Abstract
Background
Gender-based discrimination remains a substantial barrier to health care access and HIV prevention among transgender women in Brazil. The aim of this study was to investigate the association between gender-based discrimination and medical visits, as well as with HIV testing among transgender women in the last 12 months in northeast Brazil.
Methods
This is a cross-sectional study of 864 transgender women recruited using Respondent-Driven Sampling in three cities in northeastern Brazil in 2016. A socio-behavioral questionnaire was applied. Multivariate analyses were performed using logistic regression, with odds ratio and respective 95% confidence intervals estimation, to estimate the effect of gender-based discrimination on two outcomes: i) medical visits and ii) HIV testing in the last 12 months.
Results
547 transgender women (67·0%) had medical visits, and 385 (45·8%) underwent HIV testing in the last 12 months. In the multivariate analysis, gender-based discrimination was associated with a reduced likelihood of medical visits (OR: 0·29; 95%CI: 0·14–0·63) and HIV testing (OR: 0·41; 95%CI: 0·22–0·78) in the last 12 months.
Conclusion
Gender-based discrimination played an essential role in reducing the access of TGW to medical visits and HIV testing services. Furthermore, by confirming the association between gender-based discrimination and medical visits and HIV testing in the multivariate analysis, we have demonstrated how this predictive variable can affect by reducing access to health services. The findings point to the need for non-discriminatory policies based on the defense and promotion of human rights that may foster the access of transgender women to Brazilian health services.
Keywords: Transgender Women, Discrimination, Stigma, Use of health services, HIV testing
Background
Transgender women (TGW) are still disproportionately affected by the HIV epidemic, despite the global decrease in incidence over the years [1]. The worldwide estimate of HIV prevalence in this population is 19.1%, however, in Brazil, this prevalence is 33.1%, with an 84.3 times higher probability of infection than the general population of reproductive age [2].
UNAIDS 90–90-90 target establishes that, by the end of 2020, at least 90% of people living with HIV should know their status, 90% of those diagnosed should start antiretroviral treatment, and 90% of those being treated should achieve viral suppression. One of the best ways to ensure people living with HIV should know their status, start antiretroviral treatment, and being treated should achieve viral suppression, is the implementation of strategies to assure competent health services to approach and care key populations [3, 4].
The health care model geared to people at risk of HIV, suggested by the World Health Organization (WHO), basically consists of a network of services: prevention technologies (condoms, lubricants, and pre- and post-exposure prophylaxis), regular testing services (testing with a health professional or offering an HIV self-test), continued care with a health professional, and treatment. The focus is to create the individual’s bond with the health service, monitor, promote health education, and treat HIV and other sexually transmitted infections (STI) [5]. However, these services are not always available or accessible to everyone. For example, TGW have limited access to health services, which include a lower frequency of HIV testing, HIV prevention, and health care in general [6].
Studies show that gender identity discrimination operates as one of the main barriers to accessing health services, including HIV/AIDS services [7–9]. In Brazil, although the National Health Policy for Lesbian, Gay, Bisexual, and Transgender people (NHPLGBT) have ensured the inclusion and non-discrimination of this population in health services, there is still evidence of a violation of TGW’s rights: failure to respect the social name, discrimination in health services, and failure to meet the necessary health need [8, 10, 11]. Thus, gender-based discrimination (GBD) remains one of the main obstacles faced by TGW in accessing health services [12], which can hinder HIV prevention and care and increase the risk to HIV/AIDS [13, 14]. In Brazil, no other studies investigated the association between GBD, HIV testing, and access to medical visits among TGW.
This study aims to investigate the putative association between gender-based discrimination (GBD) and (i) medical visits in the last 12 months and (ii) HIV testing in the last 12 months, among TGW from three large capital cities in Northeast Brazil.
Methods
This study reports findings from a cross-sectional Biological and Behavioral Surveillance Survey among TGW, conducted in three large capitals of northeastern Brazil. These sites were part of the multicity DIVAS study (National Research Study on Behaviors, Attitudes, Practices, as well as assessment of the Prevalence of HIV, Syphilis and Hepatitis B and C among Travestis and Transsexual Women). The DIVAS study was conducted in 12 cities in Brazil from October 2016 to July 2017, aimed to estimate the prevalence of HIV, and other sexually transmitted infections (STI) and monitor risk practices for these infections [15]. DIVAS is one of the largest studies among TGW in a given nation, worldwide.
The study protocol was submitted for review and approved by the Sergio Arouca National School of Public Health (ENSP/FIOCRUZ) Research Ethics Board (CAAE-49359415.9.0000.5240). Written informed consent was asked and obtained from all participants, who could withdraw consent at any stage of the process or skip any questions perceived as too sensitive, too personal, or distressing.
Study population
TGW (864) were selected from the cities of Salvador (166), Recife (350) and Fortaleza (348) in 2017. They were recruited using respondent-driven sampling (RDS) as a sampling method aiming to obtain a more robust and diverse sample. They were eligible for the study if they self-identified themselves as transgender women, women, or other category different from the male sex designated on their birth certificate; reported spending most of their time at the selected city (living, studying, and/or working there). Each study participant was screened for eligibility prior to enrollment. The inclusion criteria for the current analysis were those as follows: to answer the questionnaire (with the option to skip some questions), to perform STI rapid tests (with the right to opt out), to will to recruit peers for the study, to sign the informed consent form, and to have had at least one sexual intercourse in the past 12 months. The exclusion criteria were: being under 18 years of age and to be under the influence of alcohol or other drugs in the moment of the interview.
Data collection and sampling
As required by the RDS method, 5 and 10 initial participants in each city − called seeds − were chosen purposively, following formative qualitative research only as an initial stage for recruitment. The formative phase of the study comprised group discussions with local TGW leaders, non-governmental organizations (NGO), potential participants, and researchers. Each seed received three coupons to distribute to other TGW from her social networks. The interviewees recruited by the seeds were defined as the first wave of the study. After participating in the interview, each participant received three additional coupons to distribute to their peers. This process was repeated until the a priori defined sample size was achieved in each site.
RDS requires a system of primary and secondary incentives. The primary incentive was US$10.00 to pay for a light meal and transportation. The secondary incentive was a payment of US$10.00 for each recruited person who participated in the study [16].
Data were collected through interviews with a standardized and previously tested questionnaire, triangulating findings from focus groups and a pilot study. Face-to-face interviews were carried out by thoroughly trained interviewers, in a private space, reserved for this sole purpose.
Study variables
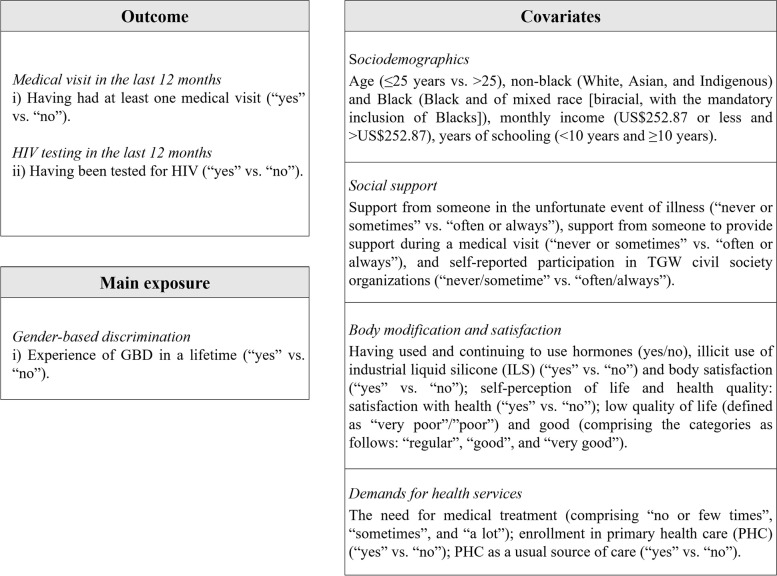
The variables presented in this study are available in Fig. 1.
Fig. 1.
Variables of the study
Data analysis
Data analysis took into consideration the complex sampling design of recruitment by RDS [17]. Each one of the three cities was defined as a stratum. In each stratum, the weighting was inversely proportional to the size of each participant's network, totaling the stratum size (RDS-II estimator) [18]. The questions in the questionnaire that measured the network size of each TGW were "How many TGW do you know, by name/nickname and who also know you by your name/ nickname, who live, work or study in your city?” Out of those you mentioned, how many have you met or spoken to personally, by phone or Facebook/WhatsApp within the last 30 days?" The analysis was conducted using the library for complex samples of STATA software version 15 (StataCorp, 2015).
We fitted independent logistic regression models yielding odds ratios (OR) adjusted for potential confounding factors, as well as their respective 95% CI. The variables with a p-value < 0.05 or defined as relevant by their magnitude in the bivariate analysis were included in the adjustments of the final multivariate models.
The bivariate and multivariate equations are presented below. In Eq. 1.0, P is the estimated probability of event occurrence P(Y = 1), represented by the odds of having had medical visits or an HIV test, when the independent variable is , GBD or any other covariate. In Eq. 1.1, P represents the odds of having had medical visits or an HIV test P(Y = 1), when the independent variable is a GBD, adjusted by the addition of x_t covariates in the model.
| 1.0 |
| 1.1 |
Percent change in effect of unadjusted and adjusted OR was used to evaluate confounding [19]. The adequacy of the final models was analyzed using the Hosmer–Lemeshow goodness-of-fit test [20].
Results
Table 1 presents the results describing each one variable analyzed in this study. Out of the total 864 TGW, 772 (87.3%) reported experience of GBD in their lifetime. 547 (67.0%) reported medical visits and 385 (45.8%) HIV testing, both in the past 12 months. Most interviewees were aged > 25 years (50.5%), self-reported black skin color (79.4%), a monthly income > US$252.87 (65.5%), and ≥ 10 years of schooling (54.5%). Most reported that they often or always have the support of someone in case of an illness (65.2%) and for accompany medical visits (57.9%), but few self-reported engagements in TGW civil society organizations (22.9%).
Table 1.
Distribution of study variables among transgender women in Northeast Brazil, 2017
| Variables | na | %a |
|---|---|---|
| Outcome | ||
| Medical visits in the last 12 months | ||
| No | 271 | 33.0 |
| Yes | 547 | 67.0 |
| HIV testing in the last12 months | ||
| No | 458 | 54.2 |
| Yes | 385 | 45.8 |
| Main exposure | ||
| GBD | ||
| No | 92 | 12.7 |
| Yes | 772 | 87.3 |
| Covariates | ||
| Age | ||
| 18 to 25 | 439 | 49.5 |
| 26 and older | 425 | 50.5 |
| Skin color | ||
| Non-black | 171 | 20.6 |
| Black | 681 | 79.4 |
| Monthly income | ||
| US$252.87 or less | 293 | 34.5 |
| > US$252.87 | 571 | 65.5 |
| Years of schooling | ||
| Up to 9 years | 378 | 45.5 |
| 10 or more years | 473 | 54.5 |
| Support in case of illness | ||
| Never or sometimes | 303 | 34.3 |
| Often or always | 553 | 65.2 |
| Support to accompany in the medical visits | ||
| Never or sometimes | 358 | 42.1 |
| Often or always | 502 | 57.9 |
| Participation in TGW civil society organizations | ||
| No | 638 | 77.1 |
| Yes | 233 | 22.9 |
| Hormone use | ||
| No | 417 | 47.5 |
| Yes | 440 | 52.5 |
| Illicit use of industrial liquid silicone | ||
| No | 633 | 87.1 |
| Yes | 228 | 12.9 |
| Body satisfaction | ||
| Dissatisfied | 396 | 45.6 |
| Satisfied | 462 | 54.4 |
| Health satisfaction | ||
| Dissatisfied | 273 | 29.7 |
| Satisfied | 587 | 70.3 |
| Self-reported quality of life | ||
| Poor | 62 | 7.7 |
| Good | 796 | 92.3 |
| Need for medical treatment | ||
| No need or very little need | 623 | 71.2 |
| Moderately or very much | 230 | 28.9 |
| Enrollment in PHC | ||
| No | 254 | 31.5 |
| Yes | 600 | 68.5 |
| PHC as a usual source of care | ||
| No | 559 | 67.0 |
| Yes | 304 | 33.0 |
GBD gender-based discrimination, TGW transgender women, PHC primary health care
a Weighted by RDS-II estimator
Following the results in Table 1, slightly more than half (52.5%) reported having used and continue to use hormones, and 12.9% reported illicit use of ILS. Most reported being satisfied or very satisfied with their bodies (54.4%), albeit in a smaller proportion than that observed for self-reported satisfaction with their health (70.3%) and self-perception of life quality (92.3%). Most reported enrollment in primary health care facilities (68.5%). However, only one third had primary health care as the usual source of care (33.0%). In addition, most reported no need or little need of a medical treatment (71.2%).
We summarize the results from the bivariate logistic regression analysis (Eq. 1.0) in Tables 2 and 3. At a significance level of 0.05, the independent variables that were significantly associated with medical visits in the last 12 months presented in Table 2 were: GBD (OR 0.37; 95% CI 0.19–0.35); age 26 years and older (OR 1.54; 95% CI 1.03–2.30); monthly income greater than US$252.87 (OR 1.69; 95% CI 1.11–2.56); 10 years or more of schooling (OR 1.54; 95% CI % 1.02–2.32); moderately or very pronounced need of medical treatment (OR 1.99; 95% CI 1.24–3.18); and enrollment in PHC (OR 2.00; 95% CI 1.29- 3.10). In Table 3, for a significance level of 0.05 the independent variables that had a significant association with HIV testing in the last 12 months were the ones as follows: GBD (OR 0.47; 95% CI 0.24–0.91); age 26 years and older (OR 1.76; 95% CI % 1.19–2.60); 10 years or more of schooling (OR 1.64; 95% CI 1.10–2.44); moderately or very pronounced need of medical treatment (OR 2.03; 95% CI 1.32–3.13); illicit use of industrial liquid silicone (OR 1.68; 95% CI 1.08–2.63). and participating in TGW civil society organizations (OR 1.80; 95% CI 1.17–2.77).
Table 2.
Bivariate analysis of factors associated with medical visits in the last 12 months among TGW in Northeast Brazil, 2017
| Variables | Medical visit in the last 12 monthsa | ||||
|---|---|---|---|---|---|
| No (%) | Yes (%) | p-value | OR | 95%CI | |
| Main exposure | |||||
| GBD | 0.005 | ||||
| No | 16.95 | 83.05 | 1.00 | - | |
| Yes | 35.33 | 64.67 | 0.37 | 0.19–0.75 | |
| Covariates | |||||
| Age | 0.036 | ||||
| Up to 25 years | 37.89 | 62.11 | 1.00 | - | |
| 26 years and over | 28.42 | 71.58 | 1.54 | 1.03–2.30 | |
| Skin color | 0.939 | ||||
| Non-black | 33.55 | 66.45 | 1.00 | - | |
| Black | 33.10 | 66.90 | 1.02 | 0.60–1.73 | |
| Monthly income | 0.014 | ||||
| US$252.87 or less | 40.56 | 59.44 | 1.00 | - | |
| > US$252.87 | 28.80 | 71.20 | 1.69 | 1.11–2.56 | |
| Years of schooling | 0.039 | ||||
| Up to 9 years of study | 37.94 | 62.06 | 1.00 | - | |
| 10 years and over | 28.44 | 71.56 | 1.54 | 1.02–2.32 | |
| Support in case of illness | 0.354 | ||||
| Never or sometimes | 36.24 | 63.76 | 1.00 | - | |
| Often or always | 31.86 | 68.14 | 1.22 | 0.80–1.84 | |
| Support to accompany in the medical visits | 0.682 | ||||
| Never or sometimes | 34.22 | 65.78 | 1.00 | - | |
| Often or always | 32.31 | 67.69 | 1.09 | 0.72–1.64 | |
| Health satisfaction | 0.044 | ||||
| Dissatisfied | 26.29 | 73.71 | 1.00 | - | |
| Satisfied | 36.07 | 63.93 | 0.63 | 0.40–0.99 | |
| Need for medical treatment | 0.004 | ||||
| No need or very little need | 37.36 | 62.64 | 1.00 | - | |
| Moderately or very much | 23.08 | 76.92 | 1.99 | 1.24–3.18 | |
| Self-reported quality of life | 0.191 | ||||
| Poor | 24.24 | 75.76 | 1.00 | - | |
| Good | 34.14 | 75.76 | 0.62 | 0.30–1.28 | |
| Hormone use | 0.648 | ||||
| No | 34.12 | 65.88 | 1.00 | - | |
| Yes | 32.03 | 67.97 | 1.10 | 0.73–1.65 | |
| Illicit use of industrial liquid silicone | 0.178 | ||||
| No | 34.82 | 65.18 | 1.00 | - | |
| Yes | 27.99 | 72.01 | 1.37 | 0.86–2.19 | |
| Enrollment in PHC | 0.002 | ||||
| No | 43.23 | 56.77 | 1.00 | - | |
| Yes | 27.60 | 72.40 | 2.00 | 1.29–3.10 | |
| PHC as a usual source of care | 0.173 | ||||
| No | 34.99 | 65.01 | 1.00 | - | |
| Yes | 28.62 | 71.38 | 1.34 | 0.88–2.52 | |
| Participation in TGW civil society organizations | 0.119 | ||||
| No | 34.95 | 65.05 | 1.00 | - | |
| Yes | 26.98 | 73.02 | 1.45 | 0.91–2.33 | |
GBD gender-based discrimination, TGW transgender women, PHC primary health care
a Weighted by RDS-II estimator
Table 3.
Bivariate analysis of factors associated with HIV testing in the last 12 months among TGW in Northeast Brazil, 2017
| Variables | HIV testing in the last 12 months a | ||||
|---|---|---|---|---|---|
| No (%) | Yes (%) | p-value | OR | 95%CI | |
| Main exposure | |||||
| GBD | 0.023 | ||||
| No | 37.91 | 62.09 | 1.00 | - | |
| Yes | 56.52 | 43.48 | 0.47 | 0.24–0.91 | |
| Covariates | |||||
| Age | 0.004 | ||||
| Up to 25 years | 61.17 | 38.83 | 1.00 | - | |
| 26 years and over | 47.23 | 52.77 | 1.76 | 1.19–2.60 | |
| Skin color | 0.623 | ||||
| Non-black | 56.61 | 43.39 | 1.00 | - | |
| Black | 53.57 | 46.43 | 1.13 | 0.69–1.85 | |
| Monthly income | 0.385 | ||||
| US$252.87 or less | 57.13 | 42.87 | 1.00 | - | |
| > US$252.87 | 52.62 | 47.38 | 1.20 | 0.79–1.81 | |
| Years of schooling | 0.015 | ||||
| Up to 9 years of study | 61.11 | 38.89 | 1.00 | - | |
| 10 years and over | 48.95 | 51.05 | 1.64 | 1.10–2.44 | |
| Support in case of illness | 0.692 | ||||
| Never or sometimes | 55.39 | 44.61 | 1.00 | - | |
| Often or always | 53.35 | 46.65 | 1.09 | 0.72–1.63 | |
| Support to accompany in the medical visits | 0.876 | ||||
| Never or sometimes | 53.43 | 46.57 | 1.00 | - | |
| Often or always | 54.22 | 45.78 | 0.97 | 0.65–1.44 | |
| Health satisfaction | 0.348 | ||||
| Dissatisfied | 50.49 | 49.51 | 1.00 | - | |
| Satisfied | 55.53 | 44.47 | 0.82 | 0.53–1.25 | |
| Need for medical treatment | 0.001 | ||||
| No need or very little need | 59.36 | 40.64 | 1.00 | - | |
| Moderately or very much | 41.83 | 58.17 | 2.03 | 1.32–3.13 | |
| Self-reported quality of life | 0.383 | ||||
| Poor | 47.83 | 52.17 | 1.00 | - | |
| Good | 55.13 | 44.87 | 0.75 | 0.38–1.45 | |
| Hormone use | 0.898 | ||||
| No | 54.41 | 45.59 | 1.00 | - | |
| Yes | 53.77 | 46.23 | 1.02 | 0.69–1.52 | |
| Illicit use of industrial liquid silicone | 0.021 | ||||
| No | 57.26 | 42.74 | 1.00 | - | |
| Yes | 44.31 | 55.69 | 1.68 | 1.08–2.63 | |
| Enrollment in PHC | 0.204 | ||||
| No | 58.23 | 41.77 | 1.00 | - | |
| Yes | 51.36 | 48.64 | 1.32 | 0.86–2.03 | |
| PHC as a usual source of care | 0.468 | ||||
| No | 52.82 | 47.18 | 1.00 | - | |
| Yes | 56.53 | 43.47 | 0.86 | 0.57–1.29 | |
| Participation in TGW civil society organizations | 0.007 | ||||
| No | 57.46 | 42.54 | 1.00 | - | |
| Yes | 42.88 | 57.12 | 1.80 | 1.17–2.77 | |
GBD gender-based discrimination, TGW transgender women, PHC primary health care
a Weighted by RDS-II estimator
The multivariate analyses (Eq. 1.1) have found statistically significant association (p < 0.05) between GBD and the two study outcomes, as shown in Tables 4 and 5. TGW who reported experience of GBD had 71% less likely to attend a medical visit (OR 0.29; 95% CI 0.14–0.63) and 59% less likely to have had an HIV test in the last 12 months when compared to TGW who did not experienced GBD (OR 0.41; 95% CI 0.22–0.78), after adjusting for potential confounders.
Table 4.
Multivariate analysis of the association between GBD and medical visit in the last 12 months among TGW in Northeast Brazil, 2017
| Model 1 | OR a | p-value | 95%CI | |
| GBD | 0.37 | 0.006 | 0.19–0.75 | |
| Model 2 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.33 | 0.005 | 0.15–0.71 | 11.97 |
| Adjusted for age, monthly income, years of schooling, need for medical treatment, self-reported quality of life, health satisfaction, illicit use of industrial liquid silicone, enrollment in PHC, PHC as a usual source of care, participation in TGW civil society organizations | ||||
| Model 3 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.30 | 0.003 | 0.14–0.66 | 18.61 |
| Adjusted for age, schooling, need for medical treatment, self-reported quality of life, health satisfaction, illicit use of industrial liquid silicone, enrollment in PHC, PHC as a usual source of care, participation in TGW civil society organizations | ||||
| Model 4 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.30 | 0.002 | 0.14–0.65 | 19.12 |
| Adjusted for age, schooling, self-reported quality of life, health satisfaction, illicit use of industrial liquid silicone, enrollment in PHC, PHC as a usual source of care, participation in TGW civil society organizations | ||||
| Model 5 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.30 | 0.002 | 0.14–0.65 | 19.33 |
| Adjusted for age, self-reported quality of life, health satisfaction, illicit use of industrial liquid silicone, enrollment in PHC, PHC as a usual source of care, participation in TGW civil society organizations | ||||
| Model 6 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.29 | 0.002 | 0.14–0.63 | 21.42 |
| Adjusted for self-reported quality of life, health satisfaction, illicit use of industrial liquid silicone, enrollment in PHC, PHC as a usual source of care, participation in TGW civil society organizations | ||||
| Hosmer–Lemeshow (p-value) | 0.979 | |||
GBD gender-based discrimination, TGW transgender women, PHC primary health care
a Weighted by RDS-II estimator
Table 5.
Multivariate adjustment of the association between GBD and HIV testing in the last 12 months among TGW in Northeast Brazil, 2017
| Model 1 | OR a | p-value | 95%CI | |
| GBD | 0.47 | 0.030 | 0.24–0.91 | |
| Model 2 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.43 | 0.009 | 0.22–0.80 | 9.47 |
| Adjusted for age, years of schooling, need for medical treatment, illicit use of industrial liquid silicone, participation in TGW civil society organizations | ||||
| Model 3 | OR a | p-value | 95%CI | Percent change in effect |
| GBD | 0.41 | 0.007 | 0.22–0.78 | 12.13 |
| Adjusted for schooling, need for medical treatment, illicit use of industrial liquid silicone, participation in TGW civil society organizations | ||||
| Hosmer–Lemeshow (p-value) | 0.995 | |||
GBD gender-based discrimination; TGW, transgender women; PHC, primary health care
a weighted by RDS-II estimator
Discussion
The estimated frequency of medical visits in the last year among TGW was relatively low (67.0%) compared to other studies conducted in the United States (US) of America, a country without a national health system, but rather a patchwork of private and public initiatives, the latter always focused on some populations and delivered on a given catchment area [21, 22]. In San Francisco, an RDS survey of TGW found a 78.0% prevalence of medical visits in the last six months [21]. Data from the US Centers for Disease Control and Prevention (CDC) from 2014 to 2016 indicated a 70.3% prevalence of PHC visits in the last year among TGW [22].
To the best of our knowledge, no studies in Brazil have estimated the prevalence of medical visits in the last year for the TGW population. In general, the production of data on the access of this population to health services comes from qualitative studies [23]. Thus, we still do not have parameters for epidemiological studies that assess such characteristics in Brazil, as there is no question about gender identity in previous studies to make this comparison.
However, the 2013 Brazilian National Health Survey (PNS) investigated this indicator of access to health for the overall adult population [24, 25], and the estimated prevalence was 71.2% for Brazil. These figures were a bit lower for northeastern Brazil (66.3%). This rate is close to the one found in this study for TGW. [25].
Although Brazil has a universal health system (in Portuguese Sistema Único de Saúde- SUS), the services made available by the Unified Health System (SUS) are not always adequate for serving the TGW population. There is still no effective strategy to link these persons to the health system and there are still many discrimination-based barriers to access: discrimination by health professionals and service users, disrespect for the social name and gender identity and failure to meet the necessary health demands. Such barriers can hinder to carry out the medical visit, as well the avoidance of the seeking for health services [10, 26, 27].
Also, medical visits should be a key opportunity to assess TGW’s specific needs. Considering the evidence from epidemiological studies, documenting that TGW face high vulnerability and risk factors for HIV/AIDS [7, 28], the visit should be an ideal moment for the offering and undertaking HIV testing and counseling. The Brazilian Ministry of Health determines a six-monthly HIV testing frequency [29], especially for populations most vulnerable to infection. Thus, the health system should offer and allow effective access to HIV prevention and care technologies.
The estimated prevalence of HIV testing in the last year in this study (45.8%) was less than that found for TGW in Ho Chi Minh, Vietnam (59.3%) in the last year [29], and Cambodia (49.2%) [30] and Pattaya, Thailand (54.7%) [31], in the last 6 months. As in Brazil, both Vietnam, Cambodia and Thailand [4] offer public services for regular HIV testing. Possibly, health services in these countries have more inclusive strategies for these populations compared to the Brazilian situation.
In a review study of 17 countries in Latin America, Silva-Santisteban et al. [32] showed that despite having implemented early HIV prevention and treatment strategies, Brazil was among the countries with the lowest access to testing in the last year for TGW and men who have sex with men (20.3%). Latin American countries with the highest level of access to HIV testing in the past year were Honduras (73.7%), Costa Rica (73.3%), Argentina (58.7%), and Paraguay (56.6%).
Attending medical visits and undergoing HIV tests in the last year indicates access to health services and HIV prevention [33]. However, this study revealed that although more than half of the interviewed TGW reported a medical visit in the last year, less than half underwent HIV testing in the same period. This substantial difference may be explained by some factors. At least, it´s possible to advance plausible hypotheses.
First, not all health services in Brazil that include medical assistance are always suitable for HIV testing. Some problems remain: the unpreparedness of services and health professionals; lack of organization and proper functioning of services, not capable to offer full access to these populations; the current implementation of decentralization strategies for PHC actions has not been effectively implemented; and finally, there is still a lack of communication between the services of PHC and specialized care. [34, 35]. That is, users will not necessarily have access to HIV testing through medical visits. A second issue is HIV/AIDS stigma. The fear of knowing the test result and the negative beliefs often associated with people living with HIV can hinder seeking the test [36].
Specifically, among TGW, besides HIV-related discrimination, GBD can also emerge as an important hurdle. Our study found that GBD was responsible for reducing 71% of medical visits and 59% of HIV testing in the last year, regardless of the other social markers studied in this population. Several other studies have shown that discrimination can be an important barrier to access health services [8, 9, 26, 37–44] and HIV testing [14, 28, 45–55].
In a systematic review study about the barriers faced by TGW in health services, Nascimento, Sousa, and Barros [12] showed that stigma and discrimination are still relevant as one of the main barriers faced by these populations. Found in several social contexts, including health services, GBD prevents them from obtaining adequate care [53, 54].
Concomitantly, by affecting access to health services, discrimination also affects access to HIV testing services. In a study with a RDS of TGW from Fortaleza, Brazil, Pinheiro Júnior et al. [14] revealed that being discriminated against increases almost fourfold the resistance to HIV testing in a lifetime. Logie et al. [16] showed that the probability of having an HIV test in a lifetime decreases with increased HIV-related stigma and that, possibly, stigma is also found in testing services.
A systematic review study on the stigma endured by TGW, Magno et al. [7] showed that stigmatization is an important element that makes this population vulnerable to HIV/AIDS, mainly through social exclusion and violence. These authors also argued that discrimination develops as a factor that hinders access to health services, causing barriers to access tests and other services and making TGW vulnerable to HIV/AIDS.
Profound changes are still required to denaturalize and disassemble GDB in society and the health system. Rocon et al. [27] argue that it is necessary to reassess the production of care by health professionals and the inclusion of the transgender population in a participatory way. Public health policies should sufficiently structure the entire service network to offer equitable access and foster effective social control [55].
This study has some limitations. Due to the difficulty of defining the sample size of an RDS study by the classic method at the time of conducting this research, we used samples of size defined a priori by the Brazilian Ministry of Health. The RDS method design prevents the generalization of our data. A selection bias may have occurred as it represents a non-probabilistic sample, and recruits invited their peers [16]. However, it does not prevent us from providing important information about the social network established. Several other studies have used this same sampling method to study TGW [14, 56–59].
Another limitation of this study is the questionnaire. It was not particularly suitable for analyzing the outcomes since it was originally designed for a comprehensive assessment, not necessarily focusing on our specific questions. For this reason, we were unable to evaluate the putative role of other confounding variables. The self-perceived discrimination variable may not capture internalized or imperceptible experiences and may underestimate our results [60]. Notwithstanding this, it also did not stop revealing statistically significant data since the sampling power was adequate in this case.
Conclusion
The study showed that the prevalence of medical visits in the last 12 months did not match the expected number and respective proportions of HIV testing in the last 12 months among TGW, which points to the loss of HIV testing opportunities since this is a population in a context of high vulnerability and risk of HIV infection. We recommend that medical visits in Brazil carry out at least the investigation of previous HIV testing and, based on anamnesis data, indicate at least one test per year, as it is already done in other countries.
Also, we observed that GBD were reported in most of the TGW, and reduced the likelihood of medical visits and HIV testing in the last 12 months. This data reinforces the role of discrimination as an important obstacle to health services and HIV testing. Thus, it is necessary to create and strengthen health policies and laws to protect TGW against discrimination, as well as to increase the equitable access of this population to public health services and HIV prevention and testing technologies.
Acknowledgements
The authors would like to express their gratitude to the study participants, the local teams that carried out the fieldwork in the three cities, and all collaborating NGOs. We are also grateful for the support of the Brazilian Ministry of Health through its Secretariat for Health Surveillance and its Department of Prevention, Surveillance and Control of Sexually Transmitted Infections, HIV/AIDS, and Viral Hepatitis. And the Coordination for the Improvement of Higher Education Personnel (CAPES- Brazil) for the master’s scholarship to BL (FINANCING CODE 001).
Abbreviations
- GBD
Gender-Based Discrimination
- HIV
Human Immunodeficiency Virus
- NGO
Non-Governmental Organizations
- NHPLGBT
National Health Policy for Lesbian, Gay, Bisexual, and Transgender people
- RDS
Respondent-Driven Sampling
- STI
Sexually Transmitted Infections
- WHO
World Health Organization
Authors’ contributions
All authors contributed to the concept of the paper and writing. BOL, DSM, LM, and ID were responsible for writing the final version of the manuscript and data analysis. FIB, CC, AB, MSC interpreted the results and revised the final version of the manuscript. All authors have read and approved the paper, have met the criteria for authorship as established by the International Committee of Medical Journal Editors, believe that the paper is an honest work, and can verify the validity of the results reported.
Funding
Brazilian Ministry of Health, through its Secretariat for Health Surveillance and its Department of Prevention, Surveillance and Control of Sexually Transmitted Infections, HIV/AIDS and Viral Hepatitis (Project 914BRZ1138 BRAZIL AIDS-SUS).
Availability of data and materials
The dataset analyzed that underlie the results reported in this article will be publicly available in the HAVARD Dataverse Repository immediately following publication.
Declarations
Ethics approval and consent to participate
The study protocol was submitted for review and approved by the Sergio Arouca National School of Public Health (ENSP/FIOCRUZ) Research Ethics Board (CAAE-49359415.9.0000.5240).
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Beo Oliveira Leite, Email: leitebeo@gmail.com.
Danielle Souto de Medeiros, Email: daniellesoutomedeiros@gmail.com.
Laio Magno, Email: laiomagnoss@gmail.com.
Francisco Inácio Bastos, Email: francisco.inacio.bastos@hotmail.com.
Carolina Coutinho, Email: coutinho.carol@gmail.com.
Ana Maria de Brito, Email: anabrito1009@gmail.com.
Maria Socorro Cavalcante, Email: socorro.cavalcante@gmail.com.
Inês Dourado, Email: ines.dourado@gmail.com.
References
- 1.Wang H, Wolock TM, Carter A, Nguyen G, Kyu HH, Gakidou E, et al. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the Global Burden of Disease Study 2015. Lancet HIV. 2016;3:e361–e387. doi: 10.1016/S2352-3018(16)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: A systematic review and meta-analysis. Lancet Infect Dis. 2013;13:214–222. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- 3.Joint United Nations Programme on HIV/AIDS (UNAIDS). 90–90–90: An Ambitious Treatment Target to Help End the AIDS Epidemic. Geneva, Switzerland: UNAIDS, 2014. Available at http://www.unaids.org/en/resources/909090. Accessed 27 Sept. 2019.
- 4.Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS 2020 Data. Geneva, Switzerland: UNAIDS, 2020. Available at https://www.unaids.org/en/resources/documents/2020/unaids-data. Accessed 27 Sept. 2019.
- 5.World Health Organization (WHO). HIV Prevention, Diagnosis, Treatment, and Care for Key Populations - 2016 Update. Geneva, Switzerland: WHO, 2018. Available at https://www.who.int/hiv/pub/guidelines/keypopulations-2016/en/. Accessed 27 Sept. 2019.
- 6.Fontanari AMV, Zanella GI, Feijó M, Churchill S, Rodrigues Lobato MI, Costa AB: HIV-related care for transgender people. A systematic review of studies from around the world. Social Science and Medicine 2019; 230:280–294. [DOI] [PubMed]
- 7.Magno L, Silva LAV da, Veras MA, Pereira-Santos M, Dourado I. Stigma and discrimination related to gender identity and vulnerability to HIV/AIDS among transgender women: a systematic review. Cad Saude Publica 2019; 35: e00112718. [DOI] [PubMed]
- 8.Monteiro S, Brigeiro M. Experiences of transgender women/transvestites with access to health services: progress, limits, and tensions. Cad Saude Publica 2019; 35: 35,e00111318. [DOI] [PubMed]
- 9.Rocon PC, Rodrigues A, Zamboni J, Pedrini MD. Difficulties experienced by trans people in accessing the Unified Health System. Cien Saude Colet. 2016;21:2517–2526. doi: 10.1590/1413-81232015218.14362015. [DOI] [PubMed] [Google Scholar]
- 10.Monteiro S, Brigeiro M, Barbosa RM. Transgender health and rights. Cad Saude Publica 2019; 35:e00047119. [DOI] [PubMed]
- 11.Bento B, Pelúcio L. Depathologization of the genre: the politicization of abject identities [Despatologização do gênero: a politização das identidades abjetas] Estud Fem. 2012;20:569–581. doi: 10.1590/S0104-026X2012000200017. [DOI] [Google Scholar]
- 12.Nascimento HM do, Sousa JA, Barros CR dos S. Health care for transvestites and transsexuals: a systematic literature review (2008–2017) [in Portuguese]. Rev Bras Estud da Homocultura 2019;1:40–58.
- 13.Logie CH, Lacombe-Duncan A, Wang Y, Jones N, Levermore K, Neil A, et al. Prevalence and Correlates of HIV Infection and HIV Testing among Transgender Women in Jamaica. AIDS Patient Care STDS. 2016;30:416–424. doi: 10.1089/apc.2016.0145. [DOI] [PubMed] [Google Scholar]
- 14.Pinheiro Júnior FML, Kendall C, Martins TA, Mota RMS, Macena RHM, Glick J, et al. Risk factors associated with resistance to HIV testing among transwomen in Brazil. AIDS Care. 2015;28:92–7. [DOI] [PubMed]
- 15.Bastos FI, Bastos LS, Coutinho C, Toledo L, Mota JC, Velasco-De-Castro CA, et al. HIV, HCV, HBV, and syphilis among transgender women from Brazil: Assessing different methods to adjust infection rates of a hard-to-reach, sparse population. Med. 2018;97:S16–S24. doi: 10.1097/MD.0000000000009447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heckathorn DD: Respondent-Driven Sampling. A New Approach to the Study of Hidden Populations. Soc Probl 1997; 44: 174–199.
- 17.Szwarcwald CL, De Souza Júnior PRB, Damacena GN, Junior AB, Kendall C. Analysis of data collected by RDS among sex workers in 10 Brazilian cities, 2009: Estimation of the prevalence of HIV, variance, and design effect. J Acquir Immune Defic Syndr. 2011;57:S129–S135. doi: 10.1097/QAI.0b013e31821e9a36. [DOI] [PubMed] [Google Scholar]
- 18.Volz E, Heckathorn D. Probability based estimation theory for respondent driven sampling. J Off Stat. 2008;24:79–97. [Google Scholar]
- 19.Rothman KJ, Greenland S, Associate TLL. Modern Epidemiology, 3st ed. Hastings Cent Rep, 2014.
- 20.Archer KJ, Lemeshow S. Goodness-of-fit test for a logistic regression model fitted using survey sample data. Stata J. 2006;6:97–105. doi: 10.1177/1536867X0600600106. [DOI] [Google Scholar]
- 21.Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. Am J Public Health. 2001;91:915–921. doi: 10.2105/AJPH.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Downing JM, Przedworski JM. Health of Transgender Adults in the U.S., 2014–2016. Am J Prev Med 2018; 55:336–344. [DOI] [PubMed]
- 23.Rocon PC, Wandekoken KD, de Barros MEB, Duarte MJO, Sodré F. Access to health by the transsexual population in brazil: between the lines of the integrative review [in Portuguese]. Trabalho, Educação e Saúde 2019, 18:e0023469.
- 24.da Silva ZP, de Almeida Ribeiro MCS, Barata RB, de Almeida MF. Socio-demographic profile and utilization patterns of the public healthcare system (SUS), 2003–2008 [in Portuguese] Cienc e Saude Coletiva. 2011;16:3807–3816. doi: 10.1590/S1413-81232011001000016. [DOI] [PubMed] [Google Scholar]
- 25.Brazil. Ministry of Health. Brazilian Institute of Geography and Statistics. National Health Survey 2013 [in Portuguese]. Brasília, Brazil, 2014.
- 26.Monteiro S, Brigeiro M. Experiences of transgender women/transvestites with access to health services: progress, limits, and tensions. Cad Saude Publica 2019; 35:e00111318. [DOI] [PubMed]
- 27.Rocon PC, Sodré F, Zamboni J, Rodrigues A, Roseiro MCFB. What trans people expect of the Brazilian National Health System? [in Portuguese] Interface Commun Heal Educ. 2018;22:43–53. [Google Scholar]
- 28.Poteat T, Reisner SL, Radix A. HIV epidemics among transgender women. Curr Opin HIV AIDS. 2014;9:168–173. doi: 10.1097/COH.0000000000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brazil. Health Surveillance Secretariat. Department of Chronic Conditions and Sexually Transmitted Infections. Clinical Protocol and Therapeutic Guidelines for Comprehensive Care for People with Sexually Transmitted Infections [in Portuguese]. Brasília, Brazil Brasília, Brazil, 2020.
- 30.Yi S, Sok S, Chhim S, Chhoun P, Chann N, Tuot S, et al. Access to community-based HIV services among transgender women in Cambodia: Findings from a national survey. Int J Equity Health. 2019;18:1–13. doi: 10.1186/s12939-019-0974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pawa D, Firestone R, Ratchasi S, Dowling O, Jittakoat Y, Duke A, et al. Reducing HIV risk among transgender women in Thailand: a quasi-experimental evaluation of the sisters program. PLoS One 2013; 8:e77113. [DOI] [PMC free article] [PubMed]
- 32.Silva-Santisteban A, Eng S, De La Iglesia G, Falistocco C, Mazin R. HIV prevention among transgender women in Latin America: Implementation, gaps and challenges. Vol. 19, Journal of the International AIDS Society. International AIDS Society 2016; 19:1–10. [DOI] [PMC free article] [PubMed]
- 33.Allin S, Masseria C, Sorenson C, Papanicolas I, Mossialos E. Measuring inequalities in access to health care. A review of the indices. London Sch Econ Polit Sci 2007; 1–24.
- 34.Zambenedetti G, da Silva RAN. Decentralization of health care to HIV-AIDS for primary care: tensions and potentialities [in Portuguese] Physis. 2016;26:785–806. doi: 10.1590/s0103-73312016000300005. [DOI] [Google Scholar]
- 35.Melo EA, Maksud I, Agostini R. HIV/Aids management at the primary care level in Brazil: a challenge for the Unified Health System? [in Portuguese]. Rev Panam Salud Pública 2018; 42:e151. [DOI] [PMC free article] [PubMed]
- 36.Kontomanolis EN, Michalopoulos S, Gkasdaris G, Fasoulakis Z. The social stigma of HIV-AIDS: Society’s role. HIV/AIDS - Res Palliat Care. 2017;9:111–118. doi: 10.2147/HIV.S129992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Romano VF. Transvestites in the Family Health Program of Lapa [in Portuguese] Saude E Soc. 2008;17:211–219. doi: 10.1590/S0104-12902008000200019. [DOI] [Google Scholar]
- 38.Magno L, Dourado I, Silva LAV da. Stigma and resistance among travestis and transsexual women in Salvador, Bahia State, Brazil [in Portuguese]. Cad Saude Publica 2018; 34:e00135917. [DOI] [PubMed]
- 39.Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: Results from the Virginia transgender health initiative study. Am J Public Health. 2013;103:1820–1829. doi: 10.2105/AJPH.2012.300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kenagy GP. Transgender health: Findings from two needs assessment studies in Philadelphia. Heal Soc Work. 2005;30:19–26. doi: 10.1093/hsw/30.1.19. [DOI] [PubMed] [Google Scholar]
- 41.Rachlin K, Green J, Lombardi E. Utilization of health care among female-to-male transgender individuals in the United States. J Homosex. 2008;54:243–258. doi: 10.1080/00918360801982124. [DOI] [PubMed] [Google Scholar]
- 42.Poteat T, German D, Kerrigan D. Managing uncertainty: A grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;84:22–29. doi: 10.1016/j.socscimed.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 43.Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, et al. Transgender people: health at the margins of society. Lancet. 2016;388:390–400. doi: 10.1016/S0140-6736(16)00683-8. [DOI] [PubMed] [Google Scholar]
- 44.Conron KJ, Scott G, Sterling Stowell G, Landers SJ. Transgender Health in Massachusetts: Results From a Household Probability Sample of Adults. Public Health. 2012;102:118–122. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Costa AB, Fontanari AMV, Catelan RF, Schwarz K, Stucky JL, da Rosa Filho HT, et al. HIV-Related Healthcare Needs and Access Barriers for Brazilian Transgender and Gender Diverse People. AIDS Behav. 2018;22:2534–2542. doi: 10.1007/s10461-017-2021-1. [DOI] [PubMed] [Google Scholar]
- 46.AIDS Care - Psychol Socio-Medical Asp AIDS/HIV 2016; 28:92–97.
- 47.Grinsztejn B, Jalil EM, Monteiro L, Velasque L, Moreira RI, Garcia ACF, et al. Unveiling of HIV dynamics among transgender women: a respondent-driven sampling study in Rio de Janeiro. Brazil Lancet HIV. 2017;4:e169–e176. doi: 10.1016/S2352-3018(17)30015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lippman SA, Moran L, Sevelius J, Castillo LS, Ventura A, Treves-Kagan S, et al. Acceptability and Feasibility of HIV Self-Testing Among Transgender Women in San Francisco: A Mixed Methods Pilot Study. AIDS Behav. 2016;20:928–938. doi: 10.1007/s10461-015-1236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schulden JD, Song B, Barros A, Mares-DelGrasso A, Martin CW, Ramirez R, et al. Rapid HIV testing in transgender communities by community-based organizations in three cities. Public Health Rep. 2008;123:101–114. doi: 10.1177/00333549081230S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee SW, Deiss RG, Segura ER, Clark JL, Lake JE, Konda KA, et al. A cross-sectional study of low HIV testing frequency and high-risk behaviour among men who have sex with men and transgender women in Lima. Peru BMC Public Health. 2015;15:1–8. doi: 10.1186/1471-2458-15-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: Findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDS. 2013;27:621–627. doi: 10.1089/apc.2013.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Woodford MR, Chakrapani V, Newman PA, Shunmugam M. Barriers and facilitators to voluntary HIV testing uptake among communities at high risk of HIV exposure in Chennai. India Glob Public Health. 2016;11:363–379. doi: 10.1080/17441692.2015.1057757. [DOI] [PubMed] [Google Scholar]
- 53.da Silva RGLB, Bezerra WC, de Queiroz SB. The impacts of transgender identities in sociability of travestis and transsexual women. Rev Ter Ocup da Univ São Paulo. 2015;26:364–372. doi: 10.11606/issn.2238-6149.v26i3p364-372. [DOI] [Google Scholar]
- 54.Radix AE, Lelutiu-Weinberger C, Gamarel KE. Satisfaction and healthcare utilization of transgender and gender non-conforming individuals in NYC: A community-based participatory study. LGBT Heal. 2014;1:302–308. doi: 10.1089/lgbt.2013.0042. [DOI] [PubMed] [Google Scholar]
- 55.Assis MMA, de Jesus WLA. Access to health services: approaches, concepts, policies and analysis model [in Portuguese] Cienc e Saude Coletiva. 2012;17:2865–2875. doi: 10.1590/S1413-81232012001100002. [DOI] [PubMed] [Google Scholar]
- 56.Martins TA, Kerr LRFS, MacEna RHM, Mota RS, Carneiro KL, Gondim RC, et al. Travestis, an unexplored population at risk of HIV in a large metropolis of northeast Brazil: A respondent-driven sampling survey. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2013;25:606–612. doi: 10.1080/09540121.2012.726342. [DOI] [PubMed] [Google Scholar]
- 57.Krüger A, Sperandei S, Bermudez XPCD, Merchán-Hamann E. Characteristics of hormone use by travestis and transgender women of the Brazilian Federal District. Rev Bras Epidemiol 2019; 22:e190004. [DOI] [PubMed]
- 58.Szwarcwald CL, Damacena GN, De Souza-Junior PRB, Guimarães MDC, De Almeida WDS, De Souza Ferreira AP, et al. Factors associated with HIV infection among female sex workers in Brazil. Med. 2018;97:S54–S61. doi: 10.1097/MD.0000000000009013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yi S, Ngin C, Tuot S, Chhoun P, Chhim S, Pal K, et al. HIV prevalence, risky behaviors, and discrimination experiences among transgender women in Cambodia: descriptive findings from a national integrated biological and behavioral survey. BMC Int Health Hum Rights. 2017;17:1–11. doi: 10.1186/s12914-017-0122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pager D. Measuring discrimination [in Portuguese] Tempo Soc. 2006;18:65–88. doi: 10.1590/S0103-20702006000200004. [DOI] [Google Scholar]
- 61.Bao A, Colby DJ, Trang T, Le BQ, Dinh TD, Nguyen QH, et al. Correlates of HIV Testing Among Transgender Women in Ho Chi Minh. Vietnam AIDS Behav. 2016;20:371–378. doi: 10.1007/s10461-016-1574-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed that underlie the results reported in this article will be publicly available in the HAVARD Dataverse Repository immediately following publication.