Abstract
What is already known about this topic?
Prompt, accurate diagnosis is an essential part of malaria elimination strategies. Insufficient malaria diagnosis capacity will be a potential risk for malaria reintroduction.
What is added by this report?
Health facilities at the county and prefectural levels were the most concentrated facilities for initial diagnosis of malaria (68.2%) and confirmation (76.4%). More than 65% of cases could not be diagnosed within 1 day of onset, and only 89.4% of laboratory-confirmed cases were accurate.
What are the implications for public health practice?
Malaria health education should be strengthened to improve public awareness and health professionals’ vigilance of malaria, thereby shortening the diagnostic intervals. In addition, the capacity of malaria diagnosis, especially Plasmodium speciation, should be improved to ensure accurate diagnosis and appropriate treatment.
Malaria had previously been one of the most serious infectious diseases in China. Fortunately, China is close to achieving malaria elimination nationwide with country-led and country-owned efforts, such as the strong case-based surveillance and response systems, especially after inauguration of the National Malaria Elimination Action Plan 2010–2020 of China. No indigenous malaria cases have been reported since 2017, although there were still more than 2,500 imported cases annually including over 100 patients with severe symptoms and approximately 10 deaths in 2017 and 2018, respectively (1-2). The prompt and reliable detection of parasites and diagnosis of malaria cases is an essential component in national malaria elimination programs as it not only assures that all patients receive appropriate treatments but also greatly improves the reliability of surveillance to the point of stopping malaria transmission. Even after elimination, it is still crucial to prevent malaria reintroduction (malaria reintroduction refers to the occurrence of introduced cases: cases of the first-generation local transmission that are epidemiologically linked to a confirmed imported case in a country or area where the disease had previously been eliminated) (3-4) and consolidate the accomplishment.
Prompt parasitological diagnosis by microscopy or a rapid diagnostic test is recommended by the World Health Organization for all patients suspected of having malaria based on a defined set of clinical criteria before therapy is initiated (4). To ensure the quality of malaria diagnosis, a reliable National Malaria Diagnosis Reference Laboratory Network (NMDRLN) has been established in China composed of 1 national and 24 historically-malaria-endemic provincial laboratories (5). The function of the network is for case verification and also for capacity building and maintenance. Species belonging to Plasmodium in all reported cases must be validated using microscopy and PCR in network laboratories. Malaria microscopists from both the national and provincial levels performed quite well in Plasmodium spp. speciation but not those from the below provincial levels, according to a series of external competency assessments and national technique competitions on malaria microscopy (6). Currently, all health facilities have potential access to testing and can become the first line of defense against imported malaria, but limited data were found about their performance in the process of malaria diagnosis in routine work.
Individual malaria case data in 2017 and 2018 were extracted from the Parasitic Diseases Information Reporting Management System (PDIRMS) of China CDC and included the date of onset, the date of the first diagnosis, the date of confirmed diagnosis, the results of the first diagnosis and confirmed diagnosis and verification, the facility for case diagnosis and reporting, the geographical distribution and Plasmodium species composition. This study aims to analyze the performance of different health facilities [medical institution, centers for disease control and prevention (CDC), Entry-Exit Inspection and Quarantine (EIQ)] and their malaria diagnostic competency at different levels, the intervals from onset to the first and confirmed diagnosis, as well as the agreement rate of species identification between the confirmed diagnosis and NMDRLN verifications. All extracted data were processed with Microsoft Excel 2007 and SPSS (version 21.0, IBM Corp. USA). Then, the differences from groups were evaluated by Pearson chi-square tests. Statistical significance was set as 0.05.
A total of 5,539 imported malaria cases were reported between 2017 and 2018. They were first diagnosed by clinicians in individual clinics (238, 4.3%), village clinics (242, 4.4%), township health centers (526, 9.5%), county medical institutions (1,451, 26.2%), county CDCs (502, 9.1%), prefectural medical institutions (1,731, 31.3%), prefectural CDCs (49, 0.9%), provincial medical institutions (630, 11.4%), provincial CDCs (11, 0.2%), prefectural EIQs (39, 0.7%), provincial EIQs (28, 0.5%), and unspecified facilities (92, 1.7%). Correspondingly, there were 1 (0.0%), 2 (0.0%), 339 (6.1%), 1,258 (22.7%), 623 (11.2%), 2,219 (40.1%), 94 (1.7%), 867 (15.7%), 41 (0.7%), 37 (0.7%), 26 (0.5%), and 32 (0.6%) cases confirmed in the above health facilities, respectively (Table 1). In addition, the detailed distributions in each province/municipality/autonomous region yearly are shown in Figure 1.
Table 1. Malaria cases diagnosed first and confirmed in various health facilities nationwide according to the Parasitic Diseases Information Reporting Management System of China (2017–2018).
| Item | First diagnosis | Confirmed diagnosis | |||||
| 2017 | 2018 | Total | 2017 | 2018 | Total | ||
| Abbreviations: EIQ=Entry-Exit Inspection and Quarantine, CDC=centers for disease control and prevention. | |||||||
| Individual clinics | 114 | 124 | 238 | 1 | 0 | 1 | |
| Village clinics | 119 | 123 | 242 | 1 | 1 | 2 | |
| Township Health Center | 319 | 207 | 526 | 213 | 126 | 339 | |
| County medical institutions | 745 | 706 | 1,451 | 667 | 591 | 1,258 | |
| County CDCs | 278 | 224 | 502 | 339 | 284 | 623 | |
| Prefectural medical institutions | 863 | 868 | 1,731 | 1,100 | 1,119 | 2,219 | |
| Prefectural CDCs | 35 | 14 | 49 | 58 | 36 | 94 | |
| Provincial medical institutions | 298 | 332 | 630 | 396 | 471 | 867 | |
| Provincial CDCs | 7 | 4 | 11 | 25 | 16 | 41 | |
| Prefectural EIQs | 22 | 17 | 39 | 25 | 12 | 37 | |
| Provincial EIQs | 14 | 14 | 28 | 14 | 12 | 26 | |
| Unspecified | 47 | 45 | 92 | 22 | 10 | 32 | |
| Total | 2,861 | 2,678 | 5,539 | 2,861 | 2,678 | 5,539 | |
Figure 1.
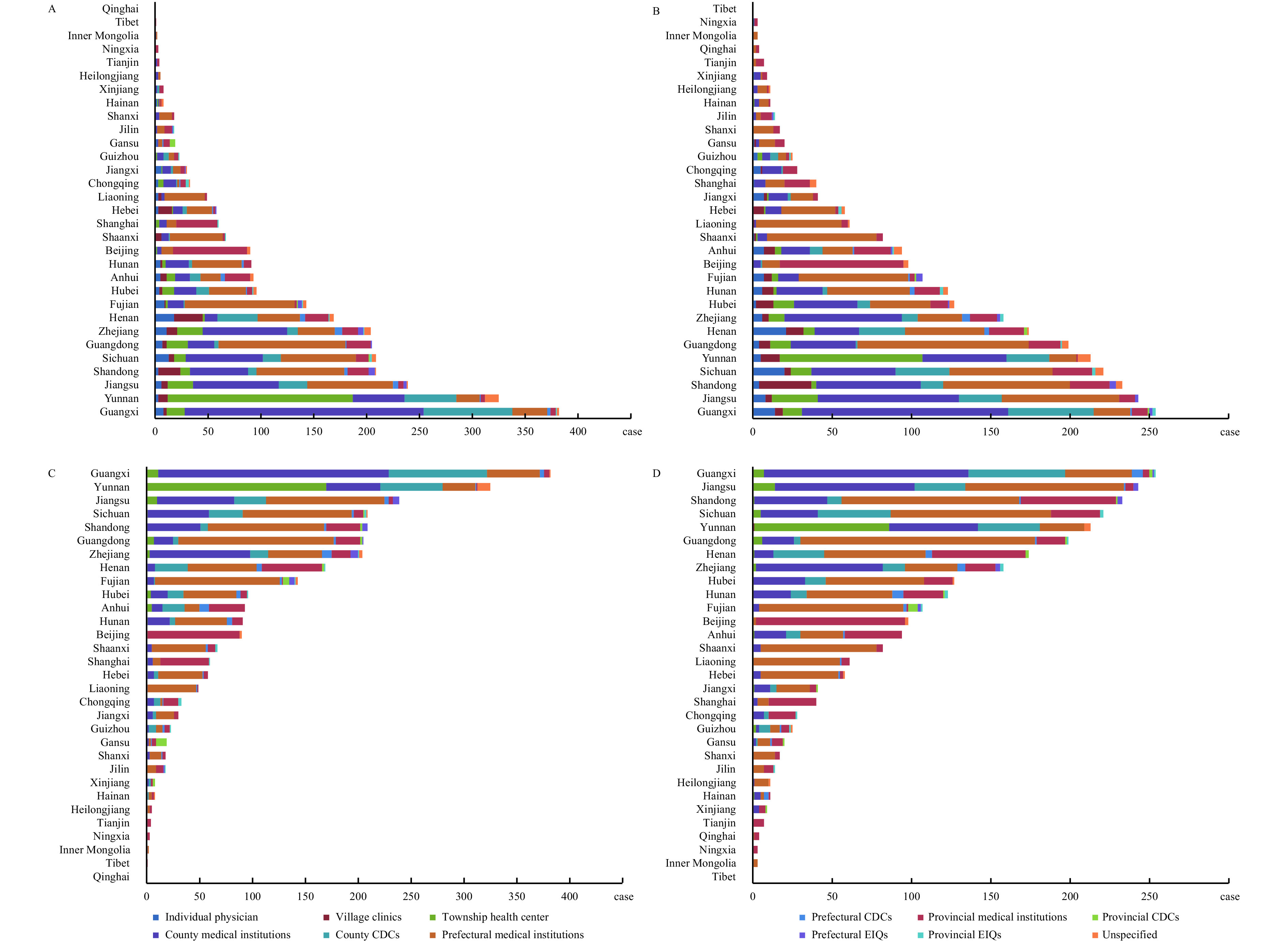
Malaria cases diagnosed first and confirmed in various health facilities in each provincial-level administrative division (PLAD) according to the Parasitic Diseases Information Reporting Management System of China (2017–2018). (A) Malaria cases diagnosed first in 2017; (B) Malaria cases diagnosed first in 2018; (C) Malaria cases confirmed in 2017; (D) Malaria cases confirmed in 2018.
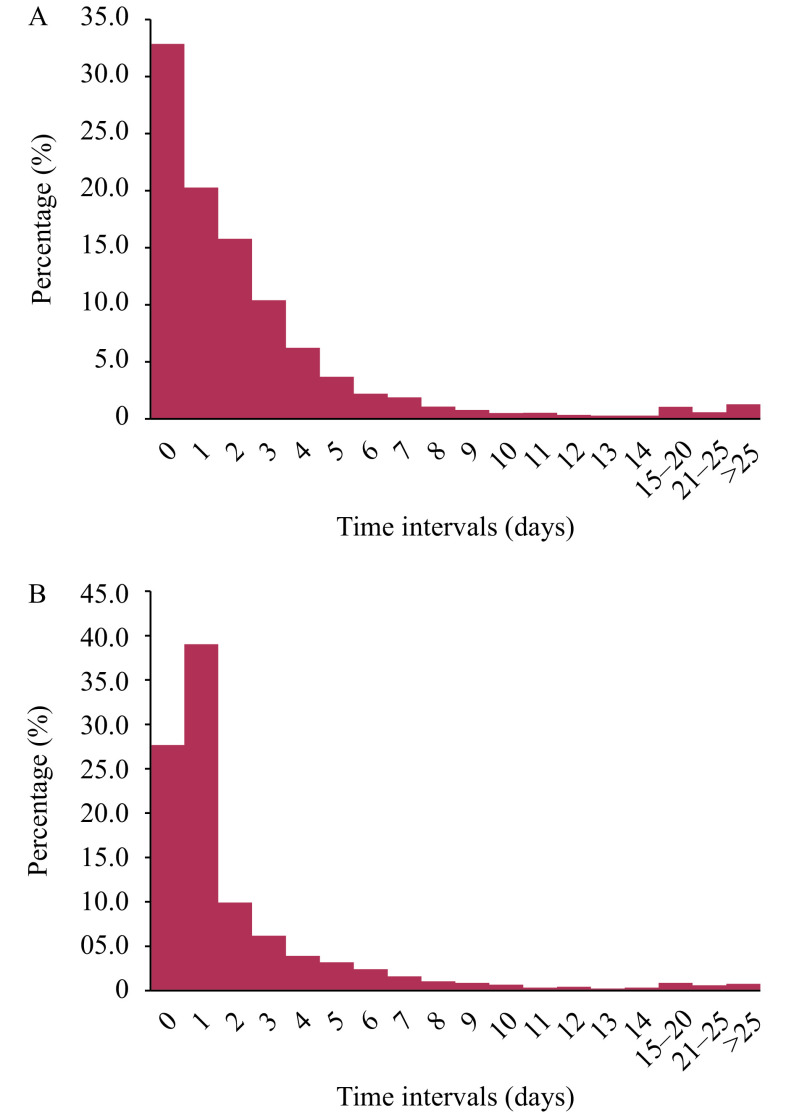
The median interval (the subtraction of the latter date from the former date) from onset to the first diagnosis was 1 day (maximum: 186 days) between 2017 and 2018 nationwide and 1 day (maximum: 112 days) from the first diagnosis to confirmed diagnosis. However, 46.9% (2,596/5,539) of cases were first diagnosed 2 days after onset, and 33.3% (1,844/5,539) of cases were confirmed more than 2 days after the first diagnosis. The median intervals from onset to the first diagnosis in the health facilities at township and below, county, prefectural, provincial and other unspecified levels were 1 day (maximum: 47 days), 1 day (maximum: 90 days), 2 days (maximum: 186 days), 1 day (maximum: 89 days), and 1 day (maximum: 25 days), respectively. The corresponding intervals from the first diagnosis to confirmed diagnosis were 0 days (maximum: 11 days), 1 day (maximum: 65 days), 1 day (maximum: 71 days), 1 day (maximum: 112 days) and 1 day (maximum: 57 days), respectively. The proportion of cases receiving the first diagnosis and confirmed diagnosis at different intervals is shown in Figure 2.
Figure 2.
Time interval from onset to the first diagnosis (A) and then to confirmed diagnosis (B) between 2017 and 2018 according to the Parasitic Diseases Information Reporting Management System of China.
All the reported cases (except 9 cases in 2017 and 5 cases in 2018 which were initially clinically diagnosed) were verified by the provincial labs, but only 76.1% (2,169/2,852) in 2017 and 73.7% (1,971/2,673) in 2018 were diagnosed as malaria on the first visit. In addition, 89.4% (4,942/5,525) of the verified cases were consistent with their original confirmation results. Agreements of 95.9% (328/342), 91.0% (1,711/1,881), 88.9% (2,088/2,350), 85.3% (797/934), and 87.5% (28/32) were found (χ2=37.3, p<0.001) in health facilities at township and below, county, prefectural, provincial, and other unspecified levels, respectively. In addition, 5.0% (180/3,587) ofP. falciparum, 7.2% (70/970) of P. vivax, 24.7% (37/150) of P. malariae, 31.9% (232/728) of P. ovale, 75.3% (67/89) of the mixed and 100% (1/1) of P. knowlesi infections were inconsistent with their originally confirmed diagnosis (χ2=908.0, p<0.001).
DISCUSSION
The accomplishment of zero indigenous malaria cases since 2017 in China is still facing challenges from reintroduction by imported cases mainly from Africa and Southeast Asia (1-2). This is even more challenging for formerly malaria-endemic areas where mosquitoes are still receptive for transmission. Several cases of malaria reintroduction have occurred in different countries (7).
To prevent reintroduction, current malaria surveillance and vigilance systems should be improved (8) starting from malaria awareness among the public, especially in travelers to or from malaria transmission areas. Public awareness of malaria in the beginning and middle stages of the national malaria elimination program in China did not meet the goal of malaria elimination (9-10). This study found that a considerable number of patients sought health care and were diagnosed 2 days after illness onset. Delayed detection by the health system will greatly increase the risk of transmission and poor prognosis of the patient. As health education and promotion have an important contribution to malaria control, prevention, and elimination, different targeted malaria awareness campaigns should be tailored to improve people’s knowledge regarding malaria and improve the timeliness of their doctor visits.
In addition, it becomes even more crucial to ensure the provision of continuous, quality early diagnosis and treatment to save lives and prevent reintroduction in the malaria post-elimination phase. However, only approximately three-quarters of cases could be diagnosed as malaria on their first visits, and the capacity of malaria diagnosis was not sufficient at below provincial levels where the number of patients is most concentrated, specifically the species identification of P. ovale, P. malariae, and mixed infections (6). As a result, the global malaria epidemiological status, careful questioning of patient travel history, and skills in malaria diagnosis and treatment should also be taught to target health professionals periodically to improve their watchfulness and capacity for any malaria cases.
In conclusion, a systematic review of malaria cases was conducted that showed good performance in the diagnosis of P. falciparum malaria and P. vivax malaria cases, which were the highest number of cases between 2017 and 2018 in China. Furthermore, the findings indicate that it is necessary to increase the public awareness of potential risk of malaria, help health professionals improve watchfulness for any malaria cases, intensify the establishment and operation of NMDRLN, hold more training courses on malaria diagnostic techniques for medical institutions, and to prevent malaria reintroduction in the elimination and post-elimination phases.
Conflict of interest:No conflicts of interest were reported.
Acknowledgement
We thank the staff of Centers for Disease Control and Prevention and Institutes of Parasitic Diseases and clinics at different levels in China for assistance. We also thank Prof. Xiaonong Zhou, Ning Xiao and Qin Chen for their kind help on improving the manuscript.
Funding Statement
This study was supported by the National Science and Technology Major Program of China (No. 2018ZX10101002–002).
References
- 1.Zhang L, Feng J, Zhang SS, Xia ZG, Zhou SS. The progress of national malaria elimination and epidemiological characteristics of malaria in China in 2017. Chin J Parasitol Parasit Dis 2018;36(3):201-9. http://www.jsczz.cn/CN/abstract/abstract6977.shtml. (In Chinese).
- 2.Zhang L, Feng J, Zhang SS, Xia ZG, Zhou SS Epidemiological characteristics of malaria and the progress towards its elimination in China in 2018. Chin J Parasitol Parasit Dis. 2019;37(3):241–7. doi: 10.12140/j.issn.1000-7423.2019.03.001. [DOI] [Google Scholar]
- 3.World Health Organization. A framework for malaria elimination. Geneva: World Health Organization; 2017. https://www.who.int/malaria/publications/atoz/9789241511988/en/.
- 4.World Health Organization. Universal access to malaria diagnostic testing: an operational manual. Geneva: World Health Organization; 2011. https://www.who.int/malaria/publications/atoz/9789241502092/en/.
- 5.Yin JH, Yan H, Huang F, Li M, Xiao HH, Zhou SS, et al Establishing a China malaria diagnosis reference laboratory network for malaria elimination. Malar J. 2015;14:40. doi: 10.1186/s12936-015-0556-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin JH, Yan H, Li M, Ruan Y, Zhang XQ, Wang LY, et al Competency and challenges in malaria microscopy in China. BioSci Trends. 2017;11(6):702–5. doi: 10.5582/bst.2017.01275. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization, Regional Office for the Eastern Mediterranean. Guidelines on prevention of the reintroduction of malaria. Cairo: World Health Organization, Regional Office for the Eastern Mediterranean; 2007. https://apps.who.int/iris/handle/10665/119851.
- 8.Mendis K Eliminating malaria should not be the end of vigilance. Nature. 2019;573(7772):7. doi: 10.1038/d41586-019-02598-1. [DOI] [PubMed] [Google Scholar]
- 9.Yin JH, Xia ZG, Wang RB, Zhang QF, Fang W, Zhou SS Public awareness of malaria at the beginning of a national malaria elimination program in China. J Infect Dev Ctries. 2015;9(4):416–20. doi: 10.3855/jidc.5307. [DOI] [PubMed] [Google Scholar]
- 10.Tang SF, Ji L, Hu T, Wang RX, Fu H, Shao T, et al Public awareness of malaria in the middle stage of national malaria elimination programme. A cross-sectional survey in rural areas of malaria-endemic counties, China. Malar J. 2016;15(1):373. doi: 10.1186/s12936-016-1428-x. [DOI] [PMC free article] [PubMed] [Google Scholar]