive enterocytes of the ileum and colon (16). Examination of C-reactive protein (CRP) levels is a reliable indicator for measuring the rate of hazardous silent inflammation in many diseases, such as atherosclerosis, Alzheimer, colon cancer, diabetes, and heart disease (17). An increase in neutrophils and a decrease in lymphocytes have been associated with disease severity and mortality. It has been demonstrated that during the disease, neutrophils, serum IL-6, and other cytokines, and CRP increased, and against lymphocytes showed a decrease (18). The leading reason for death in patients with COVID-19 is ARDS caused by cytokine storms (19). Elevated IL-6 in patients infected with the coronavirus has been reported to be a major cause of inflammation and pneumonia (20). The assumed SARS-CoV-2 receptor, ACE2, is mainly expressed in a small subset of cells in the lungs called ATII (21). To start the antiviral immune response, it is necessary first to identify the intrinsic immune cells of the virus, which often happens with Pathogen-associated molecular patterns (PAMPs). The involvement of innate immune receptors in the process of virus detection leads to the secretion of various types of cytokines, interferon type I, and other inflammatory mediators. Detection of the virus leads to cascading signaling events downstream of the cell. For example, identification is associated with a change in the state of NF-κB and IRF3 in the host cell nucleus. In the cell nucleus, the activity of transcription factors and changes in the macrophage polarization to the M1 phenotype of pro-inflammatory cause the expression of IFN-I and other pro-inflammatory cytokines such as TNF-α, IL-6, MCP-1. As a result of the increase in these factors, the host’s first line of defense against the virus at the site of virus entry, the penetration of mast cells, neutrophils, and macrophages into lung immune cells increased, which in turn increased the risk of inflammation, infection, and defects in lung function (5, 22). Preliminary studies have shown that people with underlying conditions and chronic diseases such as cardiovascular or cerebrovascular, liver, malignant tumors as well as such as diabetes and chronic kidney disease (CKD) are at higher risk for complications and death from SARS-CoV-2 infection (1, 23, 24). This infectious disease has various clinical complications, in addition to ARDS which is its most important complication, it also causes damage to myocardial cells, liver, and kidneys, immune system, thrombotic disease, circulatory failure as well as multiple organ dysfunction syndromes (MODS) and pneumothorax (16, 24–26). The kidneys are one of the target organs of the SARS-CoV-2. Some studies have shown that patients with COVID-19 have acute kidney damage with no history of kidney failure (27). In addition to the increased risk of COVID-19 disease in heart patients, coronavirus can also cause heart problems with myocardial injury, vascular inflammation, cardiac arrhythmias, and chronic damage to the cardiovascular system in healthy people (28). The harmful effects of coronavirus on the nervous system have been approved. In some cases, coronavirus has been found in the brain and cerebrospinal fluid. According to some reports causes nerve damage by invading the central nervous system (CNS) (29). A study has shown that if cancer patients become infected with the coronavirus, the severity of the disease and its complications will be higher (30). Secondary side effects of COVID-19 include type 2 diabetes and high blood pressure. Inflammation from metabolic problems raises the level of fat, blood pressure, and glucose in patients. In addition to cardiovascular problems, diabetes, and high blood pressure can endanger the immune system and disrupts the healing process (31).
Astaxanthin.
Astaxanthin is a potent carotenoid with powerful antioxidant and anti-inflammatory activity that produced by Phaffia rhodozyma, Agrobacterium aurantiacum, and Haematococcus pluvialis (32). The most important major sources of natural astaxanthin are H. pluvialis and Phaffia yeast, which many scientists have extracted astaxanthin from these compounds and increased the amount of astaxanthin in these sources in diverse ways (33–37). Years of laboratory and clinical researches that lead to commercial production have proven that natural astaxanthin has no side effects or toxicity (38). Astaxanthin safety has been confirmed by extensive experiments, including acute toxicity, mutagenesis, transgenicity, fetal toxicity, and reproductive toxicity (33, 39). In addition to balancing the immune system, astaxanthin can inhibit unnecessary inflammation by suppressing overactive immune responses (40). Astaxanthin increases the body’s immune response by increasing the number and activity of lymphocytes and natural killer cells (41). Natural astaxanthin has clinically shown excellent and unique benefits in immunity, inflammatory diseases, and neurological problems. Evidence has shown that astaxanthin, with its protective properties, has beneficial effects in the treatment and prevents various diseases such as cancer, cardiovascular disease, chronic inflammatory diseases, diabetes, and liver disease. Astaxanthin protects the heart, lungs, eyes, skin, immune system, liver, nervous system, and other organs and cells of the body against inflammation, oxidative stress, and other irritants (42–44).
Astaxanthin protective effect on the body.
Given the tremendous impact of astaxanthin on the prevention and even cure of diseases caused by oxidative stress, inflammation, and other chronic diseases of the nervous system, many researchers have focused on investigating the effect of this natural product on neurological disorders and diseases (45). In addition to its antioxidant, anti-inflammatory, and anti-apoptotic activity, the special chemical structure of astaxanthin allows it to cross the blood-brain barrier (BBB), thereby exerting its protective effect on the brain (46). Astaxanthin has an antihypertensive efficacy and brings down the danger of stroke. It has likewise experienced a positive impact on improving the cardiovascular system (47). The use of astaxanthin in the diet has significantly reduced the risk of autoimmune diseases caused by abnormal T cells (48). The outcomes of the survey indicate a positive impact of astaxanthin in restoring humoral immune responses, which has reduced due to aging (49). Due to its high antioxidant power, astaxanthin supplementation reduces arterial stiffness, oxidative stress, and inflammation in kidney transplant patients that thereby reducing cardiovascular complications in these patients (50). Numerous studies have examined the ability of astaxanthin to prevent atherosclerosis. Natural astaxanthin can be utilized as a prophylactic compound against atherosclerotic cardiovascular disease (CVD) (51).
Astaxanthin protective effect on the immune system and reduction inflammation.
One of the important roles of astaxanthin is to reduce inflammation. Astaxanthin exerts its anti-inflammatory effects through various mechanisms and pathways. This natural compound reduces the amount of these inflammatory markers by affecting various inflammatory factors such as IL-6, IL-1B, TNF-α, the NF-κB, COX 1 & 2 enzymes, NO, IFN-γ, IL-8, and prostaglandin E-2 (PGE-2) (17, 52, 53). Natural astaxanthin, with acting on inflammatory markers, can eliminate or reduce inflammation without side effects. Compared to some anti-inflammatory and analgesic drugs, astaxanthin has had a much more positive effect. In various surveys, many consumers with various inflammatory problems such as back pain, joint pain, muscle and tendon pain, carpal tunnel syndrome, rheumatoid arthritis, asthma, and prostate cancer reported complete improvement or improvement in symptoms after using this supplement (17, 54). Various studies have confirmed the significant effect of astaxanthin on inhibitory and anti-inflammatory activity against a wide range of internal and external inflammatory factors such as mast cells, UV rays, and cytokines (55). In vitro and ex-vivo studies have shown that astaxanthin could suppress not only inflammatory markers of NO, PGE-2, and TNF-α but also other inflammatory agents such as IL-1B, COX-2, and NF-κB as well. Astaxanthin via inactivating the NF-κB prevents the release of inflammatory cytokines and protects cells from oxidative stress (52, 56). Macedo et al. perused the therapeutic effect of astaxanthin on phagocytic and microbial capacity, cytokine secretion, and ROS production in human neutrophils. They have concluded that in the presence of astaxanthin, the phagocytic and microbial capacity increased and in contrast to the production of superoxide anion and hydrogen peroxide was reduced without any affecting the capacity of neutrophils as well as cytokines (IL-6 and TNF-α) (57). Research has shown that astaxanthin exerts its protective effect on the acute pulmonary inflammatory disease by inhibiting the MAPK / NF-κB signaling pathway which leads to a decrease in the production of TNF-α and IL-6 inflammatory cytokines (58). Regulation of IL-6 production is important for maintaining brain homeostasis and preventing many neurological disorders. Kim and his colleagues first concluded in a study that astaxanthin inhibits IL-6 expression and NF-κB transcriptional activation in active microglial cells (59). After treating with astaxanthin was observed improvement and reduction of cognitive impairment due to hyperglycemia in diabetic encephalopathy (DE). Astaxanthin inhibits the expression of TNF-α expression in the hippocampus and retina by inhibiting the NF-κB nuclear transfer factor, thus protecting the neurons against inflammatory damage (60). According to the mechanism of action of astaxanthin, this natural compound inhibits the cytokine storm by inhibiting the NF-kB signaling cascade and inhibiting inflammatory cytokines. It thus has the potential to prevent acute respiratory syndrome due to coronavirus infection. Due to the many benefits of natural astaxanthin, clinical trials have been conducted in various fields (61). Recent clinical trial reports on the protective effect of natural astaxanthin on the immune system are presented in Table 1.
Table 1.
Clinical trial studies investigating the protective effect of natural astaxanthin on the immune system
| Tested Parameters | Study design | dosage | Duration of study | Effects of astaxanthin | Ref |
|---|---|---|---|---|---|
| salivary IgA (sIgA) and oxidative stress status in plasma, along with changes in biochemical parameters and total/differential white cell counts | Randomized double-blind and Placebo controlled | 4 mg daily | 12 weeks | improves salivary IgA response and attenuates muscle damage | (54) |
| Immune response and tuberculin test performed | randomized double-blind, placebo-controlled | 8 mg daily | 8 weeks | Decreased DNA damage biomarkers, without affecting lipid peroxidation, decreased C-reactive protein concentration, increased cytotoxic activity of natural killer cells and increased total sub-T and B population due to mitogen-induced l ymphoproliferation, increased IFN-γ and IL-6 | (62) |
| Inflammatory markers (IL-4, IL-6, IL-8, IL-10, interferon-g, CD4, CD8, CD14, CD19, CD25 and CD30) | Randomized, placebo controlled | Not informed | 40 mg | a significant decrease in gastric inflammation in H. pylori-positive patients, no significant changes in the density of H. pylori | (63) |
CONCLUSION
The outbreak of a new coronavirus, called SARS-CoV-2 by the World Health Organization (WHO) has led to the global disease COVID-19, the control and treatment of which is a worldwide concern. The leading solution in the current situation is to avoid contamination and care to prevent its spread. In the case of illness, it is a priority to reduce its complications such as secondary infections or organ failure. The virus invades the body, causing a cytokine storm and an overgrowth of IL-6 and other inflammatory factors, leading to complications such as acute lung syndrome. Controlling and preventing the onset of cytokine storms and reducing inflammatory factors is essential in the cure and prophylaxis of COVID-19. The use of compounds with high antioxidant power in the treatment of COVID-19 is a viable and effective suggestion. Protecting the immune system with antioxidants plays a vital role in health and longevity. A healthy immune system is one indicator of health, and by examining the immune system, lifespan can be predicted. Most medications prescribed for the remedy of diseases, especially chronic diseases, have serious side effects. The ACE2 has a positive impact on the body’s defenses and, unfortunately, has destructive effects owing to its role as a receptor for the coronavirus. Through pretreatment with astaxanthin, the protective role of ACE2 can be used to manage and balance its expression. Hence, the use of natural anti-inflammatory compounds without side effects can be a good option in preventing inflammation and thus controlling cytokine storms. Side effects of Covid-19 diseases, such as metabolic inflammation, reduce the body’s ability to fight coronavirus infection. Natural astaxanthin is a robust anti-inflammatory compound that executes a protective effect on the body by controlling metabolism, balancing the immune system, and preventing the formation of cytokine storms. IL-6 plays a crucial role in various inflammatory diseases such as infections, cancer, cardiovascular disease, and autoimmune disorders and becomes an inflammatory agent with an excessive increase from one anti-inflammatory agent. Multitudinous studies and clinical trials confirm this well that astaxanthin can play a vital role in the control and prevention of inflammatory diseases. In particular, it can balance the immune system and control the release of inflammatory agents.
REFERENCES
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 2020;323:1239–1242. [DOI] [PubMed] [Google Scholar]
- 2.Yi Y, Lagniton PNP, Ye S, Li E, Xu RH. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci 2020;16:1753–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Relationships among lymphocyte subsets, cytokines, and the pulmonary inflammation index in coronavirus (COVID‐19) infected patients. Br J Haematol 2020;189:428–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol 2020;20:363–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conti P, Ronconi G, Caraffa AI, Gallenga CE, Ross R, Frydas I, et al. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents 2020;34:11–15. [DOI] [PubMed] [Google Scholar]
- 6.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020;395:565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen L, Hao G. The role of angiotensin-converting enzyme 2 in coronaviruses/influenza viruses and cardiovascular disease. Cardiovasc Res 2020;116:1932–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang Y, Kim B, Lee JY. Astaxanthin structure, metabolism, and health benefits. J Hum Nutr Food Sci 2013;1:1003. [Google Scholar]
- 9.Shukla G, Yaparthy N, Vanamali J, Kumar CS. Astashine capsules: an excellent choice to boost immune system. Int J Res Pharmacol Pharmacother 2021;5:235–239. [Google Scholar]
- 10.Zhang W, Zhao Y, Zhang F, Wang Q, Li T, Liu Z, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the experience of clinical immunologists from China. Clin Immunol 2020;214:108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chia WY, Kok H, Chew KW, Low SS, Show PL. Can algae contribute to the war with Covid-19? Bioengineered 2021;12:1226–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Talukdar J, Bhadra B, Dattaroy T, Nagle V, Dasgupta S. Potential of natural astaxanthin in alleviating the risk of cytokine storm and improve health in COVID-19. Biomed Pharmacother 2020;132:110886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shukla G, Kanade UL, Yadav M, Sabitha M, Kumar CJS. Astashine capsules: a natural antioxidant, anti-inflammatory helps in maintaining lung health and minimizing SARS-CoV-2 effects in Covid-19 infections. Asian J Basic Sci Res 2020;2:28–42. [Google Scholar]
- 14.Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol 2016;24:490–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Wit E, Van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 2016;14:523–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dariya B, Nagaraju GP. Understanding novel COVID-19: its impact on organ failure and risk assessment for diabetic and cancer patients. Cytokine Growth Factor Rev 2020;53:43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Capeli B, Shao H. (2016). A safe & natural broad-spectrum anti-inflammatory: natural astaxanthin. BGG North America, Inc. [Google Scholar]
- 18.Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science 2020;368:473–474. [DOI] [PubMed] [Google Scholar]
- 19.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. The cytokine release syndrome in severe COVID-19 and interleukin-6 receptor antagonist tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents 2020;55:105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao Y, Zhao Z, Wang Y, Zhou Y, Ma Y, Zuo W. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Am J Respir Crit Care Med 2020;202:756–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu L, Wei Q, Lin Q, Fang J, Wang H, Kwok H, et al. Anti–spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI Insight 2019;4(4):e123158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henry BM, Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol 2020;52:1193–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matsushita K, Marchandot B, Jesel L, Ohlmann P, Morel O. Impact of COVID-19 on the cardiovascular system: a review. J Clin Med 2020;9:1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet 2020;395(10228):e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950–2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Y, Shi L, Yang H, Duan G, Wang Y. Acute kidney injury is associated with the mortality of coronavirus disease 2019. J Med Virol 2020;92:2335–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rizzo P, Vieceli Dalla Sega F, Fortini F, Marracino L, Rapezzi C, Ferrari R. COVID-19 in the heart and the lungs: could we “Notch” the inflammatory storm? Basic Res Cardiol 2020;115:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 2020;87:18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang H, Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol 2020;21(4):e181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bornstein SR, Dalan R, Hopkins D, Mingrone G, Boehm BO. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol 2020;16:297–2988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yuan JP, Peng J, Yin K, Wang JH. Potential health‐ promoting effects of astaxanthin: a high‐value carotenoid mostly from microalgae. Mol Nutr Food Res 2011;55:150–165. [DOI] [PubMed] [Google Scholar]
- 33.Ambati RR, Phang SM, Ravi S, Aswathanarayana RG. Astaxanthin: sources, extraction, stability, biological activities and its commercial applications--a review. Mar Drugs 2014;12:128–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Golkhoo S, Barantalab F, Ahmadi AR, Hassan ZM. Purification of astaxanthin from mutant of Phaffia rhodozyma JH-82 which isolated from forests trees of Iran. Pak J Biol Sci 2007;10:802–805. [DOI] [PubMed] [Google Scholar]
- 35.Najafi N, Ahmadi AR, Hosseini R, Golkhoo S. Gamma irradiation as a useful tool for the isolation of astaxanthin-overproducing mutant strains of Phaffia rhodozyma. Can J Microbiol 2011;57:730–734. [DOI] [PubMed] [Google Scholar]
- 36.Najafi N, Hosseini R, Ahmadi A. Impact of gamma rays on the Phaffia rhodozyma genome revealed by RAPD-PCR. Iran J Microbiol 2011;3:216–221. [PMC free article] [PubMed] [Google Scholar]
- 37.Najafi N, Hosseini R, Ahmadi AR. The effect of gamma irradiation on astaxanthin synthetase encoding gene in two mutant strains of Phaffia rhodozyma. Iran J Microbiol 2013;5:293–298. [PMC free article] [PubMed] [Google Scholar]
- 38.Capelli B, Cysewski G. (2012). Natural astaxanthin : the worlds’ best kept health secret. 2nd ed. Cyanotech. Hawaii, United States. [Google Scholar]
- 39.Vega K, Edwards J, Beilstein P. Subchronic (13-week) toxicity and prenatal developmental toxicity studies of dietary astaxanthin in rats. Regul Toxicol Pharmacol 2015;73:819–828. [DOI] [PubMed] [Google Scholar]
- 40.Chew BP, Park JS. Carotenoid action on the immune response. J Nutr 2004;134:257S–61S. [DOI] [PubMed] [Google Scholar]
- 41.Park JS, Mathison BD, Hayek MG, Massimino S, Reinhart GA, Chew BP. Astaxanthin stimulates cell-mediated and humoral immune responses in cats. Vet Immunol Immunopathol 2011;144:455–461. [DOI] [PubMed] [Google Scholar]
- 42.Fassett RG, Coombes JS. Astaxanthin: a potential therapeutic agent in cardiovascular disease. Mar Drugs 2011;9:447–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bidaran S, Ahmadi AR, Yaghmaei P, Sanati MH, Ebrahim-Habibi A. Astaxanthin effectiveness in preventing multiple sclerosis in animal model. Bratisl Lek Listy 2018;119:160–166. [DOI] [PubMed] [Google Scholar]
- 44.Fakhri S, Abbaszadeh F, Dargahi L, Jorjani M. Astaxanthin: a mechanistic review on its biological activities and health benefits. Pharmacol Res 2018;136:1–20. [DOI] [PubMed] [Google Scholar]
- 45.Wu W, Wang X, Xiang Q, Meng X, Peng Y, Du N, et al. Astaxanthin alleviates brain aging in rats by attenuating oxidative stress and increasing BDNF levels. Food Funct 2014;5:158–166. [DOI] [PubMed] [Google Scholar]
- 46.Grimmig B, Kim SH, Nash K, Bickford PC, Shytle RD. Neuroprotective mechanisms of astaxanthin: a potential therapeutic role in preserving cognitive function in age and neurodegeneration. Geroscience 2017;39:19–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hussein G, Nakamura M, Zhao Q, Iguchi T, Goto H, Sankawa U, et al. Antihypertensive and neuroprotective effects of astaxanthin in experimental animals. Biol Pharm Bull 2005;28:47–52. [DOI] [PubMed] [Google Scholar]
- 48.Lin KH, Lin KC, Lu WJ, Thomas PA, Jayakumar T, Sheu JR. Astaxanthin, a carotenoid, stimulates immune responses by enhancing IFN-γ and IL-2 secretion in primary cultured lymphocytes in vitro and ex vivo. Int J Mol Sci 2015;17:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kidd P. Astaxanthin, cell membrane nutrient with diverse clinical benefits and anti-aging potential. Altern Med Rev 2011;16:355–364. [PubMed] [Google Scholar]
- 50.Fassett RG, Healy H, Driver R, Robertson IK, Geraghty DP, Sharman JE, et al. Astaxanthin vs placebo on arterial stiffness, oxidative stress and inflammation in renal transplant patients (Xanthin): a randomised controlled trial. BMC Nephrol 2008;9:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ursoniu S, Sahebkar A, Serban MC, Banach M. Lipid profile and glucose changes after supplementation with astaxanthin: a systematic review and meta-analysis of randomized controlled trials. Arch Med Sci 2015;11:253–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee SJ, Bai SK, Lee SK, Namkoong S, Na HJ, Ha KS, et al. Astaxanthin inhibits nitric oxide production and inflammatory gene expression by suppressing I(Kappa)B kinase-dependent NF-kB activation. Mol Cells 2003;16:97–105. [PubMed] [Google Scholar]
- 53.Miyachi M, Matsuno T, Asano K, Mataga I. Anti-inflammatory effects of astaxanthin in the human gingival keratinocyte line NDUSD-1. J Clin Biochem Nutr 2015;56:171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baralic I, Andjelkovic M, Djordjevic B, Dikic N, Radivojevic N, Suzin-Zivkovic V, et al. Effect of astaxanthin supplementation on salivary IgA, oxidative stress, and inflammation in young soccer players. Evid Based Complement Alternat Med 2015;2015:783761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yoshihisa Y, Rehman MU, Shimizu T. Astaxanthin, a xanthophyll carotenoid, inhibits ultraviolet‐induced apoptosis in keratinocytes. Exp Dermatol 2014;23:178–183. [DOI] [PubMed] [Google Scholar]
- 56.Speranza L, Pesce M, Patruno A, Franceschelli S, de Lutiis MA, Grilli A, et al. Astaxanthin treatment reduced oxidative induced pro-inflammatory cytokines secretion in U937: SHP-1 as a novel biological target. Mar Drugs 2012;10:890–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Macedo RC, Bolin AP, Marin DP, Otton R. Astaxanthin addition improves human neutrophils function: in vitro study. Eur J Nutr 2010;49:447–457. [DOI] [PubMed] [Google Scholar]
- 58.Cai X, Chen Y, Xie X, Yao D, Ding C, Chen M. Astaxanthin prevents against lipopolysaccharide-induced acute lung injury and sepsis via inhibiting activation of MAPK/NF-κB. Am J Transl Res 2019;11:1884–1894. [PMC free article] [PubMed] [Google Scholar]
- 59.Kim YH, Koh HK, Kim DS. Down-regulation of IL-6 production by astaxanthin via ERK-, MSK-, and NF-κB-mediated signals in activated microglia. Int Immunopharmacol 2010;10:1560–1572. [DOI] [PubMed] [Google Scholar]
- 60.Zhou X, Zhang F, Hu X, Chen J, Wen X, Sun Y, et al. Inhibition of inflammation by astaxanthin alleviates cognition deficits in diabetic mice. Physiol Behav 2015;151:412–420. [DOI] [PubMed] [Google Scholar]
- 61.Donoso A, González-Durán J, Muñoz AA, González PA, Agurto-Muñoz C. “Therapeutic uses of natural astaxanthin: an evidence-based review focused on human clinical trials”. Pharmacol Res 2021;166:105479. [DOI] [PubMed] [Google Scholar]
- 62.Park JS, Chyun JH, Kim YK, Line LL, Chew BP. Astaxanthin decreased oxidative stress and inflammation and enhanced immune response in humans. Nutr Metab (Lond) 2010;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Andersen LP, Holck S, Kupcinskas L, Kiudelis G, Jonaitis L, Janciauskas D, et al. Gastric inflammatory markers and interleukins in patients with functional dyspepsia treated with astaxanthin. FEMS Immunol Med Microbiol 2007;50:244–248. [DOI] [PubMed] [Google Scholar]