Abstract
Objective
To examine how the COVID-19 pandemic impacted use of home care services for individuals with dementia across service types and sociodemographic strata.
Design
Population-based time series analysis.
Setting and Participants
Community-dwelling adults with dementia in Ontario, Canada, from January 2019 to September 2020.
Methods
We used health administrative databases (Ontario Registered Persons Database and Home Care Database) to measure home care services used by participants. Poisson regression models were fit to compare weekly rates of home care services during the pandemic to historical trends with rate ratios (RRs) and 95% confidence intervals (CIs) stratified by service type (nursing, personal care, therapy), sex, rurality, and neighborhood income quintile.
Results
During the first wave of the pandemic, personal care fell by 16% compared to historical levels (RR 0.84, 95% CI 0.84, 0.85) and therapies fell by 50% (RR 0.50, 95% CI 0.48, 0.52), whereas nursing did not significantly decline (RR 1.02, 95% CI 1.00, 1.04). All rates had recovered by September 2020, with nursing and therapies higher than historical levels. Changes in services were largely consistent across sociodemographic strata, although the rural population experienced a larger decline in personal care and smaller rebound in nursing.
Conclusions and Implications
Personal care and therapies for individuals with dementia were interrupted during the early months of the pandemic, whereas nursing was only minimally impacted. Pandemic responses with the potential to disrupt home care for individuals living with dementia must balance the impacts on individuals with dementia, caregivers, and providers.
Keywords: Dementia, COVID-19, home care services, time series analysis
The COVID-19 pandemic disrupted health service delivery across health systems, particularly during the first months of local community transmission.1 Significant drops in the volume of ambulatory care occurred as services were canceled, delayed, or shifted to virtual settings to reduce the risk of COVID-19 transmission.2 , 3 Although some North American studies have shown that a number of the services that fell in the spring of 2020 had recovered by late summer and early fall, the recoveries were not necessarily equivalent across demographic and geographic groups.4 , 5
The disruption of health services can be particularly challenging for people living with dementia in the community, many of whom receive essential care from a variety of health care providers.6 Individuals with dementia in Ontario access a variety of different publicly provided home care services, including personal care, nursing, and various professional services such as physiotherapy and occupational therapy.7 Differences in the typical urgency of these services may have led to them being differentially affected by the pandemic. In addition, given evidence that the pandemic is exacerbating existing inequalities,8 , 9 it is important to examine whether the impact of the pandemic was distributed equally across sociodemographic dimensions.
The objective of this study was to investigate how the rates of home care services provided to community-dwelling adults living with dementia changed during the initial phases of the COVID-19 pandemic. Specifically, we examined rates of use across service types of personal care, nursing, and therapies and additionally examined whether the changes in rates were equivalent across strata defined by rurality, sex, and neighborhood income.
Methods
Study Design and Setting
We performed a population-based time series analysis of home care service use among community-dwelling adults with dementia in Ontario, Canada. Ontario is Canada’s most populous province with a population of nearly 15 million individuals.
Data Sources
Population-based health administrative databases were linked using unique encoded identifiers and analyzed at ICES. Databases used include the Ontario Registered Persons Database, used to identify participant demographics, and the Home Care Database, used to identify publicly funded home care services. The use of data in this project is authorized under section 45 of Ontario’s Personal Health Information Protection Act and does not require review by a Research Ethics Board.
Participants
We included all community-dwelling adults with dementia in Ontario aged 40 years and older who were eligible for Ontario’s publicly funded health insurance at the start of each week between January and September 2019 (historical period) and 2020 (pandemic period). Individuals with dementia were identified using a validated health data administrative algorithm.10 Eligibility was determined on a week-by-week basis, meaning that the participants were not a fixed cohort but could vary over time.
Measures
Home care services included personal care, nursing, and therapies (physiotherapy, occupational therapy, speech language therapy, nutritional therapy, and social work). Rates of weekly home care visits were calculated across 3 strata: sex, rurality (rural/urban), and neighborhood income quintile (Q1, lowest; Q5, highest). Rurality was defined by the Rurality Index of Ontario,11 with values higher than 40 considered rural, and neighborhood income quintile was defined using Statistics Canada census data.12 Sex, rurality, and income quintile were chosen as strata as they have been previously tied to inequalities in access to care that could be exacerbated by the pandemic.13 , 14
Analysis
We plotted the weekly rate of home care visits per 100 individuals, stratified by service type, sex, rurality, and neighborhood income quintile during both time periods. We used Poisson regression models with year as the sole independent variable to calculate rate ratios (RRs) and 95% confidence intervals (CIs) for each weekly rate in the pandemic period (2020) compared to the corresponding historical week (2019). Models were run overall and stratified by the selected sociodemographic variables. We reported RRs for the week with the lowest home care service rate in 2020 per strata, as well as the latest week in the analysis (end of September). Analyses were performed with SAS, version 9.4 (SAS Institute, Inc, Cary, NC).
Results
The number of community-dwelling adults with dementia was 131,466 as of the first week of March 2020 (and varied slightly from week to week across the time series). Persons with dementia had a median age of 80 years, 57.5% were female, and 9.2% resided in rural regions. The average rate of home care services per 100 individuals per week in 2019 was 13.1 for nursing, 179.7 for personal care, and 4.1 for therapies. Previous work indicates that individuals receiving nursing and therapies tend to be younger, have fewer functional and cognitive impairments, and more likely to be post-acute compared with patients receiving personal support.15
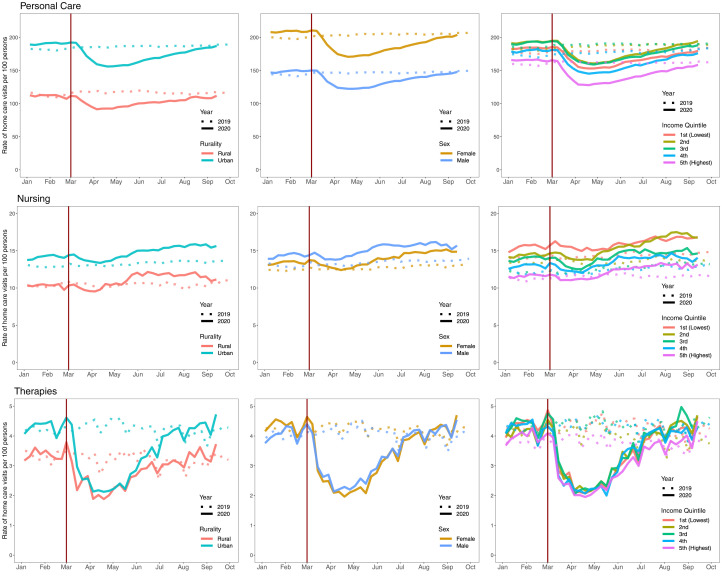
Time series plots indicate significant declines in personal care visits beginning in mid-March 2020 (Figure 1 ). At the lowest point, this corresponded to a 16% reduction (RR 0.84, 95% CI 0.84, 0.95) compared with the same week in 2019 (Table 1 ). By the end of September, the rate had recovered to the 2019 level (RR 0.99, 95% CI 0.99, 1.00) (Table 2 ). For reference, Ontario declared a state of emergency due to the COVID-19 pandemic on March 17, 2020,16 and nonessential businesses and workplaces were closed on March 24, 2020.17 A regional, graduated reopening began on June 12, 2020, and stretched across the summer.18 Individuals in rural areas experienced a slightly larger decline (RR 0.77, 95% CI 0.75, 0.79, vs urban 0.84, 95% CI 0.84, 0.85) but similar recovery. Those living in areas with the highest income (Q5) also experience larger initial declines.
Fig. 1.
Time series of home care visits for individuals living with dementia in the community, Ontario, Canada, January 2019 to September 2020.
Table 1.
Poisson Model Estimates of Home Care Service Rates in 2020 Compared to 2019 at Week of Lowest 2020 Rate Among Community-Dwelling Persons With Dementia in Ontario, Canada
| Sociodemographic Strata | At Week of Lowest Rate∗ |
||
|---|---|---|---|
| Personal Care, RR (95% CI) | Nursing, RR (95% CI) | Therapies, RR (95% CI) | |
| Overall | 0.84 (0.84, 0.85) | 1.02 (1.00, 1.04) | 0.50 (0.48, 0.52) |
| Rurality | |||
| Urban | 0.84 (0.84, 0.85) | 1.02 (1.00, 1.05) | 0.49 (0.47, 0.52) |
| Rural | 0.77 (0.75, 0.79) | 0.94 (0.87, 1.02) | 0.62 (0.52, 0.73) |
| Sex | |||
| Female | 0.84 (0.84, 0.85) | 0.99 (0.96, 1.02) | 0.45 (0.43, 0.48) |
| Male | 0.83 (0.82, 0.84) | 1.04 (1.01, 1.07) | 0.48 (0.45, 0.52) |
| Income quintile | |||
| First (lowest) | 0.85 (0.84, 0.86) | 1.05 (1.01, 1.10) | 0.50 (0.45, 0.55) |
| Second | 0.85 (0.84, 0.86) | 1.06 (1.02, 1.11) | 0.48 (0.44, 0.53) |
| Third | 0.84 (0.82, 0.85) | 1.02 (0.97, 1.07) | 0.45 (0.41, 0.50) |
| Fourth | 0.83 (0.82, 0.84) | 1.00 (0.95, 1.06) | 0.50 (0.44, 0.56) |
| Fifth (highest) | 0.79 (0.78, 0.81) | 0.94 (0.89, 0.99) | 0.51 (0.45, 0.57) |
Week of lowest rate in 2020 by strata compared to corresponding week in 2019.
Table 2.
Poisson Model Estimates of Home Care Service Rates in 2020 Compared With 2019 at Latest Week of Analysis Among Community-Dwelling Persons With Dementia in Ontario, Canada
| Sociodemographic Strata | At Latest Week∗ |
||
|---|---|---|---|
| Personal Support, RR (95% CI) | Nursing, RR (95% CI) | Therapies, RR (95% CI) | |
| Overall | 0.99 (0.99, 1.00) | 1.14 (1.11, 1.16) | 1.11 (1.07, 1.15) |
| Rurality | |||
| Urban | 0.99 (0.99, 1.00) | 1.15 (1.12, 1.17) | 1.11 (1.06, 1.15) |
| Rural | 0.97 (0.95, 0.99) | 0.99 (0.92, 1.07) | 1.10 (0.96, 1.26) |
| Sex | |||
| Female | 0.99 (0.98, 1.00) | 1.13 (1.10, 1.16) | 1.11 (1.06, 1.16) |
| Male | 0.99 (0.98, 1.00) | 1.14 (1.11, 1.18) | 1.10 (1.04, 1.16) |
| Income quintile | |||
| First (lowest) | 0.98 (0.97, 0.99) | 1.15 (1.10, 1.19) | 1.09 (1.01, 1.17) |
| Second | 1.03 (1.02, 1.05) | 1.21 (1.16, 1.26) | 1.18 (1.09, 1.28) |
| Third | 0.99 (0.98, 1.00) | 1.13 (1.08, 1.18) | 1.11 (1.02, 1.20) |
| Fourth | 0.96 (0.95, 0.98) | 1.06 (1.00, 1.11) | 1.00 (0.91, 1.09) |
| Fifth (highest) | 0.98 (0.97, 0.99) | 1.13 (1.07, 1.19) | 1.15 (1.05, 1.25) |
Week of September 20, 2020, vs week of September 22, 2019.
The trend for nursing visits appeared to dip slightly at the start of the pandemic but the lowest weekly rate in April 2020 was similar to that in 2019 (RR 1.02, 95% CI 1.00, 1.04). By the end of September 2020, the rate of nursing visits was 14% higher than 2019 (RR 1.14, 95% CI 1.11, 1.16). However, the rural population did not experience an increase in nursing visits in 2020 vs 2019 (RR 0.99, 95% CI 0.92, 1.07).
The rate of therapies declined dramatically through March and April 2020, reaching half of the level of 2019 (RR 0.50, 95% CI 0.48, 0.52). By the end of the September 2020, the overall rate was somewhat higher than that of 2019 (RR 1.11, 95% CI 1.07, 1.15). A full set of model results is available in Supplementary Table 1.
Discussion
Public home care services provided to community-dwelling adults living with dementia were interrupted during the first few months of the COVID-19 pandemic (March and April 2020) but recovered through the summer months and regained or exceeded historical levels by the end of September 2020. The degree of disruption varied by service type, with nursing declining only slightly, personal care declining by a moderate degree, and therapies declining by a larger degree. The disruptions were largely similar across strata defined by rurality, sex, and neighborhood income quintile, though individuals in rural areas experienced a larger decline in personal care and smaller rebound in nursing, and individuals in the highest income quintile experienced a larger initial decline in personal care.
Home care services are a critical component of the support system for adults with dementia in the community. Across Canada, home care services were restricted or reduced during the early months of the pandemic, particularly if they were deemed less essential.19 Home nursing in particular provides necessary care that would otherwise need to be received in other ambulatory care settings. Thus, nursing may have been considered more essential than personal care or therapies based on provincial guidelines that prioritized reducing direct impacts on safety and minimizing harms,20 explaining the differences we observed in our study. Services may also have been canceled directly by home care recipients or their caregivers over concerns regarding risk of COVID transmission.21 In addition, early in the pandemic, home care workers faced unsafe working conditions because of a lack of personal protective equipment and infection control guidance, which also may have led to cancelation of service.22 , 23
Regardless of the cause, any interruption to home care places additional burden on individuals with dementia and their caregivers. Personal care services assist an individual in the activities such as dressing, toileting, and transferring and if not provided by a home care worker would need to be provided by an unpaid caregiver. Increasing caregiver burden has been observed during the pandemic and linked to rising rates of distress and burnout.24 , 25 Although it may not be considered as essential as nursing, the loss of personal care can impact the safety of those needing care, increasing the risk of falls and injury. Additionally, loss of services may increase social isolation, which has been linked to new and worsening neuropsychiatric symptoms among individuals with dementia during the pandemic.26 Any policy or directive with the potential to disrupt home care services needs to consider the risks incurred by people with dementia, caregivers, and home care workers, all of whom may face additional burden and/or risk.
Although the impact of the pandemic across sociodemographic strata was generally consistent, rural areas experienced a greater decline in personal care and smaller rebound in nursing services. Residents in the wealthiest areas also had a larger initial decrease in personal care, which may be related to having additional options or resources to secure the necessary care. Equitable access to home care in rural areas has been previously identified as a challenge and any policy or directive that would disrupt home care services needs to ensure it will not exacerbate extant access issues.27 Future research should further examine the impact of the pandemic on individuals with dementia, including whether the interruption of home care services resulted in a downstream increase in emergency department visits or hospital admissions.
Limitations
Our data sources capture all publicly funded home care services in Ontario, but we do not have data on home care that is paid for privately. Also, we do not have information on the specific reasons why home care services were canceled or delayed. Finally, our study did not include a comparison group of older adults without dementia.
Conclusions and Implications
Home care services are an essential component of the support systems for adults living with dementia in the community. Although nursing care was largely uninterrupted during the COVID-19 pandemic, personal care and therapies declined dramatically during the early months, although service levels recovered by the end of September 2020. Pandemic responses that may interrupt home care services need to carefully consider the risks incurred by individuals with dementia, caregivers, and home care workers while not exacerbating existing inequities in access to care.
Footnotes
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This study also received funding from the Ontario Neurodegenerative Disease Research Initiative (ONDRI) through the Ontario Brain Institute, an independent nonprofit corporation funded partially by the Ontario government. A.J. was supported by a postdoctoral award from the Alzheimer’s Society of Canada. Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of CIHI. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. We thank IQVIA Solutions Canada Inc. for use of their Drug Information Database.
The authors declare no conflicts of interest.
Supplementary Data
Supplementary Table 1.
Full Poisson Model Results
| Rate Ratios (95% CIs) Comparing 2020 vs. 2019 |
||||
|---|---|---|---|---|
| At Week of Lowest Rate Between Mar 1 and Sep 20, 2020 |
At Latest Week (Week of Sep 20, 2020) |
|||
| B (95% CI) | P | B (95% CI) | P | |
| Overall | ||||
| Home care visits: nursing | 0.020 (0.000, 0.039) | .047 | 0.131 (0.104, 0.148) | <.001 |
| Home care visits: personal support | −0.174 (–0.174, −0.163) | <.001 | −0.010 (–0.010, 0.000) | .004 |
| Home care visits: therapy | −0.693 (–0.734, −0.654) | <.001 | 0.104 (0.068, 0.140) | <.001 |
| Strata: female | ||||
| Home care visits: nursing | −0.010 (–0.041, 0.020) | .47 | 0.122 (0.095, 0.148) | <.001 |
| Home care visits: personal support | −0.174 (–0.174, −0.163) | <.001 | −0.010 (–0.020, 0.000) | .006 |
| Home care visits: therapy | −0.799 (–0.844, −0.734) | <.001 | 0.104 (0.058, 0.148) | <.001 |
| Strata: male | ||||
| Home care visits: nursing | 0.039 (0.010, 0.068) | .014 | 0.131 (0.104, 0.166) | <.001 |
| Home care visits: personal support | −0.186 (–0.198, −0.174) | <.001 | −0.010 (–0.020, 0.000) | .10 |
| Home care visits: therapy | −0.734 (–0.799, −0.654) | <.001 | 0.095 (0.039, 0.148) | .001 |
| Strata: income quintile 1 (lowest) | ||||
| Home care visits: nursing | 0.049 (0.010, 0.095) | .018 | 0.140 (0.095, 0.174) | <.001 |
| Home care visits: personal support | −0.163 (–0.174, −0.151) | <.001 | −0.020 (–0.030, −0.010) | .003 |
| Home care visits: therapy | −0.693 (–0.799, −0.598) | <.001 | 0.086 (0.010, 0.157) | .024 |
| Strata: income quintile 2 | ||||
| Home care visits: nursing | 0.058 (0.020, 0.104) | .007 | 0.191 (0.148, 0.231) | <.001 |
| Home care visits: personal support | −0.163 (–0.174, −0.151) | <.001 | 0.030 (0.020, 0.049) | <.001 |
| Home care visits: therapy | −0.734 (–0.821, −0.635) | <.001 | 0.166 (0.086, 0.247) | <.001 |
| Strata: income quintile 3 | ||||
| Home care visits: nursing | 0.020 (–0.030, 0.068) | .51 | 0.122 (0.077, 0.166) | <.001 |
| Home care visits: personal support | −0.174 (–0.198, −0.163) | <.001 | −0.010 (–0.020, 0.000) | .07 |
| Home care visits: therapy | −0.799 (–0.892, −0.693) | <.001 | 0.104 (0.020, 0.182) | .011 |
| Strata: income quintile 4 | ||||
| Home care visits: nursing | 0.000 (–0.051, 0.058) | .96 | 0.058 (0.000, 0.104) | .034 |
| Home care visits: personal support | −0.186 (–0.198, −0.174) | <.001 | −0.041 (–0.051, −0.020) | <.001 |
| Home care visits: therapy | −0.693 (–0.821, −0.580) | <.001 | 0.000 (–0.094, 0.086) | .94 |
| Strata: income quintile 5 (highest) | ||||
| Home care visits: nursing | −0.062 (–0.117, −0.010) | .014 | 0.122 (0.068, 0.174) | <.001 |
| Home care visits: personal support | −0.236 (–0.248, −0.211) | <.001 | −0.020 (–0.030, −0.010) | .007 |
| Home care visits: therapy | −0.673 (–0.799, −0.562) | <.001 | 0.140 (0.049, 0.223) | .002 |
| Strata: urban | ||||
| Home care visits: nursing | 0.020 (0.000, 0.049) | .032 | 0.140 (0.113, 0.157) | <.001 |
| Home care visits: personal support | −0.174 (–0.174, −0.163) | <.001 | −0.010 (–0.010, 0.000) | .015 |
| Home care visits: therapy | −0.713 (–0.755, −0.654) | <.001 | 0.104 (0.058, 0.140) | <.001 |
| Strata: rural | ||||
| Home care visits: nursing | −0.062 (–0.139, 0.020) | .13 | −0.010 (–0.083, 0.068) | .87 |
| Home care visits: personal support | −0.261 (–0.288, −0.236) | <.001 | −0.030 (–0.051, −0.010) | .010 |
| Home care visits: therapy | −0.478 (–0.654, −0.315) | <.001 | 0.095 (–0.041, 0.231) | .15 |
References
- 1.Canadian Institute for Health Information Impact of COVID-19 on Canada’s health care systems. https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems Available at:
- 2.Glazier R.H., Green M.E., Wu F.C., et al. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193:E200–E210. doi: 10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whaley C.M., Pera M.F., Cantor J., et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2024984. doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birkmeyer J.D., Barnato A., Birkmeyer N., et al. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood) 2020;39:2010–2017. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chatterji P., Li Y. Effects of the COVID-19 pandemic on outpatient providers in the United States. Med Care. 2021;59:58–61. doi: 10.1097/MLR.0000000000001448. [DOI] [PubMed] [Google Scholar]
- 6.Bronskill S.E., Maclagan L.C., Walker J.D., et al. Trajectories of health system use and survival for community-dwelling persons with dementia: A cohort study. BMJ Open. 2020;10:e037485. doi: 10.1136/bmjopen-2020-037485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government of Ontario Home and community care. Ontario.ca. https://www.ontario.ca/page/homecare-seniors#section-3 Available at:
- 8.Topriceanu C.C., Wong A., Moon J.C., et al. Evaluating access to health and care services during lockdown by the COVID-19 survey in five UK national longitudinal studies. BMJ Open. 2021;11:e045813. doi: 10.1136/bmjopen-2020-045813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dorn A. van, Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jaakkimainen R.L., Bronskill S.E., Tierney M.C., et al. Identification of physician-diagnosed Alzheimer’s disease and related dementias in population-based administrative data: A validation study using family physicians’ electronic medical records. J Alzheimers Dis. 2016;54:337–349. doi: 10.3233/JAD-160105. [DOI] [PubMed] [Google Scholar]
- 11.Kralj B. Measuring Rurality - RIO2008_BASIC: Methodology and Results. Toronto: Ontario Medical Association. https://docplayer.net/91599736-Measuring-rurality-rio2008_basic-methodology-and-results.html Available at: Published 2009. Accessed April 20, 2021.
- 12.Statistics Canada Postal Code Conversion File Plus (PCCF+) Version 6C, Reference Guide. https://mdl.library.utoronto.ca/sites/default/public/mdldata/open/canada/national/statcan/postalcodes/pccfplus/2011/2015aug/82-F0086-XDB-2016v6c-eng.pdf Available at: Published 2016. Accessed May 4, 2021.
- 13.Sourial N., Arsenault-Lapierre G., Margo-Dermer E., et al. Sex differences in the management of persons with dementia following a subnational primary care policy intervention. Int J Equity Health. 2020;19:175. doi: 10.1186/s12939-020-01285-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bainbridge D., Seow H., Sussman J., et al. Factors associated with not receiving homecare, end-of-life homecare, or early homecare referral among cancer decedents: A population-based cohort study. Health Policy. 2015;119:831–839. doi: 10.1016/j.healthpol.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 15.Jones A., Schumacher C., Bronskill S.E., et al. The association between home care visits and same-day emergency department use: A case–crossover study. CMAJ. 2018;190:E525–E531. doi: 10.1503/cmaj.170892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Government of Ontario Archived - COVID-19: Government service changes and public closures. https://www.ontario.ca/page/covid-19-government-service-changes-and-public-closures Available at:
- 17.Ontario orders the mandatory closure of all non-essential workplaces to fight spread of COVID-19. news.ontario.ca. https://news.ontario.ca/en/release/56435/ontario-orders-the-mandatory-closure-of-all-non-essential-workplaces-to-fight-spread-of-covid-19 Available at:
- 18.Ontario permits more businesses and services to reopen in the coming days. news.ontario.ca. https://news.ontario.ca/en/release/57132/ontario-permits-more-businesses-and-services-to-reopen-in-the-coming-days Available at:
- 19.Bielska I.A., Embrett M., Jewett L., et al. Canada’s multi-jurisdictional COVID-19 Public Health response – January to May 2020. Zdr Publiczne Zarządzanie. 2020;2020:88–105. [Google Scholar]
- 20.Chief Medical Officer of Health Directive #2 for health care providers (regulated health professionals or persons who operate a group practice of regulated health professionals). Toronto, Canada. https://www.crpo.ca/wp-content/uploads/2020/03/CMOH-Directive-2-RHPA-professionals-2020-03-19.pdf Available at:
- 21.Giebel C., Hanna K., Cannon J., et al. Decision-making for receiving paid home care for dementia in the time of COVID-19: a qualitative study. BMC Geriatr. 2020;20:333. doi: 10.1186/s12877-020-01719-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rowe T.A., Patel M., O’Conor R., et al. COVID-19 exposures and infection control among home care agencies. Arch Gerontol Geriatr. 2020;91:104214. doi: 10.1016/j.archger.2020.104214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sterling M.R., Tseng E., Poon A., et al. Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: A qualitative analysis. JAMA Intern Med. 2020;180:1453–1459. doi: 10.1001/jamainternmed.2020.3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Budnick A., Hering C., Eggert S., et al. Informal caregivers during the COVID-19 pandemic perceive additional burden: Findings from an ad-hoc survey in Germany. BMC Health Serv Res. 2021;21:353. doi: 10.1186/s12913-021-06359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen S.A., Kunicki Z.J., Drohan M.M., et al. Exploring changes in caregiver burden and caregiving intensity due to COVID-19. Gerontol Geriatr Med. 2021 Feb 26;7 doi: 10.1177/2333721421999279. 2333721421999279. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manca R., De Marco M., Venneri A. The impact of COVID-19 infection and enforced prolonged social isolation on neuropsychiatric symptoms in older adults with and without dementia: A review. Front Psychiatry. 2020;11:585540. doi: 10.3389/fpsyt.2020.585540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forbes D.A., Edge D.S. Canadian home care policy and practice in rural and remote settings: Challenges and solutions. J Agromed. 2009;14:119–124. doi: 10.1080/10599240902724135. [DOI] [PubMed] [Google Scholar]