Abstract
We recently identified a constitutively expressed exopolysaccharide of Burkholderia pseudomallei which is composed of a unique linear tetrasaccharide repeating unit consisting of three galactose residues and one 3-deoxy-d-manno-2-octulosonic acid residue. In this study we developed a latex agglutination test based on monoclonal antibody 3015, which is specific for this exopolysaccharide, and evaluated this test for rapid identification of B. pseudomallei grown on agar plates. All 74 environmental and clinical B. pseudomallei strains tested, originating from different areas of Southeast Asia, northern Australia, and Africa, showed a strong and specific agglutination. B. pseudomallei-like organisms and a variety of other bacteria did not react. In conclusion this monoclonal antibody-based test is a simple, rapid, and highly specific method for identifying B. pseudomallei culture isolates from different geographic areas.
Melioidosis is an infectious disease caused by the gram-negative rod Burkholderia pseudomallei. The disease is now recognized as an important public health problem in certain areas of the tropics (4). Identification of this species can be achieved by a combination of the commercial API 20 NE biochemical kit and a simple screening system involving Gram’s stain, the oxidase reaction, typical growth characteristics, and resistance to certain antibiotics (5). However, these methods are relatively laborious, and classical identification seldom requires less than 48 h (11). The early diagnosis of B. pseudomallei is crucial for appropriate antibiotic treatment, and therefore suspicious colonies should be rapidly identified as soon as they are visible on the agar. Recently, a nonvirulent biotype of B. pseudomallei was defined by the ability to assimilate l-arabinose (8), but it could not be distinguished immunologically (12). It has been proposed that this l-arabinose-assimilating biotype should be reclassified as a B. pseudomallei-like species, termed B. thailandensis sp. nov (2).
We recently identified and purified a constitutively expressed species-specific exopolysaccharide of B. pseudomallei reactive with the monoclonal antibody (MAb) 3015 immunoglobulin G1 (IgG1) (10). This exopolysaccharide appeared to be a unique linear tetrasaccharide repeating unit consisting of three galactose residues and one 3-deoxy-d-manno-2-octulosonic acid (Kdo) residue (6). In this study we developed a latex agglutination test based on the MAb 3015 IgG1 and evaluated this test for the rapid identification of B. pseudomallei culture isolates originating from different areas in Southeast Asia, Australia, and Africa.
Bacteria and culture conditions.
All bacterial strains used in this study are listed in Table 1. The l-arabinose-nonassimilating (Ara−) B. pseudomallei strains originating from Thailand were either clinical strains obtained from patients admitted with melioidosis to Sappasitprasong Hospital, Ubon Ratchatani, northeast Thailand, or soil isolates from the surrounding area (12). l-Arabinose-assimilating (Ara+) B. pseudomallei-like strains were from the same environment (12). B. pseudomallei strains (Ara−) originating from other countries were obtained either from the National Collection of Type Cultures (NCTC), United Kingdom, or from Tyron Pitt, Laboratory of Hospital Infection, Central Public Health Laboratory, London, United Kingdom. All bacterial strains were grown on Columbia agar for 24 h at 37°C.
TABLE 1.
Reactivities of B. pseudomallei and non-B. pseudomallei isolates with the MAb 3015 IgG1-based latex test
| Strain | Source | Origin | Latex test reactiona |
|---|---|---|---|
| B. pseudomallei strains | |||
| NCTC 4845 | Monkey | Singapore | + |
| NCTC 1688 | Rat | Malaysia | + |
| NCTC 4846 | Monkey | Singapore | + |
| NCTC 6700 | Human | Malaysia | + |
| NCTC 7383 | Human | Burma | + |
| NCTC 7431 | Human | Unknown | + |
| NCTC 8016 | Sheep | Australia | + |
| NCTC 10274 | Human | Malaysia | + |
| NCTC 10276 | Human | Bangladesh | + |
| NCTC 8707 | NDb | Singapore | + |
| NCTC 8708 | ND | Singapore | + |
| NCTC 11642 | ND | Unknown | + |
| 308A | Human | Thailand | + |
| 309A | Human | Thailand | + |
| 310B | Human | Thailand | + |
| 312A | Human | Thailand | + |
| 369A | Human | Thailand | + |
| 388A | Human | Thailand | + |
| 406B | Human | Thailand | + |
| 423A | Human | Thailand | + |
| 428D | Human | Thailand | + |
| 430E | Human | Thailand | + |
| 435A | Human | Thailand | + |
| 448A | Human | Thailand | + |
| 688A | Human | Thailand | + |
| 708A | Human | Thailand | + |
| 722A | Human | Thailand | + |
| 778A | Human | Thailand | + |
| 785A | Human | Thailand | + |
| 843B | Human | Thailand | + |
| 846A | Human | Thailand | + |
| 854A | Human | Thailand | + |
| E08 | Soil | Thailand | + |
| E202 | Soil | Thailand | + |
| E203 | Soil | Thailand | + |
| E208 | Soil | Thailand | + |
| E210 | Soil | Thailand | + |
| E212 | Soil | Thailand | + |
| E213 | Soil | Thailand | + |
| E219 | Soil | Thailand | + |
| E220 | Soil | Thailand | + |
| E235 | Soil | Thailand | + |
| E237 | Soil | Thailand | + |
| 521 | Human | Pakistan | + |
| MK441 | Monkey | Philippines | + |
| MK452 | Monkey | Philippines | + |
| MK453 | Monkey | Philippines | + |
| M1900 | Monkey | Philippines | + |
| M1831 | Monkey | Indonesia | + |
| M1867 | Monkey | Indonesia | + |
| Ramal | Human | Thailand | + |
| 56-91 | Camel | Chad | + |
| 770429 | Soil | Madagascar | + |
| P19535/91 | Human | Singapore | + |
| Sar1 | Human | Sarawak | + |
| 6068 | ND | Southeast Asia | + |
| T8 + 8 | ND | Austria | + |
| 501944 | Monkey | Philippines | + |
| NT08 | Soil | Niger | + |
| 7605 | Manure | France | + |
| Ducrete | Human | Vietnam | + |
| S1 | Human | Singapore | + |
| S3 | Human | Singapore | + |
| S6 | Human | Singapore | + |
| S9 | Human | Singapore | + |
| S12 | Human | Singapore | + |
| S15 | Human | Singapore | + |
| L19 | ND | ND | + |
| L23 | ND | ND | + |
| L47 | ND | ND | + |
| L85 | ND | ND | + |
| L87 | ND | ND | + |
| L90 | ND | ND | + |
| L91 | ND | ND | + |
| B. pseudomallei-like strains | |||
| E27 | Soil | Thailand | − |
| E201 | Soil | Thailand | − |
| E205 | Soil | Thailand | − |
| E211 | Soil | Thailand | − |
| E221 | Soil | Thailand | − |
| E229 | Soil | Thailand | − |
| E232 | Soil | Thailand | − |
| E236 | Soil | Thailand | − |
| E217 | Soil | Thailand | − |
| Other Burkholderia species | |||
| B. cepacia LMGc 1222T | − | ||
| IMMd Xy450 | − | ||
| ATCCe 17478 | − | ||
| ATCC 17759 | − | ||
| ATCC 25416 | − | ||
| B. solanacearum LMG 2299T | − | ||
| LMG 7005 | − | ||
| B. pickettii LMG 5942 | − | ||
| LMG 7005 | − | ||
| Pseudomonas species | |||
| P. aeruginosa LMG 1242T | − | ||
| P. alcaligenes LMG 1224 t1 | − | ||
| P. aureofaciens LMG 1245T | − | ||
| P. fluorescens bv. 1 LMG 1794T | − | ||
| bv. 3 LMG 1244 | − | ||
| bv. 4 LMG 5939 | − | ||
| P. mendocina LMG 1223 | − | ||
| P. pseudoalcaligenes LMG 1225T | − | ||
| P. putida bv. A LMG 2257T | − | ||
| bv. B LMG 1246 t1 | − | ||
| LMG 5837 | − | ||
| LMG 12644 | − | ||
| P. stutzeri LMG 2243 | − | ||
| P. diminuta LMG 2089T | − | ||
| P. vesicularis LMG 2350T | − | ||
| Other genera | |||
| Comamonas acidovorans LMG 5932 | − | ||
| Comamonas testosteroni LMG 1787 | − | ||
| Stenotrophomonas maltophilia | − | ||
| ATCC 17448 | − | ||
| ATCC 17406 | − | ||
| Klebsiella pneumoniae ATCC 10031 | − | ||
| NCTC 11228 | − | ||
| NCTC 10996f | − | ||
| Klebsiella oxytoca IMM R18f | − | ||
| Escherichia coli ATCC 11229 | − | ||
| ATCC 10539 | − | ||
| ATCC 25922 | − | ||
| ATCC 29079 | − | ||
| Acinetobacter baumannii IM R105f | − | ||
| ATCC 19606 | − | ||
| Acinetobacter lwoffi IMM R53f | − | ||
| ATCC 15309 | − | ||
| Enterobacter cloacae ATCC 23355 | − | ||
| Citrobacter freundii IMM R24 | − | ||
| Citrobacter diversus IMM 30 | − | ||
| Serratia marcescens IMM K10 | − | ||
| Enterococcus faecium ATCC 19434 | − | ||
| Streptococcus pneumoniae IMM 46 | − | ||
| Staphylococcus epidermidis ATCC 12228 | − |
+, positive; −, negative.
ND, not documented.
LMG, Belgian Collection of Culture Strains, Universiteit Gent, Laboratorium voor Microbiologie, Ghent, Belgium.
IMM, Institute of Medical Microbiology, Hannover, Germany.
ATCC, American Type Culture Collection.
With these strains heat-treated bacterial supernatant had to be used to eliminate nonspecific reactions of bacterial cells with both the specific and control latex reagent.
ELISA.
The production of MAb 3015 IgG1 and the enzyme-linked immunosorbent assay (ELISA) used in this study have previously been described (10). Briefly, single U-shaped wells of nonflexible polystyrol microtiter plates were coated with heat-treated B. pseudomallei and B. pseudomallei-like cells (2 × 108 cells/ml) for 2 h. After washing and blocking steps, MAb 3015 IgG1 containing hybridoma supernatant (5 μg/ml) was incubated for 2 h followed by the addition of biotin-labeled rabbit anti-mouse IgG1 (1:5,000 in buffer A-BSA; Zymed, San Francisco, Calif.) (buffer A-BSA is buffer A [0.01 M potassium phosphate buffer made isotonic with saline, pH 7.5] containing 1% [wt/vol] bovine serum albumin [BSA] and 0.1% [wt/vol] NaN3) for 30 min. Microtiter plates were then developed with streptavidine coupled to β-galactosidase. 4-Methylumbelliferyl-β-d-galactopyranoside was used as substrate, and the fluorescent product was measured with a microplate fluorometer (Titertek Fluoroskan 2; Labsystems, Helsinki, Finland) with an excitation wavelength of 355 nm and an emission wavelength of 460 nm. Fluorescence intensity is given as relative fluorescence units.
Preparation of the latex reagent.
MAb 3015 containing hybridoma supernatant and a control IgG1 were concentrated by ultrafiltration with a ProVario 3 apparatus (Pall-Filtron, Karlstein, Germany) by using a membrane with a cutoff of 10 kDa and then purified by affinity chromatography on protein-G-Sepharose (Pharmacia, Uppsala, Sweden). Purified antibodies were diluted in buffer A. Latex particles (1.07 μm in diameter) supplied as a 10% (wt/vol) suspension (Sigma) were washed three times in distilled water and resuspended to the original volume. All washing steps were performed at 13,600 × g for 5 min at room temperature. Sensitization of latex particles was performed by incubating equal volumes of particle solutions and antibody solutions (1 mg/ml) for 2 h at 37°C with gentle shaking. The latex particles were then washed three times with distilled water and resuspended in buffer A-BSA to obtain a 5% (wt/vol) suspension.
Latex agglutination assay.
The agglutination test was performed by placing 10 μl of the test (MAb 3015 IgG1) or control (unrelated IgG1) latex suspension and 10 μl of buffer A on a black-coated agglutination card. A small portion of a colony was emulsified directly into the drop of buffer and mixed with the latex suspension. Agglutination was detected visually after rotation for 1 min. Agglutination with the control latex was always done in parallel to recognize nonspecific agglutination. When heat-treated bacterial supernatant was used for agglutination, one colony was emulsified in 1 ml of buffer A and heated in a microcentrifuge tube for 5 min at 100°C. The suspension was then centrifuged for 5 min at 13,600 × g, and the test was performed with 10 μl of the supernatant.
Results.
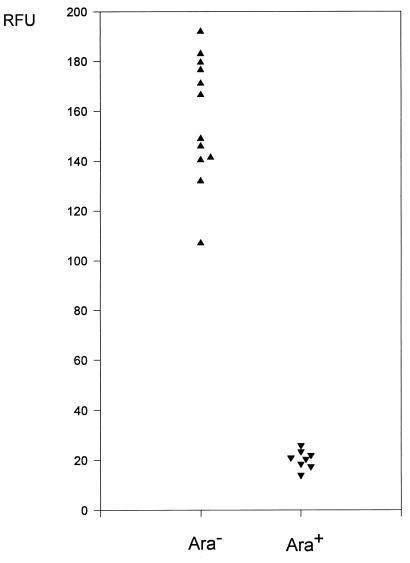
To test the capability of MAb 3015 specific for a B. pseudomallei exopolysaccharide to discriminate between Ara+ B. pseudomallei-like strains and Ara− B. pseudomallei strains we first performed an ELISA with heat-treated bacterial cells (Fig. 1). The results indicate that Ara+ B. pseudomallei-like organisms, in contrast to Ara− B. pseudomallei, do not synthesize the galactose- and Kdo-containing tetrasaccharide repeating unit recognized by MAb 3015. The results of the latex agglutination test based on MAb 3015 for the identification of B. pseudomallei cultures are shown in Table 1. All 74 B. pseudomallei strains tested including 12 NCTC strains and 62 clinical and environmental isolates originating from different areas of Southeast Asia, northern Australia, and Africa were positive, showing a strong and rapid agglutination with the MAb 3015 latex, whereas no reaction occurred with the control latex. To further evaluate the specificity of the test a variety of gram-positive and gram-negative bacteria including different Pseudomonas and Burkholderia ssp. were tested (Table 1). All 56 non-B. pseudomallei strains, including the arabinose-positive B. pseudomallei-like strains, were negative. A total of 52 strains agglutinated with neither the specific nor the control latex. Four strains showed reactions with both the B. pseudomallei-specific latex and the control latex. These nonspecific reactions were absent when bacteria were heat treated and bacterial supernatant was tested. In these tests heat-treated B. pseudomallei supernatant served as a positive control and always strongly agglutinated. The sensitized latex particles have now been stable for more than 6 months at 4°C.
FIG. 1.
Reactivity of IgG1 MAb 3015 in an ELISA with 12 B. pseudomallei isolates (Ara−, arabinose nonassimilators) and 8 environmental B. pseudomallei-like isolates (Ara+, arabinose assimilators). Each point is the mean of duplicate determinations. RFU, relative fluorescence units. RFU values of B. pseudomallei-like isolates reacted with MAb 3015 were indistinguishable from the values obtained with unrelated IgG1 and were also indistinguishable from B. pseudomallei isolates reacted with unrelated IgG1 (not shown).
Discussion.
A previous study described a latex agglutination test for the identification of B. pseudomallei isolates from patients in Thailand which was based on a polyclonal rabbit serum raised against B. pseudomallei (9). However, this test was also found to be positive with l-arabinose-assimilating B. pseudomallei-like strains (12). It seems likely that this cross-reactivity is at least partly due to common lipopolysaccharide epitopes between the avirulent B. pseudomallei-like organisms and virulent B. pseudomallei (1). Recently, a MAb of the IgM isotype which directly agglutinated B. pseudomallei strains from Thailand was described (7). The authors stated that their MAb is probably reactive with an epitope of the lipopolysaccharide. Reactivity with B. pseudomallei strains isolated from tropical areas outside of Thailand was not tested. The reactivity of our latex reagent based on the MAb 3015 IgG1, specific for a B. pseudomallei exopolysaccharide, with strains from many different locations in Southeast Asia, Australia, and Africa extends our previous finding of a constitutive expression of the B. pseudomallei exopolysaccharide independent of the geographical origin of the strain (10). The IgG1 isotype of MAb 3015 used in our test has now proved to be stable for more than 6 months, which is important for routine use in any diagnostic laboratory. In conclusion, this MAb-based test offers a rapid and simple method for the reliable identification of B. pseudomallei from different parts of the world. Future studies will determine the applicability of this test for the detection of the exopolysaccharide antigen in the body fluids of patients.
Acknowledgments
We thank T. L. Pitt for kindly providing bacterial strains and D. Bitter-Suermann for continuous encouragement.
REFERENCES
- 1.Anuntagool N, Intachote P, Wuthiekanun V, White N J, Sirisinha S. Lipopolysaccharide from nonvirulent Ara+Burkholderia pseudomallei isolates is immunologically indistinguishable from lipopolysaccharide from virulent Ara− clinical isolates. Clin Diagn Lab Immunol. 1998;5:225–229. doi: 10.1128/cdli.5.2.225-229.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brett P J, DeShazer D, Woods D E. Burkholderia thailandensis sp. nov., a Burkholderia pseudomallei-like species. Int J Syst Bacteriol. 1998;48:317–320. doi: 10.1099/00207713-48-1-317. [DOI] [PubMed] [Google Scholar]
- 3.Chaowagul W, White N J, Dance D A B, Wattanagoon Y, Naigowit P, Davis T M E, Looareesuwan S, Pitakwatchara N. Melioidosis: a major cause of community acquired septicemia in Northeastern Thailand. J Infect Dis. 1989;159:890–899. doi: 10.1093/infdis/159.5.890. [DOI] [PubMed] [Google Scholar]
- 4.Dance D A B. Melioidosis: the tip of the iceberg? Clin Microbiol Rev. 1990;4:52–60. doi: 10.1128/cmr.4.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dance D A B, Wuthiekanun V, Naigowit P, White N J. Identification of Pseudomonas pseudomallei in clinical practice: use of simple screening tests and API 2ONE. J Clin Pathol. 1989;42:645–648. doi: 10.1136/jcp.42.6.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nimtz M, Wray V, Domke T, Brenneke B, Häußler S, Steinmetz I. Structure of an acidic exopolysaccharide of Burkholderia pseudomallei. Eur J Biochem. 1997;250:608–616. doi: 10.1111/j.1432-1033.1997.0608a.x. [DOI] [PubMed] [Google Scholar]
- 7.Rugdeck P, Anuntagool N, Sirisinha S. Monoclonal antibodies to Pseudomonas pseudomallei and their potential for diagnosis of melioidosis. Am J Trop Med Hyg. 1995;52:231–235. doi: 10.4269/ajtmh.1995.52.231. [DOI] [PubMed] [Google Scholar]
- 8.Smith M D, Angus B J, Wuthiekanun V, White N J. Arabinose assimilation defines a nonvirulent biotype of Burkholderia pseudomallei. Infect Immun. 1997;65:4319–4321. doi: 10.1128/iai.65.10.4319-4321.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith M D, Wuthiekanun V, Walsh A L, Pitt T L. Latex agglutination test for identification of Pseudomonas pseudomallei. J Clin Pathol. 1993;46:374–375. doi: 10.1136/jcp.46.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinmetz I, Rohde M, Brenneke B. Purification and characterization of an exopolysaccharide of Burkholderia (Pseudomonas) pseudomallei. Infect Immun. 1995;63:3959–3965. doi: 10.1128/iai.63.10.3959-3965.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wuthiekanun V, Dance D A B, Wattanagoon Y, Suputtamongkol Y, Chaowagul W, White N J. The use of selective media for the isolation of Pseudomonas pseudomallei in clinical practice. J Med Microbiol. 1990;33:121–126. doi: 10.1099/00222615-33-2-121. [DOI] [PubMed] [Google Scholar]
- 12.Wuthiekanun V, Smith M D, Dance D A B, Walsh A L, Pitt T L, White N J. Biochemical characteristics of clinical and environmental isolates of Burkholderia pseudomallei. J Med Microbiol. 1996;44:408–412. doi: 10.1099/00222615-45-6-408. [DOI] [PubMed] [Google Scholar]