Abstract
What is already known about this topic?
The “1-3-7” approach to malaria surveillance and response was a key measure for malaria elimination in China and was first introduced into the World Health Organization (WHO) as an international guideline for malaria surveillance and response in 2018.
What is added by this report?
The “1-3-7” approach was well implemented in Henan Province from 2012−2018. Over this study period, a total of 1,294 malaria cases were detected and reported, and all cases were diagnosed and reported within 1 day with 99.23% (1,284/1,294) of cases were investigated within 3 days. In addition, 93.7% (1,212/1,294) of foci were investigated and vector control was implemented within 7 days at all residual non-active foci to prevent further spread.
What are the implications for public health practice?
The “1-3-7” controlling pattern would be an effective and approachable method for implementation especially in malaria-eliminating countries and regions, but the interval from symptom onset to diagnosis cannot be ignored. Thus, the roles and responsibilities that all actors involved in the health sector must be specified too.
The “1-3-7” approach to malaria surveillance and response was a key measure for malaria elimination in China that aims to have all cases of malaria reported within 1 day, case investigation conducted within 3 days, and an in-depth investigation conducted within 7 days. The study aimed to assess the interventions and measure the impact they may have on malaria-related burden to guide malaria programming. Data from the National Notifiable Disease Reporting System (NNDRS) and the Parasitic Diseases Information Reporting Management System (PDIRMS) from 2012 to 2018 were collected and analyzed to evaluate the implementation of the “1-3-7” approach. Additionally, the interval time from the onset of fever symptoms to diagnosis of cases were also analyzed. A total of 1,294 malaria cases were reported in Henan and all cases were reported to NNDRS within 1 day after confirmed with 99.2% (1,284/1,294) were investigated within 3 days after diagnosis. In addition, 93.7% (1,212/1,294) of foci were investigated within 7 days, 13.1% (170/1,294) of malaria cases were definitively diagnosed within 24 hours after onset, and the median onset-to-diagnosis time was 3 days. The “1-3-7” approach was well implemented around the province, but onset-to-diagnosis time is another important indicator that cannot be ignored. To shorten this time, the roles and responsibilities of all actors involved in the health sector need to be specified.
Henan Province is located in the middle eastern region of China and the middle and lower reaches of the Yellow River. Natural climate conditions here were suitable for malaria transmission, which had seriously affected the physical health and social and economic development of the whole province since the Yin and Shang Dynasties 4,000 years ago. Plasmodium vivax was endemic all over the province and Plasmodium falciparum was endemic in the area south of 33° N before 1987 (1). The remarkable feature of the malaria epidemic in Henan Province was the alternation between local outbreaks and widespread epidemics. There were three countrywide epidemics in the 1950s, 1960s, and early 1970s, and in 1970, the incidence of malaria in Henan Province reached as high as 1,694.44 / 10,000 (2). However, after the collective work and efforts of several generations, no indigenous cases have been reported since 2012, and recently with the increase of investment abroad and international communication, people who participated in international activities also increased, which resulted in an increase of imported malaria cases in Henan (3). Therefore, strict malaria control measures were of importance to the populations who returned to China.
In order to avoid local reintroduction of malaria, Henan Province implemented the “1-3-7” approach. The “1-3-7” approach to malaria surveillance and response was a key measure for malaria elimination in China that referred to the reporting of malaria cases to local health facilities within 1 day, further investigation of index cases and detection of other cases in households by case investigation teams within 3 days, and expanded case detection and entomological, ecological, and intervention assessments by focus investigation teams within 7 days (4). It is important to periodically assess the key malaria interventions and measure the impact they may have on malaria-related burden to guide malaria programming, and thus, the implementation of the “1-3-7” approach and the onset-to-diagnosis time of malaria cases between 2012 and 2018 were analyzed. The results showed that key malaria interventions were conducted well, but another problem was exposed: the median number of days for the onset-to-diagnosis time was 3 days, but 1/4 of the cases took 6 days and the longest took up to 31 days.
In this paper, we try to evaluate the implementation of the “1-3-7” approach, and the onset-diagnosis time of malaria cases. Data from the NNDRS and PDIRMS from 2012 to 2018 were collected and analyzed, which included date of onset, diagnosis and reporting, case investigation, focus investigation, and indoor residual spraying (IRS). Summary statistics and proportions were used and comparisons between groups were assessed using the chi-square test and/or the rank sum test. Level of significance was set at a p≤0.05.
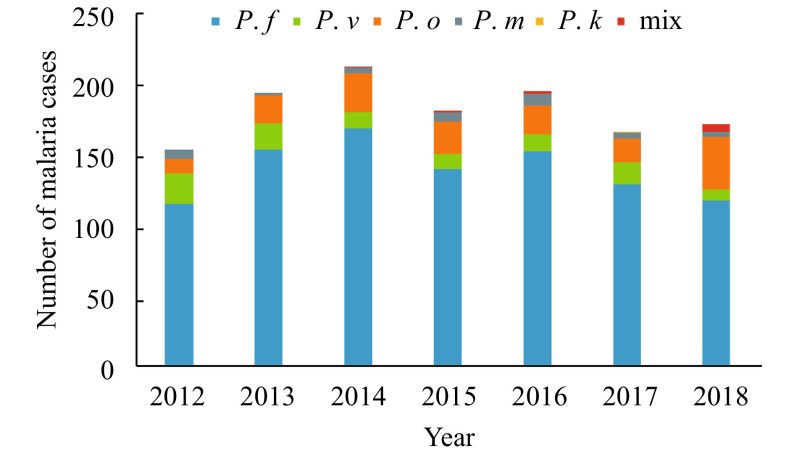
During the 7 years period, a total of 1,294 malaria cases were reported in Henan and all of them were imported cases. There were 991 cases of P. falciparum malaria, 100 cases of P. vivax, 157 cases of P. ovale, 36 cases of P. malariae, 9 cases of mixed infection, and 1 case of P. knowlesi (Figure 1).
Figure 1.
Plasmodium species of malaria cases in Henan Province, 2012–2018. Abbreviation: P. f=Plasmodium falciparum, P. v=Plasmodium vivax, P. o=Plasmodium ovale, P. m=Plasmodium malariae, P. k=Plasmodium knowlesi, mix=mixed infection.
All malaria cases were reported to NNDRS within 1 day after confirmed, 99.2% (1,284/1,294) of cases were investigated within 3 days after diagnosis, 93.7% (1,212/1,294) of foci were investigated within 7 days, 4.7% (61/1,294) of foci were residual non-active foci with potential transmission, and 100% (61/61) were carried out vector control measures with 141,217 people being protected by the IRS (Table 1).
Table 1. The “1-3-7” approach to malaria surveillance and response in Henan Province during 2012–2018.
| Year | Total no. of cases | No. of case reported within 1 day (%) | No. of case investigated within 3 days (%)* | No. of foci investigated within 7 days (%) | No. of active foci (%) | No. of active foci treated by IRS (%) | No. of people protected by IRS |
| Abbreviations: IRS=indoor residual spraying.
* χ2=3.195, p=0.784. | |||||||
| 2012 | 156 | 156(100) | 155(99.4) | 156(100.0) | 18(11.5) | 18(100) | 877 |
| 2013 | 197 | 197(100) | 196(99.5) | 197(100.0) | 9(4.6) | 9(100) | 78,400 |
| 2014 | 216 | 216(100) | 213(98.6) | 216(100.0) | 5(2.3) | 5(100) | 21,944 |
| 2015 | 184 | 184(100) | 183(99.5) | 184(100.0) | 6(3.3) | 6(100) | 17,814 |
| 2016 | 198 | 198(100) | 196(99.0) | 198(100.0) | 6(3.0) | 6(100) | 14,941 |
| 2017 | 169 | 169(100) | 169(100.0) | 96(56.8) | 11(6.5) | 11(100) | 5,704 |
| 2018 | 174 | 174(100) | 172(98.9) | 165(94.8) | 6(3.4) | 6(100) | 1,537 |
| Total | 1,294 | 1,294(100) | 1,284(99.2) | 1,212(93.7) | 61(4.7) | 61(100) | 141,217 |
In 2012−2018, 13.14% (170/1,294) of malaria cases in Henan were definitively diagnosed within 24 hours after onset, and the median onset-to-diagnosis time was 3 days [inter quartile range (IQR), 1-6 days]. The longest interval was 31 days in 2012. There was a statistical difference in the onset-diagnosis time between 2018 and 2012 (Z=5.015, p<0.05) (Table 2).
Table 2. The onset-diagnosis time of malaria cases in Henan Province during 2012–2018.
| Year | Total no. of cases | No. of case diagnosed within 1 day (%)* | The onset-diagnosis time(day) | ||
| Median | IQR | The longest interval | |||
| Abbreviations: IQR=inter quartile range.
* Z=5.015, p<0.05. | |||||
| 2012 | 156 | 23(14.74) | 3 | (1−6) | 31 |
| 2013 | 197 | 22(11.17) | 3 | (1−6) | 29 |
| 2014 | 216 | 24(11.11) | 3 | (1−6) | 27 |
| 2015 | 184 | 28(15.22) | 3 | (1−6) | 29 |
| 2016 | 198 | 41(20.71) | 3 | (1−5) | 30 |
| 2017 | 169 | 17(10.06) | 3 | (1−6) | 30 |
| 2018 | 174 | 15(8.62) | 3 | (1−5) | 30 |
| Total | 1,294 | 170(13.14) | 3 | (1−6) | 31 |
DISCUSSION
The “1-3-7” approach played a crucial role in malaria elimination in China, and this approach was therefore introduced by the World Health Organization (WHO) to be a guideline to instruct malaria control programs worldwide, especially in countries or regions where malaria is close to elimination (5). Henan Province launched a malaria elimination campaign in 2010 and strictly implemented the “1-3-7” approach across the whole province (6). As a result, the NNDRS benefitted heavily from the promptness of malaria reports, no indigenous cases have been found since 2012, and malaria elimination was achieved in 2019 (7). These experiences will pave the way for other malaria eliminating countries and areas to do the same.
All malaria cases that are diagnosed by health facilities at the provincial, district, and local levels can be reported promptly, and all Plasmodium species require reporting by law. In the era of big data, a well-defined health delivery process ensures availability of accurate, timely, and accessible health data, which is extremely important for the prevention and control of infectious diseases. While the overall treatment rate of foci within 7 days was 93.7% in 2012 to 2018, the rate was stable at 100% from 2012 to 2016 but dropped to 56.8% in 2017 before recovering to 94.8% in 2018 (3). This was likely due to the recording and statistical method being changed in 2017 where all foci were in fact disposed within 7 days, but some data were reported after 168 hours and could not be recognized by the system.
The “1-3-7” approach to malaria surveillance and response was well implemented but is limited to situations where malaria cases has just been detected. Although the implementation of the “1-3-7” approach is essential to prevent and control the reintroduction of malaria, the onset-to-diagnosis time cannot be ignored. The time before the "1" mentioned in the"1-3-7" method is not within the public health facilities' control, but it is essential for effective patient management. Malaria is generally treatable when effective treatment is commenced early, whereas delay in treatment may lead to serious consequences including death. Essentially all deaths caused by P. falciparum malaria were related to longer onset-to-diagnosis time.
While some achievements have been made during the study period, such as a decrease in the longest onset-to-diagnosis time by 2018, the onset-to-diagnosis time was still dissatisfactory and comparable to the difficult situations in Shanxi Province and along the China-Myanmar border (8-9). The exact reasons for delays in seeking care were unclear, but the roles and responsibilities of all actors involved in the health sector need to be specified. First, public awareness for malaria should be enhanced through community-based and school-based health education. Second, doctors should be trained to improve their capacity for case detection, diagnosis, and treatment to avoid the development of severe illness or unnecessary death. Finally, the entry-exit inspection and quarantine departments should oversee malaria health education over people entering and leaving China and people associated with the border ports. In addition, effective multi-sector cooperation and coordination mechanisms, particularly for CDCs and the entry-exit inspection and quarantine departments, should be strengthened to help facilitate information exchange and sharing.
However, the implementation of the “1-3-7” approach to malaria surveillance and response was subject to some challenges, such as the level of detail in epidemiological investigations, correct case classifications, accurate foci assessments, suitable foci interventions, etc. (10), so securing the quality of the approach at all levels should be the goal for further malaria control.
This study is subject to some limitations. Although data covered a significant length of time and a large geographical area, the results are based on passively-reported data and may not fully represent the current situation. Furthermore, due to the nature of the study, the results presented may not be representative of the whole of China.
References
- 1.Zhang HW, Liu Y, Zhang SS, Xu BL, Li WD, Tang JH, et al Preparation of malaria resurgence in China: case study of vivax malaria re-emergence and outbreak in Huang-Huai Plain in 2006. Adv Parasitol. 2014;86:205–30. doi: 10.1016/B978-0-12-800869-0.00008-1. [DOI] [PubMed] [Google Scholar]
- 2.Xu BL, Su YP, Shang LY, Zhang HW Malaria control in Henan Province, People’s Republic of China. Am J Trop Med Hyg. 2006;74(4):564–7. doi: 10.4269/ajtmh.2006.74.564. [DOI] [PubMed] [Google Scholar]
- 3.Liu Y, Zhou RM, Qian D, Yang CY, Zhang HW. Analysis of malaria epidemiological characteristics in Henan Province from 2005 to 2013. Chin J Parasitol Parasit Dis 2014; 32(6): 419-22. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgjscxyjscbzz201406003. (In Chinese)
- 4.Zhou SS, Zhang SS, Zhang L, Rietveld AEC, Ramsay AR, Zachariah R, et al China’s 1-3-7 surveillance and response strategy for malaria elimination: is case reporting, investigation and foci response happening according to plan? Infect Dis Poverty. 2015;4:55. doi: 10.1186/s40249-015-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Malaria surveillance, monitoring & evaluation: a reference manual. Geneva: World Health Organization; 2018. https://www.who.int/malaria/publications/atoz/9789241565578/en/.
- 6.Zhang HW, Liu Y, Yang CY, Qian D, Zhou RM, Chen JS, et al Mid-term assessment report of Malaria Elimination Action Plan in Henan. China Trop Med. 2016;16(4):328–32. doi: 10.13604/j.cnki.46-1064/r.2016.04.07. [DOI] [Google Scholar]
- 7.Zhang HW, Zhang QQ, Yang CY, Qian D, Lu DL, Zhao YL, et al Progress of malaria elimination and achievements of scientific researches in Henan Province. Henan J Prev Med. 2019;30(10):721–5. doi: 10.13515/j.cnki.hnjpm.1006-8414.2019.010.001. [DOI] [Google Scholar]
- 8.Wang T, Zhou SS, Feng J, Oo MM, Chen J, Yan CF, et al Monitoring and evaluation of intervals from onset of fever to diagnosis before “1-3-7” approach in malaria elimination: a retrospective study in Shanxi Province, China from 2013 to 2018. Malar J. 2019;18(1):235. doi: 10.1186/s12936-019-2865-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng J, Liu J, Feng XY, Zhang L, Xiao HH, Xia ZG Towards malaria elimination: monitoring and evaluation of the “1-3-7” approach at the China-Myanmar border. Am J Trop Med Hyg. 2016;95(4):806–10. doi: 10.4269/ajtmh.15-0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu GY, Liu YB, Beiersmann C, Feng Y, Cao J, Mü ller O Challenges in and lessons learned during the implementation of the 1-3-7 malaria surveillance and response strategy in China: a qualitative study. Infect Dis Poverty. 2016;5(1):94. doi: 10.1186/s40249-016-0188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]